Abstract
Background:
We compared the outcomes of patients who performed physical therapy versus those who did not in a longitudinal cohort of patients undergoing nonoperative treatment of rotator cuff tears. We also assessed whether there was a dose effect in which the pain and functional outcomes in patients performing physical therapy plateaued.
Methods:
From February 2011 to June 2015, a multicenter cohort of patients with rotator cuff tears undergoing nonoperative treatment completed a detailed health and demographic questionnaire and the Shoulder Pain and Disability Index (SPADI) at baseline and 3, 6, 12, and 18 months. Longitudinal mixed models were used to assess whether physical therapy in the first 3 months predicted SPADI scores and dose effect.
Results:
Among the 55 patients in our cohort, the performance of physical therapy within the first 3 months predicted better SPADI scores versus nonperformance of physical therapy at 3 months (P = .02). Scores were similar between groups at 6, 12, and 18 months. A threshold of 16 physical therapy sessions was observed for pain and functional improvement during follow-up, after which significant improvement was not seen.
Conclusions:
Patients who performed physical therapy within the first 3 months had statistically significant improvements in pain and function as measured by the SPADI score at 3 months compared with patients who did not report performing physical therapy. Depending on the minimal clinically important difference used for the SPADI score, our results could be interpreted as meeting the minimal clinically important difference threshold or not. Improvement in outcomes was observed up to 16 sessions of physical therapy, after which outcomes plateaued.
Level of evidence:
Level III; Retrospective Cohort Comparison; Treatment Study
Keywords: Rotator cuff, nonoperative treatment, conservative treatment, rotator cuff tears, physical therapy, physiotherapy, dosing
Physical therapy is often the first line of treatment for patients with rotator cuff tears.1,6,7 Several studies have shown improvement in outcomes with physical therapy,1,6,7 whereas others have not shown improvement.8,10 Physical therapy can be cost-effective if it is benefitting patients and outcomes; however, it is debated whether the natural history of rotator cuff tears is such that patients become asymptomatic over time without treatment and, therefore, the addition of a physical therapy program may have no additional benefits. In addition, no studies in the literature have described optimal dosing of physical therapy for rotator cuff tears.
The objective of our study was to determine whether patients who participated in physical therapy had better pain and functional outcomes over an 18-month follow-up period than those who did not. We also assessed a “dose effect” of the number of physical therapy sessions to determine when improvement plateaued in this cohort of patients.
Materials and methods
Patient population
Patients with symptomatic rotator cuff tears scheduled for nonoperative treatment were recruited into a multicenter longitudinal study termed the Rotator Cuff Outcomes Workgroup (ROW). The eligibility criteria for the study included age of 45 years or older and the presence of symptoms including pain and decreased function for at least 4 weeks. Patients were recruited from sports or shoulder clinics in 3 academic settings and 1 community setting between February 2011 and June 2015. The exclusion criteria were a current shoulder fracture, prior shoulder surgery (on the index shoulder), and active cervical radiculopathy (elicited as neck pain radiating to the shoulder, arm, and/or hand). Patients provided informed consent.
Patients were followed up at approximately 3, 6, 12, and 18 months after completion of the baseline visit at the time of recruitment. Follow-up was performed via mail, and patients received phone or e-mail reminders if they did not return the questionnaires. Seventy patients met the eligibility criteria specified earlier and underwent nonoperative treatment. Of these, patients with missing information on one of the standardized questionnaires (n = 1) or who did not undergo follow-up at the 3-month time point (n = 14) were excluded. Thus, a total of 55 patients were included in this analysis.
Structured history and physical therapy questionnaire
Patients completed a structured shoulder and general health questionnaire at baseline. An abbreviated version of this questionnaire was completed by patients at each follow-up time point. The presence or absence of injury or trauma was determined by a physician from a description of the patient’s injury by self-report. Mental health was assessed using the Mental Health Inventory (MHI-5),2 a component of the 36-item Short Form Health Survey.18 MHI-5 scores range from 0 to 100. A score of 68 or less on the MHI-5 is indicative of a probable mood disorder (including depression).5,17 Psychological distress has been associated with increased pain and decreased function by self-reported scores in patients with rotator cuff tears.4
All patients were given orders for physical therapy at baseline. This physical therapy prescription usually provided instructions on rotator cuff strengthening, scapular stabilization, and stretching exercises that were recommended. Recommendations on the use of modalities such as electrical stimulation and ultrasound were also provided to the physical therapist. At 3 months of follow-up, patients were asked whether they underwent formal physical therapy for their shoulder problem in the past 3 months. Patients could respond by marking “yes” or “no.” Information on the number of physical therapy sessions and the total duration for which physical therapy was performed during these 3 months was also elicited.
Outcome measure
Patients completed shoulder pain and function questionnaires including the Shoulder Pain and Disability Index (SPADI),14 a standardized 13-item questionnaire, at baseline and follow-up. The SPADI has a pain scale (5 items) and disability scale (8 items) that elicit information on pain and functional limitations with activities of daily living, respectively. The composite SPADI score ranges from 0 to 100, with higher SPADI scores reflecting worse pain and function. If a patient was missing more than 2 items on the SPADI questionnaire, the SPADI score was assigned a missing value. The minimal clinically important difference (MCID) for the SPADI score has been reported to be 8, 10, and 13.2 points.15,19
Diagnostic imaging
Shoulder magnetic resonance imaging (MRI) scans were read in a blinded fashion by consensus by 2 shoulder experts (either L.D.H. and N.B.J. or J.E.K. and N.B.J.). Our previous work has shown good inter-rater and intrarater reliability for these MRI readings as compared with a musculoskeletal radiologist.3 The κ values ranged from 0.75 to 0.90 for tear presence, tear size, and tear thickness.3 MRI features including tear thickness, tear size in the longitudinal and transverse planes, fatty infiltration of the rotator cuff muscles, tendon retraction, and rotator cuff muscle atrophy were assessed. The criteria for each of these measurements followed standard nomenclature as previously described.3
Diagnosis of rotator cuff tear
Rotator cuff tears were diagnosed based on the clinical impression of a sports or shoulder fellowship–trained attending physician and evidence of structural deficit on MRI (when available). Both of these conditions had to be met for a patient to receive a diagnosis of a rotator cuff tear. If MRI was unavailable because it was not clinically indicated (n = 11), the diagnosis was based on the clinician’s impression based on the patient’s history and physical examination findings.
Statistical analysis
All analyses were conducted in the R programming environment (R Foundation for Statistical Computing, Vienna, Austria).13 Continuous variables were summarized using the median, 25th percentile, and 75th percentile, as well as the mean and standard deviation. Categorical variables were summarized as frequency counts and percentages. The SPADI score (lower is better) was analyzed over time using a mixed model with an autoregressive correlation structure for repeated measures.12 Separate models were developed for the association of physical therapy (yes or no) with the SPADI score and for the number of physical therapy sessions with the SPADI score. The effects of physical therapy and the number of sessions were estimated controlling for baseline SPADI score, patient age, MHI-5 score, and number of comorbidities. We used a restricted cubic spline with 3 knots to transform number of sessions as a predictor to account for an apparent nonlinear relationship between number of physical therapy sessions and SPADI score. Because the association of the SPADI score with performance of physical therapy or number of physical therapy sessions may not be linear with duration of follow-up, interactions of physical therapy and number of sessions by time were assessed with only baseline SPADI score as a supporting covariate. Predicted mean differences in average SPADI score between physical therapy groups (yes vs no) and between the interquartile range of number of sessions were estimated and tested using the lsmeans package in R (R Foundation for Statistical Computing).9 As noted, adjustments for multiple comparisons were made using the multivariate t distribution.
Results
Fifty-five patients in the Rotator Cuff Outcomes Workgroup (ROW) cohort underwent nonoperative treatment and had data at baseline and 3 months of follow-up. This included 18 patients (33%) who did not undergo physical therapy and 37 patients (67%) who underwent physical therapy within the first 3 months (Table I). The median number of physical therapy sessions attended by patients within the first 3 months was 8. Of the patients who reported having undergone physical therapy, 86% performed strengthening exercises, 76% performed stretching exercises, and 22% underwent use of modalities such as electrical stimulation and ultrasound during their physical therapy sessions. The median age of patients in the cohort was 65 years, 53% of patients (n = 29) were women, and 49 patients (91%) were white. Traumatic tears accounted for 42% of patients. No significant different between the 2 groups was found in their baseline SPADI scores.
Table I.
Summary of selected baseline demographic, disease, and treatment characteristics of patients undergoing nonoperative treatment of rotator cuff tears in ROW cohort
| Data | |
|---|---|
| Female patients | 53% (29) |
| Age, yr | 61/65/68 (64 + 8) |
| White patients | 91% (49) |
| MHI-5 score | 75/85/90 (79 + 16) |
| SPADI score at baseline, points | 27/40/57 (44 + 23) |
| No. of comorbidities | |
| ≤1 | 45% (25) |
| >1 | 55% (30) |
| Physical therapy at 3 mo | |
| No | 33% (18) |
| Yes | 67% (37) |
| Total No. of sessions at 3 mo | 0/8/17 (9 + 10) |
| Trauma | |
| No | 53% (29) |
| Yes | 42% (23) |
| Missing | 5% (3) |
ROW, Rotator Cuff Outcomes Workgroup; MHI-5, Mental Health Inventory; SPADI, Shoulder Pain and Disability Index.
The sample size was 55 patients for all data except total number of sessions at 3 months (n = 52). Continuous variables are presented as lower quartile/median/upper quartile (mean + standard deviation). Numbers after percentages are frequencies.
Physical therapy within the first 3 months was significantly associated with improved SPADI scores at follow-up (β = −10.96, standard error = 4.62, P = .021; Table II). When we adjusting for other covariates (follow-up duration, age, MHI-5 score, baseline SPADI score, and number of comorbidities), patients who underwent physical therapy within the first 3 months since enrollment had significantly improved SPADI scores, with a model-estimated average of 10.96 points lower (95% confidence interval, −20.0 to −1.91 points) compared with patients who did not undergo physical therapy (P = .02, Table II). When interactions with time were assessed, a larger significant effect size of the difference in the average SPADI score between the 2 groups was estimated at 3 months (mean SPADI score difference, −13.03 points; 95% confidence interval, −25.7 to −0.34 points; adjusted P = .043; Table III), with the differences between the 2 groups diminishing and not being statistically significant at 6, 12, and 18 months (Fig. 1).
Table II.
Relationship of physical therapy participation with SPADI score at 18 months’ follow-up in ROW cohort
| Estimate | Standard error | P value | |
|---|---|---|---|
| Intercept | 46.58 | 21.33 | .03* |
| 6-mo follow-up† | −3.89 | 2.48 | .12 |
| 12-mo follow-up† | −6.36 | 2.61 | .02* |
| 18-mo follow-up† | −10.61 | 1.92 | <.001* |
| Age | −0.35 | 0.30 | .25 |
| MHI-5 score | −0.06 | 0.14 | .67 |
| SPADI score at baseline | 0.53 | 0.10 | <.001* |
| No. of comorbidities | 0.23 | 4.67 | .96 |
| Participation in physical therapy‡ | −10.96 | 4.62 | .021* |
SPADI, Shoulder Pain and Disability Index; ROW, Rotator Cuff Outcomes Workgroup; MHI-5, Mental Health Inventory.
Statistically significant.
Approximate time frame.
Yes versus no.
Table III.
Mixed model–based mean differences in SPADI score between patients who participated in physical therapy within first 3 months and patients who did not by period in ROW cohort
| Period | Estimate | Lower 95% CI | Upper 95% CI | P value |
|---|---|---|---|---|
| 3 mo | −13.03 | −25.72 | −0.34 | .04 |
| 6 mo | −1.26 | −17.80 | 15.28 | >.99 |
| 12 mo | −4.34 | −20.33 | 11.66 | .89 |
| 18 mo | −11.59 | −24.80 | 1.61 | .10 |
SPADI, Shoulder Pain and Disability Index; ROW, Rotator Cuff Outcomes Workgroup; CI, confidence interval.
P values were adjusted using the multivariate t distribution. The mixed model included baseline SPADI score, time, categorical physical therapy (yes vs no), and interaction between physical therapy and time.
Figure 1.
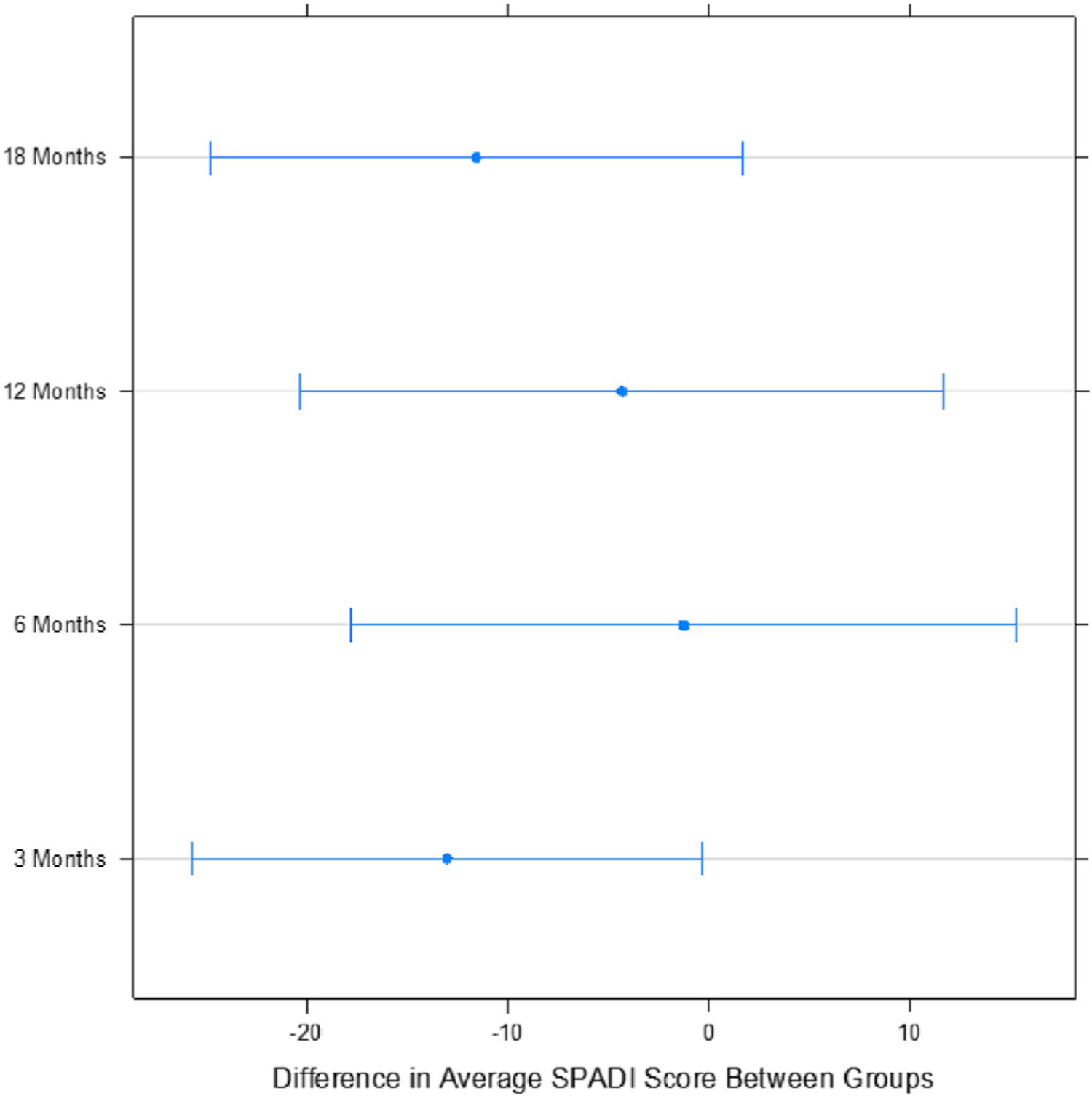
Predicted differences in average Shoulder Pain and Disability Index (SPADI) score between patients who reported performing physical therapy and patients who reported not performing physical therapy in first 3 months during 18 months of follow-up.
When adjusted for other covariates, the relationship between the number of physical therapy sessions and the SPADI score was concave over the follow-up period. The SPADI score decreased linearly by 1.99 points (standard error = 0.64, P = .003; Table IV) for every physical therapy session until the 16th session. Subsequently, a slight increase in SPADI scores occurred with each additional physical therapy session. Figure 2 shows that the decrease in SPADI scores plateaued at approximately 16 physical therapy sessions.
Table IV.
Relationship of number of physical therapy sessions with SPADI score at 18 months’ follow-up in ROW cohort
| Estimate | Standard error | P value | |
|---|---|---|---|
| Intercept | 47.19 | 19.84 | .02* |
| 6-mo follow-up† | −4.60 | 2.69 | .09 |
| 12-mo follow-up† | −7.16 | 2.87 | .01* |
| 18-mo follow-up† | −11.60 | 2.09 | <.001* |
| Age | −0.30 | 0.28 | .30 |
| MHI-5 score | −0.05 | 0.13 | .71 |
| SPADI score at baseline | 0.45 | 0.09 | <.001* |
| No. of comorbidities | 0.66 | 4.23 | .88 |
| No. of PT sessions‡ | |||
| First set | −1.99 | 0.64 | .003* |
| Second set | 1.42 | 0.63 | .03* |
SPADI, Shoulder Pain and Disability Index; ROW, Rotator Cuff Outcomes Workgroup; MHI-5, Mental Health Inventory; PT, physical therapy. A higher SPADI score represents worse shoulder pain and function.
Statistically significant.
Approximate time frame.
The relationship of the number of PT sessions to the SPADI score was not linear. The first set represents the initial decrease in SPADI scores with an increasing number of PT sessions. The second set represents the subsequent increase in SPADI scores with additional PT sessions after the first set.
Figure 2.
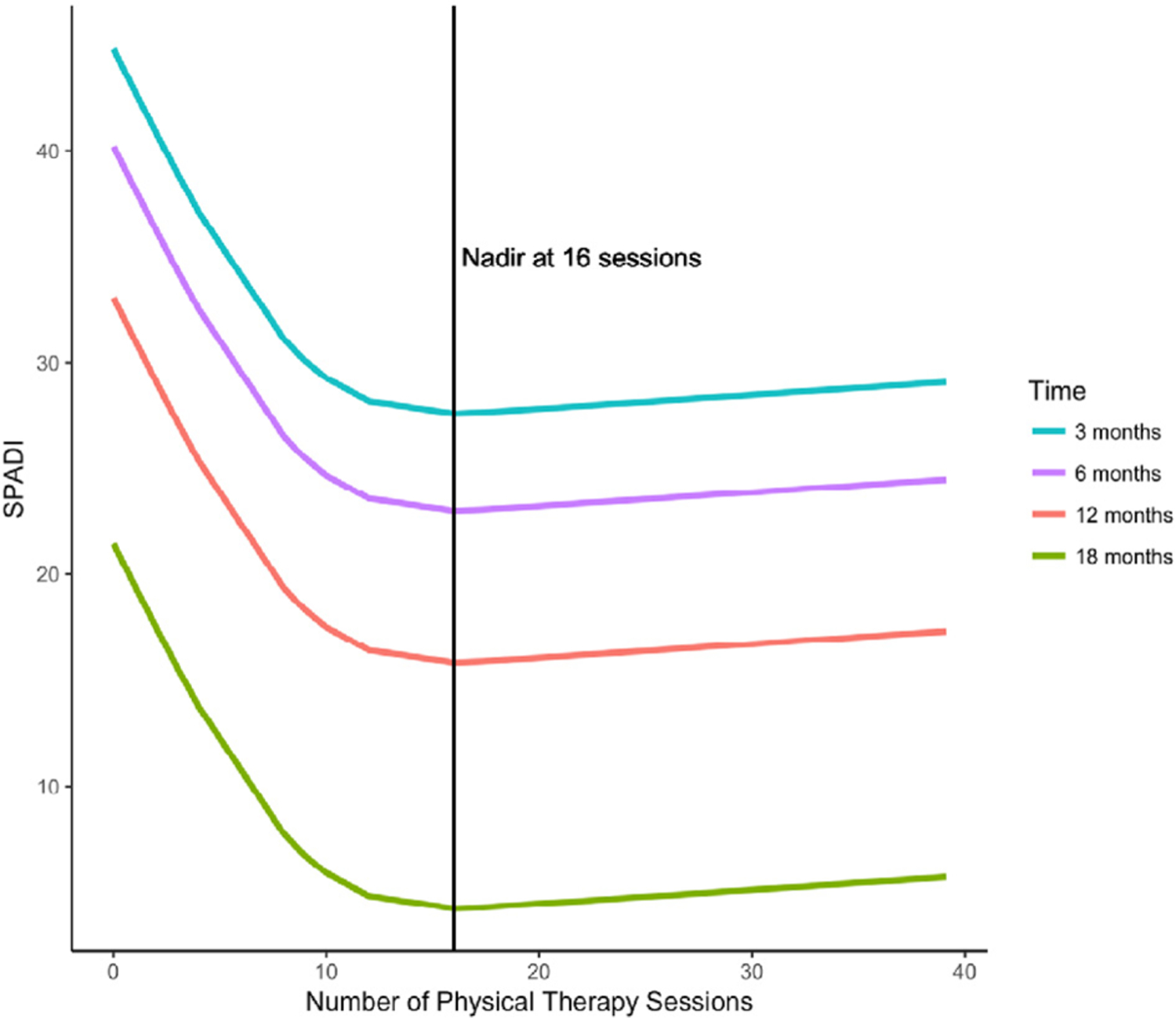
Relationship between number of physical therapy sessions and Shoulder Pain and Disability Index (SPADI) score during 18 months of follow-up.
Discussion
In a cohort of 55 patients who were followed up longitudinally after undergoing nonoperative treatment of rotator cuff tears, we found that, compared with patients who did not perform physical therapy, patients who did perform physical therapy within the first 3 months had significantly better shoulder pain and function as measured by the SPADI score during follow-up. Most of this improvement occurred during the first 3 months of follow-up. However, depending on the MCID for the SPADI score used to interpret the clinical significance of our results, the difference between the groups may be clinically meaningful or not. If we used the highest value of the MCID of 13.2 points, the differences between the 2 groups would not meet the MCID threshold. We also found that improvement in shoulder pain and function plateaued after approximately 16 physical therapy sessions. Subsequently, a slight worsening of shoulder pain and function occurred with additional physical therapy sessions.
Prior literature reviews on physical therapy to treat rotator cuff tears have shown mixed results. A recent Cochrane review of 60 trials found 1 high-quality study that showed no clinically important difference in manual therapy and exercise over placebo.11 Bennell et al1 performed a randomized trial in 120 participants. Manual therapy and home exercise were compared with placebo. No differences between the 2 groups were noted at 11 weeks, but significant improvements in the SPADI score in the manual therapy and exercise group over placebo were observed at 22 weeks.1 In a cohort of 452 patients with atraumatic full-thickness rotator cuff tears, Kuhn et al6 found that approximately 75% of patients improved with physical therapy at 2 years of follow-up and did not require surgical intervention. Tanaka et al16 followed 123 shoulders treated conservatively, of which 65 had improvements in symptoms and 58 underwent surgery. In our cohort, patients who underwent physical therapy within the first 3 months had significantly improved outcomes during follow-up, but it is questionable whether this is clinically significant depending on the MCID for the SPADI score used to interpret our results. An interaction with duration of follow-up was also found, in which most of the benefit was seen in the first 3 months of follow-up. After this point, the 2 groups had similar SPADI scores. Although we cannot ascertain the reasons for this, it is possible that patients who did not undergo physical therapy within the first 3 months went on to undergo physical therapy after this point and therefore had delayed improvement in outcomes. It is also possible that this is the natural history but there are benefits to physical therapy returning patients to work and activity faster. The MHI-5 score was not significantly associated with the SPADI score in our study. However, prior work has shown that mental health is associated with outcomes of physical therapy.4
The threshold for the number of physical therapy sessions for optimal improvement is an important issue for patients, clinicians, and payers. However, data on this issue are sparse. In the aforementioned study by Bennell et al,1 patients in the manual therapy and exercise group and placebo group were seen for 10 visits, with improvements in SPADI scores in the therapy group at 22 weeks, but this study did not report on the optimal number of physical therapy sessions. Our analysis found that outcome improvement plateaus at 16 physical therapy sessions, with a slight worsening in outcomes after 16 sessions. The worsening of outcomes after 16 sessions may be attributed to selection bias in our cohort in which patients with worse or persistent symptoms may have continued to perform physical therapy after 16 visits. This issue needs further assessment.
Limitations of our study include a relatively smaller cohort of 55 patients and limited ability to control for more variables. However, data from our analysis are valuable and can be used to confirm our findings in a larger cohort of patients or clinical trial. Complete data for all patients at each of our outcome time points were not available. We were unable to independently verify patient-reported data on physical therapy with actual medical records. We were also unable to report specifics of the physical therapy interventions including the duration of sessions and the home exercises given.
Conclusion
In a longitudinal cohort of patients with rotator cuff tears followed up for 18 months, we found that patients who performed physical therapy within the first 3 months had statistically significant improvements in pain and function as measured by the SPADI score at 3 months compared with patients who did not report performing physical therapy. Depending on the MCID used for the SPADI score, our results could be interpreted as meeting the MCID threshold or not in the first 3 months. Improvement in outcomes was observed up to 16 sessions of physical therapy, after which outcomes plateaued. Given the sample size of our cohort, these findings are preliminary and should be confirmed in larger studies and ideally in a randomized controlled trial study design.
Acknowledgment
We thank the entire Rotator Cuff Outcomes Workgroup (ROW) team for their efforts. We also thank our clinical staff at the Orthopedic and Arthritis Center at Brigham and Women’s Hospital, Shoulder Service at Massachusetts General Hospital, and clinical staff at Vanderbilt Orthopaedic Institute for their efforts and cooperation.
Disclaimer
The project described was supported by Clinical and Translational Science Awards (CTSA) award number UL1TR000445 from the National Center for Advancing Translational Sciences.
Nitin B. Jain was supported by funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (1K23AR059199 and 1U34AR069201).
Cristina Page was funded by the Rehabilitation Research Experience for Medical Students program for this study.
Laurence D. Higgins received educational funds from Arthrex and Ethicon.
Keith M. Baumgarten received consulting fees from Wright Medical and educational funds from Arthrex.
Elizabeth Matzkin received educational funds from Smith & Nephew (2014) and Nuvasive (2016).
The other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was received from Partners Human Research Committee (protocol No. 2009-P-000329/43; BWH) and Vanderbilt University Institutional Review Board (No. 140857).
References
- 1.Bennell K, Wee E, Coburn S, Green S, Harris A, Staples M, et al. Efficacy of standardised manual therapy and home exercise programme for chronic rotator cuff disease: randomised placebo controlled trial. BMJ 2010;340:c2756. 10.1136/bmj.c2756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berwick DM, Murphy JM, Goldman PA, Ware JE, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care 1991;29:169–76. [DOI] [PubMed] [Google Scholar]
- 3.Jain NB, Collins J, Newman JS, Katz JN, Losina E, Higgins LD. Reliability of magnetic resonance imaging assessment of rotator cuff: the ROW study. PM R 2015;7:245–54.e3. 10.1016/j.pmrj.2014.08.949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karels CH, Bierma-Zeinstra SM, Burdorf A, Verhagen AP, Nauta AP, Koes BW. Social and psychological factors influenced the course of arm, neck and shoulder complaints. J Clin Epidemiol 2007;60:839–48. 10.1016/j.jclinepi.2006.11.012 [DOI] [PubMed] [Google Scholar]
- 5.Kelly MJ, Dunstan FD, Lloyd K, Fone DL. Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: a comparison of five different methods. BMC Psychiatry 2008;8:10. 10.1186/1471-244x-8-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuhn JE, Dunn WR, Sanders R, An Q, Baumgarten KM, Bishop JY, et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg 2013;22:1371–9. 10.1016/j.jse.2013.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kukkonen J, Joukainen A, Lehtinen J, Mattila KT, Tuominen EK, Kauko T, et al. Treatment of nontraumatic rotator cuff tears: a randomized controlled trial with two years of clinical and imaging follow-up. J Bone Joint Surg Am 2015;97:1729–37. 10.2106/jbjs.n.01051 [DOI] [PubMed] [Google Scholar]
- 8.Lambers Heerspink FO, van Raay JJ, Koorevaar RC, Eerden PJV, Westerbeek RE, van’t Riet E, et al. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. J Shoulder Elbow Surg 2015;24:1274–81. 10.1016/j.jse.2015.05.040 [DOI] [PubMed] [Google Scholar]
- 9.Lenth RV. Least-squares means: the R package lsmeans. J Statist Softw 2016;69. 10.18637/jss.v069.i01 [DOI] [Google Scholar]
- 10.Moosmayer S, Lund G, Seljom US, Haldorsen B, Svege IC, Hennig T, et al. Tendon repair compared with physiotherapy in the treatment of rotator cuff tears. J Bone Joint Surg Am 2014;96:1504–14. 10.2106/jbjs.m.01393 [DOI] [PubMed] [Google Scholar]
- 11.Page MJ, Green S, McBain B, Surace SJ, Deitch J, Lyttle N, et al. Manual therapy and exercise for rotator cuff disease. Cochrane Database Syst Rev 2016;(6):CD012224. 10.1002/14651858.CD012224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pinheiro J, Bates D, DebRoy S, Sarkar D, R Core Team_nlme. Linear and nonlinear mixed effects models. R package version 3.1–131, <https://CRAN.R-project.org/package=nlme>; Accessed January 2018. [Google Scholar]
- 13.R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, <https://www.R-project.org/>; 2017. [Google Scholar]
- 14.Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res 1991;4:143–9. [PubMed] [Google Scholar]
- 15.Schmitt JS, Di Fabio RP. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J Clin Epidemiol 2004;57:1008–18. 10.1016/j.jclinepi.2004.02.007 [DOI] [PubMed] [Google Scholar]
- 16.Tanaka M, Itoi E, Sato K, Hamada J, Hitachi S, Tojo Y, et al. Factors related to successful outcome of conservative treatment for rotator cuff tears. Ups J Med Sci 2010;115:193–200. 10.3109/03009734.2010.493246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thorsen SV, Rugulies R, Hjarsbech PU, Bjorner JB. The predictive value of mental health for long-term sickness absence: the Major Depression Inventory (MDI) and the Mental Health Inventory (MHI-5) compared. BMC Med Res Methodol 2013;13:115. 10.1186/1471-2288-13-115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ware JE, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 19.Williams JW, Holleman DR, Simel DL. Measuring shoulder function with the Shoulder Pain and Disability Index. J Rheumatol 1995;22:727–32. [PubMed] [Google Scholar]


