Abstract
Objective: To explore the application value of mobile cabin hospitals in combating COVID-19 outbreak. Methods: The basic clinical data, the number of admission, CT scan, novel coronavirus nucleic acid testing results were collected and calculated. The operational elements of running this temporary hospital were reviewed from its construction to closing. Results: Wuhan Hanyang Mobile Cabin Hospital was transformed from Hall B1 of Wuhan International Expo Center. With a total of 930 beds in this temporary hospital, 1,028 patients were admitted, among them, 598 patients were cured, and 430 patients were transferred to designated hospitals in the special period. Totally, 1,206 mobile CT scan were conducted. 2,295 novel coronavirus nucleic acid tests were performed, among which, 1,032 tests showed two continuous negative results, 924 tests with one negative, while 302 tests with positive result (13.16%). No nosocomial infection of working staff was found due to the conduction of multiple measures. The patients’ livelihoods were well safeguarded in mobile cabin hospitals. Conclusion: The mobile cabin hospital compulsory quarantine for mild patients can serve as an alternative method to combat COVID-19.
Keywords: Infectious diseases, novel coronavirus, coronavirus disease 2019 (COVID-19), mobile cabin hospitals, prevention and control measures
Introduction
At the end of 2019, there was an outbreak of coronavirus disease 2019 (COVID-19) epidemic in Wuhan, China. Due to its long incubation period, atypical symptoms, multiple organ dysfunction, and insufficient medical resources in the early stages, the mortality rate of COVID-19 was estimated at 6%-10% [1-5]. Furthermore, COVID-19 displayed an unprecedented rate of transmission, with a basic reproduction number (R0) of about 2-3, hence the number of cases rose sharply from 41 cases on December 30, to 14,557 on February 3, including 14,411 cases in China and 146 cases in 22 other countries [6-9]. This situation led to a series of problems, such as a shortage of hospital beds, intense pressure on medical resources, and an overflow of patients in the designated hospitals. In the early stage of the epidemic outbreak, the Chinese government adopted home quarantine measures for patients with mild symptoms. However, outbreaks in familial clusters became one of the major routes of transmission at the later stage, and the previous home quarantine approach failed to effectively control the epidemic [3]. The disease continued spreading within households, which became major sources of infection. This vicious cycle sustained the spread of COVID-19, resulting in an ongoing exponential growth of new and suspected cases (Figure 1, data from the daily news announced by Chinese National Health Commission). Moreover, due to insufficient medical resources, a large number of patients were unable to receive effective treatment, which increased the mortality rate [10-12].
Figure 1.
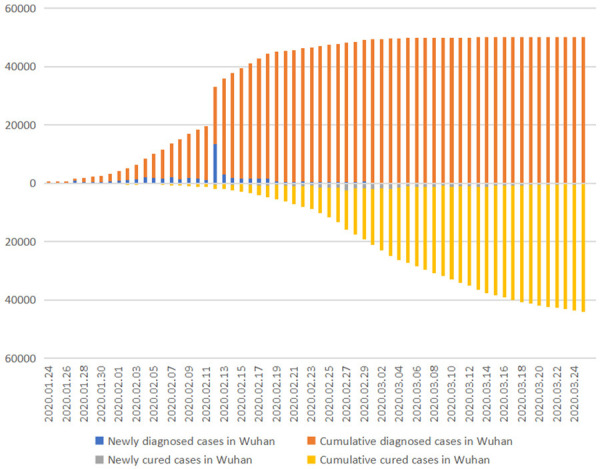
Demographics of newly diagnosed and cured cases, cumulative diagnoses and cured cases over time in Wuhan.
On February 3, 2020, Mobile Cabin Hospital (MCH) policy were conducted by China’s central government to cut off the sources of infection and prevent the deterioration of patients’ conditions, thus curbing the epidemic. The so-called mobile cabin hospitals were originally wartime field hospitals built by converting large sports centers and exhibition centers for the purposes of receiving refugees, which is not on the purpose for infectious diseases. This study intended to report the construction and fundamental contents of running MCH for this epidemic disease, so as to provide useful experiences for combatting COVID-19.
Methods
Study design and participants
The patients who met admission criteria were admitted to Hanyang MCH for central quarantine and treatment. Those who didn’t met the criteria were transferred to designated hospital. The number of admissions, clinical data, the number of CT scanning, and novel coronavirus nucleic acid testing results were collected and retrospectively analyzed. The patients who met the discharge criteria were discharged.
Admission criteria
According to the “Workbook of Mobile Cabin Hospitals (Third Edition)” released by the Bureau of Hospital Administration, Department of Medical Administration, National Health Commission of China, mild and common cases without chronic diseases like hypertension, diabetes, coronary heart disease, malignant tumors, structural lung disease, pulmonary heart disease, immunosuppression and history of mental illness, having self-care ability and independent ambulation were admitted to mobile cabin hospitals. The criteria of life sign were as follows: resting-state finger pulse oximetry SpO2 >93% and respiratory rate <30 breaths/min [13]. Those who did not meet the criteria were transferred to the designated hospital.
Discharge criteria
Relying on Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7, China) [14], patients who improved significantly underwent nucleic acid test and CT scan based on clinical presentations. Discharged criteria were as follows. [14]. (1) Normal body temperature lasted for more than three days. (2) Respiratory symptoms were improved significantly. (3) Pulmonary imaging showed significant decline of inflammation. (4) Two consecutive negative nucleic acid test results (sampling interval at least 24 h).
Novel coronavirus nucleic acid testing in Hanyang MCH was performed by KingMed Diagnostics Company. Mobile CT (Shanghai United Imaging HealthCare Co. ltd) was installed and put into use for the hospitalized patients.
A total of 1,028 patients infected with COVID-19 were enrolled, excluding 192 patients who were transferred to the designated hospital upon admission due to severe status or basic diseases, only 836 patients were treated in Hangyang MCH.
Data collection
The daily number of patients that admitted in and discharged from all mobile cabin hospitals in Wuhan and the number of newly diagnosed, cumulative diagnosed, newly cured and cumulative cured patients in Wuhan were from Chinses official news released data. The basic clinical data, the number of admissions, CT scan, novel coronavirus nucleic acid testing results were collected and calculated. The operational elements of running this temporary hospital were reviewed from its construction to closing. The ethics committee of Fujian Provincial Hospital (approval number: K2020-05-018) approved this study.
Statistical analysis
All data were analyzed with the SPSS 23 software. The data of continuous parameters were expressed as mean (variance), or median (interquartile range, IQR). Daily dynamic data were described by mapping function in the 2016 EXCEL form, the bar accumulation map was used for the number of newly diagnosed cases, admission cases, discharged cases and transferred cases in Hanyang MCH, the column accumulation diagram was used for the number of newly diagnosed cases, cumulative diagnosed cases, newly cured and cumulative cured cases in Wuhan and also the number of daily CT and nucleic acid test in Hanyang MCH. The structure of Hanyang MCH and diagrammatic sketch of the three districts and two channels were illustrated by 2017 PHOTOSHOP software, and the internal structure sketch map of Hanyang MCH was illustrated by 2016 EXCEL table.
Results
The total situation of MCH and the COVID-19 cases following the time in Wuhan
From February 3 to March 10, a total of 14 mobile cabin hospitals were set up and used in China, providing 12,365 beds [15]. All of these mobile cabin hospitals had been in operation for 35 days as of the writing of this paper, and a total of 11,309 patients had received treatment (The specific names of the mobile cabin hospitals, the number of beds, and the number of patients admitted are listed in Table 1 [16]). The using of mobile cabin hospitals had shown a significant effect on reducing transmission and slowing down the growth rate of new cases (Figure 1). Since they had operated for an incubation period of 14 days, the newly diagnosed cases dropped significantly. After two incubation periods, the number of new cases had gradually fallen to less than 10 cases. In addition, with an increase in the number of recovered patients, the number of currently confirmed cases decreased substantially (Figure 1). As a result, the trend of a rapid spreading was curbed quickly.
Table 1.
The specific names of mobile cabin hospitals, the number of beds, and the number of patients admitted in the mobile cabin hospitals in Wuhan
| Mobile Cabin Hospital Names | Locations | Competent organization | Other Units | Beds | Patients | Patients Cured and Discharged | Cabin Opening Time | Cabin Closing Time |
|---|---|---|---|---|---|---|---|---|
| Wuchang Mobile Cabin Hospital | Hongshan Stadium | Hubei Provincial People’s Hospital | NEMRT and local medical teams | 784 | 1,124 | 833 | Feb.5th | Mar.10th |
| Jianghan Mobile Cabin Hospital | Wuhan International Consultation Center | Affiliated Hospital of Huazhong University of Science and Technology, Tongji Medical College | 3 NEMRT and 5 local medical teams | 1,524 | 1,848 | 1,327 | Feb.5th | Mar.9th |
| Dongxi Lake Mobile Cabin Hospital | Wuhan Living Room Culture Expo Center | Central South Hospital of Wuhan University | 3 NEMRT and 5 local medical teams and mobile P3 laboratories | 1,461 | 1,760 | 868 | Feb.7th | Mar.8th |
| Hanyang Mobile Cabin Hospital | Wuhan International Expo Center | Maternal and Child Health Hospital of Hubei Province | 2 NEMRT and 2 provincial medical teams and imaging teams | 930 | 1,028 | 598 | Feb.11th | Mar.8th |
| Qiaokou Mobile Cabin Hospital | Qiaokou Wuhan Sports Center | The Third People’s Hospital of Hubei Province | 1 NEMRT and Shanxi medical Team | 200 | 330 | 232 | Feb.11th | Mar.9th |
| Huangpi Mobile Cabin Hospital | Huangpi District Gymnasium | Huangpi District People’s Hospital | Hubei Medical Team | 200 | 222 | 156 | Feb.11th | Mar.7th |
| Jiangan Mobile Cabin Hospital | Tazi Lake Sports Center | Hubei Province Traditional Chinese Medicine Hospital | 2 NEMRT and 2 provincial medical teams and mobile P3 laboratories | 900 | 1,011 | 760 | Feb.12th | Mar.5th |
| Wuhan Jingkai Mobile Cabin Hospital | Wuhan Sports Center | Hannan Hospital | 2 NEMRT and 2 provincial medical teams and mobile P3 laboratories | 1,000 | 1,056 | 875 | Feb.12th | Mar.8th |
| Castle Peak Mobile Cabin Hospital | WISCO Sports Center | Wuhan Ninth Hospital | 1 NEMRT and 1 provincial medical team | 388 | 519 | 330 | Feb.13th | Mar.9th |
| Optics Valley Convention and Exhibition Center Mobile Cabin Hospital | Wuhan Optics Valley Technology Exhibition Center, 1st floor | Optics Valley, Tongji Hospital, Huazhong University of Science and Technology | 1 and 4, provincial medical teams1 and 4 provincial medical teams | 840 | 875 | 691 | Feb.17th | Mar.6th |
| Zhuankou Mobile Cabin Hospital | Logistics warehouse in south area of private industrial park of Wuhan Economic Development Zone | Wuhan Asia Heart Hospital and Wuhan Asia Heart General Hospital | 1 and 5 provincial medical teams | ,996 | 990 | 576 | Feb.15th | Mar.7th |
| Donghu Rihai Mobile Cabin Hospital | Former Rihai Industrial Park of Wuhan Midland Group | Hubei Provincial People’s Hospital | NEMRT andprovincial medical teams | 3690 | NA | NA | NA | NA |
| Jianghan Jingkai Mobile Cabin Hospital | Jianghan Economic Development Zone | Affiliated Hospital of Huazhong University of Science and Technology, Tongji Medical College | 1 NEMRT and 3 provincial medical teams | 682 | 281 | 207 | Feb.21th | Mar.8th |
| Hanyang Sports School Mobile Cabin Hospital | Wuhan Sports School | Maternal and Child Health Hospital of Hubei Province | 1 NEMRT and 5 provincial medical teams | 1,160 | 265 | NA | Feb.21th | Mar.8th |
Note: NEMRT: National Emergency Medical Rescue Team, which is from the entire country except Hubei Province. All of these data were based on the “Workbook of China’s Mobile Cabin Hospitals (Third Edition)” published by Bureau of Hospital Administration, Department of Medical Administration, National Health Commission of China, Medical Management Service Guidance Center of National Health Commission, China and data announced by Wuhan official press [18].
The structures and performance of Hanyang MCH
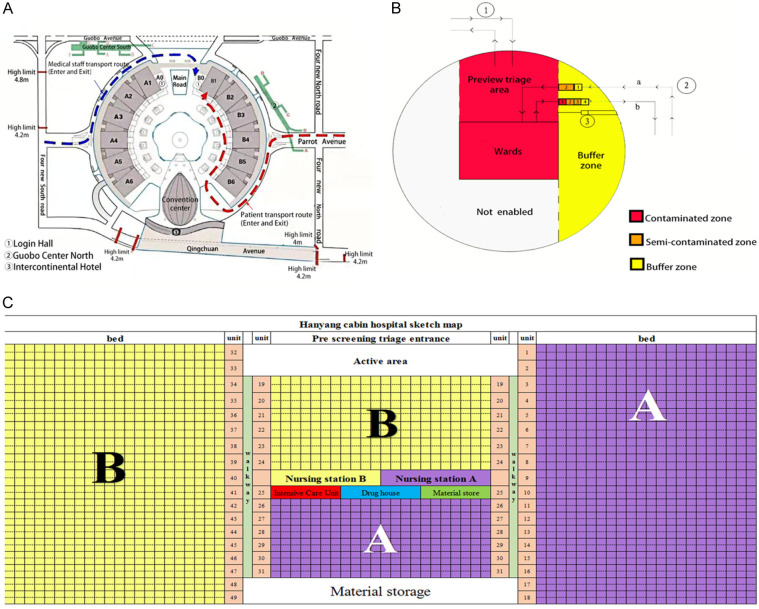
Location selection and ward layout description
Wuhan Hanyang Mobile Cabin Hospital was transformed from Hall B1 of Wuhan International Expo Center (Figure 2A). Hanyang MCH was located in Hall B1, while the headquarter was set in Hall A1, which was in the upstream of Hall B1 and considered as clean zone. There were some measures taken before it began to run in order to prevent the cross infection of medical staff and patients and ensure the smooth operation (Figure 2). Firstly, the path to enter or leave the MCH of medical staff (blue arc line with arrow) was designed to be separated from that for patients (red arc line with arrow) (Figure 2A). Secondly, three zones and two passageways were set up in MCH to facilitate the management of hospital infection control. (1) Two passage ways for doctors and for patients were separated. (2) The three zones were named as contaminated zone (red), buffer zone (yellow), and clean zone (outside the MCH, not shown). The contaminated zone contained preview triage area and the ward. In the buffer zone where doctors’ passageway was located, there was an entry channel (a) for donning PPE (1 changing room, 1 buffer rooms) and an exit channel (b) for doffing PPE. The exit channel had the first buffer room, the first doffing room, the second doffing room, and the second buffer room (Figure 2B). While the area outside the Hall B1, for example, Hall A1 was designated as the clean zone, and used as working area. Thirdly, in the middle of buffer area, a temporary CT reading area was set to facilitate the clinician to read patient’s chest imaging (Figure 2B). Lastly, in front of the MCH, in the patients’ pathway, there were two mobile CT scanners for patients’ imaging test with a waiting area in a tent. On the left, there was a simple clinical laboratory for blood testing that had been transformed from a convenience store.
Figure 2.
Location and structure of Wuhan Hanyang Mobile Cabin Hospital. Note: (A) Map displaying the structure of Wuhan International Expo Center and Location of Hanyang Mobile Cabin Hospital; (B) Graphic display of the design of Hanyang Mobile Cabin Hospital (Hall B1); (C) The internal structure of the ward. PPE: personal protective equipment.
Ward layout and requirements for medical staff
There were 48 units which consisted of 18-22 beds in each unit, making up a total of 930 beds in the ward. The general ward was divided into A and B parts, managed by Shandong medical team and Sichuan medical team, respectively. The Nurse Station was located in the central part, on the opposite side facing the Nurse Station, there were the intensive care unit (ICU), the Drug House, and the material storage room. There were reading room and activity area in the front of the ward, while at the back, it was equipped with the storage area (Figure 2C).
Space between beds was at least 1-1.5 m, Shandong and Sichuan Medical Team managed 465 beds, respectively [17]. Each team had about 300 medical staff including 100 physicians and 200 nurses who were divided into several groups. Therefore, the ratio of physicians to the nurses to patients was approximately 1:2:5. Every team had several groups for shifting works in MCH. The medical group leader (second-line physician) in each group managed the entire patients, and each front-line physician managed about 40 patients, hence at least 12 physicians were needed for each shift in each medical group. Additionally, special hospital infection teams were also established, scheduled for four shifts per day and four stations per shift, which included contaminated zones, semi-contaminated zones, buffer zones and cleaning stations.
The admission and operation of Hanyang Mobile Cabin Hospital
With a total of 930 beds in Hanyang MCH, 1,028 patients were treated, 598 patients were cured, and 430 patients were transferred to designated hospitals before the MCH was closed. As shown in Figure 3, large number of patients were admitted at an early time on Feb 11, due to the outbreak being at an early stage, the mobile cabin hospital filled up rapidly in just four days. 2,295 novel coronavirus nucleic acid tests were performed, among which, there were 1,032 tests of two consecutive negative results, 924 tests of one negative results, and 302 tests of positive (13.16%). In Figure 4A, the results indicated there were about 30-120 patients who met discharge criteria with two negative nucleic acid tests each day. The positive rate of nucleic acid detection of COVID-19 was determined to be about 10-17%.
Figure 3.
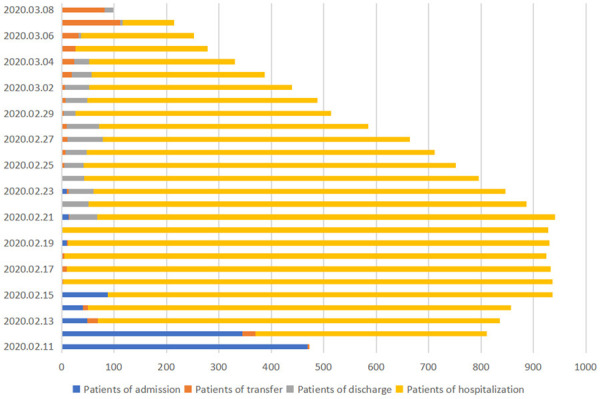
Trend of Patients undergoing hospitalization, admission, transfer and discharge in Hanyang Mobile Cabin Hospital.
Figure 4.
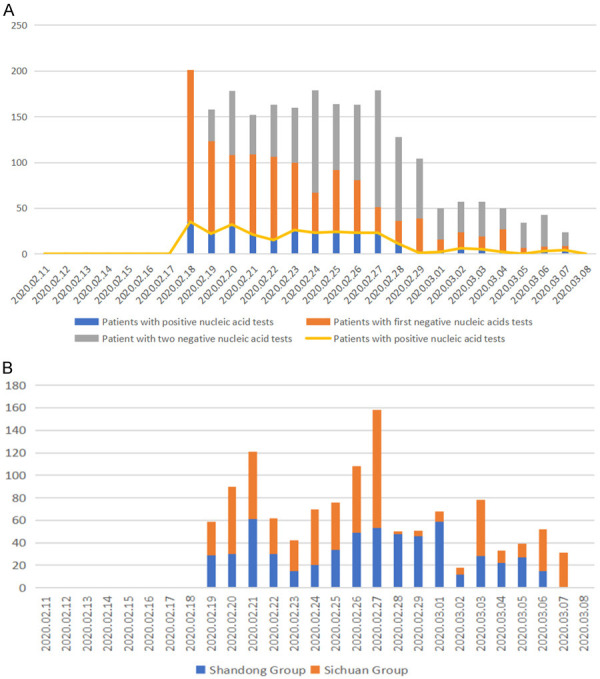
Graph showing the number of nucleic acid detections and CT scan of COVID-19 performed every day. Note: (A) Graph showing the number of nucleic acid detections; (B) Graph displaying the number of chest CT scans performed every day.
A total of 1,206 mobile CT scans were conducted for the patients. It indicated the demand for daily CT scan increased every week according to requirements of evaluation of clinical effects, there were on average about 60-120 CT scans performed, with the maximum number of CT scans being at about 160 times per day for the initial stage, while the data dropped to 20-80 due to the decrease of patients (Figure 4B). Over time, there were about 50 patients discharged every day around 10 days later. The newly diagnosed patients dropped dramatically, which demonstrated the epidemic was controlled after one incubation period of 14 days (Figure 1). No more patients were admitted to the Hanyang MCH from that time onwards.
Of all the patients, 836 patients were enrolled except 192 patients who were transferred to the designated hospital upon admission or with incomplete clinical data, and nucleic acid tests were carried out for all patients before admission. Of the 836 patients admitted to the hospital, there were 384 males (45.93%), and 452 females (54.07%), 7 patients aged less than 18 years old (0.84%), 738 patients aged between 18 and 65 years old (88.28%), and 91 patients aged ≥65 years old (10.89%). In the course of treatment in the hospital, 397 patients had negative nucleic acid results and the median time was 10.00 days (P25 8.00 days, P75 15.00 days). They were discharged with a median length of stay of 18.00 days (P25 12.00 days, P75 21.00 days, Table 2). Besides, 439 patients (52.51%) were transferred to designated hospitals for further treatment totally due to the severity of COVID-19 infections or other underlying diseases.
Table 2.
Population baseline data of the patients in Hanyang Mobile Cabin Hospital
| Population baseline data | Cases (N=836) | Constituent ratio (%) |
|---|---|---|
| Gender | ||
| Man | 384 | 45.93 |
| Female | 452 | 54.07 |
| Age (year, y) | ||
| <18 | 7 | 0.84 |
| 18-65 | 738 | 88.28 |
| ≥65 | 91 | 10.89 |
| Nucleic acid detection results | ||
| The first nucleic acid test after admission was negative | 715 | 85.53 |
| The first nucleic acid test was positive after admission | 121 | 14.47 |
| Nucleic acid was negative at the first admission and positive in the retest | 35 | 4.19 |
| The median (P25, P75) (The time from positive nucleic acid detection to negative two consecutive nucleic acid results. (n=397) (day, d) | 10.00 (8.00, 15.00) | |
| Outcome | ||
| Patients transferred to designated hospital due to basic disease or not reaching the discharge standard before the Hanyang MCB hospital being closed | 439 | 52.51 |
| Patients hospitalized and treated in Hanyang MCB hospital until they were discharged after reaching the discharge standard | 397 | 47.49 |
| The median (P25, P75) (Time from admission to discharge (n=397) (day, d) | 18.00 (12.00, 21.00) | |
Note: In addition to the 192 patients who were transferred to the designated hospital upon admission, a total of 836 patients were enrolled, and all patients tested positive for nucleic acid before admission among these patients, 397 were discharged after reaching the discharge standard, 439 were transferred to designated hospital due to basic disease or not reaching the discharge standard before the Hanyang MCB hospital being closed.
Organizational structure of mobile cabin hospitals
Like other mobile cabin hospital, Hanyang MCH had a complete organizational structure to ensure their operation. Hubei Women and Children Healthcare Centre was in charge of overall management, and different medical teams were responsible for supplementary examination, hospital infection control and medical administration, respectively. The local government served as district general commander. In addition, a local designated hospital was prepared to receive transferred patients.
A volunteer system consisting of caring people and activists from each medical unit was established to serve as unit leaders to assist in management.
Preventive measures for nosocomial infections in Hanyang Mobile Cabin Hospital
There were some measures to ensure no nosocomial infections in Hanyang MCH. First, The application of the “three zones and two passages” described above, in reconstruction of MCH help Seperate not only the medical staff and patients but also the polluted and clear area, minimizing the risk of nosocomial infections,although there was still a deficiency that airflow direction could not be guaranteed from clean zone to contaminated zone. Second, special nosocomial infection teams were formed to oversee medical staff and other non-medical staff (e.g. security and cleaning staff) in a 24 h manner. Third, no material was permitted to be taken out of the contaminated zone. The data were taken in form of pictures and transferred to headquarters outside the cabin hospital. Last but not the least, medical staff returned to their designated hotels after work instead of going home, ensuring that they would not spread the virus to their family members. Furthermore, medical staff were forbidden to take in any food and drinks without doffing PPE; once they went back to their residency after work, they conducted immediate personal hygiene, including bathing, eye, ear, mouth and washing the nose before eating; and timely disinfection of clothing were performed in order to block contamination and infection.
The patients’ livelihoods were safeguarded in MCH
MCH must safeguard the daily lives and guarantee the livelihoods of all patients, including security guarantee, hygiene, activities, entertainment, etc. Firstly, during the hospitalization and quarantine period, the patients’ livelihoods including clothing, three meals a day, bed linens, paper towels, and other daily necessities, as well as heating systems for the winter were fully managed by the government for free. Secondly, safety protection measures were implemented appropriately. In addition to taking precautions for fire safety, a plenty of security personnel were assigned. Furthermore, appropriate spaces for activities like reading rooms, entertainment areas and other facilities were set up to assist in the patients’ daily recreation, thus ensuring their emotional well-being. During the management of the patients, a volunteer system consisting of caring people and activists from each medical unit was established to serve as unit leaders to assist in management. This enhanced the patients’ daily life management efficiency and orderliness, while also greatly reducing the pressure on medical staff.
Treatment regime of patients in MCH
The combination of traditional Chinese and Western medicine was adopted as the main treatment. However, given the limited supply of drugs, the preferred medications were based on traditional Chinese medicine, the easily available arborol, and drugs with fewer side effects. Biochemical and other tests were not carried out in the mobile cabin hospitals, and hence the side effects of the drugs could not be fully monitored, which was one of the limitations of MCH. The special treatment approaches adopted in MCH included psychological treatment, such as providing comfort, alleviation, and social activities. These measures could all effectively reduce patients’ mental anxiety, enhancing the enthusiasm of doctors and patients in working harmoniously together to combat the disease as well.
Discussion
Throughout human history, infectious diseases posed a huge threat to mankind, killing millions of people. The 1,918 Pandemic, the Black Death, SARS, killed 50 million, 25 million and 744 people worldwide, respectively [18-20]. In the course of history, there had been precedents using temporary hospitals to fight against epidemics. For example, during the plague outbreak in Qin Dynasty, temporary buildings were employed to quarantine patients so as to cut off the source of infection, resulting in curbing the spread of diseases effectively. Moreover, a special infectious hospital (Xiaotangshan Hospital) was established in combating SARS in China in 2003. Nevertheless, there has no application of the cabin hospital in dealing with an emergency of infectious diseases. COVID-19 was shown to be more highly infectious than any other previous contagious disease [21,22]. In this case, there had been over ten thousand new cases in less than one month, causing an emergency because medical resources could not be increased accordingly. Home quarantine was adopted extensively at an early stage in China for mild patients [23,24] but unfortunately it turned out to be ineffective due to the consistent spread of the virus in households in Wuhan. In order to cut off the source of infection thoroughly, China initiated to employ cabin hospitals accompanied with a free treatment strategy to achieve the aim of accepting all infected patients, which was shown to be extremely effective, leading to a curbing of the epidemic in Wuhan in only two incubation period of 14 days. There were also other alternative measures such as the use of hotels to provide basic home care for patients with mild cases in Korea, which might have provided a more comfortable livelihood and privacy for patients. Otherwise, this kind of management could only have worked in a setting with limited spreading of the virus but would be difficult to cope with an epidemic which had caused large scale impact. Therefore, in the case of the widespread epidemic, the employment of cabin hospital maybe an alternative and effective measure to control the infectious diseases.
There were several benefits from the employment of MCH. With this kind of temporary hospital, all confirmed mild cases received compulsory quarantine, which decreased the number of newly diagnosed cases and facilitated centralized treatment by medical staff, which allowed the rapid recovery for patients. On the other hand, the severe cases developed from those patients in MCH were identified at an early stage and promptly treated in designated hospital effectively, causing a significant increasing recovery probability. What is more, sufficient beds in designated hospitals were available for critically ill patients, as that centralized treatment could be performed effectively, leading to a dramatic decrease in mortality rate, and a significant increase recovery rate from 14% to 89%, and thereby a gradual increase in the number of cured and discharged patients. In summary, after 2 incubation periods of using MCH to combat COVID-19, the epidemic was effectively curbed, the number of cumulative cases dropped from its peak of more than 80,000 to 14,000. So, all the MCH completed their tasks and were closed before Mar 10 [25].
In China, 34000 medical staff who aided in Hubei province successfully controlled the spreading of COVID-19 by adhering to the following points. Firstly, everyone was very cautious and attached great importance to it, so they pursued the personal protection as rigorous as possible. Secondly, China took a series of very strict measures to prevent the spread of the virus. Due to the risk of aerosol transmission of the new coronavirus disease [26], all possible transmission routes were cut off, including different entry and exit routes for medical staff and patients, three zones and two channels constructed for prevention of cross infection, 24 h supervision by special team for reducing the risk of self-contamination by PPE, strict three-level protection medical personnel, timely cleaning after work and so on. These measures may be regarded as excessive protection, but because of strict adherence, Chinese medical workers were protected well with no cross infection rather than the highly infected rate of about 16% in the United States [27]. Therefore, these preventive measures were worth of reference for severe infectious diseases.
Although MCH had played an important role in combatting COVID-19 in China, in our view, some management strategies should be optimized: (1) A mature and rapid response management system for infectious disease should be established. Although a powerful management team of MCH was organized by the emergency medical rescue team, there were many defects in the working systems initially, it consumed much time because many strategies were constantly honed due to immaturity. (2) The structure of the medical staff can be adjusted. Since most patients in MCH were mild patients who could take care of themselves, the core problems of MCH operation were quarantine, basic medical care, arrangement of life and daily management of the patients. The demand of medical staff was not necessarily high. For example, the number of senior professional clinicians could be reduced appropriately, and the number of junior doctors of healthcare staff could be increased to do general care observation, which can greatly reduce the demand for medical personnel (3). Leader patients chosen from each unit to help manage the life of the patients was a useful and effective method to improve management efficiency of MCH and might also reduce the cost and human resources. (4) Intelligent management links could be recommended if possible. Automatic simple COVID-19 electronic case history system can be filled in before admission, and the increased use of video instruments in the ward round may greatly reduce the exposure of medical staff as well as the use of PPE.
However, mobile cabin hospitals also have several notable limitations. For example, they had modest facilities, poor conditions for medical treatment, and a low level of nosocomial infection protection. So, severe cases or patients with worsened conditions or underlying diseases could not be well handled. Additionally, MCH could not provide comfortable living condition or secured privacy. Therefore, once the epidemic had eased, patient should be transferred to designated hospitals for further treatment as soon as possible [28].
Other than the limitations of the mobile cabin hospitals, there were also some limitations in this study. Firstly, this was a temporary experience in a special period, so descriptive research was conducted because it could not be compared with other methods. Secondly, clinical data such as complete case history, symptoms and signs could not be achieved well in emergency status. Finally, basic research including atmosphere virus concentration were not pursued to discover the effect of prevention of nosocomial infection of COVID-19. Some further research may be conducted to confirm the most essential factors of running MCH for the epidemics.
In summary, after nearly two incubation periods, the epidemic was effectively curbed in Wuhan and China in April 2020. As the COVID-19 epidemic spread throughout the world, it has killed more than millions of people in the world. Fighting against COVID-19 with an MCH was a useful initiative in China and proved to be effective in handling the epidemic [29]. These experiences may serve as a helpful reference for other countries with epidemic outbreaks.
Acknowledgements
This work was supported by the National Major Science and Technology Project for the Control and Prevention of Major Infectious Diseases in China (2017ZX10103004), Fujian Natural Science Foundation (2019J01178) and High-level Hospital Foster Grants from Fujian Provincial Hospital, Fujian Province, China (2019HSJJ11). Fujian Science and Technology Research Guide Project (2020Y0005). We would like to thank Editage (www.editage.cn) for English language editing.
Disclosure of conflict of interest
None.
References
- 1.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W China Novel Coronavirus I and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Lancet. Emerging understandings of 2019-nCoV. Lancet. 2020;395:311. doi: 10.1016/S0140-6736(20)30186-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riou J, Althaus CL. Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Euro Surveill. 2020;25:2000058. doi: 10.2807/1560-7917.ES.2020.25.4.2000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ryu S, Chun BC. An interim review of the epidemiological characteristics of 2019 novel coronavirus. Epidemiol Health. 2020;42:e2020006. doi: 10.4178/epih.e2020006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qiu YY, Wang SQ, Wang XL, Lu WX, Qiao D, Li JB, Gu YY, Zeng Y, Chen Y, Bai WZ, Xu BL, Han TW. Epidemiological analysis on a family cluster of COVID-19. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:494–497. doi: 10.3760/cma.j.cn112338-20200221-00147. [DOI] [PubMed] [Google Scholar]
- 11.Special Expert Group for Control of the Epidemic of Novel Coronavirus Pneumonia of the Chinese Preventive Medicine Association. An update on the epidemiological characteristics of novel coronavirus pneumonia (COVID-19) Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:139–144. doi: 10.3760/cma.j.issn.0254-6450.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Farzan AN. ‘Italy has abandoned us’: people are being trapped at home with their loved ones’ bodies amid coronavirus lockdown March 12, 2020. https://www.washingtonpost.com/nation/2020/03/12/coronavirus-bodies-italy-quarantine 2020.
- 13.COVID-19 Emergency Response Key Places Protection and Disinfection Technology Team, Chinese Center for Disease Control and Prevention. Technologies and requirements of protection and disinfection in key places during COVID-19 outbreak. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54:340–341. doi: 10.3760/cma.j.cn112150-20200217-00131. [DOI] [PubMed] [Google Scholar]
- 14.Wei PF. Diagnosis and treatment protocol for novel coronavirus pneumonia (Trial Version 7) Chin Med J (Engl) 2020;133:1087–1095. doi: 10.1097/CM9.0000000000000819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mahaney WE. In: Workbook of current English (3rd edition) Foresman , editor. Scott; 1985. [Google Scholar]
- 16.Smith DR. Herd immunity. Vet Clin North Am Food Anim Pract. 2019;35:593–604. doi: 10.1016/j.cvfa.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 17.Liu JF, Zhai XH, Xiang Z, Zhao J, Zhang JY, Wang J. Discussion on the cabin hospital construction management of COVID-19 epidemic situation. Chin Hosp Manag. 2020;40:12–14. [Google Scholar]
- 18.Wever PC, van Bergen L. Death from 1918 pandemic influenza during the First World War: a perspective from personal and anecdotal evidence. Influenza Other Respir Viruses. 2014;8:538–546. doi: 10.1111/irv.12267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rutherford AWJ. Black death. Trends Mol Med. 2001;7:12. doi: 10.1016/s1471-4914(00)01899-2. [DOI] [PubMed] [Google Scholar]
- 20.Paules CI, Marston HD, Fauci AS. Coronavirus infections-more than just the common cold. JAMA. 2020;323:707–708. doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- 21.Zhao S, Lin Q, Ran J, Musa SS, Yang G, Wang W, Lou Y, Gao D, Yang L, He D, Wang MH. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020;92:214–217. doi: 10.1016/j.ijid.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rahimi F, Talebi Bezmin Abadi A. Practical strategies against the novel coronavirus and COVID-19-the imminent global threat. Arch Med Res. 2020;51:280–281. doi: 10.1016/j.arcmed.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J Pediatr. 2020;87:281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.China’s State Council Information Office. The white paper titled “Fighting COVID-19: China in Action”. 2020 [Google Scholar]
- 26.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.CDC COVID-19 Response Team. Characteristics of Health Care Personnel with COVID-19 - United States, February 12-April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477–481. doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen Z, Zhuang XL, Li J, Yang XL, Feng Y. Medical management of hospitals designated for patients with COVID-19. Chin J Nosocomiol. 2020;30:821–825. [Google Scholar]
- 29.Chen S, Zhang Z, Yang J, Wang J, Zhai X, Bärnighausen T, Wang C. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395:1305–1314. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]