Abstract
Objective: To investigate the nursing effect of cold therapy combined with enhanced recovery after surgery (ERAS) in patients undergoing total knee arthroplasty (TKA). Methods: Eighty patients with knee osteoarthritis who underwent TKA in our hospital from August 2020 to January 2021 were enrolled in this study, and they were divided into a control group (n=40) and a study group (n=40) according to the nursing procedures. The time and cost of rehabilitation, pain level, recovery of knee function, incidence of postoperative complications, self-care ability, quality of life, and nursing satisfaction were compared between the two groups. Results: The time of rehabilitation and time to out-of-bed activities in the study group were significantly shorter than those in the control group (P < 0.05), and the cost of rehabilitation in the study group was significantly lower than that in the control group (P < 0.05). There was no significant difference in preoperative visual analogue scale (VAS) scores (at rest, during exercise) between the two groups (P > 0.05). These scores in the study group were significantly lower than those in the control group at 6 h, 24 h, 48 h, and 72 h postoperatively (P < 0.05). The preoperative Hospital for Special Surgery (HSS), range of motion (ROM) and Barthel scores did not differ significantly between the two groups (P > 0.05). The postoperative ROM and Barthel scores were decreased to the lowest at 3 d postoperatively and gradually increased with time, and the HSS, ROM and Barthel scores in the study group were significantly higher than those in the control group (P < 0.05). The incidence of postoperative complications in the study group was significantly lower than those in the control group, and overall nursing satisfaction in the study group was significantly higher than those in the control group (P < 0.05). After discharge, the SF-36 scores of patients in both groups were higher than those before surgery, and the SF-36 scores in the study group were significantly higher than those in the control group (P < 0.05). Conclusion: The cold therapy combined with ERAS for patients undergoing TKA can improve the postoperative swelling and pain of the affected limb, inspire patients’ autonomy in postoperative rehabilitation training, shorten the time to out-of-bed activity, prevent patients from developing venous thrombosis, promote recovery of knee function, and improve patients’ postoperative self-care ability and quality of life.
Keywords: Cold therapy, enhanced recovery after surgery, total knee arthroplasty
Introduction
With the overall aging of China’s population, the prevalence of osteoporosis such as rheumatoid and osteoarthritis (OA) is increasing annyally, which seriously reduces the quality of life of middle-aged and elderly people. OA is a chronic, multiple synovitis, which is a degenerative joint disease caused by physical or pathological reasons, of which knee osteoarthritis (KOA) has the highest incidence [1]. According to the World Health Organization (WHO), the prevalence of KOA progressively increases with age, with an incidence of 50% in people over 60 years old and 80% in people over 75 years old [2]. According to a longitudinal survey, the number of KOA patients in China reached 250 million in 2010, showing an alarming increase in incidence [3]. Most KOA patients suffer from painful symptoms and knee deformities, which severely limit their mobility and affect their normal life.
Total knee arthroplasty (TKA) is a procedure to replace the deformed joint with an artificial knee prosthesis made of biocompatible and mechanically sound materials to correct the deformity, relieve pain, and reconstruct knee function [4]. Since Repicci et al. first completed knee replacement through invasive surgery, TKA has become the most effective option for the treatment of end-stage or severe KOA [5]. With the continuous development of medical technology, the survival rates of TKA patients have been reported at 90% over the past 15 years [6]. Kurtz et al. has predicted that the worldwide demand for TKA will increase by 673% by 2030, to about 3.4 million cases per year [7].
Although TKA can improve knee function and relieve pain in patients, it is an invasive procedure, and the majority of patients undergoing TKA are the elderly. Therefore, the prevention of postoperative complications in patients is gaining increasing attention from medical staff. The concept of enhanced recovery after surgery (ERAS) was first proposed by Danish surgeon Henrik Kehlet in 2001, and was applied to patients after coronary artery bypass grafting with good clinical results [8]. In recent years, medical staff have applied the concept of ERAS to patients who underwent TKA, indicating that ERAS can improve clinical outcomes, shorten the time to first out-of-bed activity and time to discharge, and reduce hospitalization expenses [9].
Cold therapy is the application of cryogenic substances on human skin to reduce local or systemic temperature, and then slow down nerve signal transmission, and decrease the activities of various biological enzymes to achieve the purpose of pain relief and detumescence [10]. At present, cold therapy has been widely used in all kinds of surgery. After TKA, patients are prone to knee swelling and pain, even leading to the loss of knee function in severe cases. Postoperative cold therapy can reduce pain sensation and enhance the effectiveness of early rehabilitation training [11].
The purpose of this study was to investigate the effect of cold therapy combined with ERAS and traditional nursing on postoperative pain, early joint function recovery, and postoperative complication in patients undergoing TKA, aiming to provide a theoretical basis for the rapid rehabilitation of patients undergoing TKA.
Materials and methods
General data
The clinical data of 80 patients diagnosed with KOA who had undergone TKA after ineffective conservative treatment from August 2020 to January 2021 were retrospectively analyzed in this study, and the patients were divided into a control group (n=40) and a study group (n=40) according to the different nursing methods they received.
Inclusion criteria: (1) patients aged 50-75 years old; (2) patients with first TKA; (3) patients with morning stiffness ≤ 30 min; (4) patients with no vital organ diseases such as heart and lung diseases; (5) patients with clear consciousness and no cognitive impairment.
Exclusion criteria: (1) patients with presence of infection in the knee joint; (2) patients with severe dysfunction caused by retroflexion deformity of the knee joint; (3) patients with functional failure of major organs; (4) patients who were lost to follow-up.
The study was reviewed and approved by the ethics committee of Huzhou Central Hospital. All patients signed an informed consent form and voluntarily participated in this study.
Intervention methods
Patients in control group received routine care. No special heat preservation method was adopted during the surgery. At 6 h after surgery, patients could eat digestible food according to their own wishes without any discomfort. The drainage tube was removed 2 d after surgery, and the methods of functional exercise and the benefits of out-of-bed exercise were introduced to the patients, but the intensity of exercise was not prescribed. The patients were assisted to get out of bed when they intended to do so.
Patients in the study group received cold therapy combined with ERAS as follows.
(1) Establishment of an ERAS care team: The team consisted of the joint surgeon, nursing staff, dietician, rehabilitator and psychological counselor, and all personnel were trained in nursing methods, scales, criteria and procedures used for assessment.
(2) Pre-operative intervention: After admission, the doctor assessed the patient’s vital signs, knee function and pain level, and introduced the ERAS nursing procedures, preoperative precautions, perioperative multimodal analgesia and rehabilitation training plan to the patients and their family through demonstration and video, etc. The psychological counselor gave emotional guidance based on patient’s mental status to eliminate fear and reduce the psychological burden of patients. Patients were assessed for pain level, and oral anti-inflammatory and analgesic drugs were given for preventive analgesia according to the patient’s condition. Preoperatively, 200 mL of 10% glucose solution was administrated orally followed by abstinence from water and fasting for 8 h before surgery. The rehabilitation training was performed according to the patient’s maximum tolerance before surgery, and alprazolam (Qilu Pharmaceutical Co., Ltd., Approval No. H37021277) 0.4 mg was taken orally the night before surgery. For patients with sleep disorders, the dosage should be prescribed with caution.
(3) Intraoperative intervention: Color ultrasound-guided femoral nerve block, GA was achieved through a laryngeal mask airway (LMA). The operation room temperature was adjusted to 23-26°C before the patient entered, and all fluids except blood used intraoperatively were heated to 35-37°C using a water bath. The patient’s intraoperative body temperature was monitored, and a thermal mattress was used for temperature control.
(4) Postoperative intervention: The vital signs of patients were assessed every 0.5 h within 4 h postoperatively. When the patients returned to consciousness with stable vital signs, they could drink 50-80 mL of water, and if there was no discomfort after 30 min, they could take liquid food. Multimodal analgesia was performed, including an epidural analgesic pump, 400 mg of oral celecoxib (Pfizer Pharmaceuticals Ltd., Approval No. J20030098) once a day, and cold therapy with ice packs around knee joints. The temperature around the knee was monitored every 30 min to maintain the temperature at 10-15°C. The cold therapy was interrupted if the patient had unusual sensations such as numbness and coldness. Patients were encouraged and instructed to perform postoperative functional exercises. On the day after operation, ankle pump exercises, quadriceps muscle contraction, passive knee flexion and extension exercises, etc. were performed. The exercise program was enriched progressively after surgery. After discharge, regular lectures on rehabilitation knowledge and interactive communication were organized. WeChat was used to publicize health knowledge and follow up the patients’ rehabilitation.
Outcome measurements
Early postoperative recovery indices
The rehabilitation time and cost and the time to out-of-bed activities after surgery were recorded in both groups.
The period from 1 day before surgery to the day of discharge was recorded as rehabilitation time, and the cost invoiced during this period was the cost of rehabilitation.
On an unassisted basis, time to first out-of-bed activities was recorded as patients standing with both feet on the ground for more than 3 min, during which the patients’ first ambulation time with the aid of some tools was recorded.
Visual analogue scale (VAS) scoring at multiple times
VAS scale was used to evaluate the pain level at rest and during exercise before surgery, at 6 h, 24 h, 48 h and 72 h after surgery. VAS scoring was done by drawing a 10 cm line on the paper, with the left end representing no pain and the right side representing severe pain, and patients marked their pain on the line according to their subjective feelings.
Knee Hospital for Special Surgery (HSS) score and joint mobility range of motion (ROM)
Knee HSS score was assessed before and upon discharge, 1 month and 3 months after surgery, and the ROM was measured before and at 3 d after surgery, at discharge, 1 month and 3 months after surgery.
The HSS scale was first proposed by the New York Hospital for Special Surgery in 1976 to assess the recovery of knee function after TKA. The scale includes pain evaluation, functional status, limb ROM, degree of limb flexion deformity, joint stability, and muscle strength. A score of < 59 indicates poor, 60-69 indicates fair, 70-84 indicates good, and 85-100 indicates excellent [12]. The higher score represented better recovery of knee function.
ROM is one of the crucial indices to assess knee function after TKA. ROM is determined by a goniometer, and the average value of three measurements is ROM value [13].
Postoperative complications
The circumference of the affected limb was compared with the preoperative circumference by measuring the circumference of the thickest part of the lower leg in the horizontal position, and a difference greater than 2 cm was considered to be swelling of the affected limb [14]. Venous thrombosis of the affected limb was determined by color Doppler ultrasonography. Infection was determined by bacterial culture results of wound drainage fluid.
Self-care ability and quality of life
The Barthel index was used to assess the patients’ self-care ability in daily life, including eating, bathing, dressing before surgery, 3 d after surgery, at discharge, 1 month and 3 months after surgery. The patients were scored based on whether they needed assistance in daily life, with 10 points for no need, 5 points for partial need, and 0 point for complete need, and the higher score indicated the better self-care abilities [15].
The SF-36 scale was used to assess the quality of life of patients before surgery, 1 month and 3 months after surgery, respectively. The SF-36 scale contains 8 domains, including physical functioning (PF), physical role functioning (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH). The higher score indicates the better quality of life [16].
Nursing satisfaction
The satisfaction questionnaire prepared by the hospital itself was used to assess the satisfaction of patients with nursing care during hospitalization. The questionnaire contains five dimensions, including admission reception (20 points), health education (35 points), service attitude (50 points), service quality (35 points), and discharge guidance (10 points), with the total score of 150 points. The total score was the sum of the scores of each item, and the higher score represents the higher satisfaction with nursing care during hospitalization.
Statistical methods
SPSS 21.0 software was used for data analysis. The measurement data were expressed as x̅ ± s, and the counting data were expressed as frequencies or percentages. The independent samples t-test was used for measurement data, while χ2 test was used for counting data. Repeated measure ANOVA was used for data at multiple time points between two groups, SNK test was used for pairwise comparison. Graphpad Prism 8.0 software was used for graphing. P < 0.05 was considered as a significant difference.
Results
Comparison of baseline data
No significant difference was found between the two groups in terms of gender, age, disease duration, location, and grading (P > 0.05), which were comparable (Table 1).
Table 1.
Comparison of baseline data (x̅ ± s)/[n (%)]
| Control group (n=40) | Study group (n=40) | t/χ2 | P | |
|---|---|---|---|---|
| Gender | 0.205 | 0.651 | ||
| Male | 18 (45.0) | 16 (40.0) | ||
| Female | 22 (55.0) | 24 (60.0) | ||
| Mean age (years) | 65.32±5.42 | 64.79±5.36 | 0.152 | 0.725 |
| Duration of disease (years) | 21.02±2.34 | 20.98±2.26 | 0.090 | 0.132 |
| Location | 0.503 | 0.478 | ||
| Left knee | 28 (70.0) | 25 (62.5) | ||
| Right knee | 12 (30.0) | 15 (27.5) | ||
| Grading | 0.222 | 0.895 | ||
| Grade II | 5 (12.5) | 6 (15.0) | ||
| Grade III | 10 (25.0) | 11 (27.5) | ||
| Grade IV | 25 (62.5) | 23 (57.5) |
Comparative analysis of early recovery indices
The time of rehabilitation and the time to first out-of-bed activities in the study group were significantly shorter than those in the control group (P < 0.05), and the cost of rehabilitation in the study group was significantly lower than that in the control group (P < 0.05) (Figure 1).
Figure 1.
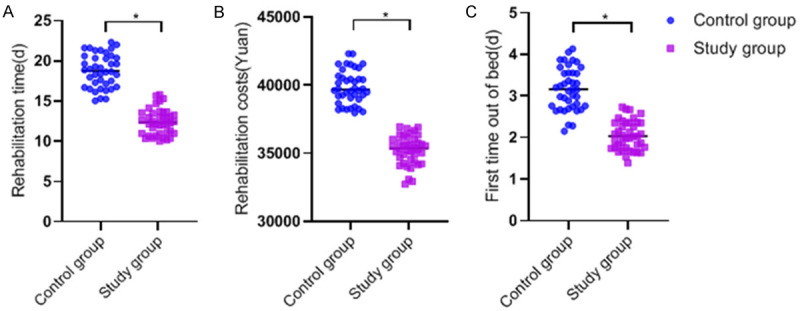
Comparison of early rehabilitation indices. The time of rehabilitation and the time to out-of-bed activities for the first time were significantly shorter in the study group than in the control group, and the cost of rehabilitation was significantly lower in the study group than in the control group (*P < 0.05).
Comparative analysis of VAS scores at multiple time points
The preoperative VAS scores at resting and during exercise were not significantly different between the two groups (P > 0.05). Repeated measure ANOVA showed that main effects of time and group were statistically significant (P < 0.05), the interaction effect was not statistically significant (P > 0.05); pairwise comparison showed that the VAS scores of the study group at 6 h, 24 h, 48 h, and 72 h after surgery were significantly lower than those of the control group (P < 0.05) (Figure 2).
Figure 2.
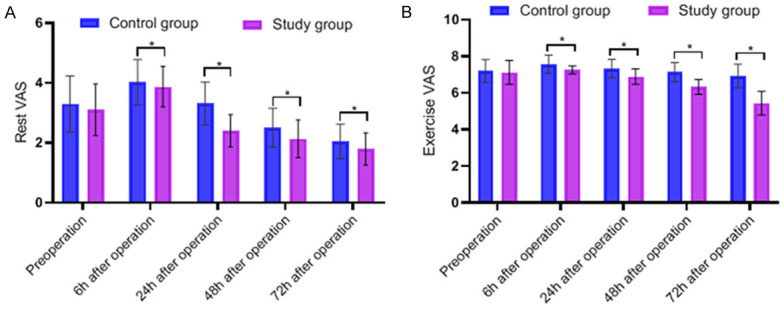
Comparison of VAS scores. The differences in resting and exercise VAS scores between the two groups were not significant (P > 0.05). Repeated measure ANOVA: F value of time (Ft )=36.286 (P < 0.001), F value of group (Fg )=18.326 (P < 0.001), F value of interaction effect (Fi )=1.607 (P=0.184); pairwise comparison: the VAS scores of the study group at 6 h, 24 h, 48 h, and 72 h after surgery were significantly lower than those of the control group (P < 0.05).
Comparative analysis of HSS scores and ROM scores of the knee joint
There was no significant difference in preoperative HSS and ROM scores between the two groups (P > 0.05). The HSS scores of patients in both groups increased at discharge, and gradually increased with time. Repeated measure ANOVA showed that main effects of time and group were statistically significant (P < 0.05), the interaction effect was statistically significant (P < 0.05), the HSS score of study group increased more significantly; pairwise comparison showed that the HSS scores of study group at discharge, 1st month after surgery, 3rd month after surgery were significantly lower than those of the control group (P < 0.05) (Figure 3A). The ROM scores decreased to the lowest in both groups at 3rd day after surgery, increased at discharge, and gradually increased over time, and the ROM scores of study group were significantly higher than those of control group at all-time points after surgery (P < 0.05) (Figure 3B).
Figure 3.
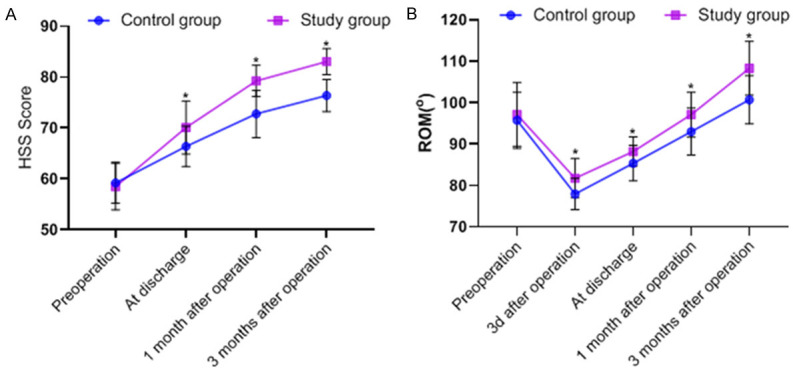
Comparison of HSS scores and ROM scores. A. The difference between the preoperative HSS scores of patients in the two groups was not significant; the HSS scores of patients in the two groups increased at discharge, and the HSS scores gradually increased with time; the HSS scores of the study group were significantly higher than those of the control group. Repeated measure ANOVA: Ft =42.139 (P < 0.001), Fg =15.133 (P < 0.001), Fi =9.823 (P < 0.001); pairwise comparison: the HSS scores of study group at discharge, 1st month after surgery, 3rd month after surgery were significantly lower than those of the control group (P < 0.05). B. The difference in preoperative ROM scores between the two groups was not significant; the ROM scores decreased to the lowest in 3rd d after surgery, increased at discharge, and gradually increased over time. Repeated measure ANOVA: Ft =48.320 (P < 0.001), Fg =12.539 (P < 0.001), Fi =1.513 (P=0.216); pairwise comparison: the ROM scores of the study group were significantly higher after surgery than those of the control group (P < 0.05).
Comparative analysis of postoperative complications
In the study group, the incidence of swelling in the affected limbs was 10%, venous thrombosis was 5%, infection was 2.5%, and the overall postoperative complication rate was 17.5%, while in the control group, the incidence of swelling in the affected limbs was 25%, venous thrombosis was 17.5%, infection was 12.5%, and the overall postoperative complication rate was 55%. The incidence of postoperative complications in the control group was significantly higher than that in the study group (P < 0.05) (Table 2).
Table 2.
Comparison of postoperative complications [n (%)]
| Item | Control group (n=40) | Study group (n=40) | χ2 | P |
|---|---|---|---|---|
| Swelling | 10 (25.0) | 4 (10.0) | 3.117 | 0.077 |
| Venous thrombosis | 7 (17.5) | 2 (5.0) | 2.003 | 0.157 |
| Infection | 5 (12.5) | 1 (2.5) | 1.622 | 0.203 |
| Complications | 17 (55.0) | 7 (17.5) | 12.170 | <0.001 |
Comparative analysis of self-care ability and quality of life of patients
There was no significant difference in Barthel scores and SF-36 scores between the two groups before surgery (P > 0.05). Barthel scores decreased to the lowest level at 3rd day after surgery, and gradually increased with time. Repeated measure ANOVA of Barthel scores and SF-36 scores showed that the main effects of time and group were statistically significant (P < 0.05), the interaction effects were statistically significant (P > 0.05); pairwise comparison showed that Barthel scores of patients of the study group were significantly higher than those of the control group at all-time points after surgery (P < 0.05) (Figure 4A), and SF-36 scores were significantly higher at 1st and 3rd month after surgery (P < 0.05) (Figure 4B).
Figure 4.
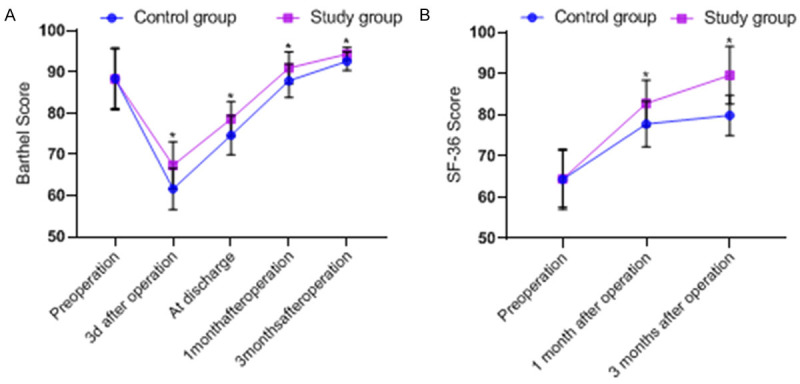
Comparison of self-care ability and quality of life scores. A. The difference between the preoperative Barthel scores of patients in the two groups was not significant; the Barthel scores would be the lowest in the 3rd d after surgery; the Barthel scores gradually increased over time. Repeated measure ANOVA: Ft =50.281 (P < 0.001), Fg =16.425 (P < 0.001), Fi =1.128 (P=0.317); pairwise comparison: the Barthel scores of the study group were significantly higher than those of the control group at all-time points after the intervention (P < 0.05). B. The difference between the preoperative SF-36 scores of the two groups was not significant; after discharge, the SF-36 scores of patients in both groups increased compared with the preoperative scores. Repeated measure ANOVA: Ft =25.874 (P < 0.001), Fg =8.136 (P < 0.001), Fi =0.834 (P=0.389); pairwise comparison: the SF-36 scores of patients in the study group were significantly higher than those of patients in the control group at 1st and 3rd month after surgery (P < 0.05).
Comparative analysis of nursing satisfaction
The overall nursing satisfaction scores of patients in the study group was significantly higher than that in the control group (P < 0.05), and the satisfaction of patients in the study group was significantly higher than that in the control group in terms of admission reception, health education, and discharge instruction (P < 0.05). There was no significant difference between the two groups in terms of service attitude and service quality (P > 0.05) (Table 3).
Table 3.
Comparison of patient satisfaction
| Item | Control group (n=40) | Study group (n=40) | t | P |
|---|---|---|---|---|
| Overall satisfaction | 133.45±6.60 | 138.09±4.15 | -7.68 | 0.000 |
| Admission reception | 14.58±0.73 | 14.83±0.52 | -2.19 | 0.032 |
| Health education | 30.72±3.05 | 33.98±2.09 | -6.17 | 0.000 |
| Service attitude | 44.29±0.67 | 44.67±0.37 | -1.48 | 0.153 |
| Service quality | 34.28±1.28 | 34.68±0.92 | -0.32 | 0.729 |
| Discharge guidance | 9.58±0.87 | 9.93±0.25 | -4.83 | 0.000 |
Discussion
ERAS covers anesthesia modality, multimodal analgesia, rehydration management, nutritional interventions, and early rehabilitation exercises to reduce the postoperative traumatic stress response of patients, stabilize the internal environment, reduce postoperative complications, and enable patients to recover rapidly after surgery [17]. Soffin et al. showed that an ERAS program, including preoperative education, intraoperative anesthetic techniques, postoperative analgesia, and early postoperative activities after arthroplasty could accelerate postoperative rehabilitation of TKA patients [18]. Sixty percent of patients have severe postoperative pain after TKA, which, if not treated in a timely manner, can stimulate sensitization of the nociceptive center, reduce the pain threshold, increase the postoperative pain stress response, and the patient may refuse rehabilitation exercises, and eventually increase the risk of postoperative complications such as venous thrombosis and muscle atrophy, which is detrimental to the postoperative recovery of patients [19,20]. Kumar et al. showed that ERAS can accelerate functional recovery, reduce pain, improve patient comfort and satisfaction, reduce surgical complications, shorten hospital stay, and reduce hospitalization costs of patients undergoing TKA [21].
In this study, it was found that the rest and exercise VAS scores at 6 h after operation were increased in both groups compared to preoperatively, probably due to traumatic pain caused by surgery. The rest and exercise VAS scores in the study group were significantly lower than those in the control group at 6 h, 24 h, 48 h, and 72 h postoperatively (P < 0.05). The reason may be that the patients in the control group did not receive effective pain intervention, while the patients in the study group received preoperative prophylactic analgesia combined with multimodal paroxysmal pain nursing modality to improve pain threshold of patients, reduce local temperature through cold therapy, which could induce microvascular constriction, reduce bleeding and injury as well as postoperative pain, thereby exerting a positive effect for patients with rehabilitation training after surgery. Li et al. conducted a study of multimodal analgesia in patients undergoing TKA and found that multimodal analgesia could alleviate postoperative pain, promote knee recovery, and reduce the occurrence of adverse reactions, which is basically the same with the findings of this study [22]. Preoperative education and exercise for patients undergoing TKA can improve the initiative and compliance of patients in postoperative exercise [23]. Postoperative physiotherapy and standardized rehabilitation can accelerate the recovery of knee function and shorten the length of hospital stay [24]. In this study, the time of rehabilitation and the time to first out-of-bed activities in the study group were significantly shorter than those in the control group (P < 0.05), the cost of rehabilitation in the study group was significantly lower than those in the control group (P < 0.05), and the HSS and ROM scores in the study group were significantly higher than those in the control group (P < 0.05). The reason may be that with a rehabilitation exercise plan formulated before surgery and preoperative health education through video, audio, on-site guidance, etc., the patients recognized the importance of postoperative rehabilitation exercises, which significantly shortened the time to first out-of-bed activities. Early rehabilitation training can accelerate recovery of knee function. Regular rehabilitation education lectures were conducted after discharge, and relevant knowledge was released through WeChat to consolidate the rehabilitation outcomes. Oktas et al. found that patients recovered knee function faster through early intensive rehabilitation exercises in TKA patients [25], which is consistent with the findings in this study. The incidence of postoperative complications in the control group was significantly higher than those in the study group. Since the local skin and blood vessels of patients are damaged following TKA, the implantation of the prosthesis can induce tissue fluid exudation and local inflammatory responses; cold therapy can actually reduce vasoconstriction and permeability, blood pressure and fluid accumulation on the affected limb and improve the swelling of the affected limb, which is consistent with the findings of Sadoghi et al. [26]. Millar et al. found that the ERAS reduced the incidence of venous thrombosis after TKA by introducing a multimodal, interdisciplinary intervention after total hip, total knee and hip fracture surgery [27]. In this study, the incidence of venous thrombosis was 5% in the study group and 17.5% in the control group, indicating that early postoperative rehabilitation exercises could promote tissue fluid infiltration and diffusion, prevent tendon and joint capsule adhesions, and reduce the incidence of venous thrombosis in the lower limbs, which is similar to findings of Millar et al. The nursing staff in both groups had good working attitudes and operational capacity, and the difference between the two groups was not significant in terms of service attitude and service quality. Nursing staff in the study group introduced the hospital environment to patients and their families upon admission, carried out preoperative psychological education, nutritional support, and preventive analgesia to eliminate patients’ fears, and provided postoperative rehabilitation guidance to improve the rehabilitation of patients, enabling patients to trust and cooperate more with nursing staff, bringing patients a better nursing experience and improving overall nursing satisfaction.
In conclusion, cold therapy combined with ERAS for patients undergoing TKA can shorten the hospitalization time and reduce hospitalization costs. Through preoperative health education and demonstration, patients can realize the importance of postoperative rehabilitation training, which shortens the time to first out-of-bed activities after surgery, improve patients’ initiative to participate in rehabilitation training and plays a good role in promoting the recovery of knee function. The combined therapy can improve the pain threshold of patients and reduce the incidence of postoperative complications, and further improve the self-care ability and quality of life of patients. The deficiency of this study is that the time and temperature of continuous or intermittent cold therapy were not analyzed systematically. Therefore, a more systematic analysis should be conducted in the next step, so as to provide a more detailed reference for postoperative rehabilitation of TKA patients.
Acknowledgements
This research received no specific grants from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure of conflict of interest
None.
References
- 1.Hawker GA. Osteoarthritis is a serious disease. Clin Exp Rheumatol. 2019;37(Suppl 120):3–6. [PubMed] [Google Scholar]
- 2.Lespasio MJ, Piuzzi NS, Husni ME, Muschler GF, Guarino A, Mont MA. Knee osteoarthritis: a primer. Perm J. 2017;21:16–183. doi: 10.7812/TPP/16-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tang X, Wang S, Zhan S, Niu J, Tao K, Zhang Y, Lin J. The Prevalence of symptomatic knee osteoarthritis in China: results from the China health and retirement longitudinal study. Arthritis Rheumatol. 2016;68:648–653. doi: 10.1002/art.39465. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto K, Takagi M, Ito H. Emerging insights on surgical techniques and biomaterials for total hip and knee arthroplasty. Biomed Res Int. 2016;2016:1496529. doi: 10.1155/2016/1496529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Repicci JA, Eberle RW. Minimally invasive surgical technique for unicondylar knee arthroplasty. J South Orthop Assoc. 1999;8:20–27. discussion 27. [PubMed] [Google Scholar]
- 6.Lachiewicz PF, Soileau ES. Fifteen-year survival and osteolysis associated with a modular posterior stabilized knee replacement. A concise follow-up of a previous report. J Bone Joint Surg Am. 2009;91:1419–1423. doi: 10.2106/JBJS.H.01351. [DOI] [PubMed] [Google Scholar]
- 7.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 8.Carlson GL, Kehlet H. Improving surgical outcome - time for a change. Colorectal Dis. 2010;12:731–732. doi: 10.1111/j.1463-1318.2010.02286.x. [DOI] [PubMed] [Google Scholar]
- 9.Masaracchio M, Hanney WJ, Liu X, Kolber M, Kirker K. Timing of rehabilitation on length of stay and cost in patients with hip or knee joint arthroplasty: a systematic review with meta-analysis. PLoS One. 2017;12:e0178295. doi: 10.1371/journal.pone.0178295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freiman A, Bouganim N. History of cryotherapy. Dermatol Online J. 2005;11:9. [PubMed] [Google Scholar]
- 11.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–765. [PubMed] [Google Scholar]
- 12.Wang S, Zhang Y, Li J. Clinical application of unicompartmental knee arthroplasty and total knee arthroplasty in patient with bilateral knee osteoarthritis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34:1568–1573. doi: 10.7507/1002-1892.202005065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benner RW, Shelbourne KD, Bauman SN, Norris A, Gray T. Knee osteoarthritis: alternative range of motion treatment. Orthop Clin North Am. 2019;50:425–432. doi: 10.1016/j.ocl.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Loyd BJ, Stackhouse S, Dayton M, Hogan C, Bade M, Stevens-Lapsley J. The relationship between lower extremity swelling, quadriceps strength, and functional performance following total knee arthroplasty. Knee. 2019;26:382–391. doi: 10.1016/j.knee.2019.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castorina S, Guglielmino C, Castrogiovanni P, Szychlinska MA, Ioppolo F, Massimino P, Leonardi P, Maci C, Iannuzzi M, Di Giunta A, Musumeci G. Clinical evidence of traditional vs fast track recovery methodologies after total arthroplasty for osteoarthritic knee treatment. A retrospective observational study. Muscles Ligaments Tendons J. 2017;7:504–513. doi: 10.11138/mltj/2017.7.3.504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Santić V, Legović D, Sestan B, Jurdana H, Marinović M. Measuring improvement following total hip and knee arthroplasty using the SF-36 health survey. Coll Antropol. 2012;36:207–212. [PubMed] [Google Scholar]
- 17.Frassanito L, Vergari A, Nestorini R, Cerulli G, Placella G, Pace V, Rossi M. Enhanced recovery after surgery (ERAS) in hip and knee replacement surgery: description of a multidisciplinary program to improve management of the patients undergoing major orthopedic surgery. Musculoskelet Surg. 2020;104:87–92. doi: 10.1007/s12306-019-00603-4. [DOI] [PubMed] [Google Scholar]
- 18.Soffin EM, YaDeau JT. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth. 2016;117:iii62–iii72. doi: 10.1093/bja/aew362. [DOI] [PubMed] [Google Scholar]
- 19.Wiesmann T, Piechowiak K, Duderstadt S, Haupt D, Schmitt J, Eschbach D, Feldmann C, Wulf H, Zoremba M, Steinfeldt T. Continuous adductor canal block versus continuous femoral nerve block after total knee arthroplasty for mobilisation capability and pain treatment: a randomised and blinded clinical trial. Arch Orthop Trauma Surg. 2016;136:397–406. doi: 10.1007/s00402-015-2403-7. [DOI] [PubMed] [Google Scholar]
- 20.Kandarian BS, Elkassabany NM, Tamboli M, Mariano ER. Updates on multimodal analgesia and regional anesthesia for total knee arthroplasty patients. Best Pract Res Clin Anaesthesiol. 2019;33:111–123. doi: 10.1016/j.bpa.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Kumar L, Kumar AH, Grant SA, Gadsden J. Updates in enhanced recovery pathways for total knee arthroplasty. Anesthesiol Clin. 2018;36:375–386. doi: 10.1016/j.anclin.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 22.Li JW, Ma YS, Xiao LK. Postoperative pain management in total knee arthroplasty. Orthop Surg. 2019;11:755–761. doi: 10.1111/os.12535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moyer R, Ikert K, Long K, Marsh J. The value of preoperative exercise and education for patients undergoing total hip and knee arthroplasty: a systematic review and meta-analysis. JBJS Rev. 2017;5:e2. doi: 10.2106/JBJS.RVW.17.00015. [DOI] [PubMed] [Google Scholar]
- 24.Henderson KG, Wallis JA, Snowdon DA. Active physiotherapy interventions following total knee arthroplasty in the hospital and inpatient rehabilitation settings: a systematic review and meta-analysis. Physiotherapy. 2018;104:25–35. doi: 10.1016/j.physio.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 25.Oktas B, Vergili O. The effect of intensive exercise program and kinesiotaping following total knee arthroplasty on functional recovery of patients. J Orthop Surg Res. 2018;13:233. doi: 10.1186/s13018-018-0924-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sadoghi P, Hasenhütl S, Gruber G, Leitner L, Leithner A, Rumpold-Seitlinger G, Kastner N, Poolman RW, Glehr M. Impact of a new cryotherapy device on early rehabilitation after primary total knee arthroplasty (TKA): a prospective randomised controlled trial. Int Orthop. 2018;42:1265–1273. doi: 10.1007/s00264-018-3766-5. [DOI] [PubMed] [Google Scholar]
- 27.Millar JS, Lawes CM, Farrington B, Andrew P, Misur P, Merriman E, Walker M. Incidence of venous thromboembolism after total hip, total knee and hip fracture surgery at Waitemata District Health Board following a peer-reviewed audit. N Z Med J. 2020;133:52–60. [PubMed] [Google Scholar]


