Abstract
Objective
The long‐term favorable safety profile of nusinersen provides an opportunity to consider a higher dose. We report on the relationships between nusinersen cerebrospinal fluid (CSF) exposure, biomarker levels, and clinical efficacy.
Methods
The analyses used data from the CS3A and ENDEAR studies of nusinersen in participants with infantile‐onset spinal muscular atrophy (SMA). Steady‐state CSF trough (C trough) levels, plasma phosphorylated neurofilament heavy chain (pNF‐H) levels, body weight, and Children's Hospital of Philadelphia Infant Test of Neuromuscular Disorders (CHOP INTEND) scores were selected as parameters of interest. A validated population pharmacokinetic (PK) model was applied to predict the nusinersen CSF C trough. PK/pharmacodynamic (PK/PD) models used nusinersen CSF C trough measurements, which were time‐matched with CHOP INTEND scores.
Results
Higher nusinersen CSF exposure was associated with a greater decrease in pNF‐H levels and greater efficacy, as measured by change in the CHOP INTEND score from baseline. These findings indicate a dose–response relationship between CSF nusinersen levels and treatment response. The higher dose is predicted to lead to approximately a 2.4‐fold increase in nusinersen CSF levels with fewer loading doses. PK/PD modeling indicates that a higher concentration of nusinersen may predict an additional 5‐point increase in CHOP INTEND score beyond that observed with 12 mg.
Interpretation
Our data indicate that a higher dose of nusinersen may lead to additional clinically meaningful improvement in efficacy when compared with the currently approved 12‐mg dose. The efficacy, safety, and PK of a higher nusinersen dose are currently under investigation in the ongoing phase 2/3 DEVOTE study (NCT04089566).
Introduction
Spinal muscular atrophy (SMA) is a progressive motor neuron disorder caused by deletions or mutations in the survival motor neuron (SMN1) gene. 1 Nusinersen is a synthetic antisense oligonucleotide administered intrathecally, which modifies splicing of SMN2 pre‐mRNA, resulting in exon 7 inclusion and increased production of full‐length and functional SMN protein. 2 Nusinersen is approved for treatment of SMA in the United States, Europe, and other countries with a recommended dosing regimen of four 12‐mg loading doses, followed by maintenance doses every 4 months. 3 , 4
Nusinersen has been evaluated in a comprehensive clinical study program across a broad spectrum of SMA populations. Infants genetically diagnosed with SMA during the presymptomatic stage (most likely to develop SMA Type I or II) who were treated with nusinersen had substantial clinical benefit with improvements in permanent ventilation‐free survival, as well as motor, bulbar, and pulmonary function. 5 Participants with infantile‐onset SMA who initiated nusinersen at a young age were more likely to be alive and achieved significant improvements in motor function compared with a control group and a natural history cohort. 6 , 7 , 8 Similar findings were observed in the clinical studies of children with later‐onset SMA, whereby nusinersen provided significant and clinically meaningful improvements in motor function. 9 , 10 Participants who enrolled in the open‐label extension SHINE study (NCT02594124) had continued improvements in motor function throughout 5 years of treatment (based on interim analysis), with no reports of treatment‐related serious adverse events (AEs). 11 , 12 , 13 , 14 , 15 , 16 Elevated phosphorylated neurofilament heavy chain (pNF‐H) levels result from axonal degeneration and are a biomarker for SMA, correlating with disease severity. 5 , 17 Plasma pNF‐H levels were reduced significantly with nusinersen treatment in both presymptomatic and symptomatic infantile‐onset SMA. 5 , 17 Overall, these data demonstrate significant and clinically meaningful effect from nusinersen that continues with long‐term treatment. Treatment with nusinersen has been well tolerated, with the highest incidence AEs considered unrelated to study drug and associated with SMA disease: pyrexia, scoliosis, and upper respiratory tract infections. 5 , 6 , 7 , 9 , 10 The favorable safety profile has been consistent for up to 7.6 years of treatment 11 , 18 , 19 and provides an opportunity to explore higher doses of nusinersen.
We present analyses indicating a dose–response relationship between nusinersen levels in cerebrospinal fluid (CSF), neurofilament levels, and efficacy measured by the Children's Hospital of Philadelphia Infant Test of Neuromuscular Disorders (CHOP INTEND). Furthermore, our pharmacokinetic/pharmacodynamic (PK/PD) analysis indicates that increased exposures obtained with a higher dose of nusinersen may lead to a clinically meaningful increase in efficacy above that seen with the 12‐mg approved dose. The efficacy, safety, and PK of higher doses of nusinersen are currently under investigation in the ongoing phase 2/3 DEVOTE study (NCT04089566).
Methods
The relationship between nusinersen CSF levels and plasma pNF‐H levels was analyzed using data from 93 participants with infantile‐onset SMA who had two SMN2 copies from the CS3A (NCT01839656) and ENDEAR (NCT02193074) studies. Briefly, the CS3A study was an open‐label, phase 2, escalating‐dose clinical study that assessed the safety and efficacy of nusinersen in 20 participants with infantile‐onset SMA (eligibility criteria: 3 weeks to 7 months of age, symptom onset at 3 weeks to 6 months, and confirmed 5q SMA). 6 , 8 Participants received loading doses (or equivalent adjusted for those <2 years of age) of 6‐mg or 12‐mg equivalent nusinersen on days 1, 15, and 85, followed by 12‐mg equivalent doses on day 253 and every 4 months thereafter. 6 , 8 The ENDEAR study was a randomized, double‐blind, sham‐controlled, phase 3, efficacy and safety study of nusinersen with 121 participants with infantile‐onset SMA (eligibility criteria: age ≤7 months, symptom onset at ≤6 months of age, and two SMN2 gene copies). 7 Infants were randomly assigned in a 2:1 ratio to 12‐mg equivalent doses of nusinersen or sham administered on days 1, 15, 29, and 64, and maintenance doses on days 183 and 302. 7 For the CSF and pNF‐H analysis, data were plotted separately for participants with SMA who received a different number of loading doses and different dosages. CSF PK, CSF and plasma pNF‐H levels, and the relevant standard errors were calculated and plotted as a function of time after the first dose was administered. The steady‐state nusinersen CSF and plasma levels were modeled for both the 12‐mg approved dose and the higher dose for a range of body weights (9–115 kg [20–254 lbs]).
To generate the PK/PD model, CSF trough concentration (C trough) measurements were time‐matched with CHOP INTEND scores in 82 participants with two SMN2 copies from CS3A and ENDEAR. A maximum effect (E max) model was constructed assuming a direct correlation between the C trough and improvement in CHOP INTEND scores. The model includes data after three loading doses when both PK and CHOP INTEND were collected; days 253, 379, 505, 631, and 757 from CS3A, and days 64, 183, and 302 from ENDEAR. The E max model was fitted to this PK/PD data set. Baseline characteristics of participants from CS3A and ENDEAR that were included in this analysis were similar. For CS3A, 11 participants were included who had a mean (SD) age at SMA onset of 1.9 (1.3) months, mean (SD) age at first dose of nusinersen of 146.5 (61.2) days, mean (SD) disease duration at first dose (i.e., time from symptom onset to first dose) of 2.9 (1.2) months, mean (SD) baseline weight of 6.4 (0.8) kg, and a mean (SD) baseline CHOP INTEND score of 26.1 (6.9) points. For ENDEAR, 71 participants were included who had a mean (SD) age at SMA onset of 1.79 (0.9) months, mean (SD) age at first dose of nusinersen of 159.9 (48.3) days, mean (SD) disease duration at first dose of 3.5 (1.4) months, mean (SD) baseline weight of 6.6 (1.0) kg, and a mean (SD) baseline CHOP INTEND score of 27.1 (7.9) points.
A previously published population PK model was applied to predict the nusinersen C trough in the CSF. 20 Briefly, the model is a four‐compartment model where nusinersen is administered to a CSF compartment. This compartment equilibrates with adjacent tissues and drains unidirectionally into the plasma compartment. Nusinersen within the plasma compartment clears linearly and equilibrates with peripheral tissues and matrices adjacent to circulation. Combined, this results in pharmacokinetics that are linear within the range of concentrations simulated, and a half‐life within the CSF of approximately 4 months. Further, body weight (and, consequently, participant age) was identified as a relevant covariate impacting plasma exposure and, at weights below 20 kg, exposure within the CSF. However, the exposure within the CSF even below 20 kg and in young infants was not meaningfully impacted by the age and growth of the participants. The model was informed by a large body of clinical data from 10 different clinical studies covering a broad range of ages, SMA types, and body weights, including infants dosed at <6 months of age.
The higher‐dose regimen for the DEVOTE study was simulated to predict the anticipated CSF exposure as a function of time. The model described the steady‐state C trough concentration in the CSF, which is the value most robustly associated with efficacy, and compared with the steady‐state C trough concentration of the 12‐mg approved dose.
Results
Nusinersen CSF levels and plasma pNF‐H Levels
To assess the potential dose–response relationship, nusinersen CSF levels and plasma pNF‐H levels were analyzed from participants with infantile‐onset SMA in the CS3A and ENDEAR studies. Three different dosing regimens of nusinersen were administered in this population, enabling us to explore exposure response. Specifically, participants with SMA in CS3A received three loading doses of 6‐mg or 12‐mg equivalent doses of nusinersen on days 1, 15, and 85, followed by 12‐mg equivalent doses on day 253. Participants with SMA in ENDEAR received four loading doses of 12‐mg equivalent doses on days 1, 15, 29, and 64, followed by 12‐mg equivalent doses on days 183 and 302 (Fig. 1A). Data were plotted separately for these three groups for both nusinersen CSF levels and plasma pNF‐H levels. Data from participants with two SMN2 copies were used for the analysis. As expected, the lowest nusinersen CSF levels were observed in the CS3A group treated with the 6‐mg three loading dose regimen (1.1 ng/mL at day 85). Higher nusinersen CSF levels were seen in the CS3A group treated with three 12‐mg loading doses (3.7 ng/mL at day 85), and the highest levels were observed in the ENDEAR group treated with the 12‐mg four loading dose regimen (6.1 ng/mL at day 64; Fig. 1A and B). The higher nusinersen CSF levels also corresponded with a greater percentage reduction in plasma pNF‐H levels (Fig. 1C). The mean percentage reductions from baseline in plasma pNF‐H among those treated with 6‐mg and 12‐mg nusinersen loading doses in CS3A at day 85 were 25.0% and 62.7%, respectively. The greatest decrease (71.4%) in plasma pNF‐H levels was observed among the ENDEAR participants at day 64. Similar results were observed when using absolute pNF‐H values (Fig. 1D), although the different levels of plasma pNF‐H at baseline need to be accounted for when considering the degree of change. 17 A similar inverse relationship was observed between nusinersen CSF levels and reductions of CSF pNF‐H levels (data not shown).
Figure 1.
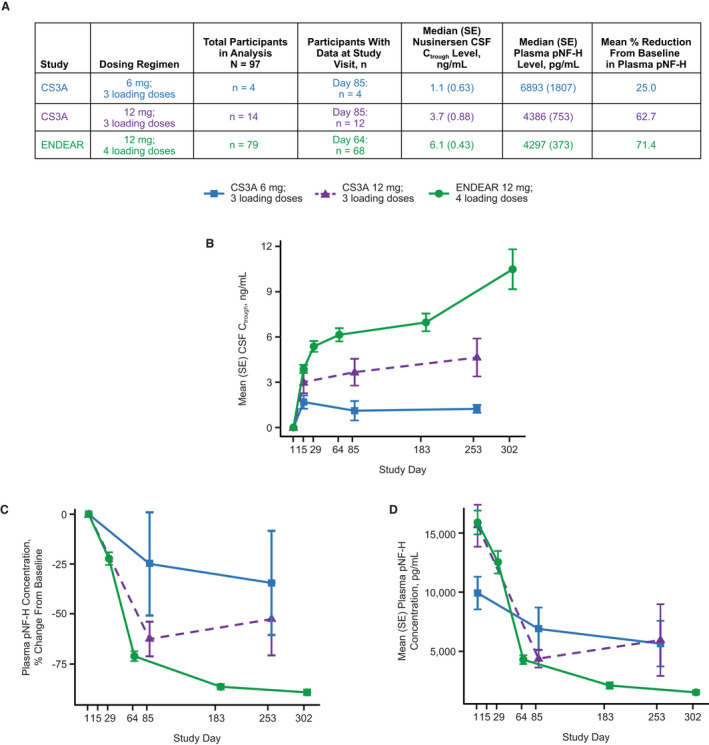
Higher nusinersen CSF levels are associated with greater reduction in plasma pNF‐H levels. (A) Summary table showing median nusinersen CSF C trough, median plasma pNF‐H levels, and percentage reduction in plasma pNF‐H levels in each treatment group. (B) Higher Nusinersen CSF C trough levels were observed with higher and/or more frequent doses, as expected. (C) Greater percentage decreases in plasma pNF‐H levels were seen in groups with higher nusinersen levels. (D) Similar results were observed with absolute plasma values. CSF = cerebrospinal fluid; C trough = trough concentration; LD = loading dose; pNF‐H = phosphorylated neurofilament heavy chain; SE = standard error.
Three participants in the CS3A study did not have two SMN2 copies (two participants had three SMN2 copies, one participant had an unknown number of SMN2 copies). When data from these participants were added to the analysis (all in the 12‐mg, three loading doses group), similar results were observed with a 75% reduction in CSF pNF‐H levels, compared with a 63% reduction when data from these participants were not included.
PK/PD modeling of motor function and CSF nusinersen levels
To further explore the dose–response relationship, we developed a PK/PD model using nusinersen CSF levels obtained at the same time as CHOP INTEND assessments from the CS3A and ENDEAR studies based on data from participants with two SMN2 copies. This analysis indicated that the higher the CSF concentration of nusinersen, the greater the efficacy as measured by CHOP INTEND change from baseline (Fig. 2). Using a population PK model, the steady‐state CSF concentration of the 12‐mg approved dose is 5 ng/mL. 20 In the PK/PD model, the nusinersen concentration attained with the 12‐mg ENDEAR dosing regimen (5 ng/mL) was associated with an estimated improvement of 7.5 points from baseline in CHOP INTEND score (Fig. 2), which is consistent with the mean 9.1‐point improvement observed in the ENDEAR study. We also conducted a sensitivity analysis using all available data that included two additional participants with three SMN2 copies and observed nearly identical results, also with an estimated improvement in CHOP INTEND score of 7.5 points from baseline (data not shown).
Figure 2.
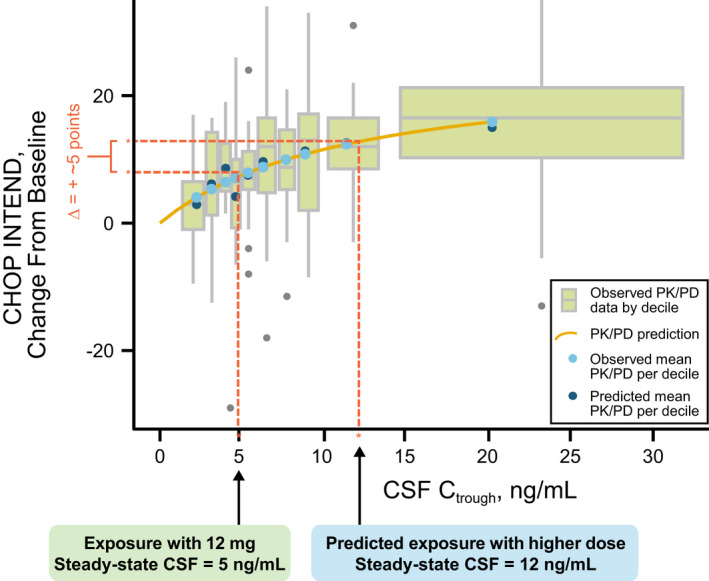
PK/PD modeling indicates that higher nusinersen CSF levels are associated with higher efficacy, and that higher dose may lead to clinically meaningful increase in efficacy above that seen with 12‐mg approved dose. PK/PD modeling using CS3A and ENDEAR data from participants with two SMN2 copies shows higher nusinersen CSF levels are associated with higher efficacy as measured by change from baseline in the CHOP INTEND score. This model indicates that a higher dose of nusinersen may lead to additional clinically meaningful improvement in efficacy (~5 points in CHOP INTEND) above that seen with the 12‐mg approved dose of nusinersen. CHOP INTEND change from baseline estimated with exposure at 12 mg is 7.5 points, whereas the exposure at the higher dose is expected to lead to CHOP INTEND change from baseline of 12.7 points (incremental gain of 5.2 points above 12 mg). Exposures are based on steady‐state concentrations calculated using population PK model 20 – 12‐mg approved dose of nusinersen leads to 5 ng/mL nusinersen CSF levels and higher dose of nusinersen is expected to lead to 12 ng/mL nusinersen CSF levels. Both observed and predicted mean PK/PD values per decile (10% of values) are similar, indicating this model is representative of the observed values. Each box represents one decile of the data, shown as a standard box plot (whiskers 90% CI, box 50% CI, line in box represents median value, outliers are shown as single points outside of the box). CHOP INTEND = Children's Hospital of Philadelphia Infant Test of Neuromuscular Disorders; CI = confidence interval; CSF = cerebrospinal fluid; C trough = trough concentration; PD = pharmacodynamic; PK = pharmacokinetic.
Using a population PK model, we modeled a number of dosing regimens (data not shown) to select one that would be expected to lead to nusinersen CSF levels associated with a clinically meaningful increase (≥4 points in CHOP INTEND score) above the 12‐mg dose based on the PK/PD model. We selected the dosing regimen with two loading doses of 50 mg separated by 2 weeks and maintenance doses of 28 mg (Fig. 3A). Using the population PK model, this regimen is predicted to lead to nusinersen CSF steady‐state levels of 12 ng/mL, a 2.4‐fold increase in nusinersen CSF concentrations over the 12‐mg approved dose of nusinersen (Fig. 3B). Based on the PK/PD model (using data from participants with two SMN2 copies), this higher concentration is estimated to lead to a 5.2‐point increase in CHOP INTEND score above that observed with 12‐mg approved dosing regimen (Fig. 2).
Figure 3.
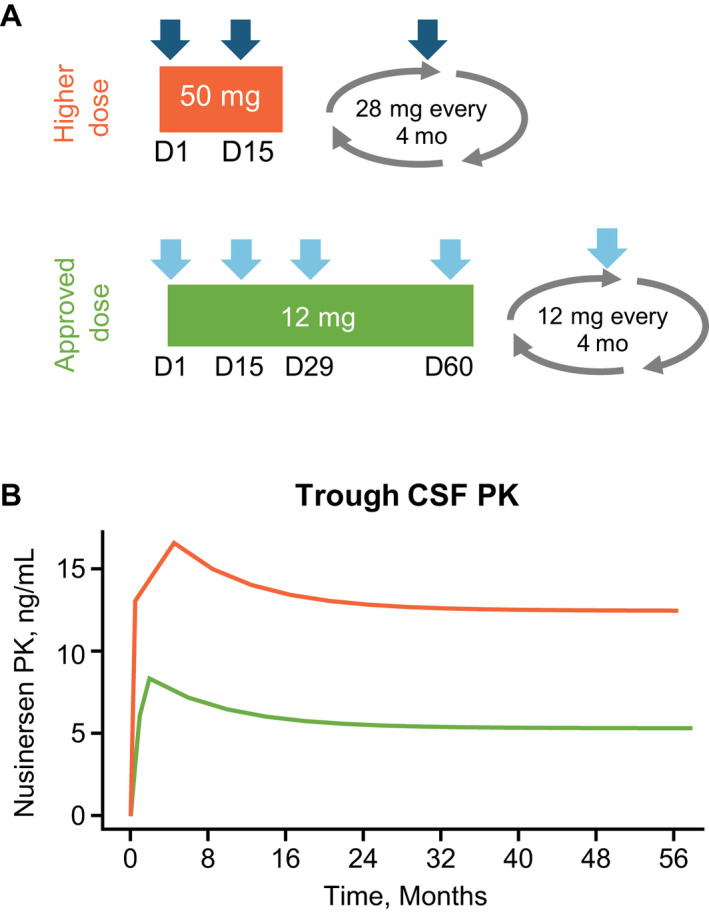
Higher dose of nusinersen is expected to lead to ~2.4‐fold increase in nusinersen levels in CSF compared with the approved 12‐mg dose. (A) Schematic illustrating higher‐dose regimen (two loading doses 2 weeks apart of 50 mg and maintenance dose 28 mg every 4 months) and the 12‐mg approved dose of nusinersen (four loading doses of 12 mg and maintenance dose 12 mg every 4 months). (B) Population PK model estimates steady‐state CSF concentration of nusinersen of 5 ng/mL with the 12‐mg approved dose of nusinersen and 12 ng/mL with the higher nusinersen dosing regimen. Steady state is predicted to be achieved after six maintenance doses, or 24 months after the final loading dose. Median values are shown; the confidence intervals for 12‐mg dose were previously described in MacCannell et al. 20 Data for the higher dose will be obtained from the DEVOTE study. CSF = cerebrospinal fluid; D = day, PK = pharmacokinetic.
Given that age at first dose represents an important determinant of response, 7 , 8 , 21 we conducted additional analyses to determine whether our PK/PD analysis could have an alternative explanation and be driven primarily by younger participants with a higher change from baseline in CHOP INTEND score. First, we separated the data according to median participant age at first dose (i.e., 150 days) and plotted the PK/PD curve for data of participants below (Fig. 4A) and above (Fig. 4B) median age at first dose. We hypothesized that if age was the key driver for this analysis, we should not see any PK/PD relationships, or potentially only in one group or substantially altered PK/PD curves. In contrast, we observed similar PK/PD curves in both groups. As expected, the mean change from baseline in CHOP INTEND total score was greater in the group that was younger at first dose than in the group that was older at first dose. This applied both at exposures associated with steady state of 12 mg and a higher dose of nusinersen (28 mg). Importantly, the additional improvement in CHOP INTEND score expected with the higher dose of nusinersen above that seen with the 12‐mg regimen was similar in both younger and older participants based on age at first dose with 5.2‐ and 5.1‐point improvement in CHOP INTEND scores, respectively (Fig. 4C). This analysis suggests that while age at first dose is an important contributing factor to change in CHOP INTEND score from baseline, it is not a contributor to the higher efficacy predicted in this model with the higher dose of nusinersen.
Figure 4.
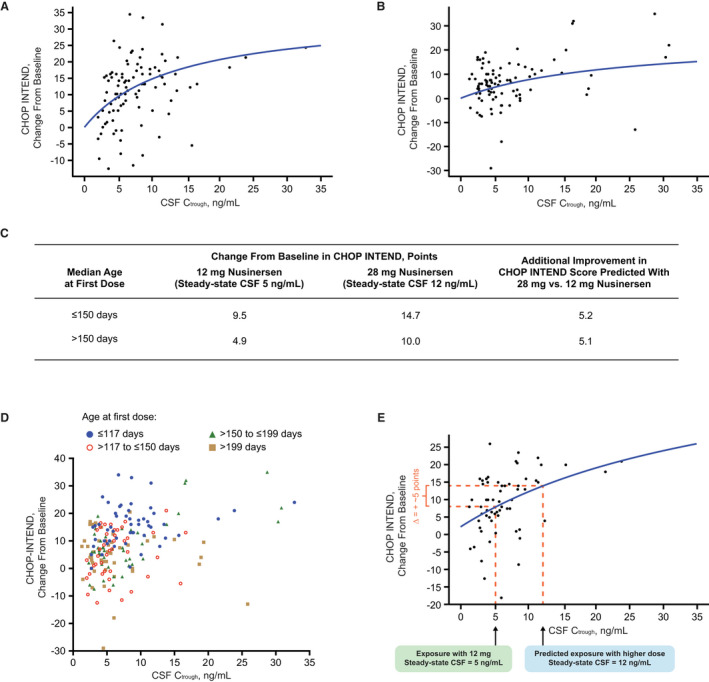
Age at first dose of nusinersen does not meaningfully impact the predicted increase in CHOP INTEND score with a higher dose of nusinersen compared with 12 mg. (A) In younger participants with age at first dose ≤150 days (at or below median in this data set), a higher nusinersen CSF concentration was associated with higher CHOP INTEND change from baseline. (B) In older participants with age at first dose >150 days (above median in this data set), higher nusinersen CSF concentration was also associated with higher CHOP INTEND change from baseline, albeit with a flatter curve. (C) As expected, the change from baseline in CHOP INTEND scores was greater in younger participants at exposures associated with the steady state of 12 mg and higher dose of nusinersen (28 mg). Importantly, the additional improvement in CHOP INTEND score expected with the higher dose of nusinersen compared with 12 mg was similar in each population (~5 points). (D) No clear relationship between CSF C trough and age was observed when patients were stratified into four different quartiles according to their age at first dose. As expected, younger participants (first quartile) have greater change from baseline in CHOP INTEND scores, consistent with Figure 3C and results from the ENDEAR study. 7 (E) A similar PK/PD relationship indicating 5.0‐point increase in CHOP INTEND above 12 mg at exposures expected with the higher dose of nusinersen was observed using only data from the time of first maintenance dose administration (day 183 for ENDEAR study and day 253 for CS3A study). The E max value in this model could not be determined, likely due to the limited a data set. CHOP INTEND = Children's Hospital of Philadelphia Infant Test of Neuromuscular Disorders; CSF = cerebrospinal fluid; C trough = trough concentration; E max = maximum effect.
To analyze for potential impact of age on nusinersen levels in CSF in this data set, we separated the data in the PK/PD model into four different quartiles by age at first dose (Fig. 4D). We did not observe any clear pattern of age and CSF levels, consistent with our analyses described above (Fig. 4A–C).
In summary, age at first dose of nusinersen does not impact the predicted additional increase in CHOP INTEND score with a higher dose of nusinersen compared with 12‐mg nusinersen.
Our PK/PD model uses data from participants in ENDEAR and CS3A who had different dosing regimens and doses, which lead to different nusinersen concentrations (Fig. 1B) and thus allows for exploration of PK/PD. SMA is a rare disease, and our data set is relatively limited because of the small sample size in the clinical studies; thus, we used the maximum data set available to use in our PK/PD modeling (Fig. 2). We then conducted sensitivity analysis using only PK/PD data from the first maintenance dose (day 253 for CS3A and day 183 for ENDEAR). Similar results were observed with an additional increase of approximately 5.0 points from baseline in CHOP INTEND score with a higher dose of nusinersen compared with the 12‐mg dose (Fig. 4E).
Steady‐state nusinersen CSF exposures across different body weights
Given the relationship between nusinersen CSF concentrations and efficacy, we assessed the potential changes of nusinersen CSF levels as participants age and grow. The steady‐state nusinersen CSF levels for both the 12‐mg approved dose and higher dose were modeled for a range of body weights using the population PK model. The steady‐state concentrations of nusinersen CSF were similar across the different body weights of 9–115 kg (20–254 lbs) for both the 12‐mg approved dose and higher dose of nusinersen (Fig. 5). Similarly, sex was not identified as a significant covariate in CSF or plasma pharmacokinetics (data not shown).
Figure 5.
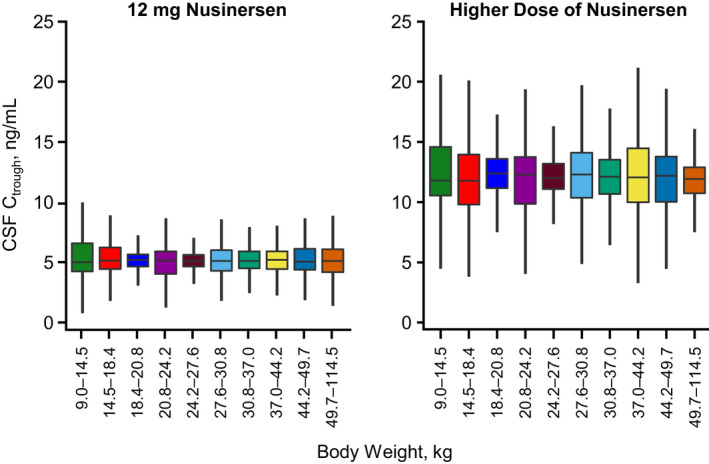
Nusinersen CSF levels are similar as participants age and grow. Body weight is predicted to have minimal impact upon the C trough either at the 12‐mg or 28‐mg dose of nusinersen. Steady‐state trough concentrations were simulated over a wide range of body weights (9.0–114.5 kg). Despite an over 10‐fold change in body weight, the volume of the CNS is predicted not to change significantly over a wide range of body weights, leading to consistent exposure within the CNS. The total simulated patient population was divided into weight deciles (the range of body weights is presented on the x‐axis). The boxes represent 50% of the simulated population, bisected by the median value. The whiskers represent the predicted range for 95% of the simulated population. CNS = central nervous system; CSF = cerebrospinal fluid; C trough = trough concentration.
Discussion
Nusinersen has been evaluated in a clinical development program across a broad spectrum of SMA populations: infants treated in the presymptomatic stage of SMA, infants and children with infantile‐onset SMA, and children, teenagers, and adults with later‐onset SMA. Results from the clinical studies have demonstrated significant and clinically meaningful effect on motor function and survival endpoints. 5 , 7 , 9 , 10 , 22 The favorable safety profile, with up to 7.6 years of follow‐up during nusinersen treatment, provides an opportunity to explore higher doses of nusinersen. 11 , 18 , 19 This is further supported by preclinical toxicology studies of higher doses (data not shown).
Our analyses demonstrate a dose–response relationship between nusinersen CSF levels and plasma pNF‐H levels. Plasma pNF‐H levels have been suggested to be a valuable biomarker in SMA, with an observed 10‐fold higher level in infants with SMA compared with age‐matched non‐neurological disease controls. 17 Treatment with nusinersen rapidly reduces pNF‐H levels in both participants in the presymptomatic stage of SMA and those with symptomatic infantile‐onset SMA. 5 , 17 Additionally, levels of plasma pNF‐H after treatment (day 64) were the best predictors of future motor function achievement in participants treated with nusinersen in the presymptomatic stage of SMA in the NURTURE (NCT02386553) study. 5 Although our analysis does not allow us to predict the degree of reduction in pNF‐H at the higher dose, our results showing a dose response (Fig. 1C) raise the possibility that pNF‐H levels may be reduced further and faster owing to the higher expected nusinersen CSF levels achieved after only two loading doses.
The potential for additional clinical efficacy at the higher dose of nusinersen is supported by our PK/PD analysis, which shows that higher nusinersen CSF levels are associated with higher efficacy as measured by CHOP INTEND change from baseline in infantile‐onset SMA. Our PK/PD model indicates that the higher dose of nusinersen may lead to a clinically meaningful increase in the CHOP INTEND score, estimated at approximately 5 points above that observed with the 12‐mg approved dose of nusinersen. Although this analysis uses time‐matched observations and relies on actual data collected at different times in the CS3A and ENDEAR studies, the majority of the data are from the ENDEAR study from day 64 and day 183. As a result, this model likely predicts effects expected after 6 months of treatment.
While age is an important contributing factor to change in CHOP INTEND score from baseline in our studies, our sensitivity analyses suggest it is not a contributor to the higher efficacy predicted by our model with the higher dose of nusinersen. This is consistent with lack of any clear pattern between age at first dose and nusinersen CSF levels.
Additional analyses support the dose–response relationship between nusinersen and clinical outcomes. Among participants with infantile‐onset SMA, higher nusinersen CSF area under the curve values in the initial few months of treatment were associated with a higher probability of being a motor milestone responder (Fig. S1). In participants with later‐onset SMA, the median change from baseline in Hammersmith Functional Motor Scale – Expanded score associated with higher exposures (10–15 ng/mL) was twice that associated with lower exposures (0–5 ng/mL) (Fig. S2). However, given the relatively limited data in participants with later‐onset SMA, lower nusinersen exposures, and heterogeneous participant population, it is difficult to estimate efficacy of higher doses in this population or draw quantitative conclusions with respect to any potential PK/PD relationship. Our assessment of the greater efficacy of higher dose nusinersen relies primarily on data from the infantile‐onset SMA studies since these enrolled the largest number of participants and included different dosing regimens, allowing for construction of PK/PD models. Furthermore, given the likely relationship between higher nusinersen levels and higher SMN levels in the central nervous system, the higher dose of nusinersen has the potential for additional efficacy beyond that observed with the 12‐mg approved dose in the broad SMA population.
Our PK model shows that steady‐state concentrations of nusinersen in CSF are predicted to increase approximately 2.4‐fold with the higher dose of nusinersen. In addition, the analysis of nusinersen CSF levels across a wide range of body weights shows that nusinersen levels remain similar as participants age and grow, as expected with intrathecal administration.
The modeled weight range was selected to enable comparison across steady‐state concentrations in CSF as the most relevant comparisons. Specifically, maximum weight (115 kg) was selected based on highest weight of a participant in the clinical development program, and minimum weight modeled was selected based on when we were confident steady‐state concentration would be established even in the youngest patients, given the long half‐life of nusinersen. As steady‐state concentrations are achieved after five half‐lives (~20 months), patients with lower weights will also have similar concentrations of nusinersen in CSF after ~20 months of nusinersen administration. During the initial loading phase, the CSF trough concentration exceeds the steady state by approximately 34% (16 vs. 12 ng/mL at steady state) and returns to a steady‐state value, which remains stable throughout the duration of dosing. The steady‐state CSF trough concentration is minimally impacted by age or body weight in all simulated patient populations. Furthermore, our PK modeling shown in Figure 3B indicates that nusinersen CSF concentrations are similar even before reaching steady state.
Thus, a higher dose of nusinersen is expected to lead to higher concentrations of nusinersen across broad SMA populations, which may in turn lead to additional clinical benefit. Therefore, we expect that once a steady‐state concentration of nusinersen is achieved in patients with SMA, remaining α‐motor neurons are likely exposed to similar concentrations of nusinersen independent of body weight or age, leading to maintenance of SMN protein levels.
The limitations of the analyses described in more detail above include primarily a limited number of participants from clinical studies, as SMA is a rare disease, and interpretations are based primarily on data from clinical studies with participants with infantile‐onset SMA treated with nusinersen using efficacy data matched with nusinersen CSF exposures. Nonetheless, the totality of the data indicates that the higher dose of nusinersen may lead to additional clinically meaningful improvement in efficacy when compared with the currently approved 12‐mg dose. This hypothesis is currently being evaluated in the DEVOTE clinical study.
The long‐term favorable safety profile of nusinersen provides an opportunity to explore higher doses for patients with SMA. Higher nusinersen CSF levels were associated with a greater decrease in pNF‐H levels, suggesting a dose–response relationship. The PK/PD model indicates that the higher dose of nusinersen may be associated with a clinically meaningfully increase in efficacy above that seen with the 12‐mg approved dose of nusinersen. The efficacy, safety, and PK of the higher dose of nusinersen are currently being investigated in the ongoing DEVOTE study.
Author Contributions
R.S.F., M.M.R., S.I.P.P., J.W.D., E.M., D.C.D., and J.M. participated in the collection of data. R.S.F., M.M.R., S.I.P.P., J.W.D., E.M., D.C.D., R.F., J.M., J.G‐G., D.M., and Z.B. participated in the design of the analyses, R.F. conducted the statistical analyses, and D.M. conducted the pharmacokinetic and pharmacodynamic analyses. All authors (R.S.F., M.M.R., S.I.P.P., J.W.D., E.M., D.C.D., R.F., J.M., J.G‐G., D.M., and Z.B.) participated in the analysis and interpretation of data and in drafting and critically revising the manuscript.
Conflict of Interest
These analyses were sponsored by Biogen (Cambridge, MA, USA). Biogen provided funding for medical writing support in the development of this report; Nancy Niguidula from Excel Scientific Solutions provided writing assistance in the development of the first and subsequent drafts based on input from authors, and Cara Dickinson and Jackie Parker from Excel Scientific Solutions copyedited and styled the manuscript per journal requirements. The authors had full editorial control of the paper and provided their final approval of all content.
R.S.F. served as a consultant for AveXis/Novartis Gene Therapies, Biogen, Neurogene, and Roche/Genentech; received honoraria for speaking from AveXis, Biogen, Elsevier, Excerpta Medica, and Roche; received travel support from Cure SMA, SMA Europe, and the SMA Foundation; received grants from Biogen to St Jude Children's Hospital for conduct of the DEVOTE study; received grants paid to his prior institution, Nemours Children's Health System, for the conduct of clinical trials from AveXis, Cytokinetics, Roche, and Scholar Rock; received research funding from Cure SMA to support an SMA study group; served in an advisory capacity for nonprofit organizations: Cure SMA, EveryLife Foundation, and n‐Lorem Foundation with no payments received; and received royalty payments from Children's Hospital of Philadelphia for licensing fees for co‐invention of the CHOP INTEND motor function scale.
M.M.R. has participated in advisory boards for nonprofit organizations: FSHD Global Research Foundation, Muscular Dystrophy Foundation, and Save Our Sons Duchenne Foundation; received honoraria from Biogen, BioMarin, and Novartis; and received research funding from Biogen, FSHD Global Research Foundation, Genzyme, MD NSW, and Save Our Sons Duchenne Foundation paid to her institution.
S.I.P.P. has participated in advisory boards for SMA studies for AveXis, Biogen, Ionis, Novartis, and Roche; and has served as a Principal Investigator for Biogen/Ionis and Roche clinical trials.
J.W.D. has served as a consultant for Shift Therapeutics; has participated on an advisory board or data safety monitoring board for AveXis/Novartis Gene Therapies, Biogen, Cytokinetics, Epirium Bio, Ionis, Pfizer, Roche, and Scholar Rock; received research support from AveXis/Novartis Gene Therapies, Biogen, Cytokinetics, Ionis, Roche/Genentech, and Scholar Rock; and is an inventor on patents related to genetic testing of myotonic dystrophy type 2 (US patent 7442782) and spinocerebellar ataxia type 5 (US patent 7527931) assigned to Regents of the University of Minnesota and licensed to Athena Diagnostics and has received royalty payments from Athena Diagnostics.
E.M. has participated in advisory boards for SMA studies for AveXis, Biogen, Ionis, Novartis, and Roche; has been a Principal Investigator for ongoing Biogen and Roche clinical trials; and received research grants from Famiglie SMA Italy, Italian Telethon, Novartis, Scholar Rock, and SMA Europe.
D.C.D. has served as an advisor/consultant for AveXis, Biogen, Cytokinetics, Ionis, METAFORA, Roche, Sanofi, Sarepta, Scholar Rock, SMA Foundation, and Ultragenyx, with no financial interests in these companies; received grants from Cure SMA, Department of Defense, Glut1 Deficiency Foundation, Hope for Children Research Foundation, National Institutes of Health, and SMA Foundation; received research funding from Department of Defense, Glut1 Deficiency Foundation, Hope for Children Research Foundation, iSMAC initiative (Biogen), National Institutes of Health, Sanofi, and SMA Foundation; received clinical trial funding from Ionis, Mallinckrodt, PTC, Santhera, Sarepta, Scholar Rock, and Ultragenyx; serves as the Data Safety Monitoring Committee Chair for Aspa Therapeutics; and is an inventor on a patent on gene therapy for Glut1DS.
J.M. has participated in advisory boards for Biogen, Roche, and Scholar Rock; has served as a consultant for Biogen, Genentech, Sarepta, and Scholar Rock; and received research support paid to her institution from Cure SMA, Eunice Kennedy Shriver National Institute for Child Health and Human Development (K01HD084690), Genentech Independent Medical Education Grant (G‐88736), and Muscular Dystrophy Association (575870 and 629259).
J.G.‐G. has participated in advisory boards for Astellas, AveXis/Novartis Gene Therapies, Biogen, BioMarin, Novartis, PTC, Roche, and Sarepta; received research support paid to Hospital das Clínicas (UFMG) from PTC, Roche, and Sarepta; and has received research funding paid to Universidade Federal de Minas Gerais (UFMG) from FAPEMIG (Brazil).
R.F., D.M., and Z.B. are employees of and hold stock/stock options in Biogen.
Supporting information
Figure S1. Exposure response analysis of motor milestone response.
Figure S2. Median change from baseline in HFMSE total score associated with higher exposures (10–15 ng/mL) of nusinersen was twice that associated with lower exposures (0–5 ng/mL) of nusinersen in participants with later‐onset SMA.
Funding Information
This work was supported by Biogen.
Funding Statement
This work was funded by Biogen .
Data Availability Statement
Requests for the data supporting this manuscript should be submitted to the Biogen Clinical Data Request Portal (www.biogenclinicaldatarequest.com).
References
- 1. Lunn MR, Wang CH. Spinal muscular atrophy. Lancet. 2008;371:2120‐2133. [DOI] [PubMed] [Google Scholar]
- 2. Hua Y, Sahashi K, Hung G, et al. Antisense correction of SMN2 splicing in the CNS rescues necrosis in a type III SMA mouse model. Genes Dev. 2010;24:1634‐1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. SPINRAZA (nusinersen) injection, for intrathecal use. Prescribing Information. 2018. Accessed April 23, 2018. www.spinraza.com/content/dam/commercial/specialty/spinraza/caregiver/en_us/pdf/spinraza‐prescribing‐information.pdf
- 4. SPINRAZA (nusinersen) . Summary of product characteristics. 2018. Accessed April 23, 2018. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_‐_Product_Information/human/004312/WC500229704.pdf
- 5. De Vivo DC, Bertini E, Swoboda KJ, et al. Nusinersen initiated in infants during the presymptomatic stage of spinal muscular atrophy: interim efficacy and safety results from the phase 2 NURTURE study. Neuromuscul Disord. 2019;29:842‐856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Finkel RS, Chiriboga CA, Vajsar J, et al. Treatment of infantile‐onset spinal muscular atrophy with nusinersen: a phase 2, open‐label, dose‐escalation study. Lancet. 2016;388:3017‐3026. [DOI] [PubMed] [Google Scholar]
- 7. Finkel RS, Mercuri E, Darras BT, et al. Nusinersen versus sham control in infantile‐onset spinal muscular atrophy. N Engl J Med. 2017;377:1723‐1732. [DOI] [PubMed] [Google Scholar]
- 8. Finkel RS, Chiriboga CA, Vajsar J, et al. Treatment of infantile‐onset spinal muscular atrophy with nusinersen: final report of a phase 2, open‐label, multicentre, dose‐escalation study. Lancet Child Adolesc Health. 2021;5:491‐500. [DOI] [PubMed] [Google Scholar]
- 9. Mercuri E, Darras BT, Chiriboga CA, et al. Nusinersen versus sham control in later‐onset spinal muscular atrophy. N Engl J Med. 2018;378:625‐635. [DOI] [PubMed] [Google Scholar]
- 10. Darras BT, Chiriboga CA, Iannaccone ST, et al. Nusinersen in later‐onset spinal muscular atrophy: long‐term results from the phase 1/2 studies. Neurology. 2019;92:e2492‐e2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Finkel RS, Castro D, Farrar MA, et al. Nusinersen in infantile‐onset spinal muscular atrophy: longer‐term treatment results from the open‐label SHINE extension study. World Muscle Society Virtual Congress. Neuromuscul Disord. 2020;30:S124. [Google Scholar]
- 12. Finkel RS, Kirschner J, Mercuri E, et al. Longer‐term effects of nusinersen on motor function outcomes based on age at treatment initiation. World Muscle Society Virtual Congress. Neuromuscul Disord. 2020;30:S123‐S124. [Google Scholar]
- 13. Mercuri E, Darras BT, Chiriboga CA, et al. Longer‐term treatment with nusinersen: results in later‐onset spinal muscular atrophy from the SHINE study. World Muscle Society Virtual Congress. Neuromuscul Disord. 2020;30:S121. [Google Scholar]
- 14. Darras BT, Day JW, Swoboda KJ, et al. Nusinersen in adolescents and young adults with SMA: longitudinal experience from an expanded cohort of CS2/CS12 and SHINE participants. World Muscle Society Virtual Congress. Neuromuscul Disord. 2020;30:S120. [Google Scholar]
- 15. Castro D, Finkel RS, Tulinius M, et al. Integrated analysis of annualized incidence of serious adverse events in infantile‐onset SMA treated with nusinersen. 16th International Congress on Neuromuscular Diseases, 2021 May 21–22 & 28–29; Virtual meeting
- 16. Saito K, Castro D, Finkel RS, et al. Integrated analysis of incidence of serious adverse events in nusinersen‐treated later‐onset SMA. 63rd Annual Meeting of the Japanese Society of Child Neurology, 2021 May 27‐29; Fukuoka, Japan.
- 17. Darras BT, Crawford TO, Finkel RS, et al. Neurofilament as a potential biomarker for spinal muscular atrophy. Ann Clin Transl Neurol. 2019;6:932‐944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Darras BT, Farrar MA, Mercuri E, et al. An integrated safety analysis of infants and children with symptomatic spinal muscular atrophy (SMA) treated with nusinersen in seven clinical trials. CNS Drugs. 2019;33:919‐932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Farrar M, Castro D, Finkel R, et al. Longer‐term safety data in individuals with later‐onset SMA support the favourable tolerability profile of nusinersen. Eur J Neurol. 2021;28:287. [Google Scholar]
- 20. MacCannell D, Berger Z, East L, et al. Population pharmacokinetics‐based recommendations for a single delayed or missed dose of nusinersen. Neuromuscul Disord. 2021;31:310‐318. [DOI] [PubMed] [Google Scholar]
- 21. Dangouloff T, Servais L. Clinical evidence supporting early treatment of patients with spinal muscular atrophy: current perspectives. Ther Clin Risk Manag. 2019;15:1153‐1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Day JW, Swoboda KJ, Darras BT, et al. Longer‐term experience with nusinersen in teenagers and young adults with spinal muscular atrophy: results from the CS2/CS12 and SHINE studies. Neurology. 2020;94:1132. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Exposure response analysis of motor milestone response.
Figure S2. Median change from baseline in HFMSE total score associated with higher exposures (10–15 ng/mL) of nusinersen was twice that associated with lower exposures (0–5 ng/mL) of nusinersen in participants with later‐onset SMA.
Data Availability Statement
Requests for the data supporting this manuscript should be submitted to the Biogen Clinical Data Request Portal (www.biogenclinicaldatarequest.com).


