Abstract
Background
The lack of racial and ethnic concordance between patients and their physicians may contribute to American health disparities.
Objective
To examine the level of racial and ethnic concordance for patients and primary care clinicians and its association with measures of patient experience.
Design
Multivariate cross-sectional analysis of nationally representative data.
Participants
Adults 18 to 64 in the 2019 Medical Expenditure Panel Survey who had at least one medical visit in the past year.
Main Measures
Key independent variables include having a racially/ethnically concordant primary care clinician, lacking a usual source of care, and having a usual source that is a place rather than a person. Outcomes include overall satisfaction with health care, number of medical visits, having enough time in care, ease of understanding the clinician, and receiving respect.
Key Results
The comparison between the actual level of concordance with an expected distribution if all patients had the same probability of having a clinician of a given race or type indicates that Black, Latino, and Asian patients are three or more times as likely to have a concordant clinician than expected, suggesting a strong preference for clinicians of the same race or ethnicity. Racial or ethnic concordance has a modest positive association with overall health care satisfaction and respect but is not significantly associated with the number of medical visits or other outcomes. Poor health status, being uninsured, and lacking a usual source of care are more strongly associated with patient experience.
Discussion
Efforts to increase the diversity of the primary care workforce could increase racial/ethnic concordance but may have only modest effects on patients’ experience of care. Policies like lowering the number of uninsured or increasing those with a usual source of care may be more salient in improving experience of care.
KEY WORDS: racial/ethnic concordance, primary care clinician, racial equity, insurance
INTRODUCTION
The problems of racial and ethnic inequities in American health care and the role of structural racism are well documented.1–4 Racial and ethnic minorities, particularly Black patients, often receive lower quality of care and have worse outcomes than similar White patients. A portion of these racial inequities may be explained by financial, social, and cultural factors, but racial/ethnic differences persist. One factor that is sometimes mentioned as a possible contributor is the relatively low proportion of Black or Latino physicians in the American health workforce,5,6 which increases the likelihood that Black and Latino patients lack physicians of the same race or ethnicity. The racial and ethnic discordance between patients and physicians could harm the quality of care received.7
Racial concordance, which occurs when a patient and clinician have the same race or ethnicity, can generate a shared identity which may facilitate trust and improve other dimensions of patient-physician relationships including communication and patient involvement in shared decision-making.8,9 Prior research has found that racial concordance can influence a patient’s decision to seek care from a clinician, the likelihood of visiting their clinician for preventive care, satisfaction with the care received, and more distal health care outcomes.10–13
However, recent systematic reviews examining literature to better understand the effects of race and racial concordance on patient-centered outcomes have revealed mixed results. A 2009 review of the literature by Meghani and colleagues focused on the role of racial concordance on health outcomes broadly and found no clear pattern for the effect of racial concordance.14 In a 2018 review, Shen et al. concluded that racial concordance was more clearly associated with better communication across all domains except quality, for which there was no effect.15 The reviews suggested that measurement error and reporting biases may explain the lack of clarity and inconsistency of the findings. Another study evaluated the association between racial/ethnic concordance and health care utilization using a multi-dimensional approach with a variety of supply-side and demand-side barriers but focused on coverage expansions. In particular, the results suggested that while racial concordance remains a significant factor, it accounted for a small share of the decision to seek medical treatment when financial barriers to health services were reduced.16
The aims of this study are three-fold. First, we use nationally representative data (the 2019 Medical Expenditure Panel Survey) to determine which patients report a racially concordant primary care clinician as well as the share who lack an individual primary care clinician because they lack a usual source of care or because the usual source is a facility (e.g., a clinic or center) rather than an individual. Second, we measure how these patterns indicate a preference for same race/ethnicity clinicians by comparing the actual distribution versus the expected distribution if all patients had the same probability of having a clinician of a given race or type. Third, we estimate the influence of racial/ethnic concordance on several measures of patient experience and the role of other social and health factors, such as insurance coverage, health status, education, or income. Our results can further inform the research on racial concordance by critically assessing its role on health care outcomes and provide evidence on the contextual factors that might influence outcomes in the presence of racial concordance.
METHODS AND DATA
Our data are drawn from the 2019 Medical Expenditure Panel Survey (MEPS), a nationally representative household survey conducted by the Agency for Healthcare Research and Quality; it was collected before the COVID-19 pandemic. The survey asks whether a respondent has a usual source of health care (i.e., a primary care clinician) and, if so, whether that clinician is a person, a person within a facility, or a facility (e.g., a clinic or hospital). When the clinicians are individuals, their race/ethnicity (White non-Hispanic, Black non-Hispanic, Latino, Asian non-Hispanic, or other/multi-race) is reported by the survey respondent, but in many cases an individual primary care clinician was not identified because the respondent lacked a usual source of care, or the source was a facility. The individual primary care clinicians identified are mostly physicians but could also be nurse practitioners or other primary care clinicians.
This analysis is limited to 10,858 adults aged 18 to 64 who reported at least one medical visit in the past 12 months. For each patient, we recorded the race/ethnicity of the patient and primary care clinician. If the patient was White, Black, Latino, or Asian, we recorded whether the primary care clinician was concordant (concordance was not determined for those who are other/multi-race). We also identified respondents who lacked a usual source of care or whose usual source of care was a facility rather than an individual.
A self-administered questionnaire asked about five outcomes examined in this analysis: (1) the respondent’s overall satisfaction with health care (“Using any number from 0 to 10, where 0 is the worst health care possible and 10 is the best health care possible, what number would you use to rate all your health care in the last 12 months?”), (2) the number of medical visits in the year, (3) whether the clinician was easy to understand, (4) whether enough time was spent with the patient, and (5) whether the clinician showed respect.
Multivariate analyses controlled for the respondent’s age, gender, race/ethnicity, racial/ethnic concordance, type of health insurance (private, public, or uninsured), self-reported health and mental health status (fair/poor vs. excellent/very good/good) and the presence of functional limitations, years of education, and income/poverty category. We also examined the role of gender concordance, but this was generally not significant, so those results are not shown. Our criterion for statistical significance was p < .05 (two-tailed). All analyses incorporated survey weights and survey design adjustments. Because we analyzed de-identified secondary data, this study was exempt from human subjects review.
Limitations
The analyses are based on cross-sectional associations and do not demonstrate causality. Second, the data are self-reported and may be subject to misreporting. In particular, patients might not be accurate in describing the race or ethnicity of their clinicians. On the other hand, the patient’s perception of clinician identity may be more salient to patient experience than actual status. In this analysis, we examine concordance based on whether the respondent reports having an individual primary care clinician, as opposed to those without a usual source of care or without an individual clinician at a clinic. These patients’ experiences may be shaped by the clinicians who happen to provide care, even if they are not their regular doctor, as well as being shaped by specialists or other health care staff. Finally, the race of clinicians is limited by the available supply; e.g., a Black patient cannot select a Black physician if none practices at the patients’ clinic.
RESULTS
Table 1 shows that about one-third (33.7%) of patients report having a primary care clinician who shares the same race/ethnicity (concordant), 19.3% have discordant clinicians, 25.0% lack a usual source of care, and 22.0% have a usual source that is a facility, not an individual clinician. White patients are the most likely to have a same race clinician (46%), but that is largely because White clinicians are the most frequent. Latino and Black patients are less likely to have concordant clinicians (11% each), while 20% of Asian patients have a concordant clinician. A majority of Latino, Black, and Asian patients lack a specific primary care clinician, as do about two-fifths of White patients.
Table 1.
Patient and Clinician Racial/Ethnic Concordance and Primary Clinician Type
| Patient’s race/ethnicity | Primary care clinician concordance status | |||
|---|---|---|---|---|
| Concordant race/ethnicity | Not concordant | No usual source of care | Source is a facility | |
| Percent within race group | ||||
| White non-Hispanic | 46.0 | 11.9 | 21.7 | 20.4 |
| Black non-Hispanic | 11.2 | 35.7 | 28.9 | 24.2 |
| Latino | 11.2 | 29.1 | 33.9 | 25.8 |
| Asian non-Hispanic | 20.6 | 24.9 | 29.1 | 25.4 |
| Other/multi-race | 0.0 | 52.0 | 25.7 | 22.3 |
| Total | 33.7 | 19.3 | 25.0 | 22.0 |
Source: 2019 Medical Expenditure Panel Survey (n = 10,838)
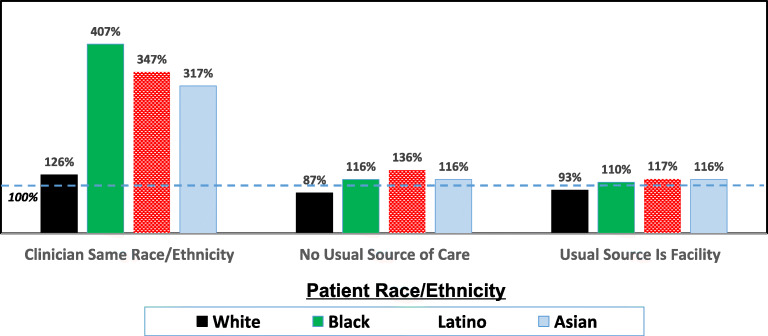
Figure 1 presents these data from a different perspective, seeking to assess patients’ preferences by examining the ratio of the observed level of concordance with the expected level if the distribution of clinicians was uniform nationally. The expected level is based on the weighted national average distribution of clinicians in the MEPS data: overall, 36.7% of patients report a White clinician, 3.2% Latino, 2.8% Black, 6.5% Asian, and 3.9 other/multi-race, while 25.0% have no usual source of care and 22.0% report a facility, not an individual clinician. If there was no relationship between patient and clinician race/ethnicity, then every patient would have a 2.8% probability of having a Black primary care clinician. But if the observed level for Black patients is that 8.4% have a Black clinician, then concordance for Black patients is three times higher than expected if the distribution was uniform.
Fig. 1.
Ratio of observed to expected racial/ethnic concordance of patient and primary care clinician and primary clinician type. Source: 2019 Medical Expenditure Panel Survey.
Figure 1 illustrates the ratio of the observed to expected concordance and type of clinician. Latino, Black, and Asian patients are three to four times more likely to have a racially concordant clinician than expected if the distribution was uniform, while White non-Hispanic patients are 26% more likely to have a White clinician than expected. Figure 1 also shows that Latino, Black, and Asian patients are more likely than White patients to lack a usual source of care or to have a facility (e.g., a clinic) as their usual source rather than an individual clinician.
Table 2 presents results of multivariate analyses of factors associated with overall satisfaction with health care and the number of medical appointments. Using ordinary least squares regression, racial/ethnic concordance is associated with a small but significant increase in satisfaction (.165 out of a 10-point scale), compared to having a non-concordant clinician. But other factors, including being in fair/poor health or mental health, having functional limitations, being uninsured, being older, and being Latino, were more important factors associated with satisfaction. (To assess importance, we computed standardized coefficients in which each independent variable is divided by its standard deviation and examined the factors with the largest beta scores.) Having no usual source of care or having a facility as the usual source was not significantly different than non-concordance. (An alternative analysis tested an ordered logistic regression model and the results were mostly the same as the main model, but racial concordance had an odds ratio of 1.15 but was marginally significant, p = 0.057.)
Table 2.
Association of Patients’ Race, Concordance, and Other Factors on Satisfaction with Health Care and Number of Medical Visits in Last Year
| Rating of health care (0 to 10) | Number of medical visits | |||
|---|---|---|---|---|
| Coeff. | 95% conf. intvl. | Odds ratio | 95% conf. intvl. | |
| Patient race/ethnicity (ref = white non-hisp) | ||||
| Latino | 0.360 | 0.204–0.516 | 0.799 | 0.687–0.928 |
| Black | 0.209 | 0.057–0.362 | 0.764 | 0.655–0.890 |
| Asian | 0.005 | −0.214 to 0.224 | 0.789 | 0.628–0.991 |
| Other/multi-race | −0.006 | −0.311 to 0.300 | 0.958 | 0.730–1.258 |
| Clinician racial/ethnic concordance (ref = not concordant) | ||||
| Concordant | 0.165 | 0.032–0.298 | 0.946 | 0.812–1.102 |
| No usual source | −0.059 | −0.213 to 0.095 | 0.561 | 0.475–0.664 |
| Source is facility | 0.025 | −0.112 to 0.162 | 0.737 | 0.632–0.859 |
| Insurance coverage (ref = private insurance) | ||||
| Public insurance | 0.078 | −0.102 to 0.258 | 0.993 | 0.851–1.159 |
| Uninsured | −0.500 | −0.824 to −0.176 | 0.428 | 0.339–0.540 |
| Health measures | ||||
| Fair/poor health | −0.639 | −0.819 to −0.458 | 2.090 | 1.810–2.412 |
| Fair/poor mental health | −0.376 | −0.556 to −0.195 | 2.166 | 1.880–2.495 |
| Have any limitations | −0.310 | −0.467 to −0.153 | 1.522 | 1.285–1.801 |
| Demographic traits | ||||
| Age (in years) | 0.009 | 0.005–0.013 | 1.007 | 1.003–1.011 |
| Female (vs. male) | 0.117 | 0.033–0.201 | 1.579 | 1.441–1.731 |
| Education (in years) | 0.008 | −0.010 to 0.026 | 1.031 | 1.013–1.049 |
| Income category (ref = below poverty) | ||||
| 100–124% of poverty | −0.088 | −0.361 to 0.185 | 0.820 | 0.619–1.087 |
| 125–199% of poverty | −0.001 | −0.237 to 0.236 | 0.748 | 0.614–0.911 |
| 200–399% of poverty | 0.118 | −0.092 to 0.327 | 0.770 | 0.623–0.952 |
| 400% or more | 0.170 | −0.048 to 0.388 | 0.868 | 0.698–1.079 |
Note: Bold marks p < .05
The number of medical visits was associated with lacking a usual source of care, having a facility for the source, and being uninsured, as were being Latino or being Black Racial/ethnic, but racial concordance was not significantly related. Measures of poorer health were associated with more medical visits. (MEPS uses grouped categories for those with 5 to 9 visits and 10 or more visits, so ordered logistic regression models were used; all our analyses exclude those with no medical visits in the last year.)
Table 3 presents results from logistic regression models of factors associated with having enough time with the clinician, whether the clinician was easy to understand, and whether the clinician showed respect (all categorized as usually/always vs. never/sometimes). Racial/ethnic concordance was associated with higher levels of respect, as were being Hispanic or Black (vs. White). Lacking a usual source of care was associated with less respect, as were having worse health, mental health, or having functional limitations. For ease of understanding, Latino and Black patients, the uninsured, and those with worse mental health reported greater difficulties understanding their clinicians; the concordance variables were not significantly related. For having enough time, being uninsured, lacking a usual source of care, and having poorer mental or physical health status or functional limitations were associated with less time, but being Black was associated with more time.
Table 3.
Association of Patients’ Race, Concordance, and Other Factors on Satisfaction with Having Enough Time with Clinicians, Clinician Being Easy to Understand, and Showing Respect
| Enough time (usually/always) | Easy to understand (usually/always) | Respect (usually/always) | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% conf. intvl. | Odds ratio | 95% conf. intvl. | Odds ratio | 95% conf. intvl. | |
| Patient race/ethnicity (ref = white non-hisp) | ||||||
| Latino | 1.232 | 0.943–1.609 | 0.619 | 0.431–0.890 | 1.475 | 1.092–1.992 |
| Black | 1.325 | 1.026–1.712 | 0.477 | 0.318–0.716 | 1.805 | 1.274–2.557 |
| Asian | 1.083 | 0.725–1.618 | 0.565 | 0.310–1.027 | 1.364 | 0.888–2.095 |
| Other/multi-race | 0.953 | 0.609–1.492 | 0.870 | 0.414–1.827 | 1.190 | 0.686–2.063 |
| Clinician racial/ethnic concordance (ref = not concordant) | ||||||
| Concordant | 1.150 | 0.889–1.489 | 1.313 | 0.899–1.918 | 1.368 | 1.002–1.868 |
| No usual source | 0.653 | 0.526–0.810 | 0.756 | 0.485–1.181 | 0.745 | 0.566–0.980 |
| Source is facility | 0.829 | 0.661–1.039 | 0.744 | 0.490–1.131 | 0.968 | 0.742–1.262 |
| Insurance coverage (ref = private insurance) | ||||||
| Public insurance | 0.973 | 0.749–1.264 | 0.791 | 0.553–1.133 | 0.768 | 0.555–1.062 |
| Uninsured | 0.646 | 0.437–0.956 | 0.416 | 0.256–0.677 | 0.647 | 0.399–1.050 |
| Health measures | ||||||
| Fair/poor health | 0.638 | 0.498–0.819 | 0.673 | 0.453–1.001 | 0.590 | 0.435–0.800 |
| Fair/poor mental health | 0.608 | 0.488–0.758 | 0.503 | 0.352–0.719 | 0.702 | 0.533–0.925 |
| Have any limitations | 0.798 | 0.643–0.991 | 0.924 | 0.645–1.324 | 0.662 | 0.514–0.852 |
| Demographic traits | ||||||
| Age (in years) | 1.009 | 1.002–1.016 | 0.998 | 0.987–1.010 | 1.005 | 0.996–1.014 |
| Female (vs. male) | 1.060 | 0.914–1.228 | 1.057 | 0.821–1.361 | 0.958 | 0.803–1.143 |
| Education (in years) | 1.001 | 0.968–1.035 | 1.067 | 1.022–1.115 | 1.018 | 0.978–1.058 |
| Income category (ref = below poverty) | ||||||
| 100–124% of poverty | 1.384 | 0.924–2.072 | 1.000 | 0.561–1.783 | 1.176 | 0.710–1.949 |
| 125–199% of poverty | 0.997 | 0.725–1.371 | 1.224 | 0.764–1.961 | 1.140 | 0.781–1.663 |
| 200–399% of poverty | 1.139 | 0.864–1.503 | 1.284 | 0.862–1.912 | 1.039 | 0.740–1.461 |
| 400% or more | 1.280 | 0.946–1.732 | 1.795 | 1.107–2.908 | 1.288 | 0.869–1.908 |
Note: Bold marks p < .05
DISCUSSION
This study, using a nationally representative sample of non-elderly adults, indicates that while having a primary care clinician who is the same race or ethnicity as the patient matters to many, almost half of patients do not have a regular primary care clinician because they lack a usual source of care or have a usual place for care, but not a specific clinician. Among those who have an individual primary care clinician, White patients are the most likely to have a same race clinician (46%), substantially more than for Black, Latino, or Asian patients (11 to 20%). But much of the reason for this is that far more primary care clinicians (mostly physicians) are White.
We also examined the ratio of observed concordance to the expected level, if every patient had the same probability of having a White, Black, Latino, or Asian clinician. The ratio was more than three times higher than expected for Black, Latino, and Asian patients and over 100% for White patients as well. This indicates there is a substantial level of “affinity bias”—preferring people like yourself—in the selection of health care clinicians. There may be many reasons for these preferences: a belief that a clinician with the same racial/ethnic background can better understand your needs, can communicate better, is more trustworthy, or is less likely to discriminate against you. In some cases, especially for Latinos and Asians, concordance can increase the probability that the patient and clinician speak the same language, although this is not always the case (e.g., an Asian doctor from India probably does not speak Korean). It is important to remember, however, that concordance or non-concordance is not necessarily caused by explicit choices about particular clinicians. If, for example, Latino patients go to clinic in a heavily Hispanic area, they may be more likely to have Latino clinicians simply because of the clinic’s location. Conversely, if Black patients get care from a clinic with no or few Black clinicians, the risk of non-concordance rises regardless of whether they would prefer a Black physician. Finally, a large share of patients, including a majority of Black, Latino, and Asian patients, lack individual primary care clinicians because they lack a usual source of care or their usual source is a facility, rather than a person.
In multivariate models that examined the association of concordance with patient experience, we found no significant association of racial concordance with the number of medical visits, ease of understanding the clinician, or having enough time for care. Associations with overall health satisfaction and respect were modest in magnitude, even if they were statistically significant. For example, with a 10-point scale of satisfaction, racial concordance was associated with a 0.17-point increase. These findings are consistent with prior reviews that found mixed evidence of the association of concordance with patient experience or outcomes.17,18
Other factors are often more important in associations with the outcomes measured. In particular, health measures such as the patient’s self-reported overall health, mental health, and the presence of functional limitations were strongly related to patients’ experience. Those with worse health consistently reported significantly receiving more medical visits and having lower levels of satisfaction, having enough time in care, or getting adequate respect. Patients in poorer health demand more care but are less happy with the care they receive; these are among the most influential factors in patient experience.
Patients who are uninsured are significantly less satisfied, get less time in appointments, have more difficulty understanding their clinician, and perceive less respect; they also have fewer medical visits. Being uninsured is more strongly associated with patient experience than racial concordance. Of policy significance, we found no significant differences in patient experience between those with public insurance (mostly Medicaid) and private health insurance coverage.
Patients who lack a usual source of care have fewer medical visits, do not get enough time for care, or have less respect from their clinicians. The effect is less clear when a person lists a facility as the clinician, rather than an individual clinician. Some health clinics do not assign regular primary care clinicians to patients, particularly uninsured or walk-in patients, or may assign patients to “care teams” rather than to individual clinicians. Patient experience did not differ significantly from having a non-concordant clinician, although those without an individual clinician had fewer visits. In principle, we might expect that the lack of an individual primary care clinician may lead to weaker continuity of care or fewer bonds of trust; more research might be needed to understand the significance of a regular place vs. a regular clinician for care. A 2002 study found that having a specific regular doctor was more important than having a usual place for care in promoting preventive care services.17
Independent of patient-clinician racial concordance and other factors, the patient’s race or ethnicity was often associated with outcomes. Black and Latino patients reported greater satisfaction and respect than White patients but had fewer medical visits and described more problems understanding their clinicians. Even after controlling for racial concordance and several health and socioeconomic factors, race and ethnicity still played a role.
In conclusion, the findings from this analysis indicate that patients often prefer racially concordant primary care clinicians, but concordance has only modest associations with health care satisfaction or perceived respect, and it is not significantly associated with the number of medical visits or other outcomes. Being uninsured or lacking a usual source of care tends to have stronger influences on patient experience and access to care. Other research has demonstrated that Medicaid expansions have increased insurance coverage and reduced racial disparities in insurance coverage18,19 and that adults with Medicaid generally have a usual source of care.20 From a policy perspective, Medicaid expansion remains an important strategy to reduce racial gaps in coverage and improve access to care and patient experience in the twelve states that have not yet expanded Medicaid.
Disparities exist in the racial and ethnic composition of the health care workforce, including physicians, nurse practitioners, and physician assistants, who are the core of primary care clinicians.6,7 Policies to increase the diversity of the health care workforce and to ensure that diverse clinicians are in practices used by minority patients can help improve racial/ethnic concordance. But these analyses suggest that other policies, such as reducing the number of uninsured and/or increasing those with a usual source of care, are also needed to improve gaps in patient experience. The consistent problems experienced by patients with more serious health problems also suggest a need to improve methods of communicating with and caring for patients with serious chronic diseases. It will be important to align the goals of the Triple Aim (to improve patient experience, population health and lower cost of care) with the goals of health equity as the nation moves forward.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bailey ZD, Krieger N, Agénor M, et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463. doi: 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- 2.Manuel JI. Racial/ethnic and gender disparities in health care use and access. Health Serv Rees. 2018;53(3):1407–1429. doi: 10.1111/1475-6773.12705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smedley B, Stith A, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US); 2003. [PubMed]
- 4.Agency for Healthcare Research and Quality. 2021 National Health care Quality and Disparities Report Introduction and Methods. AHRQ Publication No.21(22)-0054-EF. Dec 2021. AHRQ Publication No.21(22)-0054-EF. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr21/index.html
- 5.Salsberg E, Richwine C, Westergaard S, et al. Estimation and comparison of current and future racial/ethnic representation in the U.S. health care workforce. JAMA Netw Open. 2021;4(3):e213789. doi: 10.1001/jamanetworkopen.2021.3789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dent R, Vichare A, Casimir J. Addressing Structural Racism in the Health Workforce. Med Care. 2021;59(10 Suppl 5):S409–S412. doi: 10.1097/MLR.0000000000001604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saha S, Komaromy M, Koepsell TD, Bindman A. Patient-physician racial concordance and the perceived quality and use of health care. Arch Internal Med. 1999;159(9):997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- 8.Cooper L, Beach MC, Johnson RL, Inui TS. Delving below the surface. J Gen Int Med. 2006;21(1):21–27. doi: 10.1111/j.1525-1497.2006.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooper L. A 41-year-old African American man with poorly controlled hypertension: review of patient and physician factors related to hypertension treatment adherence. JAMA. 2009;301(12):1260–1272. doi: 10.1001/jama.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Powe N, Cooper L. Disparities in patient experiences, health care processes, and outcomes: The role of patient–clinician racial, ethnic, and language concordance. New York: Commonwealth Fund. Jul. 1, 2004. https://www.commonwealthfund.org/publications/fund-reports/2004/jul/disparities-patient-experiences-health-care-processes-and
- 11.LaVeist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43(3):296–306. doi: 10.2307/3090205. [DOI] [PubMed] [Google Scholar]
- 12.Greenwood BN, Hardeman RR, Huang L, Sojourner A. Physician–patient racial concordance and disparities in birthing mortality for newborns. PNAS. 2020;117(35):21194–21200. doi: 10.1073/pnas.1913405117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jetty A, Jabbarpour Y, Pollack J, et al. Patient-physician racial concordance associated with improved healthcare use and lower healthcare expenditures in minority populations. J Racial Eth Health Disparities. 2022;9(1):68–81. doi: 10.1007/s40615-020-00930-4. [DOI] [PubMed] [Google Scholar]
- 14.Meghani S, Brooks J, Gipson-Jones R, et al. Patient–provider race-concordance: does it matter in improving minority patients’ health outcomes? Ethn Health. 2009;14(1):107–130. doi: 10.1080/13557850802227031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shen M, Peterson E, Costas-Muñiz R, et al. The Effects of Race and Racial Concordance on Patient-Physician Communication: A Systematic Review of the Literature. J Racial Ethn Health Disparities. 2018;5(1):117–140. doi: 10.1007/s40615-017-0350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ma A, Sanchez A, Ma M. Racial disparities in health care utilization, the affordable care act and racial concordance preference. Intl J Health Econ Mgmt. 2021;22(1):91–110. doi: 10.1007/s10754-021-09311-8. [DOI] [PubMed] [Google Scholar]
- 17.Xu KT. Usual Source of Care in Preventive Service Use: A Regular Doctor versus a Regular Site. Health Serv Res. 2002;37(6):1509–029. doi: 10.1111/1475-6773.10524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Council of Economic Advisers. The Effects of Earlier Medicaid Expansions: A Literature Review. Washington DC: White House. June 2021. https://www.Whitehouse.gov/wp-content/uploads/2021/06/Medicaid-Expansions-Lit-Review-CEA-.pdf
- 19.Guth M, Artiga S, Pham O. Effects of the ACA Medicaid Expansion on Racial Disparities in Health and Health Care. Kaiser Family Foundation. Sept. 30, 2020. https://www.kff.org/medicaid/issue-brief/effects-of-the-aca-medicaid-expansion-on-racial-disparities-in-health-and-health-care/
- 20.Medicaid and CHIP Payment and Access Commission. Access in Brief: Adults’ Experiences in Accessing Medical Care. Nov. 2021. https://www.macpac.gov/wp-content/uploads/2012/06/Access-in-Brief-Adults-Experiences-in-Accessing-Medical-Care.pdf