Abstract
Background: Polycystic ovary syndrome (PCOS) patients are prone to early pregnancy loss. Studies have found that the blood fibrinolytic activity of PCOS patients is closely related to the high abortion rate. At present, it is considered that the combination of traditional Chinese and Western medicine in the treatment of PCOS with threatened abortion has a good effect on fetal protection. Therefore, the clinical efficacy of the combination of traditional Chinese and Western medicine in the treatment of PCOS with threatened abortion was systematically evaluated, and the effect of traditional Chinese medicine on the blood fibrinolytic status of patients was also evaluated. Methods: The clinical randomized controlled trials (RCTs) of integrated traditional Chinese and Western medicine in the treatment of PCOS with threatened abortion were reviewed from four Chinese databases (CNKI, WANFANG, VIP, and SINOMED) and two English databases (PubMed, EMBASE) from their time of establishment to May 2021. According to the inclusive and exclusive criteria, tests were selected, data were extracted and evaluated, the systematic review was carried out by description analysis, and the meta-analysis was conducted using RevMan 5.3 software from Cochrane Collaboration. Begg’s and Egger’s tests were performed for assessing symmetries of funnel plot by the software Stata 16.0. Results: 6 RCTs involving 361 participants were included. Meta-analysis results showed that integrated traditional Chinese and Western medicine can increase the total efficacy compared with the control groups [RR=1.22, 95% CI (1.10, 1.35), P=0.0002]. Meanwhile, the improvement of TCM syndrome integral [MD=-2.11, 95% CI (-2.56, -1.66), P<0.00001], D-II [MD=-0.29, 95% CI (-0.49, -0.09), P=0.004], Hcy [MD=-3.02, 95% CI (-3.64, -2.39, P=0.00001], PAI-I [SMD=-2.38, 95% CI (-2.82, -1.73), P<0.00001] were better than a single Western medicine treatment. And it can increase the level of β-HCG [SMD=3.44, 95% CI (1.87, 5.01), P<0.0001], P [MD=7.70, 95% CI (7.10, 8.31), P<0.00001], E2 [MD=205.36, 95% CI (140.93, 269.80), P<0.00001]. The funnel plot, Egger’s test (P=0.210), and Begge’s test (P=0.573) suggested that there was no evidence of substantial publication bias. Conclusions: The effect of integrated traditional Chinese and Western medicine is better than that of Western medicine alone in the treatment of PCOS with threatened abortion, and it has certain advantages in improving the fibrinolytic status of patients. However, due to the limitation of the quality and quantity of the included literature, more rigorous and larger sample studies are needed to confirm these conclusions in the future.
Keywords: Polycystic ovarian syndrome, threatened abortion, coagulation and fibrinolysis system, integrated traditional Chinese and Western medicine meta-analysis
Introduction
Polycystic ovary syndrome (PCOS) is a reproductive endocrine disease with oligoanovulation or anovulation as the main clinical manifestation. PCOS infertility accounts for about 30% of all female infertility, and PCOS is the main cause of infertility with ovulation disorder [1]. However, even if infertile patients with PCOS get pregnant after induction of ovulation, early pregnancy loss is also very easy to occur in the process of pregnancy, and the incidence of post-pregnancy spontaneous abortion is as high as 40% [2]. A previous study showed that women with PCOS are three times more likely to miscarry [3].
Therefore, the prevention and treatment of early pregnancy loss in PCOS patients have become the focus and difficulty of obstetrics and gynecology experts. Studies have found that the blood fibrinolysis activity of PCOS patients is closely related to the high abortion rate, and women with PCOS are prone to form pre-thrombosis state (PTS) [4,5]. PTS refers to the continuous hypercoagulability of the blood system [6], which is an important factor in spontaneous abortion [7].
At present, Western medicine mainly treats PCOS patients with threatened abortion with progesterone, human chorionic gonadotropin (HCG), and other symptomatic treatments, but some patients still develop unavoidable abortions. In recent years, many clinical studies have reported that PCOS with threatened abortion combined with traditional Chinese medicine based on the conventional treatment of Western medicine has a good effect on fetal preservation, but most of them are small sample studies, which have certain limitations in guiding clinical practice.
Therefore, this study systematically evaluated the clinical control studies published in the past on the treatment of PCOS with threatened abortion by integrated traditional Chinese and western medicine and controlled Western medicine alone, and evaluated the effect of traditional Chinese medicine on the improvement of blood fibrinolysis status of patients, to provide a reference for the prevention and treatment of PCOS with threatened abortion.
Method
Inclusion and exclusion criteria in our study
Studies were included in the meta-analysis if they met the following conditions: (a) the randomized controlled study was conducted in the literature; (b) patients were diagnosed with PCOS with threatened abortion; (c) The control group was treated with Western medicine alone, while the experimental group was treated with Chinese medicine (including Chinese patent medicine, Chinese medicine decoction, etc.) based on the Western medicine regimen in the control group. Studies were excluded if: (a) review papers, case reports, or animal or cell culture studies; (b) the research content is repeated in the literature; (c) literature on outcome indicators related to the absence of PTS; (d) the Western medicine treatment plan of the experimental group and the control group was inconsistent; (e) the diagnostic criteria were not clearly stated in the trial.
Systematic search and strategy
A systematic literature search was conducted in four Chinese databases (CNKI, WANFANG, VIP, and SINOMED) and two English databases (PubMed, EMBASE) from their time of establishment to May 2021. We searched using different combinations of keywords, including “traditional Chinese medicine”, “combined traditional Chinese and Western medicine treatment”, “Polycystic Ovary Syndrome”, Threatened Abortion”, “Fetal Leakage”, “Fetal Irritability”, “Abdominal Pain in Pregnancy”. To avoid the omission of relevant research, references in the eligible literature after retrieval were also browsed and manually retrieved.
Outcomes
The main analysis included the treatment outcome indicators as measured by one or more of the following items: total effective rate of symptom treatment, TCM syndrome integral, related indicators of pre-thrombus state (such as D-II, Hcy, PAI-I, etc.). The secondary results included serum β-HCG level, serum P level, and serum E2 level.
Quality assessment
All the literature was independently evaluated by two reviewers, and the different opinions were resolved through discussion or soliciting the opinions of a third reviewer. In the process of literature screening, the title is first read, and the full text is further read to determine whether to include or not after the unrelated literature is excluded based on the title and abstract. Cochrane Collaboration tools for assessing the risk of bias in randomized trials [8] were also independently applied by two reviewers, with disagreements resolved by a third reviewer or consensus discussion.
Data analysis
All meta-analyses were conducted in the Review Manager (RevMan, Version 5.3, the Cochrane Collaboration, Copenhagen, Denmark). The homogeneity test showed no statistical significance (P>0.5, I2<50%), and the fixed-effect model was used for meta-analysis. If there is heterogeneity (P≤0.5, I2≥ 50%), the random-effects model is selected for analysis. Subgroup analysis or sensitivity analysis was performed according to the source of heterogeneity, and descriptive analysis was used for the data that could not be merged. Enumeration data were calculated using 95% confidence interval (CI) and relative risk (RR). For measurement data, weighted mean square deviation (WMD) and its 95% CI were used when the clinical trials used the same metric method, and standard mean difference (SMD) and 95% CI were used when different measurement methods or different units of measure were used.
Results
Flow chart of study selection
A total of 178 potential studies were found by searching online databases (CNKI n=58, WANFANG n=82, VIP n=82, SINOMED n=14, PubMed n=0, EMBASE=0). After excluding 66 duplicates, the remaining 111 papers were filtrated by reading their titles and abstracts. After further screening, a total of 57 papers entered the full-text acquisition and detailed screening. After excluding two repetitive studies based on the same case group and two for missing outcome indicators, another 46 were excluded for not mentioning the diagnostic criteria or the inclusion criteria. Finally, 6 articles met the inclusion criteria and eventually merged into the study, including six randomized controlled studies and one retrospective study (Figure 1).
Figure 1.
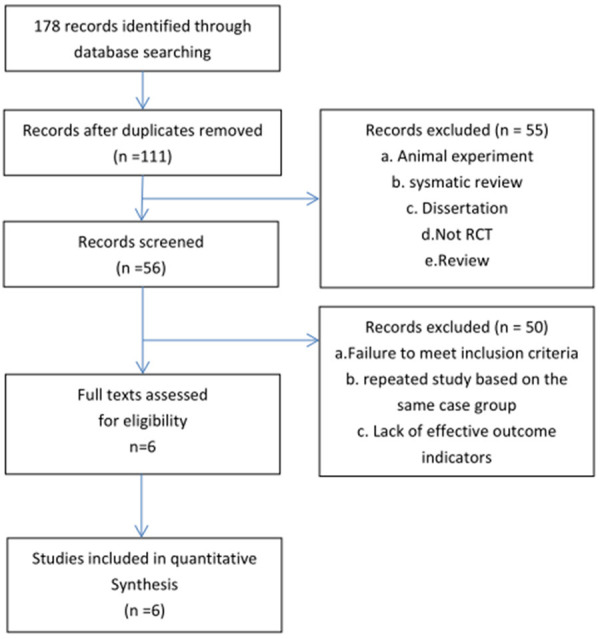
Flow diagram of selection and inclusion process.
Characteristics of included studies
The 6 studies [9-14] included 6 randomized controlled clinical trials, with a total of 361 patients, including 184 patients in the experimental group and 177 patients in the control group. The experimental group was treated with Luteal support combined with traditional Chinese medicine on this basis, while the control group was treated with Luteal support. The characteristics of the 6 studies are shown in Table 1.
Table 1.
Characteristics of included studies
| Study ID | Study design | n | Intervention | Outcome | Duration | |
|---|---|---|---|---|---|---|
|
|
|
|||||
| T/C | T | C | ||||
| Zeng 2014 | RCT | 20/20 | Chinese Medicine Decoction + Conventional treatment of western medicine | Progesterone Benzonate Injection 20 mg + HCG2000IU | ③④⑤⑥⑫⑭⑮ | 21 d |
| Liu 2014 | RCT | 20/20 | Chinese Medicine Decoction + Conventional treatment of western medicine | Progesterone Benzonate Injection 20 mg + HCG2000IU | ⑤⑥⑨⑩⑫ | 21 d |
| Lv et al. 2018 | RCT | 52/45 | Chinese Medicine Decoction + Conventional treatment of western medicine | Progesterone Benzonate Injection 20 mg | ④⑤⑥⑩⑫ | To 12 weeks of gestation |
| Zou 2019 | RCT | 30/30 | Chinese Medicine Decoction + Conventional treatment of western medicine | Dydrogesterone 10 mg + Progesterone Benzonate Injection 20 mg | ⑤⑥⑩⑫⑭ | To 12 weeks of gestation |
| Guo et al. 2020 | RCT | 32/32 | Chinese Medicine Decoction + Conventional treatment of western medicine | Progesterone Benzonate Injection 40 mg + VitE100 mg | ⑤⑥⑦⑨⑩ | 21 d |
| Chen et al. 2020 | RCT | 30/30 | Chinese Medicine Decoction + Conventional treatment of western medicine | Progesterone Benzonate Injection 20 mg + aspirin 75 mg | ⑤⑥⑦⑩⑬⑯⑰⑱⑲ | To 12 weeks of gestation |
① Activated partial thromboplastin time, APTT; ② Coagulation factor X; ③ Tissue plasminogen activator, t-PA; ④ Plasminogen activator inhibitor l, PAI-1; ⑤ Serum β-human chorionic gonadotropin (serum β-HCG); ⑥ Progesterone, P; ⑦ Estradiol,E2; ⑧ Pregnancy outcomes; ⑨ Homocys-teine, HCY; ⑩ Clinical effective rat; ⑪ Comparison of effective rate of fetal protection, abortion rate and other indicators related to follow-up pregnancy outcome; ⑫ TCM syndrome integral; ⑬ Human insulin-like growth factor binding protein-1, IGFBP-1; ⑭ D-II; ⑮ Plasma fibrin, Fib; ⑯ HbA1c, FINS, FPG, HOMA-IR; ⑰ Uterine artery blood flowI; ⑱ The ACA positive rate; ⑲ Symptoms of TCM scores.
Quality assessment
Six randomized controlled clinical trials were scored using the Cochrane Collaboration tools [8].
Three studies were grouped by random number table [9,11,14], while the remaining studies only mentioned randomness in words without reporting specific randomization methods. None of the six studies reported allocation concealment. Five studies did not blind the subjects or the experimenter [9,11-14], and one study did not report the blind method for the subjects or the experimenter [10]. None of the studies reported blinding outcome evaluators. One study reported 2 cases of loss in the control group, but the proportion of data loss was not enough to have a relevant clinical impact on the intervention effect [11], and the other studies reported complete data. Results were not selectively noted in all studies. None of the studies can judge whether there are other biases. There was no significant difference in age and days of menopause between the experimental group and the control group (P>0.05), indicating comparability (Figures 2, 3).
Figure 2.
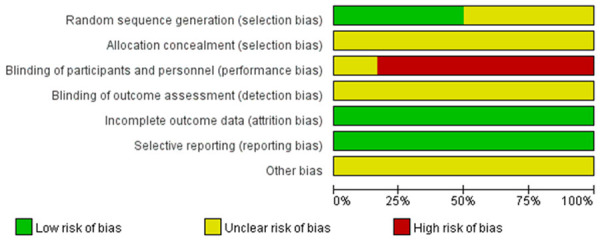
Risk of bias graph.
Figure 3.
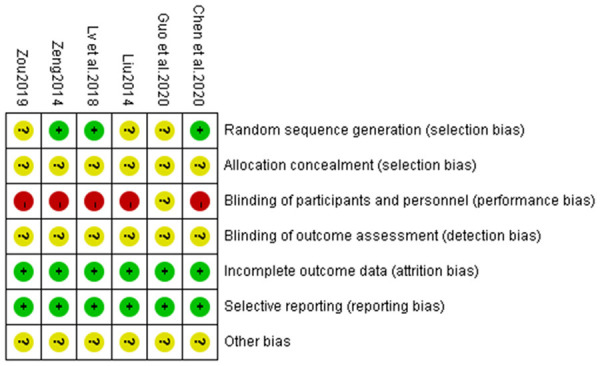
Risk of bias summary.
Meta-analysis results
Plasminogen activator inhibitor l, PAI-1
Three studies [11,14] reported PAI-1. After the heterogeneity test, I2=0, and P=0.53 for Q test were found, suggesting that the heterogeneity among the selected literature in this study was statistically significant, and random effects models could be selected for meta-analysis. The SMD value of the three studies was -2.38, with a 95% confidence interval [-2.82, -1.93], which was statistically significant (Z=10.50, P<0.00001), suggesting that integrated traditional Chinese and Western medicine treatment was superior to pure Western medicine treatment in reducing serum PAI-I level of PCOS patients with threatened abortion (Figure 4).
Figure 4.
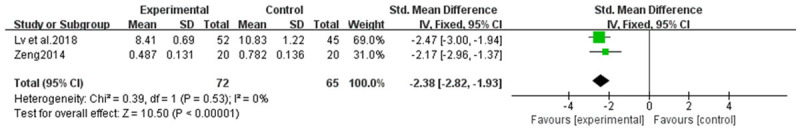
Forest plot of reducing serum PAI-I level.
D-dimer, D-II
Two studies [13,14] reported serum D-dimer levels. After the heterogeneity test, I2=98%, and P=0.000001 for Q test were found, suggesting that the heterogeneity among the selected literature in this study was statistically significant, the clinical homogeneity of the two studies is good, and the source of heterogeneity is unclear, so random-effects models could be selected for meta-analysis. The combined MD value of the two studies was -0.29, with a 95% confidence interval [-0.49, -0.09], which was statistically significant (Z=2.89, P=0.004), suggesting that integrated traditional Chinese and Western medicine was better than Western medicine alone in reducing serum D-dimer level of PCOS patients with threatened abortion (Figure 5).
Figure 5.
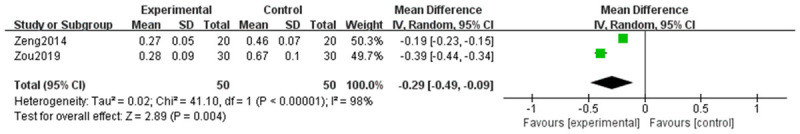
Forest plot of reducing serum D-II level.
Homocysteine, HCY
Two studies [10,12] reported serum Hcy level. After the heterogeneity test, I2=0, and P=0.87 for the Q test were found, suggesting that the heterogeneity among the selected literature in this study was not statistically significant, and the fixed effects model could be selected for meta-analysis. The combined MD value of the two studies was -3.02, with a 95% confidence interval [-3.64, -2.39], which was statistically significant (Z=9.47, P=0.00001), suggesting that integrated traditional Chinese and Western medicine treatment was superior to Western medicine treatment alone in reducing serum Hcy level of PCOS patients with threatened abortion (Figure 6).
Figure 6.
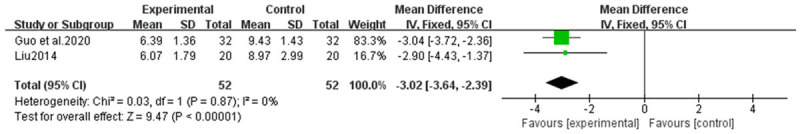
Forest plot of reducing serum Hcy level.
Serum β-human chorionic gonadotropin, serum β-HCG
Six studies [9-14] reported serum β-HCG level. After the heterogeneity test, I2=97%, and P=0.00001 for Q test were found, suggesting that the heterogeneity among the selected literature in this study was statistically significant, the clinical homogeneity of 6 studies was good, and the heterogeneity was still high after sensitivity analysis. At the same time, the source of heterogeneity was not found by subgroup analysis, so the random effects model could be selected for meta-analysis. The SMD value of the 6 studies was 3.33, with a 95% confidence interval [1.65, 5.01], which was statistically significant (Z=3.88, P<0.0001), suggesting that the treatment of integrated Chinese and Western medicine was superior to Western medicine alone in improving serum β-HCG level of PCOS patients with threatened abortion (Figure 7).
Figure 7.
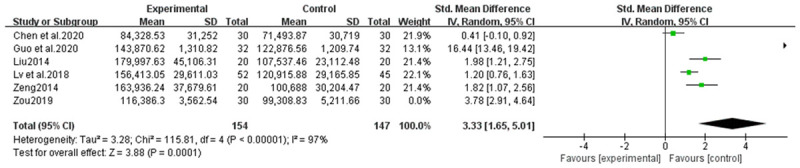
Forest plot of improving serum β-HCG level.
Progesterone, P
Six studies [9-14] reported serum P levels. After the heterogeneity test, I2=90%, and P<0.00001 for Q test were found, suggesting that the heterogeneity among the selected literature in this study was statistically significant, and a randomized effects model could be selected for meta-analysis. The SMD value of the 6 studies was 6.39, with a 95% confidence interval [4.02, 8.77], which was statistically significant (Z=5.27, P<0.00001). The source of heterogeneity was considered mainly because one study [11] reported negative results, and sensitivity analysis was conducted. After excluding this study and merged again, the heterogeneity disappeared significantly (MD 7.70, 95% CI [7.10, 8.31]; I2=0%, P<0.00001), suggesting that the treatment of integrated traditional Chinese and Western medicine was superior to Western medicine alone in improving serum P level of PCOS patients with threatened abortion (Figure 8).
Figure 8.
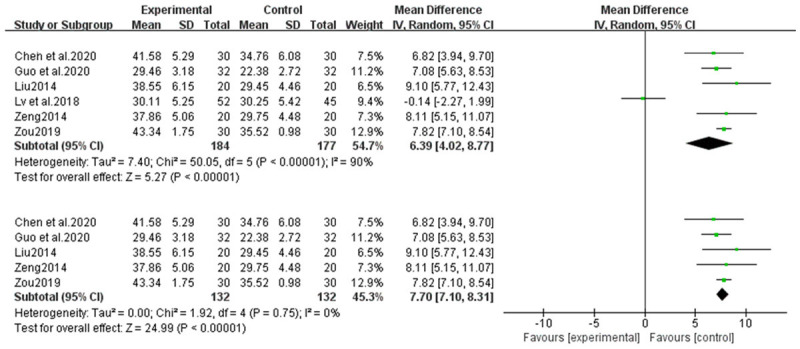
Forest plot of improving serum P level.
Estradiol, E2
Two studies [9,10] reported serum E2 levels. After heterogeneity test, I2=88%, and P =0.004 for Q test were found, suggesting that the heterogeneity among the selected literature in this study was statistically significant, the clinical homogeneity of the two studies is good, and the source of heterogeneity is unclear, so random-effects model could be selected for meta-analysis. The two studies summarized the MD value of 205.36, 95% confidence interval [-140.93, 269.80], which was statistically significant (Z=6.25, P=0.00001), suggesting that integrated traditional Chinese and Western medicine was better than Western medicine alone in improving serum E2 level of PCOS patients with threatened abortion (Figure 9).
Figure 9.
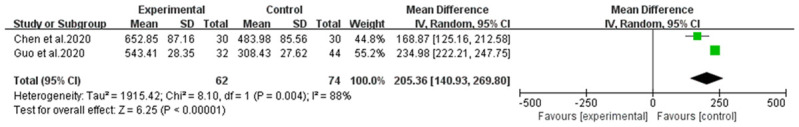
Forest plot of improving serum E2 level.
TCM syndrome integral
Four studies [11-14] reported TCM syndrome integral. After the heterogeneity test, I2=94%, and P<0.00001 for Q test were found, suggesting that the heterogeneity among the selected literature in this study was statistically significant, and random effects model could be selected for meta-analysis. The MD value of the four studies was -3.14, with a 95% confidence interval [-4.59, -1.69], which was statistically significant (Z=4.25, P<0.0001). The source of heterogeneity was considered mainly because one study [11] reported negative results, and sensitivity analysis was conducted. After excluding this study and merged again, the heterogeneity disappeared significantly (MD -2.11, 95% CI [-2.56, -1.66]; I2=35%<50%, P<0.00001), suggesting that the improvement of TCM symptoms under the treatment of integrated traditional Chinese and Western medicine was significantly better than that under the treatment of Western medicine alone (Figure 10).
Figure 10.
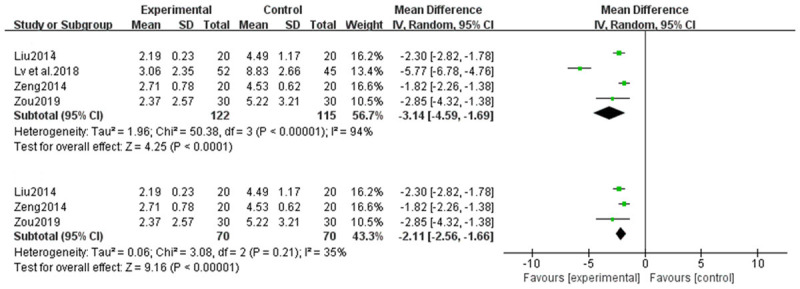
Forest plot of TCM syndrome integral.
Clinical effective rate
Six studies [9-14] reported clinical response rates. After the heterogeneity test, I2=0%, and P=0.51 for the Q test were found, suggesting that the heterogeneity among the selected literature in this study was not statistically significant, and the fixed effects model could be selected for meta-analysis. The summarized RR value of the five studies was 1.22, and the 95% confidence interval was [1.10, 1.35], which was statistically significant (Z=3.77, P=0.0002), suggesting that the treatment of PCOS with threatened abortion with integrated Chinese and Western medicine was superior to Western medical treatment alone (Figure 11).
Figure 11.
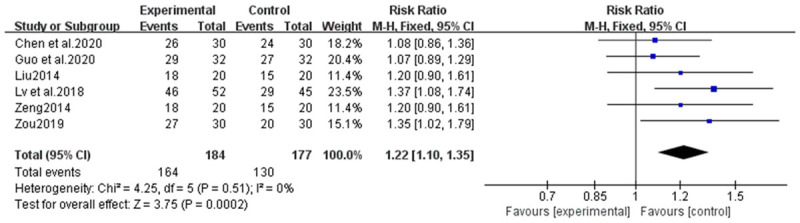
Forest plot of clinical response rates.
Publication bias
A funnel plot was made for the included studies to analyze the publication bias. The funnel plot of the clinical effective rate was symmetrical [9-14]. Meanwhile, the results of Egger’s test (P=0.210) and Begge’s test (P=0.573) showed that there was no significant publication bias (Figure 12).
Figure 12.
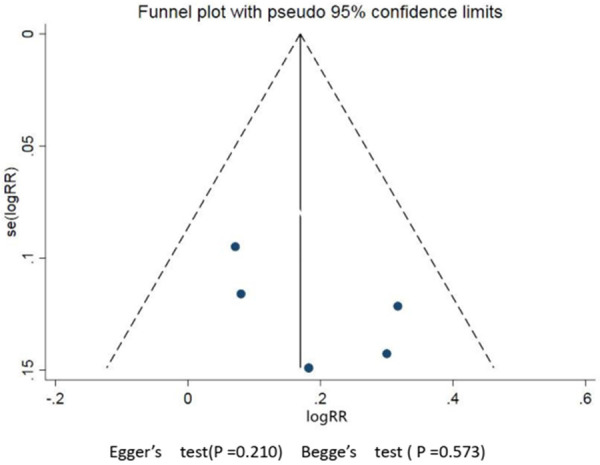
Clinical effective rate’s funnel plot.
Discussion
PCOS is a type of reproductive endocrine disease with unknown etiology and diverse clinical manifestations. It is characterized by clinical or biochemical manifestations of high androgen, persistent anovulation, and polycystic ovarian changes. PCOS is most common in women of reproductive age, with an incidence of 6.8-18% [15], and 50-70% of ovulatory dysfunction infertility is associated with this disease [16]. Recent studies have found that its incidence is increasing year by year and tends to be younger [17,18]. Even after pregnancy, early pregnancy loss may occur due to luteal defect during pregnancy, and the incidence of spontaneous abortion after pregnancy is as high as 40% [2].
Threatened abortion (TA) refers to the occurrence of a small amount of vaginal bleeding before 28 weeks of pregnancy followed by paroxysmal lower abdominal pain or low back pain. In a gynecological examination, the cervical opening was not opened, the fetal membrane was not broken, the pregnancy products were not discharged, the size of the uterus was consistent with the number of weeks of menopause, symptoms disappeared after rest and treatment, and the pregnancy could continue [7]. If this condition persists, it may lead to miscarriage.
The incidence of early spontaneous abortion in PCOS patients is as high as 40% [2]. Studies have shown that the abortion rate of women with PCOS is 3 times that of normal women [3]. At present, there is no definite qualitative treatment for polycystic ovary syndrome combined with threatened abortion in western medicine. Studies have shown that progesterone has significant morphological effects on estrogen-activated endometrium in vivo and is necessary to maintain pregnancy [19]. Therefore, progesterone can be used to treat threatened abortion and habitual abortion, etc. However, the high dose of progesterone will make the uterine mouth closed, affect the outcome of pregnancy, increase the rate of miscarriage of pregnant women, and the Chinese medicine in the treatment of this disease has a better effect and development prospects. Studies have shown that 70.7% of women with abortion in polycystic ovary syndrome (PCOS) are prone to thrombosis [20], and the incidence of placental infarction in pregnant women with pre-thrombosis is 72-89% [19]. This pre-thrombotic state does not necessarily lead to thrombotic disease, but it may lead to poor placental perfusion or even infarction due to the imbalance of coagulation-anticoagulation mechanism or fibrinolytic activity, micro thrombosis of a uterine spiral artery or villous vessel, and thus adverse pregnancy outcome.
The results of this meta-analysis showed that combined TCM treatment of PCOS with threatened abortion based on luteal support could further improve the total clinical response rate, symptom improvement score, HCG level, P level, and E2 level (all P<0.05), and reduce the levels of PAI-I, D-II, and Hcy (all P<0.05). There were no obvious adverse drug reactions in all the studies. Therefore, it can be concluded that TCM combined with luteal support in the treatment of PCOS with threatened abortion has good efficacy and safety, and can improve the pre-thrombosis state, which is worthy of clinical promotion and application.
There are some shortcomings in this study: (1) The included studies were all Chinese studies, lacking studies in other languages, and the overall quality was low, which reduced the credibility of the conclusions to some extent. (2) All the included literature in this study lacked evaluation of pregnancy outcome. Long-term follow-up of the tested patients should be carried out in future studies to observe pregnancy outcomes, including live birth rate, premature birth rate, and abortion rate. (3) In the literature included in this study, TCM prescriptions were different, and in one study [9], a combined treatment with aspirin was used for intervention. In addition, the dosage of progesterone and the method of medication (oral or intramuscular injection), the course of medication, and the follow-up time of endpoint and outcome indexes were inconsistent, so the evaluation of outcome indexes should be cautious. (4) The evaluation indicators of the included literature were diverse, varied, and poorly standardized. In addition to the included outcome indicators, there were also many evaluation indicators with great differences, which could not be analyzed and combined, leading to a significant decrease in the utilization of literature resources.
Therefore, in combination with the limitations of this study and the deficiencies in the methodological design of the included studies, to obtain the support of higher evidence-based medicine evidence, it is still necessary to include high-quality controlled clinical trials with large sample size, rigorous design, comprehensive evaluation and long-term follow-up results for verification.
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (Grant No. 82074542) and the Science and Technology Project of Fujian Province (Grant No.2019I0024) and the Natural Science Foundation of Fujian Province (Grant No. 2018J01866) and Joint Funds for the Innovation of Science and Technology, Fujian Province (Grant number: 2020Y9138).
Disclosure of conflict of interest
None.
References
- 1.Song Y, Li R. Interpretation of Chinese guidelines for diagnosis and treatment of polycystic ovary syndrome. Obstet Gynecol. 2018;34:737–741. [Google Scholar]
- 2.Mendoza N, Abad P, Baró F, Cancelo MJ, Llaneza P, Manubens M, Quereda F, Sánchez-Borrego R. Spanish menopause society position statement: use of tibolone in postmenopausal women. Menopause. 2013;20:754–60. doi: 10.1097/GME.0b013e31827b18c5. [DOI] [PubMed] [Google Scholar]
- 3.Katulski K, Czyzyk A, Podfigurna-Stopa A, Genazzani AR, Meczekalski B. Pregnancy complications in polycystic ovary syndrome patients. Gynecol Endocrinol. 2015;31:87–91. doi: 10.3109/09513590.2014.974535. [DOI] [PubMed] [Google Scholar]
- 4.Mannerås-Holm L, Baghaei F, Holm G, Janson PO, Ohlsson C, Lönn M, Stener-Victorin E. Coagulation and fibrinolytic disturbances in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2011;96:1068–76. doi: 10.1210/jc.2010-2279. [DOI] [PubMed] [Google Scholar]
- 5.Ravn P. New paradigms in PCOS: impaired glucose tolerance and cardiovascular risk. Clinical approach. Minerva Ginecol. 2015;67:217–23. [PubMed] [Google Scholar]
- 6.Shen Y, Qian FB, Yin TT. Value of detection of related genes of prethrombotic state in predicting adverse pregnancy. Journal of Clinical Medicine in Practice. 2020;24:58–60. [Google Scholar]
- 7.Xie X. Obstetrics and Gynecology 9th version. People’s Medical Publishing House; [Google Scholar]
- 8.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, Ltd.; [Google Scholar]
- 9.Chen W, Yu TH, Ji Y. Effect of Yishen Huoxue Antai recipe on uterine artery blood flow, glucose metabolism,serum β-human chorionic gonadotropin and anticardiolipin antibody in PCOS insulin-resistance patients with threa-tened abortion of kidney deficiency and blood stasispattern. Hebei J TCM. 2020;42:1501–1507. [Google Scholar]
- 10.Guo WX. Treatment of 32 cases of polycystic ovary syndrome with threatened abortion in early pregnancy by Bushen Antai Decoction. Zhejiang Journal of Traditional Chinese Medicine. 2020;55:584. [Google Scholar]
- 11.Lv BL, Wang H, Wang C, Zhao M. Clinical research on tocolysis efficacy of therapy of nourishing kidney, activating blood and resolving phlegm on polycystic ovarian syndrome with threatened abortion. Shanghai Journal of Traditional Chinese Medicine. 2018;52:53–58. [Google Scholar]
- 12.Liu DQ. Kidney blood activing Hcy threatened abortion patients with polycystic ovary syndrome in clinical research Hcy. Guangxi University of Chinese Medicine. 2014 [Google Scholar]
- 13.Zou HQ. The clinical study on the treatment of PCOS Abortion with kidney-tonifying and phlegm-moistening prescription. Jiangxi University of Chinese Medicine. 2019 [Google Scholar]
- 14.Zeng QR. Kidney blood activing polycystic ovary syndrome threatened abortion patients blood fibrinolytic clinical research. Guangxi University of Chinese Medicine. 2014 [Google Scholar]
- 15.Liu BW, Bao ST, Yang YQ, Ni Y, Pang XL, Chen J, Yang J. Comparison of pregnancy outco-mes of three controlled ovarian stimulation protocols for patients with polycyst-ic ovary syndrome. Journal of Reproductive Medicine. 2019;28:1396–1401. [Google Scholar]
- 16.Ning JL, Peng X. Clinical effects of different ovulation induction schemes in infertile women with poly cystic ovary syndrome. Maternal and Child Health Care of China. 2019;34:5252–5254. [Google Scholar]
- 17.Qu C, Hou LH. Research progress of Chinese and Western medicine in the treatment of adolescent polycystic ovary syndrome. Asia-Pacific Traditional Medicine. 2015;11:50–51. [Google Scholar]
- 18.Han X, Wang BL, Luo L, Zhao J, Wang YY. Incidence of metabolic syndrome in patie-nts with polycystic ovary syndrome. Shaanxi Medical Journal. 2015;44:170–172. [Google Scholar]
- 19.Costantino M, Guaraldi C, Costantino D. Resolution of subchorionic hematoma and symptoms of threatened miscarriage using vaginal alpha lipoic acid or progesterone: clinical evidences. Riv Eur Sci Med Farmacol. 2016;20:1656–1663. [PubMed] [Google Scholar]
- 20.Moini A, Tadayon S, Tehranian A, Yeganeh LM, Akhoond MR, Yazdi RS. Association of thrombophilia and polycystic ovarian syndrome in women with history of recurrent pregnancy loss. Gynecol Endocrinol. 2012;28:590–3. doi: 10.3109/09513590.2011.650754. [DOI] [PubMed] [Google Scholar]


