Abstract
Background
In December 2019, Wuhan City in Hubei Province, China witnessed an outbreak of a novel type of coronavirus (COVID-19), named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The sharp rise in the number of infected cases and the surge spike in fatalities worldwide prompted the World Health Organization (WHO) to declare this rapid outbreak a global pandemic in March 2020. The economic, health, and social ramifications of COVID-19 induced fear and anxiety all over the world.
Objective
The purpose of this review is to discuss how precautionary measures and restrictions imposed by governments, such as quarantines, lockdowns, and social distancing, have not only caused economic losses, but also a rise in mental health problems specifically post-traumatic stress disorder (PTSD).
Methods
A deep comprehensive review of the relevant literature regarding the pandemic and its debilitating consequences on the psychological status of the public was performed.
Results
This review illustrates that the pandemic had a traumatic impact on the psychological functioning of the public, particularly COVID-19 survivors, older adults, and healthcare workers, due to difficulties in coping with new realities and uncertainties.
Conclusion
In this review, we have discussed the psychological implications of this pandemic and we have provided an extensive background for understanding options regarding PTSD management in healthy individuals and those with preexisting conditions.
Keywords: COVID-19, SARS-CoV-2, post-traumatic stress disorder, PTSD, stigma, health care workers
1. INTRODUCTION
In 2009, Mak et al. wrote, “Severe acute respiratory syndrome (SARS) was the first massive infectious disease outbreak of the 21st century. However, it is unlikely that this outbreak will be the last” [1]. Sadly, his prediction eventuated by the end of 2019, when the world witnessed the spread of a novel virus from the coronavirus family, termed SARS-CoV-2, causing COVID-19 disease. The condition quickly evolved from being a “pneumonia of unknown etiology”, as reported by the World Health Organization (WHO) on December 31st, 2019, to 282 confirmed cases from four different countries on January 20, 2020 [2]. On January 30, 2020, the SARS-CoV-2 outbreak was declared a Public Health Emergency of International Concern (PHEIC) by the WHO, and then as a global pandemic on March 11, 2020 [3]. Based on the most recent report published by the WHO on January 10, 2021, more than 88 million COVID-19 cases have been confirmed and the death toll has surpassed 1.9 million across all continents [4, 5]. As a result, a wide range of precautionary measures aimed at curbing and preventing the spread of the virus, were implemented by many countries. Nationwide lockdowns, mass quarantines, border shutdowns, airport closure, and cancellation of public events had to be imposed to contain this infectious disease.
Unfortunately, the enforced restrictions, and the fearmongering tactics adopted by several media outlets, have greatly impacted the psychological functioning of many people [6, 7]. High levels of distress, anxiety, mood alterations, sleep disturbances, obsessional cleaning, and post-traumatic stress disorder (PTSD) symptoms have been reported [8-11]. At present, the long-term adverse effects of the COVID-19 pandemic on mental health remain uncertain. Nevertheless, evaluation of previous outbreaks of infectious diseases that occurred this century may shed light on mental health disorders spawned by the pandemics. Two viral infections have previously caused global pandemics similar to the current COVID-19 pandemic during the 21st century: Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS). To better understand the possible ramifications of COVID-19, a systematic review and a meta-analysis study by Ahmed et al. [12] have collated the long-term clinical complications among survivors of SARS and MERS. Results clearly demonstrated reduced exercise tolerance in a considerable number of survivors, 6 months after discharge from the hospital, in addition to pulmonary dysfunction and psychological impairment. Post-traumatic stress disorder (PTSD), anxiety, and depression were observed in up to one-third of survivors at 6 months and beyond. Additionally, some of those who were infected struggled with a low quality of life even one year after their hospital discharge [12]. The study has also revealed that the long-lasting mental health consequences did not result from the infectious disease alone, but also from fear [6], stigma [6, 13], and difficulties accompanying the quarantine experience [6]. Concerning role limitation in survivors, a study by Tansey et al. [14] reported that 17% of SARS survivors suffered from persistent work dysfunction even a year after contracting the virus. Furthermore, pain disorders have been detected 3.5 years after SARS infection in around one-third of patients as reported in a study by Lam et al. [13]. At this stage, it is still premature to conclude that the same long-term psychological effects identified in individuals who experienced SARS and MERS outbreaks, will be observed in those experiencing the novel COVID-19 pandemic. However, given that SARS, MERS, and COVID-19 belong to the same family of viruses and have similar clinical features, it is reasonable to anticipate similar ramifications [12].
The prevailing sense of despondent uncertainty and anxiety, at the individual and community levels, stemming from fears of contracting a new and highly infectious life-threatening disease, renders the COVID-19 pandemic a traumatic event [7]. People who have contracted the virus or those who have had a close relative unexpectedly die from the illness may consider the experience traumatic. For others, the experience could be classified as a case of persistent worry and stress but not exactly a trauma [11]. As stress causes neurological changes and precipitates mental illnesses, the risk of developing PTSD in these individuals is greatly increased [8]. According to the American Psychiatric Association, PTSD is “a psychiatric trauma and stressor-related disorder that develops in some people after experiencing or witnessing a traumatic event, such as combat, crime, serious accident, natural disaster, rape, or violent personal assault [15].” As demonstrated in the meta-analysis by Ahmed et al. [12], PTSD has also been reported in the months following the SARS and MERS outbreaks. In the first studies conducted in China and Italy tackling the initial phase of COVID-19, PTSD symptoms were reported [8, 9] where certain groups showed a higher risk of developing PTSD than others [7]. These include COVID-19 survivors, bone-weary health care workers (HCWs), people living in constant fear due to close contact with infected people, and the general population affected by the restrictive measures [7]. Besides the higher risk of contracting the virus, frontline workers in private and public sectors are at a higher risk of facing adverse psychological outcomes such as burnout, anxiety, depression, fear of transmitting infection, increased substance-dependence, and PTSD [6].
In this review, we discuss how the COVID-19 pandemic, along with the strict precautionary measures undertaken by governments and the resulting social stigma, had resulted in psychological stress. People across different age groups, specifically those who were more susceptible to contracting the virus, as well as the ones who had pre-existing psychiatric disorders were more prone to mental illnesses and PTSD. The review also sheds light on the different therapeutic approaches that could and have been implemented to ease the resulting anxiety and treat mental illnesses and PTSD.
2. PUBLIC RESPONSE TO THE GLOBAL PANDEMIC AND SOCIAL STIGMA ASSOCIATED WITH COVID-19
In response to the rapidly growing pandemic, several measures were put in place in an attempt to contain the virus spread and hinder its transmission: isolation of cases, quarantine of exposed individuals, travel bans, and social distancing, among other measures were enforced [16]. In parallel to these governmental attempts at containment, fear and worry kept spreading among the public [17-20]. Such fear of COVID-19, now termed “coronaphobia”, was fueled by all the uncertainties that surround the novel virus [17, 21]. Other fear-inciting events include COVID-19’s high transmissibility, wavering trust in governments’ response to the pandemic, and the shortage of medical supplies and personal protective equipment (PPE) [17]. In addition, the emergence of new variant strains of SARS-CoV-2 – that harbor a series of mutations – in the United Kingdom (UK), South Africa, and Japan at the beginning of this year (2021) threatens to make the pandemic and its effects on people’s mental health far worse. The extent of fear should not be underestimated; one man in India [22] and nurses in Italy [23] committed suicide out of fear of contracting the virus or spreading it to others. All of this has served to set the stage for the stigma associated with COVID-19.
2.1. Social Stigma Associated with COVID-19
While the term stigma has been used extensively and in various situations, settling for one encompassing definition is challenging. To be able to understand the relationship between stigma and COVID-19, it is important, first, to explore some elements of the former and why the latter carries such elements. In Conceptualizing Stigma, Link and Phelan identified 4 elements, such that stigma develops when (1) certain differences are highlighted, (2) these differences are looked upon negatively, (3) the different groups are set as an “us” group versus a “them” group, and (4) members of “them” group with the negative associations lose their status in society and are discriminated against [24]. One such difference, based on who experiences discrimination, is the presence versus absence of the disease. Thus, a health-related stigma has been associated with many disease conditions, whether infectious, such as HIV/AIDS, or non-infectious, such as epilepsy [25]. It is, therefore, no surprise that stigma could arise in outbreaks, such as SARS, MERS, or today with COVID-19.
Quarantine, defined as separating individuals possibly exposed to the virus from non-exposed [26], aids in highlighting the differences between these two individual groups, thus fulfilling the first element of stigma. So does isolation, which is the separation of those infected by the virus from those who are not [27]. This association between quarantine or isolation and stigma has been confirmed in several studies and outbreaks [20, 28-36]. The way media portrays news on an outbreak can also precipitate stigma by setting people apart, sensationalizing the negative attributes, and spreading fear. Such dramatization was reported in the SARS outbreak [31, 37] as well as COVID-19 [36]. For example, referral to the novel coronavirus as the “Chinese virus” by a group of people on social media, particularly world leaders and Twitter influencers, might help sustain the stigma against certain ethnicities in the light of the pandemic [38]. Furthermore, inconsistent governmental responses may further foster fear and negativity [17, 31]. That is, when a government portrays to the public a sense of uncertainty in its containment of an outbreak, it will cause even more uncertainty amongst the people, hence more fear and stigmatization. What sets COVID-19 apart from other outbreaks, however, and further increases the chance of stigmatization is its long incubation period with many individuals being asymptomatic carriers, and other individuals testing positive even after having tested negative more than once [36]. Therefore, people might still fear and avoid others even if they are asymptomatic or have been deemed to be “coronavirus survivors.”
2.2. Stigma Manifestations in Outbreaks
Manifestations of stigma in outbreaks are plenty. For example, in the 2003 SARS outbreak, stigmatization was noted in confirmed cases [39], quarantined individuals [29, 30], residents of an apartment complex with outbreak of cases [31], HCWs [28, 40-42], and individuals with Asian features [28, 37]. As a result, those stigmatized experienced rejection from their social circle and community as well as discriminatory treatment in their work environments [28-31, 39, 40]. In the 2014-2016 Ebola outbreak, survivors and family members were also rejected by their community, including their employers [32, 43]. One patient was even threatened to be harmed for “bringing” Ebola into his country [32]. In the 2015 MERS-CoV outbreak in a hospital in KSA, HCWs imposed stigma upon other HCWs who were in contact with confirmed cases [44]. This also applied to survivors, who were also socially excluded, as one describes feeling like “the dirtiest person in the world” [44].
Similarly, the above patterns of exclusion and rejection are seen in today’s COVID-19 pandemic [18, 45]. Cases of racist rejection against Chinese in many countries were reported, such as the UK, Germany, and France in virtue of these individuals’ origins [46]. This rejection even occurred online and within China itself, by discriminating against those from areas of an outbreak [46, 47]. Patients, contacts, and HCWs are being stigmatized as well [48]. One contact in Kuwait was asked to leave the apartment he lived in [49]. Another man in India was supposedly killed because he told on potential cases [50]. Several other incidents of assault were also reported against HCWs and police members to prevent them from collecting samples [51]. In addition to the populations mentioned previously, the Disease Control and Prevention (CDC) predicts that those who live in groups, have chronic cough, have difficulties in adhering to recommendations, and work on the frontlines (like clerks in grocery stores) might face stigma too [52].
Stigma persists even after the outbreak subsides [31, 39, 43], so does its impact. Ostracism (exclusion of others) was shown to diminish one’s self-regard and sense of belonging [53], and the effects are similar in different disease states [25]. In terms of public health, stigma may push individuals to hide their status, whether their exposure to the virus or their symptoms if present, and thus may contribute further to the spread of disease [16, 36, 39, 48, 54]. Out of fear of being stigmatized, people may also go as far as collecting antiviral drugs (such as Tamiflu) to self-medicate should symptoms appear, then “hide at home, and no one will know”, as happened in the Avian Influenza outbreak in 2005 [39]. Furthermore, several studies showed that health-related stigma is one of the factors that negatively affect mental health after outbreaks [13, 31, 33-35, 43, 48, 55-57]. Notably, increased stress among HCWs may reflect negatively on their work performance [48]. For these reasons, it is imperative to tackle stigma as early as possible, especially in the context of outbreaks. It is also important to be on the lookout for anticipated post-outbreak psychiatric conditions, such as PTSD. Different studies showed that stigma against people who carry COVID-19 is one of the factors that can contribute to PTSD, which can stay even after the confinement of the outbreak [58]. This stigmatization was very obvious in the SARS 2003 outbreak even after years of exposure [6].
Families of COVID-19 cases not only face the burden of stigma but also that of the trauma of having a loved one infected with the virus. The isolation associated with admitting the patient to the intensive care unit (ICU) may have negative effects on the mental health of family members, as manifested in symptoms of anxiety or depression [59]. It can also disrupt the family’s coping, as well as grief should the patient die [60, 61]. As a result, family members might develop what is known as complicated grief, which persists for more than 6 months and considerably impairs daily life functioning [62]. This may worsen or cause psychiatric problems, among which is PTSD [62, 63].
3. EFFECTS OF COVID-19 ON MENTAL AND PSYCHOLOGICAL HEALTH
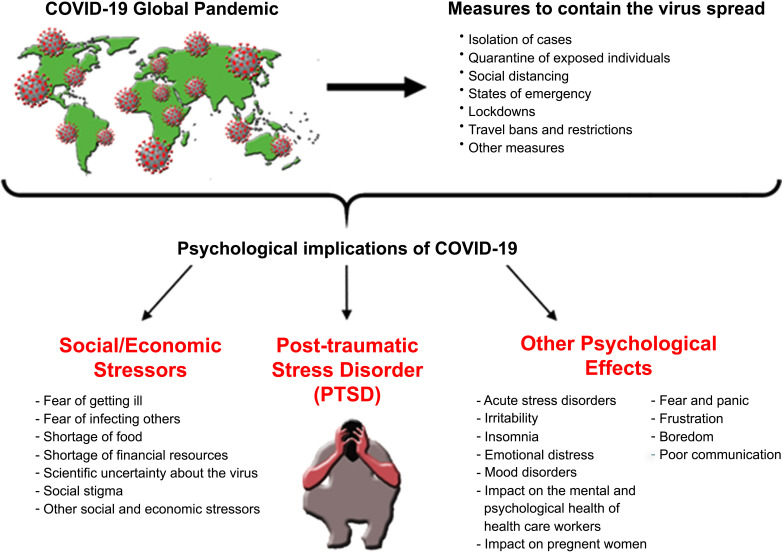
When a pandemic hits, people become intimidated by different threat factors, such as fear of getting ill or infecting others, shortage of food and financial resources, scientific uncertainty about the pandemic [64], social and economic stressors, in addition to the sense of anxiety and discomfort associated with quarantine and isolation [65] (Fig. 1).
Fig. (1).
Sketch summarizing measures to contain COVID-19 spread and its resulting psychological implications. (A higher resolution/colour version of this figure is available in the electronic copy of the article).
During such uncertain times, there is no clear foresight for the crisis and its possible trajectories. The pandemic has already generated ripples of change at every level and caused unprecedented chaos worldwide; this anticipated transformation was highlighted by the statement made by the WHO director-general Tedros Adhanom in his media briefing on COVID-19 on July 13, 2020, in which he said that there will be no return to the old normal for the foreseeable future [66].
While change can be beneficial at times, it can also have a deleterious effect on our mental health. Many studies have emphasized the wide psychological impact associated with outbreaks, including PTSD in individuals not suffering from mental illnesses, and the increased psychiatric symptoms seen in those with pre-existing mental illnesses. During the SARS outbreak, studies reported a rise in many psychological problems ranging from poor sleep, short sleep, anxiety, and depressive symptoms leading to PTSD [67, 68]. According to Hawryluck et al., the examination of 129 quarantined people during the SARS epidemic revealed a high prevalence of PTSD where 28.9% of them had symptoms similar to ones of extreme cases such as terrorist attacks or earthquakes [69]. Another study found that 44.1% of patients diagnosed with SARS developed PTSD over a 2 to 46 months period, after being discharged from the hospital [70]. This suggests that during an epidemic/pandemic, individuals become more susceptible to various degrees of psychological deterioration.
On the 21st of January 2020, when SARS-CoV-2 was announced to possess a human-to-human transmission, a widespread public panic occurred. China and other countries that were mostly infected back then declared a mass lockdown. Soon after, on March 11, 2020, COVID-19 was declared a global pandemic by WHO [3]. Similar to the SARS outbreak, COVID-19 is considered a major stressor capable of inducing acute stress disorders, irritability, insomnia, emotional distress, mood disorders, fear, panic, frustration, boredom, and poor communication [58]. Collectively, these factors may result in conditions that affect people’s mental health leading to PTSD [71]. Cumulative incidence of PTSD was reported to be 47.8% of the participants even 30 months after the SARS outbreak [1]. This gives insight about the probability of development of PTSD in individuals post COVID-19 experience.
Nonetheless, neurological complications have been reported in people who have recovered from COVID-19. A recent report indicates that people who had recovered may experience what is being referred to as “brain fog” due to PTSD. Such an impact has been reported in outbreaks of previous coronaviruses such as the SARS and MERS [72]. Symptoms include anxiety, headache, fatigue, depressive mood, loss of concentration, and in some cases sleep disorders such as insomnia [72]. One possible explanation is that systemic hyper-inflammation or a cytokine storm, induced by maladaptive innate immunity could impair neurovascular endothelial function, disrupt blood brain barrier (BBB), activate CNS innate immune signaling pathways, and induce para-infectious autoimmunity. All potentially contributing to the Central nervous system (CNS) complications associated with COVID-19 infection [73, 74]. Neurotropism is also a common characteristic of coronaviruses as it was evident in the cerebrospinal fluid and CNS of previous coronaviruses [75-78]. However, for COVID-19, whether there is an invasion to the brain and whether neurotropism is involved is still controversial and is yet to be identified [79]. Nonetheless, a heightened immune response has been linked to hippocampal atrophy and cognitive impairment and may underlie several manifestations in the brain. Therefore, significant psychological sequelae, such as PTSD, would be anticipated in COVID-19 survivors [80, 81].
3.1. Impact of Quarantine during the COVID-19 Pandemic
The practice of quarantine is not new and is usually imposed to control the spread of the disease. This term is different from that of isolation, which means separating people who have been diagnosed with a contagious disease from healthy ones. Yet, these two terms are used interchangeably [58]. The first official recognition of the word “Quarantine” was recorded in 1127 in Venice, Italy, and it was derived from quarantenaria meaning forty days period [82]. In the late sixteenth century, it was enforced in the United Kingdom during the Black Death pandemic [82, 83]. During a pandemic, the imposed mass quarantining can produce mass hysteria, anxiety, and panic [20]. People fear contracting the virus and associate every symptom with the disease; moreover, they fear infecting others and this leaves them with guilt and several psychological outcomes that may last for several months [6]. Among the general public, the fear of COVID-19 is now termed as “coronaphobia”.
Studies have shown that one of the main factors that induce stress during a pandemic is the duration of the quarantine, in which longer periods of quarantine lead to poorer mental health and consequently higher risk for PTSD [6]. In a sample of Toronto residents who were placed at home- or work-quarantine during the SARS epidemic, Hawryluck et al. found that 28.9% of the participants reported elevated PTSD symptomatology [69]. What worsens the quarantine side effects is the fact that many people lost their jobs and faced financial crises, which created serious socioeconomic distress and resulted in the inability to buy sufficient food supplies and accommodation for their families. This was found to be a risk factor for psychological disorders even at 4-6 months after the release of lockdown [58]. To sum it up, different studies showed that lower household income and longer quarantine duration were associated with higher PTSD symptomatology [69, 84].
3.2. COVID-19 Fake News and Misinformation
Although social media and news outlets play an important role during pandemics, misleading information and fake news manipulate our minds and threaten the public’s health. At a time of heightened stress, misinformation may lead to distress and greater uncertainty in vulnerable individuals, who are at a greater risk for developing PTSD [58]. Chatterjee and Chauhan studied the link between exposure to mass media information and the prevalence of PTSD. They showed that 33% of the studied sample from younger Tunisian population reported high prevalence of PTSD (r=1.41, p<0.01, n=603) [85]. In addition, Tang et al. investigated the prevalence of PTSD symptomology one month after the outbreak of COVID-19 among Chinese university students. All participants reported high levels of stress when exposed to mass media information [86]. Also, Garfin et al. showed that repeated media exposure during the outbreak was a major cause of mental health problems [87].
3.3. COVID-19 and Post-traumatic Stress Symptoms (PTSS)
In a recently published study, 6049 Chinese participants (including frontline HCWs, patients, close contact, and suspected patients) were recruited to assess the psychological impact of COVID-19 exposure on PTSD symptoms and emotional regulation [88]. The results obtained support the hypothesis that exposure to COVID-19 increases PTSD symptomology (80.9%) [88]. In fact, it has been reported that among the public in mainland China, the prevalence of post-traumatic stress symptoms (PTSS) was 4.6% only 1 month after the outbreak [8]. Another Chinese survey found that the prevalence of PTSD was 18.4% in participants who had greater exposure to COVID-19 [89]. One further study, conducted in China, indicated a high prevalence of PTSD among patients who were hospitalized due to Coronavirus, in which 96.2% of the patients met the cutoff score of probable PTSD [84]. Moreover, a study conducted on an Italian population showed a significant correlation between PTSD and COVID-19 (r=0.70, p<0.0001) [90]. In general, the Italian population has registered a considerably high percentage of PTSD (29.5%) [7]. Moreover, a study that aimed at investigating the prevalence and associated risk factors for psychological morbidities in confirmed COVID-19 patients found out that 43.9% of patients presented with impaired general mental health, 12.2% had PTSD symptoms, 26.8% had anxiety and/or depression symptoms and 53.6% had fatigue [91]. In Lebanon, a similar study investigating PTSD in times of COVID-19 was performed on 1067 quarantined Lebanese citizens in different Lebanese geographic areas. The questionnaire measured the prevalence of PTSD symptoms at 2 weeks and 4 weeks after quarantine. The response rate was 89.03% and showed that the symptoms of PTSD appear to be more prevalent during the fourth week of quarantining in comparison to the second week [92]. The participants were more distressed at week 4 (62.63%) in comparison to week 2 (33.2%). They were also feeling more distant (68.94%) at week 4 than week 2 (43.36%). In summary, the results of this study showed that a noteworthy proportion of the participants have reported PTSD symptoms during quarantine [92].
3.4. PTSD Across Different Age Groups Amid COVID-19 Pandemic
During the current COVID-19 pandemic, the complete lockdown of schools, playgrounds, and parks caused a disruption in children’s usual lifestyle and prevented some children from meeting their developmental milestones. Despite their reduced susceptibility to COVID-19 infection, children’s coping with lifestyle modifications can be stressful and challenging. Stress can manifest itself through changes in their behavior, which include complaining, agitation, withdrawal from regular activities, crying, and irregular sleep-wake pattern. These changes will inevitably affect their health and lead to serious outcomes [93, 94]. Children who were infected or suspected to be infected with COVID-19 are more likely to experience different, more difficult adverse psychological effects than those who were quarantined with their parents or relatives. The former had to be quarantined in hospitals and under special care. Some kids, on the other hand, lost a parent or a relative due to COVID-19. Studies about psychological impact during COVID-19 reported restlessness, irritability, anxiety, and distraction among children [95]. In previous pandemics, it has been reported that children who were quarantined were more likely to develop grief along with acute stress disorder and adjustment disorder. Also, 30% of children who were quarantined met the clinical criteria for PTSD diagnosis [93]. Another impactful stressor for both children and adolescents is the sudden shift to online education, which has deprived them of peer interactions and put parents under pressure to help with their kids’ teaching.
For adolescents, the impact of quarantine came as a deprivation of outdoor leisure activities and social gatherings. Furthermore, to some children and teenagers, home quarantine could mean being more exposed to domestic violence. During COVID-19, reports were emerging from all over the world about a significant increase in domestic violence [96-98]. Such exposure significantly affects the mental health of children and adolescents and can have long-term psychological consequences. A large-scale nationwide survey of psychological distress during the COVID-19 pandemic reported that 35% of 52,730 respondents experienced psychological distress and the highest scores of Peritraumatic Distress Index (PDI) were obtained among the young adults group [99]. It is suggested that the high PDI among young adults correlates with higher levels of education and self-awareness and most importantly continuous exposure to news from all social media platforms that can be quick to trigger distress and anxiety [100, 101].
The elderly are particularly highly influenced during quarantine times, especially those suffering from comorbidities. They are more susceptible to infection with COVID-19; therefore, their fear rates are much higher [102]. Moreover, they are the most vulnerable social group in this pandemic. Due to their weakened immune response, they are at higher risk for contacting COVID-19 and developing more severe symptoms than younger age groups. So far, the highest death rates of COVID-19 recorded were among the elderly population. More than 50% of all COVID-19 deaths were people above the age of 80. The CDC has reported that 8 out of 10 deaths in the U.S. have been in adults 65 years or older. The risk of severe illness and symptoms increases with age and ultimately leads to hospitalization and intensive care. This adds up to the psychological stress and fear that the elderly age group is already experiencing.
3.5. PTSD among People with Pre-existing Psychiatric Disorders during the COVID-19 Pandemic
The strict domestic quarantine policies implemented in most countries that had COVID-19 outbreak threatened the psychological well-being of the entire population in those countries. However, a particularly sensitive population already suffers from mental illnesses and hence is at a greater risk of developing serious adverse effects during the pandemic and its ongoing consequences. There is sparse research on mental health disorders in previous cases of pandemics. During times of stress, isolation, and fear, such as that experienced during the COVID-19 outbreak, it is very likely that mental health issues and symptoms of psychiatric illness would be exacerbated. Quarantine can lead to all sorts of feelings from fear, anxiety, loneliness, anger, and boredom to panic from further worse outcomes of the pandemic. Such feelings can be detrimental in people with previous psychiatric disorders as they can surface in a more overwhelming severe pattern and can sometimes exceed rational thinking leading to PTSD or suicidal thoughts [103, 104].
For people with recurrent depressive disorder, quarantine is considered a major stress factor that jeopardizes their normal daily routine and thereby increases their body stress levels and cortisol levels, leading to a vicious cycle of further exacerbation of depressive symptoms [105]. Young people with autism spectrum disorder (ASD) are also at risk of developing psychological distress during the lockdown as they are most vulnerable to unpredicted or sudden or complex changes. Online parental surveys reported that ASD children presented more intense and frequent disruptive behavioral changes with more difficulties in managing daily activities [106]. In addition, obsessive-compulsive disorder (OCD) patients are expected to suffer the most because of the advice and recommendations on improving personal hygiene that has been shown to exacerbate contamination obsession and washing compulsions [99, 107]. A study that was performed on OCD patients that had completed their therapeutic path for OCD before quarantine showed that 6 weeks after quarantining, these patients had remission and a significant increase in obsession and compulsive behavior [107]. Moreover, for patients with bipolar disorder or schizophrenia, there is the fear of relapses in case of jeopardy to the availability of their medication or their medication compliance. All this emphasizes the importance of developing alternative strategies such as online consultation and digital tools for psychiatric support management in periods of social distancing and quarantine.
3.6. Psychological Impact of COVID-19 on Pregnant Women
Another vulnerable population during the corona outbreak is pregnant women who are at higher risks for more severe illness from respiratory infections [108, 109]. Almost 85% of pregnant women will experience only mild symptoms and the most common reported symptoms for pregnant women are fever, cough, shortness of breath, and diarrhea [110-112]. Psychological distress is common among pregnant women since even daily stressors would usually cause them more anxiety. During major stressors, such as economic crises, natural disasters, wars, or pandemics, pregnant women would exhibit an upsurge of anxiety and depressive symptoms. Depressive and anxiety symptoms include high psychological distress, high negative affectivity, and low positive affectivity, in addition to symptoms of dissociation and PTSD. The current coronavirus outbreak had major psychological repercussions on maternal mental health [113]. This was evident during the COVID-19 pandemic, where pregnant women that were assessed post-pandemic announcement had significantly higher rates of depressive symptoms when compared to pregnant women who were assessed before the pandemic [114]. The depressive rates and symptoms were positively correlated with the number of cases and deaths announced per day. Moreover, pregnant women who were full-time employed with middle income were more likely to exhibit depressive symptoms and anxiety during the outbreak [114, 115]. Moreover, it should be noted that maternal prenatal psychological distress can have drastic effects on fetal brain growth, metabolism, and cortical maturation [116]. Early data suggested that pregnancy and childbirth do not increase the risk of acquiring COVID-19 infection and do not worsen the clinical outcome compared to individuals of the same age [117-121]. However, the US Centers for Disease Control and Prevention (CDC) has most recently stated that pregnant women might be at an increased risk for severe illness from COVID-19 compared to non-pregnant women [122]. This discrepancy in data, in addition to the sparse and delayed knowledge of whether the virus would be transmitted to the fetus or whether it would have detrimental effects on both the mother and the fetus, intensifies “coronaphobia” during pregnancy. So far, the intrauterine transmission of COVID-19 is still ambiguous with many questions remaining unanswered [123].
3.7. Impact of COVID-19 on the Mental and Psychological Health of Health Care Workers
Outbreaks due to microbiological agents have been known to instigate substantial psychological effects not only on the public but also on HCWs, especially the ones who are at the first line of defense. COVID-19 pandemic came as a challenge to healthcare systems which were underprepared causing substantial acute stress in the healthcare workplace and sustaining the baseline stress levels and epidemic physician burnout [124]. Studies during and after previous pandemics of viruses, like SARS and MERS, revealed high levels of depression, moral injury, anxiety, and PTSD among HCWs [125-128]. Multiple factors could trigger anxiety related to the pandemic including increasing workload, worries about access to PPEs, fear of contracting the virus and transmitting it to family or colleagues, concerns about caring for one’s children and family, and the uncertainty with changing protocols and lack of access to up-to-date data [129]. This increased acute stress on top of the baseline burnout rates in HCWs may drive more burnout and result in amplified rates of PTSD among doctors [130].
A study was conducted at the peak of the COVID-19 pandemic in Italy to evaluate burnout and physical symptoms among frontline Italian health care professionals [131]. The results showed that a high proportion of participants sustained high scores on at least one of the Maslach Burnout Inventory (MBI); more than 1 out of 3 scored high in emotional exhaustion, 1 out of 4 had elevated levels of depersonalization, but only around 15% described low levels of personal gratification. Almost half of the participants (45%) reported a minimum of one physical symptom in the previous 4 weeks including: elevated irritability, alteration in eating habits, difficulty sleeping, and muscle tension, with higher intensities of burnout associated with increased frequency of these symptoms. Females and nurses experienced more physical symptoms than males and physicians, respectively. These somatic symptoms and psychological pressures faced by HCWs demand attention, as previous studies show that emotional distress could have a massive effect on the health care professionals’ long-term health, PTSD being one of them [124].
A multinational, multicenter study conducted on HCWs in 5 major hospitals in Singapore and India showed that among the physical symptoms reported by HCWs were headache (being the most prevalent), throat pain, anxiety, lethargy, and insomnia [132]. The presence of these physical symptoms was found to be significantly associated with psychological effects like anxiety, stress, depression, and PTSD. Previous studies also showed that burnout and PTSD tend to coexist in HCWs and they reported evidence suggesting that there is a significant positive correlation between burnout and medical error risk [124, 133]. Burnout in physicians also results in high suicide rates and substance abuse, in addition to healthcare infrastructure instability [124, 134]. This shed light on how critical it is to assess and promptly respond to such findings in HCWs.
In a study done by Sun et al. the prevalence of PTSD symptoms in HCWs combating COVID-19 was 4.4% [8]. This falls in line with results of research on the mental health of medical staff involved in the 2003 SARS outbreak which recorded 10% of the sample having high levels of PTSD symptoms [135]. It is important to note that the study by Sun et al. alludes to the severity of PTSS which could vary based on factors like gender, current location, reporting date, subjective sleep quality, and classification of the population [8]. Moreover, Song et al. conducted a study to evaluate the mental health of emergency department HCWs in China during the COVID-19 pandemic [136]. Having surveyed 14,825 doctors and nurses across 31 provinces of China, the prevalence of PTSD was found to be 9.1%. Nurses were at a higher risk of having PTSD than physicians which is consistent with a previous study conducted during the SARS outbreak on medical staff of emergency department which also indicated higher levels of distress in nurses compared to physicians [137]. Among the factors that showed an increased risk of PTSD were longer working hours, shorter work tenure, and lower levels of social support. Social support had the strongest association with PTSD where the widowed, divorced, or unmarried HCWs proved to be at an elevated risk of PTSD. This study also indicated that men are more likely to have PTSD than women which is inconsistent with a previous study by Lai et al. that showed symptoms of distress and anxiety to be more severe in women compared to men [138]. The difference in the timing of the studies was proposed as a possible explanation to these discrepancies. In a study conducted earlier, just 1 month after the outbreak of the pandemic, on a smaller sample of HCWs from different provinces of China, prevalence of PTSS was 3.8% and higher in females than in males [139]. Another study conducted in Italy on a total of 1,379 HCWs during COVID-19 pandemic revealed that 49.38% of respondents presented with PTSS [140]. This study also showed that being a frontline HCW, a general practitioner or a female, and having colleagues deceased, hospitalized or in quarantine were all associated with increased risk of PTSS.
Having inadequate PPEs has been reported as one of the critical sources of anxiety related to COVID-19 among HCWs [129]. These circumstances are outside the scope of the usual experiences in the workplace and thus could be instigators of anxiety, and later on PTSD [130]. A study that was conducted on military personnel, to assess the effect of perception of having no adequate protective equipment on mental health, showed that those with a perception of having insufficient protective equipment were more likely to present with symptoms of common mental disorders, PTSD, and poorer mental health [141]. Drawing parallels with HCWs whose needs for PPEs are essential for their safety during fulfilling their roles, the perception of scarcity of PPEs could also be associated with higher risks of PTSD and mental health deterioration. To mitigate against the progression of PTSS into PTSD and the possible chronic psychological ramifications consequent to the COVID-19 outbreak, psychological interventions appear to be imperative to optimize recovery [7].
4. THERAPEUTIC APPROACHES TO MANAGE PTSD AND MENTAL HEALTH EFFECTS IN THE COVID-19 ERA:
In the COVID-19 era, PTSD is one of the consequences of the pandemic crisis. People with pre-existing mental and physical health conditions such as depression, substance use, and many more are at a higher risk of developing PTSD. Following a traumatic event, PTSD patients can easily relive the disturbing scenarios by-way-of nightmares and flashbacks, leading to discomfort, sadness, anger, or fear. In certain cases, they avoid situations, places, or people that remind them of the traumatic event they once witnessed or experienced, to escape the reliving of painful memories. Moreover, they may develop negative strong reactions to a normal regular loud noise, accidental touch, or any situation that was normally perceived in the past by the person. Concerning SARS survivors, 10 to 35% developed features of anxiety, depression, or both simultaneously, one month after being discharged [69, 142]. A study done in China has also shown that 10.8% of 673 workers returning back to work during the severe global threat (COVID-19) met the diagnosis of PTSD [143].
Before delving deep into the treatment strategies used for PTSD, it is crucial to note that many patients will have their symptoms reduced progressively or disappearing over time, especially with the support of family members and friends. However, it is highly important to consider the serious effect of the psychological distress that can disable someone’s daily life; hence, professional treatment is highly recommended.
4.1. Cognitive Processing Therapy (CPT) for PTSD via Telehealth
Cognitive-behavioral therapies (CBT) are significantly important for the treatment of PTSD, knowing that they target the correlation between thoughts, feelings, and behaviors, and focus on changing patterns of behaviors, feelings, and thoughts that were once leading to difficulties in the day-to-day functioning of the patient. Among the various types of CBT, cognitive processing therapy (CPT) is a trauma-focused and evidence-based treatment that aims to modify negative emotions and beliefs that cause pain to the patient; in other words, confronting distressing memories and emotions, and reducing symptoms of PTSD after experiencing or witnessing traumatic events. This treatment is usually delivered over 12 sessions, individually or in a group, so the patient can create a new conceptualization and understanding of her or his traumatic event, thus reducing its negative effect on daily activity. Treatment starts with psychoeducation about PTSD, emotions, and thoughts to a stage where the patient can identify and define automatic thoughts that are maintaining PTSD symptoms. Once the patient has developed skills to identify and modify unhelpful thoughts, she or he will continue to do so with other traumatic events outside of the current treatment, improving their quality of life and day-to-day functioning [144-146]. Consequently, CPT remains an efficacious and adequate treatment for PTSD in various populations around the world.
Telebehavioral therapy or telehealth is an adequate method of delivering psychotherapy for people who cannot reach therapists physically such as populations residing in rural areas or even individuals practicing social distancing and self-quarantine during the current COVID-19 pandemic [147]. Telehealth uses communication technologies such as telephone and video conferencing in order to deliver behavioral health services [148]. As already known, SARS-CoV-2 was rapidly sweeping around the world. Vulnerable people and patients with preexisting mental health conditions sought psychotherapy for treatment, especially people with PTSD. Accordingly, several modifications were crucial to meet the needs of these individuals and deliver professional services; thus, guidelines have been set by the American Psychological Association regarding the practice of telehealth [149]. Interestingly, several studies showed that CPT, when delivered via telehealth, is efficacious: PTSD symptoms were significantly reduced in populations receiving telehealth treatment at rates that were comparable to in-person therapy [150, 151]. However, not all kinds of therapy can be delivered by-way-of telephone or videoconferencing.
4.2. Hypnotic Therapy for PTSD and COVID-19
The mind is divided into a conscious mental status that relies on analyzing, judging, and thinking rationally, and a subconscious mental status that is mainly a reservoir of senses, feelings, thoughts, and memories. In many cases, the brain might bury the traumatic experiences from consciousness, as a protective mechanism. Inadvertent stimuli linked to those experiences can trigger acute flashbacks, which are one of the main characteristics of PTSD. Ultimately, the identification of these stimuli may help PTSD patients in coping better and in healing. Here comes the importance of hypnosis therapy, which tries to tackle these triggers and lead to the healing of patients [152]. Hypnosis induces increased relaxation and high-focus states of mind needed for patients to reach a higher capacity of responsiveness to suggestions [153]. During sessions, the patient is in a deep state of relaxation, she or he is hyper-focused and concentrated, with increased suggestibility, awareness, consciousness, and actively participating in the session, especially when remembering and accessing memories. With the control of the therapist, this therapeutic technique tends to recover the patient’s repressed memories and aims at coupling dissociated memories from a traumatic event with their positive restructuring. The patient can thereby place the traumatic event in a different context and into a broader perspective. Hypnosis is not considered as a therapy per se, it is an adjunct to psychodynamic therapy, cognitive behavioral therapy, and others [154]. Still, it is considered efficacious in many clinical conditions, such as PTSD, by making the patient change her or his habits. Of course, some patients might resist the use of this technique because of mistaken preconceptions or any other reasons.
4.3. Other Treatment Approaches for PTSD and COVID-19
4.3.1. Prolonged Exposure (PE) Therapy
Among several types of CBT, prolonged exposure (PE) therapy is a fifteen-session protocol that aims at teaching individuals to approach their trauma-related feelings, situations, and memories instead of avoiding them [155]. After understanding the patient’s past experiences, the therapist makes the adequate assessment and starts the exposure process, which is considered as an anxiety-provoking point for the patient. Imaginal and in-vivo exposures are taken into account [156]. In imaginal exposure sessions, the patient describes her or his traumatic event in detail while it is being recorded [157]. The patient then listens to the recordings and adopts a breathing technique for relaxation. Concerning in-vivo exposure, the therapist and the patient identify a list of stimuli that are connected to the traumatic event itself.
4.3.2. Stress inoculation Therapy (SIT)
The big difference between PE therapy, CPT, and stress inoculation therapy (SIT) is that SIT is not a trauma-focused therapy [158]. A study comparing PE and SIT showed that both reduced the symptoms of PTSD in female assault victims. SIT aims to let the patient have a structured exposure to a stressor and help building tolerance that puts the person in a protected zone against any other stressors or psychological illnesses. It focuses on helping patients cope with stressful life events. The therapy mainly focuses on the education of relaxation methods, cognitive practices, problem-solving, behavior practices, and cognitive-behavioral methods. This helps the individual change her or his attitude towards stressful events and use positive self-talk as a stress coping method [159, 160].
4.3.3. Group Therapy
In group therapy, people share similar traumatic experiences, in a safe and supportive environment where their beliefs, emotions, and thoughts are not judged or criticized. It is an effective therapeutic method for treating many psychological problems, including anxiety, panic attacks, and depression. It aims to normalize trauma responses and reduce the feeling of shame, guilt, and stigma. Group members feel safe to express their emotions by listening to others with a similar predicament. Group psychotherapy is sometimes more beneficial than an individual approach, knowing that it offers interpersonal feedback, mutual support between group members, and altruism [161]. In some cases, family therapy might also be very helpful [162].
4.3.4. Eye Movement Desensitization and Reprocessing (EMDR)
Eye movement desensitization and reprocessing (EMDR) is a psychotherapy treatment used to alleviate trauma-associated distress. This type of therapy tries to access and process traumatic memories to reach an adaptive resolution and help in reducing negative emotions linked to the traumatic memory [163]. It uses the patient’s saccadic eye movement to weaken the effect of disturbing memories of past traumatic events. Sessions are delivered once or twice a week, for a total number of 6 to 12 sessions. Unlike other therapies, EMDR aims to modify the way the traumatic memory is stored in the human brain and reduce negative feelings without revealing the details of the traumatic experience [164].
4.3.5. Relaxation Techniques
Relaxation is a therapeutic technique that works on reducing tension. Sessions result in a reduction of tension in the musculature leading to physical and psychological relaxation, which helps in the treatment of the patient [165]. Relaxation increases the activity of the limbic system to enhance emotional regulation. As already known, stress has physiological manifestations, such as muscle tension and tachycardia, which are reduced by relaxation techniques. This leads to the development of new coping skills to help the patient better manage her or his symptoms [166]. Furthermore, patients who are resistant to exposure-based therapies or medication can benefit from relaxation therapy to reduce their stress as well as the physiological manifestations of PTSD and to enhance their emotional regulation [167]. When facing a stress response, the human body aims to increase energy sources and prevent body functions, judged as unnecessary, in order to address the threat. Therefore, the body reacts with an increased heart rate, blood pressure, and glucose levels, whereas digestion, reproduction, and immune responses are inhibited. Relaxation techniques tend to work on a network of mediators including sympathetic, neuroendocrine, and behavioral factors to maintain physiological homeostasis and to ultimately result in stress reduction [166]. Moreover, relaxation techniques might be considered as a gateway for patients with PTSD who are not able to participate in evidence-based treatments, where relaxation sessions help in decreasing hypervigilance and increasing focus and attention [168]. Yoga and meditation are very helpful and powerful relaxation tools for both the body and the mind and could be potential adjunctive treatments for COVID-19 [169, 170]. Yoga has been described by the WHO as a valuable tool that increases physical activity, mental wellbeing, and decreases non-communicable diseases. In addition, it has been shown to have anti-inflammatory effects that could further help COVID-19 patients [170]. All in all, relaxation techniques have a crucial role in reducing the damage caused by the body's stress hormones and should be considered as an important treatment for many clinical cases.
4.3.6. Pharmacological Interventions
Medications play a crucial role in the management of PTSD-related symptoms and help patients participate more effectively in psychotherapy sessions. The most effective antidepressants used to treat PTSD are selective serotonin reuptake inhibitors (SSRIs) and selective norepinephrine reuptake inhibitors (SNRIs). Paroxetine and Sertraline are the only U.S. Food and Drug Administration (FDA)-approved medications to reduce PTSD symptoms [171]. Other alternative treatments such as acupuncture and animal-assisted interventions are being studied and might be recommended for PTSD [172].
5. EFFECT OF SOCIAL MEDIA, WORKING FROM HOME, AND HAVING VIRTUAL SOCIAL LIFE OVER THE INTERNET
Social media plays a crucial role in facilitating the delivery of information, and in this case, its use was inevitable for the transmission of health-related information to help in improving health outcomes [173]. Due to its powerful effect, however, social media was also used as a platform for misinformation, conspiracy theories, disinformation, and rumors [174]. This ended up in an infodemic phenomenon during the pandemic, where excessive amount of information spread fast and created more confusion and distrust in people. Fortunately, some platforms removed many contents that were falsified, and Google took the initiative to create an SOS Alert that made the WHO resources more accessible to people when searching for ‘Coronavirus’ or ‘COVID-19’. Ultimately, people were encouraged to seek out information from reliable sources and not from user-generated sources that contain misinformation.
During the last decade, communication and interaction between people witnessed an obvious advancement especially with the rapid development of social media platforms. In parallel, telecommuting – known as teleworking – is when employees have no personal contact with co-workers, but still can communicate with them via new technology such as social media and emails. To protect workers during the spread of the COVID-19 pandemic, teleworking was highly adopted. However, there are several advantages and disadvantages to it. Some of the advantages of working from home are that employees tend to spend less time away from their families, reduce their commute from and to work, and gives more flexibility in working hours. Although telecommuting is considered to have plenty of benefits, it also has disadvantages as well, starting with social isolation. This might put people at risk of facing psychological stress and eventually suffer from PTSS or even develop PTSD. Presenteeism is another problem caused by teleworking, where people are not able to take time off work even when they are sick. In addition, working from home tends to cause an increased work-family role conflict. Although teleworking might reduce stress, it can lead to over-work as well, an overlap between home and work. Having a social life on the Internet has a prominent role in deindividuating the person who will likely develop a self-centered behavior instead of having a regulated social behavior with an impoverished social interaction. Not to forget that people with stigmatized identities prefer to participate in virtual groups on the Internet as anonymous rather than joining these groups in real life.
CONCLUSION AND FUTURE DIRECTIONS
While the world recovers from COVID-19, it will awaken to the long-term damage and several consequences it left behind just like the aftermath of a war. The COVID-19 pandemic has so far been extending across the globe for the last 6 months. Over 1.9 million people have lost their lives to the virus and many families were scattered and left shattered as they had to bury their loved ones in mass graves with simple or no funerals. The global healthcare system faces a great deal of challenges with COVID-19 management, control, and treatment. In addition to the fear of the coronavirus, people were left in frustration as no hopes for vaccination were expected soon. Whether it’s the mandate quarantine or complete country lockdowns or the scenes of mass graves or world economy crashing, it has all left people all over the world with feelings of hopelessness, frustration, and a higher risk of developing mood disorders and mental health issues. A pandemic may leave behind more significant and long-lasting damage to mental health than to the economy. This has been evident in the increase in cases of PTSD where several studies conducted during the pandemic have reported high numbers of people diagnosed with acute trauma or PTSD.
Medical health workers at the frontline to combat the ongoing surge of the virus are one of the most who recorded high levels of stress and anxiety. In addition, adolescents, pregnant women, people with mental illness, and children who contracted the virus or lost a parent were among the most sensitive to psychological distress and trauma. The general population all suffered to a certain extent from psychological trauma from the pandemic’s consequences or the implemented quarantines. Amidst the pandemic, the only known solution that helped contain the virus was quarantine. Depending on the severity of the pandemic in different countries, people were quarantined for periods not less than 2 months. The long period of quarantine is bound to leave psychological distress on people of all ages for several reasons such as loss of jobs and economic crisis, loss of loved ones, continuous exposure to social media or fake news, fear of death, transfer to online education, domestic violence, fear and anxiety from contacting the virus. All of the aforementioned are social stressors that trigger depression or anxiety in previously healthy people and further add psychological burden to the mentally ill.
All of this suggests that more attention needs to be paid to vulnerable groups, chief among them are children, adolescents, pregnant women, medical staff workers, and elderly people. Existing public health services need to be re-assessed and reformed to provide such groups with the best treatment and care and help them cope with the crisis. This should be done in coordination with psychological health experts, by using implementation strategies tailored to their needs. In China, mental health crisis interventions, such as online education, awareness, and counseling services were implemented nationwide. Interestingly, artificial intelligence programs can also be put in use as interventions for mental health surveillance during the pandemic such as the Tree Holes Rescue program that has been used in China to recognize individuals at high risk of suicide. In Italy, due to quarantine, several psychologists and psychotherapists switched to digital devices to offer their services via either telephone, teleconference, websites, and others. Such actions and medical interventions need to be implemented worldwide and be accessible by people of all economic statuses to help minimize psychological distress and the surge in cases of PTSD among the population. The need for such applications and new measures are crucial as the virus continues to spread in many countries and the threat of a second wave is foreseeable while the promise of an effective vaccine has yet to be delivered.
ACKNOWLEDGEMENTS
Declared none.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest. The research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
REFERENCES
- 1.Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31(4):318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization 2020.
- 3.World Health Organization Archived https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19
- 4.World Health Organization Coronavirus disease (COVID-19). Situation Report. 2020;178:2020. [Google Scholar]
- 5.https://covid19.who.int/
- 6.Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S., Lahiri D., Lavie C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. 2020;14(5):779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forte G., Favieri F., Tambelli R., Casagrande M. The Enemy Which Sealed the World: Effects of COVID-19 Diffusion on the Psychological State of the Italian Population. J. Clin. Med. 2020;9(6):E1802. doi: 10.3390/jcm9061802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun L., Sun Z., Wu L., Zhu Z., Zhang F., Shang Z., Jia Y., Gu J., Zhou Y., Wang Y., Liu N., Liu W. Prevalence and Risk Factors of Acute Posttraumatic Stress Symptoms during the COVID-19 Outbreak in Wuhan, China. MedRxiv. 2020:2020.03.06.20032425
- 9.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R. C Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health. 2020;17(5):E1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blackman J.S. A psychoanalytic view of reactions to the coronavirus pandemic in China. Am. J. Psychoanal. 2020;80(2):119–132. doi: 10.1057/s11231-020-09248-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahmed H., Patel K., Greenwood D.C., Halpin S., Lewthwaite P., Salawu A., Eyre L., Breen A., O’Connor R., Jones A., Sivan M. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: A systematic review and meta-analysis. J. Rehabil. Med. 2020;52(5):jrm00063. doi: 10.2340/16501977-2694. [DOI] [PubMed] [Google Scholar]
- 13.Lam M.H-B., Wing Y-K., Yu M.W-M., Leung C-M., Ma R.C.W., Kong A.P.S., So W.Y., Fong S.Y-Y., Lam S-P. Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Arch. Intern. Med. 2009;169(22):2142–2147. doi: 10.1001/archinternmed.2009.384. [DOI] [PubMed] [Google Scholar]
- 14.Tansey C.M., Louie M., Loeb M., Gold W.L., Muller M.P., de Jager J., Cameron J.I., Tomlinson G., Mazzulli T., Walmsley S.L., Rachlis A.R., Mederski B.D., Silverman M., Shainhouse Z., Ephtimios I.E., Avendano M., Downey J., Styra R., Yamamura D., Gerson M., Stanbrook M.B., Marras T.K., Phillips E.J., Zamel N., Richardson S.E., Slutsky A.S., Herridge M.S. One-year outcomes and health care utilization in survivors of severe acute respiratory syndrome. Arch. Intern. Med. 2007;167(12):1312–1320. doi: 10.1001/archinte.167.12.1312. [DOI] [PubMed] [Google Scholar]
- 15.https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd
- 16.Bruns D.P., Kraguljac N.V., Bruns T.R. COVID-19: Facts, cultural considerations, and risk of stigmatization. J. Transcult. Nurs. 2020;31(4):326–332. doi: 10.1177/1043659620917724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dong L., Bouey J. Public Mental Health Crisis during COVID-19 Pandemic, China. Emerg. Infect. Dis. 2020;26(7):1616–1618. doi: 10.3201/eid2607.200407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Passavanti M. The psychological impact of COVID-19 and restrictive measures in the world. J. Affect. Disord. 2021;283:36–51. doi: 10.1016/j.jad.2021.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fofana N.K., Latif F., Sarfraz S. Bilal; Bashir, M.F.; Komal, B. Fear and agony of the pandemic leading to stress and mental illness: An emerging crisis in the novel coronavirus (COVID-19) outbreak. Psychiatry Res. 2020;291:113230. doi: 10.1016/j.psychres.2020.113230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rubin G.J., Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 21.Asmundson G.J.G., Taylor S. Coronaphobia: Fear and the 2019-nCoV outbreak. J. Anxiety Disord. 2020;70:102196–102196. doi: 10.1016/j.janxdis.2020.102196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goyal K., Chauhan P., Chhikara K., Gupta P., Singh M.P. Fear of COVID 2019: First suicidal case in India! Asian J. Psychiatr. 2020;49:101989–101989. doi: 10.1016/j.ajp.2020.101989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Montemurro N. The emotional impact of COVID-19: From medical staff to common people. Brain Behav. Immun. 2020;87:23–24. doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Link B.G., Phelan J.C. Conceptualizing stigma. Annu. Rev. Sociol. 2001;27(1):363–385. doi: 10.1146/annurev.soc.27.1.363. [DOI] [Google Scholar]
- 25.Van Brakel W.H. Measuring health-related stigma--a literature review. Psychol. Health Med. 2006;11(3):307–334. doi: 10.1080/13548500600595160. [DOI] [PubMed] [Google Scholar]
- 26.https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/quarantine.html
- 27.https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/isolation.html
- 28.Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M., Sadavoy J., Verhaeghe L.M., Steinberg R., Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10):1245–1251. [PMC free article] [PubMed] [Google Scholar]
- 29.Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). J. Trauma. Stress. 2005;18(1):39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cava M.A., Fay K.E., Beanlands H.J., McCay E.A., Wignall R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs. 2005;22(5):398–406. doi: 10.1111/j.0737-1209.2005.220504.x. [DOI] [PubMed] [Google Scholar]
- 31.Lee S., Chan L.Y.Y., Chau A.M.Y., Kwok K.P.S., Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Soc. Sci. Med. 2005;61(9):2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Desclaux A., Badji D., Ndione A.G., Sow K. Accepted monitoring or endured quarantine? Ebola contacts’ perceptions in Senegal. Soc. Sci. Med. 2017;178:38–45. doi: 10.1016/j.socscimed.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 33.Gammon J., Hunt J., Musselwhite C. The stigmatisation of source isolation: A literature review. J. Res. Nurs. 2019;24(8):677–693. doi: 10.1177/1744987119845031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020;113(8):531–537. doi: 10.1093/qjmed/hcaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hossain M.M., Sultana A., Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: A systematic umbrella review of the global evidence. Epidemiol. Health. 2020;42:e2020038. doi: 10.4178/epih.e2020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li W., Yang Y., Ng C.H., Zhang L., Zhang Q., Cheung T., Xiang Y-T. Global imperative to combat stigma associated with the coronavirus disease 2019 pandemic. Psychol. Med. 2020;1-2 doi: 10.1017/S0033291720001993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Person B., Sy F., Holton K., Govert B., Liang A., Garza B., Gould D., Hickson M., McDonald M., Meijer C., Smith J., Veto L., Williams W., Zauderer L., Team S.C.O. Fear and stigma: the epidemic within the SARS outbreak. Emerg. Infect. Dis. 2004;10(2):358–363. doi: 10.3201/eid1002.030750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Budhwani H., Sun R. Creating COVID-19 Stigma by referencing the novel coronavirus as the “chinese virus” on twitter: quantitative analysis of social media data. J. Med. Internet Res. 2020;22(5):e19301. doi: 10.2196/19301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Siu J.Y. The SARS-associated stigma of SARS victims in the post-SARS era of Hong Kong. Qual. Health Res. 2008;18(6):729–738. doi: 10.1177/1049732308318372. [DOI] [PubMed] [Google Scholar]
- 40.Bai Y., Lin C-C., Lin C-Y., Chen J-Y., Chue C-M., Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004;55(9):1055–1057. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- 41.Mok E., Chung B.P.M., Chung J.W.Y., Wong T.K.S. An exploratory study of nurses suffering from severe acute respiratory syndrome (SARS). Int. J. Nurs. Pract. 2005;11(4):150–160. doi: 10.1111/j.1440-172X.2005.00520.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lin C.Y., Peng Y.C., Wu Y.H., Chang J., Chan C.H., Yang D.Y. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg. Med. J. 2007;24(1):12–17. doi: 10.1136/emj.2006.035089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matua G.A., Wal D.M. Living under the constant threat of ebola: a phenomenological study of survivors and family caregivers during an ebola outbreak. J. Nurs. Res. 2015;23(3):217–224. doi: 10.1097/jnr.0000000000000116. [DOI] [PubMed] [Google Scholar]
- 44.Almutairi A.F., Adlan A.A., Balkhy H.H., Abbas O.A., Clark A.M. “It feels like I’m the dirtiest person in the world.”: Exploring the experiences of healthcare providers who survived MERS-CoV in Saudi Arabia. J. Infect. Public Health. 2018;11(2):187–191. doi: 10.1016/j.jiph.2017.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.He J., He L., Zhou W., Nie X., He M. Discrimination and social exclusion in the Outbreak of COVID-19. Int. J. Environ. Res. Public Health. 2020;17(8):E2933. doi: 10.3390/ijerph17082933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jones D.S. History in a Crisis - Lessons for Covid-19. N. Engl. J. Med. 2020;382(18):1681–1683. doi: 10.1056/NEJMp2004361. [DOI] [PubMed] [Google Scholar]
- 47.Jakovljevic M., Bjedov S., Jaksic N., Jakovljevic I. COVID-19 pandemia and public and global mental health from the perspective of global health securit. Psychiatr. Danub. 2020;32(1):6–14. doi: 10.24869/psyd.2020.6. [DOI] [PubMed] [Google Scholar]
- 48.Shuja K.H., Aqeel M., Jaffar A., Ahmed A. COVID-19 pandemic and impending global mental health implications. Psychiatr. Danub. 2020;32(1):32–35. doi: 10.24869/psyd.2020.32. [DOI] [PubMed] [Google Scholar]
- 49.Ramaci T., Barattucci M., Ledda C., Rapisarda V. Social Stigma during COVID-19 and its Impact on HCWs Outcomes. Sustainability (Basel, Switzerland) 2020;12(9):3834. [Google Scholar]
- 50.Garcia B. Coronavirus 'stigma' follows people in Kuwait. 2020.
- 51.Bhatti O.A., Rauf H., Aziz N., Martins R.S., Khan J.A. Violence against Healthcare Workers during the COVID-19 pandemic: a review of incidents from a lower-middle-income country. Ann. Glob. Health. 2021;87(1):41. doi: 10.5334/aogh.3203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Centers for Disease Control and Prevention Reducing Stigma https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/reducing-stigma.html
- 54.Nezlek J.B., Wesselmann E.D., Wheeler L., Williams K.D. Ostracism in everyday life. Group Dyn. 2012;16(2):91–104. doi: 10.1037/a0028029. [DOI] [PubMed] [Google Scholar]
- 55.https://www.who.int/publications/m/item/a-guide-to-preventing-and-addressing-social-stigma-associated-with-covid-19?gclid=CjwKCAjwxqX4BRBhEiwAYtJX7RtGQLru-juK-UtTgAOMbUBbIsfILyTuKNBVv7bQGVPSb3nhuc94WRoCMLMQAvD_BwE
- 56.Fischer L.S., Mansergh G., Lynch J., Santibanez S. Addressing disease-related stigma during infectious disease outbreaks. Disaster Med. Public Health Prep. 2019;13(5-6):989–994. doi: 10.1017/dmp.2018.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Doppalapudi L., Lippmann S. Psychiatric Morbidities among COVID-19 Survivors. South. Med. J. 2020;113(9):466–467. doi: 10.14423/SMJ.0000000000001146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mak I.W., Chu C.M., Pan P.C., Yiu M.G., Ho S.C., Chan V.L. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen. Hosp. Psychiatry. 2010;32(6):590–598. doi: 10.1016/j.genhosppsych.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kotfis K., Williams R.S., Wilson J., Pun B., Ely E.W., Jeżowska I., Jezierska M., Dabrowski W. COVID-19: What do we need to know about ICU delirium during the SARS-CoV-2 pandemic? Anaesthesiol. Intensive Ther. 2020;52(2):132–138. doi: 10.5114/ait.2020.95164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Montauk T.R., Kuhl E.A. COVID-related family separation and trauma in the intensive care unit. Psychol. Trauma. 2020;12(S1):S96–S97. doi: 10.1037/tra0000839. [DOI] [PubMed] [Google Scholar]
- 62.Kentish-Barnes N., Cohen-Solal Z., Morin L., Souppart V., Pochard F., Azoulay E. lived experiences of family members of patients with severe COVID-19 Who Died in intensive care units in france. JAMA Netw. Open. 2021;4(6):e2113355–e2113355. doi: 10.1001/jamanetworkopen.2021.13355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kentish-Barnes N., Chaize M., Seegers V., Legriel S., Cariou A., Jaber S., Lefrant J-Y., Floccard B., Renault A., Vinatier I., Mathonnet A., Reuter D., Guisset O., Cohen-Solal Z., Cracco C., Seguin A., Durand-Gasselin J., Éon B., Thirion M., Rigaud J-P., Philippon-Jouve B., Argaud L., Chouquer R., Adda M., Dedrie C., Georges H., Lebas E., Rolin N., Bollaert P-E., Lecuyer L., Viquesnel G., Léone M., Chalumeau-Lemoine L., Garrouste M., Schlemmer B., Chevret S., Falissard B., Azoulay É. Complicated grief after death of a relative in the intensive care unit. Eur. Respir. J. 2015;45(5):1341–1352. doi: 10.1183/09031936.00160014. [DOI] [PubMed] [Google Scholar]
- 64.Kross E.K.M.D., Engelberg R.A.P., Gries C.J.M.D., Nielsen E.L.M.P.H., Zatzick D., Curtis J.R. ICU care associated with symptoms of depression and posttraumatic stress disorder among family members of patients who die in the ICU. Chest. 2011;139(4):795–801. doi: 10.1378/chest.10-0652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Han P.K.J., Zikmund-Fisher B.J., Duarte C.W., Knaus M., Black A., Scherer A.M., Fagerlin A. Communication of scientific uncertainty about a novel pandemic health threat: ambiguity aversion and its mechanisms. J. Health Commun. 2018;23(5):435–444. doi: 10.1080/10810730.2018.1461961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bonanno G.A., Ho S.M.Y., Chan J.C.K., Kwong R.S.Y., Cheung C.K.Y., Wong C.P.Y., Wong V.C.W. Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: A latent class approach. Health Psychol. 2008;27(5):659–667. doi: 10.1037/0278-6133.27.5.659. [DOI] [PubMed] [Google Scholar]
- 67. World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19 - 13 July 2020 . 2020.
- 68.Chen R., Chou K-R., Huang Y-J., Wang T-S., Liu S-Y., Ho L-Y. Effects of a SARS prevention programme in Taiwan on nursing staff’s anxiety, depression and sleep quality: A longitudinal survey. Int. J. Nurs. Stud. 2006;43(2):215–225. doi: 10.1016/j.ijnurstu.2005.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Johal S.S. Psychosocial impacts of quarantine during disease outbreaks and interventions that may help to relieve strain. N. Z. Med. J. 2009;122(1296):47–52. [PubMed] [Google Scholar]
- 70.Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hong X., Currier G.W., Zhao X., Jiang Y., Zhou W., Wei J. Posttraumatic stress disorder in convalescent severe acute respiratory syndrome patients: A 4-year follow-up study. Gen. Hosp. Psychiatry. 2009;31(6):546–554. doi: 10.1016/j.genhosppsych.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Perrin P.C., McCabe O.L., Everly G.S., Jr, Links J.M. Preparing for an influenza pandemic: mental health considerations. Prehosp. Disaster Med. 2009;24(3):223–230. doi: 10.1017/S1049023X00006853. [DOI] [PubMed] [Google Scholar]
- 73.Newman K.L. Shutt up: bubonic plague and quarantine in early modern England. J. Soc. Hist. 2012;45(3):809–834. doi: 10.1093/jsh/shr114. [DOI] [PubMed] [Google Scholar]
- 74.Rosen G. In: Discipline and Punish: The Birth of the Prison. Foucault M., editor. New York: Vintage; 1979. A History of Public Health. p. 198. [Google Scholar]
- 75.Boyraz G., Legros D.N. Coronavirus Disease (COVID-19) and traumatic stress: probable risk factors and correlates of posttraumatic stress disorder. J. Loss Trauma. 2020:1–20. doi: 10.1080/15325024.2020.1763556. [DOI] [Google Scholar]
- 76.Chatterjee K., Chauhan V.S. Epidemics, quarantine and mental health. Med. J. Armed Forces India. 2020;76(2):125–127. doi: 10.1016/j.mjafi.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Garfin D.R., Silver R.C., Holman E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychol. 2020;39(5):355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jiang H-j., Nan J., Lv Z-y., Yang J. Psychological impacts of the COVID-19 epidemic on Chinese people: Exposure, post-traumatic stress symptom, and emotion regulation. Asian Pac. J. Trop. Med. 2020;13(6):252–259. doi: 10.4103/1995-7645.281614. [DOI] [Google Scholar]
- 80.Sun Y., Shi L., Bao Y., Sun Y., Shi J., Lu L. The bidirectional relationship between sleep duration and depression in community-dwelling middle-aged and elderly individuals: evidence from a longitudinal study. Sleep Med. 2018;52:221–229. doi: 10.1016/j.sleep.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 81.Forte G., Favieri F., Tambelli R., Casagrande M. COVID-19 Pandemic in the Italian Population: Validation of a Post-Traumatic Stress Disorder Questionnaire and Prevalence of PTSD Symptomatology. Int. J. Environ. Res. Public Health. 2020;17(11):E4151. doi: 10.3390/ijerph17114151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Qi R., Chen W., Liu S., Thompson P.M., Zhang L.J., Xia F., Cheng F., Hong A., Surento W., Luo S., Sun Z.Y., Zhou C.S., Li L., Jiang X., Lu G.M. Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: prevalence and associated biopsychosocial risk factors. MedRxiv. :2020.05.08.20031666
- 83.Fawaz M., Samaha A. COVID-19 quarantine: Post-traumatic stress symptomatology among Lebanese citizens. Int. J. Soc. Psychiatry. 2020;66(7):666–674. doi: 10.1177/0020764020932207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.de Figueiredo C.S., Sandre P.C., Portugal L.C.L., Mázala-de-Oliveira T., da Silva Chagas L., Raony Í., Ferreira E.S., Giestal-de-Araujo E., Dos Santos A.A., Bomfim P.O. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2021;106:110171. doi: 10.1016/j.pnpbp.2020.110171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Imran N., Aamer I., Sharif M.I., Bodla Z.H., Naveed S. Psychological burden of quarantine in children and adolescents: A rapid systematic review and proposed solutions. Pak. J. Med. Sci. 2020;36(5):1106–1116. doi: 10.12669/pjms.36.5.3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Campbell A.M. An increasing risk of family violence during the Covid-19 pandemic: Strengthening community collaborations to save lives. Forensic Sci. Intl. Reports. 2020;2:100089. doi: 10.1016/j.fsir.2020.100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Boserup B., McKenney M., Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am. J. Emerg. Med. 2020;38(12):2753–2755. doi: 10.1016/j.ajem.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Usher K., Bhullar N., Durkin J., Gyamfi N., Jackson D. Family violence and COVID-19: Increased vulnerability and reduced options for support. Int. J. Ment. Health Nurs. 2020;29(4):549–552. doi: 10.1111/inm.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatr. 2020;33(2):e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Roberts T., Miguel Esponda G., Krupchanka D., Shidhaye R., Patel V., Rathod S. Factors associated with health service utilisation for common mental disorders: A systematic review. BMC Psychiatry. 2018;18(1):262. doi: 10.1186/s12888-018-1837-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cheng C., Huang J., Liang B. Psychological Health Diathesis Assessment System: A Nationwide Survey of Resilient Trait Scale for Chinese Adults. 2014.
- 93.Killgore W.D.S., Cloonan S.A., Taylor E.C., Allbright M.C., Dailey N.S. Trends in suicidal ideation over the first three months of COVID-19 lockdowns. Psychiatry Res. 2020;293:113390. doi: 10.1016/j.psychres.2020.113390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chatterjee S.S., Barikar C.M., Mukherjee A. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian J. Psychiatr. 2020;51:102071. doi: 10.1016/j.ajp.2020.102071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ran L., Hadar N., Jonathan D.H., Eyal K. Impact of COVID-19 on obsessive–compulsive disorder patients. Psychiatry Clin. Neurosci. 2020;74(12):660–661. doi: 10.1111/pcn.13152. [DOI] [PubMed] [Google Scholar]
- 96.Littman R., Naftalovich H., Huppert J.D., Kalanthroff E. Impact of COVID-19 on obsessive-compulsive disorder patients. Psychiatry Clin. Neurosci. 2020;74(12):660–661. doi: 10.1111/pcn.13152. [DOI] [PubMed] [Google Scholar]
- 97.Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and Behavioral Impact of COVID-19 in Autism Spectrum Disorder: An Online Parent Survey. Brain Sci. 2020;10(6):E341. doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Davide P., Andrea P., Martina O., Andrea E., Davide D., Mario A. The impact of the COVID-19 pandemic on patients with OCD: Effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Res. 2020;291:113213. doi: 10.1016/j.psychres.2020.113213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ramsey P.S., Ramin K.D. Pneumonia in pregnancy. Obstet. Gynecol. Clin. North Am. 2001;28(3):553–569. doi: 10.1016/S0889-8545(05)70217-5. [DOI] [PubMed] [Google Scholar]
- 100.Rasmussen S.A., Kissin D.M., Yeung L.F., MacFarlane K., Chu S.Y., Turcios-Ruiz R.M., Mitchell E.W., Williams J., Fry A.M., Hageman J., Uyeki T.M., Jamieson D.J. Preparing for influenza after 2009 H1N1: Special considerations for pregnant women and newborns. Am. J. Obstet. Gynecol. 2011;204(6) Suppl. 1:S13–S20. doi: 10.1016/j.ajog.2011.01.048. [DOI] [PubMed] [Google Scholar]
- 101.Dashraath P., Wong J.L.J., Lim M.X.K., Lim L.M., Li S., Biswas A., Choolani M., Mattar C., Su L.L. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am. J. Obstet. Gynecol. 2020;222(6):521–531. doi: 10.1016/j.ajog.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yu N., Li W., Kang Q., Xiong Z., Wang S., Lin X., Liu Y., Xiao J., Liu H., Deng D., Chen S., Zeng W., Feng L., Wu J. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: A retrospective, single-centre, descriptive study. Lancet Infect. Dis. 2020;20(5):559–564. doi: 10.1016/S1473-3099(20)30176-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ryan G.A., Purandare N.C., McAuliffe F.M., Hod M., Purandare C.N. Clinical update on COVID-19 in pregnancy: A review article. J. Obstet. Gynaecol. Res. 2020;46(8):1235–1245. doi: 10.1111/jog.14321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Thapa S.B., Mainali A., Schwank S.E., Acharya G. Maternal mental health in the time of the COVID-19 pandemic. Acta Obstet. Gynecol. Scand. 2020;99(7):817–818. doi: 10.1111/aogs.13894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wu Y., Zhang C., Liu H., Duan C., Li C., Fan J., Li H., Chen L., Xu H., Li X., Guo Y., Wang Y., Li X., Li J., Zhang T., You Y., Li H., Yang S., Tao X., Xu Y., Lao H., Wen M., Zhou Y., Wang J., Chen Y., Meng D., Zhai J., Ye Y., Zhong Q., Yang X., Zhang D., Zhang J., Wu X., Chen W., Dennis C.L., Huang H. Perinatal depressive and anxiety symptoms of pregnant women along with COVID-19 outbreak in China. Am. J. Obstet. Gynecol. 2020;223(2):240.e1–240.e9. doi: 10.1016/j.ajog.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Liu X., Chen M., Wang Y., Sun L., Zhang J., Shi Y., Wang J., Zhang H., Sun G., Baker P.N., Luo X., Qi H. Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID-19 outbreak: A cross-sectional study. BJOG. 2020;127(10):1229–1240. doi: 10.1111/1471-0528.16381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Breslin N., Baptiste C., Gyamfi-Bannerman C., Miller R., Martinez R., Bernstein K., Ring L., Landau R., Purisch S., Friedman A.M., Fuchs K., Sutton D., Andrikopoulou M., Rupley D., Sheen J.J., Aubey J., Zork N., Moroz L., Mourad M., Wapner R., Simpson L.L., D’Alton M.E., Goffman D. Coronavirus disease 2019 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am. J. Obstet. Gynecol. MFM. 2020;2(2):100118. doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Di Mascio D., Khalil A., Saccone G., Rizzo G., Buca D., Liberati M., Vecchiet J., Nappi L., Scambia G., Berghella V., D’Antonio F. Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. MFM. 2020;2(2):100107. doi: 10.1016/j.ajogmf.2020.100107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Schwartz D.A. An Analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of sars-cov-2: maternal coronavirus infections and pregnancy outcomes. Arch. Pathol. Lab. Med. 2020;144(7):799–805. doi: 10.5858/arpa.2020-0901-SA. [DOI] [PubMed] [Google Scholar]
- 110.Khan S., Jun L. Association of COVID-19 with pregnancy outcomes in health-care workers and general women. Clin. Microbiol. Infect. 2020;26(6):788–790. doi: 10.1016/j.cmi.2020.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Qiancheng X., Jian S., Lingling P., Lei H., Xiaogan J., Weihua L., Gang Y., Shirong L., Zhen W. Coronavirus disease 2019 in pregnancy. Int. J. Infect. Dis. 2020;95:376–383. doi: 10.1016/j.ijid.2020.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Ellington S., Strid P., Tong V.T., Woodworth K., Galang R.R., Zambrano L.D., Nahabedian J., Anderson K., Gilboa S.M. Characteristics of Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status - United States, January 22-June 7, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69(25):769–775. doi: 10.15585/mmwr.mm6925a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Shahbazi S.S., Ebrahimi Kalan M. Care of newborns born to mothers with COVID-19 infection; a review of existing evidence. J. Matern. Fetal Neonatal Med. 2020;23:1–13. doi: 10.1080/14767058.2020.1777969. [DOI] [PubMed] [Google Scholar]
- 114.Panagioti M., Geraghty K., Johnson J., Zhou A., Panagopoulou E., Chew-Graham C., Peters D., Hodkinson A., Riley R., Esmail A. Association between physician burnout and patient safety, professionalism, and patient satisfaction: A Systematic Review and Meta-analysis. JAMA Intern. Med. 2018;178(10):1317–1331. doi: 10.1001/jamainternmed.2018.3713. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 115.Koh D., Lim M.K., Chia S.E., Ko S.M., Qian F., Ng V., Tan B.H., Wong K.S., Chew W.M., Tang H.K., Ng W., Muttakin Z., Emmanuel S., Fong N.P., Koh G., Kwa C.T., Tan K.B., Fones C. Risk perception and impact of Severe Acute Respiratory Syndrome (SARS) on work and personal lives of healthcare workers in Singapore: what can we learn? Med. Care. 2005;43(7):676–682. doi: 10.1097/01.mlr.0000167181.36730.cc. [DOI] [PubMed] [Google Scholar]
- 116.Lancee W.J., Maunder R.G., Goldbloom D.S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 2008;59(1):91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tam C.W., Pang E.P., Lam L.C., Chiu H.F. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004;34(7):1197–1204. doi: 10.1017/S0033291704002247. [DOI] [PubMed] [Google Scholar]
- 119.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 Pandemic. JAMA. 2020;323(21):2133–2134. doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 120.Restauri N., Sheridan A.D. (COVID-19) Pandemic: intersection, impact, and interventions. J. Am. Coll. Radiol. 2020;17(7):921–926. doi: 10.1016/j.jacr.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Barello S., Palamenghi L., Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020;290:113129. doi: 10.1016/j.psychres.2020.113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., Yeo L.L.L., Ahmad A., Ahmed K.F., Napolean S.G., Sharma A.K., Komalkumar R.N., Meenakshi P.V., Shah K., Patel B., Chan B.P.L., Sunny S., Chandra B., Ong J.J.Y., Paliwal P.R., Wong L.Y.H., Sagayanathan R., Chen J.T., Ying Ng A.Y., Teoh H.L., Tsivgoulis G., Ho C.S., Ho R.C., Sharma V.K. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mealer M., Burnham E.L., Goode C.J., Rothbaum B., Moss M. The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depress. Anxiety. 2009;26(12):1118–1126. doi: 10.1002/da.20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chetlen A.L., Chan T.L., Ballard D.H., Frigini L.A., Hildebrand A., Kim S., Brian J.M., Krupinski E.A., Ganeshan D. Addressing burnout in radiologists. Acad. Radiol. 2019;26(4):526–533. doi: 10.1016/j.acra.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Song X., Fu W., Liu X., Luo Z., Wang R., Zhou N., Yan S., Lv C. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav. Immun. 2020;88:60–65. doi: 10.1016/j.bbi.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wong T.W., Yau J.K., Chan C.L., Kwong R.S., Ho S.M., Lau C.C., Lau F.L., Lit C.H. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur. J. Emerg. Med. 2005;12(1):13–18. doi: 10.1097/00063110-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 128.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yin Q., Sun Z., Liu T., Ni X., Deng X., Jia Y., Shang Z., Zhou Y., Liu W. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin. Psychol. Psychother. 2020;27(3):384–395. doi: 10.1002/cpp.2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Rossi R., Socci V., Pacitti F., Di Lorenzo G., Di Marco A., Siracusano A., Rossi A. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) Pandemic in Italy. JAMA Netw. Open. 2020;3(5):e2010185. doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Simms A., Fear N.T., Greenberg N. The impact of having inadequate safety equipment on mental health. Occup. Med. (Lond.) 2020;70(4):278–281. doi: 10.1093/occmed/kqaa101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Au A., Chan I., Li P., Chan J., Chan Y., Ng F. Correlates of psychological distress in discharged patients recovering from severe acute respiratory syndrome in Hong Kong. Int. J. Psychosoc. Rehabil. 2004;8:41–51. [Google Scholar]
- 133.Tan W., Hao F., McIntyre R.S., Jiang L., Jiang X., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Zhang Z., Lai A., Ho R., Tran B., Ho C., Tam W. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 2020;87:84–92. doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Moring J.C., Dondanville K.A., Fina B.A., Hassija C., Chard K., Monson C., LoSavio S.T., Wells S.Y., Morland L.A., Kaysen D., Galovski T.E., Resick P.A. Cognitive processing therapy for posttraumatic stress disorder via telehealth: Practical Considerations During the COVID-19 Pandemic. J. Trauma. Stress. 2020;33(4):371–379. doi: 10.1002/jts.22544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Monson C.M., Schnurr P.P., Resick P.A., Friedman M.J., Young-Xu Y., Stevens S.P. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. J. Consult. Clin. Psychol. 2006;74(5):898–907. doi: 10.1037/0022-006X.74.5.898. [DOI] [PubMed] [Google Scholar]
- 136.Galovski T.E., Blain L.M., Mott J.M., Elwood L., Houle T. Manualized therapy for PTSD: flexing the structure of cognitive processing therapy. J. Consult. Clin. Psychol. 2012;80(6):968–981. doi: 10.1037/a0030600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fortney J.C., Heagerty P.J., Bauer A.M., Cerimele J.M., Kaysen D., Pfeiffer P.N., Zielinski M.J., Pyne J.M., Bowen D., Russo J., Ferro L., Moore D., Nolan J.P., Fee F.C., Heral T., Freyholtz-London J., McDonald B., Mullins J., Hafer E., Solberg L., Unützer J. Study to promote innovation in rural integrated telepsychiatry (SPIRIT): Rationale and design of a randomized comparative effectiveness trial of managing complex psychiatric disorders in rural primary care clinics. Contemp. Clin. Trials. 2020;90:105873. doi: 10.1016/j.cct.2019.105873. [DOI] [PubMed] [Google Scholar]
- 138.Brown F.W. Telepsychiatry and Health Technologies: A Guide for Mental Health Professionals. Am. J. Psychiatry. 2017;174(11):1126–1126. doi: 10.1176/appi.ajp.2017.17040418. [DOI] [Google Scholar]
- 139.American Psychological Association Guidelines for the Practice of Telepsychology https://www.apa.org/practice/guidelines/telepsychology
- 140.Hassija C., Gray M.J. The effectiveness and feasibility of videoconferencing technology to provide evidence-based treatment to rural domestic violence and sexual assault populations. Telemed. J. Health. 2011;17(4):309–315. doi: 10.1089/tmj.2010.0147. [DOI] [PubMed] [Google Scholar]
- 141.Maieritsch K.P., Smith T.L., Hessinger J.D., Ahearn E.P., Eickhoff J.C., Zhao Q. Randomized controlled equivalence trial comparing videoconference and in person delivery of cognitive processing therapy for PTSD. J. Telemed. Telecare. 2016;22(4):238–243. doi: 10.1177/1357633X15596109. [DOI] [PubMed] [Google Scholar]
- 142.Peebles-Kleiger M.J. Using countertransference in the hypnosis of trauma victims: A model for turning hazard into healing. Am. J. Psychother. 1989;43(4):518–530. doi: 10.1176/appi.psychotherapy.1989.43.4.518. [DOI] [PubMed] [Google Scholar]
- 143.Vickers A., Zollman C., Payne D.K. Hypnosis and relaxation therapies. West. J. Med. 2001;175(4):269–272. doi: 10.1136/ewjm.175.4.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Effective treatments for PTSD: practice guidelines from the International Society for Traumatic Stress Studies; Guilford Press, 2010. pp. 592–595. [Google Scholar]
- 145.Eftekhari A., Stines L.R., Zoellner L.A. Do you need to talk about it? prolonged exposure for the treatment of chronic PTSD. Behav. Anal. Today. 2006;7(1):70–83. doi: 10.1037/h0100141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Treanor M., Craske M.G. In: Encyclopedia of Mental Health. 2nd ed. Friedman H.S., editor. Oxford: Academic Press; 2016. Exposure Therapy. pp. 181–185. [Google Scholar]
- 147.Zoellner L.A., Feeny N.C., Bittinger J.N., Bedard-Gilligan M.A., Slagle D.M., Post L.M., Chen J.A. Teaching trauma-focused exposure therapy for ptsd: critical clinical lessons for novice exposure therapists. Psychol. Trauma. 2011;3(3):300–308. doi: 10.1037/a0024642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Resick P.A., Nishith P., Weaver T.L., Astin M.C., Feuer C.A. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. J. Consult. Clin. Psychol. 2002;70(4):867–879. doi: 10.1037/0022-006X.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Jackson S., Baity M.R., Bobb K., Swick D., Giorgio J. Stress inoculation training outcomes among veterans with PTSD and TBI. Psychol. Trauma. 2019;11(8):842–850. doi: 10.1037/tra0000432. [DOI] [PubMed] [Google Scholar]
- 150.Kashani F., Kashani P., Moghimian M., Shakour M. Effect of stress inoculation training on the levels of stress, anxiety, and depression in cancer patients. Iran. J. Nurs. Midwifery Res. 2015;20(3):359–364. [PMC free article] [PubMed] [Google Scholar]
- 151.Yalom I.D. The theory and practice of group psychotherapy. AZ: Basic books; 1995. [Google Scholar]
- 152.Schwartze D., Barkowski S., Strauss B., Knaevelsrud C., Rosendahl J. Efficacy of group psychotherapy for posttraumatic stress disorder: Systematic review and meta-analysis of randomized controlled trials. Psychother. Res. 2019;29(4):415–431. doi: 10.1080/10503307.2017.1405168. [DOI] [PubMed] [Google Scholar]
- 153.Shapiro F. EMDR, Adaptive Information Processing, and Case Conceptualization. JEMDR Prac. Res. (2):68–87. [Google Scholar]
- 154.Shapiro F., Laliotis D. 2015. EMDR Therapy for Trauma-Related Disorders. [Google Scholar]
- 155.Samantha K.N., Ashley L., Jeffery M.K. Relaxation Techniques. https://www.ncbi.nlm.nih.gov/books/NBK513238/
- 156.Varvogli L. Stress management techniques: evidence-based procedures that reduce stress and promote health. 2011. [Google Scholar]
- 157.Galea S., Basham K., Culpepper L., Davidson J., Foa E., Kizer K., McCormick R. Treatment for posttraumatic stress disorder in military and veteran populations: Initial assessment. Washington, DC: The National Academies; 2012. [PubMed] [Google Scholar]
- 158.Watkins L.E., Sprang K.R., Rothbaum B.O. Treating PTSD: a review of evidence-based psychotherapy interventions. Front. Behav. Neurosci. 2018;12:258–258. doi: 10.3389/fnbeh.2018.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Alexander W. Pharmacotherapy for post-traumatic stress disorder in combat veterans: focus on antidepressants and atypical antipsychotic agents. P&T. 2012;37(1):32–38. [PMC free article] [PubMed] [Google Scholar]
- 160.O’Haire M.E., Guérin N.A., Kirkham A.C. Animal-assisted intervention for trauma: A systematic literature review. Front. Psychol. 2015;6:1121–1121. doi: 10.3389/fpsyg.2015.01121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ventola C.L. Social media and health care professionals: benefits, risks, and best practices. P&T. 2014;39(7):491–520. [PMC free article] [PubMed] [Google Scholar]
- 162.Starbird K., Spiro E.S., Koltai K. https://mediawell.ssrc.org/literature-reviews/misinformation-crisis-and-public-health
- 163.Ferri C. Social media’s response to COVID-19 misinformation. https://www.apc.org/en/news/social-medias-response-covid-19-misinformation
- 164.Bargh J.A., McKenna K.Y.A. The internet and social life. Annu. Rev. Psychol. 2004;55(1):573–590. doi: 10.1146/annurev.psych.55.090902.141922. [DOI] [PubMed] [Google Scholar]
- 165.Grant C.A., Wallace L.M., Spurgeon P.C. An exploration of the psychological factors affecting remote e‐worker’s job effectiveness, well‐being and work‐life balance. Employee Relat. 2013;35(5):527–546. doi: 10.1108/ER-08-2012-0059. [DOI] [Google Scholar]
- 166.Hartig T., Kylin C., Johansson G. The telework tradeoff: stress mitigation vs. constrained restoration. Appl. Psychol. 2007;56(2):231–253. doi: 10.1111/j.1464-0597.2006.00252.x. [DOI] [Google Scholar]
- 167.Mann S., Holdsworth L. The psychological impact of teleworking: stress, emotions and health. New Technol. Work Employ. 2003;18(3):196–211. doi: 10.1111/1468-005X.00121. [DOI] [Google Scholar]
- 168.McKenna K.Y.A., Bargh J.A. Coming out in the age of the Internet: Identity “demarginalization” through virtual group participation. J. Pers. Soc. Psychol. 1998;75(3):681–694. doi: 10.1037/0022-3514.75.3.681. [DOI] [Google Scholar]
- 169.Pantic I. Online social networking and mental health. Cyberpsychol. Behav. Soc. Netw. 2014;17(10):652–657. doi: 10.1089/cyber.2014.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Dutheil F., Mondillon L., Navel V. PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychol. Med. 2020;1-2 doi: 10.1017/S0033291720001336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Banerjee D. The COVID-19 outbreak: Crucial role the psychiatrists can play. Asian J. Psychiatr. 2020;50:102014. doi: 10.1016/j.ajp.2020.102014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Liu S., Yang L., Zhang C., Xiang Y-T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wang Y. The Chinese suicides prevented by AI from afar. BBC World Service; 2019. [Google Scholar]
- 174.Tullio V., Perrone G., Bilotta C., Lanzarone A., Argo A. Psychological support and psychotherapy via digital devices in Covid-19 emergency time: Some critical issues. Med. Leg. J. 2020;88(2):73–76. doi: 10.1177/0025817220926942. [DOI] [PubMed] [Google Scholar]