Abstract
This study aimed to analyze the possible impacts on the prison population's mental health in the context of the new COVID-19 pandemic. Qualitative study was carried out following a lexical and content analysis using the software IRaMuTeQ, version 0.7 alpha 2, in the speech of the short communication and headlines from newspapers. Three groups emerged from the analysis: “spatial conditions for infection” (39.2% of the text segments); “disease outbreaks in prisons” (30,4%) and “public responsibility” (30,4%). Precarious conditions of prisons, high rate of infections and psychiatric illnesses, and lack of government assistance are issues that should be given special attention in order to formulate health promotion and prevention policies focusing on mental health in prison population.
Keywords: Coronavirus infection, Health promotion, Mental health, Prison, Public health
1. Introduction
Over 2548,885 people are held in penal institutions throughout the world, according to the latest edition of the World Prison Population List (BBC, 2020). The United States is the world leader in incarceration with 737 prisoners per 100,000 people, followed by Russia (615), Ukraine (350), South Africa (334), Poland (235), Mexico (196), and Brazil (195) (World Population Review, 2020).
According to the World Health Organization (WHO), imprisonment harms mental health. Overcrowding, various forms of violence, enforced solitude, lack of privacy, lack of meaningful activity, isolation from social networks, insecurity about prospects (work, relationships), and inadequate health services, especially mental health ones, damage mental health. The prevalence of poor mental health among prisoners is considerably higher than in the community, and studies worldwide have shown that suicide rates in prisons are up to 10 times higher than those in the general population (WHO, 2020a). Hence, the already fragile situation of minorities (including refugees and prisoners) has become a worry and has been challenged in the face of the new coronavirus, SARS-CoV-2 (COVID-19) pandemic, which occurred in Wuhan, China, in December of 2019 (Gonçalves Júnior et al., 2020).
Accelerated by human migration, exported cases of COVID-19 have been reported in several regions of the world, including Europe, Asia, North America, and Oceania (Anzai et al., 2020). As of May 01 of 2020, a total of 3175,207 cases have been confirmed in 215 countries with 224,172 deaths (WHO, 2020b).
Since the beginning of the COVID-19 pandemic, the mental health of prisoners has been a public health issue. Routine changes had a major impact on the general population's mental health, but these changes were much more aggressive in populations in a state of social vulnerability, such as prisoners. Therefore, this study aimed to analyze, through lexical and content analysis techniques from recent original publications, the possible impacts of the new COVID-19 pandemic in prison population's mental health. Moreover, a lexical analysis could be considered as a complementary approach to a thematic analysis once it allows a deeper investigation of textual data.
2. Method
2.1. Design and participants
A qualitative study whose sample (not probabilistic, i.e. convenience) was made up of brief communications was carried out in PubMed and Virtual Health Library (VHL), which hosts recognized databases – LILACS (Literatura Latino-americana e do Caribe em Ciências da Saúde), MEDLINE and SciELO (Scientific Electronic Library Online). It was complemented by the selection of headlines in the world's top five newspapers, according to the “2019 Newspaper Web Ranking” by the 4th International Media and Newspaper (2019): The New York Times, The Guardian, The Wall Street Journal, The Daily Mail, Kompas and Liberty Times.
2.2. Procedure
Data were collected in two phases: (1) in databases, in which the following descriptors were used: #1 "coronavirus infections" [MeSH] AND #2 "prison" [MeSH] AND #3 “mental health" [MeSH]; #1 AND #3, as well as their equivalents in the Portuguese and Spanish languages; (2) in newspapers, in the order in which they were cited in the text above, they were searched for in their headlines with the words "coronavirus infections" AND "prison" AND “mental health” that referred the mental health situations of prisoners during the SARS-CoV-2 pandemic.
2.3. Eligibility criteria
The period reported in the literature ranged from December 2019 to March 2020 for the two phases, because this was the starting date of the pandemic. Compilation of the data was performed in April of 2020. The manuscript and newspaper selection occurred primarily through the analysis of abstracts (for papers) and titles. The analysis followed some eligibility criteria: being in English, Portuguese or Spanish; address psychiatric impact of COVID-19 pandemic on prisoners; in the case of articles, whose full text is available through the Portal of Journals from CAPES (Coordination of Personal Improvement of Higher Level), a virtual library was created by the Brazilian Department of Health where content is restricted to authorized users. Monographs, dissertations, and theses were excluded. Manuscripts or news repeated in more than one of the databases were counted only once. Some articles and news were excluded because they generally approached the mental health of prisoners in other viruses/pandemics.
To ensure trustworthiness of the findings, data were collected individually, by two researchers, and their divergences were solved by a third senior researcher.
2.4. Data analysis
After tabulation, data were processed by using the IRaMuTeQ (Interface de R pour les Analyses Multidimensionnelles de Textes et de Questionnaires) software, version 0.7 alpha 2, developed by Pierre Ratinaud, which allows statistical analysis of textual corpus and individual tables/words (Mendes et al., 2016). IRaMuTeQ provides five types of analysis: classical textual statistics; research regarding group specificities; descending hierarchical rank; similarity analysis; and word cloud (Camargo and Justo, 2013; Castro et al., 2014; Santos et al., 2017).
The abstracts and headlines were transformed into three corpora named by the letter “A” and assessed through similarity, word cloud, confirmatory factorial analysis (CFA), and descendent hierarchical classification (DHC) (Camargo and Justo, 2013; Castro et al., 2014).
Before the analysis, in the text segment parameters, only “full” language elements were selected as assets: adjectives, unrecognized forms, nouns, verbs, as well as auxiliary nouns and verbs such as complementary (supplementary), with the aim of enriching text content.
2.5. Ethical issues
Considering this is a qualitative study with public domain information, Resolution 510/16 of the Brazilian National Health Council (CNS, acronym in Portuguese) ensures the dispensation of submission to a Human Beings Research Ethics Committee. The ethical criteria of the Declaration of Helsinki and international standards were observed.
3. Results
In the first-phase research strategy, three articles were found and two were selected in PubMed, whereas three articles were found in the VHL, but any of these texts was selected because one was repeated and the other two were out of context. In the second phase, 16 headlines were found and two were selected in The New York Times, whereas The Wall Street Journal presented four headlines, and two of them were selected. In addition, The Daily Mail had four headlines and Kompas presented six results, but none of them was selected. The Guardian included 881 headlines, of which 12 were selected.
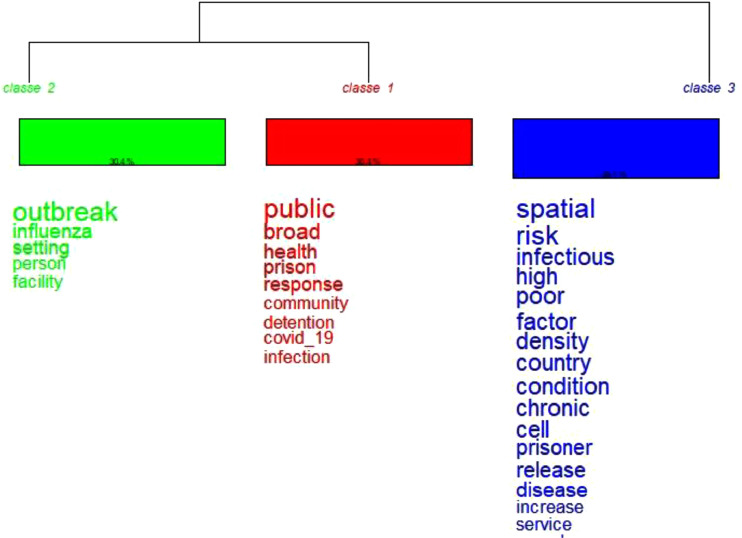
Initially, the corpus was built with three texts separated by 29 text segments, in which only 24 were used (82.76%). The lexicographic analysis of the textual corpus produced 1029 occurrences (words and forms), being 328 active forms. The most frequent active words were prison (n = 32), health (n = 21), Covid_19 (n = 14), outbreak (n = 13), and release (n = 12). Moreover, the DHC of active words produced three lexical classes divided into two major groups, shown in the dendrogram of Fig. 1 .
Fig. 1.
Descending Hierarchical Classification (Reinert Analysis).
The first group, formed by the red and green classes, was the most representative, totaling 60.8% of the text segments (30.4% for each class). Complementarily, the second group presents 39.2% of the text segments. The three lexical classes received the following names: “Disease outbreaks in prisons”, “Public responsibility”, and “Spatial conditions for infection”.
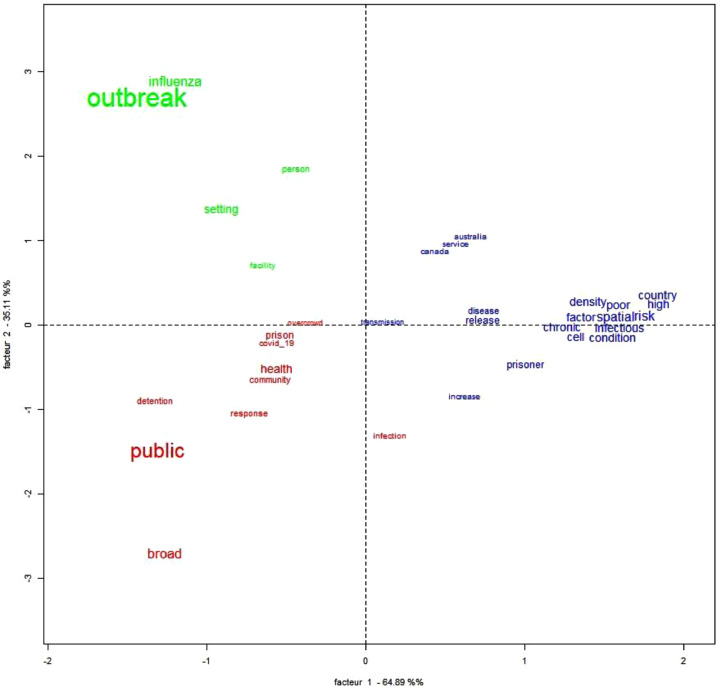
Regarding the confirmatory factorial analysis, two factors explain 35.11 and 64.89% of the model, which are represented on the X and Y axes in Fig. 2 . The two-dimensional view clearly presents three distinct areas, which are directly associated with the three classes previously presented.
Fig. 2.
Correspondence Factorial Analysis regarding prisoners' mental health in the COVID-19 pandemic.
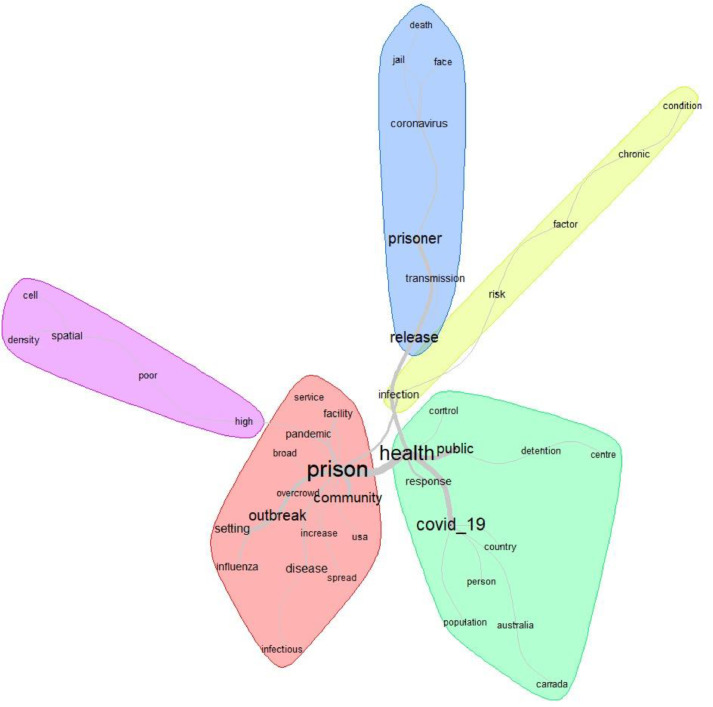
Fig. 3 shows the similitude analysis, using a graph that represents the connection between words in the analyzed textual corpus (Salviati, 2017). In this case, five groups of words were constructed. The first DHC class, “Disease outbreaks in prisons”, is similar to the red group of words. Furthermore, the second class, “Public responsibility”, seems to be related to the green and blue groups of words. Finally, the third class, “Spatial conditions for infection”, is closely associated with the purple and yellow groups.
Fig. 3.
Similitude Dendrogram on prisoners' mental health in the COVID-19 pandemic.
4. Discussion
After the lexical analysis using the DHC, the words in the speeches were evoked and aggregated around common themes. In the blue group (“Spatial conditions for infection”) that presents 39.2% of the text segments, “spatial”, “risk”, “infection”, “high”, “poor” and “density” (Figs. 1 and 2) are references made to the unhealthy conditions to which the prison population is subjected to. In the COVID-19 pandemic, the lack of basic conditions, such as adequate physical space, quality food or pleasant environment, can be enhanced (Ornell et al., 2020) and deteriorate mental health; therefore, people become more vulnerable to get an infection (Gonçalves Júnior et al., 2020) and become mentally ill.
According to Xiang et al. (2020), three main factors should be considered when developing mental health strategies in the COVID-19 pandemic: multidisciplinary mental health teams (including psychiatrists, psychiatric nurses, clinical psychologists, and other mental health professionals); clear communication involving regular and accurate updates on the COVID-19 outbreak; and safe psychological counseling services (for example, via electronic devices or apps). However, in general, neither the prisoners nor the population have access to effective public health measures to promote mental health.
In the face of the current COVID-19 pandemic situation, prison experiences a major challenge fighting this disease, whose most effective treatment still relies on preventive measures related to personal and public space hygiene, appropriate ventilation and social isolation (Santos et al., 2020) corroborating with an association of words evoked in the blue group.
The second group in Fig. 1 has two great correlated categories (Fig. 2) – red (“Public responsibility”) and green (“Disease outbreak in prison”), which correspond to 60.8% of the text segments and 30.4% for each class. The first group evokes “public”, “response”, “broad”, and “control detention” (Figs. 2 and 3).
In a pandemic, such as the COVID-19, it is important to remember that psychological and psychiatric problems can be triggered or amplified. In addition to the concrete fear of death, the COVID-19 pandemic has had an epidemiological impact both individually and collectively during all phases of the event, increasing the suffering and psychiatric symptom rates of the population, which contributed to increases in the indirect mortality from causes other than the virus (Ornell et al., 2020). Studies in the United States (Yi et al., 2017) and in Brazil (Soares Filho and Bueno, 2016) have reported high rates of depression, life dissatisfaction, heavy drinking, and illicit drug use in prison. A systematic review shows that prisoners have elevated the rates of psychiatric disorders compared with the general population, including for psychosis, personality disorder and risk factors for increased suicide rates, premature mortality on discharge from prison, and increased reoffending rates (Fazel and Seewald, 2012).
Hence, prisoners have many risk factors that make them a quite vulnerable population regarding mental issues. Thus, the Brazilian Government and health authorities have the responsibility of appropriating measures for the prevention and promotion of mental health in a pandemic (Silva et al., 2020). The WHO, in their publication “Good governance for prison health in the 21st century: a policy brief on the organization of prison health”, affirms that: “(i) managing and coordinating all relevant agencies and resources contributing to the health and well-being of prisoners is a whole-of-government responsibility, and (ii) health ministries should provide and be accountable for health care services in prisons and advocate healthy prison conditions” (WHO, 2013). This also included Mental Health according to the Caracas Declaration (1990), which reformulated psychiatric care services in Latin America and the world, changing its paradigms and calling on civil society and local governments to act and take responsibility for psychiatric patients (PAHO, 1990). Therefore, it is the Government's obligation to identify, manage, and care for new cases of COVID-19 (WHO, 2020c) and its consequences, including promotion on mental health, according to the red group.
The green group evokes “outbreak”, “influenza” and “settings” that refer to the overload risk that prison has in acquiring diseases (Figs. 1 and 3). The presence of words that evoke infectious diseases is worrying, considering that psychiatric patients in prisons are extremely more aggressive due to their immunogenetic vulnerability. They can also be exposed to more barriers in accessing timely health services, because of discrimination associated with mental health in health care settings, they are more susceptible to stress compared with the general population (Yao et al., 2020), and they may have difficulties adopting “barrier measures” (behavioral measures to protect oneself and others from the virus) and complying with confinement instructions (Chevance et al., 2020). Besides, most of the 9.8 million people imprisoned worldwide are from the poorest and most marginalized sections of society and are, therefore, more likely to be at greater risk for diseases (Herbert et al., 2012).
5. Conclusions
This study aims to carry out a lexical analysis of recent publications on the relationship between COVID-19 pandemic and prison population's mental health. Therefore, a priori, a search for original paper was conducted. Then, based on the findings, a lexical analysis was performed using IRaMuTeQ software.
From this discursive textual analysis, it appears that the prison population's mental health during the COVID-19 pandemic is negatively influenced by the precarious conditions of the prisons, the high rate of infections and psychiatric illnesses to which this group is subject to. Government must be a fundamental ‘actor’ by assisting with health promotion and prevention policies focusing on mental health.
As a fragility of this study, we can highlight the scarcity of works and papers that approached prison population's mental health, which made the analysis difficult. This fact also provided an overall analysis of prisoners' mental health throughout the world, not allowing for a regional assessment. On the one hand, it shows marginalization/neglect of this population, especially when it comes to their mental health, but on the other hand, it shows the need of greater and better theoretical contributions.
Funding
The authors declare that they have no funding.
CRediT authorship contribution statement
Jucier Gonçalves Júnior: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology. Jair Paulino de Sales: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology. Flaviane Cristine Troglio da Silva: Project administration, Resources, Software, Supervision, Validation. João de Deus Quirino Filho: Project administration, Resources, Software, Supervision, Validation. Rita de Cassia Pires Bezerra Cavalcanti: Project administration, Resources, Software, Supervision, Validation. José Marcondes Macedo Landim: Visualization, Writing - original draft, Writing - review & editing. Nádia Nara Rolim Lima: Visualization, Writing - original draft, Writing - review & editing. Francisco Facundo de Matos Neto: Visualization, Writing - original draft, Writing - review & editing. Fábio Cardoso: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology. Modesto Leite Rolim Neto: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology.
Declaration of Competing Interest
The authors declare that they have no competing interests.
Acknowledgements
The authors would like to thank the Suicidology Research Group from Universidade Federal do Ceará (UFC), Scientific Writing Lab, Medicine School – Universidade Federal of Cariri (UFCA) and the Brazilian National Council for Scientific and Technological Development (CNPq) – institution linked to the Brazilian Department of Science, Technology and Scientific Writing Lab, Medicine School – Universidade Federal of Cariri (UFCA).
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113669.
Appendix. Supplementary materials
References
- Anzai A., et al. Assessing the impact of reduced travel on exportation dynamics of Novel Coronavirus infection (COVID-19) J. Clin. Med. 2020;9:601. doi: 10.3390/jcm9020601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camargo B.V., Justo A.M. IRAMUTEQ: um software gratuito para análise de dados textuais. Temas. Psicol. 2013;21:513–518. doi: 10.9788/TP2013.2-16. [DOI] [Google Scholar]
- Castro A., Koelzer L.P., Camargo B.V., Bousfield A.B.S. Representações sociais na internet sobre cotas para negros em universidades federais. Cad. Pesq. Inter. Cis. Hums. 2014;15:201–220. doi: 10.5007/1984-8951.2014v15n106p202. [DOI] [Google Scholar]
- Chevance, et al. Ensuring mental health care during the SARS-CoV-2 epidemic in France: a narrative review. L. Encéphale. 2020:S0013–S7006. doi: 10.1016/j.encep.2020.04.005. 30073-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4th International Media and Newspaper, 2019. 2019 Newspaper Web Rankings. https://www.4imn.com/top200/ (Accessed 26 April 2020).
- Fazel S., Seewald K. Severe mental illness in 33 588 prisoners worldwide: systematic review and metaregression analysis. Br. J. Psychiatry. 2012;200:364–373. doi: 10.1192/bjp.bp.111.096370. [DOI] [PubMed] [Google Scholar]
- Gonçalves Júnior J., et al. A crisis within the crisis: the mental health situation of refugees in the world during the 2019 coronavirus (2019-nCoV) outbreak. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.113000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert K., Plugge E., Foster C., Doll H. Prevalence of risk factors for non-communicable diseases in prison populations worldwide: a systematic review. Lancet. 2012;379:1975–1982. doi: 10.1016/s0140-6736(12)60319-5. [DOI] [PubMed] [Google Scholar]
- Mendes F.R.P., et al. Representações sociais dos estudantes de enfermagem sobre assistência hospitalar e atenção primária. Rev. Bras. Enferm. 2016;69:343–350. doi: 10.1590/0034-7167.2016690218i. [DOI] [PubMed] [Google Scholar]
- Salviati, M.E., 2017. Manual do Aplicativo IRAMUTEQ. Versão 0.7 Alpha 2 e R Versão 3.2.3. http://www.iramuteq.org/documentation/fichiers/manual-do-aplicativo-iramuteq-par-maria-elisabeth-salviati.
- Ornell F., et al. Pandemic fear and COVID-19: mental health burden and strategies. Braz. J. Psychiat. 2020 doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang Y.T., et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatr. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos A.B.S., Vasconcelos E., Cardoso P.R. first edition. Sociedade Brasileira de Medicina de Família e Comunidade; Rio de Janeiro: 2020. Measures and guidelines against covid-19 in prisons; p. 15.https://www.sbmfc.org.br/wp-content/uploads/2020/04/Measures-and-guidelines-against-COVID-19-in-prisons.pdf [Google Scholar]
- Santos V., et al. IRAMUTEQ nas pesquisas qualitativas brasileiras da área da saúde: scoping review. Atas CIAIQ. 2017;2:392–401. [Google Scholar]
- Soares Filho M.M., Bueno P.M.M.G. Demography, vulnerabilities and right to health to Brazilian prison population. Ciênc. Saúde Coletiva. 2016;21:1999–2010. doi: 10.1590/1413-81232015217.24102015. [DOI] [PubMed] [Google Scholar]
- World Population Review, 2020. Incarceration rates by country 2020. https://worldpopulationreview.com/countries/incarceration-rates-by-country/.
- World Health Organization – WHO, 2013. Regional Office for Europe, 2013. Good governance for prison health in the 21st century: a policy brief on the organization of prison health. https://apps.who.int/iris/handle/10665/326388.
- PAHO – Pan American Health Organization. World Health Organization, 1990. Declaração de Caracas. Caracas. https://bvsms.saude.gov.br/bvs/publicacoes/declaracao_caracas.pdf(accessed 26 April 2020).
- World Health Organization – WHO, 2020a. Mental Health. http://www.euro.who.int/en/health-topics/health-determinants/prisons-and-health/focus-areas/mental-health (accessed 26 April 2020).
- World Health Organization – WHO, 2020 b. Coronavirus disease (COVID-19) outbreak situation, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- World Health Organization – WHO, 2020 c. Preparedness, prevention and control of COVID-19 in prisons and other places of detention. http://www.euro.who.int/en/health-topics/health-determinants/prisons-and-health/publications/2020/preparedness,-prevention-and-control-of-covid-19-in-prisons-and-other-places-of-detention-2020.
- Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiat. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi Y., Turney K., Wildeman C. Mental Health among jail and prison inmates. Am. J. Mens. Health. 2017;11:900–909. doi: 10.1177/1557988316681339. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.