Background:
The coronavirus disease 2019 (COVID-19) pandemic has affected people of all ages, races, and socioeconomic groups, and placed extraordinary stress on health care workers (HCWs). We measured the prevalence of burnout and assessed wellbeing and quality of life (QoL) in HCWs at a single UK neuroscience center after the first pandemic surge.
Methods:
A 38-item electronic questionnaire was disseminated through local team email lists between May 22 and June 7, 2020, to HCWs in a university neurosciences center. Burnout was measured using the single-item Emotional Exhaustion and Depersonalization scales, and wellbeing and QoL assessed using the Linear Analogue Self-Assessment Scale and the EuroQol-5 Dimension instrument.
Results:
The response rate was 57.4% (n=234); 58.2% of respondents were nurses, 69.4% were women and 40.1% were aged 25 to 34 years. Overall, 21.4% of respondents reported burnout assessed by the Emotional Exhaustion scale; burnout was higher for nurses (23.5%) and allied health care professionals (22.5%) compared with doctors (16.4%). HCWs from ethnic minority groups reported a higher rate of burnout (24.5%) compared with white HCWs (15.0%). There were no differences in reported wellbeing or QoL between professional groups, or HCW age, sex, or race. Nurses (36.8%) and staff from ethnic minority groups (34.6%) were more fearful for their health than others.
Conclusions:
Our findings highlight the prevalence of HCW burnout after the first surge of the pandemic, with an increased risk of burnout among nurses and staff from ethnic minority groups. Both nursing and staff from ethnic minority groups were also more fearful for their health. With ongoing pandemic surges, the impact on HCW wellbeing should be continuously assessed to ensure that local strategies to support staff wellbeing are diverse and inclusive.
Key Words: COVID-19, burnout, wellbeing, intensive care, health care workers, neuroscience
Coronavirus disease 2019 (COVID-19), caused by the novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), first emerged in Wuhan, China in December 2019.1 As at January 2021, over 95 million cases have been reported worldwide with over 3 million cases in the UK.2 COVID-19 continues to be a serious concern, affecting people of all ages, races, and socioeconomic groups, and disrupting many aspects of daily life.
A secondary analysis of a UK longitudinal population study on personal wellbeing found that by late April 2020 (6 wk after the beginning of the national first lockdown) levels of depression and anxiety had increased compared with pre–COVID-19 levels.3 It is postulated that this trend will continue as the pandemic progresses, owing to growing concerns especially around unemployment and financial stability. Recent studies investigating the mental health and wellbeing of UK health care workers (HCWs), conducted before the COVID-19 pandemic, found that staff were demoralized as well as mentally and physically exhausted. Staff reported having experienced work-related stress and burnout due to increasing demands, reducing staffing levels, and more limited resources.4–6 Evidence from previous epidemics and pandemics highlight the extraordinary additional stress related to the high risk of infection, stigmatization, workload, and general uncertainty experienced by HCWs, with a resultant increased risk of deterioration in their wellbeing.7
As part of the local pandemic surge response, our institution repurposed and expanded its neurointensive care unit to manage (non-neurological) patients with severe COVID-19 while retaining the capacity for patients with neurosurgical and neurological emergencies.8 Staff from multiple professional groups were redeployed to the neurocritical care unit as part of this surge response. Subsequently, we invited all staff at our institution that had cared for COVID-19 patients in any clinical area to participate in an electronic survey to assess their wellbeing. Our primary objective was to measure the prevalence of burnout and to compare prevalence between staff groups.9 Secondary objectives were assessment of wellbeing and quality of life (QoL), as well as their predictors.
METHODS
We developed a cross-sectional, self-reporting, anonymized survey designed to assess the wellbeing of HCWs at a tertiary neuroscience center in the UK after the initial COVID-19 pandemic surge. This observational study was registered as a local service evaluation (17-202021-SE), and in keeping with local guidelines no formal ethics review was required. Consent was implied through participation. Our findings are presented using the STROBE reporting guidelines.
The survey was conducted using SurveyMonkey and disseminated through local team email lists between May 2 and June 7, 2020. Three reminders were sent. All health care staff working at our hospital during the first pandemic surge were invited to participate in the survey; this included all grades of doctors, nurses, and allied health professionals (AHPs). During the surge response, HCWs rotated between managing patients in COVID-19 and non–COVID-19 areas.
Survey Development
The 38-item survey was developed by a multidisciplinary group comprising 2 consultant neuroanesthesiologists, 2 consultant neurosurgeons, 1 neuroanesthesiology fellow, 1 neurosurgical specialist registrar, and 1 senior clinical nurse specialist. The questions were designed to cover the following areas: (a) sociodemographics; (b) working hours during the pandemic surge; (c) training, redeployment, and access to personal protective equipment; (d) experience of personal risk, and: (e) psychological state assessed using previously validated questions9–11 incorporating Likert scales, Visual Analogue Scales (VAS) and dichotomous answers (Supplementary Digital Content: Survey Questions, http://links.lww.com/JNA/A367). Unsocial hours were defined as hours worked outside usual working hours, including night shifts, weekends, and public holidays. Normal working hours varied between staff groups and ranged from 6 am to 8 pm. The survey was peer-reviewed and piloted by a local 15-member multidisciplinary research group before dissemination. The pilot survey assessed the feasibility, ease of use, and appropriateness of the questions.
Outcome Measures
Our primary objective was to measure the prevalence of burnout using the single-item Emotional Exhaustion (EE) and Depersonalization (DP) scales,9 and to compare the prevalence between staff groups. Secondary objectives were: (a) assessment of wellbeing using the Linear Analogue Self-Assessment (LASA) Scale,10 (b) assessment of health-related QoL using the EuroQol-5 Dimension (EQ-5D),11 instrument (c) reporting of personal risk and fatigue, and (d) predictors of wellbeing.
Burnout and QoL were assessed using 3 validated instruments.9–11 The single-item EE and DP scales9 combine to form a 2-item abbreviation of the Maslach Burnout Inventory-Human Services Survey (the gold standard for burnout assessment) using a 7-point (0 to 6) Likert scale to measure burnout. The 2 items are “I feel burned out from my work” (EE) and “I have become more callous towards people since I took this job” (DP). A score >3 for either item risk stratifies high burnout symptom burden and defines overall burnout, with results consistent with the full Maslach Burnout Inventory-Human Services Survey instrument. The LASA Scale10 is a measure of QoL consisting of 5 single items assessing physical, emotional, spiritual, intellectual, and overall wellbeing. Respondents rate their perceived level of functioning on an 11-point Likert scale (0: “as bad as it can be” to 10: “as good as it can be”) for each domain; a score ≤5 indicates a clinically significant deficit in overall QoL. The EQ-5D11 is a standardized measure of health-related QoL developed by the EuroQol group to provide a simple, generic measure of health; permission was granted for use. The instrument comprises a questionnaire across 5 domains: mobility, self-care, usual activities, pain and anxiety/depression, and a VAS (0 to 100: “the worst health [0] and the best health [100] health you can imagine”) recording an overall self-rated health assessment. Health state is represented by a single summary index reflecting how good or bad an individual’s health state is compared with the general population of a country, and the VAS score.
Statistical Analysis
Data were recorded using SurveyMonkey graphical tools and Microsoft Excel (v16.43.1). Data are presented as mean (±SD) and percentage for noncategorical and categorical data, respectively. Differences in categorical variables were assessed using the χ2 test and analysis of variance was used to compare means. Statistical analysis was performed using Stata software (STATA 13; StataCorp, College Station, TX). A P-value <0.05 was considered to be statistically significant.
RESULTS
There were 234 survey respondents and 215 complete responses. The overall response rate was 57.4% (doctors=56.5%, nursing staff=61.7%, and AHPs=52.9%). Respondent characteristics and working patterns are shown in Table 1. The majority of respondents were nurses (58.2%), women (69.4%), and aged between 25 and 34 years (40.1%). Overall, 46.1% of respondents were white, 24.1% were Asian, 6.9% were black, and 7.3% were mixed race.
TABLE 1.
Respondent Characteristics and Working Patterns
| n (%) | |
|---|---|
| Demographics | |
| Women | 161 (69.4) |
| Race/ethnicity | |
| Asian/Asian British | 56 (24.1) |
| Black/Black British | 16 (6.9) |
| Mixed race | 17 (7.3) |
| White | 107 (46.1) |
| Prefer not to say | 19 (8.2) |
| Other | 17 (7.3) |
| Age (y) | |
| 18-24 | 7 (3) |
| 25-34 | 93 (40.1) |
| 35-44 | 68 (29.3) |
| 45-54 | 52 (22.4) |
| 55-64 | 12 (5.2) |
| 65+ | |
| Clinical department | |
| Anesthetics | 38 (16.4) |
| Operating department | 23 (9.9) |
| Neurocritical care | 80 (34.5) |
| Neurosurgery | 66 (28.5) |
| Neurology | 23 (9.9) |
| Physiotherapy | 15 (6.5) |
| Nursing | 27 (11.6) |
| Other | 9 (3.9) |
| Professional group | |
| Consultant (doctor) | 30 (12.9) |
| Fellow/registrar (doctor) | 24 (10.3) |
| Senior house officer (doctor) | 11 (4.7) |
| Nurse | 135 (58.2) |
| Health care assistant | 10 (4.3) |
| Operating department practitioner | 4 (1.7) |
| Physiotherapist | 17 (7.3) |
| Other | 1 (0.4) |
| Working patterns | |
| Approximate extended hours/week being worked during COVID-19 (h) | |
| 0-5 | 50 (21.8) |
| 6-10 | 29 (12.7) |
| 11-15 | 13 (5.7) |
| 16-20 | 4 (1.8) |
| >20 | 10 (4.4) |
| Not applicable | 123 (53.7) |
| Working more antisocial hours during COVID-19 | |
| Strongly agree | 50 (21.8) |
| Agree | 58 (25.3) |
| Neither agree nor disagree | 54 (23.6) |
| Disagree | 46 (20.1) |
| Strongly disagree | 21 (9.2) |
COVID-19 indicates coronavirus disease 2019.
Most respondents (65.5%) did not work beyond their contracted hours during the pandemic surge. If they did work additional hours, the most common perceived increase in workload was up to 5 hours per week (21.8%). Increased working hours were most frequently reported by AHPs (82.3%). Overall, 44.6% of respondents agreed or strongly agreed that they were working more unsocial hours. Overall, 42.8% of respondents were redeployed outside their usual area of practice, of which 68.2% were redeployed to the neurocritical care unit.
Primary Objective
The overall prevalence of burnout measured using the EE and DP scales was 21.4% and 12.1%, respectively. When assessed using the EE scale, nurses and AHPs reported higher rates of burnout compared with doctors (23.5% vs. 20% vs. 16.4%, respectively), whereas doctors reported higher rates than nurses and AHPs when burnout was assessed using the DP scale (18% vs. 11.2% vs. 6.7%, respectively) (Fig. 1). There was a higher incidence of burnout measured by EE (24.5% vs. 15%) and DP (17.6% vs. 7%) in HCWs from ethnic minority groups compared with white HCWs. By age, the highest prevalence of burnout assessed using EE was among HCWs aged between 35 and 44 years (24.5%) and, using DP, in those aged between 45 and 54 years (14.9%). There were no sex-related differences in reported burnout rates.
FIGURE 1.
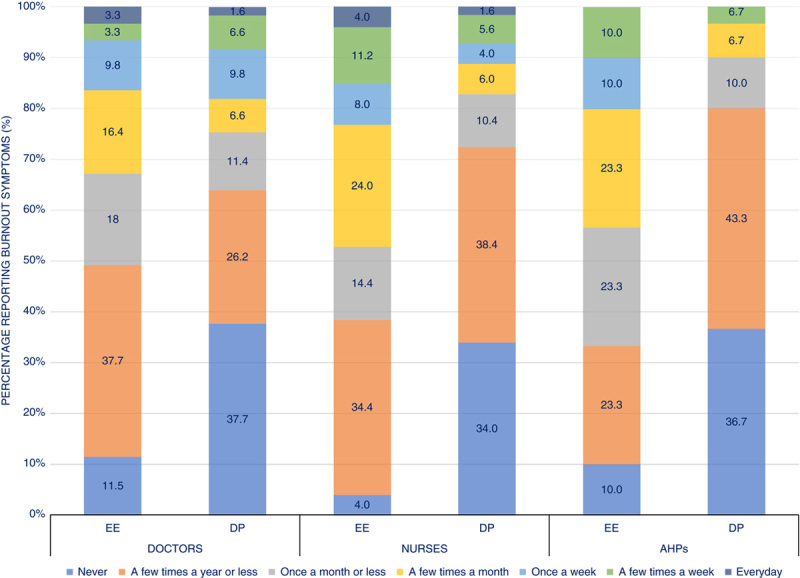
Prevalence of burnout in health care workers. Burnout was defined by the EE and DP scales.9 “Once a week” or more frequently is used to indicate burnout. AHP indicates allied health professional; EE, Emotional Exhaustion Score; DP, Depersonalization Score.
Secondary Objectives
Overall mean (SD) LASA score was 6.92 (1.8); there was no difference in wellbeing between professional groups, or in HCWs of different ages, sex, or race (Table 2). The total EQ-5D summary index was 0.89 and the mean (SD) VAS was 82.1 (15.9). Again, there was no significant difference between professional groups, age groups, or by sex, or race. Overall, 26.7% of respondents reported that their personal health was at risk “often” or “all of the time” during the pandemic, with 46.1% similarly worried about the potential risk to family and loved ones. Overall, 65.4% of respondents had witnessed loved ones, friends, or colleagues become ill with COVID-19. Nurses were more worried for their own health when compared with AHPs and doctors (36.8% vs. 23.1% vs. 14.8%, respectively), and there were higher rates of “fear for health” among ethnic minorities compared with white HCW groups (34.6% vs. 15%). Overall, 24.4% of respondents reported insufficient sleep during the pandemic, and 40.9% that their communication had been poor (a subjective determination) due to workplace fatigue.
TABLE 2.
Quality of Life and Wellbeing Scores Among Health Care Workers
| N | Total Population | Doctors | Nurses | AHPs | P | |
|---|---|---|---|---|---|---|
| Health-related quality of life11 | ||||||
| EQ-5D VAS* | ||||||
| Mean (±SD) | 231 | 82.1 (15.9) | 83.4 (11.2) | 80.5 (18.4) | 86.3 (12.5) | 0.15 |
| EQ-5D summary index* | 231 | 0.89 | 0.90 | 0.89 | 0.89 | — |
| Linear Analogue Self-Assessment Scale (wellbeing), mean (±SD)10 | ||||||
| Overall | 215 | 6.92 (1.8) | 7.1 (1.6) | 6.8 (1.9) | 7.1 (1.9) | 0.49 |
| Physical | 215 | 7.0 (1.99) | 7.4 (1.7) | 6.8 (2.1) | 7.3 (2.0) | 0.12 |
| Emotional | 215 | 6.48 (2.1) | 6.8 (1.9) | 6.3 (2.1) | 6.6 (2.3) | 0.27 |
| Spiritual | 215 | 7.0 (2.5) | 7.1 (2.4) | 6.9 (2.6) | 7.3 (2.7) | 0.68 |
| Intellectual | 215 | 7.1 (1.92) | 7.2 (1.9) | 7.0 (1.9) | 7.2 (2.9) | 0.77 |
EQ-5D UK summary index=0.86, VAS=82.7.
AHP indicates allied health professional; EQ-5D, EuroQol-5 Dimension; VAS, Visual Analogue Score.
Nurses were more likely to feel unprepared for the pandemic; 28% of nurse respondents felt “completely “or “somewhat unprepared” compared with 21.4% of AHPs and 18.1% of doctors. Most respondents (78.9%) felt that their colleagues were supportive during the pandemic and that they had worked well together either “often” or “all of the time.” In total, 79.2% believed their work was “worthwhile and meaningful.” Overall, 90.9% of respondents received training for donning and doffing personal protective equipment, and 78.4% on the use of personal protective equipment during aerosol-generating procedures.
DISCUSSION
This study investigated the prevalence of burnout and wellbeing in HCWs at a neuroscience center in the UK. The overall prevalence of burnout among staff was 21.4% and 12.1%, measured using the EE and DP scales, respectively. Nursing staff and ethnic minority groups reported higher rates of burnout compared with other professional and racial groups. Both nursing and ethnic minority cohorts were also more likely to be worried or fearful for personal and family health. The overall scores for wellbeing and QoL measured using the LASA score (6.92) and EQ-5D (82.1, summary index=0.89) were similar to general population norms (LASA=7.00 and EQ-5D=82.8, summary index=0.86).12
A study investigating a UK intensive care unit health care population before the pandemic found that over one third were at high risk for burnout.13 Nursing staff had a higher incidence of burnout (50.0%) compared with doctors (34.6%) when assessed using the EE score, and more nurses scored as “high risk.”13 During the pandemic peak in Wuhan, China, Hu et al14 reported that 41.5% of the frontline nursing staff had a high EE score and 27.6% a high DP score, which are indicative of high burnout rates. Although burnout was common in our survey, its incidence was lower than previously reported despite feelings of unpreparedness for the pandemic among staff, high levels of staff redeployment and changes to working practices and patterns including those generated by the repurposing and expansion of the neurocritical care unit. The lower incidence of burnout reported in our study might be a reflection of local organizational responses to the pandemic and other circumstances unique to our institution, including our program of intensive staff engagement, education, and training during the local pandemic surge response.8 The prevalence of burnout reported in this survey is measured at a single time point in an ongoing pandemic and, for a more complete picture, ongoing assessment of wellbeing and burnout is required.
Fears for health and workplace fatigue have frequently been identified among HCWs during the pandemic. Hu et al14 identified high levels of fear of COVID-19 infection and transmission to loved ones in 63.2% of frontline nurses. Studies from China15 and Italy,16 two of the earliest affected nations, reported that a considerable proportion of HCWs providing care for patients with COVID-19 experienced symptoms of insomnia (34% and 8.3%, respectively), depression (50.4% and 24.7%, respectively), anxiety (44.6% and 19.8%, respectively), and distress (71.5% and 21.9%, respectively).
In the UK, Public Health England identified disproportionately high levels of mortality from COVID-19 among ethnic minority populations, and that more than one third of patients admitted to intensive care units with COVID-19 were from ethnic minority groups despite such groups constituting only 17% of the UK population.17 Surveys conducted by the Royal College of Physicians, the British Medical Association, and the Royal College of Nursing in the UK, all identified and highlighted common themes among their ethnic minority members: (a) increased concerns for safety, especially due to lack of personal protective equipment; (b) lack of confidence that enough was being done to protect them; and (c) fear of raising concerns owing to organizational culture.18–20 These findings are reflected in our survey which found that ethnic minority staff were more fearful for personal and family health; although, this was not reflected in wellbeing scores or self-reported QoL.
Our survey has several limitations. First, it is a survey of frontline HCWs managing COVID-19 in a neuroscience center so the survey population may be subject to selection bias. We did not measure all factors that could have contributed to burnout and the responses may also be reflective of bias; those with burnout may be more or less likely to respond. Second, the survey was designed as a single-center snapshot, thereby limiting the generalizability of its findings. Third, as a cross-sectional study, it is difficult to infer causality; only associations can be inferred. We also did not involve a neuropsychology expert in the survey development. Finally, we are unaware of the prepandemic prevalence of burnout in our survey population and thus unable to assess any changes that might have resulted as a direct result of the pandemic and our local response to it.
CONCLUSIONS
Although levels of burnout among frontline workers at our institution appear to be lower than those reported in previous studies, we identified an increased risk of burnout among nurses and staff from ethnic minority groups. Moreover, both nursing and ethnic minority staff reported an increased fear for personal and family health. Our findings highlight the importance of clear strategies to support staff wellbeing and the need for ongoing assessment during and after this pandemic.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.jnsa.com.
ACKNOWLEDGMENTS
The authors acknowledge the support and hard work of all staff working in the neurocritical care unit, operating department, and in the neurosurgery and neuroanesthesiology teams during the pandemic. Without their dedication and professionalism, it would not have been possible to maintain a clinical service for our patients.
Footnotes
Data from this study was presented at the Annual Society for Neuroscience in Anesthesiology and Critical Care conference, September 11-13, 2020.
H.J.M. is funded by the Wellcome Centre for Interventional and Surgical Sciences and the National Institute of Health Research Biomedical Research Centre.
The authors have no conflicts of interest to declare.
Contributor Information
Deborah R. Douglas, Email: douglas.deborahr@gmail.com.
David Choi, Email: David.choi@nhs.net.
Hani J. Marcus, Email: h.marcus@ucl.ac.uk.
Will Muirhead, Email: w.muirhead@ucl.ac.uk.
Ugan Reddy, Email: ugan.reddy@nhs.net.
Trudy Stewart, Email: trudy.stewart1@nhs.net.
Astri M.V. Luoma, Email: val.luoma@nhs.net.
REFERENCES
- 1. World Health Organization Rolling updates on Coronavirus Disease (COVID-19). 2020. Available at: www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen . Accessed November 19, 2020.
- 2. European Centre for Disease Prevention and Control. COVID-19 situation update worldwide. 2020. Available at: www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases . Accessed January 25, 2021.
- 3. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Copeland A. NHS Sickness absence: let’s talk about mental health. King’s Fund Blog. 2019. Available at: www.kingsfund.org.uk/blog/2019/10/nhs-sickness-absence . Accessed November 19, 2020.
- 5. Health Education England. NHS staff and learners’ mental wellbeing commission report; 2019. Available at: www.hee.nhs.uk/our-work/mental-wellbeing-report . Accessed November 19, 2020.
- 6. Brooks SK, Gerada C, Chalder T. Review of literature on the mental health of doctors: are specialist services needed? J Ment Health. 2011;20:146–156. doi: 10.3109/09638237.2010.541300 [DOI] [PubMed] [Google Scholar]
- 7. Preti E, Di Mattei V, Perego G, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. 2020;22:1–22. doi: 10.1007/s11920-020-01166-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Raith EP, Luoma AMV, Earl M, et al. Repurposing a neurocritical care unit for the management of severely ill patients with COVID-19: a retrospective evaluation. J Neurosurg Anesthesiol. 2021;33:77–81. doi: 10.1097/ana.0000000000000727 [DOI] [PubMed] [Google Scholar]
- 9. West CP, Dyrbye LN, Satele DV, et al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27:1445–1452. doi: 10.1007/s11606-012-2015-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lall MD, Gaeta TJ, Chung AS, et al. Assessment of physician well-being, part two: beyond burnout. West J Emerg Med. 2019;20:291–304. doi: 10.5811/westjem.2019.1.39666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. EuroQol Group. EuroQol: a new facility for the measure ment of health related quality of life. Health Policy Open. 2000;16:199–208. doi: 10.1016/0168-8510(90)90421-9 [DOI] [PubMed] [Google Scholar]
- 12. Szende A, Janssen B. Cabases J. Cross-country analysis of EQ-5D data. Self-reported Population Health: An International Perspective Based on EQ-5D. New York, London: Springer, Dordrecht, Heidelberg; 2014:31–36. [Google Scholar]
- 13. Vincent L, Brindley PG, Highfield J, et al. Burnout syndrome in UK intensive care unit staff: data from all three burnout syndrome domains and across professional groups, genders and ages. J Intensive Care Soc. 2019;20:363–369. doi: 10.1177/1751143719860391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hu D, Kong Y, Li W, et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalMedicine. 2020;24:100424. doi: 10.1016/j.eclinm.2020.100424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976–e203976. doi: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rossi R, Socci V, Pacitti F, et al. Mental health outcomes among front and second line health workers associated with the COVID-19 pandemic in Italy. JAMA Netw Open. 2020;3:e2010185. doi: 10.1001/jamanetworkopen.2020.1018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Public Health England. Disparities in the risk and outcomes of COVID-19; 2020. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/908434/Disparities_in_the_risk_and_outcomes_of_COVID_August_2020_update.pdf . Accessed November 19, 2020.
- 18. Royal College of Nursing. Debate on a Motion of the effect of COVID-19 on Black, Asian and Minority Ethnic (BAME) Communities; 2020. Available at: www.rcn.org.uk/about-us/our-influencing-work/policy-briefings/BR-0420 . Accessed November 19, 2020.
- 19. British Medical Association. BAME doctors being placed at risk due to lack of COVID-19 risk assessments, BMA survey reveal; 2020. Available at: www.bma.org.uk/bma-media-centre/bame-doctors-being-placed-at-risk-due-to-lack-of-covid-19-risk-assessments-bma-survey-reveals . Accessed November 19, 2020.
- 20. Royal College of Physicians. What are we learning from the workforce about the impacts of COVID-19? 2020. Available at: www.rcplondon.ac.uk/news/what-are-we-learning-workforce-about-impacts-covid-19 . Accessed November 19, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.jnsa.com.


