Abstract
Drug resistance in tuberculosis is exacerbating the threat this disease is posing to human beings. Antibiotics that were once effective against the causative agent, Mycobacterium tuberculosis (Mtb), are now no longer usable against multi- and extensively drug-resistant strains of this pathogen. To address this issue, new drug combinations and novel methods for targeted drug delivery could be of considerable value. In addition, studies have shown that the use of the antidepressant drug fluoxetine, a serotonin reuptake inhibitor, can be useful in the treatment of infectious diseases, including bacterial infections. In this study, an isoniazid and fluoxetine-conjugated multi-walled carbon nanotube nanofluid were designed to increase drug delivery efficiency alongside eliminating drug resistance in vitro. The prepared nanofluid was tested against Mtb. Expression levels of inhA and katG mRNAs were detected by Real-time PCR. ELISA was applied to measure levels of cytokine secretion (TNF-α, and IL-6) from infected macrophages treated with the nano delivery system. The results showed that these nano-drug delivery systems are effective for fluoxetine at far lower doses than for free drugs. Fluoxetine also has an additive effect on the effect of isoniazid, and their concomitant use in the delivery system can have significant effects in treating infection of all clinical strains of Mtb. In addition, it was found that the expression of isoniazid resistance genes, including inhA, katG, and the secretion of cytokines TNFα and IL6 under the influence of this drug delivery system is well regulated. It was shown that the drug conjugation can improve the antibacterial activity of them in all strains and these two drugs have an additive effect on each other both in free and conjugated forms. This nano-drug delivery method combined with host targeted molecules could be a game-changer in the development of a new generation of antibiotics that have high therapeutic efficiencies, low side effects, and the potential to overcome the problem of drug resistance.
Subject terms: Biotechnology, Microbiology, Drug delivery, Pharmaceutics
Introduction
According to the WHO reports, tuberculosis (TB) is among the top ten annual major causes of fatality and morbidity worldwide1. The disease is mainly caused by Mycobacterium tuberculosis (Mtb), a human pathogen that has been evolving to acquire resistance to drugs, leading to the emergence of multidrug-resistant (MDR) and extensively drug-resistant (XDR) phenotypes2,3. To prevent the further spread of such strains, novel approaches to diagnosis and treatment are intensely needed.
Isonicotinic acid hydrazide or isoniazid (INH) has a strong antimycobacterial activity and is being used in the clinic as the main first-line agent for decades. The treatment however suffers from its length and presence of side effects. The emergence of bacterial resistance is also a detrimental issue that should be addressed to maintain the usability of this life-saving drug4–7. Two genes that are highly involved in INH resistance are katG and inhA, with the former coding for KatG, responsible for INH bio-activation8, and the latter coding the target of the INH metabolite9. Therefore, resistance to INH in Mtb is associated with mutations within these two genes10,11. Rapid sequencing of INH-resistant strains showed significant differences in mutation rates from country to country. Differences in katG and inhA gene mutation rates between Beijing strains and non-Beijing strains could explain such discrepancies. For example, reverse hybridization studies successfully detected over 80% of INH-resistant strains among Korean isolates. Similar studies indicated that mutations in these two genes (katG and inhA) were found in 89.3% of the MDR and XDR isolates in Shanghai (China), 64% in Africa, and about 70–90% in Iran12–16.
Assessment of different antidepressant drugs including fluoxetine (FLX) revealed the antibacterial feature of CNS drugs, when used alone or in combination with different antibiotics, mainly through inhibition of efflux pumps17. Likewise, the reported synergic effects of FLX with gentamycin and erythromycin in treating MDR strains of Pseudomonas aeruginosa and Escherichia coli illustrate not only its antimicrobial activity but also its antibiotic modulatory role18. In a recent review article, the collective impact of FLX with other antiviral drugs has been proposed as a promising treatment and preventative approach for coronavirus disease19.
FLX is an approved serotonin reuptake inhibitor upregulating serotonin levels through agonistic activity toward 5-HT2B20, as well as 5-HT2C receptors21, both belonging to the G- protein-coupled receptor family. When used in macrophages infected with Mtb, FLX was found to inhibit mycobacterial growth by enhancing TNF-α secretion and inducing autophagy in infected macrophages22.
In terms of targeted drug delivery, conjugation of drugs with carbon nanotubes (CNTs) has drawn much attention with regards to their potential use in the diagnosis and therapy of different diseases23–25. To circumvent multidrug resistance in bacteria and reduce the dosage of drugs, nano-drug delivery via functionalized CNTs can be utilized. Studies have shown that both single-walled CNT (SWCNT) and multi-walled CNT (MWCNT) were able to hinder multidrug resistance, exerting their antibacterial effect through cell wall destruction, induction of oxidative stress, and fracturing of the bacterial DNA or macromolecules26. This CNT system can also be formulated in the form of nanofluids or nanoparticle suspension as they have high dispersion stability and bioavailability, and, therefore, are a viable method for drug delivery. Besides, the recommended therapeutic drugs for the treatment of TB have various neurotoxicity and hepatotoxicity side effects. So, Nano drug delivery systems of these drugs have extensive potential to solve these problems via improvement of the bioavailability of drugs and reducing the dosage and frequency of administration27,28.
In our previous study, we developed a nano-drug delivery system for INH that displayed a higher antimicrobial effect in vitro against the reference laboratory strain of Mtb (H37Rv) compared to the pure drug29. The primary goal of this study was to investigate the possible antibacterial effect of the FLX and INH combination when used as a synthesized nano-drug delivery system, as compared to the pure drugs used in combination or alone on three different strains of Mtb: the reference laboratory strain H37Rv and two clinical isolates classified as MDR or XDR. In addition, our study aimed at exploiting MWCNTs, which have lower toxicity compared to SWCNTs30. Further, the gene expression profile of inhA and katG in all treated groups were captured to understand the influence of these drug formulations on bacterial resistance. Finally, variations in the level of TNF-α and IL-6, both pivotal markers of TB-induced inflammation, were analyzed in response to the treatment.
Materials and methods
Preparation of INH, FLX, and MWCNTs
4-pyridine carboxylic acid hydrazide (INH) was purchased from Darou Pakhsh Pharmaceutical Co. (Tehran, Iran). Carboxylated (-COOH) MWCNTs were purchased from Neutrino Co. (Tehran, Iran) with specifications as presented in Table 1. Fluoxetine (FLX) was purchased from Abidi Pharmaceutical Co. (Tehran, Iran).
Table 1.
Specifications of carboxyl multi-walled carbon nanotubes (MWCNT-COOH).
| Purity | > 95% |
|---|---|
| -COOH content | 3.86 wt% |
| The rate of surface carbon atom | 8–10 mol% |
| Outer diameter | < 8 nm |
| Inner diameter | 2–5 nm |
| Length | 10–30 µm |
| Special surface area | > 500 m2/g |
| Color | Black |
| Tap density | 0.27 g/cm3 |
| True density | ~ 2.1 g/cm3 |
| Electric conductivity | > 100 s/cm |
| Manufacturing method | CVD |
Chlorination of functionalized MWCNTs
A suspension of 200 mg MWCNT in 20 ml thionyl chloride (Merck, Germany) was refluxed for 14 h at 60 °C in a chemical hood. Then the chlorinated (COCl) MWCNT was dried at 60 °C under the hood.
Drug conjugation
For loading the drug on CNT, a suspension of 100 mg chlorinated MWCNT and 300 mg drug (ratio 1:3 w/w) in 20 ml dimethylformamide (DMF) (Merck, Germany) was stirred for 20 min before sonication at 200 W in an ultrasonic device. The obtained fluid was incubated at room temperature for 6 h, then refluxed at 70° C for 16 h. This was followed by several stages of centrifugation (at 8000 rpm, 15 min each time) and washing with tetrahydrofuran, methanol, and ethanol (96%). Finally, the precipitate was dried at room temperature.
Nano-drug characterization
To ensure the binding of the drug on the CNT, elemental analysis (C-H-N-S) and Fourier transform infrared (FT-IR) analysis tests were carried out. Conjugated nanotubes and nanotubes alone were also observed and analyzed under scanning electron microscopic observation (SEM).
Nanofluid preparation
To a suspension of 200 mg nano-drug powder in 6 mL of ethanol (96%) was added 60 mg of Arabic gum dissolved in 100 mL of deionized water and the resulting mixture was stirred for 20 min. The mixture was then placed on ice and sonicated for 20 min at 200 W.
Stocks preparation and microbial testing
Mtb strains including the reference laboratory strain H37Rv, together with an MDR, and XDR clinical isolates were obtained from the microbial bank of the Mycobacterium and Pulmonary Research Department, Pasteur Institute, Iran. For each strain, microbial suspension of 0.5 McFarland turbidity (equal to 1.5 × 108 bacteria) was prepared and bacterial strains were cultured in a Lowenstein-Jensen culture medium.
Initial stocks of INH, FLX, MWCNT-INH and MWCNT-FLX were prepared with the first concentration of 1 mg/mL, 1 mg/mL, 2 mg/mL, and 2 mg/mL respectively. Then different dilutions of INH and FLX were prepared with the first concentration of 143, and 40 µg/mL respectively. MWCNT-INH and MWCNT-FLX were prepared, starting from an initial concentration of 100 and 111 µg/mL respectively. The summary of all dilutions and the corresponding concentrations is presented in Table 2.
Table 2.
Dilutions and concentrations of pure and conjugated drugs used in this study.
| Dilution | Concentration (µg/mL) | |||
|---|---|---|---|---|
| INH | FLX | MWCNT-INH | MWCNT-FLX | |
| 40 | – | 1600 | – | – |
| 20 | – | 800 | – | – |
| 10 | – | 400 | – | – |
| 5 | – | 200 | – | – |
| 2 | – | 80 | – | 222 |
| 1 | 143 | 40 | 100 | 111 |
| 1/2 | 71.5 | 20 | 50 | 55.5 |
| 1/4 | 35.75 | 10 | 25 | 27.75 |
| 1/8 | 17.87 | 5 | 12.5 | 13.87 |
| 1/16 | 8.93 | 2.5 | 6.25 | 6.93 |
| 1/32 | 4.47 | 1.25 | 3.125 | 3.47 |
| 1/64 | 2.23 | – | 1.56 | 1.73 |
| 1/128 | 1.12 | – | 0.78 | 0.87 |
| 1/256 | 0.56 | – | 0.39 | 0.43 |
| 1/512 | 0.28 | – | 0.19 | 0.22 |
| 1/1024 | 0.14 | – | – | – |
| 1/2048 | 0.07 | – | – | – |
Evaluation of the drug effects and their dose-dependencies were conducted on the bacterial strains using both the pure and conjugated forms of the drugs. At first, for the determination of growth, a microplate-based assay that uses Alamar blue reagent was evaluated for all studied concentrations. Then each obtained results of MICs against Mtb H37Rv, MDR, and XDR strains were validated by tube assay test. A checkerboard assay was performed for the combination of MWCNT-INH and MWCNT-FLX. Observations were made based on the growth of bacteria after two to three weeks of incubation.
Evaluation of synergy
The fractional inhibitory concentration (FIC) index was calculated to characterize quantitatively the activity of the antimicrobial combinations. The FIC represents the sum of the FICs of each drug tested. The calculation was done based on the following equation: A/ MICA+ B/ MICB = FICA + FICB = FIC Index, where A and B are the MIC of each antibiotic in combination (in a single well), and MICA and MICB are the MIC of each drug individually31,32. The FIC index value is then used to categorize the interaction of the INH and FLX, and also MWCNT-INH and MWCNT-FLX as follow:
FIC value < 0.5 = synergy, > 4 = antagonism, and 0.5–4 = Additive or indifference.
Cell culture
Experiments were carried out with A549 and THP-1 human cell lines, which were provided by the National Cell Bank of Iran (NCBI) (Pasteur Institute, Iran). A549 and THP-1 cells were cultured at 37° C in DMEM and RPMI, respectively, supplemented with 10% of fetal bovine serum (FBS). The cells were seeded in 6 well plates and THP-1 cells differentiated in macrophages with PMA at a concentration of 50 ng/µL for one day.
In vitro Mtb infection and cellular treatments
The supernatant was removed from each well and the cells were washed with PBS, followed by the addition of a fresh culture medium. Cells were infected for 4 h at 37 °C, at a multiplicity of infection (MOI) of 10, with a suspension of the MDR, XDR, or the H37Rv bacterial strain, adjusted to a turbidity of 0.5 McFarland with RPMI medium.
Based on the results obtained from the tube-tests studies, further evaluations such as gene expression and cytokine quantification were performed. The cells were treated with INH, FLX, MWCNT-INH, MWCNT-FLX, and a combination of drugs and nano-drugs. In each 6 well plates, the different doses (1/512, 1/1024, 1/2048) of the INH, (1/32, 1/64, 1/128) of MWCNT-INH, (60, 40) of FLX, and (2, 4, 8) of MWCNT-FLX were repeated twice. At the end of the incubation period, the pellets and supernatants of treated cells were collected for molecular and cytokines studies.
Analysis of gene expression
RNA extraction was performed for cells treated with doses less than the obtained MIC value of each group. Total RNAs were extracted from tubes in which bacteria had less growth than the control using the Gene all kit (Cat. No. 301-001) according to the manufacturer's protocol. Total RNA was transcribed into single-stranded cDNA using the Easy™ cDNA Synthesis Kit (Pars Tous, Iran). Finally, Real-Time PCR was carried out using specific primer pairs as shown in Table 3.
Table 3.
Primer sequences used for RT-PCR.
| Target gene | Forward primer 5′-3′ | Reverse primer 5′-3′ | Product (bp) |
|---|---|---|---|
| katG | AGAAGAAGTACGGCAAGAAG | TACCGCTGTAACGCTCAT | 183 |
| inhA | CATCTCGGCGTATTCGTA | CGTCATCCAGTTGTAGGC | 124 |
| 16s rRNA | AAGTCGGAGTCGCTAGTA | TACGGCTACCTTGTTACG | 183 |
Cytokine quantification and statistical analysis
ELISA was performed on supernatant collected 24 h after treatment to quantify the secretion of IL6 and TNF-α cytokines using specific kits (IBL International, Germany). The data were organized in Excel and analyzed by ANOVA using Prism software (GraphPad). Results were considered significant when P-value was lower than 0.05.
Results
Characterization of the nanosystems
Elemental analysis
The results of the elemental analysis conducted to ensure the binding of drugs to the carbon nanotubes can be seen in Table 4. Naked carbon nanotubes do not contain any nitrogen, but detectable amounts were seen in drug-functionalized nanotubes, indicating effective binding of the drugs to the carbon nanotubes. Considering the mass content of azote (N) in 100 g of MWCNT, a loading of 0.6 mmol INH/g can be inferred for MWCNT-INH, and 1.4 mmol FLX/g for MWCNT-FLX. Because of minor CNT mass reduction due to centrifugation and washing, the carbon balance could not be used to estimate the loading.
Table 4.
CHNS elemental analysis results of isoniazid and fluoxetine nano systems.
| Sample name | %C | %H | %N | %S |
|---|---|---|---|---|
| MWCNT | 96.40 | 0.04 | 0.00 | 0.00 |
| INH | 60.00 | 6.02 | 34.70 | 0.00 |
| MWCNT-INH | 90.71 | 0.62 | 2.66 | 0.00 |
| FLX | 61.00 | 5.70 | 4.26 | 0.00 |
| MWCNT-FLX | 71.28 | 0.51 | 1.29 | 0.00 |
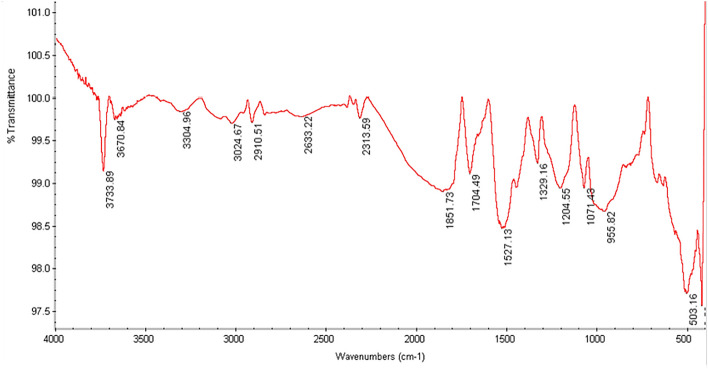
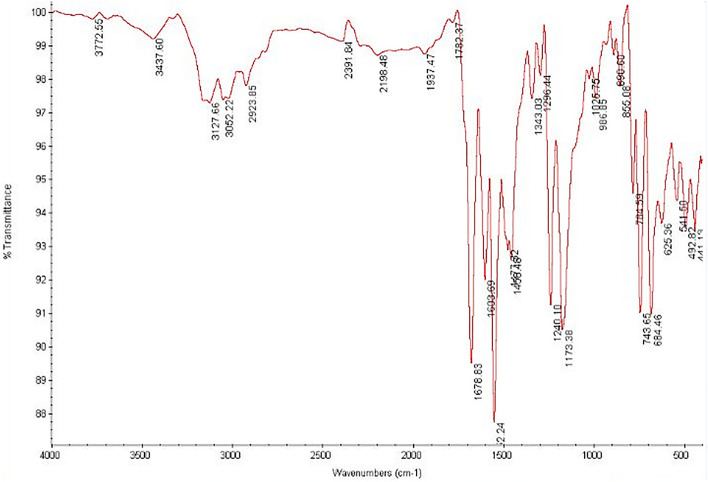
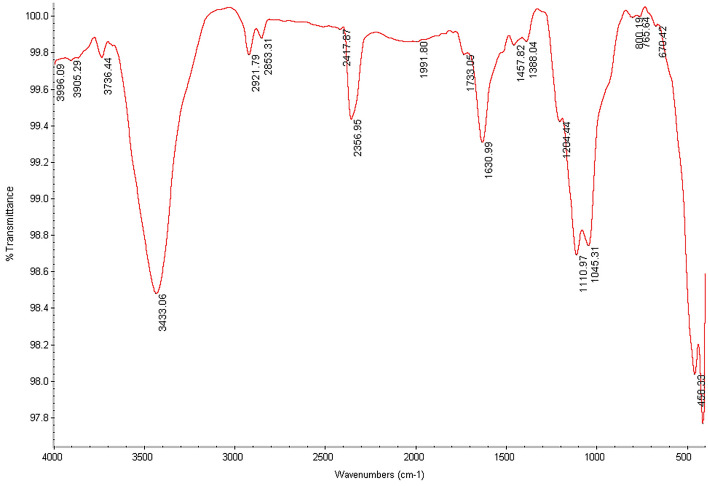
Comparison of infrared spectroscopy of non-functionalized nanotubes with drug-activated nanotubes
The Fourier Transform Infrared (FTIR) spectrums of carboxylated and drug-functionalized nanotubes are shown in Figs. 1, 2 and 3. The peak at ~ 1525 cm−1 corresponds to the C=C double bonds from the nanotube wall. Also, the peaks at 3304 cm−1 (Fig. 1) 3437 cm−1 (Fig. 2), and 3433 cm−1 (Fig. 3) correspond to the carboxylic acid group. The appearance of new peaks with lower wave numbers at ~ 1678 cm−1 in Fig. 2 and ~ 1630 cm−1 in Fig. 3 were assigned to the amide bond. So The FTIR spectrum of MWCNTs-INH (Fig. 2) and MWCNTs-FLX (Fig. 3) confirmed the formation of amide groups on the MWCNTs surface.
Figure 1.
The infrared spectrum of carboxylated nanotubes.
Figure 2.
The infrared spectrum of nanotubes functionalized with INH.
Figure 3.
The infrared spectrum of nanotubes functionalized with FLX.
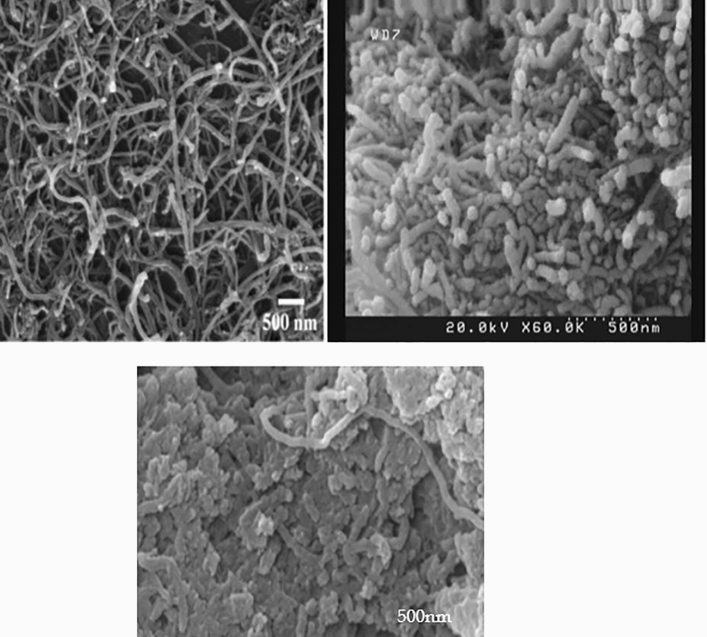
Scanning electron microscopic results
Evidence for the functionalization of multi-walled carbon nanotubes can be obtained by SEM electron microscopy images. Figure 4 shows the SEM images of MWCNTs, MWCNTs-INH, and MWCNTs-FLX. As visible in the figures, the drug-functionalized nanotubes have a different morphology and appear rougher compared to the naked nanotubes, which confirms that MWCNTs were functionalized with drugs.
Figure 4.
SEM images of the raw MWCNTs (Left), MWCNTs—INH (Right) and MWCNTs—FLX (Below).
Results of different types of treatment with INH, FLX, MWCNTs-INH, and MWCNTs-FLX
The effective concentration which could be considered as the MIC value for each treatment is summarized in Table 5. The results obtained by bacterial growth observation for all treatment groups for H37Rv, MDR, and XDR strains are summarized below.
Table 5.
Summary table of effective concentrations.
| Treatment | Strain | ||
|---|---|---|---|
| H37Rv | MDR | XDR | |
| Concentration that inhibited bacterial growth (µg/mL) | |||
| INH | 0.28 | 1.12 | 1.12 |
| FLX | 1600 | 1600 | 1600 |
| INH + FLX | 0.56 + 800 | 0.56 + 800 | 0.56 + 800 |
| MWCNT-INH | 3.125 (INH 0.26) | 6.25 (INH 0.52) | 12.5 (INH 1.04) |
| MWCNT-FLX | 222 (FLX 96) | 55.5 (FLX 24) | 6.93 (FLX 3.50) |
| MWVNT-INH + MWCNT-FLX | 0.78 + 55.5 (INH 0.067 + FLX 24) | 3.125 + 55.5 (INH 0.26 + FLX 24) | 12.5 + 6.93 (INH 1.04 + FLX 3.50) |
H37Rv treatments with the different doses of INH, FLX, INH + FLX, MWCNTs-INH, MWCNTs-FLX, and MWCNTs- INH + MWCNTs- FLX
After incubation with INH for two weeks, a significant decrease in bacterial growth was observed from a dose of 1/1024 (0.14 µg/mL) and no growth was observed from dilutions of 1/512 (0.28 µg/mL) (Figure S1). Also, a significant reduction in growth was observed at a dilution of 1/64 from MWCNTs-INH (1.56 µg/mL containing 0.13 µg/mL INH) and no growth was observed at a dilution of 1/32 (3.125 µg/mL containing 0.26 µg/mL INH) (Figure S2). The efficacy results for FLX indicate that bacterial growth is stopped at dilutions of 40, (1.6 mg/mL) (Figure S3). The treatment results of MWCNTs-FLX showed that no growth was observed from dilution of 2 (222 µg/mL, containing 96 µg/mL FLX) (Figure S4). For Checkerboard treatments on H37Rv, the different concentrations of both drugs from dilution of 2 to 1/4 for MWCNT-FLX and 1/64 to 1/512 of MWCNT-INH were tested. The bacterial growth was significantly reduced when the two nano-drug systems were combined, with dilutions of 1/128 (0.78 µg/mL containing 0.067 µg/mL of INH) of MWCNTs-INH sufficient to prevent bacterial growth when used in combination with the dilution of 1/2 (55.5 µg/mL containing 24 µg/mL of FLX) of MWCNTs- FLX (Figure S5). Checkerboard treatment on H37Rv with FLX and INH was carried out in a previous study and results showed that dilutions of 1/256 of INH (0.56 µg/mL) combined with the dilution of 20 of fluoxetine (0.8 mg/mL) inhibited bacterial growth. The antibacterial effect of MWCNT alone on H37Rv was observed at a concentration of 228 µg/mL (Figure S6).
MDR & XDR treatments with the different doses of INH, FLX, INH + FLX, MWCNTs-INH, MWCNTs-FLX, and MWCNTs-INH + MWCNTs-FLX
For the MDR strain, INH at dilution of 1/128 (1.12 µg/mL) was required to observe a significant effect on bacterial growth (Figure S7). Similarly for the XDR strain, INH at dilution of 1/128 (1.12 µg/mL) had a significant effect on bacterial growth (Figure S8). Besides, growth of the MDR strain was observed at the dose of 3.2 mg/mL and only has a few growth reductions at 1.6 mg/mL for FLX (Figure S9), while for the XDR strain only a slight growth reduction was observed at this dose of FLX (Figure S10). Results showed that bacterial growth of MDR and XDR strains were been inhibited at the dilution of 1/16 (6.25 µg/mL, containing 0.52 µg/mL of INH) and 1/8 (12.5 µg/mL, containing 1.04 µg/mL of INH) of the MWCNTs-INH respectively (Figures S11, S12).
MWCNTs-FLX has few antibacterial effects on MDR at dilution of 1/2 (55.5 µg/mL, containing 24 µg/mL of FLX) (Figure S13) and also on XDR at the dilution of 1/16 (6.9 µg/mL, containing 3.5 µg/mL of FLX) (Figure S14).
Checkerboard treatment results of MDR and XDR strains with INH and FLX showed that, in the treatment with the dilution of FLX 20 (800 µg/mL) in combination with isoniazid in the dilution of 1/256 (0.56 µg/mL), the bacterial growth was stopped (Figure S15). Besides, in the XDR treatment group at the dose of FLX 40 (1.6 mg/mL) in combination with INH at a dose of 1/128 (1.12 µg/mL) and also at doses of FLX 20 (800 µg/mL) in combination with INH at a dose of 1/256 (0.56 µg/mL), a significant reduction in growth was observed (Figure S16).
After the effect of MWCNTs-INH and MWCNTs-FLX, bacterial growth observation indicated that in the MDR strain, at the dose of 1/2 of MWCNTs-FLX (55.5 µg/mL, containing 24 µg/mL of FLX) in combination with the dose of 1/32 of MWCNTs-INH (3.125 µg/mL, containing 0.26 µg/mL of INH), no growth was observed. In the XDR strain group, the results showed that at doses of 1/16 of MWCNTs-FLX (6.93 µg/mL, containing 3.5 µg/mL of FLX) with a dose of 1/8 of MWCNTs-INH (12.5 µg/mL, containing 1.04 µg/mL of INH), bacterial growth was inhibited (Figure S17).
Quantitative analyses by Fractional Inhibitory Concentration Index (FICI) for FLX and INH
According to the calculations of the FIC index value for all states of action of isoniazid and fluoxetine in both free and conjugated form with carbon nanotubes, it was shown that in all strains, these two drugs have an additive effect on each other both in free and conjugated forms (Table 6).
Table 6.
FIC index calculation of treated groups.
| Treatment and MIC/µg/mL | INH | FLX | INH + FLX | FIC Index | MWCNT-INH | MWCNT-FLX | MWCNT-INH + MWCNT-FLX | FIC Index |
|---|---|---|---|---|---|---|---|---|
| H37Rv | 0.28 | 1600 | 0.56 + 800 | 2.5 | 3.125 | 222 | 0.78 + 55.5 | 0.5 |
| MDR | 1.12 | 1600 | 0.56 + 800 | 1 | 6.25 | 55.5 | 3.125 + 55.5 | 1.5 |
| XDR | 1.12 | 1600 | 0.56 + 800 | 1 | 12.5 | 6.93 | 12.5 + 6.93 | 2 |
Significant values are in [bold].
Gene expression analysis and IL6 and TNFα secretion studies
The data analysis of gene expression in various treatment groups was carried out by the One Way ANOVA method and showed that the expression of both inhA and katG genes in all strains increased significantly in the presence of INH (Figure S18–S20). In the presence of FLX however, both gene expressions were unchanged. For all strains tested, every treatment group involving INH saw a sharp increase in inhA expression, irrespective of the presence of FLX or the formulation in MWCNT. In contrast, the expression of katG was significantly reduced by combination therapy with free FLX, and the conjugated form of INH led to weaker levels of expression (Figure S18–S20). Results of the cytokine secretion studies showed that the levels of IL6 and TNFα secretion were significantly increased in all the treated groups, indicating that the drug treatment was able to induce pro-inflammatory pathways in TB-infected macrophages (Figure S21–S23), presumably due to efficient killing of the bacteria. The secretion of IL6 and TNF-α cytokines from TB-infected macrophages were similar between free and MWCNT-conjugated drugs, indicating that the CNT vectorization strategy could maintain an efficient targeting of the intracellular bacteria.
Discussion
In this study, the main focus was on comparing the efficacy of nano-type drugs with that of the pure, free drugs and evaluating the combined effects with host targeting agents like FLX, belonging to the group of serotonin reuptake inhibitors (SSRIs). INH is still one of the most active anti-tuberculosis agents, used for both the treatment and prevention of TB. Although INH is one of the safest and most cost-effective drugs for the treatment of TB, it causes many side effects in patients with high and long-term doses7.
Selective serotonin reuptake inhibitors are antidepressants and have shown significant activity against bacterial resistance, but the antibacterial effects, as well as the antibiotic modulatory properties of FLX, are not yet clear. The results of previous studies showed that SSRIs drugs have significant antimicrobial activity against gram-positive bacteria, but are ineffective against Enterobacteria other than Citrobacter and Pseudomonas aeroginosa33. In this study, the mentioned effects of FLX were confirmed against different strains of Mtb34, including the MDR and XDR strains. Additional studies are needed to describe the antimicrobial properties of this drug as well as the clinical implications of its use in the treatment of infections by resistant microorganisms. On the other hand, the molecular mechanisms of INH resistance include several genes that are involved in several biosynthetic networks and pathways. Mutations in the katG and inhA genes are major factors in INH resistance, followed by ahpC, kasA, ndh, iniABC, and fadE35,36. Therefore, in this research, the expression of these two main genes (inhA, katG) was studied before and after drug treatments by Real-Time PCR. The results of this study showed that the expression of katG was significantly reduced by combination therapy with both free and conjugated drugs.
As a result of a study in 2018 on a large number of CNS drugs, a synthetic analog of FLX was introduced as a selective and specific anti-tuberculosis agent and the antibacterial effects of this drug on the standard strain of tuberculosis (H37RV) were tested37. The results of some research showed that the use of a series of small molecules called Host-targeted inhibitors could target TB-infected macrophages and stop the growth of Mtb. The use of drugs such as FLX, a selective serotonin reuptake inhibitor, can increase the secretion of pro-inflammatory cytokines, induce autophagy in TB-infected macrophages and stop the growth of Mtb38,39. However, extensive studies on the toxicity of these nanostructures need to be conducted. Targeting the host is one strategy considered in this study. Also, in this research usage of FLX which is belonging to the group of serotonin reuptake inhibitors (SSRIs) has shown significant antimicrobial activity.
On the other hand, nanotubes can be activated with groups that give them new properties so that they can be easily used in the environment. With the help of nanotubes and their attachment to drug compounds such as INH and FLX by chemical reactions, a new nano product was prepared. We showed here that these new compounds have equivalent biological activity and could be classified in the family of nano-drugs3,24,40,41. Since anti-tuberculous drugs usually cannot target macrophages and have a low concentration in the lesion, so they cannot successfully kill mycobacterium tuberculosis. In addition, these drugs have no efficient penetration in the cell wall of the bacteria because of their unique cell envelope structure and composition, containing a peptidoglycan layer and its drug resistance mechanisms. In the study, we constructed a CNT-based drug delivery system, which directs the drug to the target area as well as effectively destroys the bacterial cell wall. Even in recent studies was found that the outstanding application of nano-drug delivery systems in this way is to target infected macrophages or macrophage-targeted delivery systems for enhanced intracellular Mycobacterium tuberculosis killing efficiency42.
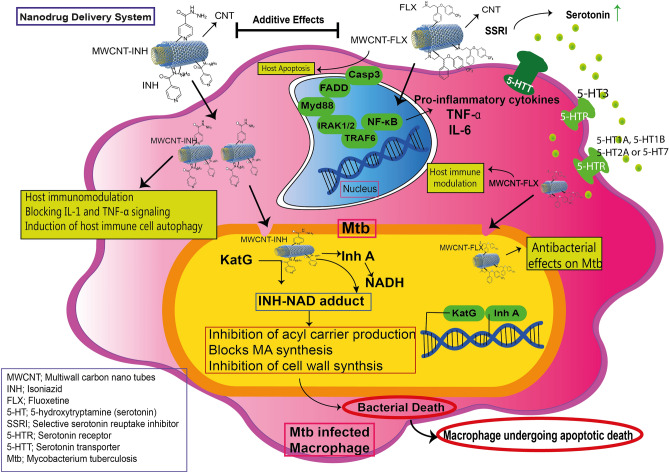
It is suggested that the uptake of functionalized MWCNTs performs by two ways, first direct penetration via the plasma membrane, and second, endocytosis processes25. Therefore, it seems that CNTs have several function in drug delivery including improve cellular uptake via disruption of bacterial cell wall, optimization of release rate, and less toxicity for host cells43. Figure 5 depicted the chemical structures of the MWCNTs conjugated with drugs and also the mechanism of drug release from MWCNTs.
Figure 5.
The chemical structures, mechanism of drug release and signaling pathway of the MWCNTs conjugated with drugs.
Conclusion
In this study, using MWCNTs, a new form of the antibiotic INH and the drug FLX were made to improve antibacterial activity by taking advantage of the additive effect that these two drugs have on each other. However, the results of this investigation, confirmed previous reports that the use of serotonin receptor agonists or antagonists can activate the autophagy pathway to kill TB bacteria, more detailed and complete studies on the relevant signaling pathways are necessary.
Because the process of approving a drug is time-consuming and costly, these methods can be obtained sooner through combination therapies because these drugs are known for their pharmacokinetic profile, and safety, are cheaper, more accessible, and can enter Phase 2 of the clinical trial faster. Also, with the increase in the number of people affected with MDR-TB, XDR-TB, and so-called drug-resistant tuberculosis (TDR-TB), new treatment strategies are needed that go beyond the conventional antibiotics.
Supplementary Information
Acknowledgements
We thank our colleagues from the Department of Mycobacteriology and Pulmonary Research, Microbiology Research Center, Pasteur Institute of Iran.
Author contributions
M.S.H.: designed and supervised the clinical study, interpreted data, read and approved manuscript; V.D.: interpreted data, read and approved the final manuscript; A.B.K.: interpreted data; V.A.: performed the experiments; M.M.: performed the experiments; M.S.: interpreted data; N.E., M.M., and S.H.P.: performed the experiments. All authors reviewed the manuscript.
Data availability
All data generated or analysed during this study are included in this published article (and its supplementary information file).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-13682-4.
References
- 1.WHO. Global Tuberculosis Report. 2020. (2020).
- 2.Mabhula A, Singh V. Drug-resistance in Mycobacterium tuberculosis: where we stand. MedChemComm. 2019;10:1342–1360. doi: 10.1039/C9MD00057G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saifullah B, Hussein MZB, Al Ali SHH. Controlled-release approaches towards the chemotherapy of tuberculosis. Int. J. Nanomed. 2012;7:5451. doi: 10.2147/IJN.S34996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tafazoli S, Mashregi M, O'Brien PJ. Role of hydrazine in isoniazid-induced hepatotoxicity in a hepatocyte inflammation model. Toxicol. Appl. Pharmacol. 2008;229:94–101. doi: 10.1016/j.taap.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 5.Saifullah B, et al. Development of a biocompatible nanodelivery system for tuberculosis drugs based on isoniazid-Mg/Al layered double hydroxide. Int. J. Nanomed. 2014;9:4749. doi: 10.2147/IJN.S63608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Erwin ER, Addison AP, John SF, Olaleye OA, Rosell RC. Pharmacokinetics of isoniazid: The good, the bad, and the alternatives. Tuberculosis (Edinburgh, Scotland) 2019;116s:S66–S70. doi: 10.1016/j.tube.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Schaberg T, Rebhan K, Lode H. Risk factors for side-effects of isoniazid, rifampin and pyrazinamide in patients hospitalized for pulmonary tuberculosis. Eur. Respir. J. 1996;9:2026–2030. doi: 10.1183/09031936.96.09102026. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y, Heym B, Allen B, Young D, Cole S. The catalase: Peroxidase gene and isoniazid resistance of Mycobacterium tuberculosis. Nature. 1992;358:591–593. doi: 10.1038/358591a0. [DOI] [PubMed] [Google Scholar]
- 9.Banerjee A, et al. inhA, a gene encoding a target for isoniazid and ethionamide in Mycobacterium tuberculosis. Science. 1994;263:227–230. doi: 10.1126/science.8284673. [DOI] [PubMed] [Google Scholar]
- 10.Musser JM, et al. Characterization of the catalase-peroxidase gene (katG) and inhA locus in isoniazid-resistant and-susceptible strains of Mycobacterium tuberculosis by automated DNA sequencing: Restricted array of mutations associated with drug resistance. J. Infect. Dis. 1996;173:196–202. doi: 10.1093/infdis/173.1.196. [DOI] [PubMed] [Google Scholar]
- 11.Basso LA, Zheng R, Musser JM, Jacobs WR, Jr, Blanchard JS. Mechanisms of isoniazid resistance in Mycobacterium tuberculosis: Enzymatic characterization of enoyl reductase mutants identified in isoniazid-resistant clinical isolates. J. Infect. Dis. 1998;178:769–775. doi: 10.1086/515362%JTheJournalofInfectiousDiseases. [DOI] [PubMed] [Google Scholar]
- 12.Park YK, et al. Comparison of drug resistance genotypes between Beijing and non-Beijing family strains of Mycobacterium tuberculosis in Korea. J. Microbiol. Methods. 2005;63:165–172. doi: 10.1016/j.mimet.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Luo T, et al. Selection of mutations to detect multidrug-resistant Mycobacterium tuberculosis strains in Shanghai, China. Antimicrob. Agents Chemother. 2010;54:1075–1081. doi: 10.1128/AAC.00964-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haas WH, et al. Molecular analysis of katG gene mutations in strains of Mycobacterium tuberculosis complex from Africa. Antimicrob. Agents Chemother. 1997;41:1601–1603. doi: 10.1128/AAC.41.7.1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doustdar F, Khosravi AD, Farnia P, Masjedi MR, Velayati AA. Molecular analysis of isoniazid resistance in different genotypes of Mycobacterium tuberculosis isolates from Iran. Microb. Drug Resist. 2008;14:273–279. doi: 10.1089/mdr.2008.0842. [DOI] [PubMed] [Google Scholar]
- 16.Khosravi AD, Goodarzi H, Alavi SM. Detection of genomic mutations in katG, inhA and rpoB genes of Mycobacterium tuberculosis isolates using polymerase chain reaction and multiplex allele-specific polymerase chain reaction. Braz. J. Infect. Dis. 2012;16:57–62. doi: 10.1016/s1413-8670(12)70275-1. [DOI] [PubMed] [Google Scholar]
- 17.Munoz-Bellido JL, Munoz-Criado S, Garcıa-Rodrıguez JA. Antimicrobial activity of psychotropic drugs: Selective serotonin reuptake inhibitors. Int. J. Antimicrob. Agents. 2000;14:177–180. doi: 10.1016/S0924-8579(99)00154-5. [DOI] [PubMed] [Google Scholar]
- 18.de Sousa AK, et al. New roles of fluoxetine in pharmacology: Antibacterial effect and modulation of antibiotic activity. Microb. Pathog. 2018;123:368–371. doi: 10.1016/j.micpath.2018.07.040. [DOI] [PubMed] [Google Scholar]
- 19.Sheikhpour M. The current recommended drugs and strategies for the treatment of coronavirus disease (COVID-19) Ther. Clin. Risk Manag. 2020;16:933. doi: 10.2147/TCRM.S262936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peng L, Gu L, Li B, Hertz L. Fluoxetine and all other SSRIs are 5-HT2B agonists-importance for their therapeutic effects. Curr. Neuropharmacol. 2014;12:365–379. doi: 10.2174/1570159X12666140828221720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ni YG, Miledi R. Blockage of 5HT2C serotonin receptors by fluoxetine (Prozac) Proc. Natl. Acad. Sci. 1997;94:2036–2040. doi: 10.1073/pnas.94.5.2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stanley SA, et al. Identification of host-targeted small molecules that restrict intracellular Mycobacterium tuberculosis growth. PLoS Pathog. 2014;10:e1003946. doi: 10.1371/journal.ppat.1003946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheikhpour M, Golbabaie A, Kasaeian A. Carbon nanotubes: A review of novel strategies for cancer diagnosis and treatment. Mater. Sci. Eng., C. 2017;76:1289–1304. doi: 10.1016/j.msec.2017.02.132. [DOI] [PubMed] [Google Scholar]
- 24.Yang W, Thordarson P, Gooding JJ, Ringer SP, Braet F. Carbon nanotubes for biological and biomedical applications. Nanotechnology. 2007;18:412001. doi: 10.1088/0957-4484/18/41/412001. [DOI] [Google Scholar]
- 25.Kamazani FM, Siadat SD, Pornour M, Sheikhpour M. A success targeted nano delivery to lung cancer cells with multi-walled carbon nanotubes conjugated to bromocriptine. Sci. Rep. 2021;11:1–15. doi: 10.1038/s41598-021-03031-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mocan T, et al. Carbon nanotubes as anti-bacterial agents. Cell. Mol. Life Sci. 2017;74:3467–3479. doi: 10.1007/s00018-017-2532-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sheikhpour M, Arabi M, Kasaeian A, Rabei AR, Taherian Z. Role of nanofluids in drug delivery and biomedical technology: Methods and applications. Nanotechnol. Sci. Appl. 2020;13:47. doi: 10.2147/NSA.S260374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.da Silva P, et al. Nanotechnology-based drug delivery systems for treatment of tuberculosis: A review. J. Biomed. Nanotechnol. 2016;12(2):241–260. doi: 10.1166/jbn.2016.2149. [DOI] [PubMed] [Google Scholar]
- 29.Zomorodbakhsh S, Abbasian Y, Naghinejad M, Sheikhpour M. The effects study of isoniazid conjugated multi-wall carbon nanotubes nanofluid on Mycobacterium tuberculosis. Int. J. Nanomed. 2020;15:5901. doi: 10.2147/IJN.S251524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sheikhpour M, et al. The applications of carbon nanotubes in the diagnosis and treatment of lung cancer: A critical review. Int. J. Nanomed. 2020;15:7063. doi: 10.2147/IJN.S263238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jain SN, et al. Antibiotic synergy test: Checkerboard method on multidrug resistant Pseudomonas aeruginosa. Int. Res. J. Pharm. 2011;2:196–198. [Google Scholar]
- 32.Lorian V. Antibiotics in Laboratory Medicine. Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 33.Munoz-Bellido J, Munoz-Criado S, Garcıa-Rodrıguez J. Antimicrobial activity of psychotropic drugs: Selective serotonin reuptake inhibitors. Int. J. Antimicrob. Agents. 2000;14:177–180. doi: 10.1016/S0924-8579(99)00154-5. [DOI] [PubMed] [Google Scholar]
- 34.Ni Y, Miledi R. Blockage of 5HT2C serotonin receptors by fluoxetine (Prozac) Proc. Natl. Acad. Sci. 1997;94:2036–2040. doi: 10.1073/pnas.94.5.2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rawat R, Whitty A, Tonge PJ. The isoniazid-NAD adduct is a slow, tight-binding inhibitor of InhA, the Mycobacterium tuberculosis enoyl reductase: Adduct affinity and drug resistance. Proc. Natl. Acad. Sci. 2003;100:13881–13886. doi: 10.1073/pnas.2235848100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vögeli B, et al. InhA, the enoyl-thioester reductase from Mycobacterium tuberculosis forms a covalent adduct during catalysis. J. Biol. Chem. 2018;293:17200–17207. doi: 10.1074/jbc.RA118.005405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kumar MMK, Madhavi K, Mohan T, Nagasree KP, Sangeeta G. Novel synthetic analogues of Fluoxetine as potent and selective anti-TB agents. J. Appl. Pharm. Sci. 2018;8:107–115. [Google Scholar]
- 38.Schrlau MG, Falls EM, Ziober BL, Bau HH. Carbon nanopipettes for cell probes and intracellular injection. Nanotechnology. 2007;19:015101. doi: 10.1088/0957-4484/19/01/015101. [DOI] [PubMed] [Google Scholar]
- 39.Ladel CH, et al. Lethal tuberculosis in interleukin-6-deficient mutant mice. Infect. Immun. 1997;65:4843–4849. doi: 10.1128/iai.65.11.4843-4849.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sheikhpour M, Barani L, Kasaeian A. Biomimetics in drug delivery systems: A critical review. J. Control. Release. 2017;253:97–109. doi: 10.1016/j.jconrel.2017.03.026. [DOI] [PubMed] [Google Scholar]
- 41.Ma W, et al. Efficacy of dual-targeting combined anti-tuberculosis drug delivery system in the treatment of tuberculous meningitis. J. Biomed. Nanotechnol. 2021;17(10):2034–2042. doi: 10.1166/jbn.2021.3169. [DOI] [PubMed] [Google Scholar]
- 42.Mazlan MKN, et al. Antituberculosis targeted drug delivery as a potential future treatment approach. Antibiotics. 2021;10(8):908. doi: 10.3390/antibiotics10080908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mohammadi M, Arabi L, Alibolandi M. Doxorubicin-loaded composite nanogels for cancer treatment. J. Control. Release. 2020;328:171–191. doi: 10.1016/j.jconrel.2020.08.033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article (and its supplementary information file).