Abstract
Purpose
Implementing early mobilisation in intensive care is challenging, and a detailed knowledge of factors that may hinder or facilitate implementation is essential for success. The study was done to explore the perceived barriers and facilitators to early mobilisation by physiotherapists in Zimbabwean and South African public sector hospital ICUs.
Methods
A qualitative study was done in eight public sector hospitals from South Africa and four hospitals from Zimbabwe. Physiotherapists from the participating hospitals who had at least two years working experience in ICU were invited to participate in semi-structured, in-depth, face-to-face interviews. Purposive sampling was done. Data collected included interpretation of early mobilisation, perceived barriers, and facilitators to early mobilisation. Data analysis was done using the content analysis method.
Findings
A total of 22 physiotherapists were interviewed. In defining the activities regarded as early mobilisation, there was diversity in relation to the specific activities and the nature of the patients in which the defined activities were suitable for. Perceived barriers which emerged included lack of professional autonomy or boundaries, motivation, and clinical skills. Perceived facilitators to early mobilisation included the availability of guidelines, good communication, adequate staff, and mobilisation equipment.
Conclusions
Barriers and facilitators to early mobilisation are multifactorial. There is need for multidisciplinary team collaboration and planning before implementing early mobilisation activities.
Keywords: Mobilisation, physiotherapy, barriers, facilitators, critically ill
Introduction
Critical care service provision in low and middle income countries in the public healthcare sector is often challenged by restricted availability of equipment, shortage of staff, and the limited number of and high demand for intensive care unit (ICU) beds [1]. The burden of ICU admissions is further increased by the high prevalence of human immunodeficiency virus (HIV), tuberculosis (TB), and malaria, with more than 80% of the population being served by the public healthcare sector [2].
The focus of critical care medicine has traditionally been on the restoration of physiological function, hemodynamic stability, and prevention of death through bed rest and sedation [3,4]. However, such interventions are associated with ICU delirium, impaired exercise capacity, poorer functional outcomes, and quality of life observed in patients after discharge [5]. Consequently, the focus of research has shifted to the implementation of early mobilisation and rehabilitation to become standard practice in the management of critically ill patients on a global level [5]. Evidence supports the use of early mobilisation of patients in ICUs as it is shown to be feasible, safe, and associated with improved clinical outcomes. These include improvements in peripheral and respiratory muscle strength, reductions in shortness of breath, shorter durations of delirium spells and more ventilator-free days, improved functional recovery within the hospital setting, improved walking distance at hospital discharge, reduced length of hospital stay and lastly, improvements in patients’ quality of life after hospital discharge [3,6–9].
Despite the positive body of evidence on early mobilisation, translation of research evidence into clinical practice has been slow [10]. Globally, a low proportion of patients (10–30%) are being mobilised out of bed, especially among those who are mechanically ventilated [11–16]. The evidence-practice gap might be the reason why early mobilisation is not frequently practiced in several units around the world, especially in the case of mechanically ventilated patients. The reasons why there are an increase in the evidence-practice gap when it comes to early mobilisation of ICU patients is poorly understood, especially in public healthcare sectors in low- and middle-income countries. Understanding whether and how the early mobilisation of patients in ICUs is currently performed by physiotherapists or any other member of the ICU team is critical to the design and implementation of strategies to improve on its application in the diverse population of critically ill patients in ICUs [17,18]. Implementing early mobilisation in intensive care is challenging, and a detailed knowledge of factors that may hinder or facilitate implementation is essential for success [19]. The strategies used to bridge the evidence-practice gap include the active identification of perceived barriers and facilitators to early mobilisation which exist in each unit. This study was done to explore the perceptions of physiotherapists regarding early mobilisation practices in ICUs in relation to the perceived barriers and facilitators experienced in Zimbabwean and South African public sector hospital ICUs.
Study design
A qualitative study design was used. This work is part of a larger study describing the early mobilisation practices in Zimbabwean and South African public sector ICUs [20,21].
Study setting
The study was conducted in public sector hospitals: four in Zimbabwe (ZM) and eight in South Africa (SA). All the units in ZM are mixed ICUs, admitting both medical and surgical patients. The units have a low bed capacity, ranging from 6 to 10 beds per unit, resulting in high demands for ICU beds in all the hospitals. In SA, most hospitals have specialised ICUs, some with more than one unit. The bed capacity varies, ranging from 4 to 24 beds.
The physiotherapy (PT) coverage in ICU in the two countries also varies, with units being covered by at least one physiotherapist at a time. Physiotherapists from ZM and SA have first contact status. This means that patients can have access to health care primarily through a physiotherapist without requiring a referral from a general practitioner or physician. However, the practices in ICU differ across the hospitals in the two countries. In some units, physiotherapists only treat patients who have been referred by the attending general practitioner or physician; in others, physiotherapists treat any patient requiring treatment based on their own assessment.
Sampling and study participants
Physiotherapists who worked in the public sector hospital ICUs and participated in the previous quantitative surveys [20,21], were invited to participate in semi-structured, in-depth, face-to-face interviews. A non-probability purposive sampling technique was used to select the participating hospitals and ICUs. Sampling included hospitals from different provinces and different ICUs in hospitals in SA and Zimbabwe. Criteria for inclusion of physiotherapists were: (1) having worked in ICUs in public sector hospitals for at least two years; (2) currently working in at least one of the adult ICUs in public sector hospitals; (3) having had experience of performing early mobilisation with patients in ICU.
Semi-structured interview guide
A semi-structured interview guide was developed based on the available literature on early mobilisation practices in ICU (Web Appendix A). Questions included: perception and attitude towards early mobilisation; knowledge about early mobilisation in the ICU; benefits of early mobilisation to the patients and the hospital; perceived barriers and facilitators to early mobilisation; and recommendations to improve the implementation and execution of early mobilisation programmes in ICUs in public sector hospitals. The interview guide was sent to two experts in the field of ICU and qualitative research, for content and face validation.
Data collection
At each hospital, a quantitative survey was conducted prior to this qualitative study. This allowed the researchers extended exposure to the context and time to establish rapport with the participants before conducting the face-to-face interviews. The time and the specific venue were set with each participant. The interviews were conducted in English in both countries as all participants were able to speak and understand English. The interviews were conducted within the hospital setting in a place that was convenient for each interviewee. The interviews lasted between 20 and 55 min. Additional issues (not in the interview guide) that were raised by some participants during the interviews allowed the researcher to explore a wide range of topics, which were further developed in subsequent interviews with other participants. Participants were encouraged to talk frankly and were assured that their responses would be anonymised. The interview sessions were audio recorded using Livescribe 4GB Echo Smartpen. Interviews were conducted until saturation level of the information was reached.
There are four components to trustworthiness in qualitative research; credibility, transferability, dependability, and confirmability [22]. Credibility was assured based on the researcher’s: (1) familiarity with the role of PT in the ICU, (2) knowledge and experience in the area of early mobilisation, and (3) request for frankness. In addition, the transcript analysis was reviewed by a more experienced researcher, and by five physiotherapists who had participated in the interviews. Transferability was ensured by providing a detailed description of the study setting and the working conditions of the physiotherapists. Dependability was ensured by a detailed description of the study methodology. Confirmability was ensured through record keeping and by using physiotherapists working in different types of ICUs and from different regions to provide a coherent and deeper perspective.
Analysis
One member of the study team transcribed verbatim the audio-recorded interviews and reviewed the transcripts for consistency and accuracy, using the content analysis method which focuses on systematically organising data into a structured format [23,24]. Content analysis aims to attain a condensed and broad description of the phenomenon with the outcome of the analysis being concepts or categories describing the phenomenon [25]. The theoretical domains framework (TDF) was used to analyse the perceived barriers and facilitators [26]. The content analysis was performed by classifying quotes into the relevant TDF domains and then summarising quotes under corresponding domains into barriers and facilitators. The naming of the barriers and facilitators was guided by the theoretical constructs associated with each domain of the TDF [26,27]. The TDF was initially developed for implementation research to identify influences on health professional behaviour related to implementation of evidence based recommendations [26].
Two members of the study team were independently involved in the coding (CT and HvA) as the latter had experience in critical care and qualitative research. One member with expertise in qualitative research and analysis (VN) was responsible for the verification and validation of the codes from the two encoders. The researchers used ATLAS.ti® v.8.4.15 Scientific Software Development GmbH (Berlin, Germany) to undertake organisation and analysis of the data. Descriptive statistics were used to summarise participants’ demographic and clinical profiles.
Ethical considerations
All ethical principles according to the Declaration of Helsinki were followed [28,29]. Prior to the commencement of the study, written institutional approval was obtained from the review boards of all government hospitals in Zimbabwe. For the hospitals in SA, permission was obtained from the Provincial Departments of Health through the online submission system. The study was registered on the National Health Research Database website (https://nhrd.hst.org.za/). Permission to conduct the study was obtained from the Joint Research Ethics Committee for University of Zimbabwe College of Health Sciences and Parirenyatwa Group of Hospitals (JREC REF: 377/15), Medical Research Council of Zimbabwe (MRCZ/A/2040), and the University of the Witwatersrand Human Research Ethics Committee (Medical) (REF: M150927) in SA. Informed written consent was obtained from the participants. To ensure confidentiality, participant code numbers were used.
Findings
Description of the participants
A total of 22 physiotherapists were interviewed; four participants were from four ICUs in four Zimbabwean hospitals and 18 participants were from 18 ICUs in eight of the hospitals in SA. The majority of participants were women (n = 14, 63.4%). ICU bed capacity was on average greater in SA than in Zimbabwe. Participants from both countries mostly worked in mixed medical and surgical ICUs (Table 1).
Table 1.
Description of study participants and Intensive Care Units in which they work in Zimbabwe and South Africa
| Characteristics | Zimbabwe (n=4) | SA (n=18) |
|---|---|---|
| Women, n | 2 | 14 |
| Experience in physiotherapy, (years) (median (IQR)) | 5.5 (2–9) | 9 (7–10) |
| ICU experience, years (median (IQR)) | 3.5 (2.5–6.5) | 7.5 (6–8) |
| ICU capacity, beds (median (IQR)) | 7.5 (6–9) | 9 (8–13) |
| Physiotherapists in a unit, median (IQR) | 1.5 (1–2) | 2 (1–3) |
| Type of ICUs Physiotherapists worked in, n | ||
| Mixed medical & surgical | 4 | 8 |
| Neurosurgical | 2 | |
| Trauma | 2 | |
| Cardiothoracic | 1 | |
| Medical | 1 | |
| General ICU and Trauma ICU | 4 |
Factors influencing implementation of early mobilisation in SA and Zimbabwean government hospitals
A total of 23 barriers and 12 facilitators were identified from the in-depth interviews. The perceived barriers were classified into seven relevant TDF domains whilst the perceived facilitators were classified into six domains (Table 2).
Table 2.
Identified barriers and facilitators to early mobilisation of ICU patients in the various domains of TDF
| Domain | Barrier | Facilitator |
|---|---|---|
| 1. Knowledge (An awareness of the existence of something) |
1.Awareness programmes | |
| 2. Skills (An ability or proficiency acquired through practice) |
1.Lack of experience | |
| 3. Social/professional role and identity (A coherent set of behaviours and displayed personal qualities of an individual in a social or work setting) |
2.Undefined roles 3.Resistance from nursing staff 4.Lack of clarity 5.Unaccountability |
2.Good communication 3.Respect teamwork |
| 4. Beliefs about capabilities (Acceptance of the truth, reality or validity about an ability, talent or facility that a person can put to constructive use) | ||
| 5. Optimism (The confidence that things will happen for the best or that desired goals will be attained) |
||
| 6. Beliefs about Consequences (Acceptance of the truth, reality, or validity about outcomes of a behaviour in a given situation) | 6.Haemodynamic instability 7.Raised intracranial pressure 8.Low platelet count 9.Mental instability |
|
| 7. Reinforcement (Increasing the probability of a response by arranging a dependent relationship, or contingency, between the response and a given stimulus) |
||
| 8. Intentions (A conscious decision to perform a behaviour or a resolve to act in a certain way) |
10.Lack of motivation 11.Inadequate remuneration |
|
| 9. Goals (Mental representations of outcomes or end states that an individual wants to achieve) |
12.Low prioritisation 13.Patient too sick for mobilisation |
4.Stability of the patient |
| 10. Memory, attention and decision processes (The ability to retain information, focus selectively on aspects of the environment and choose between two or more alternatives) |
||
| 11. Environmental context and resources (Any circumstance of a person’s situation or environment that discourages or encourages the development of skills and abilities, independence, social competence and adaptive behaviour) | 14.Lack of appropriate equipment 15.Inadequate human resources 16.Multiple patient attachments 17.Length of attachments 18.Location of the attachments |
5.Availability of standard operational procedures 6.Adjustable electrical beds 7.Space availability 8.Use of sedation scales 9.Reduction in sedation 10.Increase in number of Physiotherapists in unit |
| 12. Social influences (Those interpersonal processes that can cause individuals to change their thoughts, feelings, or behaviours) |
11.Standard of care | |
| 13. Emotion (A complex reaction pattern, involving experiential, behavioural, and physiological elements, by which the individual attempts to deal with a personally significant matter or event) |
||
| 14. Behavioural regulation (Anything aimed at managing or changing objectively observed or measured actions) | 19.Inconsistent patient referrals 20.Delayed specialist consultations 21.Delayed investigations 22.Reshuffling of the physiotherapist (unsustainability) 23.Discord between team members |
12.Non rotational physiotherapy coverage |
| 10. Memory, attention and decision processes (The ability to retain information, focus selectively on aspects of the environment and choose between two or more alternatives) |
||
| 11. Environmental context and resources (Any circumstance of a person’s situation or environment that discourages or encourages the development of skills and abilities, independence, social competence and adaptive behaviour) | 14.Lack of appropriate equipment 15.Inadequate human resources 16.Multiple patient attachments 17.Length of attachments 18.Location of the attachments |
5.Availability of standard operational procedures 6.Adjustable electrical beds 7.Space availability 8.Use of sedation scales 9.Reduction in sedation 10.Increase in number of Physiotherapists in unit |
| 12. Social influences (Those interpersonal processes that can cause individuals to change their thoughts, feelings, or behaviours) |
11.Standard of care | |
| 13. Emotion (A complex reaction pattern, involving experiential, behavioural, and physiological elements, by which the individual attempts to deal with a personally significant matter or event) |
||
| 14. Behavioural regulation (Anything aimed at managing or changing objectively observed or measured actions) | 19.Inconsistent patient referrals 20.Delayed specialist consultations 21.Delayed investigations 22.Reshuffling of the physiotherapist (unsustainability) 23.Discord between team members |
12.Non rotational physiotherapy coverage |
Interpretation of early mobilisation
The participants were asked to explain what they understood by the term “early mobilisation”. The two themes which emerged in relation to how participants interpreted early mobilisation included “procedural knowledge” and “social influences” (Figure 1).
Figure 1:
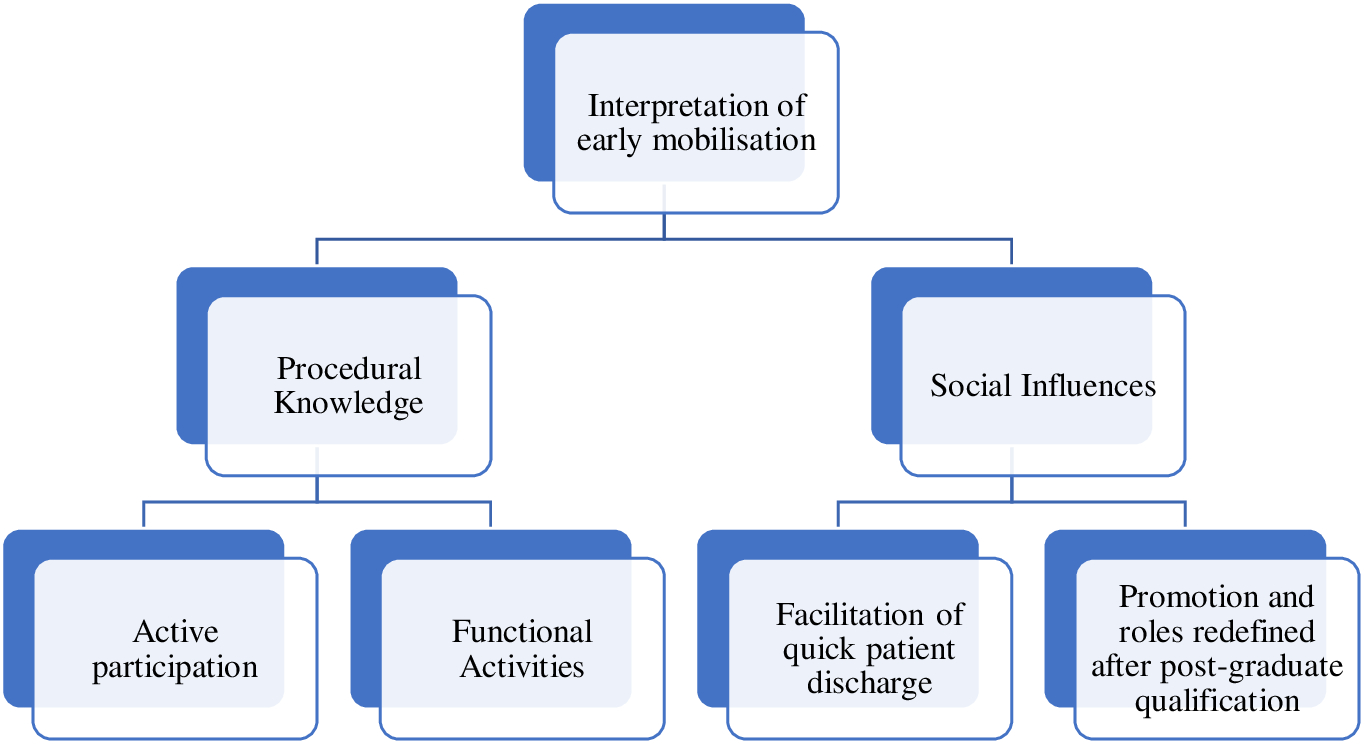
Interpretation of early mobilisation by physiotherapists from SA and Zimbabwean government hospitals.
Procedural knowledge
Active participation
Participants from both countries felt that the early mobilisation activities should be done progressively and as early as possible, depending on the patient’s condition. They felt that the patient should be able to participate actively for the exercise to be beneficial. Some participants felt that early mobilisation incorporated both active and passive activities. Passive movements alone were not regarded as part of early mobilisation as reported below:
I think the patient should be able to participate in the mobilisation, uh… it shouldn’t be a complete passive endeavour or a passive procedure, uh …, the patient should actively participate in it, otherwise I feel like that there won’t be as much benefit, that is in terms of mobilisation out-of-bed … SA001:7 years physiotherapy (PT) experience
Functional activities
The participants felt that early mobilisation performed by physiotherapists incorporates functional activities to get the patient active. Early mobilisation of patients was understood to include first sitting the patient up in bed unsupported, then later incorporating sitting with other activities:
… in terms of physiotherapy mobilisation, we (physiotherapists) try to do lots of functional activities and try to incorporate lots of exercise therapy in the mobilisation, so you try to do some sit-to-stand, marching on the spot, stretches and strengthening exercises, then mobilise the patient to a chair… SA006:9 years PT experience
Social influences
There were interpersonal processes that can cause individuals to change their thoughts, feelings, or behaviour that were highlighted to affect implementation of early mobilisation of the patients. In ICUs with limited bed capacity but catering for a large population group, early mobilisation was important to quickly stabilise and discharge patients to free up beds for new patients. One participant commented:
… our ICU is a provincial ICU and we cater for the whole province and it is a four-bed ICU, so usually we want the patients to stabilise early so that they can be discharged early for us to receive other new patients. ZM005: 2 years PT experience
The participants felt that a postgraduate qualification in PT was not valued as there was no difference in clinical roles, which affects the implementation of early mobilisation in the units, as reported in one interview:
Right now, even furthering your education by getting a Masters or a PhD is not of any benefit because it does not change your duties in the hospital setting, so in the end, people are not keen to pursue their studies… ZM007: 4 years PT experience
Barriers to early mobilisation resulting in variability in clinical practice
Social/professional roles and identity
Some participants highlighted the issue of undefined roles within the ICU team during the implementation of early patient mobilisation. Participants felt that it was not clear who had the authority to prescribe early mobilisation activities for patients in the ICU. Participants who had recommended early mobilisation reported experiencing resistance from the nursing staff:
…even if you want to mobilise the patient, they will (nurses) ask you if that is what the doctor (general practitioner/physician) has recommended for that patient. If the answer is “yes”, they (nurses) are most likely to be cooperative but if that is not the doctor’s (general practitioner/physician) order then they are not keen to assist you on mobilisation… ZM012: 7 years PT experience
Participants reported a lack of clarity regarding which profession would be held accountable (accountability) for returning the patient to bed after he/she had been sitting in a chair:
So, the question will remain to say, whose responsibility is it to take the patient back to the bed after mobilisation because I have other wards to go to. Therefore, I cannot spend most of my time in ICU waiting to take the patient back to bed … SA003:2 years PT experience
Intentions
Participants from Zimbabwean and SA ICUs described alack of motivation among physiotherapists as a reason to discourage early mobilisation. This could result in delays in implementing early mobilisation activities in eligible patients or the selection of in-bed activities in patients who cannot participate in out-of-bed activities.
Motivation to do the job is the main problem. Even if you are attending to a patient who is now stable and recovering well, the type of patients you can do quite a number of sessions with, but you are just de-motivated and do not have time to do that, so you just tell yourself that you will attend to the patient when she/he is discharged to the ward… ZM007:4 years PT experience
Inadequate remuneration was highlighted as a factor affecting motivation of the physiotherapists to mobilise patients in ICU as reported below:
… because of the salaries. So I find that they will do the least amount of work possible. So people clearly say that I am not doing that because the government does not pay me enough. SA013:15 years PT experience
Goals
Some participants suggested that clinicians do not generally regard early mobilisation as a treatment option when a patient has been referred for chest PT. As a result, such interventions in ICUs are low on the prioritisation list as shown below:
In my unit [neurosurgical ICU], I think the priority now is their chest, I think the respiratory system is more important than anything else … not that I am going to completely ignore mobilisation, I do mobilise but that is not my priority, my priority is the chest … SA002:2 years PT experience
Some SA participants felt that certain types of patients in ICU should not participate in high levels of mobilisation, as these were regarded as too intense owing to the nature of their illness (too sick for mobilisation):
As for having a walking frame in the unit, it [just] doesn’t get there in the ICU [neurosurgical]. Usually, when I can just get them to sit, it’s when they are stable and they [doctors (general practitioner/physician)] can extubate them … SA002: 2 years PT experience
Skills
Another issue affecting the level of early mobilisation is the lack of experience of the ICU physiotherapists. Participants felt that there was a wide range of clinical reasoning skills among ICU physiotherapists, directly related to their level of experience. In the absence of a screening guideline, which might increase the level of early mobilisation, physiotherapists have to rely on the skills that they have developed through their own experience.
… because you will see that it comes with the therapist’s years of experience, someone who recently graduated will not feel comfortable to mobilise a patient, especially during the acute phase, but for someone with more years of experience, they are not reluctant to mobilise the patient even when on a mechanical ventilator. SA004: 11 years PT experience
Behavioural regulation
Participants highlighted the importance of referrals of patients for early mobilisation. At present, there is highly inconsistent referrals in some units, in which physiotherapists treat only those patients referred to them by the attending doctor (general practitioner/physician). However, participants reported that some doctors (general practitioner/physician) never specifically request early mobilisation activities for patients:
… because we do work on referrals based on ward rounds, our ICU … it’s not blanket cover; so we do not see every patient every day. Also, chest is the priority in our ICU setting and our doctors (general practitioner/physician) usually request specifically for chest physiotherapy first and mobilisation comes later. SA009:7 years PT experience
The delay in early mobilisation in general ICUs was frequently attributed to delayed consultations by specialist physicians and delayed investigations:
You can find that the patient can be admitted and only a few days later, you are still seeing on the patient’s notes: “Awaiting neurosurgeon’s consultation”; and some … they delay coming and these people give different orders at different times and it causes a lot of confusion on the nursing staff for they do not know which order to follow. SA004:11 years PT experience
Participants also expressed concern that due to the reshuffling of the physiotherapists (rotation of physiotherapists through different clinical areas in a hospital), there was no guarantee of continuity in services (unsustainability of early mobilisation activities). In fact, the rotational coverage of physiotherapists in the ICU negatively impacts on the rate of early mobilisation.
… the thing is we can try and do stuff when we are in the rotation, but we cannot guarantee that the person replacing us is actually going to carry over the activities, so the question is on sustainability. SA019:10 years PT experience
Discord between team members was also identified as a factor delaying early mobilisation. This was especially evident in the general units and in patients who had sustained either multiple injuries or were living with multiple comorbidities. In the words of one physiotherapist:
… every specialist will be saying” “Fix this first before we come in”, and the others will be saying: “Address that first before we address the problem relevant to us”, and the nurses do not understand what to do. Then the physiotherapist comes and you do not know what to do with the patient as you are awaiting the further [medical and/or surgical] management of the patient, and this delays the time for early mobilisation. SA004:11 years PT experience
Beliefs about consequences
The participants identified the following factors affecting the early mobilisation of patients: the haemodynamic instability, raised intracranial pressure, low platelet count, mental instability in patients with head injury and condition of the patient:
… most of the patients come in quite haemodynamically unstable, so as soon as they are haemodynamically stable, and it is appropriate, then we start mobilising…. most of the patients we have, they are not allowed to sit up because of the intracranial pressures (ICPs), because of the drains. However, as soon as the patient is allowed to, they are generally quite ok with sitting up in bed… SA006:9 years PT experience
Environmental context and resources
Another key factor in determining the activities which can be carried out with a patient at any given time is the available manpower to assist with early mobilisation. In addition to inadequate human resources, the units lacked appropriate equipment to facilitate the transfer and mobilisation of ICU patients (e.g., portable ventilators, hoists, and chairs), thereby reducing the rate of early mobilisation of patients:
It is not possible for me to mobilise all the patients in the unit if they are eligible for mobilisation when you are only one (physiotherapist) … the chairs we have in the unit are the standard chair with arm and back rests and these might be difficult to use with ICU patients because they are too low, and the arm rests are not adjustable… ZM012:7 years PT experience
T he presence of multiple patient attachments, the length of the attachments, and the location of the attachments also limited the early mobilisation of patients in ICU:
Sometimes the lines … you can’t move around with them, they are so short that you have to disconnect completely, or things end up falling … It’s never a plan that everything is on one side of the bed so that you can easily manoeuvre… SA014:9 years PT experience
Facilitators of early mobilisation
Knowledge
Awareness programmes implemented in some ICUs increased the rate of early mobilisation by advocating for this benefit during training, conducting relevant research and running workshops to disseminate information to team members:
I find it is the awareness of the benefits of early mobilisation … If people know the benefits, they will implement it … willingness … once they have the knowledge, the knowledge of the indications and contra-indications, the willingness not only of the therapist but of the whole team… SA013:15 years PT experience
Social influences
Key to the implementation of early mobilisation was the acceptance of early mobilisation treatment as the standard of care by the entire ICU team, which also increased motivation among the physiotherapists:
… there has definitely been an improvement and when people walk in and see that we have put a ventilated patient in a chair, no one is having a heart attack. SA016:7 years PT experience
Behavioural regulation
Non-rotational physiotherapy coverage in ICU was reported to result in high levels of mobility in patients. Physiotherapists were able to develop skills and expertise in the specific area of critical care and to establish a good working relationship with the entire ICU team. As a result, they received support and assistance when needed.
…I have worked so long in the unit with the nurses …. so I have a very good relationship…. they know how we operate, and they know that if I want to mobilise the patient, I will help them with other nursing duties if they help me…You really grow a relationship with the other staff in the unit, so you can negotiate with them if you want to mobilise a difficult patient and they are not too keen… so you really create a nice relationship, and that is always an advantage… SA006:9 years PT experience
Social/professional role and identity
Some participants felt that good communication was key in raising mobility levels in the units. This included having an ICU team which supported early mobilisation and respected teamwork:
Ah! I think in our unit it is the team work with the nursing staff and the doctors (general practitioner/physician). They are on board and they promote mobilisation… SA006:9 years PT experience
Goals
Participants felt that stability of the patients contributed to early mobilisation as it was more easily achieved in patients with medical and surgical conditions, for example:
… most of our patients in ICU are post-op patients so when they are admitted in ICU, usually by the second day post, we get them out-of-bed, sitting out-of-bed in a chair, or standing. ZM017:9 years PT experience
Environmental context and resources
Participants expressed that use of sedation scales or reduced use of sedation in patients created an environment which promotes the implementation of early mobilisation in the units.
We have protocols, we have an awake cycle, within the sedation days, just to assess the GCS in the morning, unless the patient is completely restless, so they keep them sedated…. SA006:9 years PT experience
Participants also mentioned that the availability of standardised operational procedures, including the availability of mobilisation protocols and clinical practice guidelines, helped to increase mobilisation of ICU patients.
… I use a mobilisation guideline called MOVE. I check the myocardial stability of the patient, looking at the ECG tracing that there are no signs of arrhythmias, infarctions or cardiac arrest in the past 24 hours, check blood pressure and heart rate, then check on the orientation of the patient, patient not confused or agitated or sedated, is cooperative and able to follow commands, like you ask them to do something, and they cooperate. Vasopressor use: … Are they on the lowest possible doses, and [they should] not have been increased in the past 24 hours; and lastly, the effort of the patient: Are they able to actively participate in the mobilisation or will it be more of a passive transfer by checking on the upper limb and lower limb muscle strength? They should be at least a grade 3… ZM007:4 years PT experience
Early mobilisation was facilitated by having two or more physiotherapists covering each unit, with physiotherapists less reliant on the availability of nursing staff for assistance.
Having two therapists covering the unit … they help each other … SA014:9 years PT experience
Mobilisation was increased in units with adjustable electrical beds, as these allow for a change in position without straining the physiotherapist’s lower back.
Another good thing in our unit is the availability of the hydraulic beds [electric beds] so you can prop up patients in bed. Those who can’t actively come up to sitting independently … you can at least prop them up in bed, and by doing that, you are having a positive effect on most systems of the body in that patient … ZM012:7 years PT experience
Having space for unobstructed movement in the ICU also promoted early mobilisation as the relevant activities could be carried out without any spatial limitations.
The staff is very supportive … the environment … The setup is such that there is space available for us to do what we want to do, unless the patient is ventilated, we [are] really able to do what we want to do… ZM017:9 years PT experience
Discussion
The study explored the perceptions of physiotherapists regarding the implementation of early mobilisation practices in ICUs, to understand the perceived barriers and facilitators specific to ICUs in SA and Zimbabwean public sector hospitals. The two themes which emerged under the interpretation of early mobilisation were “procedural knowledge” and “social influences”. The study revealed a total of 23 perceived barriers and 12 facilitators clustered into seven and six domains of the TDF, respectively. These were synthesised to provide a theoretical lens to view the cognitive, affective, social, and environmental influences on behaviour with regard to implementation of early mobilisation practice in ICU. Majority of the identified barriers and facilitators were mainly categorised under four domains of TDF which are (1) social/professional role and identity (i.e., professional identity/role or boundaries); (2) beliefs about consequences (i.e., patient related factors relating to stability or instability of the condition); (3) environment context and resources (i.e., material resources availability and management), and (4) behavioural regulation (i.e., action planning and goal setting in the unit). There was a relationship between the perceived barriers and facilitators to early mobilisation as the identified facilitators were also noted to be the specific interventions to address the barriers identified by the participants.
Differing definitions of early mobilisation and the goals of treatment may have resulted in low levels of early mobilisation. Physiotherapists perceived the concept of early mobilisation as including both active and passive activities. Active participation of the patient emerged as the most important factor for the intervention to be perceived as beneficial to the patient. Early mobilisation is defined as the intensification and early application (within the first two to five days of critical illness) of any active exercises in which the patient could assist using his/her own muscle strength and control that occurs while the patient is receiving mechanical ventilation [30–33]. The widely used definition of early mobilisation above includes all the aspects which were highlighted by the participants (active participation of the patient, early execution, progressive activities, and functional activities). Our findings are in line with previous studies which reported that standard mobilisation practice in ICU was poorly defined, different techniques were employed and there was variability in defining the “early” period [30]. The period after ICU admission was particularly important, as physical functioning impairments are increasingly common during the first few days of invasive ventilation [32,34]. Cameron et al. [5] reported that delaying mobilisation until the acute phase of the illness has subsided may not only significantly reduce the benefits but also result in poorer patient outcomes. Therefore, barriers to early mobilisation during the first few days of critical illness must be addressed to avoid any delay in initiating the early mobilisation of ICU patients.
Role clarity and accountability during early mobilisation can also be a barrier to implementation within a multidisciplinary team, who may believe that early mobilisation should be carried out by only one discipline [35–37]. Other barriers included the lack of clearly defined professional roles in early mobilisation, and perceiving early mobilisation as a physiotherapist’s role. Physiotherapists should be an integral part of the interdisciplinary team in the ICU and should be involved in the implementation of early mobilisation as they are the experts in movement and exercise [30,38]. However, the physiotherapists cannot work entirely alone and without the support of the other ICU team members, which include the physicians/general practitioners and nurses. These become the professions which constitute an early mobilisation team in the ICU environment, with each professional member providing information and education to the rest of the team regarding their potential individualised roles in early mobilisation and in the ICU in general [30,39–41]. Multidisciplinary team engagement was also pointed out to be one of the facilitators of early mobilisation by the participants. This shows that early mobilisation should be a collaborative initiative and that each member of the team has a specific role to play in order for the intervention to be successful, with some being responsible for the delivery and others supporting the delivery of the programme.
Low staff motivation emerged as a major barrier to implementation, as has been reported by others [42,43]. Further, early mobilisation can be deprioritised due to the lack of awareness of the benefits to patient outcomes or merely the negative perceptions associated with it [10,39,43,44]. Early mobilisation is frequently not considered as a treatment option when the patient has a respiratory dysfunction, due to lack of awareness of the patient-level benefits. Mobilisation should be regarded as a treatment option when a patient has been referred for chest PT, as it results in the optimisation of oxygenation through improved ventilation, alveolar recruitment and lung perfusion, and assists in the clearance of retained secretions from the airways [38,45]. Another factor which was also highlighted by the participants as a facilitator to early mobilisation was availability of awareness programmes. Increased awareness about the benefits of early mobilisation would increase the levels of early mobilisation in ICU patients, resulting in better patient outcomes.
Variability in clinical skills and experience was also raised as a barrier to the implementation process, mainly by SA participants who had on average twice the duration of ICU working experience compared with Zimbabwean staff. Stiller et al. [46] previously reported that experienced clinicians were often able to discern which patients would tolerate mobilisation despite marginal cardiac and/or respiratory conditions by taking into account more objective parameters and observing or interpreting the more subjective factors. In our study, many junior staff were reluctant to implement early mobilisation activities for patients or delayed initiating out-of-bed mobilisation due to lack of confidence and knowledge, and feeling overwhelmed by the ICU environment [44,47]. The ICU setting is a complex environment. Minimum standards of clinical practice for PT to facilitate the optimal care of patients during their ICU stay are in place in Australia and New Zealand, SA and the UK [48–51]. According to these standards, physiotherapists working in ICU should be able to mobilise both non-ventilated and ventilated patients. They should also understand the indications and contra-indications, provide evidence to the effect that they are applying the technique, and keep a record of the progression of the exercise activity [48]. Physiotherapists should receive adequate in-service clinical skills training to work effectively in ICU and be confident in their implementation of early mobilisation activities.
Key barriers that emerged and classified under the behavioural regulation domain included the following: inconsistent patient referrals, delayed specialist consultations, delayed investigations, discord between team members, and reshuffling of the ICU physiotherapists. In our study, depending on the participant or the specific ICU, staffing, policies and guidelines, and communication channels in ICUs were regarded as either barriers or facilitators. Staff shortages were reportedly the main reason why physiotherapists did not provide blanket cover to their ICUs, relying on the general practitioner/physician to refer them to the specific patients requiring PT interventions. Valentin and Ferdinande [52] reported that one physiotherapist with dedicated training and expertise in the management of critically ill patients should be available per five ICU beds on a seven-day-per-week basis. For out-of-bed mobilisation of mechanically ventilated patients, it requires a minimum of two people to guard the vital lines and attachments [39,53]. The numbers of physiotherapists working in some of the ICUs in Zimbabwean and SA public sector hospitals should be revised so that this measure fits the recommended international standard of staffing based on the bed capacity of each unit. Having enough PT staff covering each unit is one way of making sure that there is blanket cover of ICU patients and the timely delivery of treatment interventions. The creation of new posts for physiotherapists and having one dedicated physiotherapist at the disposal of the ICU to promote and sustain an early mobility programme can ensure the sustainability of such an intervention [39,47,52,54].
Delayed consultation by specialists, largely in the general ICUs, was a barrier to early mobilisation in both countries. The delay was most marked in patients with traumatic injury resulting in either a neurological or a musculoskeletal injury. Although the African Region possesses only 2% of the world’s vehicles, it contributes 16% to global road traffic deaths and has the highest road fatality rate of all World Health Organisation regions. The general lack of resources to manage trauma patients in low- and middle-income countries has been reported [55,56]. In Africa, consisting mainly of low- and middle-income countries, there is an average of one neurosurgeon per 6.36 million of the population [57], compared to one neurosurgeon per every 65 580 of the population in high-income countries [58]. The few specialists are overwhelmed with workload given the high incidence of trauma-related injuries in sub-Saharan Africa [55,56], resulting in delayed consultations in the ICUs and further delays in the management of such patients. There is a need to increase the resources for the management of trauma patients in low- and middle-income countries, where the burden of the disease is extremely high.
Haemodynamic instability, mental instability, raised intracranial pressure (ICP) and thrombocytopenia were perceived as patient-related barriers to early mobilisation. These have also been reported as barriers associated with out-of-bed mobilisation by others [12,35,47,59,60]. Mental instability, which included confusion, drowsiness, raised ICP or a low Glasgow Coma Scale Score, was flagged in our study as a common barrier to early mobilisation. This was reported mainly in patients with neurological instability, resulting in the low prioritisation of early mobilisation in patients with neurological injuries. Neurological instability, characterised by a low Glasgow Coma Scale Score, drowsiness and difficulty to control ICP, was reported by others as a major contributor to immobility in the ICU [15,17,37,61]. However, a recent study showed that early mobilisation initiated within 72 h of ICU admission in patients with a low Glasgow Coma Scale Score can be considered to be safe and effective [62]. In relation to platelet count, a study done in Canada reported that activity restrictions were not necessary for patients who had thrombocytopenia [63]. There are conflicting views on the optimal limit of the platelet count that should be considered for safe early mobilisation. However, parameters indicated in the early mobilisation guidelines or protocols are not intended to be absolute contra-indications or to be interpreted in isolation but should be used in conjunction with sound clinical judgement [46].
Under the environmental context and resources domain, it included barriers to early mobilisation such as inadequate staff numbers, the lack of appropriate equipment, the number, length, and position of attachments. A lack of staffing to assist with the out-of-bed mobilisation of patients, especially in terms of the number of available physiotherapists, resulted in the low prioritisation of early mobilisation in units, as has been previously reported in different settings [10,35,37,44,59,60].
Finally, the lack of appropriate equipment constrained the delivery of early mobilisation to patients in ICUs in ZM and SA. Equipment includes both transfer and mobilisation equipment. If it is inadequate and there is a lack of resources, it may be a barrier to early mobilisation [10,44,54,59,60]. Although standard hospital equipment may generally be adequate to enable patients to walk during early mobilisation activities [30,38], their safety, efficiency, and effectiveness may be compromised when clinicians have to hold all the attachments and lines in their hands [53]. Therefore, based on the available evidence, adequate equipment which maximises safety, efficiency, and effectiveness should be provided in all ICUs to promote the early mobilisation of patients in a safe environment.
The findings of the study identified influences on behaviour in the implementation of an evidence based practice. Behaviour change has been identified to be a key element when it comes to improving healthcare and healthcare outcomes [64]. The TDF was used in this study as it was seen to provide a broad perspective and means of understanding the implementation problems and potential solutions in the theoretical terms [26,64]. The advantage of using this framework is that it makes links between theories of behaviour change and it has a comprehensive coverage of possible influences on behaviour [64], thereby providing explicit statements of the structural and psychological process hypothesised to regulate behaviour and behaviour change [26]. Findings from this study may then be used in the designing and evaluation of interventions targeted at implementation of early mobilisation practice as an evidence based practice.
One strength of the study is the study setting. The findings obtained were elicited from a wide range of ICU settings from different provinces in the two countries. An effort was made to represent the different types of ICUs, including specialised units from all the provinces in SA, which gave their approval for the study to be conducted. Yet another strength of the study is the study design. The qualitative study design allowed exploration of the problem based on the experience of the participants. The study had some limitations. The target group that identified the barriers and facilitators to the early mobilisation of patients in ICU was composed of physiotherapists only. However, the perceptions of all the members of the ICU multidisciplinary team are necessary since their individual professional roles and clinical expertise are just as important in making decisions on mobilisation. Another limitation of this study was the lack of time to conduct full interviews with the respective physiotherapists on account of their busy schedule and workload, which resulted in some physiotherapists rushing through the interview and not providing sufficient feedback on some of the questions. In order to promote more use of early mobilisation practices in patient management, there is need for guidelines to standardise practices and address critical issues which have been raised. Since early mobilisation requires teamwork for it to be successful, the implementation guidelines should be formulated by the multidisciplinary team involved in the early mobilisation of patients, covering all of the aspects which have been highlighted to be barriers.
Conclusions
To enhance the level of early mobilisation of patients in public sector ICUs in SA and Zimbabwe, certain barriers must be addressed. These barriers to early mobilisation in public sector ICUs included factors related to patients, ICU environment, organisation of ICU services, and the implementation process. The changes which must happen in the ICU or hospital settings for the implementation process of early mobilisation to advance include coming up with strategies to address the barriers. Investing in resources which include those aspects related to manpower and equipment is of paramount importance in order to facilitate the implementation of early mobilisation. Considering the early mobilisation intervention itself, there is a need to standardise practice by clearly defining the type of activity, the dosage of exercise, and the progression of early mobilisation activities. This qualitative study highlighted the importance of multidisciplinary team collaboration and planning before implementing early mobilisation activities.
Supplementary Material
Figure 2.
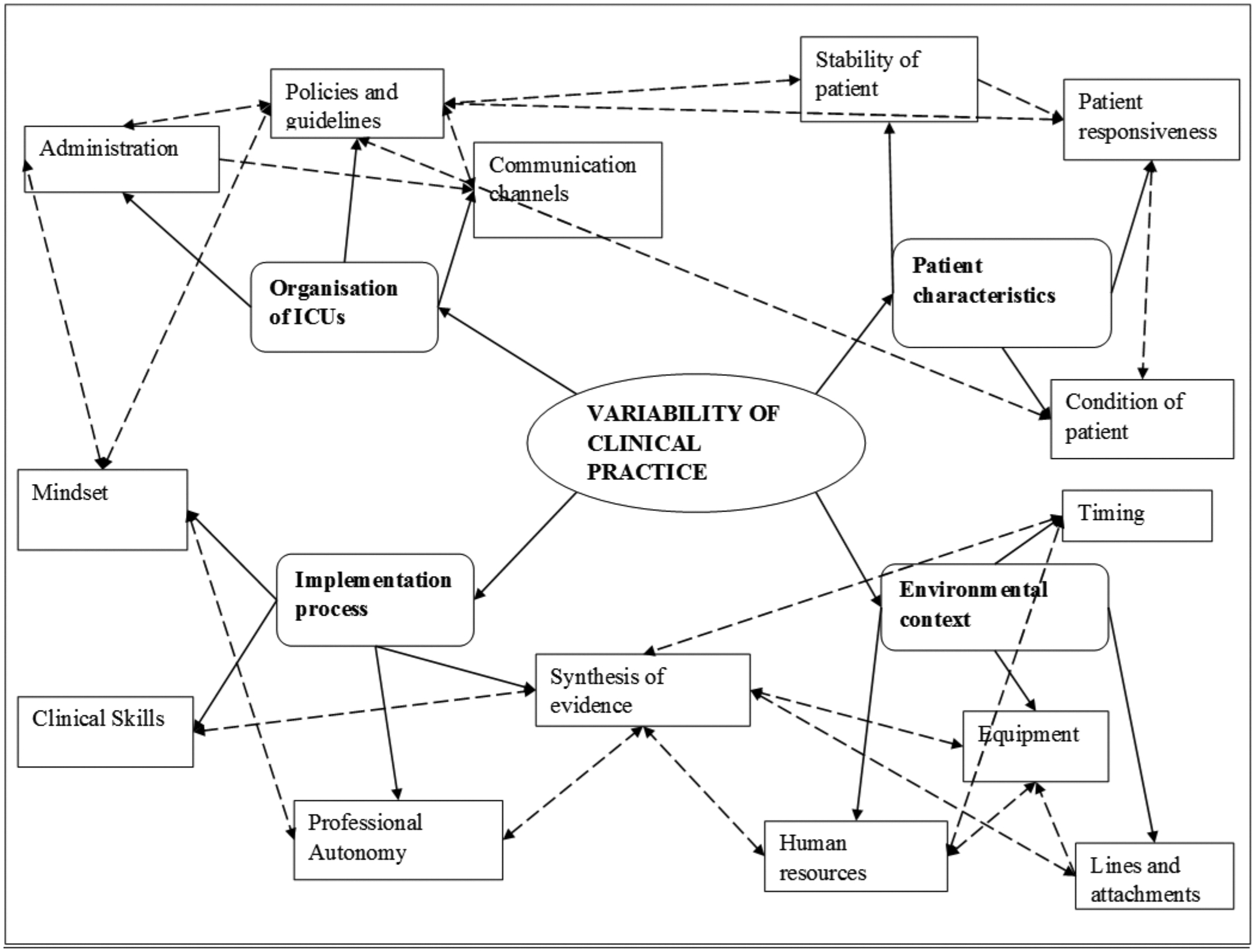
Barriers to early mobilisation of ICU patients in SA and Zimbabwean government hospitals. Solid lines indicate the categories under each theme and the interrupted lines indicate the linkage between categories.
Figure 3.
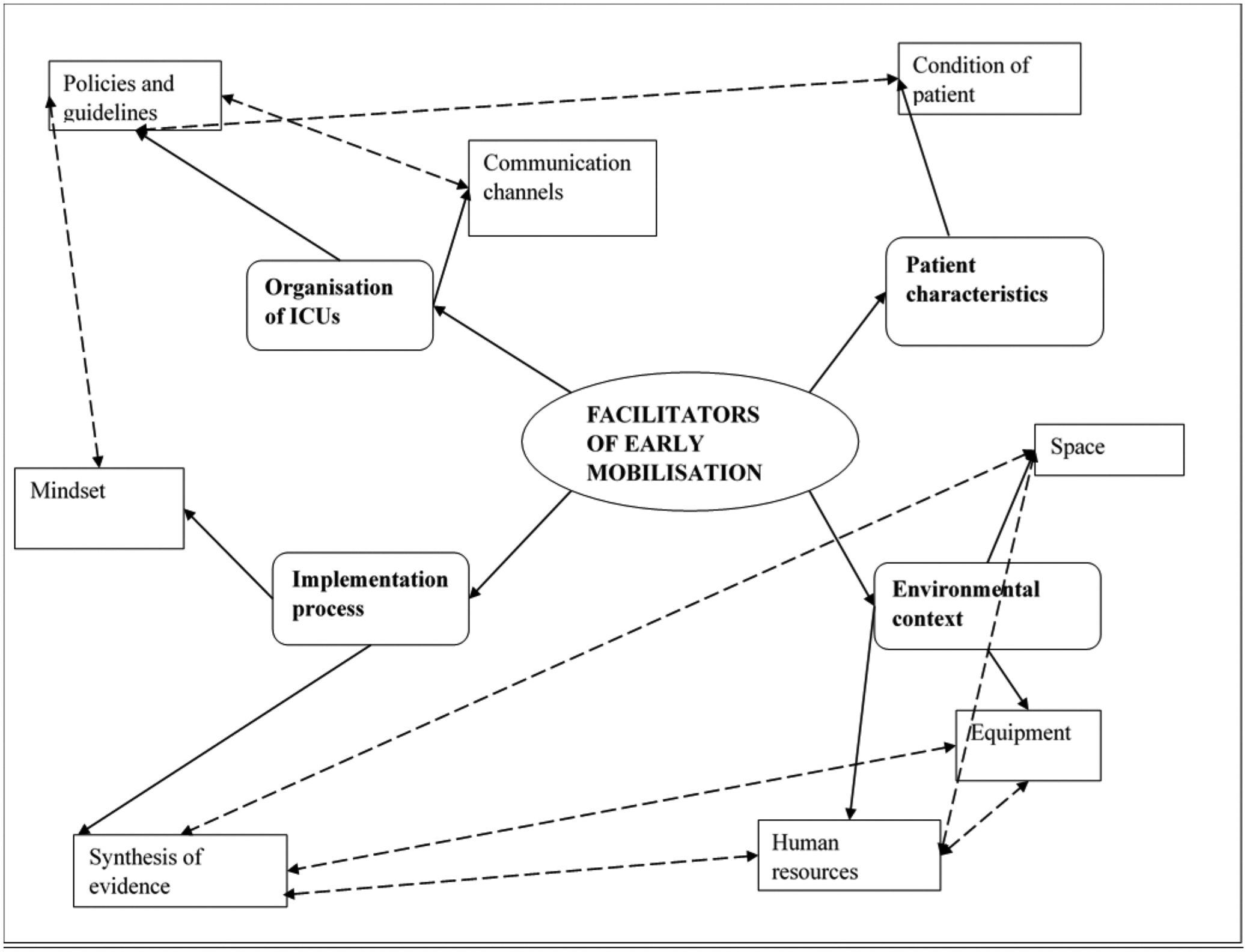
Facilitators of early mobilisation practices in SA and Zimbabwean government hospitals. Solid lines indicate the categories under each theme and the interrupted lines indicate the linkage between categories.
Implications to rehabilitation.
Professional roles/identity and or boundaries emerged to be a barrier that hinder implementation of early mobilisation if not clearly defined.
Non-rotational physiotherapy coverage was highlighted to be important in facilitating good communication and teamwork and sustainability of services in ICU.
Good communication channels and referrals between different disciplines should be employed in ICU to prevent delay in rendering services to ICU patients.
Acknowledgements
The authors would like to thank the physiotherapists who participated in the study and the other health workers in all the study sites for their support. The authors are so grateful for the assistance in writing this manuscript received from Dr Morna Cornell through a writing retreat workshop arranged by Biomedical Research and Training Institute.
Fogarty International Center (Office Of The Director, National Institutes Of Health (OD), National Institute Of Nursing Research (NINR), National Institute Of Mental Health (NIMH), National Institute Of Dental & Craniofacial Research (NIDCR), National Institute Of Neurological Disorders And Stroke (NINDS), National Heart, Lung, And Blood Institute (NHLBI), Fogarty International Center (FIC)) of the National Institutes of HealthD43 TW010137Fogarty International Center of the National Institutes of HealthD43 TW009539D43 TW009343University of California Global Health Institute (UCGHI; San Francisco, CA, USA)10.13039/100004676Research reported in this publication was supported by the Fogarty International Center (Office Of The Director, National Institutes Of Health (OD), National Institute Of Nursing Research (NINR), National Institute Of Mental Health (NIMH), National Institute Of Dental & Craniofacial Research (NIDCR), National Institute Of Neurological Disorders And Stroke (NINDS), National Heart, Lung, And Blood Institute (NHLBI), Fogarty International Center (FIC)) of the National Institutes of Health under Award Number D43 TW010137; Fogarty International Center of the National Institutes of Health under Award Number (D43 TW009539; D43 TW009343) and the University of California Global Health Institute (UCGHI; San Francisco, CA, USA).
Footnotes
Ethics approval and consent to participate: Ethical clearance for this study was obtained from the Joint Research Ethics Committee for University of Zimbabwe College of Health Sciences and Parirenyatwa Group of Hospitals (JREC REF: 377/15), Medical Research Council of Zimbabwe (MRCZ/A/2040), and the University of the Witwatersrand Human Research Ethics Committee (Medical) (REF: M150927) in SA. Each questionnaire contained information on the study and participation was anonymous and voluntary for unit staff. Informed consent was obtained from each participant.
Disclosure statement
The authors declare that they have no competing interests.
Data availability statement
All data and materials are available and are with the first author.
References
- 1.Okafor UV. Challenges in critical care services in Sub-Saharan Africa: perspectives from Nigeria. Indian J Crit Care Med. 2009;13(1):25–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Argent AC. Critical care in Africa. South Afr J Crit Care. 2009;25(1):4–8. [Google Scholar]
- 3.Adler J, Malone D. Early mobilization in the intensive care unit: a systematic review. Cardiopulm Phys Ther J. 2012;23(1):5–13. [PMC free article] [PubMed] [Google Scholar]
- 4.Goddard SL, Lorencatto F, Koo E, et al. Barriers and facilitators to early rehabilitation in mechanically ventilated patients—a theory-driven interview study. J Intensive Care. 2018;6:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cameron S, Ball I, Cepinskas G, et al. Early mobilization in the critical care unit: a review of adult and pediatric literature. J Crit Care. 2015;30(4):664–672. [DOI] [PubMed] [Google Scholar]
- 6.Tipping CJ, Harrold M, Holland A, et al. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med. 2017;43(2):171–183. [DOI] [PubMed] [Google Scholar]
- 7.Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med. 2013;41(6):1543–1554. [DOI] [PubMed] [Google Scholar]
- 8.Roberson AR, Starkweather A, Grossman C, et al. Influence of muscle strength on early mobility in critically ill adult patients: systematic literature review. Heart Lung. 2018;47(1):1–9. [DOI] [PubMed] [Google Scholar]
- 9.Chiarici A, Andrenelli E, Serpilli O, et al. An early tailored approach is the key to effective rehabilitation in the intensive care unit. Arch Phys Med Rehabil. 2019;100(8):1506–1514. [DOI] [PubMed] [Google Scholar]
- 10.Barber EA, Everard T, Holland AE, et al. Barriers and facilitators to early mobilisation in intensive care: a qualitative study. Aust Crit Care. 2015;28(4):177–182; quiz 83. [DOI] [PubMed] [Google Scholar]
- 11.Berney SC, Harrold M, Webb SA, et al. Intensive care unit mobility practices in Australia and New Zealand: a point prevalence study. Crit Care Resusc. 2013;15(4):260–265. [PubMed] [Google Scholar]
- 12.Nydahl P, Ruhl AP, Bartoszek G, et al. Early mobilization of mechanically ventilated patients: a 1-day point-prevalence study in Germany. Crit Care Med. 2014;42(5):1178–1186. [DOI] [PubMed] [Google Scholar]
- 13.Jolley SE, Moss M, Needham DM, et al. Point prevalence study of mobilization practices for acute respiratory failure patients in the United States. Crit Care Med. 2017;45(2):205–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sibilla A, Nydahl P, Greco N, et al. Mobilization of mechanically ventilated patients in Switzerland. J Intensive Care Med. 2020;35(1):55–62. [DOI] [PubMed] [Google Scholar]
- 15.Capell EL, Tipping CJ, Hodgson CL. Barriers to implementing expert safety recommendations for early mobilisation in intensive care unit during mechanical ventilation: a prospective observational study. Aust Crit Care. 2019;32(3):185–190. [DOI] [PubMed] [Google Scholar]
- 16.Fontela PC, Lisboa TC, Forgiarini-Junior LA, et al. Early mobilization practices of mechanically ventilated patients: a 1-day point-prevalence study in Southern Brazil. Clinics. 2018;73:e241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harrold ME, Salisbury LG, Webb SA, et al. Early mobilisation in intensive care units in Australia and Scotland: a prospective, observational cohort study examining mobilisation practises and barriers. Crit Care. 2015;19(1):336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malone D, Ridgeway K, Nordon-Craft A, et al. Physical therapist practice in the intensive care unit: results of a national survey. Phys Ther. 2015;95(10):1335–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phelan S, Lin F, Mitchell M, et al. Implementing early mobilisation in the intensive care unit: an integrative review. Int J Nurs Stud. 2018;77:91–105. [DOI] [PubMed] [Google Scholar]
- 20.Tadyanemhandu C, van Aswegen H, Ntsiea V. Early mobilisation practices of patients in intensive care units in Zimbabwean government hospitals – a cross-sectional study. South Afr J Crit Care. 2018;34:16–21. [PMC free article] [PubMed] [Google Scholar]
- 21.Tadyanemhandu C, van Aswegen H, Ntsiea V. Organizational structures and early mobilization practices in South African public sector intensive care units—a cross-sectional study. J Eval Clin Pract. 2021;27(1):42–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Korstjens I, Moser A. Series: practical guidance to qualitative research. Part 4: trustworthiness and publishing. Eur J Gen Pract. 2018;24(1):120–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neuendorf KA, Kumar A. Content analysis. The international encyclopedia of political communication; 2016. John Wiley and Sons. New York. USA. p. 1–10. [Google Scholar]
- 24.Bengtsson M How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2016;2:8–14. [Google Scholar]
- 25.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115. [DOI] [PubMed] [Google Scholar]
- 26.Atkins L, Francis J, Islam R, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anekwe DE, Milner SC, Bussières A, et al. Intensive care unit clinicians identify many barriers to, and facilitators of, early mobilisation: a qualitative study using the theoretical domains framework. J Physiother. 2020;66(2):120–127. [DOI] [PubMed] [Google Scholar]
- 28.World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001;79(4):373–374. [PMC free article] [PubMed] [Google Scholar]
- 29.World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. [DOI] [PubMed] [Google Scholar]
- 30.Hodgson CL, Berney S, Harrold M, et al. Clinical review: early patient mobilization in the ICU. Crit Care. 2013;17(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hodgson CL, Stiller K, Needham DM, et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit Care. 2014;18(6):658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The TSI. Early mobilization and recovery in mechanically ventilated patients in the ICU: a bi-national, multi-centre, prospective cohort study. Crit Care. 2015;19(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nydahl P, Sricharoenchai T, Chandra S, et al. Safety of patient mobilization and rehabilitation in the intensive care unit. Systematic review with meta-analysis. Ann Am Thorac Soc. 2017;14(5):766–777. [DOI] [PubMed] [Google Scholar]
- 34.Jolley SE, Regan-Baggs J, Dickson RP, et al. Medical intensive care unit clinician attitudes and perceived barriers towards early mobilization of critically ill patients: a cross-sectional survey study. BMC Anesthesiol. 2014;14:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boehm LM, Vasilevskis EE, Mion LC. Interprofessional perspectives on ABCDE bundle implementation: a focus group study. Dimens Crit Care Nurs. 2016;35(6):339–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dubb R, Nydahl P, Hermes C, et al. Barriers and strategies for early mobilization of patients in intensive care units. Ann Am Thorac Soc. 2016;13(5):724–730. [DOI] [PubMed] [Google Scholar]
- 37.Parry SM, Knight LD, Connolly B, et al. Factors influencing physical activity and rehabilitation in survivors of critical illness: a systematic review of quantitative and qualitative studies. Intensive Care Med. 2017;43(4):531–542. [DOI] [PubMed] [Google Scholar]
- 38.Asher A Equipment used for safe mobilization of the ICU patient. Crit Care Nurs Q. 2013;36(1):101–108. [DOI] [PubMed] [Google Scholar]
- 39.Engel HJ, Tatebe S, Alonzo PB, et al. Physical therapist-established intensive care unit early mobilization program: quality improvement project for critical care at the University of California San Francisco Medical Center. Phys Ther. 2013;93(7):975–985. [DOI] [PubMed] [Google Scholar]
- 40.Jolley SE, Dale CR, Hough CL. Hospital-level factors associated with report of physical activity in patients on mechanical ventilation across Washington State. Ann Am Thorac Soc. 2015;12(2):209–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marshall JC, Bosco L, Adhikari NK, et al. What is an intensive care unit? A report of the task force of the world federation of societies of intensive and critical care medicine. J Crit Care. 2017;37:270–276. [DOI] [PubMed] [Google Scholar]
- 42.Carrothers KM, Barr J, Spurlock B, et al. Contextual issues influencing implementation and outcomes associated with an integrated approach to managing pain, agitation, and delirium in adult ICUs. Crit Care Med. 2013;41(9 Suppl. 1):S128–S135. [DOI] [PubMed] [Google Scholar]
- 43.Hodgson CL, Capell E, Tipping CJ. Early mobilization of patients in intensive care: organization, communication and safety factors that influence translation into clinical practice. Crit Care. 2018;22(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Parry SM, Remedios L, Denehy L, et al. What factors affect implementation of early rehabilitation into intensive care unit practice? A qualitative study with clinicians. J Crit Care. 2017;38:137–143. [DOI] [PubMed] [Google Scholar]
- 45.Gosselink R, Bott J, Johnson M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med. 2008;34(7):1188–1199. [DOI] [PubMed] [Google Scholar]
- 46.Stiller K, Phillips A, Lambert P. The safety of mobilisation and its effect on haemodynamic and respiratory status of intensive care patients. Physiother Theory Pract. 2004;20(3):175–185. [Google Scholar]
- 47.van Willigen Z, Collings N, Richardson D, et al. Quality improvement: the delivery of true early mobilisa tion in an intensive care unit. BMJ Qual Improv Rep. 2016;5(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Skinner EH, Thomas P, Reeve JC, et al. Minimum standards of clinical practice for physiotherapists working in critical care settings in Australia and New Zealand: a modified Delphi technique. Physiother Theory Pract. 2016;32(6):468–482. [DOI] [PubMed] [Google Scholar]
- 49.Plani N, van Aswegen H, Patman S, et al. Developing minimum clinical standards for physiotherapy in South African intensive care units: a mixed method approach. Eur J Physiother. 2017;19(Suppl. 1):31–33. [Google Scholar]
- 50.van Aswegen H, Patman S, Plani N, et al. Developing minimum clinical standards for physiotherapy in South African ICUs: a qualitative study. J Eval Clin Pract. 2017;23(6):1258–1265. [DOI] [PubMed] [Google Scholar]
- 51.Twose P, Jones U, Cornell G. Minimum standards of clinical practice for physiotherapists working in critical care settings in the United Kingdom: a modified Delphi technique. J Intensive Care Soc. 2019;20(2):118–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Valentin A, Ferdinande P. Recommendations on basic requirements for intensive care units: structural and organizational aspects. Intensive Care Med. 2011;37(10):1575–1587. [DOI] [PubMed] [Google Scholar]
- 53.Needham DM, Truong AD, Fan E. Technology to enhance physical rehabilitation of critically ill patients. Crit Care Med. 2009;37(10 Suppl.):S436–S441. [DOI] [PubMed] [Google Scholar]
- 54.Bassett R, Adams KM, Danesh V, et al. Rethinking critical care: decreasing sedation, increasing delirium monitoring, and increasing patient mobility. Jt Comm J Qual Patient Saf. 2015;41(2):62–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Laing GL, Skinner DL, Bruce JL, et al. Understanding the burden and outcome of trauma care drives a new trauma systems model. World J Surg. 2014;38(7):1699–1706. [DOI] [PubMed] [Google Scholar]
- 56.Tran TM, Fuller AT, Kiryabwire J, et al. Distribution and characteristics of severe traumatic brain injury at Mulago National Referral Hospital in Uganda. World Neurosurg. 2015;83(3):269–277. [DOI] [PubMed] [Google Scholar]
- 57.Jerome E, Laing GL, Bruce JL, et al. An audit of traumatic brain injury (TBI) in a busy developing-world trauma service exposes a significant deficit in resources available to manage severe TBI. S Afr Med J. 2017;107(7):621–625. [DOI] [PubMed] [Google Scholar]
- 58.Rosman J, Slane S, Dery B, et al. Is there a shortage of neurosurgeons in the United States? Neurosurgery. 2013;73(2):354–355, discussion 65–66. [DOI] [PubMed] [Google Scholar]
- 59.Bakhru RN, McWilliams DJ, Wiebe DJ, et al. Intensive care unit structure variation and implications for early mobilization practices. An international survey. Ann Am Thorac Soc. 2016;13(9):1527–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Castro-Avila AC, Serón P, Fan E, et al. Effect of early rehabilitation during intensive care unit stay on functional status: systematic review and meta-analysis. PLOS One. 2015;10(7):e0130722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Brock C, Marzano V, Green M, et al. Defining new barriers to mobilisation in a highly active intensive care unit – have we found the ceiling? An observational study. Heart Lung. 2018;47(4):380–385. [DOI] [PubMed] [Google Scholar]
- 62.Schaller SJ, Scheffenbichler FT, Bose S, et al. Influence of the initial level of consciousness on early, goal-directed mobilization: a post hoc analysis. Intensive Care Med. 2019;45(2):201–210. [DOI] [PubMed] [Google Scholar]
- 63.Koo KK, Choong K, Cook DJ, et al. Early mobilization of critically ill adults: a survey of knowledge, perceptions and practices of Canadian physicians and physiotherapists. CMAJ Open. 2016;4(3):E448–E454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data and materials are available and are with the first author.


