Abstract
Background
Data on the interplay between sexual hormones balance, platelet function and clinical outcomes of adults with ischemic heart disease (IHD) are still lacking.
Objective
To assess the association between the Testosterone (T)-to-Estradiol (E2) Ratio (T/E2) and platelet activation biomarkers in IHD and its predictive value on adverse outcomes.
Methods
The EVA study is a prospective observational study of consecutive hospitalized adults with IHD undergoing coronary angiography and/or percutaneous coronary interventions. Serum T/E2 ratios E2, levels of thromboxane B2 (TxB2) and nitrates (NO), were measured at admission and major adverse events, including all-cause mortality, were collected during a long-term follow-up.
Results
Among 509 adults with IHD (mean age 67 ± 11 years, 30% females), males were older with a more adverse cluster of cardiovascular risk factors than females. Acute coronary syndrome and non-obstructive coronary artery disease were more prevalent in females versus males. The lower sex-specific T/E2 ratios identified adults with the highest level of serum TxB2 and the lowest NO levels. During a median follow-up of 23.7 months, the lower sex-specific T/E2 was associated with higher all-cause mortality (HR 3.49; 95% CI 1.24–9.80; p = 0.018). In in vitro, platelets incubated with T/E2 ratios comparable to those measured in vivo in the lowest quartile showed increased platelet activation as indicated by higher levels of aggregation and TxB2 production.
Conclusion
Among adults with IHD, higher T/E2 ratio was associated with a lower long-term risk of fatal events. The effect of sex hormones on the platelet thromboxane release may partially explain such finding.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40618-022-01771-0.
Keywords: Testosterone, Estradiol, Ischemic heart disease, Thromboxane, Mortality
Introduction
Although adverse outcomes from ischemic heart diseases (IHD) have been declining over the last decade, the worldwide burden of IHD remains high in both sexes. Even if females have an age-standardized incidence and prevalence of IHD lower than males [1, 2], the absolute number of females is greater than that of males. Furthermore, sex difference exists in the pathogenesis, progression and response to treatment. Indeed, IHD is not anymore synonymous only with obstructive flow-limiting coronary artery disease (CAD), especially in females that are more commonly affected by non-obstructive disease [3]. Traditionally, biological attributes have been claimed as main drivers of the sex differences across the spectrum of IHD, specifically sex hormones might play a role on the status of the vascular health [4].
Mechanistic understanding of the association between sex steroids and IHD is challenging.
Testosterone (T) and estrogen-related steroid hormones (including 17b estradiol, E2) have been shown to, directly and indirectly affect vascular health [5]. The effects of sex hormones have been analyzed separately with conflicting data in males and females for their protective or harmful effects on cardiovascular health. The disturbance of the physiological balance between E2 and T has been studied to understand its contribution to cardiovascular disease (CVD) progression in a synergistic or co-dependent interplay [6]. For example, in males with severe carotid atherosclerosis, low T/E2 ratio is associated with systemic and plaque inflammation and is a powerful predictor of future cardiovascular events [7]. Interestingly, in females, the reverse regarding T/E2 ratio has been observed, with higher T/E2 ratio being associated with worse CVD outcomes/events in post-menopausal women [8].
In the interplay between sex hormones and vascular health, differences in vasoactive molecules modulated by the T/E2 balance might be relevant. In experimental models, females are at reduced risk of ischemia–reperfusion damage and E2 administered acutely to males can reduce infarct size [9]. The non-genomic effects of sex hormones on vascular cells and platelets recruited at the athero-thrombotic process site are a matter of debate [10, 11]. A sex difference in platelet reactivity has been reported in response to agonists both with and without concomitant antiplatelet therapy [12]. Mechanisms that could account for such differences in platelet biology are mostly unknown. Platelets mainly express estrogen receptor beta (ER-β) on their surfaces [13]. Treating human platelets from healthy men with E2 did not elicit any functional platelet response, but it primed thrombin-induced platelet aggregation through a non-genomic effect [13]. Whether this occurs in platelets from females or in individuals of both sexes with IHD has not been investigated.
In light of this, among adults with IHD we investigated: (i) the relation between sex-specific T/E2 ratio and vasoactive molecules, such as thromboxane B2 and NO metabolites; (ii) the existence of an association between sex-specific T/E2 ratio and long-term adverse clinical outcomes; and (iii) whether the association between T/E2 ratio and outcomes can be explained at least in part through sex hormone-dependent effects on platelet function.
Methods
The data underlying this article will be shared upon reasonable request to the corresponding author.
Study population
The “Endocrine Vascular disease Approach” (EVA) project (ClinicalTrials.gov identifier NCT02737982), is an observational, prospective study, aimed at exploring sex- and gender-related differences in the interaction between platelet function, sex hormones, and coronary microvascular dysfunction in IHD. The EVA Study design has been previously published [14]. Briefly, EVA enrolled consecutively Italian adults (> 18 years), who were referred to the cardiac catheterization laboratory (cath-lab) undergoing coronary angiography and/or percutaneous coronary intervention for suspected IHD. Based on angiography, IHD patients were classified as follows: (1) ischemia with obstructive CAD, that is, ≥ 50% diameter stenosis; and (2) ischemia with no obstructive CAD (INOCA) < 50% diameter stenosis [15, 16].
During the angiography, blood samples were collected before PCI. Measurements were ascertained while blinded to the sample origin. All samples were assayed in duplicate, and those showing values above the standard curve were retested with appropriate dilutions. According to a previously reported study, the arterial samples are suitable for testing biomarkers of platelet function [17].
The study was conducted in full conformance with the Declaration of Helsinki principles, and it was approved by the local Ethics Committee of Policlinico Umberto I, Sapienza University of Rome, Rome, Italy (reference 3786, 24/09/2015). Written informed consent has been obtained from all patients.
Sex-hormone measurements
The concentration of sex hormones was measured in batch by the Laboratory of the Department of Experimental Medicine (Section of Medical Pathophysiology), Sapienza University of Rome in serum samples stored at − 80 °C. Serum E2 and T were measured by chemiluminescent micro-particle immunoassay (CMIA, Architect System) (Abbott Laboratories, IL, USA). The T/E2 ratio was calculated using the following formula: Testosterone/(10*estradiol) as previously reported [7].
Vasoactive biomarkers measurements
Serum thromboxane B2 (TxB2), the stable product of the non-enzymatic hydration of TxA2, which itself has a half-life of only 37 s under physiologic conditions, was measured by ELISA (Cusabio, TX, USA) according to the manufacturer instructions and expressed as picograms per milliliter (pg/ml). Intra-assay and inter-assay coefficients of variation were 4.0% and 3.6%, respectively.
Nitric oxide (NO) bioavailability was determined with a colorimetric assay kit (Cell Biolabs, San Diego, California, USA) by measuring the NO metabolites, nitrite and nitrate, in the serum. Intra-assay and inter-assay coefficients of variation were 2.9% and 1.7%, respectively.
Platelet preparation and platelet aggregation
To obtain platelet-rich plasma (PRP), citrated [3.8%, 1/10 (v: v)] blood samples from healthy volunteers were centrifuged for 15 min at 180 g at room temperature and the supernatant PRP was separated (2 × 105 platelets/μl). Only the top 75% of the PRP was collected, to avoid leukocyte contamination.
PRP samples were incubated with different concentrations of T and E2 to achieve the T/E2 ratio corresponding to the male-specific lowest (11.6, [T] 9.97 nM and [E2] 0.086 nM) and highest (22.2, [T] 18.3 nM and [E2] 0.0824 nM) quartiles and to the female-specific lowest (0.90, [T] 0.52 nM and [E2] 0.0577 nM) and highest (2.71, [T] 1.15 nM and [E2] 0.0424 nM) quartiles. Following incubation, platelets were stimulated with a sub-threshold concentration of collagen (STC, 0.25 μg/ml), defined as the highest concentration that elicited < 20% platelet aggregation. Platelet aggregation was monitored continuously as light transmission increment. Finally, samples were centrifuged for 3 min at 3000 rpm and supernatants and pellets were stored at − 80 °C to measure TxB2.
Platelet TxB2 assay
Platelet TxB2 was evaluated in the platelet supernatant by an ELISA commercial kit (Cusabio, TX, USA), according to manufacturer instructions. The values were expressed as pg/ml. Intra- and inter-assay coefficients of variation for TxB2 were < 8% and < 10%, respectively.
Follow-up
Participants were followed up by phone and outpatient visits when feasible for at least one year after discharge; after 12 months, phone interviews were conducted periodically each 3 months. In case of events, the adjudication of the adverse clinical outcomes was performed by assessing the medical chart reviews. For the purpose of this analysis, we assessed all-cause mortality, defined as death for any cause during follow-up.
Statistical analysis
All continuous variables were tested for normality with the Shapiro–Wilk test. Continuous variables with normal distribution were reported as mean ± standard deviation (SD), non-parametric variables as median and interquartile range (IQR). Between-groups comparisons were performed using T test for normally distributed variables and using an appropriate non-parametric test for non-normally distributed variables (Mann–Whitney U test or Kruskal–Wallis H test). Categorical variables were reported as count and percentages. Between-groups comparisons were made using a χ2 test, or a Fisher’s exact test if any expected cell count was < 5. For categorical variables with more than two possible values, exact P values have been estimated according to the Monte Carlo method. Quartiles of T/E2 ratio have been separately computed for males and females to account for the different physiological distribution of sex hormones and then a pooled sex-specific T/E2 ratio variable was used in all the analyses.
Survival curves were formally compared using the log-rank test. Cox proportional hazards analysis was used to calculate the adjusted relative hazards of outcome events. The final multivariable Cox regression model was selected via a purposeful selection of potential confounders. Given the limited number of events, the relationship of interest has been adjusted for age, sex and the type of CAD (obstructive vs. non-obstructive) and the presence of an acute coronary syndrome).
A two-sided p value < 0.05 was considered statistically significant. All analyses were performed using SPSS v. 25.0 statistical software (IBM, NY, USA).
Results
Among the 509 consecutive adults with IHD recruited in the EVA study (Table S1), 434 (85%) were analyzed as they had both ratio T/E2 measured at baseline and follow-up data (Fig. 1). None of the participants was under hormonal therapies. The baseline clinical characteristics stratified by sex are summarized in Table 1. Males were younger, with a more adverse cluster of cardiovascular risk factors than females. The referral reason for coronary angiography was acute coronary syndrome (ACS) in half of the cases. Females more frequently exhibited non-obstructive coronary artery disease than males.
Fig. 1.
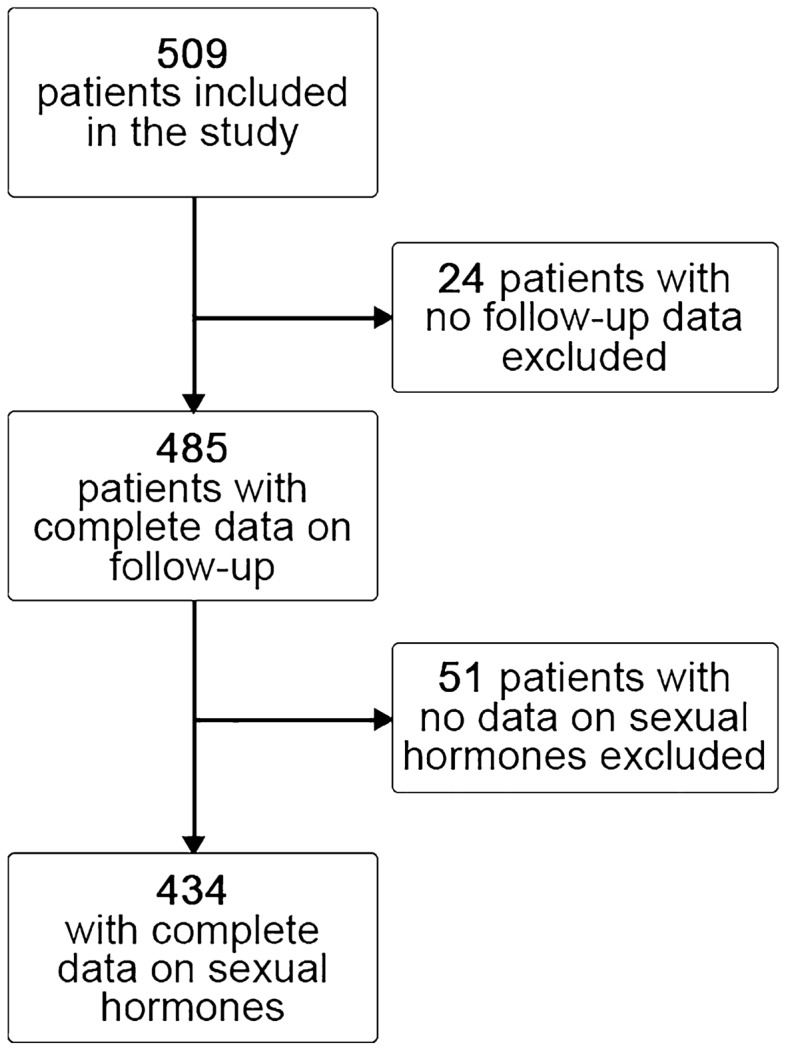
Study population
Table 1.
Baseline characteristics stratified by sex
| Variables | Women (n = 133) |
Men (n = 301) |
p value |
|---|---|---|---|
| Age (years) mean ± SD | 69.8 ± 11.5 | 65.4 ± 10.7 | < 0.001 |
| BMI (kg/m2) mean ± SD | 26.3 ± 5.0 | 27.5 ± 4.0 | 0.009 |
| Family Hx CVD | 72 (55.8) | 191 (64.7) | 0.08 |
| Smoking | 25 (19.1) | 86 (28.9) | 0.031 |
| Hypertension | 97 (73.5) | 246 (81.7) | 0.05 |
| Heart Failure | 11 (8.3) | 45 (14.9) | 0.59 |
| Dyslipidemia | 61 (46.2) | 162 (54.2) | 0.12 |
| Type 2 Diabetes | 28 (21.2) | 90 (29.9) | 0.061 |
| Known IHD | 27 (20.4) | 127 (42.2) | < 0.001 |
| Prior AMI | 18 (13.5) | 92 (30.6) | < 0.001 |
| Vascular Disease# | 27 (20.4) | 82 (27.2) | 0.13 |
| Prior Stroke/TIA | 18 (13.6) | 28 (9.3) | 0.17 |
| Dementia | 1 (0.8) | 2 (0.7) | 0.91 |
| End Stage Chronic Kidney/Dialysis | 0 (0) | 6 (1.9) | 0.10 |
| COPD | 15 (11.4) | 32 (10.6) | 0.82 |
| Statins at admission | 50 (37.9) | 148 (49.2) | 0.029 |
| Anti-platelets at admission | < 0.001 | ||
| Single | 49 (37.1) | 147 (48.8) | |
| DAPT | 8 (6.1) | 46 (15.3) | |
| Acute Coronary Syndrome Yes | 78 (58.6) | 149 (49.5) | 0.07 |
| Type of CAD | < 0.001 | ||
| Obstructive CAD | 83 (62.4) | 236 (78.4) | |
| Non-obstructive CAD | 50 (37.6) | 65 (21.6) | |
| Creatinine (mg/dl) mean ± SD | 0.85 ± 0.30 | 1.07 ± 0.54 | < 0.001 |
| Platelet Count (× 103) mean ± SD | 241.6 ± 71.5 | 209.8 ± 58.0 | < 0.001 |
| Hemoglobin (g/dL) media ± SD | 13.1 ± 1.5 | 14.4 ± 1.6 | < 0.001 |
| Estradiol (pg/mL) median [IQR] | 10.0 [9.5–17.0] | 24.0 [16.0–31.0] | < 0.001 |
| Testosterone (nmol/L) median [IQR] | 0.8 [0.5–1.2] | 14.1 [9.9–17.6] | < 0.001 |
| T/E2 Ratio median [IQR] | 1.8 [0.9–2.71] | 15.8 [11.5–22.0] | < 0.001 |
| Thromboxane (pg/ml), median [IQR]* | 152.0 [116.0–187.0] | 147.3 [96.0–220.6] | 0.40 |
| NO (uM) median [IQR]* | 21.5 [12.5–30.2] | 17.9 [8.1–38.8] | 0.39 |
AMI Acute Myocardial Infarction, BMI body mass index, CAD coronary artery disease, COPD chronic obstructive pulmonary disease, DAPT dual-antiplatelet therapy, Hx history, PAD TIA transient ischemic attack
*Data available on 428 patients
#Peripheral artery disease and/or Carotid Stenosis
The serum levels of TxB2 and NO were not different between males and females (Table 1).
The ranges of the sex-specific quartiles of T/E2 ratio were as follows: (1) male group (Q1 < 11.63; Q2 = 11.63–15.93; Q3 = 15.94–22.19; Q4 > 22.19); (2) female group (Q1 < 0.89; Q2 = 0.89–1.76; Q3 = 1.76–2.71; Q4 > 2.71).
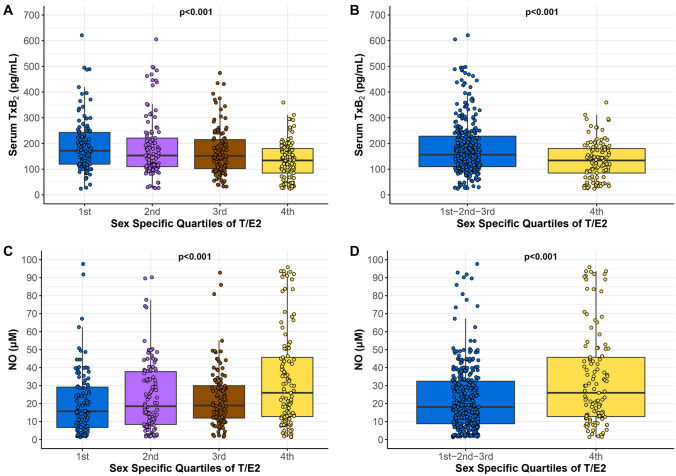
When considering the entire cohort based on sex-specific quartiles of the T/E2 ratio, we observed a progressive decrease of TxB2 and a progressive increase of NO across the increasing T/E2 sex-specific quartiles (Fig. 2A and B). Specifically, participants in Q4 showed lower levels of serum TxB2 (134 [78–181] vs. 158 [110–231] pg/ml; p < 0.001) and higher levels of NO 26.0 [12.7–46.1] vs. 18.1 [8.7–32.5] µM; p < 0.001), compared to the other quartiles (Q1-3) (Fig. 2C and D).
Fig. 2.
Levels of Vasoactive Molecules by Sex-specific Quartiles of T/E2 Ratio. Serum thromboxane B2 (TxB2) across quartiles of T/E2 (A) and comparing the highest versus the other quartiles of T/E2 ratio (I–II–III vs IV) (B); Serum nitric oxide (NO) across quartiles of T/E2 (C) comparing the highest versus the other quartiles of T/E2 ratio (I–II–III vs IV) (D). TxB2 and NO levels were compared with Mann–Whitney U (for the comparisons between two groups, I–II–III vs IV) and Kruskal–Wallis H (for the comparisons between three or more group)
During a median of 23.7 (IQR 11.7–38.8) months of follow-up, 41 patients died (16 cardiac deaths, 3 fatal strokes, 8 cardiovascular deaths, 14 non-vascular deaths).
Patients who died were older (75.5 ± 10.9 vs. 65.9 ± 10.7; p < 0.0001), more likely to have obstructive coronary disease (87.8% vs. 72%; p = 0.029) and, to have an ACS (65.9% vs. 50.9%; p = 0.06), and to be females (43.9% vs. 29.3%; p = 0.05).
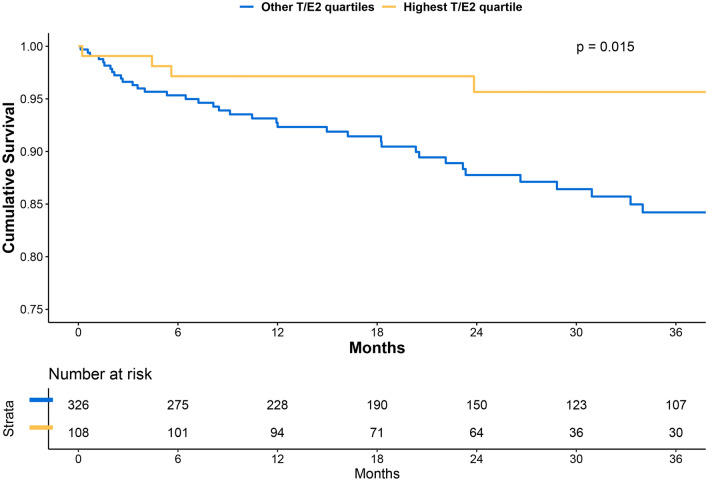
The rate of all-cause death was lower among adults in the sex-adjusted T/E2 highest quartile than those in the other quartiles (Q1-3) (3.7% vs. 11.3%; p = 0.015) (Fig. 3).
Fig. 3.
Cumulative Incidence of All-cause Death by Sex-specific T/E2 Quartiles. Log-Rank test was used to compare the two groups
At univariate Cox regression analyses, the sex-adjusted T/E2, the lower quartiles (Q1-3 vs. Q4 as reference group) (HR 3.333; 95% CI 1.187–9.355; p = 0.022), and age (HR 1.103; 95% CI 1.064–1.143; p < 0.001) were significantly associated with mortality; female sex (HR 1.668; 95% CI 0.929–3.098; p = 0.086), ACS presentation (HR 1.788; 95% CI 0.943–3.390), and obstructive CAD (HR 2.514; 0.986–6.408; p = 0.053) showed a tendency to be associated with mortality.
A multivariable Cox regression analysis showed that the lower quartiles of sex-adjusted T/E2 (HR 3.487; 95% CI 1.241–9.798; p = 0.018) and age (HR 1.100; 95% CI 1.062–1.138; p < 0.001) were independently associated with mortality after adjusting for sex, ACS presentation and obstructive type of CAD).
In vitro study
To confirm the interplay of sex-adjusted T/E2 ratio and platelet function, platelets from healthy volunteers (3 males, mean age 60.7 ± 6.0 and 3 females, mean age 63.3 ± 4.2) were incubated with sex-adjusted quartiles of the T/E2 ratio and stimulated with STC of collagen. Priming platelets with T/E2 ratio resulted in a strong potentiation of platelet aggregation and TxB2 biosynthesis induced by STC of collagen, as shown in Fig. 4. However, the sex-adjusted T/E2 Q4 induced less pronounced priming of platelet activation.
Fig. 4.
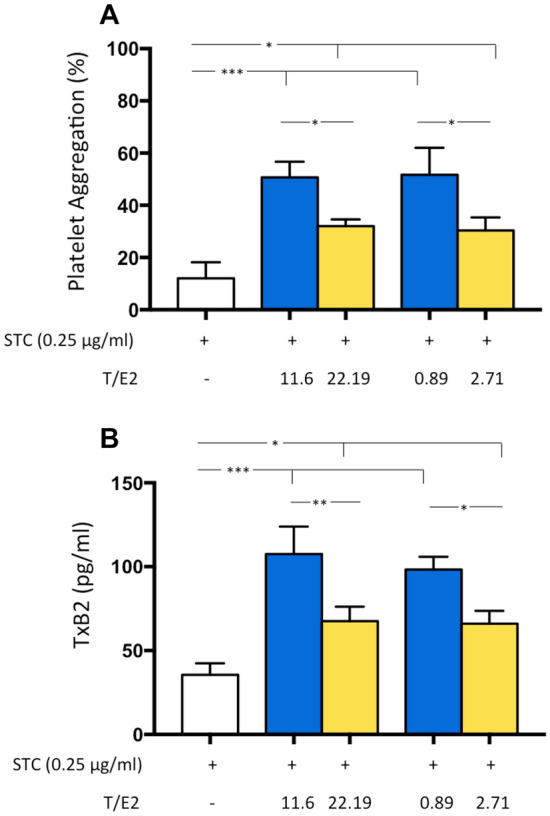
Sex-specific Quartiles of T/E2 Ratio and Platelet Activation. Platelet aggregation (A) and TxB2 biosynthesis (B) were evaluated in platelets from healthy subjects incubated with different T/E2 ratio, 11.63 or 22.19 corresponding to the lowest and highest quartiles of the T/E2 ratio for male and 0.897 or 2.71 corresponding to the lowest and highest quartiles of the T/E2 ratio for female, before stimulation with a subthreshold concentration of collagen (STC, 0.25 μg/ml). Data shown are means ± SD and were compared with Mann–Whitney U (for the comparisons between two groups) and Kruskal–Wallis H (for the comparisons between three or more group). *p < 0.05; **p < 0.01; ***p < 0.001
Discussion
In an Italian cohort of consecutive hospitalized patients with IHD, the sex-specific lower T/E2 ratios were associated with an increased risk of adverse fatal event during a long-term follow-up. The association with fatal events persisted after adjustment for age, clinical presentation, and type of CAD. The assessment of in vivo vasoactive molecules and the in vitro experiments demonstrated that the lower sex-specific T/E2 ratios induced an increase in platelet thromboxane release and a decrease in NO bioavailability that may partially explain why endogenous sex hormones favors the occurrence of fatal adverse events.
Despite advancements in diagnostics and therapeutics, IHD has a high burden globally both in males and females, CVD being the leading cause of mortality worldwide [18]. The role of sex hormones and their implications in vascular health is a matter of debate in the scientific community [19]. Despite biologically plausible pathological pathways linking endogenous sex hormones and clinical adverse events, prospective studies have yielded conflicting results [8, 20]. Of note, the same category of sex hormones exerts a different effect depending on the individual’s sex. For example, in males, several studies have demonstrated the increased endogenous T levels, as well as elevated luteinizing hormone and sex hormone-binding globulin, were associated with a decrease in CV events [21, 22]. Conversely, among female individuals, some studies reported a protective effect of elevated E2 levels in terms of IHD development and progression while an increased risk with elevated FSH [23]. The number of challenges faced in understanding the interrelations between sex hormones, biological sex, and vascular health has fostered a research approach based on the use of ratio between T and E2 rather than the absolute concentration of individual hormones. In fact, a balanced T/E2 ratio is needed for contrasting early-stage atherosclerosis [24]. Accordingly, we used such approach in a cohort of hospitalized female and male individuals with IHD to assess the sex-specific effect of T/E2 ratios on vasoactive biomarkers that reflect the propensity to develop myocardial ischemia. The lower sex-specific T/E2 ratios among adults with ischemia resulted in higher TxB2 and lower NO levels, suggesting that the contribution of sex hormones is mediated, at least in part, by their effect on vasoactive molecules.
However, the vasoactive theory is not the only one that could explain the increased platelet reactivity. Platelets from females are more reactive in response to various agonists than those of male counterparts [12, 25]. Sex hormones may partially be responsible for such sex difference in platelet function. It has been suggested that sex hormones exert either a non-genomic effect directly on platelets or a genomic effect on megakaryocytes. Administration of testosterone to healthy men was shown to increase the thromboxane A2 receptor expression and was associated with an increased platelet activation [26]. Furthermore, the impact of reproductive age (i.e., pre- versus post-menopause), as well as the effect of hormone replacement therapy in post-menopause on female platelets has been explored both in experimental models and humans although with discordant results, likely related with the different approaches used for assessing the platelet function (e.g., flow cytometry or surrogate markers such as mean platelet volume). In fact, while initially the platelet activation assessed in female subjects through flow cytometry resulted in conflicting data [27, 28], later on evidence supported that proteins [29], mRNAs and miRNAs [30] are differentially expressed by sex in platelets and changes in platelet reactivity in relation to the hormonal status. Of note, administration of estradiol to mice has been shown to change the expression level of the collagen receptor GPVI [31] and of the cytoskeletal protein beta-tubulin [32]. The advantage of using sex-adjusted T/E2 ratios is to account for the well-known differences in sex hormone system along the lifespan of individuals, regardless of the reproductive age.
The mechanisms responsible for the detrimental effect of the sex-specific lower T/E2 ratios on vascular health and clinical outcomes are not clearly elucidated. Recently, clinical studies have also explored the contribution of testosterone in cardiovascular disease [33] sometimes with contradictory results. The MrOS prospective study of 552 elderly male patients found no relationship between sex hormones levels (i.e., testosterone and T/E2 ratio quartiles) and the risk of cardiovascular events [34]. Conversely, our study includes younger patients of both sexes, and we found that lower T/E2 quartiles were associated with increased risk of all-cause death. Taken together, these results may underlie how the effect of sex hormones can be different across age strata, perhaps with increased importance in younger cohorts. However, further confirmation is needed to support this hypothesis. Indeed, in the MESA (Multi-Ethnic Study of Atherosclerosis) study among racially/ethnically diverse 2834 post-menopausal women with long-term follow-up, a higher T/E2 ratio was associated with an elevated risk for incident CVD [8]. In contrast, in men, the opposite pattern is seen with low testosterone being associated with endothelial dysfunction and CHD. Prior work has shown that in males with atherosclerotic disease, the impairment of vascular health has been mainly related to inflammatory milieu and to the endocrine function. In fact, among 611 male carotid endarterectomy patients included in the Athero-Express Biobank Study, low T/E2 ratio was associated with increased systemic inflammation and an increased risk of future CV events [7]. Notably, the BMI resulted as an important effect modifier of T/E2 ratio effect on future events, suggesting that the aromatase activity that produces E2 via conversion of T in the visceral/abdominal adipose tissue can be linked to a pro-inflammatory and more vulnerable pattern of the atherosclerotic disease. Beyond the metabolic pattern, we hypothesized that activated platelets, which are major pathogenetic players in myocardial ischemia and express sex hormone receptors on their surface, release potent molecules favoring vasoconstriction, explaining at least in part the effect of sex hormone balance on vascular status. More specifically, platelets have been reported to contribute to the coronary microvascular dysfunction by several mechanisms that include forming distal micro-emboli, adhering to re-perfused endothelium, releasing vasoconstrictor or toxic molecules and inflammatory mediators that further enhance the activation of the endothelial monolayer and the recruitment of circulating neutrophils [35–37]. Hyperactive platelets are therefore implicated in the pathogenesis of ischemia. Of note, the platelet function has been reported to be different between males and females [38, 39]. Of note, according to the available literature, platelets from men and women express comparable levels of AR and ERbeta and of COX1 [40]. However, testosterone regulates AR expression in megakaryocytes in a non-linear manner (i.e., low testosterone upregulates AR, while high testosterone downregulates AR) and this may account at least in part for the different effects of sex hormones. Moreover, the non-genomic signaling pathways activated by these receptors are still poorly understood. Thus, we cannot exclude that sex differences in the expression of signaling proteins downstream of these receptors may contribute to the different effects.
Among molecules released during platelet activation, TxB2 production represents an amplification mechanism of platelet aggregation. As we observed in vivo that the lower sex-adjusted T/E2 ratios among adults with ischemia resulted in higher TxB2, we performed in vitro experiments to better define the role of sex hormones in platelet activation. We found that the incubation of human platelets with sex-specific quartiles of T/E2 results in a strong potentiation of platelet aggregation and TxB2 biosynthesis confirming the role of sex-specific T/E2 in modulating platelet function. However, we observed that the highest sex-adjusted T/E2 quartile induced less pronounced priming of platelet activation, suggesting that the strategy to optimize the balance between sex hormone may play a role in the regulation of platelet function.
Strengths and limitations
The present study has several strengths worth mentioning. Through a translational approach, we provided sex-specific evidence that supported a platelet-mediated mechanism on how endogenous hormones affect vascular health and consequently clinical outcome. Fostering the understanding of sex disparities in adverse outcomes among individuals with IHD is a remarkable priority to reduce the global burden of CVD and achieve equity in cardiovascular health [3, 18].
This study should be interpreted in the context of several limitations. As any observational cohort study, some confounders might not have been assessed and could influence our final multivariate model, as could any missing data. The findings refer to a selected cohort of Italian individuals at very high cardiovascular risk, hospitalized for an ischemic event, at a single center, limiting the generalizability of our results. A larger participation of female in our study and a higher rate of adverse events would have increase the clinical relevance of our findings. Also, due to sample size limitation, we were unpowered to explore whether the relationship between T/E2 ratio and platelet activations may differ in patients with obstructive vs. non-obstructive CAD; further studies are required to evaluate whether significant related differences may exist. Moreover, due to the paucity of blood samples for some participants, we could not assess the sex hormones balance in the original cohort of 509 participants. Finally, local metabolism of testosterone to estrogen by aromatase in cardiac tissue [41] adds complexity in the understanding hormonal modulation of cardiac and coronary vascular function. Unfortunately, serum concentrations of the hormones may not also reflect the contribution of hormones tissue metabolism.
Finally, vasoactive molecules other than platelet TxB2 biosynthesis and NO should be investigated along with the contribution of other cellular lines, such as endothelial cells, to better define the effect of sex hormones balance on platelet function.
Conclusion
Among individuals with IHD, the sex-specific higher T/E2 ratio was associated with a lower long-term risk of fatal events among adults with IHD. The effect of the T/E2 ratio on the platelet TxB2 release may partially explain such finding and foster the development of sex-specific tailored strategy to counteract hormone-related platelet activity. Therefore, further larger prospective clinical study should be designed to assess whether measuring endogenous sex hormones, regardless of age, can contribute to a better sex-specific stratification and management of adverse clinical outcomes in individuals with IHD.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
EVA Collaborative Group: Claudio Tiberti, Federica Panimolle, Andrea Isidori, Elisa Giannetta, Mary Anna Venneri, Laura Napoleone, Marta Novo, Silvia Quattrino, Simona Ceccarelli, Eleni Anastasiadou, Francesca Megiorni, Cinzia Marchese (Department of Experimental Medicine, Medical Physiopathology, Food Science and Endocrinology Section, Sapienza University of Rome, Rome, Italy); Enrico Mangieri, Gaetano Tanzilli, Nicola Viceconte, Francesco Barillà, Carlo Gaudio, Vincenzo Paravati, Guglielmo Tellan, Evaristo Ettorre, Adriana Servello, Fabio Miraldi, Andrea Moretti, Alessandra Tanzilli, Piergiovanni Mazzonna, Suleyman Al Kindy, Riccardo Iorio, Martina Di Iorio, Gennaro Petriello, Laura Gioffrè, Eleonora Indolfi, Gaetano Pero, Nino Cocco, Loredana Iannetta, Sara Giannuzzi, Emilio Centaro, Sonia Cristina Sergi (Department of Cardiovascular, Respiratory, Nephrologic, Anaesthesiologic and Geriatric Sciences, Sapienza University of Rome, Rome, Italy); Pasquale Pignatelli, Daria Amoroso, Simona Bartimoccia, Giovanni Talerico, Salvatore Minisola, Sergio Morelli, Antonio Fraioli, Silvia Nocchi, Mario Fontana (Department of Internal Medicine and Medical Specialties, Sapienza University of Rome, Rome, Italy); Filippo Toriello, Eleonora Ruscio, Tommaso Todisco, Nicolò Sperduti, Giuseppe Santangelo, Giacomo Visioli, Marco Vano, Marco Borgi, Ludovica Maria Antonini, Silvia Robuffo, Claudia Tucci, Agostino Rossoni, Valeria Spugnardi, Annarita Vernile, Mariateresa Santoliquido, Verdiana Santori, Giulia Tosti, Fabrizio Recchia, Francesco Morricone, Roberto Scacciavillani, Alice Lipari, Andrea Zito, Floriana Testa, Giulia Ricci, Ilaria Vellucci, Marianna Vincenti, Silvia Pietropaolo, Camilla Scala, Nicolò Rubini, Marta Tomassi, Gloria Rozzi, Floriana Santomenna, Claudio Cantelmi, Giacomo Costanzo, Lucas Rumbolà, Salvatore Giarrizzo, Carlotta Sapia, Biagio Scotti (Department of Translational and Precision Medicine, Sapienza University of Rome, Rome, Italy); Danilo Toni, Anne Falcou (Emergency Department Stroke Unit, Sapienza University of Rome, Rome, Italy); Louise Pilote, Amanpreet Kaur, Zhara Azizi (McGill University Health Centre Research Institute, Centre for Outcomes Research and Evaluation, Montreal, QC, Canada); Anna Rita Vestri (Department of Public Health and Infectious Disease, Sapienza University of Rome, Roma, Italy); Patrizia Ferroni (San Raffaele Roma Open University and Inter-institutional Multidisciplinary Biobank, IRCCS San Raffaele Pisana, Rome, Italy); Clara Crescioli, Cristina Antinozzi, Francesca Serena Pignataro (Department of Movement, Human and Health Sciences Section of Health Sciences, Unit of Endocrinology, Università degli Studi di Roma "Foro Italico", Rome, Italy); Tiziana Bellini (Department of Biomedical and Specialty Surgical Sciences, University of Ferrara, Ferrara, Italy); Giovanni Zuliani, Angelina Passaro, Brombo Gloria, Andrea Cutini, Eleonora Capatti, Edoardo Dalla Nora, Francesca Di Vece, Andrea D’Amuri, Tommaso Romagnoli, Francesco Luciani, Michele Polastri, Alessandra Violi, Valeria Fortunato, Alessandro Bella (Department of Translational Medicine, University Internal Medicine Unit, University Hospital - Arcispedale Sant'Anna, University of Ferrara, Ferrara, Italy); Roberto Manfredini, Alfredo De Giorgi, Fabio Fabbian (Clinica Medica Unit, University Hospital - Arcispedale Sant'Anna, Department of Medical Sciences, University of Ferrara, Ferrara, Italy); Roberto Carnevale (Department of Medico-Surgical Sciences and Biotechnologies, Sapienza University of Rome, Latina, Italy); Cristina Nocella (Department of AngioCardioNeurology, IRCCS NeuroMed, Pozzilli, Italy); Carlo Catalano, Iacopo Carbone, Nicola Galea (Department of Radiological, Oncological and Pathological Sciences, Sapienza University of Rome, Rome, Italy); Giuliano Bertazzoni, Marianna Suppa, Antonello Rosa, Gioacchino Galardo, Maria Alessandroni (Department of Emergency Medicine, Policlinico Umberto I, Sapienza University of Rome, Rome, Italy); Alessandro Coppola, Mariangela Palladino (Chest Pain Unit, Policlinico Umberto I, Rome, Italy); Giulio Illuminati, Fabrizio Consorti (Department of Surgical Sciences, Sapienza University of Rome, Rome, Italy); Paola Mariani, Fabrizio Neri, Paolo Salis, Antonio Segatori, Laurent Tellini, Gianluca Costabile (Nursing Team Catheterization Lab Policlinico Umberto I, Rome, Italy).
Author contributions
VR, MP and SB conceived the study; CN, SB, LS, VC and RC designed and performed laboratory experiments; VR, BC, GFR, NV and GT perform clinical investigation and enrolled patients; VR, MP, GFR, BC and RC analyzed data; VR and RC drafted the first version of the manuscript; AL and LP revised the manuscript and gave important intellectual contributions.
Funding
Open access funding provided by Università degli Studi di Ferrara within the CRUI-CARE Agreement. This work was supported by the Italian Ministry of Education, University and Research (MIUR)—Scientific Independence of young Investigators (SIR) program (RBSI14HNVT).
Declarations
Conflict of interest
SB received research grant from MSD, outside the scope of this manuscript. SB and VR are members of the Editorial Board of JEI. All other Authors have nothing to disclose.
Research involving human participants and/or animals
The study was conducted in full conformance with the Declaration of Helsinki principles, and it was approved by the local Ethics Committee of Policlinico Umberto I, Sapienza University of Rome, Rome, Italy (reference 3786, 24/09/2015).
Informed consent
All participants provided informed written consent prior to their participation.
Footnotes
Full names of EVA Collaborators are listed in the Acknowledgements section.
The original online version of this article was revised to add missing OASIS funding note.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
V. Raparelli, Email: valeria.raparelli@unife.it
The EVA Collaborators:
Claudio Tiberti, Federica Panimolle, Andrea Isidori, Elisa Giannetta, Mary Anna Venneri, Laura Napoleone, Marta Novo, Silvia Quattrino, Simona Ceccarelli, Eleni Anastasiadou, Francesca Megiorni, Cinzia Marchese, Enrico Mangieri, Gaetano Tanzilli, Nicola Viceconte, Francesco Barillà, Carlo Gaudio, Vincenzo Paravati, Guglielmo Tellan, Evaristo Ettorre, Adriana Servello, Fabio Miraldi, Andrea Moretti, Alessandra Tanzilli, Piergiovanni Mazzonna, Suleyman Al Kindy, Riccardo Iorio, Martina Di Iorio, Gennaro Petriello, Laura Gioffrè, Eleonora Indolfi, Gaetano Pero, Nino Cocco, Loredana Iannetta, Sara Giannuzzi, Emilio Centaro, Sonia Cristina Sergi, Pasquale Pignatelli, Daria Amoroso, Simona Bartimoccia, Giovanni Talerico, Salvatore Minisola, Sergio Morelli, Antonio Fraioli, Silvia Nocchi, Mario Fontana, Filippo Toriello, Eleonora Ruscio, Tommaso Todisco, Nicolò Sperduti, Giuseppe Santangelo, Giacomo Visioli, Marco Vano, Marco Borgi, Ludovica Maria Antonini, Silvia Robuffo, Claudia Tucci, Agostino Rossoni, Valeria Spugnardi, Annarita Vernile, Mariateresa Santoliquido, Verdiana Santori, Giulia Tosti, Fabrizio Recchia, Francesco Morricone, Roberto Scacciavillani, Alice Lipari, Andrea Zito, Floriana Testa, Giulia Ricci, Ilaria Vellucci, Marianna Vincenti, Silvia Pietropaolo, Camilla Scala, Nicolò Rubini, Marta Tomassi, Gloria Rozzi, Floriana Santomenna, Claudio Cantelmi, Giacomo Costanzo, Lucas Rumbolà, Salvatore Giarrizzo, Carlotta Sapia, Biagio Scotti, Danilo Toni, Anne Falcou, Louise Pilote, Amanpreet Kaur, Zhara Azizi, Anna Rita Vestri, Patrizia Ferroni, Clara Crescioli, Cristina Antinozzi, Francesca Serena Pignataro, Tiziana Bellini, Giovanni Zuliani, Angelina Passaro, Brombo Gloria, Andrea Cutini, Eleonora Capatti, Edoardo Dalla Nora, Francesca Di Vece, Andrea D’Amuri, Tommaso Romagnoli, Francesco Luciani, Michele Polastri, Alessandra Violi, Valeria Fortunato, Alessandro Bella, Roberto Manfredini, Alfredo De Giorgi, Fabio Fabbian, Roberto Carnevale, Cristina Nocella, Carlo Catalano, Iacopo Carbone, Nicola Galea, Giuliano Bertazzoni, Marianna Suppa, Antonello Rosa, Gioacchino Galardo, Maria Alessandroni, Alessandro Coppola, Mariangela Palladino, Giulio Illuminati, Fabrizio Consorti, Paola Mariani, Fabrizio Neri, Paolo Salis, Antonio Segatori, Laurent Tellini, and Gianluca Costabile
References
- 1.Timmis A, Townsend N, Gale CP, et al. European society of Cardiology: cardiovascular disease statistics 2019 (executive summary) Eur Hear J Qual Care Clin Outcomes. 2020;6:7–9. doi: 10.1093/ehjqcco/qcz065. [DOI] [PubMed] [Google Scholar]
- 2.Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020;141:E139–E596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 3.Perrino C, Ferdinandy P, Bøtker HE, et al. Improving translational research in sex-specific effects of comorbidities and risk factors in ischaemic heart disease and cardioprotection: position paper and recommendations of the ESC Working Group on Cellular Biology of the Heart. Cardiovasc Res. 2021;117:367–385. doi: 10.1093/cvr/cvaa155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aggarwal NR, Patel HN, Mehta LS, et al. Sex differences in ischemic heart disease: advances, obstacles, and next steps. Circ Cardiovasc Qual Outcomes. 2018;11:e004437. doi: 10.1161/CIRCOUTCOMES.117.004437. [DOI] [PubMed] [Google Scholar]
- 5.Arnold AP, Cassis LA, Eghbali M, et al. Sex hormones and sex chromosomes cause sex differences in the development of cardiovascular diseases. Arterioscler Thromb Vasc Biol. 2017;37:746–756. doi: 10.1161/ATVBAHA.116.307301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Figtree GA, Ngo DTM, Bubb KJ. Testosterone to estradiol ratio and plaque inflammation: mechanistic insights and biomarker potential? Cardiovasc Res. 2019;115:255–257. doi: 10.1093/cvr/cvy260. [DOI] [PubMed] [Google Scholar]
- 7.Van Koeverden ID, De Bakker M, Haitjema S, et al. Testosterone to oestradiol ratio reflects systemic and plaque inflammation and predicts future cardiovascular events in men with severe atherosclerosis. Cardiovasc Res. 2019;115:453–462. doi: 10.1093/cvr/cvy188. [DOI] [PubMed] [Google Scholar]
- 8.Zhao D, Guallar E, Ouyang P, et al. Endogenous sex hormones and incident cardiovascular disease in post-menopausal women. J Am Coll Cardiol. 2018;71:2555–2566. doi: 10.1016/j.jacc.2018.01.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lagranha CJ, Deschamps A, Aponte A, et al. Sex differences in the phosphorylation of mitochondrial proteins result in reduced production of reactive oxygen species and cardioprotection in females. Circ Res. 2010;106:1681–1691. doi: 10.1161/CIRCRESAHA.109.213645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ventura-Clapier R, Dworatzek E, Seeland U, et al. Sex in basic research: concepts in the cardiovascular field. Cardiovasc Res. 2017;113:711–724. doi: 10.1093/cvr/cvx066. [DOI] [PubMed] [Google Scholar]
- 11.Regitz-Zagrosek V, Kararigas G. Mechanistic pathways of sex differences in cardiovascular disease. Physiol Rev. 2017;97:1–37. doi: 10.1152/physrev.00021.2015. [DOI] [PubMed] [Google Scholar]
- 12.Wang TY, Angiolillo DJ, Cushman M, et al. Platelet biology and response to antiplatelet therapy in women: Implications for the development and use of antiplatelet pharmacotherapies for cardiovascular disease. J Am Coll Cardiol. 2012;59:891–900. doi: 10.1016/j.jacc.2011.09.075. [DOI] [PubMed] [Google Scholar]
- 13.Moro L, Reineri S, Piranda D, et al. Nongenomic effects of 17β-estradiol in human platelets: potentiation of thrombin-induced aggregation through estrogen receptor β and Src kinase. Blood. 2005;105:115–121. doi: 10.1182/blood-2003-11-3840. [DOI] [PubMed] [Google Scholar]
- 14.Raparelli V, Proietti M, Lenzi A, et al. Sex and gender differences in ischemic heart disease: endocrine vascular disease approach (EVA) study design. J Cardiovasc Transl Res. 2020;13:14–25. doi: 10.1007/s12265-018-9846-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pasupathy S, Tavella R, Beltrame JF. Myocardial infarction with nonobstructive coronary arteries (MINOCA): the past, present, and future management. Circulation. 2017;135:1490–1493. doi: 10.1161/CIRCULATIONAHA.117.027666. [DOI] [PubMed] [Google Scholar]
- 16.Kunadian V, Chieffo A, Camici PG, et al. An EAPCI Expert Consensus Document on Ischaemia with Non-Obstructive Coronary Arteries in Collaboration with European Society of Cardiology Working Group on Coronary Pathophysiology & Microcirculation Endorsed by Coronary Vasomotor Disorders International Study Group. Eur Heart J. 2020;41:3504–3520. doi: 10.1093/eurheartj/ehaa503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah B, Sedlis SP, Mai X, et al. Comparison of platelet activity measurements by use of arterial and venous blood sampling. J Thromb Haemost. 2013;11:1922–1924. doi: 10.1111/jth.12370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vogel B, Acevedo M, Appelman Y, et al. The lancet women and cardiovascular disease commission: reducing the global burden by 2030. Lancet. 2021 doi: 10.1016/S0140-6736(21)00684-X. [DOI] [PubMed] [Google Scholar]
- 19.Type 2 diabetes in adults: management | Guidance and guidelines | NICE
- 20.Subramanya V, Zhao D, Ouyang P, et al. Association of endogenous sex hormone levels with coronary artery calcium progression among post-menopausal women in the Multi-Ethnic Study of Atherosclerosis (MESA) J Cardiovasc Comput Tomogr. 2019;13:41–47. doi: 10.1016/j.jcct.2018.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boardman HMP, Hartley L, Eisinga A. Hormone therapy for preventing cardiovascular disease in post-menopausal women. Cochrane Database Syst Rev. 2015;3:CD002229–10.1002/14651858.CD002229.pub4. doi: 10.1002/14651858.CD002229.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan YX, Knuiman MW, Hung J, et al. Neutral associations of testosterone, dihydrotestosterone and estradiol with fatal and non-fatal cardiovascular events, and mortality in men aged 17–97 years. Clin Endocrinol (Oxf) 2016;85:575–582. doi: 10.1111/cen.13089. [DOI] [PubMed] [Google Scholar]
- 23.Wang N, Shao H, Chen Y, et al. Follicle-stimulating hormone, its association with cardiometabolic risk factors, and 10-year risk of cardiovascular disease in postmenopausal women. J Am Heart Assoc. 2017 doi: 10.1161/JAHA.117.005918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dai W, Ming W, Li Y, et al. Synergistic effect of a physiological ratio of estradiol and testosterone in the treatment of early-stage atherosclerosis. Arch Med Res. 2015;46:619–629. doi: 10.1016/j.arcmed.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 25.Zuern CS, Lindemann S, Gawaz M. Platelet function and response to aspirin: gender-specific features and implications for female thrombotic risk and management. Semin Thromb Hemost. 2009;35:295–306. doi: 10.1055/s-0029-1222608. [DOI] [PubMed] [Google Scholar]
- 26.Ajayi AAL, Mathur R, Halushka PV. Testosterone increases human platelet thromboxane A2 receptor density and aggregation responses. Circulation. 1995;91:2742–2747. doi: 10.1161/01.CIR.91.11.2742. [DOI] [PubMed] [Google Scholar]
- 27.Aldrighi JM, Oliveira RLS, D’Amico É, et al. Platelet activation status decreases after menopause. Gynecol Endocrinol. 2005;20:249–257. doi: 10.1080/09513590500097549. [DOI] [PubMed] [Google Scholar]
- 28.Roshan TM, Normah J, Rehman A, Naing L. Effect of menopause on platelet activation markers determined by flow cytometry. Am J Hematol. 2005;80:257–261. doi: 10.1002/ajh.20472. [DOI] [PubMed] [Google Scholar]
- 29.Koupenova M, Mick E, Mikhalev E, et al. Sex differences in platelet toll-like receptors and their association with cardiovascular risk factors. Arterioscler Thromb Vasc Biol. 2015;35:1030–1037. doi: 10.1161/ATVBAHA.114.304954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Simon LM, Edelstein LC, Nagalla S, et al. Human platelet microRNA-mRNA networks associated with age and gender revealed by integrated plateletomics. Blood. 2014 doi: 10.1182/blood-2013-12-544692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leng XH, Zhang W, Nieswandt B, Bray PF. Effects of estrogen replacement therapies on mouse platelet function and glycoprotein VI levels. Circ Res. 2005;97:415–417. doi: 10.1161/01.RES.0000181025.43762.cf. [DOI] [PubMed] [Google Scholar]
- 32.Valéra MC, Gratacap MP, Gourdy P, et al. Chronic estradiol treatment reduces platelet responses and protects mice from thromboembolism through the hematopoietic estrogen receptor α. Blood. 2012;120:1703–1712. doi: 10.1182/blood-2012-01-405498. [DOI] [PubMed] [Google Scholar]
- 33.Kaur H, Werstuck GH. The effect of testosterone on cardiovascular disease and cardiovascular risk factors in men: a review of clinical and preclinical data. CJC Open. 2021;3:1238–1248. doi: 10.1016/j.cjco.2021.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Collet TH, Ewing SK, Ensrud KE, et al. Endogenous testosterone levels and the risk of incident cardiovascular events in elderly men: the MrOS prospective study. J Endocr Soc. 2020 doi: 10.1210/jendso/bvaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gavins FNE, Li G, Russell J, et al. Microvascular thrombosis and CD40/CD40L signaling. J Thromb Haemost. 2011;9:574–581. doi: 10.1111/j.1538-7836.2010.04176.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Niccoli G, Scalone G, Lerman A, Crea F. Coronary microvascular obstruction in acute myocardial infarction. Eur Heart J. 2016;37:1024–1033. doi: 10.1093/eurheartj/ehv484. [DOI] [PubMed] [Google Scholar]
- 37.Stokes KY, Granger DN. Platelets: a critical link between inflammation and microvascular dysfunction. J Physiol. 2012;590:1023–1034. doi: 10.1113/jphysiol.2011.225417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gurbel PA, Becker RC, Mann KG, et al. Platelet function monitoring in patients with coronary artery disease. J Am Coll Cardiol. 2007;50:1822–1834. doi: 10.1016/j.jacc.2007.07.051. [DOI] [PubMed] [Google Scholar]
- 39.Lau ES, Paniagua SM, Guseh JS, et al. Sex differences in circulating biomarkers of cardiovascular disease. J Am Coll Cardiol. 2019;74:1543–1553. doi: 10.1016/j.jacc.2019.06.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khetawat G, Faraday N, Nealen ML et al (2000) Human megakaryocytes and platelets contain the estrogen receptor beta and androgen receptor (AR): testosterone regulates AR expression. Blood 95:2289–2296. http://www.ncbi.nlm.nih.gov/pubmed/10733498. Accessed 17 Nov 2017 [PubMed]
- 41.Biegon A, Alexoff DL, Kim SW, et al. Aromatase imaging with [N-methyl-11C]vorozole PET in healthy men and women. J Nucl Med. 2015;56:580–585. doi: 10.2967/jnumed.114.150383. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.