Abstract
Objectives
To examine whether use of expressed human milk in the first two weeks postpartum is associated with cessation of human milk feeding and non-exclusive human milk feeding up to 6 months.
Design
Pooled data from two prospective cohort studies
Setting
Three Canada Prenatal Nutrition Program (CPNP) sites serving vulnerable families in Toronto, Canada.
Participants
337 registered CPNP clients enrolled prenatally from 2017 to 2020; 315 (93%) were retained to 6 months postpartum. Exclusions: pregnancy loss or participation in prior related study; Study B: preterm birth (<34 weeks); plan to move outside Toronto; not intending to feed human milk; hospitalisation of mother or baby at 2 weeks postpartum.
Primary and secondary outcome measures
Main exposure variable: any use of expressed human milk at 2 weeks postpartum. Outcomes: cessation of human milk feeding by 6 months; non-exclusive human milk feeding to 4 months and 6 months postpartum.
Results
All participants initiated human milk feeding and 80% continued for 6 months. Exclusive human milk feeding was practiced postdischarge to 4 months by 28% and to 6 months by 16%. At 2 weeks postpartum, 34% reported use of expressed human milk. Any use of expressed human milk at 2 weeks was associated with cessation of human milk feeding before 6 months postpartum (aOR 2.66; 95% CI 1.41 to 5.05) and with non-exclusive human milk feeding to 4 months (aOR 2.19; 95% CI 1.16 to 4.14) and 6 months (aOR 3.65; 95% CI 1.50 to 8.84).
Trial registration numbers
Keywords: public health, community child health, nutrition & dietetics
Strengths and limitations of this study.
This is one of the first studies to examine expressed human milk use by vulnerable women.
Infant feeding data were collected prospectively at four time points from 2 weeks to 6 months postpartum, limiting the recall period to improve data accuracy.
Analysis of associations between expressed human milk use and later human milk feeding practices focused on the first 2 weeks postpartum when lactation is being established.
Data collection did not include intentions to pump or feed expressed human milk, reasons for use of expressed human milk or maternal employment status.
Background
The WHO recommendation that all infants receive exclusive human milk (HM) feeding for the first 6 months of life in order to optimise health and development outcomes is an important global public health goal.1 The WHO definition does not differentiate between feeding HM directly at the breast and HM expressed either by hand or use of a breast pump and fed to the infant via a cup, bottle or other device.2 Over the past two decades, breast pump use has become widespread in high-income countries and the provision of expressed HM is now a major component of HM feeding for many families with term-born infants.3–5 Several studies have found high rates of obtaining pumps by the early postpartum period including use of expressed HM during the hospital stay.4 6 7 However, there is growing evidence that expressed HM is not equivalent to HM obtained through direct feeding at the breast. Observational studies with large sample sizes have found that provision of expressed HM but no formula is associated with higher risks of otitis media, wheezing and rapid weight gain within the first year of life in comparison to exclusive feeding at the breast.8–10 These findings have prompted the call for more nuanced assessment of HM feeding practices to include data on pumping and use of expressed HM.11 12
In addition to concerns about health effects, use of expressed HM feeding has been associated with shorter duration of any and exclusive HM feeding, although findings are mixed.13 It is likely that this inconsistency relates to variations between studies in factors such as infant age at the start of pumping or expressed HM feeding, and reasons for providing and degree of reliance on expressed HM. Recent analyses of longitudinal prospective cohort studies have found that pumping and/or expressed HM feeding earlier in the postpartum period, for non-elective reasons (ie, to manage difficulties feeding at the breast or return to work) and with higher frequency is associated with early cessation of any and exclusive HM feeding.7 14–16 However, the samples in these studies tend to be biased towards women of higher-socioeconomic status and therefore may not reflect expressed HM feeding practices of more vulnerable women.
In this paper, we report expressed HM feeding practices and associated HM feeding outcomes over the first 6 months postpartum among women recruited through the Canada Prenatal Nutrition Program (CPNP; a national programme designed to serve socially and/or economically vulnerable women) at three sites in Toronto. Our objectives were to examine: (i) the prevalence of expressed HM use at 2 weeks and 2, 4 and 6 months postpartum and (ii) associations between use of expressed HM at 2 weeks and HM feeding outcomes (cessation before 6 months and non-exclusive HM feeding to 4 and 6 months postpartum).
Methods
Study setting and participants
This analysis used infant feeding data collected prospectively from birth mothers in two studies conducted within a research programme designed to examine the potential for delivering postnatal lactation support through the CPNP. The CPNP is a federally funded initiative implemented through community agencies with the aims of improving birth outcomes and HM feeding among vulnerable women, such as those with low income or education, newcomers, adolescents, single parents and those with a history of trauma or substance use.17 CPNP activities vary between sites based on local needs and available partnerships, but are usually implemented as weekly drop-in programmes. Core services include group health and nutrition education, provision of food and/or grocery vouchers, individual supports such as nutrition counselling and referrals to other community services.17
Participants in both studies were registered in the CPNP at one of three specific sites in Toronto, Canada, and were recruited prenatally. The population of the combined catchment areas of the three CPNP sites is over 180 000. Detailed methods for both studies have been published previously. Study A was a prospective cohort study of infant feeding practices among clients of a CPNP site offering skilled postnatal lactation support with additional charitable funding from The Sprott Foundation.18 Study B was a pre/post intervention study designed to examine the effectiveness of implementing similar lactation support services in two other CPNP sites.19 The target sample size for Study B was 210, based on an anticipated 20 percentage point difference in exclusive HM feeding at 4 months postpartum between the pre-intervention and post-intervention groups, with 80% power, alpha=0.05, and allowance for 10% attrition.19
Inclusion criteria were prenatal registration in one of the CPNP sites, and for Study B, intention to feed HM and to continue living in Toronto with the infant. Exclusion criteria were pregnancy loss and, for Study A, participation in a prior related study. Exclusion criteria for Study B were preterm birth (<34 weeks gestation), medical issue affecting feeding and hospitalisation of either the mother or infant at 2 weeks postpartum. Recruitment was conducted from August 2017 to January 2020 for Study A and from November 2018 to March 2020 for Study B. Due to the COVID-19 pandemic, Study B was suspended in March 2020 following a brief intervention period and incomplete recruitment of the post-intervention group, but data collection was completed with all enrolled participants. Data from Study B participants recruited to both the pre-intervention and post-intervention groups were pooled with Study A data for the current analysis.
All participants in Study A and those recruited to the post-intervention group in Study B had access to two free, in-home visits from an International Board Certified Lactation Consultant (IBCLC) for postpartum lactation support, with additional visits approved for complex needs. This service was promoted prenatally and offered proactively by telephone call around the time of birth. Double-electric breast pumps were provided by the IBCLCs as needed, but criteria for pump provision were more flexible for Study A participants as the lactation support was provided as a community programme rather than a research intervention.
Patient and public involvement statement
Participants in this study were not clinical patients but clients of community perinatal services. At the time of the study, no engagement committee existed for these service-users to inform the research. The community programmes had participant feedback mechanisms in place regarding service delivery. Community programme staff were directly involved in the design, implementation, interpretation of findings and reporting of this research, including contributing service-user perspectives.
Data collection
All data collection for Study A was conducted by JF and for Study B by AM or a Mandarin speaking research assistant. Data collection occurred either in person at the participating CPNP sites or by telephone. Professional interpreter services were used for Study A participants who did not speak English (n=14) and Study B participants who did not speak either English or Mandarin (n=20).
In Studies A and B, infant feeding data were collected prospectively at 2 weeks and 2, 4 and 6 months postpartum using the same standardised and validated interviewer-administered questionnaire used previously by our group.20 21 In Study B, data were also collected at postpartum months 1, 3 and 5, but only the time points shared with Study A are reported here. At each time point, participants reported the average number of milk feeds provided to their infant per 24 hours, divided into feeds at the breast, expressed HM feeds and formula feeds. Expressed HM or formula use as a top-up after feeding at the breast was recorded as well as provision of other liquids and introduction of solids. The recall period was 2 weeks. Infant sex and in-hospital formula supplementation (yes/no) were recorded at the first postpartum contact. Participants who stopped all HM feeding were asked to recall the last date they provided any HM to their infant and main reasons for cessation.
Participants were categorised as yes or no for any HM feeding, exclusive HM feeding and any expressed HM feeding at each postpartum time point. Exclusive HM feeding was defined as provision of HM only, either at the breast or expressed, with the exception of vitamins, medicines and infrequent (less than daily) water feeds. In accordance with WHO and Health Canada guidance to introduce solids ‘around’ 6 months postpartum, participants who introduced solids up to 14 days prior to 6 months but otherwise provided only HM were classified as exclusively HM feeding at 6 months postpartum.1 22 Participants who were exclusively HM feeding at 2 weeks, 2 months and 4 months were classified as practicing exclusive HM feeding postdischarge to 4 months, and those who were also exclusively HM feeding at 6 months were classified as practicing exclusive HM feeding postdischarge to 6 months. Hospital formula supplementation (yes/ no) was considered an independent predictor of HM feeding outcomes.23
Maternal sociodemographic data were collected via interviewer-administered questionnaire prenatally in Study B and at 2 weeks postpartum in Study A. Sociodemographics included maternal age (years); parity (primiparous, multiparous); education level (high school or less, postsecondary); length of time in Canada (<1 year, 1 to <3 years, >3 years, born in Canada) and ethnicity. Participants self-reported their ethnicity using a standardised list of geographically based options developed and validated for a large birth cohort study based in Toronto.24 Based on the distribution of responses to the list of geographically based ethnicities, five categories were defined for analysis (East Asian, Other Asian, African, Latin American and European/Caribbean/Other).
Gestational age at birth was assessed using participant-reported due dates and infant birth dates. Participants who gave birth before 37 completed weeks of gestation were classified as having a preterm birth, with late preterm defined as 34 to <37 completed weeks and moderate preterm as 32 to <34 completed weeks.25
In Study A, household income was assessed at 2 weeks postpartum and classified as above or below the Statistics Canada size-adjusted Low Income Cut-Off.26 In Study B, household income adequacy was assessed at 6 months postpartum and classified as meeting all, most, some, very little or none of regular household expenses, using standardised questions from Statistics Canada’s Employment Insurance Coverage Survey.27 Participants in Study B were also asked about receipt of federal Employment Insurance maternity leave benefits (yes/no). In both studies, food insecurity was assessed at 6 months postpartum using the Household Food Security Survey Module of the Canadian Community Health Survey and classified as none, marginal, moderate or severe based on the number of affirmative responses.28 29
Receipt of the IBCLC services (yes/no) and number of IBCLC visits (0, 1, >1) was recorded from CPNP site records for Study A participants and from research records of Study B participants recruited to the post-intervention group. Although some participants received breast pumps through the IBCLCs, we did not collect data on the use of these pumps or participants’ access to pumps through other sources.
In Study B only, the Breastfeeding Self-Efficacy Scale-Short Form was administered at 2 weeks postpartum.30 This is a validated and widely used 14-item scale which produces a score from 14 to 70, with higher scores indicating greater breastfeeding self-efficacy.
Statistical analysis
Descriptive statistics were calculated for all variables of interest. Continuous measures such as age were summarised using means and SD whereas categorical measures were summarised using counts and percentages. For Study B only, a t-test was used to compare mean breastfeeding self-efficacy scores between participants who did and did not use expressed HM at 2 weeks postpartum.
Associations between any expressed HM use at 2 weeks postpartum and HM feeding outcomes were first assessed by χ2 tests then studied further using multivariable logistic regression analysis. Participants with data for all exposure variables and the outcome measure were included in each model. Outcome measures were: (i) cessation of any HM feeding before 6 months postpartum; (ii) non-exclusive HM feeding postdischarge to 4 months postpartum and (iii) non-exclusive HM feeding postdischarge to 6 months postpartum. The global recommendation is exclusive HM feeding for 6 months,1 but a separate analysis of Study B data showed that this practice was frequently compromised after 4 months by introduction of solids and non-formula fluids.31 We therefore assessed non-exclusive HM feeding to both 4 and 6 months in order to examine associations with and without the influence of complementary feeding.
Potential exposure variables considered for inclusion in the multivariable logistic regression analysis were: maternal age, education level, parity, years in Canada, geographically-based ethnicity, infant sex, any household food insecurity, household food insecurity category, hospital formula supplementation and access to IBCLC services through the CPNP. Preterm birth was not considered as the frequency count fell below 10%. Each potential variable was first assessed in bivariate screening for its association with each outcome, using χ2 tests for categorical variables and t-tests for continuous variables. Variables with p values less than 0.15 in bivariate screening were included in the multivariable logistic regression models for each outcome. Prior to modelling, multicollinearity was assessed using tolerance statistics. A tolerance value of <0.4 was used as the cut-point for the presence of multicollinearity. In such cases, only one member of a correlated set would be retained for the multivariable model.
The models were developed to meet the statistical requirements for the number of covariates in a valid logistic regression model. If the model did not have numerical tolerance for all identified covariates, those deemed most relevant to the objective and with lowest p values were retained. Model fit was assessed using the Hosmer-Lemeshow goodness-of-fit test and area under the curve. Results are presented using ORs and their associated 95% CI.
As preterm birth could not be included as a covariate, we conducted a sensitivity analysis including only participants with term-born infants. We also conducted an exploratory analysis with the subsample of participants who had access to IBCLC services through the CPNP sites. We followed the procedures described above to assess the effect of receiving IBCLC visits on the association between expressed HM use at 2 weeks postpartum and HM feeding outcomes. In addition to the potential exposure variables noted above, bivariate screening included the number of IBCLC visits received (0, 1 or >1) and multivariable logistic regression models tested for the interaction between expressed HM use and the number of IBCLC visits. If the interaction was not significant, the interaction term was removed and the model rerun.
All statistical analyses were performed using IBM SPSS Statistics for Windows, V.26 (IBM, Armonk, New York, USA).
Results
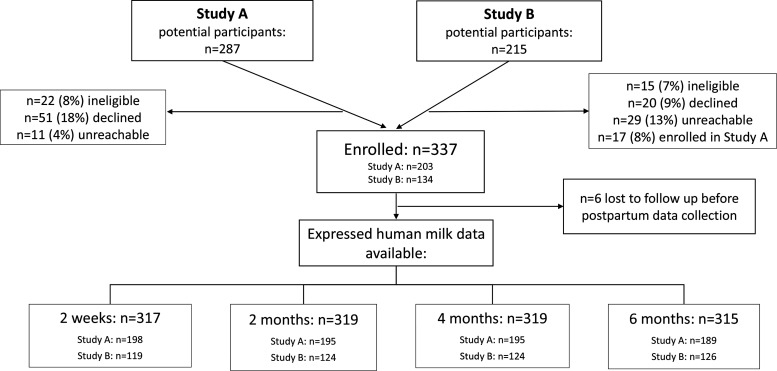
There were 287 potential participants for Study A and 215 for Study B, of whom 337 were enrolled and 331 provided infant feeding data (figure 1). Study retention was high (93%), and 315 participants provided data on expressed HM feeding at 6 months postpartum. Fourteen participants attended more than one CPNP site and enrolled in both studies simultaneously, and three participants enrolled in both studies but for separate pregnancies. Only the Study A record was retained for each of these participants in the pooled dataset, in order to account for their access to IBCLC services. The mean age of participants was 32 years, the majority (66%) had postsecondary education and 51% were primiparous (table 1). Almost all participants had term-born infants, and of the 11 (3%) who gave birth before 37 weeks’ gestation, 10 were classified as late preterm and one was moderately preterm. Ethnic diversity was high in our sample, and 91% of participants were immigrants to Canada, with 38% having lived in Canada for less than 3 years. Nearly half (44%) reported household food insecurity.
Figure 1.
Participant flow diagram.
Table 1.
Participant characteristics
| Characteristic | Indicator | n (%) |
| Age (N=330) |
Mean age (SD): 31.9 years (4.9) | |
| Education (N=331) |
<High school Postsecondary |
113 (34.1) 218 (65.9) |
| Parity (N=330) |
Primiparous Multiparous |
167 (50.6) 163 (49.4) |
| Newcomer status (N=331) |
<1 year in Canada 1 to <3 years in Canada >3 years in Canada Born in Canada |
46 (13.9) 80 (24.2) 175 (52.9) 30 (9.1) |
| Ethnicity (N=326) |
East Asian Other Asian African Latin American European/Caribbean/Other |
129 (39.6) 51 (15.6) 42 (12.9) 59 (18.1) 45 (13.8) |
| Infant sex (N=331) |
Male Female |
176 (53.2) 155 (46.8) |
| Preterm birth (N=326) |
No Yes |
315 (96.6) 11 (3.4) |
| Household food security (N=316) |
Secure Marginal insecurity Moderate insecurity Severe insecurity |
176 (55.7) 31 (9.8) 74 (23.4) 35 (11.1) |
| Household income (Study A only; N=197) |
Below low income cut-off Above low income cut-off Don’t know/prefer not to answer |
108 (54.8) 71 (36.0) 18 (9.1) |
| Proportion of regular expenses met by household income* (Study B only; N=124) | All Most Some Very little None Don’t know/prefer not to answer |
60 (48.4) 30 (24.2) 21 (16.9) 10 (8.1) 1 (0.8) 2 (1.6) |
| Receipt of maternity benefits† (Study B only; N=124) |
No Yes Don’t know/prefer not to answer |
85 (68.5) 38 (30.6) 1 (0.1) |
*Categorical variable from Statistics Canada Employment Insurance Coverage Survey used to assess household income adequacy to meet regular expenses during the first 6 months postpartum.
†Categorical variable used to assess receipt of maternity benefits through the federal Employment Insurance programme, which has eligibility criteria based on prior employment.
All participants initiated HM feeding but in-hospital formula supplementation was common (57%) (table 2). Eighty per cent of participants continued feeding HM for at least 6 months but exclusivity was low. Of the total sample, only 28% practiced exclusive HM feeding postdischarge to 4 months and 16% to 6 months. Nearly three-quarters of all study participants had access to IBCLC services through the CPNP sites. Of these, 72% used the service, with 36% receiving one visit, 30% receiving two visits and 6% receiving more than two visits.
Table 2.
Infant feeding practices and utilisation of IBCLC services (N=333)
| Indicator | n (%) |
| Initiated human milk feeding | 333 (100.0) |
| Infant received formula in hospital (N=325) | 186 (57.2) |
| Continued human milk feeding for 6 months (N=323) | 257 (79.6) |
| Exclusively fed human milk for at least 4 months (N=320) | 91 (28.4) |
| Exclusively fed human milk for 6 months (N=322) | 52 (16.1) |
| Access to IBCLC services through the CPNP | 245 (73.6) |
| Received ≥1 IBCLC visit (N=245) | 177 (72.2) |
CPNP, Canada Prenatal Nutrition Program; IBCLC, International Board Certified Lactation Consultant.
At 2 weeks postpartum, 34% of participants reported using expressed HM (table 3). The frequency dropped at each subsequent data collection point to 8% at 6 months. Nine participants (3%) provided expressed HM at all time points, while 49% never provided expressed HM. Most participants who provided expressed HM used it for at least one daily feed at all time points (75% at 2 weeks, 78% at 2 and 4 months and 69% at 6 months). The provision of expressed HM as a top-up to feeds at the breast was greatest at 2 weeks postpartum (6%), and by 6 months, only one participant was using expressed HM in this way (table 3).
Table 3.
Expressed human milk feeding practices
| Time point | Any expressed HM n (%) |
Daily expressed HM feeds n (%) |
Occasional expressed HM feeds n (%) |
Daily expressed HM top-ups n (%) |
| 2 weeks | 107 (33.8) N=317 |
80 (25.5) N=314 |
7 (2.2) N=314 |
20 (6.4) N=314 |
| 2 months N=319 |
79 (24.8) | 62 (19.4) | 11 (3.4) | 7 (2.2) |
| 4 months N=319 |
46 (14.4) | 36 (11.3) | 7 (2.2) | 4 (1.3) |
| 6 months N=315 |
26 (8.3) | 18 (5.7) | 7 (2.2) | 1 (0.3) |
Note: both daily expressed HM feeds and top-ups to were provided by 3 participants at 2 weeks and by 1 participant at 2 months.
HM, human milk; Occasional, less than daily frequency; Top-ups, expressed HM provided immediately after feeding at the breast.
For Study B participants (n=112), the mean breastfeeding self-efficacy score at 2 weeks postpartum was significantly lower among those using expressed HM (mean (SD): 47.8 (13.6) vs 58.6 (10.6); p<0.001).
Table 4 presents the associations between any use of expressed HM at 2 weeks postpartum and HM feeding outcomes. All multivariable regression models demonstrated goodness-of-fit based on the Hosmer-Lemeshow test (p>0.05) and area under the curve (>0.7). In the adjusted analyses, expressed HM use at 2 weeks postpartum was associated with cessation of HM feeding before 6 months (OR 2.66; 95% CI 1.41 to 5.05) and with non-exclusive HM feeding to 4 months (OR 2.19; 95% CI 1.16 to 4.14) and to 6 months (OR 3.65; 95% CI 1.50 to 8.84). In-hospital formula supplementation was also associated with cessation of HM feeding before 6 months (OR 2.37; 95% CI 1.16 to 4.84) and non-exclusive HM feeding to 4 months (OR 4.46; 95% CI 2.47 to 8.02) and 6 months (OR 3.45; 95% CI 1.67 to 7.15). Other variables significantly associated with cessation of HM feeding were multiparity (OR 2.52; 95% CI 1.31 to 4.86), not having access to IBCLC visits through the CPNP (OR 2.21; 95% CI 1.08 to 4.52) and ethnicity (p=0.02). Participants of self-reported African origin were least likely to stop HM feeding before 6 months postpartum in comparison with all other ethnicity categories (online supplemental file 1). Ethnicity was not associated with exclusivity of HM feeding but education below postsecondary was associated with non-exclusive HM feeding for 6 months (OR 2.48; 95% CI 1.11 to 5.52).
Table 4.
Multivariable logistic regression results: associations between expressed human milk use at 2 weeks postpartum and human milk feeding outcomes
| Model | Outcome (sample size for unadjusted; adjusted) |
OR (95% CII) | |||
| Unadjusted | P value | Adjusted | P value | ||
| 1 | Cessation before 6 months (N=309; N=296) | 3.01 (1.69 to 5.35) | <0.001 | 2.66 (1.41 to 5.05) | 0.003 |
| 2 | Non-exclusive human milk feeding postdischarge for 4 months (N=311; N=300) | 2.70 (1.51 to 4.84) | 0.001 | 2.19 (1.16 to 4.14) | 0.016 |
| 3 | Non-exclusive human milk feeding postdischarge for 6 months (N=310; N=299) | 4.00 (1.74 to 9.23) | 0.001 | 3.65 (1.50 to 8.84) | 0.004 |
Model 1 adjusted for parity, hospital formula, ethnicity and access to IBCLC services; Model 2 adjusted for hospital formula and ethnicity; Model 3 adjusted for hospital formula, ethnicity and postsecondary education.
IBCLC, International Board Certified Lactation Consultant.
bmjopen-2021-055830supp001.pdf (165KB, pdf)
These findings were consistent in the sensitivity analysis including only participants with term-born infants. In the subsample of participants with access to IBCLC services through the CPNP sites, expressed HM use at 2 weeks was associated with HM feeding cessation (OR 4.66; 95% CI 2.10 to 10.34) and non-exclusive HM feeding to 6 months (OR 3.44; 95% CI 1.12 to 10.61) in the multivariable regression models (table 5). There was also an association with non-exclusive HM feeding to 4 months in unadjusted analysis but significance was not retained in the adjusted model (OR 1.50; 95% CI 0.69 to 3.28). There was no significant interaction between the number of IBCLC visits and use of expressed HM at 2 weeks postpartum in any of the models. However, not receiving an IBCLC visit compared with receipt of either 1 or >1 visit was an independent predictor of HM feeding cessation (p=0.003). Receipt of >1 IBCLC visit compared with one visit was associated with non-exclusive HM feeding for 6 months (OR 3.74; 95% CI 1.35 to 10.31). These models demonstrated goodness-of-fit based on the Hosmer-Lemeshow test (p>0.05) and area under the curve (>0.7).
Table 5.
Multivariable logistic regression results: associations between expressed human milk use at 2 weeks postpartum and human milk feeding outcomes in the subsample with access to IBCLC services through the CPNP
| Model | Outcome (sample size for unadjusted; adjusted) |
OR (95% CII) | |||
| Unadjusted | P value | Adjusted | P value | ||
| 4 | Cessation before 6 months (N=234; N=231) | 2.87 (1.43 to 5.74) | 0.003 | 4.66 (2.10 to 10.34) | <0.001 |
| 5 | Non-exclusive human milk feeding postdischarge for 4 months (N=233; N=223) | 2.15 (1.08 to 4.27) | 0.028 | 1.50 (0.69 to 3.28) | 0.305 |
| 6 | Non-exclusive human milk feeding postdischarge for 6 months (N=234; N=229) | 4.55 (1.55 to 13.36) | 0.006 | 3.44 (1.12 to 10.61) | 0.031 |
Model 4 adjusted for parity and number of IBCLC visits; Model 5 adjusted for hospital formula, ethnicity and number of IBCLC visits; Model 6 adjusted for hospital formula and number of IBCLC visits.
CPNP, Canada Prenatal Nutrition Program; IBCLC, International Board Certified Lactation Consultant.
Discussion
In this prospective study, expressed HM use was common in a multiethnic cohort of socially and economically vulnerable women with primarily term-born infants, with the highest prevalence at 2 weeks postpartum (34%). In adjusted analysis, use of expressed HM at 2 weeks postpartum, regardless of the intensity of use, was associated with cessation of any HM feeding before 6 months and with non-exclusive HM feeding to both 4 and 6 months postpartum. These findings demonstrate that early postpartum use of expressed HM may not support longer-term recommended HM feeding practices.
Prior studies have reported high rates of expressed HM use in high-income countries, with some evidence of lower rates among vulnerable women, such as those with lower education or income.3 8 32 To our knowledge, the only other relevant Canadian data are from the Canadian Healthy Infant Longitudinal Development cohort study (n=2553), in which 55% of participants providing any HM at 3 months postpartum reported some expressed HM use; 74% continued breastfeeding for at least 6 months.8 We found a similar rate of continued breastfeeding but a lower prevalence of expressed HM use. Further studies of expressed HM use in Canada and among vulnerable sub-populations are needed.
There are few prior studies examining the association between early postpartum expressed HM use and later HM feeding practices, and differences in study methods limit comparability. Rates of any and exclusive HM feeding also vary between studies. In an Australian cohort study, 46% of participants (n=914) provided expressed HM during the postpartum hospital stay and 68% were still providing some amount of HM at 6 months.6 In adjusted analysis, not feeding exclusively at the breast in the first 24–48 hours predicted cessation of any and exclusive HM feeding before 6 months, but the specific association between expressed HM feeding and later practices was not assessed, and exclusive HM feeding referred to milk feeds only.6 In an American study (n=946) in which 71% of participants continued HM feeding for at least 12 weeks, expressing HM within the first 3 weeks postpartum predicted HM feeding cessation by 12 weeks, while pumping after 3 weeks was protective of continued HM feeding.33 A pooled analysis of two cohort studies in Hong Kong (n=2450) found that only exclusive use of expressed HM at 1 month postpartum predicted cessation of any HM feeding before 6 months and did not find a significant association with exclusive HM feeding in the adjusted analysis.16 However, ‘exclusive expressed HM’ was determined by the proportion of HM feeds, not all feeds, that were expressed HM, and use of formula or other milks was not reported. The rate of continued HM feeding to 6 months was low in this study (29%), and by 1 month postpartum, 35% of the sample had already stopped any HM feeding and were not included in the analysis.16
Secondary analyses of the Infant Feeding Practices Study II in the USA found that pumping before 1.5 months postpartum, regularly and for non-elective reasons (such as difficulties feeding at the breast or return to work) increased the risk of cessation of both any and exclusive HM feeding.14 15 We did not collect data on reasons for expressed HM use, but based on the patterns we observed, we hypothesise that our findings reflect the use of expressed HM as a strategy to manage the early stages of lactation and suggest it may be a marker of difficulties feeding at the breast. This aligns with our finding that breastfeeding self-efficacy scores were significantly lower among Study B participants using expressed HM at 2 weeks postpartum. Other studies have found difficulties feeding at the breast and concerns about milk supply to be commonly reported reasons for expressed HM use during the hospital stay6 34 and up to 4.5 months postpartum.3 4 32 These are also the most common reasons reported for early cessation of any and exclusive HM feeding.35 36 Using expressed HM to address early lactation concerns may result in disruption to the establishment of a full milk supply, which relies on frequent suckling and effective milk removal by the infant.37 Use of a high quality breast pump which mimics infant suckling may assist in this process, but this requires frequent pumping sessions with full drainage of the breasts.37 We also found that, in addition to expressed HM use, in-hospital formula supplementation and not having access to IBCLC services through the CPNP predicted early cessation of HM feeding in our cohort.
Taken together, these findings reinforce long-standing guidance on the need for both hospitals and community services to support women to successfully establish and maintain lactation through prenatal preparation, access to skilled lactation support from birth, enhanced breastfeeding self-efficacy and maternal mental healthcare.33 38–41 These findings also suggest that breast pump provision should be embedded within a larger framework of lactation education and skilled support to avoid or reduce potential unintended negative influences on continued HM feeding. Explicit information on the benefits and risks of pumping is currently lacking in Canadian infant feeding guidelines.22
The findings have implications for strengthening the specific programmes that provided the context for this study and beyond. Three-quarters of participants had access to free, in-home IBCLC visits for postpartum lactation support and 72% of these did receive at least one visit. The results suggest this specific localised intervention could be strengthened through greater focus on the establishment of lactation, including prenatal preparation.42 Maternal mental healthcare is also critical in this study population, as immigrant women are at higher risk of postpartum depression.43
Strengths and limitations
Strengths of this study include prospective data collection at multiple time points over the first 6 months postpartum with a short recall period to improve data accuracy.44 Data collection included the proportion of feeds that were expressed HM and the use of expressed HM as a top-up to feeding at the breast, which provide more nuanced understanding of expressed HM feeding practices. There were high recruitment and retention rates in both Studies A and B, which we attribute to the embeddedness of the lead researchers (AM and JF) in the weekly CPNP programmes, which helped build trust and rapport with vulnerable study participants.45
A limitation is that we did not collect data on pump ownership or use, which are needed for a full understanding of HM production and feeding practices.46 We also did not assess participants’ intentions regarding pump use or expressed HM feeding, reasons for providing expressed HM, experiences with lactation difficulties in the early postpartum period or employment status. Inclusion of these data is recommended for future studies. We were unable to include income or breastfeeding self-efficacy as potential covariates in our regression analyses as these data were not collected consistently between the two studies. The multivariable regression models assessing associations with HM feeding cessation and non-exclusive HM feeding for 6 months did not have room for all potential predictors identified in bivariate screening, while few predictors were identified for non-exclusive HM feeding for 4 months. Thus, we may not have identified or included all relevant covariates, although all models demonstrated goodness-of-fit. The findings are not generalisable to other CPNP sites or to the population in general, and all data were self-reported by participants. This introduces risk of recall and social desirability biases, which may have resulted in higher than actual rates of any and exclusive HM feeding. These biases were mitigated through the use of prospective data collection with a short recall period, rapport building with participants and collecting data on all infant feeding practices, not just HM.
Conclusion
In a multiethnic cohort of vulnerable women attending the CPNP at three sites in Toronto, expressed HM use was highest at 2 weeks postpartum, and this was associated with increased risk of early HM feeding cessation and non-exclusive HM feeding for 4 and 6 months postpartum. These findings suggest that feeding expressed HM in the early postpartum period may be a marker of lactation difficulties, but further research is needed to confirm this. The majority of study participants had access to free, in-home IBCLC visits through the participating CPNP sites, and this study provides insights to strengthen and tailor this intervention. A greater focus on prenatal preparation for lactation and access to skilled lactation support in the immediate postpartum period is recommended to assist in the establishment of effective feeding at the breast and to build breastfeeding self-efficacy in order to enable women to achieve their HM feeding goals.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the contribution of all study participants, and Yiqin Mao and Stephanie Zhang for their assistance with recruitment and data collection.
Footnotes
Twitter: @ed4socialchange
Contributors: AM contributed to the design and conceptualisation of the work, led implementation and data collection for Study B, conducted primary data analysis for this work, drafted the manuscript and finalised it for submission. JF contributed to the design and conceptualisation of the work, led implementation and data collection for Study A, assisted with data analysis for this work and critically reviewed the manuscript. SS, BU, YMN and CR facilitated the integration of research activities into the community CPNP programs and critically reviewed the manuscript. EDR contributed to the design and conceptualisation of the work, including the designs of both Studies A and B and critically reviewed the manuscript. C-LD contributed to the design and conceptualisation of the work, including the design of Study B, and critically reviewed the manuscript. AK provided oversight to the statistical analysis and critically reviewed the manuscript. DLO and DS gave oversight to the design and conceptualisation of the study and to Studies A and B, provided support for data collection and analysis and critically reviewed the manuscript. All authors gave final approval of the manuscript.
Funding: This work was supported by a Canadian Institutes of Health Research Doctoral Research Award (#GSD-157928) to AM and by The Sprott Foundation and the Joannah and Brian Lawson Centre for Child Nutrition. The graduate student stipend of JF was supported by an Ontario Graduate Scholarship and Peterborough K.M. Hunter Charitable Foundation Graduate Award.
Disclaimer: The funders had no role in the study design, data analysis, interpretation or drafting of the manuscript.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. The datasets generated and/or analysed for this study are not publicly available in order to protect participant anonymity and confidentiality.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethics approval was obtained for Studies A and B from the Office of Research Ethics at the University of Toronto (protocol #34482 and #35845, respectively). Study B was also approved by the Research Ethics Board of Toronto Public Health (#2018-11). All participants provided written informed consent to participate.
References
- 1.World Health Organization . Global strategy for infant and young child feeding. Geneva: WHO, 2003. http://apps.who.int/iris/bitstream/handle/10665/42590/9241562218.pdf?sequence=1 [Google Scholar]
- 2.World Health Organization . Indicators for assessing infant and young child feeding practices: definitions and measurement methods. Geneva: WHO, 2021. https://www.who.int/publications/i/item/9789240018389doi:https://www.who.int/publications/i/item/9789240018389 [Google Scholar]
- 3.Labiner-Wolfe J, Fein SB, Shealy KR, et al. Prevalence of breast milk expression and associated factors. Pediatrics 2008;122 Suppl 2:S63–8. 10.1542/peds.2008-1315h [DOI] [PubMed] [Google Scholar]
- 4.Fan HSL, Fong DYT, Lok KYW, HSL F, KYW L, et al. Expressed breast milk feeding practices in Hong Kong Chinese women: a descriptive study. Midwifery 2020;91:102835. 10.1016/j.midw.2020.102835 [DOI] [PubMed] [Google Scholar]
- 5.Binns CW, Win NN, Zhao Y, et al. Trends in the expression of breastmilk 1993-2003. Breastfeed Rev 2006;14:5–9. [PubMed] [Google Scholar]
- 6.Forster DA, Johns HM, McLachlan HL, et al. Feeding infants directly at the breast during the postpartum hospital stay is associated with increased breastfeeding at 6 months postpartum: a prospective cohort study. BMJ Open 2015;5:e007512. 10.1136/bmjopen-2014-007512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jiang B, Hua J, Wang Y, et al. Evaluation of the impact of breast milk expression in early postpartum period on breastfeeding duration: a prospective cohort study. BMC Pregnancy Childbirth 2015;15:268. 10.1186/s12884-015-0698-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azad MB, Vehling L, Chan D, et al. Infant feeding and weight gain: separating breast milk from breastfeeding and formula from food. Pediatrics 2018;142:e20181092. 10.1542/peds.2018-1092 [DOI] [PubMed] [Google Scholar]
- 9.Li R, Magadia J, Fein SB, et al. Risk of bottle-feeding for rapid weight gain during the first year of life. Arch Pediatr Adolesc Med 2012;166:431–6. 10.1001/archpediatrics.2011.1665 [DOI] [PubMed] [Google Scholar]
- 10.Boone KM, Geraghty SR, Keim SA. Feeding at the breast and expressed milk feeding: associations with otitis media and diarrhea in infants. J Pediatr 2016;174:118–25. 10.1016/j.jpeds.2016.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noel-Weiss J, Boersma S, Kujawa-Myles S. Questioning current definitions for breastfeeding research. Int Breastfeed J 2012;7:9. 10.1186/1746-4358-7-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rasmussen KM, Felice JP, O'Sullivan EJ, et al. The meaning of "breastfeeding" is changing and so must our language about it. Breastfeed Med 2017;12:510–4. 10.1089/bfm.2017.0073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johns HM, Forster DA, Amir LH, et al. Prevalence and outcomes of breast milk expressing in women with healthy term infants: a systematic review. BMC Pregnancy Childbirth 2013;13:212. 10.1186/1471-2393-13-212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Felice JP, Cassano PA, Rasmussen KM. Pumping human milk in the early postpartum period: its impact on long-term practices for feeding at the breast and exclusively feeding human milk in a longitudinal survey cohort. Am J Clin Nutr 2016;103:1267–77. 10.3945/ajcn.115.115733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yourkavitch J, Rasmussen KM, Pence BW, et al. Early, regular breast-milk pumping may lead to early breast-milk feeding cessation. Public Health Nutr 2018;21:1726–36. 10.1017/S1368980017004281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bai DL, Fong DYT, Lok KYW, et al. Practices, predictors and consequences of expressed breast-milk feeding in healthy full-term infants. Public Health Nutr 2017;20:492–503. 10.1017/S136898001600241X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Public Health Agency of Canada. Canada Prenatal Nutrition Program (CPNP) , 2020. Available: https://www.canada.ca/en/public-health/services/health-promotion/childhood-adolescence/programs-initiatives/canada-prenatal-nutrition-program-cpnp.html
- 18.Francis J, Mildon A, Stewart S, et al. Breastfeeding rates are high in a prenatal community support program targeting vulnerable women and offering enhanced postnatal lactation support: a prospective cohort study. Int J Equity Health 2021;20:71. 10.1186/s12939-021-01386-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mildon A, Francis J, Stewart S, et al. Effect on breastfeeding practices of providing in-home lactation support to vulnerable women through the Canada prenatal nutrition program: protocol for a pre/post intervention study. Int Breastfeed J 2021;16:49. 10.1186/s13006-021-00396-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Francis J, Unger S, Bando N, et al. Postdischarge feeding of very-low-birth-weight infants: adherence to nutrition guidelines. J Pediatr Gastroenterol Nutr 2018;67:401–8. 10.1097/MPG.0000000000002041 [DOI] [PubMed] [Google Scholar]
- 21.O'Connor DL, Khan S, Weishuhn K, et al. Growth and nutrient intakes of human milk-fed preterm infants provided with extra energy and nutrients after hospital discharge. Pediatrics 2008;121:766–76. 10.1542/peds.2007-0054 [DOI] [PubMed] [Google Scholar]
- 22.Health Canada, Canadian Pediatric Society, Dietitians of Canada and Breastfeeding Committee for Canada . Nutrition for healthy term infants: recommendations from birth to six months. Ottawa: Health Canada, 2014. https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/infant-feeding/nutrition-healthy-term-infants-recommendations-birth-six-months.html [DOI] [PubMed] [Google Scholar]
- 23.Semenic S, Loiselle C, Gottlieb L. Predictors of the duration of exclusive breastfeeding among first-time mothers. Res Nurs Health 2008;31:428–41. 10.1002/nur.20275 [DOI] [PubMed] [Google Scholar]
- 24.Omand JA, Carsley S, Darling PB, et al. Evaluating the accuracy of a geographic closed-ended approach to ethnicity measurement, a practical alternative. Ann Epidemiol 2014;24:246–53. 10.1016/j.annepidem.2013.12.015 [DOI] [PubMed] [Google Scholar]
- 25.Shapiro-Mendoza CK, Lackritz EM. Epidemiology of late and moderate preterm birth. Semin Fetal Neonatal Med 2012;17:120–5. 10.1016/j.siny.2012.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Statistics Canada . Table 11-10-0241-01Low income cut-offs (LICOs) before and after tax by community size and family size, in current dollars. Ottawa: Statistics Canada, 2020. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1110024101 [Google Scholar]
- 27.Statistics Canada . Employment Insurance Coverage Survey – 2018. Ottawa: Statistics Canada, 2018. https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=assembleInstr&lang=en&Item_Id=494316#qb367084 [Google Scholar]
- 28.Health Canada . Canadian Community Health Survey cycle 2.2, nutrition (2004) - Income-related household food security in Canada. Ottawa: Health Canada, 2007. https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fn-an/alt_formats/hpfb-dgpsa/pdf/surveill/income_food_sec-sec_alim-eng.pdf [Google Scholar]
- 29.Health Canada . Determining food security status. Ottawa: Government of Canada, 2020. https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/household-food-insecurity-canada-overview/determining-food-security-status-food-nutrition-surveillance-health-canada.html [Google Scholar]
- 30.Dennis C-L. The breastfeeding self-efficacy scale: psychometric assessment of the short form. J Obstet Gynecol Neonatal Nurs 2003;32:734–44. 10.1177/0884217503258459 [DOI] [PubMed] [Google Scholar]
- 31.Mildon A, Francis J, Stewart S, et al. High levels of breastmilk feeding despite a low rate of exclusive breastfeeding for 6 months in a cohort of vulnerable women in Toronto, Canada. Matern Child Nutr 2022;18:e13260. 10.1111/mcn.13260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pang WW, Bernard JY, Thavamani G. Direct vs. expressed breast milk feeding: relation to duration of breastfeeding. Nutrients 2017;9:547. 10.3390/nu9060547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schwartz K, D'Arcy HJS, Gillespie B, et al. Factors associated with weaning in the first 3 months postpartum. J Fam Pract 2002;51:439–44. [PubMed] [Google Scholar]
- 34.Loewenberg Weisband Y, Keim SA, Keder LM, et al. Early breast milk pumping intentions among postpartum women. Breastfeed Med 2017;12:28–32. 10.1089/bfm.2016.0142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Odom EC, Li R, Scanlon KS, et al. Reasons for earlier than desired cessation of breastfeeding. Pediatrics 2013;131:e726–32. 10.1542/peds.2012-1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gatti L. Maternal perceptions of insufficient milk supply in breastfeeding. J Nurs Scholarsh 2008;40:355–63. 10.1111/j.1547-5069.2008.00234.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kent JC, Prime DK, Garbin CP. Principles for maintaining or increasing breast milk production. J Obstet Gynecol Neonatal Nurs 2012;41:114–21. 10.1111/j.1552-6909.2011.01313.x [DOI] [PubMed] [Google Scholar]
- 38.World Health Organization . Evidence for the ten steps to successful breastfeeding. Geneva: WHO, 1998. http://apps.who.int/iris/bitstream/handle/10665/43633/9241591544_eng.pdf;jsessionid=220F8D9CA6C3BE610A529B8EDB4F2595?sequence=1 [Google Scholar]
- 39.Pérez-Escamilla R, Martinez JL, Segura-Pérez S. Impact of the Baby-friendly Hospital Initiative on breastfeeding and child health outcomes: a systematic review. Matern Child Nutr 2016;12:402-17. 10.1111/mcn.12294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.World Health Organization . Guideline: counselling of women to improve breastfeeding practices. Geneva: WHO, 2018. https://apps.who.int/iris/bitstream/handle/10665/280133/9789241550468-eng.pdf?ua=1 [PubMed] [Google Scholar]
- 41.Dias CC, Figueiredo B. Breastfeeding and depression: a systematic review of the literature. J Affect Disord 2015;171:142–54. 10.1016/j.jad.2014.09.022 [DOI] [PubMed] [Google Scholar]
- 42.Francis J, Mildon A, Stewart S, et al. Vulnerable mothers' experiences breastfeeding with an enhanced community lactation support program. Matern Child Nutr 2020;16:e12957. 10.1111/mcn.12957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Falah-Hassani K, Shiri R, Vigod S, et al. Prevalence of postpartum depression among immigrant women: a systematic review and meta-analysis. J Psychiatr Res 2015;70:67–82. 10.1016/j.jpsychires.2015.08.010 [DOI] [PubMed] [Google Scholar]
- 44.Li R, Scanlon KS, Serdula MK. The validity and reliability of maternal recall of breastfeeding practice. Nutr Rev 2005;63:103–10. 10.1111/j.1753-4887.2005.tb00128.x [DOI] [PubMed] [Google Scholar]
- 45.Barnett J, Aguilar S, Brittner M, et al. Recruiting and retaining low-income, multi-ethnic women into randomized controlled trials: successful strategies and staffing. Contemp Clin Trials 2012;33:925–32. 10.1016/j.cct.2012.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Felice JP, Rasmussen KM. Breasts, pumps and bottles, and unanswered questions. Breastfeed Med 2015;10:412-5. 10.1089/bfm.2015.0107 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-055830supp001.pdf (165KB, pdf)
Data Availability Statement
No data are available. The datasets generated and/or analysed for this study are not publicly available in order to protect participant anonymity and confidentiality.