Abstract
Research on the psychological impact of the COVID-19 pandemic highlighted negative effects on the general population and particularly on parents. However, little is known about families of children with Neurodevelopmental Disorder (NDD). The present study investigated parental stress, coparenting, and child adjustment in Italian families with children with NDD (N = 82) and typical developing children (TD, N = 82) during lockdown, using an online survey. Results of quantitative analyses showed a significant increase in parental stress and child externalizing behaviors, but not of coparenting. Parental stress is predicted by externalizing behaviors, and coparenting acted as a moderator in the relationship between the change in the amount of time spent with the children before and during lockdown and parental stress. In children with NDD, the decrease in therapeutic/rehabilitation support predicted higher externalizing behaviors. Qualitative analysis showed that beyond the difficulties and worries arising during lockdown, most of the parents appreciated the opportunity of spending more time with their children and strengthening the parent-child relationship. In conclusion, our results point out the importance of ensuring continuity of care for children with NDD (e.g. telehealth) during home confinement and of providing psychological support for parents.
Keywords: Parental stress, Child externalizing behaviors, Coparenting, Neurodevelopmental disorders, COVID-19 pandemic
What this paper adds
This paper shed new light on the effects of home confinement on mental health of families with children with neurodevelopmental disorder and with typical development during the COVID 19 pandemic. Parental stress and child problematic behavior were reported as higher during lockdown compared to before the pandemic. The quality of coparenting remained stable and mediated the relation between parental and child adjustment.
1. Introduction
In February 2020, the cases of people affected by COVID-19 - a respiratory disease caused by the novel virus SARS-CoV-2 - started to increase abruptly in Northern Italy leading to the introduction of strict limitations by the Italian Government. Leaving home was forbidden except for non-deferrable work or for health reasons; all non-essential services and manufacturing were stopped; shops were closed except those selling essential products; all sports and artistic events were cancelled; and all schools and universities across the country stopped classroom based teaching and gradually moved to online learning platforms. Notably, after-school educational and recreational activities for children were suspended and the educational and therapeutic services directed to children with special needs of all ages were closed. In Italy, these emergency measures lasted 55 days followed by, a gradual resumption to normality. Similar measures were taken in different periods all over the world, generating negative consequences for public mental health across the globe especially for individuals with special psychological needs - such as children with neurodevelopmental disorders (NDD) - and their families (Kong, 2020; Lazzerini & Putoto, 2020). However, the impact of these measures in families with children with NDD is still poorly understood.
1.1. Psychological impact of quarantine
According to the literature on the impact of previous epidemic infections (Wang, Zhang, Zhao, Zhang, & Jiang, 2020; Zhang et al., 2020), the COVID-19 emergency might represent a significant risk for public health given its implications on a psychological, emotional, and behavioral level. The first studies conducted during the COVID-19 pandemic in different countries confirmed increased psychological symptoms in the general population, with more notable symptoms in women, people with higher levels of education, younger adults and parents (Liu et al., 2020; Salari et al., 2020). These results suggest that parents are a risk group for developing psychological distress during pandemic circumstances.
1.2. Parenting during home confinement
During home confinement, family daily routines suddenly changed, and the role of parents required additional psychological resources. After school closure, most parents had to balance housework, childcare, and homeschooling, without any help from their usual support systems (e.g. school, grandparents, therapists, etc.). Nevertheless, the quarantine may also have had positive implications for parents’ wellbeing (Brooks et al., 2020; Sprang & Silman, 2013) such as increased feelings of closeness in interpersonal relationships and shared every-day problem solving. Moreover, given the increase in time available, parents might have had the chance to better support the development of autonomy skills amongst their children. Thus, on the one hand, the quarantine allowed parents to spend an increased amount of time together with their children whilst on the other hand, it forced them to manage educational, caregiving, and therapeutic roles together with daily work and personal commitments.
1.3. Home confinement for children with NDD and their families
Health associations have warned about specific risks connected to the pandemic-related emergency measures, especially for the mental health of children with NDD, calling for prevention and support strategies (Aishworiya & Kang, 2020). In fact, the unexpected lifestyle changes generated by the restrictive measures to control the COVID 19 pandemic, may be even more difficult for children with NDD and their families (Nonweiler, Rattray, Baulcomb, Happé, & Absoud, 2020). The first time-sensitive studies on the impact of home-confinement on family wellbeing highlighted the significant role of parental stress in influencing child psychological adjustment in families with neurotypical children (Daks, Peltz, & Rogge, 2020; Liu, Bao, Huang, Shi, & Lu, 2020; Wang et al., 2020). However, very little is known about parental stress and child wellbeing in families of children with NDD.
For children with NDD, the lockdown implied a drastic change in daily routine, which is a crucial strategy to limit problem behavior (Rodger & Umaibalan, 2011; Schaaf, Toth-Cohen, Johnson, Outten, & Benevides, 2011). Parents were expected to reorganize daily activities and to structure them according to the children’s needs. Importantly, children with NDD require personalized and significant support delivered by physicians, occupational and speech therapists, school educators and psychologists. Nevertheless, the forced closure of schools and clinical center restrictions led children with NDD to lose professional support that they constantly need (Kong, 2020). Therefore, parents of children with NDD were also directly involved in the daily rehabilitative-therapeutic activities of their children that could not take place as usual and, in best case scenarios, were adapted to an online setting requiring partial or total engagement of parents (Spinelli & Pellino, 2020). In light of this, parenting and coparenting children with NDD during home confinement might be more demanding and potentially stressful.
1.4. Parental stress and coparenting in families of children with NDD
In general, several studies showed that parents of children with NDD experience higher levels of parental stress compared to those of typically developing children (Estes et al., 2013; Hayes & Watson, 2013; Tomanik, Harris, & Hawkins, 2004). In this regard, child behavioral problems and cognitive impairment have been found to contribute to parental stress (Neece, Green, & Baker, 2012; Theule, Wiener, Tannock, & Jenkins, 2013). Specifically, prior research highlighted that the severity of children externalizing behavior is a significant predictor of parental stress (Baykal, Karakurt, Çakır, & Karabekiroğlu, 2019; Dunn, Burbine, Bowers, & Tantleff-Dunn, 2001).
Additionally, positive coparenting has been found to be significantly associated with lower parenting stress in both mothers and fathers (May, Fletcher, Dempsey, & Newman, 2015). Coparenting indicates the way that partners work together in rearing their children and it is characterized by the presence of a collaborative involvement, mutual alliance, and moral support between parents (McHale & Lindahl, 2011; McHale & Rotman, 2007). In the last decade, this construct has been applied also to parents of children with NDD. Indeed, given the high level of energy required on a daily basis to care for children with NDD, the involvement of multiple caregivers is important not only to share the efforts in caring, but also to manage challenges in effectively, efficiently, and creatively (Maynard, McDonald, & Stickle, 2016). Previous studies have demonstrated that poor coparenting alliance can significantly increase parenting stress (Morrill, Hines, Mahmood, & Cordova, 2010). A recent study pointed out that when parents use shared strategies to cope with the child’s difficulties, this may have positive effects on the containment and management of a child’s challenging behavior (Hirsch & Paquin, 2019), that is frequent in children with NDD (Matson & Nebel-Schwalm, 2007). Additionally, the maternal and paternal perception of coparenting behavior was found to mediate the relationship between parenting self-efficacy and parental stress levels (May et al., 2015).
1.5. Aims
Starting from the negative psychological impact of the COVID-19 outbreak on the general population and the additional challenges that families of children with NDD might face under such circumstances, the general purpose of this study is to investigate parental, couple, and child adjustment in Italian families with children with NDD and typical developing (TD) children during lockdown. Firstly, we aimed 1) to assess if the perceived levels of parental stress, coparenting quality, and child externalizing symptoms changed in response to the COVID-19 outbreak; 2) to examine if the impact of the outbreak was different between families of children with NDD and TD. In addition, we aimed 3) to investigate the predictive role of different individual and family adjustment dimensions on parental stress, and 4) to understand the impact of family adjustment and remote therapy on the externalizing behavior of children with NDD. Finally, 5) in an attempt to understand better the impact of the pandemic on family adjustment, we also qualitatively analyzed the most remarkable aspects of the home confinement experience reported by parents of children with NDD.
2. Methods
2.1. Participants
The study included a total of 164 parents, 82 parents of children with neurodevelopmental disabilities (NDD) and 82 parents of typically developing children (TD). Participants selected for this study were involved in a larger research project (titled “Parenting during the COVID-19 Pandemic”), on parenting and child adjustment conducted during the lockdown related to the COVID-19 outbreak through an online survey. The project was conducted in collaboration with several Universities, one in Italy, one in Spain, one in the USA, and two in Africa [Universities’ name omitted for blind revision]. For the purpose of the present study, only the data collected in Italy was considered. In total, 1161 people participated in the italian survey. Among those who completed it, for the purpose of the present study, we selected all of those reporting to have a child with NDD aged between 3 and 17 years and a matched group of parents of children with TD. In the NDD group, 59 % of children (N = 49) had a diagnosis of Autism Spectrum Disorder (ASD) and 41 % of other neurodevelopmental disorders (N = 33). Participants in the control group were selected in order to match the participants in the NDD group according to the following criteria: parent gender, child gender, family SES, living area at the time of survey completion and child age (Table 1 ). The population of interest was reached using a snowball participants recruitment strategy and by promoting the link on free access webpages and social media through specific posts and advertising. Any person older than eighteen years old and having at least one child below 18 years of age could participate in the study, regardless of gender, sexual orientation, socioeconomic status, or family structure. Single parents, or mothers and fathers not living with their offspring or with the other parent of the child at the time of recruitment, could also participate in the study. Similarly, parents of children with physical or intellectual disabilities as well as neuroatypical development were included. Being an Italian speaker and living in Italy during the lockdown period were further inclusion criteria for this study.
Table 1.
Characteristics of the participants.
| Variables | NDD | TD | p |
|---|---|---|---|
| Parent’s age | 42.01 (6.59) | 41.28(6.39) | p = .47 |
| Partner’s age | 44.19 (6.10) | 44.03(7.27) | p = .87 |
| SES | 32.26 (14.60) | 32.48 (14.90) | p = .92 |
| Parents’ gender | p = .50 | ||
| Female | 73 (89.0 %) | 74 (90.2 %) | |
| Male | 9 (11.0 %) | 8 (9.8 %) | |
| Children’s gender | p = .34 | ||
| Female | 20 (24.1 %) | 23 (28 %) | |
| Male | 63 (75.9 %) | 59 (72 %) | |
| Children’s age | 7.63 (3.77) | 7.67 (3.86) | p = .95 |
| Provenience: | |||
| North | 60 (73.2 %) | 64(78.0 %) | p = .73 |
| Centre | 13 (15.8 %) | 9 (11.0 %) | |
| South | 9 (11.0 %) | 9 (11.0 %) | |
Note. NDD: Neurodevelopmental disorder, TD: Typical Development, SES: Socioeconomic Status.
2.2. Measures
The present survey was developed to investigate different domains of parenting and child behavior that might have changed during the COVID-19 outbreak contributing to individual and family adaptation. In particular, the survey included questions about sociodemographic information, ad-hoc questions about current organization and experience in relation to the COVID-19 outbreak, parental stress, coparenting, and child externalizing behavior.
2.2.1. General information
Firstly, participants were asked to respond to some general questions about sociodemographic information, their job status, and family routines during the Lockdown. Among those variables, for the purposes of this study, only sociodemographic information and the change in the amount of time spent by the parent doing activities with the child (Δtime_w_child) were considered in the analyses. The variable Δtime_w_child was calculated using a specific item of the survey: parents were asked to indicate “On average, how much time do you spend with your child doing activities?” using a 5-points Likert scale (from 1= never to 5= always), both referring to the period pre and during the COVID-19 lockdown. The predictor Δtime_w_child was calculated by subtracting the response referred to pre from the one referred to during the lockdown (i.e. higher Δtime_w_child corresponded to greater amount of time spent with the children during the lockdown).
2.2.2. Parental Stress Scale (PSS)
As a measure of parental stress, we used 10 items of the Parental Stress Scale (PSS, Berry & Jones, 1995), a freely accessible questionnaire that includes 18 items describing feelings and perceptions about the experience of being a parent, exploring both positive themes (emotional benefits, self-enrichment, personal development) and negative components (demands on resources, opportunity costs and restrictions) of parenthood. We selected a subset of 10 items that we considered more relevant for the lockdown situation, in an attempt to reduce the duration of the survey and minimize the participant drop-out rate. Specifically, we excluded the items regarding the general perception of the parental role and selected the more specific aspects of parenting, including the aforementioned positive and negative themes in all the areas covered by the questionnaire (emotional benefits, self-enrichment, personal development, demands on resources, opportunity costs and restrictions). For example, an item investigating a positive theme was “My child is an important source of affection for me”, and an item investigating a negative component was “It is difficult to balance different responsibilities because of my child.” The participants were asked to indicate their agreement with the item, using a 5-points Likert scale (from 1 = “I strongly disagree” to 5 = “I strongly agree”). The theoretical raw scores of this short version of PSS ranged from 10 to 50; the obtained raw scores ranged from 11 to 45. Different studies have found adequate psychometric properties of the whole PSS (e.g Berry & Jones, 1995, for more recent a review see Louie, Cromer, & Berry, 2017) also in clinical populations (Holly et al., 2019; Zelman & Ferro, 2018). In our total sample, the shortened version revealed adequate internal consistency with Cronbach alpha values ranging from 0.77 for the responses that referred to the lockdown period to 0.743 for the ones referred to the period before the lockdown (from 0.785 to 0.788 in the NDD group, and from 0.746 to 0.671 in TD group). Data were light-tailed relative to a normal distribution: skewness was .177 and .113 pre and during lockdown, respectively; kurtosis was -.577 and -.030 pre and during lockdown, respectively.
2.2.3. Coparenting Relationship Scale (CRS)
As a measure of coparenting, we used the brief form of the Coparenting Relationship Scale (CRS, Feinberg, Brown, & Kan, 2012) which includes 14 items that evaluates different aspects of coparenting: agreement, closeness, exposure to conflict, support, undermining, endorse partner parenting, and division of labor (e.g.: “My partner likes to play with our child and then leaves the dirty work to me”). Participants were asked to select the response that best described the way they and their partner work together as parents, using a 0–6 Likert scale (from 0 = “Not true for us” to 6 = “Very true for us”). The theoretical raw scores ranged from 0 to 98, the obtained raw scores ranged from 32 to 96, skewness ranged between -.646 and -.739 and kurtosis ranged between -.168 and .013 pre and during lockdown, respectively.
The full form Coparenting Relationship Scale has shown to possess good reliability, stability, construct validity, and interrater agreement (Feinberg et al., 2012). The 14-item brief measure (used in this study) has been shown to have good internal consistency both in mothers and in fathers, with alphas ranging from .81 to .89 (Cronbach’s alpha) (Feinberg et al., 2012). This measure has been validated also in Portuguese (Lamela, Figueiredo, Bastos, & Feinberg, 2016), and Swedish populations (Lee, Feinberg, & Wells, 2020), confirming good internal consistency and that all subscales were adequately or strongly correlated with CRS-brief total scores. Also, Feinberg and collaborators (Feinberg et al., 2012) showed that the CRS-brief scale was an excellent approximation of the full CRS scale, with a correlation of .97 for mothers and .94 for fathers, and suggested that it can be used to adequately assess coparenting in clinical settings and when time is limited. In addition, we calculated Cronbach's Alpha for coparenting responses in our TD and NDD groups, which ranged between .843 and .808 and showed good internal consistency.
2.2.4. Strengths and Difficulties Questionnaire (SDQ)
The child externalizing behavior was assessed through the omonimous scale (SDQ_ext) of the Strengths and Difficulties Questionnaire (SDQ, Goodman, 2001, 1997; Klasen et al., 2000). The SDQ_ext scale includes only 2 subscales of the SDQ, namely the hyperactivity/inattention and conduct problems scales, each of which including 5 items. For each item, participants were asked to rate to what extent the statement was true for their child, using a 3-points response scale (0 = not true; 1 = somewhat true; 2 = completely true). The theoretical raw scores ranged from 10 to 30, the obtained raw scores ranged from 10 to 29, skewness ranged between .704 and .848 and kurtosis ranged between .537 and .721 pre and during lockdown, respectively.
Previous studies have shown satisfactory SDQ’s internal consistency, cross-informant correlation, and retest stability after 4–6 months (Goodman, 2001). More recently, the adequate internal consistency, test-retest indices, and five-factor structure were confirmed in a cross-cultural study across European countries (Husky et al., 2018; Di Riso et al., 2010), with good screening detection especially for externalizing disorders. In addition, we calculated Cronbach's Alpha for SDQ responses in our TD and NDD groups, which ranges between .751 and .780 and showed good internal consistency.
2.2.5. Specific information about children with NDD
Finally, only for the NDD group, we also assessed how much the child was followed by therapists and/or rehabilitation specialists compared to the period before the lockdown (Δtherapy). Specifically, participants were asked to say whether, compared to the period before the lockdown, the child received fewer or more hours of therapy using a 5-points Likert scale (from 1 = “Much less than before” to 5 = “Much more than before”).
2.2.6. Open question
At the end of the survey, we inserted an optional open question, where participants were asked to freely describe what was the most significant aspect of their experience as a parent during the COVID-19 outbreak.
2.3. Procedure
An anonymous survey was collected online using a secure survey service (Qualtrics, Provo, UT). The duration of the survey was around 15−20 min. In the case of parents with more than one child aged between 3 and 17 years, participants were asked to respond by referring to the younger one. Participants could withdraw at any time by closing the survey. Each participant was allowed to complete the survey only once. All the collected data (including the information about the relatives) were anonymous and did not contain any personally identifiable information. For the Parental Stress Scale, Coparenting Relationship Scale, and Strengths and Difficulties Questionnaire, participants were asked to respond to each item twice: firstly, with reference to the current moment (“Now”, that corresponded with the lockdown phase) and secondly, with reference to the month just before the lockdown’s beginning (“Before”). The study was not submitted to the Ethical Committee of our University because the ethical approval from our IRB is required only for the studies that imply a risk to the participants, which was not the case in the present study. In fact, participation in the study only entailed completion of an online survey which was completely anonymous and no personal or identifiable information was collected.
According to the University of [omitted for blind review purpose] research policy, the research project was deposited to the Department of [omitted for blind review purpose] and no additional ethical approval was required as participation did not imply any risk nor required collection of personal/identifiable information. The study was conducted in accordance with the standards of the National Code of Ethics for Research in Psychology of the Italian Psychological Association (http://www.aipass.org/node/11560). Moreover, data was collected, treated, and stored anonymously, according to the Italian (Law 31 dicembre 1996 n. 675, 676, Gazzetta Ufficiale del 08/01/1997, art. 7 del D. Lgs. 30 giugno 2003, n. 196) and European current regulation (European General Data Protection Regulation - GDPR UE 2016/67) as disclosed to participants. Specifically, in the initial part of the survey, participants were informed about the aim and the procedure of the study, and the areas that would be investigated (General information; Wellbeing of the parent; Parenting styles and parent-related stress; Coparenting with parent/partner; Child behavior). Then, they were asked to read the information carefully about the treatment of personal data. Participants’ names or identifiable information did not appear anywhere in the survey and collected data of each participant was associated with an anonymous identification code. Participants were also informed that the data collected could be inserted in publications or congresses, conferences and scientific seminaries, as well as published as an accessible form on the social platform in aggregated and anonymous form. At the end of the privacy information, the e-mail and telephone number of our laboratory were indicated and participants were invited to contact the researchers in case they had any question or desired further information about the study. Only at this point, participants provided their informed consent in participating in the study and could proceed with the questionnaires’ completion.
2.4. Statistical analyses
To explore differences between before and during the lockdown phase, the variables parental stress, CRT, SDQ_Ext were analyzed separately using 2 × 2 mixed ANOVAs, with Group (TD vs NDD) as between factor, and Time (Before vs During COVID-19 lockdown) as within factor (See Table 2 ). Furthermore, to investigate which factors would predict parental stress during the COVID-19 lockdown, we performed a hierarchical regression analysis on parental stress. Hierarchical regression is a statistical procedure in which hypothesized predictors of a dependent variable are included in an analysis in several steps that illuminate the contribution of each set of variables (APA dictionary of Psychology, https://dictionary.apa.org/hierarchical-regression). It consists of building several regression models by adding independent variables to a previous model at each step; later models always include smaller models in previous steps. In this hierarchical regression the dependent variable was the parental stress. In the first step, we wanted to explore the parental stress in relation to the presence/absence of neurodevelopmental disorder in the children and we initially entered Group as predictor; in the second step we wanted to explore factors related to the family environment and we entered the CRS as predictor; finally, in the third step, we wanted to explore variables specifically related to the adjustment in response to COVID-19 and we entered the SDQ_ext and the difference in the amount of time spent doing activities with the child during lockdown compared to before (Δtime_w_child) as predictors. For parental stress, CRS and SDQ_ext, we considered only the responses referred to the lockdown period. In addition, we performed a moderation analysis with parental stress as a dependent variable, Δtime_w_child as predictor, and Group and CRS as moderators. Next, we investigated if relevant aspects of adaptation to the lockdown in families with children with NDD (such as change in the therapeutic support received by the child and the change in the time that parents spent in doing activities with the child) had influenced their externalizing behaviors. To this aim, we performed a linear regression only in the NDD group, with SDQ_ext (during lockdown) as dependent variable, and changes in therapy (Δtherapy) and Δtime_w_child as predictors.
Table 2.
Mean and standard deviations of the measured variables (rows) in the two study groups (columns).
| Variables | NDD | TD | Between Statistics |
|---|---|---|---|
| Parental stress during covid-19 | 27.44 (6.94) | 25.01 (6.73) | F(1,162) = 4.46, p <.036 |
| Parental stress pre covid-19 | 25.56 (6.89) | 23.98 (5.47) | |
| Within statistics | F (1,162) = 15.03, p < .001 | ||
| Coparenting during covid-19 | 72.05 (15.66) | 72.58 (13.74) | F(1,149) = .029, p = .706 |
| Coparenting pre covid-19 | 72.28 (15.37) | 72.82 (13.41) | |
| Within statistics | F(1,149) = .143, p < .706 | ||
| Child ext. behaviour during covid-19 | 17.48 (3.50) | 16.02 (6.78) | F(1,162) = 10.5, p = .001 |
| Child ext. behaviour pre-covid-19 | 16.82 (3.19) | 14.91 (3.62) | |
| Within statistics | F(1,162) = 23.58, p < .001 | ||
Note. NDD: Neurodevelopmental disorder, TD: Typical Development, Ext: externalizing.
All the analyses were conducted using SPSS Version 22 (Released, I. B. M. C. O. R. P., 2013). For the moderation analysis, we used the package PROCESS (Hayes, 2017) implementation for SPSS.
Finally, the responses to the open question were analyzed using a qualitative content analysis (Chabrol, 1974; Krippendorff, 2018). This methodology allowed us to highlight the principal themes that emerged from the parents’ open responses and to quantify (in percentage) how often they were reported by the parents.
3. Results
3.1. Repeated measures pre-during lockdown between groups
Results of the ANOVA on the PSS showed a significant effect of Time (F(1,162) = 15.03, p < 0.001, eta-sq = .085) with greater parental stress during lockdown compared to before the lockdown phase. Also, there was a significant effect of Group (F(1,162) = 4.46, p = 0.036, eta-sq = .027), with greater parental stress in the NDD group compared to the TD group. The interaction between Time*Group was not significant (F(1,162) = 1.125, p = 0.265). ANOVA on CRS showed no significant main or interaction effects. Similarly to what we found for parental stress, results of the ANOVA on SDQ_ext showed a significant effect of Time (F(1,162) = 23.59, p < 0.001, eta-sq = .127), and a significant effect of Group (F(1,162) = 10.53, p = 0.001, eta-sq = .061) with greater externalizing behaviors in children with NDD compared to TD. The interaction Time*Group was not significant (F(1,162) = 1.54, p = 0.217).
3.2. Hierarchical regression on parental stress
The variance explained by the model with Group, CRS, Δtime_w_child, and SDQ_ext as predictors (Model 3, R2 = 0.142) was greater than the variance explained by the model with Group and CRS (Model 2, R2 = 0.053) and by the model with only Group (Model 1, R2 = 0.033) as predictors. The three models were compared using ANOVAs, which confirmed a significant difference between the Model 1 and the null model (F(1,153) = 5.224, p = 0.024), between Model 2 and Model 1 (F(2,153) = 4.185, p = 0.017), and between the Model 3 and Model 2 (F(4,153) = 6.155, p < 0.001). Results of the Model 3 showed a significant effect of SDQ_ext (β = .311, p < 0.001) while Δtime_w_child was not significant. Group and CRS were significant (or showed a tendency toward significance) only in Model 1 and 2 (see Table 3 ), but not in Model 3.
Table 3.
Hierarchical regression predicting parental stress.
| Predictors | Parental stress |
|||||
|---|---|---|---|---|---|---|
| β | t | 95 % CI | F | R2 | ΔR2 | |
| Block 1 | 5.22 | .033* | . | |||
| Child clinical status | −.182* | −2.28 | [−4.63, −.337] | |||
| Block 2 | 4.18 | .053* | .01 | |||
| Child clinical status | −.180* | 2.26 | [−4.59, −.317] | |||
| Coparenting | −.113 | 1.75 | [−138, −.008] | |||
| Block 3 | 6.15 | .142*** | .08 | |||
| Child clinical status | −.115 | −1.48 | [−3.67, −.523] | |||
| Coparenting | −.090 | −1.16 | [−.114, −.029] | |||
| Δ time with the child | .028 | .361 | [−1.10, −1.59] | |||
| Child externalizing behavior | .311*** | 3.93 | [.282, −.851] | |||
Note. 95 % CI: Confidence Interval; Δ time with the child: change in the amount of time spent by the parent doing activities with the child before and during covid-19. **p < .01.
p < .05.
p < .001.
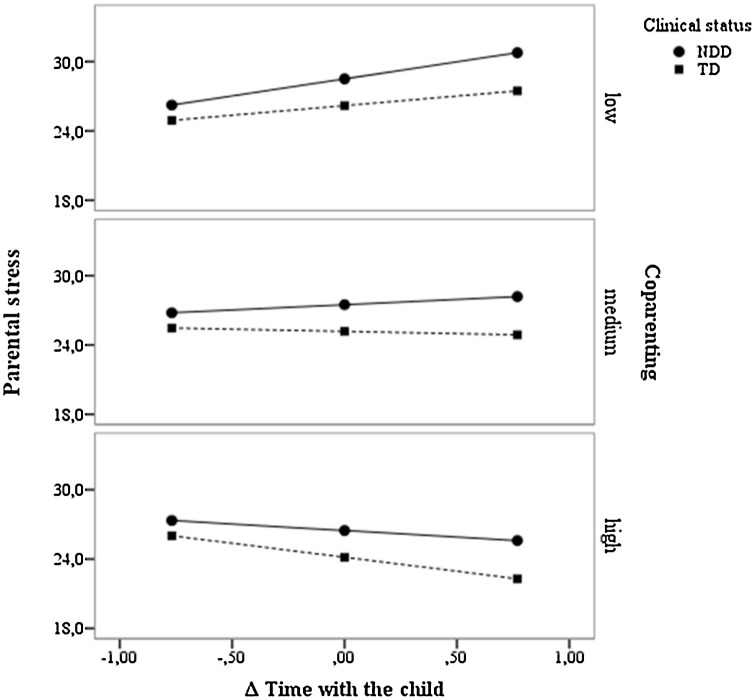
3.3. Moderation analysis parental stress
We initially hypothesized that the time spent with the child/children might influence the parental stress, but this did not result from the regression analysis. Therefore, we explore the hypothesis that CRS and/or child clinical status may act as moderators. To this aim, we performed a moderation analysis with PSS as dependent variable, Δtime_w_child as predictor, and CRS and Group as moderator (R2 = 0.116, F(5,148) = 3.89, p = 0.002). The results highlighted a significant effect of the Group (β = -2.42, p = 0.023) and a significant interaction between Δtime_w_child*CRS during the lockdown period (β = -,138, p = 0.004). In addition, we conducted the simple slopes analysis to analyze the association between Δtime_w_child and PSS at low (-1SD), medium (at 0), and high (+1SD) levels of coparenting (Fig. 1 ). The effect of Δtime_w_child was significant when coparenting was low in NDD (β = 2.86, p = .016) and when coparenting was high in TD (β = 2.41, p = .027).
Fig. 1.
Moderation model with Δ time with the child and parental stress at different levels of coparenting.
Note. NDD: Neurodevelopmental Disorder; TD: Typical development.
The low level of coparenting is 1 SD below the mean, the medium level is at the mean, and the high level is 1 SD above the mean.
3.4. Linear regression on SDQ_ext in NDD group
Finally, we investigate whether some aspects, specifically related to the lockdown, contribute to explaining externalizing behavior in children with NDD. In particular, we explored whether the change in the therapeutic support received during lockdown (Δtherapy) and the increasing/decreasing amount of time that parents spent in doing activities with their children (Δtime_w_child) could influence the externalizing behavior. To this aim, we performed a linear regression analysis only on the clinical group, with SDQ_ext as dependent variable, and CRS, Δtime_w_child, and Δtherapy as predictors (R2 = 0.144, p = 0.013). The results showed a marginally significant effect of CRS (β= -.210, p = 0.066) and a significant effect of the Δtherapy (β = -.30, p = 0.012), while the effect of Δtime_w_child resulted not significant.
3.5. Qualitative content analysis
Among the group of parents having children with NDD, 56 out of 83 participants replied to the open question. Through qualitative content analysis, we first extracted from the 56 responses 15 distinct thematic units each expressed by 1–14 participants. Successively, we aggregated the 15 theme units into three thematic macro-categories: 1) Experience of opportunities, 2) Experience of excessive load and difficulties and 3) Worrying about the child.
The first macro-category “Experience of opportunities” counted 41 occurrences among the 56 responses and included references to the opportunity to spend time with the child and strengthen the parent-child relationship. Specifically, the following thematic units were included: - Pleasure/opportunity to have more time to dedicate to the child (n = 14; 25 % of respondents); Sense of protection or tranquility (n = 10; 18 %); Interpretation of the challenges as an opportunity for improvement (n = 8; 14 %); Closeness, getting to know the children better (n = 6; 11 %); Increased confidence as parents (n = 3; 5%). The second macro-category “Experience of excessive load and difficulties” counted 19 occurrences among the 56 responses and included references to the lockdown period as negative, demanding, or difficult. In particular the following themes emerged: a) having to do everything by oneself or to be parent, teacher, and therapist at the same time (n = 12; 21 % of respondents); b) difficulties in managing the child’s presence h24 (n = 2; 4%); c) worries about managing the situation (n = 3; 5%) and d) Negative feelings (n = 2; 4%).
The third macro-category “Worrying about the child” occurred 11 times among the 56 responses and included references to the worries about the specific risks to the child relating to the lockdown, such as: a) worries about absence of social interactions/loneliness (n = 4; 7%); b) worries about interrupted therapy (n = 3; 5%); c) inadequacy of remote learning (n = 2; 4%) and d) lack of routine/increasing difficulties (n = 2; 4%). To summarize the qualitative results based on occurrence (Braun & Clarke 2008), looking at the macro-categories, we observed that the “Experience of opportunity” had more than twice the occurrences of the “experience of excessive load” and three times that of “worrying about the child”. Moreover, looking at the occurrence of the basic theme units, we observed that the pleasure and opportunity of spending time with children” was the most frequent unit (25 % of respondents) in parents’ replies, followed by the difficulty of being alone all the time with the children and dealing with them without the usual help of school and therapy (21 % respondents).
4. Discussion
In this study, we explored the impact of the COVID-19 outbreak on parents’ and children's psychological wellbeing, with particular reference to families of children with NDD. More specifically, we investigated differences in parental, child and couple adjustment during and before the pandemic. Moreover, we analyzed which factors predicted parental stress and child externalizing behaviors.
With respect to parental stress, we found that the COVID 19 pandemic and the related strict containment measures had a negative impact, independently of the children's diagnostic status. In fact, both the parents of children with and without NDD, reported increased parental stress during the lockdown compared to before. This is in line with a study carried out in the UK which showed an increase of level of mental health problems in caregivers of children and adults with an intellectual disability (Willner et al., 2020). This result highlights that, during the COVID 19 pandemic, all parents seem to experience increased challenges and/or an additional burden in trying to meet the demands inherent to their parental role. In addition, our results showed that parental stress was higher in the NDD group, compared to the TD, both during and before the lockdown phase, consistent with a plethora of previous studies conducted in non-emergency times (Estes et al., 2013; Hayes & Watson, 2013; Tomanik et al., 2004). Thus, in parents of children with NDD the level of perceived stress increases as in parents with TD children, but starting from a higher baseline it reaches a more intense level.
As a second step, we investigated which factors could predict parental stress during the lockdown. We found that the externalizing behaviors were the main predictors of parental stress, regardless of children's diagnosis. This highlights the strong interplay between children and parental psychological domains and their reciprocal influence in determining the family’s wellbeing.
Regarding the children’s behavior (as perceived by the parents), we found that parents reported an increase in externalizing behavior during the lockdown, independent of child diagnostic status. This could be explained by the impact on child wellbeing of the restrictions imposed by the lockdown that hindered their peer relationships and upset their routine. However, parents’ perception of child distress could be biased by their own stress condition (Briggs-Gowan, Carter, & Schwab-Stone, 1996; Richters, 1992; Nonweiler et al., 2020). The overreporting of child behavioral difficulties could have also stemmed from the additional time they spent with him/her compared to non-emergency times.
Furthermore, consistent with previous studies (Baykal et al., 2019; Dunn et al., 2001; Kennedy, 2012), child externalizing behaviors were perceived as higher by parents of children with NDD compared to parents of children with TD both during and before the lockdown. Thus, the increase in child externalizing behaviors related to the pandemic is grafted on an already high baseline in children with NDD.
Importantly, in the NDD group the increase in child externalizing behavior was related to the decrease in provided therapy. These results have particular clinical relevance, because they clearly underline the importance of activating telehealth programs (Narzisi, 2020) to limit the worsening of externalizing symptoms and, in turn, to contain parental stress. Indeed, our findings showed that the level of parental stress was primarily driven by the children’s externalizing behavior. It is relevant to note that this was true for all the parents, independently of the children’s diagnosis. Nevertheless, it is of particular relevance with regards to NDD, as the baseline of both parental stress and externalizing behaviors were higher in this group and seem to be exacerbated by home confinement conditions. These results are consistent with a growing number of studies promoting the usefulness and feasibility of a telehealth approach to interventions for children with NDD, and especially for parent-mediated interventions (Bearss et al., 2018).
With respect to the parent's perception of the quality of the coparenting relationship, we found no effect of the lockdown in either families of children with NDD or TD. This result supports the idea that coparenting is a substantially stable dimension that is not directly affected by changes in the external context (Feinberg et al., 2012; Morrill et al., 2010). Importantly, in line with previous studies (May et al., 2015), we found that the quality of coparenting acted as a moderator between the time spent with the child and level of parental stress, but differently between families of children with NDD and TD (Hayes & Watson, 2013). Specifically, in families of children with NDD, a low quality of coparenting intensifies parental stress when parents spend more time with their children. Instead, in families of TD children, a high level of coparenting leads to a decrease in parental stress, when parents spend more time with their children. In other words, these results confirm that in families facing the challenges of parenting a child with NDD, a low level of support and sharing with the partner could be a risk factor for parental psychological distress. Therefore, this is an important aspect that should be considered in planning support interventions, as it can reduce parental stress and, in turn, improve the families’ wellbeing. Overall, our quantitative results revealed a worsening in the wellbeing both in parents and in children in the NDD group during the quarantine, with a general increase in parental stress as well as in child’s externalizing behaviors.
However, previous research also suggested the presence of positive aspects related to home confinement (Brooks et al., 2020). Thus, to enrich our understanding of both the positive and negative feelings experienced by parents of NDD children, we conducted a qualitative content analysis on spontaneous parental reports, from which some important considerations emerged. First, the majority of contents extracted from the open parental reports referred to home confinement as an opportunity to dedicate more time to their children and to strengthen the parent-child relationship. Although our results highlighted the presence of higher levels of stress and the perception of increased child’s problematic behavior, the increased amount of time spent with children was often considered by the parents as a chance to get to know their child better or to experience enhanced closeness. Regarding the negative themes, it emerged that the most difficult challenge during the home confinement for parents of children with NDD was being “left alone” in dealing with their children’s special needs, without support from professionals. This result is consistent with the study of Willner et al. (2020) that highlighted how the increase in parental stress is highly related to the decrease in perceived social support. Consistent with the impact of the decrease in regular therapy on child externalizing behaviors that we found, this qualitative analysis underlines again the importance of promoting a telehealth approach to help parents and children when standard interventions in person are prevented.
Some limitations have to be considered when interpreting the findings of this study. First, despite including ratings of the different dimensions of interest with reference to both the lockdown and the period before the pandemic, this study employed a cross-sectional design. Second, we used a survey consisting of different self-reported parental measures, which could have been biased by parents’ individual psychological distress in facing the pandemic. Third, information about what kind of support children with NDD were receiving (e.g. parent training, parent-mediated remote intervention, and speech therapy) was not available. The lack of clinical information is another limitation, in fact the only data available to us is represented by the diagnoses reported by parents. Fourth, child externalizing behaviors were not directly measured but reported by their parents. Finally, the absence of follow-up data collection after the lockdown period represents a limitation to the understanding of the middle-term impact of quarantine on parents and their children’s with NDD. Another possible limitation to the strength of our results is that we cannot test the construct comparability for the three constructs that we measured, because some of the questionnaires used in our survey were changed from their original version and because of the limited sample size of this study. Thus, we cannot ascertain the group invariance of the constructs measured in our survey and we cannot exclude that the differences between groups reflect a constructs’ variability instead of group differences in invariant constructs. This imposes caution to interpreting the group differences. However, in the attempt to partially overcome this issue, we calculated internal consistency of the shortened parental stress version used here, which resulted to be adequate in both TD and NDD groups. Nonetheless, to build upon this limitation, future research is needed and should include a larger sample in order to test for constructs comparability and invariance between the groups. This would allow group comparisons from latent variables instead of raw scores and, thus, to draw stronger and unbiased conclusions on group differences.
Besides the limitations, we would like to acknowledge some strengths of our study. To our best knowledge, this is the first study offering empirical results on the effects of pandemic home confinement on children with NDD and their parents wellbeing. To date, the majority of work about COVID-19 psychological effects in NDD have been conceptual papers, while we provided data on this important issue. Our results demonstrated negative effects of home confinement on parental stress and children externalizing behaviors, and highlighted the importance of a positive coparenting relationship to limit these negative effects. Although the study’s limits impose caution to interpreting the data, our results can be a starting point for future research in this field and offer initial, but pivotal, information for guiding intervention and prevention policies to support families of children with NDD wellbeing.
5. Conclusions
To sum up, our quantitative results revealed a general increase in parental stress and child externalizing behaviors during home confinement. Parental stress is predicted by externalizing behaviors regardless of child clinical status. Specifically, in the NDD group the reduced therapeutic support produced an increase in children’s externalizing behaviors. The coparenting remained stable before and during lockdown, and acted as a moderator in the relationship between the amount of time spent in carrying out activities with the children and parental stress. To conclude, our data suggests paying great attention to the psychological wellbeing of families of children with NDD that undergo home confinement and to investigate it using a multi-domain approach, either in planning time-sensitive post-pandemic support intervention or in preparing strategies to face future pandemic breakdowns. In addition, our results indicate the relevance of activating telehealth interventions that directly involve the parents. Finally, despite all the difficulties that have arisen during the quarantine period, we found that some parents appreciated the opportunity to spend more time with their children and felt that this has strengthened the parent-child relationship.
Fundings
NM is funded by the Municipality of Rovereto, MG is funded by the Italian Ministry of Education, University and Research (MIUR), Research Projects of National Relevance (PRIN-2017).
CRediT authorship contribution statement
Arianna Bentenuto: Conceptualization, Writing - original draft, Writing - review & editing. Noemi Mazzoni: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing - original draft, Writing - review & editing. Michele Giannotti: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing - original draft, Writing - review & editing. Paola Venuti: Project administration, Supervision, Writing - review & editing. Simona de Falco: Conceptualization, Data curation, Project administration, Supervision, Writing - original draft, Writing - review & editing.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
We thank all the parents for their participation in this study.
References
- Aishworiya R., Kang Y.Q. Including children with developmental disabilities in the equation during this COVID-19 pandemic. Journal of Autism and Developmental Disorders. 2020:1–4. doi: 10.1007/s10803-020-04670-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baykal S., Karakurt M.N., Çakır M., Karabekiroğlu K. An examination of the relations between symptom distributions in children diagnosed with autism and caregiver burden, anxiety and depression levels. Community Mental Health Journal. 2019;55(2):311–317. doi: 10.1007/s10597-018-0343-8. [DOI] [PubMed] [Google Scholar]
- Bearss K., Burrell T.L., Challa S.A., Postorino V., Gillespie S.E., Crooks C.…Scahill L. Feasibility of parent training via telehealth for children with autism spectrum disorder and disruptive behavior: A demonstration pilot. Journal of Autism and Developmental Disorders. 2018;48(4):1020–1030. doi: 10.1007/s10803-017-3363-2. [DOI] [PubMed] [Google Scholar]
- Berry J.O., Jones W.H. The parental stress scale: Initial psychometric evidence. Journal of Social and Personal Relationships. 1995;12:463–472. [Google Scholar]
- Briggs-Gowan M.J., Carter A.S., Schwab-Stone M. Discrepancies among mother, child, and teacher reports: Examining the contributions of maternal depression and anxiety. Journal of Abnormal Child Psychology. 1996;24(6):749–765. doi: 10.1007/BF01664738. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020 doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabrol C. Que peut-on demander à l’analyse du discours? Connexions. 1974;12:5–34. [Google Scholar]
- Daks J.S., Peltz J.S., Rogge R.D. Psychological flexibility and inflexibility as sources of resiliency and risk during a pandemic: Modeling the cascade of COVID-19 stress on family systems with a contextual behavioral science lens. Journal of Contextual Behavioral Science. 2020;18 doi: 10.1016/j.jcbs.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Riso D., Salcuni S., Chessa D., Raudino A., Lis A., Altoè G. The Strengths and Difficulties Questionnaire (SDQ). Early evidence of its reliability and validity in a community sample of Italian children. Personality and Individual Differences. 2010;49(6):570–575. [Google Scholar]
- Dunn M.E., Burbine T., Bowers C.A., Tantleff-Dunn S. Moderators of stress in parents of children with autism. Community Mental Health Journal. 2001;37(1):39–52. doi: 10.1023/a:1026592305436. [DOI] [PubMed] [Google Scholar]
- Estes A., Olson E., Sullivan K., Greenson J., Winter J., Dawson G.…Munson J. Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain & Development. 2013;35(2):133–138. doi: 10.1016/j.braindev.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinberg M.E., Brown L.D., Kan M.L. A multi-domain self-report measure of coparenting. Parenting. 2012;12(1):1–21. doi: 10.1080/15295192.2012.638870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. Guilford publications; 2017. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Hayes S.A., Watson S.L. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013;43(3):629–642. doi: 10.1007/s10803-012-1604-y. [DOI] [PubMed] [Google Scholar]
- Hirsch K.H., Paquin J.D. The stress of the situation has changed us both: A grounded theory analysis of the romantic relationship of parents raising children with autism. Journal of Child and Family Studies. 2019;28(10):2673–2689. [Google Scholar]
- Holly L.E., Fenley A.R., Kritikos T.K., Merson R.A., Abidin R.R., Langer D.A. Evidence-base update for parenting stress measures in clinical samples. Journal of Clinical Child and Adolescent Psychology. 2019;48(5):685–705. doi: 10.1080/15374416.2019.1639515. [DOI] [PubMed] [Google Scholar]
- Husky M.M., Otten R., Boyd A., Pez O., Bitfoi A., Carta M.G., Kovess-Masfety V. Psychometric properties of the Strengths and Difficulties Questionnaire in children aged 5–12 years across seven European countries. European Journal of Psychological Assessment. 2018;36(1):65. [Google Scholar]
- Released, I. B. M. C. O. R. P . IBM Corp.; Armonk, NY: 2013. IBM SPSS statistics for windows, version 22.0. [Google Scholar]
- Kennedy D. none; 2012. The relationship between parental stress, cognitive distortions, and child psychopathology. PCOM Psychology Dissertations. [Google Scholar]
- Klasen H., Woerner W., Wolke D., Meyer R., Overmeyer S., Kaschnitz W.…Goodman R. Comparing the German versions of the strengths and difficulties questionnaire (SDQ-Deu) and the child behavior checklist. European Child & Adolescent Psychiatry. 2000;9(4):271–276. doi: 10.1007/s007870070030. [DOI] [PubMed] [Google Scholar]
- Kong M. What COVID-19 means for non-neurotypical children and their families. Pediatric Research. 2020:1–2. doi: 10.1038/s41390-020-0913-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krippendorff K. Sage publications; 2018. Content analysis: An introduction to its methodology. [Google Scholar]
- Lamela D., Figueiredo B., Bastos A., Feinberg M. Typologies of post-divorce coparenting and parental well-being, parenting quality and children’s psychological adjustment. Child Psychiatry and Human Development. 2016;47(5):716–728. doi: 10.1007/s10578-015-0604-5. [DOI] [PubMed] [Google Scholar]
- Lazzerini M., Putoto G. COVID-19 in Italy: Momentous decisions and many uncertainties. The Lancet Global Health. 2020;8(5):e641–e642. doi: 10.1016/S2214-109X(20)30110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.K., Feinberg M.E., Wells M.B. The Swedish Brief Coparenting Relationship Scale: Psychometrics and concurrent validity among primiparous and multiparous fathers. Family Relations. 2020 [Google Scholar]
- Liu J.J., Bao Y., Huang X., Shi J., Lu L. Mental health considerations for children quarantined because of COVID-19. The Lancet Child & Adolescent Health. 2020;4(5):347–349. doi: 10.1016/S2352-4642(20)30096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D., Ren Y., Yan F., Li Y., Xu X., Yu X., Yao Y. Psychological impact and predisposing factors of the coronavirus disease 2019 (COVID-19) Pandemic on General Public in China. 2020 [Google Scholar]
- Louie A.D., Cromer L.D., Berry J.O. Assessing parenting stress: Review of the use and interpretation of the parental stress scale. The Family Journal. 2017;25(4):359–367. [Google Scholar]
- Matson J.L., Nebel-Schwalm M. Assessing challenging behaviors in children with autism spectrum disorders: A review. Research in Developmental Disabilities. 2007;28(6):567–579. doi: 10.1016/j.ridd.2006.08.001. [DOI] [PubMed] [Google Scholar]
- May C., Fletcher R., Dempsey I., Newman L. Modeling relations among coparenting quality, autism-specific parenting self-efficacy, and parenting stress in mothers and fathers of children with ASD. Parenting. 2015;15(2):119–133. [Google Scholar]
- Maynard D.W., McDonald T.A., Stickle T. Parents as a team: Mother, father, a child with autism spectrum disorder, and a spinning toy. Journal of Autism and Developmental Disorders. 2016;46(2):406–423. doi: 10.1007/s10803-015-2568-5. [DOI] [PubMed] [Google Scholar]
- McHale J.P., Lindahl K.M. American Psychological Association; 2011. Coparenting: A conceptual and clinical examination of family systems. [Google Scholar]
- McHale J.P., Rotman T. Is seeing believing?: Expectant parents’ outlooks on coparenting and later coparenting solidarity. Infant Behavior & Development. 2007;30(1):63–81. doi: 10.1016/j.infbeh.2006.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrill M.I., Hines D.A., Mahmood S., Cordova J.V. Pathways between marriage and parenting for wives and husbands: The role of coparenting. Family Process. 2010;49(1):59–73. doi: 10.1111/j.1545-5300.2010.01308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narzisi A. Handle the autism spectrum condition during coronavirus (COVID-19) Stay At home period: Ten tips for helping parents and caregivers of young children. Brain Sciences. 2020;10(4):207. doi: 10.3390/brainsci10040207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neece C.L., Green S.A., Baker B.L. Parenting stress and child behavior problems: A transactional relationship across time. American Journal on Intellectual and Developmental Disabilities. 2012;117(1):48–66. doi: 10.1352/1944-7558-117.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nonweiler J., Rattray F., Baulcomb J., Happé F., Absoud M. Prevalence and associated factors of emotional and behavioural difficulties during COVID-19 pandemic in children with neurodevelopmental disorders. Children. 2020;7(9):128. doi: 10.3390/children7090128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qualtrics, Provo, UT, USA. https://www.qualtrics.com.
- Richters J.E. Depressed mothers as informants about their children: A critical review of the evidence for distortion. Psychological Bulletin. 1992;112(3):485. doi: 10.1037/0033-2909.112.3.485. [DOI] [PubMed] [Google Scholar]
- Rodger S., Umaibalan V. The routines and rituals of families of typically developing children compared with families of children with autism spectrum disorder: An exploratory study. The British Journal of Occupational Therapy. 2011;74(1):20–26. [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M.…Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Globalization and Health. 2020;16(1):1–11. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaaf R.C., Toth-Cohen S., Johnson S.L., Outten G., Benevides T.W. The everyday routines of families of children with autism examining the impact of sensory processing difficulties on the family. Autism. 2011;15:373–389. doi: 10.1177/1362361310386505. [DOI] [PubMed] [Google Scholar]
- Spinelli A., Pellino G. COVID‐19 pandemic: perspectives on an unfolding crisis. The British Journal of Surgery. 2020 doi: 10.1002/bjs.11627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Theule J., Wiener J., Tannock R., Jenkins J.M. Parenting stress in families of children with ADHD: A meta-analysis. Journal of Emotional and Behavioral Disorders. 2013;21(1):3–17. [Google Scholar]
- Tomanik S., Harris G.E., Hawkins J. The relationship between behaviours exhibited by children with autism and maternal stress. Journal of Intellectual & Developmental Disability. 2004;29(1):16–26. [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395(10228):945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willner P., Rose J., Stenfert Kroese B., Murphy G.H., Langdon P.E., Clifford C.…Cooper V. Effect of the COVID‐19 pandemic on the mental health of carers of people with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities. 2020 doi: 10.1111/jar.12811. [DOI] [PubMed] [Google Scholar]
- Zelman J.J., Ferro M.A. The parental stress scale: Psychometric properties in families of children with chronic health conditions. Family Relations. 2018;67(2):240–252. [Google Scholar]
- Zhang J., Litvinova M., Liang Y., Wang Y., Wang W., Zhao S.…Ajelli M. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science. 2020;368:1481–1486. doi: 10.1126/science.abb8001. [DOI] [PMC free article] [PubMed] [Google Scholar]