Abstract
Background:
Acculturation is an important predictor of asthma in Latino youth, specifically, Mexican Americans. Less is known about acculturation and pulmonary function measures.
Objective:
To estimate the association of acculturation measures with asthma and pulmonary function in Latino youth and determine whether this association varies across Latino subgroups.
Methods:
We included 1,849 Latinos (302 Caribbean Spanish, 193 Central or South Americans, 1,136 Mexican Americans, 218 other Latino children) aged 8–21 years old from 4 urban regions in the U.S. Acculturation measures include nativity status, age of immigration, language of preference, and generation in the U.S. We used multivariable logistic and linear regression models to quantify the association of acculturation factors with the presence of asthma (case-control study) and pulmonary function (case-only study) adjusting for demographic, socio-environmental, and clinical variables.
Results:
For all acculturation measures (nativity status, age of immigration, language of preference, and generation in the U.S.), higher levels of acculturation were associated with greater odds of asthma. Among cases, high (English preference) and medium (equal preference for Spanish and English) levels of language acculturation were associated with decreased bronchodilator response compared with low (Spanish preference) levels (p=0.009 and 0.02, respectively). Similarly, high language acculturation was associated with increased FEV1 compared with low language acculturation (p=0.02). There was insufficient evidence of heterogeneity for associations across Latino subgroups.
Conclusions:
Acculturation was associated with diagnosed asthma and pulmonary function in Latino children and is important factor to consider in the management of Latino youth with asthma.
Keywords: Latino, Asthma, Acculturation, Pediatric, Health Disparities, Social Determinants of Health
Capsule Summary:
High acculturation increases likelihood of diagnosed asthma whereas low acculturation is associated with lower pulmonary function and increased bronchodilator response in Latinos; cultural and behavioral practices should be considered when determining risk and managing asthma.
INTRODUCTION
In the U.S., Latinos often have better health outcomes than other minority groups of similar low socioeconomic status [1], this difference is referred to as the Hispanic Paradox. Despite living in areas with high exposure to indoor and outdoor pollution [2,3] and having limited access to regular health care [4,5], childhood asthma prevalence is significantly lower among Latinos when compared with African Americans (6.7% vs. 15.7%) and lower than non-Hispanic Whites (7.1%) [6]. To explain this paradox, the healthy migrant effect [7,8], cultural characteristics [9], and acculturation [10,11], have been proposed.
Despite this paradox, there is high variability in asthma prevalence between Latino subgroups: Puerto Ricans have one of the highest life-time prevalence of asthma (36.5%) in the U.S., followed by Cuban (21.8%) and Dominican Americans (15.4%), while Mexican Americans have the lowest (7.5%) [12–14]. Although Latino populations are aggregated into a single ethnic group in the U.S. and are bound by the Spanish language, there is considerable heterogeneity in their genetic makeup, cultural upbringing, and environmental exposures [12,14]. Each Latino subgroup has a unique relationship with the U.S. that not only differs in the types of environmental exposures but also in the process of immigration to the U.S.[1]. These differences may translate to varying risks for asthma and related outcomes across Latino subgroups [15,16]. Several studies have demonstrated that low acculturation is associated with lower odds of asthma in Mexican Americans [17–19]. However, the role of acculturation in asthma may not only differ by Latino subgroups [20] but also by how acculturation is defined. Thus, acculturation may play a role in explaining the wide variability in asthma prevalence observed across Latino subgroups in the U.S. [20] and may partially explain the recent trend of increasing asthma prevalence in Mexican Americans [6].
While acculturation reflects the adoption of cultures of the dominant society, it also captures the duration of time spent in the host country, and thus, the changes in early life exposures to known asthma risk factors [21]. Therefore, studies have argued that the change in socio-environmental exposures and adaption of the dominant culture’s behavioral attributes may explain the observed association between acculturation and asthma, and more recently, with lung function [19,22,23]. Early life exposures to environmental toxins, including air pollution, are important factors in determining impaired lung function and asthma risk [24]; thus, the country of birth and/or the age at which one immigrates to the U.S. may be important factors in defining risk. In addition, behaviors associated with acculturation (e.g., increased tobacco use and decreased breastfeeding) may increase risk for asthma and impaired lung function [25,26]. Therefore, including attributes of acculturation that affect changes in behaviors [21], such as language preference, would allow for deeper exploration of acculturation.
A systematic review summarizing the association between immigration status with asthma and allergic disease in diverse populations found that, in general, asthma prevalence was lower in immigrants compared with the host population and, among immigrants, lower in first generation compared with second generation immigrants [27]. However, of the 54 articles included in this review, only seven focused on acculturation and Latinos, and of which, two were focused in Mexican American populations[28,29], two in Puerto Rican and Dominican populations [16,30], and three in Latinos in aggregate[31–33]; of these, only one assessed pulmonary function [33]. Since the publication of this review, additional studies have examined the relationship between acculturation and asthma in the Mexican American population and found conflicting results. We previously demonstrated that acculturation (defined as generation in the U.S) partially explains the association observed between high socioeconomic status and diagnosed asthma in Mexican American children living in the San Francisco Bay Area [34]. Grineski et al. demonstrated that high acculturation, derived from an abbreviated version of the Cultural Life Style Inventory, was significantly associated with asthma in Hispanic youth from El Paso, TX [35] even after considering neighborhood factors [36]; however, after accounting for undiagnosed asthma this association no longer persisted [37]. Another study, after accounting for Native genetic ancestry, also failed to demonstrate an association between acculturation and asthma [38]. Given this evidence, further examination of the relationship between acculturation and asthma is warranted to best understand how this potentially important risk factor operates within and across Latino subgroups.
These studies stress the importance of examining different domains of acculturation and including measures that may co-occur or change with acculturation and provide a better understanding of how acculturation relates to various asthma outcomes across Latino subgroups. In the present study, we include the Genes-Environment & Admixture in Latino Americans (GALA II) study [39] participants and will leverage the ethnic diversity across study sites to 1) examine the association between several acculturation measures with reported asthma diagnosis and with lung function among Latino youth; 2) determine whether the association remains after consideration of socio-environmental factors; and 3) whether this association varies according to Latino subgroup.
METHODS
Study Population
GALA II is a case-control study of asthma in Latino children and adolescents designed to examine the complex genetic and socio-environmental contributors to asthma prevalence, control, and severity. The study was initiated in 2006 and participants were sampled through community- and clinic-based recruitment at health maintenance organizations and community health clinics from five urban study centers across the mainland U.S. and Puerto Rico (see Table E1 in the Online Repository). The current analysis was limited to the four urban centers in the mainland U.S.
All participants were 8–21 years old and had no history of other lung or chronic illnesses (other than atopy and allergy related diseases in the cases). Within each study center, controls were frequency matched by hospital or community clinic site. Those in the third trimester of pregnancy, with ≥10 pack-year smoking history, and current smokers were not eligible (Table E2). Trained bilingual interviewers administered comprehensive questionnaires to the parents/caretakers of the participants to collect socio-demographic information, medical histories, and environmental exposure-related information. Interviewers were recruited from the same communities of potential participants and trained to respectfully ascertain sensitive information through questionnaires. Written, age-appropriate informed consent/assent was obtained from all participants and their legal guardians. The University of California, San Francisco and each study site institutional review board (IRB) approved the GALA II protocol (GALA II UCSF-IRB# 10-00889, Reference#164561).
Ascertainment of Ethnicity
The parents and all four grandparents of the participants must have self-identified as Latino to be eligible for the study. Ethnicity was collected through the question “Do you consider yourself Spanish/Hispanic/Latino?” with a “Yes/No” choice (if yes, please specify: Mexican, Mexican American, Chicano; Spanish, Hispanic, Latino; Dominican; Cuban, and so forth). Multiple selections were allowed. The participant (or the participant’s parents) selected the appropriate answers to all questions for the participant, parents, and grandparents. Responses were used to categorize participants as per their Nationality or country of origin subgroup.
Outcome Assessment
Asthma status was based on physician diagnosis and report of symptoms and medication use within two years prior to recruitment. Eligible controls had no reported history of asthma, lung disease or chronic illness, and no reported symptoms of wheezing or shortness of breath when not sick (see Table EII). Spirometry testing was conducted with a KoKo® PFT Spirometer (nSpire Health Inc., Louisville, CO) according to American Thoracic Society recommendations [40]. All asthma medications were withheld for at least 8 hours before testing.
Pulmonary function, including forced expiratory volume in one second (FEV1) and bronchodilator response, was assessed only in asthma cases. Forced expiratory volume in one second (FEV1) was collected as a standard measurement of airway obstruction. Predicted pulmonary function was calculated based on Hankinson’s formulas for Mexican Americans for all Latino participants [41]. After completing baseline measurements, participants were given four puffs of albuterol (90 μg per puff) through a metered-dose inhaler with a spacer, and spirometry was repeated after 15 minutes. Spirometry was repeated a third time after a second dosage of albuterol (two puffs if < 16 years old or four puffs if ≥ 16 years old). We assessed the maximal bronchodilator response by measuring the percent change in measured FEV1 before and after albuterol administration, using the post-bronchodilator measurement with the greatest change. That is, bronchodilator response (% change in FEV1) = (Post-FEV1 − Pre-FEV1)/Pre-FEV1 * 100.
Exposure Assessment
Acculturation was specified using four variables: nativity status, age at immigration to the U.S., language acculturation, and generational status (16, 30, 31). Nativity status classified participants as whether or not they were born in the U.S. To account for length of time in the U.S., “age at immigration to the U.S.” was specified as: “U.S. Born,” “Ages 0–3,” “Ages 4–9,” and “Ages 10+” [42]. Language acculturation was specified as low, medium, and high to reflect the preferred language spoken at home by the mother and child, and the degree of discordance between their preferences: Low indicates that the child and mother both preferred Spanish; Medium was used when either the child or mother preferred Spanish or neither preferred a primary language; and High classified instances when one person from a mother/child pair preferred English while the other person had a preference to speak English or had no preference. Generational status is a measure based on the participant’s and the parents’ country of birth. Participants born outside of the U.S. were classified as first generation or foreign-born, regardless of parents’ country of birth; children born in the U.S. whose parents were both born outside of the U.S. were classified as second generation; and children born in the U.S. who had at least one parent born in the U.S. were classified as third generation (Table EIII). We created a composite acculturation index based on language preference and generation in the US whereas participants were categorized as having a high index if they had either high language acculturation or were third generation; medium if they had medium language acculturation and were second generation; and low if they did not fit the above categories (Table EIV).
Covariate Selection
Informed by previous studies, age [6], maternal age at birth [43], sex [44], socioeconomic status [34,45], environmental exposures [46–50], birthweight [51,52], global genetic ancestry [53,54] were considered potential confounders in the analyses. The socioeconomic indicators included were maternal educational attainment and insurance status. Maternal education, considered a stable measure of SES [55], was ascertained as the highest grade level or year completed by the mother and categorized as high/low based on high school graduate status. Health insurance status, a marker of access to healthcare services [56], was ascertained through questionnaire data and categorized as no health insurance, government subsidized insurance, or privately-owned health insurance. Environmental exposures include in-utero tobacco exposure and report of mold and cockroach exposure; these exposures were collected as present or absent. Low birthweight was a binary variable used to indicate whether participants were less than 5.5 pounds at birth [57]. Participants were genotyped using the LAT1 array (World Array 4, Affymetrix, Santa Clara, CA [53]). Estimates of global Native and African genetic ancestry were obtained using an unsupervised analysis in ADMIXTURE assuming three ancestral populations. For participants with asthma, the brief medication questionnaire [58] was used to ascertain reported use of controller medications. The use of controller medication was defined as the report of inhaled corticosteroid, leukotriene inhibitor, and/or long-acting-beta agonist in the two weeks prior to recruitment.
By July 2014, there were 4,702 participants in GALA II. Of those, 2,578 participants lived in mainland U.S. and, thus, eligible for the current analysis. Participants were excluded from the analysis if a participant had missing data for child or parent country of birth (n = 1), self-reported maternal educational level (n = 35), insurance status (n = 29), mold exposure (n = 27), birthweight (n = 356), and/or additional covariate or demographic information (n = 281). Excluded participants were more likely to be older, female, born outside the U.S., have no health insurance, and did not report mold exposure (p-values <0.05). Our analytical size included 1,849 participants (1,136 Mexican Americans, 193 Central or South Americans, 302 Caribbean Spanish, and 218 other Latino children). The case-only analytic sample used for the lung function analysis included 928 participants.
Statistical Analysis
We used chi-squared, t-test, and Kruskal-Wallis statistics to determine significant associations of each covariate with case-control status. Using multivariable logistic regression, we first examined for an association between measures of acculturation and asthma diagnosis before and after controlling for age, sex, child’s Latino subgroup, region of recruitment, and Native and African ancestry (Model 1). In the second model, we additionally adjusted for maternal education, maternal age at birth, insurance status, in utero tobacco exposure, birth weight, breastfeeding, and report of household mold and cockroaches. Pulmonary function models were additionally adjusted for current smokers in the household. Because previous research showed the prevalence of asthma varies across Latino ethnic groups [6,14], we included an interaction term between each measure of acculturation and Latino subgroup in the final models. Among children with asthma, we use linear regression to assess the association of lung function measurements (FEV1 and bronchodilator response) with the acculturation measures. We then complete two sub-analyses: first, we limited the analysis to U.S. born participants to determine if the observed acculturation effects persist; and, second, we examined if the effects of acculturation differed by atopy status. This second sub-analysis was informed by the finding that the risk factors for atopic versus non-atopic asthma differ and may even have opposing associations dependent on atopy status [34]. We used a total IgE of 100 IU/mL or greater as a proxy for atopic status. All analyses were performed with R 3.3.0 [59].
RESULTS:
Characteristics of the children and adolescents included in the study are displayed in Table 1. When compared with healthy controls, participants with asthma were younger, more likely to be male, had mothers with higher levels of education and with older maternal age at birth, were less likely to be uninsured, were less likely to have been breastfed, and more likely to have mothers who smoked during pregnancy (p-values < 0.05). Moreover, asthma cases were more likely to report exposure of household mold, had lower global Native genetic ancestry and higher African genetic ancestry, less likely to be born outside of the U.S., have immigrated to the U.S. at an older age, have low language acculturation, and be first generation in the U.S. compared with participants without asthma (p-values<0.001).
Table 1.
Selected Characteristics of Participants in the GALA II Study, 2006–2014
| Healthy Control | Asthma Case | p-value | |
|---|---|---|---|
| N | 897 | 952 | |
| Age, median (IQR) | 13.0 (10.6–15.7) | 12.0 (9.9–14.5) | <0.001 |
| Sex, male | 382 (42.6) | 540 (56.7) | <0.001 |
| Ethnicity Sub-group | 0.001 | ||
| Caribbean Spanish | 126 (14.0) | 176 (18.5) | |
| Central American | 92 (10.3) | 75 (7.9) | |
| Mexican American | 578 (64.4) | 558 (58.6) | |
| South American | 15 (1.7) | 11 (1.2) | |
| other Latino^ | 86 (9.6) | 132 (13.9) | |
| Mother’s Education | 0.016 | ||
| Lower than high school grad | 496 (55.3) | 473 (49.7) | |
| High school grad or greater | 401 (44.7) | 479 (50.3) | |
| Insurance status | <0.001 | ||
| None | 76 (8.5) | 36 (3.8) | |
| Government-subsidized | 704 (78.5) | 747 (78.5) | |
| Private Insurance | 117 (13.0) | 169 (17.8) | |
| Maternal age at birth, median (IQR) | 23.0 (20.0–28.0) | 25.0 (21.0–29.0) | <0.001 |
| Ever breastfed, Yes | 704 (78.5) | 653 (68.6) | <0.001 |
| < 5.5 pounds at birth, Yes | 64 (7.1) | 78 (8.2) | 0.393 |
| In Utero Tobacco Exposure, Yes | 26 (2.9) | 47 (4.9) | 0.024 |
| Current smokers in household | 0.796 | ||
| None | 675 (75.3) | 740 (77.7) | |
| One | 144 (16.1) | 145 (15.2) | |
| Two or more | 44 (4.9) | 46 (4.8) | |
| Missing | 34 (3.8) | 21 (2.2) | |
| Report of Mold Exposure, Yes | 243 (27.1) | 352 (37.0) | <0.001 |
| Report of Cockroach Exposure, Yes | 335 (37.3) | 349 (36.7) | 0.760 |
| Nativity Status | 240 (26.8) | 110 (11.6) | <0.001 |
| Born outside of the U.S. | |||
| Language Acculturation # | <0.001 | ||
| Low (Spanish-Spanish) | 226 (25.2) | 170 (17.9) | |
| Medium (Spanish-English) | 523 (58.3) | 490 (51.5) | |
| High (English-English) | 148 (16.5) | 292 (30.7) | |
| Age at immigration | <0.001 | ||
| Ages 10 and older | 63 (7.0) | 21 (2.2) | |
| Ages 4–9 | 107 (11.9) | 54 (5.7) | |
| Ages 0–3 | 70 (7.8) | 35 (3.7) | |
| US Born | 657 (73.2) | 842 (88.4) | |
| Generation in the United States | <0.001 | ||
| 1st Generation | 240 (26.8) | 110 (11.6) | |
| 2nd Generation | 521 (58.1) | 563 (59.1) | |
| 3rd Generation | 136 (15.2) | 279 (29.3) | |
| Composite Acculturation Measure a | 347 (38.7) | 226 (23.7) | <0.001 |
| Low | 379 (42.3) | 387 (40.7) | |
| Medium | 171 (19.1) | 339 (35.6) | |
| High | |||
| Study Site | 0.192 | ||
| Chicago | 217 (24.2) | 233 (24.5) | |
| New York | 220 (24.5) | 245 (25.7) | |
| San Francisco | 337 (37.6) | 318 (33.4) | |
| Texas | 123 (13.7) | 156 (16.4) | |
| Native Ancestry, %, median (IQR) | 53.9 (38.2–71.2) | 48.9 (25.3–61.4) | <0.001 |
| African Ancestry, %, median (IQR) | 5.0 (3.0–9.0) | 5.8 (3.6–13.1) | <0.001 |
| Spirometry, mean (SD) | |||
| FEV1, % predicted | ---- | 94.2 (14.5) | |
| Missing, n(%) | 22 (2.3) | ||
| Bronchodilator Response, % Change | ---- | 9.5 (8.8) | |
| Missing, n(%) | 24 (2.5) | ||
| Controller Medication Use, Yes* | ---- | 396 (41.6%) |
Results are presented as n (%) unless otherwise noted; P-values are from chi-square and Kruskal-Wallis tests
Definition of abbreviations: IQR= Interquartile Range; FEV1 = Forced Expiratory Volume in one second; FVC = Forced Expiratory Volume
Includes those that identify as more than one Latino subgroup or as Spanish
Language acculturation describes the concordance between the mother and child’s language preference. If both prefer Spanish, they have low language acculturation and if both prefer English, they have high language acculturation.
Controller medication include yes/no to luketriene Inhibitor, inhaled corticosteroids, long-acting bronchodilator or combination therapy
Clinical Outcomes
Asthma Status
Higher levels of acculturation across all four variables (nativity status, age at immigration to the U.S., language preference, and generational status) were associated with increased odds of asthma when compared with the lowest category, even after adjusting for socio-environmental factors (Table 2, Figure 1). In the fully adjusted model, U.S. born participants were 2.10 (95% CI:1.60–2.77) times more likely to have asthma compared with those born outside the U.S. Similarly, child-mother dyads who preferred English as their primary language had 2.20 (95% CI:1.54–3.14) greater odds of asthma compared with those that preferred Spanish. In addition, U.S. born had 2.47 (95%CI:1.46–4.33) times the odds of asthma compared with individuals who moved to the U.S. after the age of 10. No significant association was observed among participants who immigrated to the U.S. at an age younger than 10 years. We found 1.94 (95%CI:1.47–2.57) and 2.94 (95%CI: 2.06–4.22) higher odds of asthma among second and third generation participants, respectively, compared with first generation individuals. When we examined the relationship using a composite measure of acculturation, we found 1.49 (95%CI:1.17–1.92) and 2.43 (95%CI:1.78–3.34) higher odds of asthma in those with a medium and high acculturation index score, respectively, compared with those with a low index score. No significant changes were observed when analyses were adjusted for total IgE in participants with available data (Table EV) nor was a significant interaction observed with high/low total IgE (all p’s >0. 14). Lastly, when associations were limited to U.S. born participants, higher levels of acculturation were associated with asthma diagnosis compared with children with low acculturation (Table EVI). We did not find evidence for these associations to vary by self-reported Latino subgroup, as each of the interaction terms between each acculturation variable and Latino subgroup were not significant (p-values ≥0.09, Table EVII).
Table 2.
Estimated Odds Ratios and 95% Confidence Intervals (CI) of Diagnosed Asthma for Acculturation Measures in the GALA II Study, 2006–2014
| Unadjusted (95% CI) |
Model 1a (95% CI) |
Model 2b (95% CI) |
|
|---|---|---|---|
|
| |||
| Acculturation Measure | |||
| Nativity | |||
| Not born in the U.S. | Ref | Ref | Ref |
| Born in the U.S. | 2.80 (2.19, 3.59) | 2.38 (1.84, 3.10) | 2.10 (1.60, 2.77) |
| Language Acculturation | |||
| Low (Spanish-Spanish) | Ref | Ref | Ref |
| Medium (Spanish-English) | 1.25 (0.99, 1.58) | 1.34 (1.04, 1.73) | 1.26 (0.97, 1.65) |
| High (English-English) | 2.62 (1.98, 3.48) | 2.32 (1.68, 3.23) | 2.20 (1.54, 3.14) |
| Age at immigration | |||
| Ages 10 and older | Ref | Ref | Ref |
| Ages 4–9 | 1.51 (0.85, 2.78) | 1.24 (0.68, 2.31) | 1.26 (0.68, 2.38) |
| Ages 0–3 | 1.50 (0.80, 2.87) | 1.16 (0.60, 2.28) | 1.19 (0.61, 2.36) |
| U.S. Born | 3.84 (2.36, 6.51) | 2.76 (1.66, 4.77) | 2.47 (1.46, 4.33) |
| Generation in the U.S. | |||
| 1st Generation | Ref | Ref | Ref |
| 2nd Generation | 2.36 (1.83, 3.05) | 2.19 (1.68, 2.87) | 1.94 (1.47, 2.57) |
| 3rd Generation | 4.48 (3.31, 6.09) | 3.37 (2.40, 4.76) | 2.94 (2.06, 4.22) |
| Acculturation index | |||
| Low | Ref | Ref | Ref |
| Medium | 1.57 (1.26, 1.95) | 1.68 (1.32, 2.13) | 1.49 (1.17, 1.92) |
| High | 3.04 (2.38, 3.91) | 2.68 (2.00, 3.60) | 2.43 (1.78, 3.34) |
Model 1 adjusted for age sex, child’s Latino subgroup, Native and African ancestry, and study site
Model 2: Model 1 additionally adjusted for maternal education, maternal age at birth, insurance status, in utero tobacco exposure, breastfeeding, birthweight, report of mold, and report of cockroaches
Figure 1. Adjusted odds of having asthma with Acculturation Measure (Nativity Status, Age Moved to U.S., Language Preference, and Generational Status) for participants from the GALA II: 2006–2014.
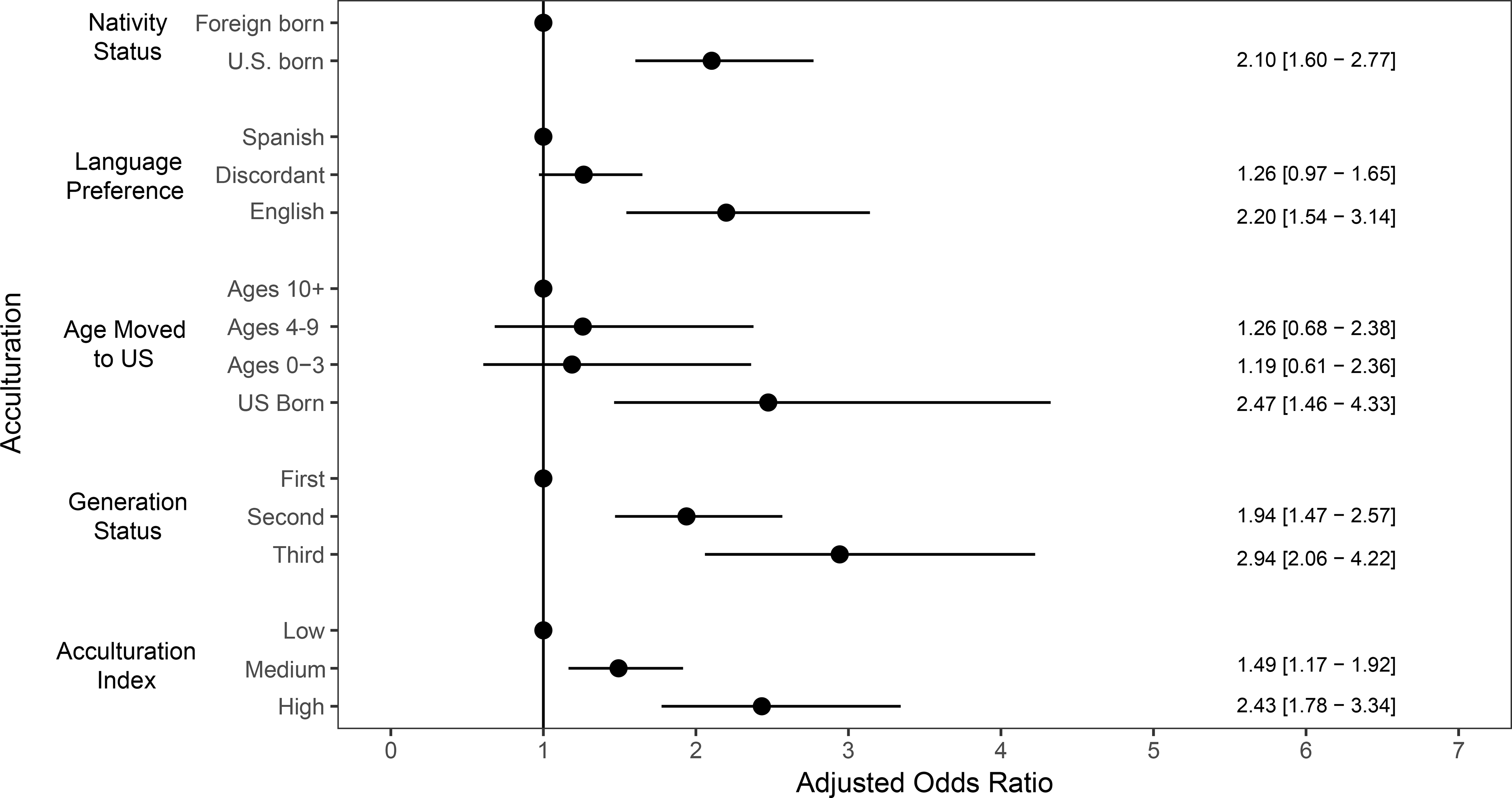
Models adjusted for age, sex, in utero tobacco exposure, maternal education, maternal age at birth, insurance status, report of household mold and cockroaches, breastfeeding, birthweight, study site, global African and Native genetic ancestry, and child’s Latino subgroup.
Pulmonary Function
When we examined the association between each acculturation variable and pulmonary function measures (FEV1 and bronchodilator response), we found higher FEV1 % in child-mother dyads that preferred English compared with child-mother dyads who preferred Spanish (3.70%, 95%CI: 0.56, 6.84). A high acculturation index was also associated with higher FEV1 % when compared with a low acculturation index (3.59%, 95%CI: 0.77, 6.41; Table 3). Compared with child-mother dyads who preferred Spanish exclusively, we observed lower bronchodilator response among dyads discordant for language preference (−1.98%, 95%CI: −0.34, −3.62) and dyads that preferred English (−3.05%, 95%CI: −1.05, −5.06; Table 4). We also found a lower bronchodilator response among participants with a high acculturation index (−3.23%, 95%CI: −1.44, −5.03) compared with those with a low acculturation index. Nativity status, age moved to U.S. and generation status in the U.S. were not associated with pulmonary function measures. No significant changes were observed when analyses were adjusted for total IgE in participants with available data (Table EV) nor was a significant interaction observed with high/low total IgE (p-values >0.36). Among U.S. born participants, the significant associations between acculturation measures and diagnosed asthma persisted, additionally, we observed that language acculturation, generation in the U.S., and the composite acculturation index to be associated with higher FEV1 (Table EVI).
Table 3:
Estimated FEV1* % Predicted Mean Difference and 95% Confidence Intervals for Acculturation Measures in Participants with Asthma from the GALA II Study, 2006–2014 (n=931)
| Unadjusted Mean difference (95% CI) |
Model 1a Mean difference (95% CI) |
Model 2b Mean difference (95% CI) |
|
|---|---|---|---|
|
| |||
| Acculturation Measure | |||
| Nativity | |||
| Not born in the U.S. | Ref | Ref | Ref |
| Born in the U.S. | 0.63 (−2.28, 3.54) | 2.37 (−0.42, 5.16) | 2.35 (−0.51, 5.22) |
| Language Acculturation | |||
| Low (Spanish-Spanish) | Ref | Ref | Ref |
| Medium (Spanish-English) | 0.63 (−1.92, 3.18) | 2.13 (−0.38, 4.63) | 1.73 (−0.84, 4.31) |
| High (English-English) | −1.82 (−4.59, 0.94) | 3.52 (0.60, 6.44) | 3.70 (0.56, 6.84) |
| Age at immigration | |||
| Ages 10 and older | Ref | Ref | Ref |
| Ages 4–9 | 0.99 (−6.33, 8.30) | 0.33 (−6.53, 7.20) | 0.06 (−6.89, 7.01) |
| Ages 0–3 | 1.89 (−6.05, 9.83) | −0.22 (−7.71, 7.26) | −0.72 (−8.27, 6.84) |
| U.S. Born | 1.70 (−4.59, 7.98) | 2.47 (−3.49, 8.43) | 2.16 (−3.86, 8.17) |
| Generation in the U.S. | |||
| 1st Generation | Ref | Ref | Ref |
| 2nd Generation | 1.77 (−1.20, 4.75) | 2.15 (−0.69, 4.99) | 2.11 (−0.82, 5.03) |
| 3rd Generation | −1.68 (−4.90, 1.53) | 3.06 (−0.21, 6.32) | 3.10 (−0.28, 6.48) |
| Acculturation index | |||
| Low | Ref | Ref | Ref |
| Medium | 0.20 (−2.20, 2.61) | 1.65 (−0.70, 3.99) | 1.30 (−1.12, 3.71) |
| High | −1.94 (−4.40, 0.53) | 3.50 (0.85, 6.14) | 3.59 (0.77, 6.41) |
Model 1 adjusted for age sex, child’s Latino subgroup, controller medication use, Native and African ancestry, and study site
Model 2: Model 1 additionally adjusted for maternal education, maternal age at birth, insurance status, in utero tobacco exposure, current smokers in household, breastfeeding, birthweight, and report of mold, and report of cockroaches
Definition of abbreviations: FEV1 = Forced Expiratory Volume in one second
Table 4:
Estimated Bronchodilator Response (%) Mean Difference and 95% Confidence Intervals for Acculturation Measures in Participants with Asthma from the GALA II Study, 2006–2014 (n=931)
| Unadjusted Mean difference (95% CI) |
Model 1a Mean difference (95% CI) |
Model 2b Mean difference (95% CI) |
|
|---|---|---|---|
|
| |||
| Acculturation Measure | |||
| Nativity | |||
| Not born in the U.S. | Ref | Ref | Ref |
| Born in the U.S. | 0.05 (−1.72, 1.82) | −0.47 (−2.26, 1.32) | −0.05 (−1.89, 1.78) |
| Language Acculturation | |||
| Low (Spanish-Spanish) | Ref | Ref | Ref |
| Medium (Spanish-English) | −2.32 (−3.87, −0.77) | −2.20 (−3.80, −0.60) | −1.98 (−3.62, −0.34) |
| High (English-English) | −2.44 (−4.12, −0.76) | −3.41 (−5.27, −1.55) | −3.05 (−5.06, −1.05) |
| Age at immigration | |||
| Ages 10 and older | Ref | Ref | Ref |
| Ages 4–9 | 3.55 (−0.91, 8.00) | 3.31 (−1.09, 7.70) | 3.24 (−1.21, 7.68) |
| Ages 0–3 | 1.89 (−2.94, 6.73) | 1.66 (−3.13, 6.45) | 1.65 (−3.19, 6.48) |
| U.S. Born | 2.40 (−1.43, 6.23) | 1.69 (−2.12, 5.51) | 2.05 (−1.79, 5.90) |
| Generation in the U.S. | |||
| 1st Generation | Ref | Ref | Ref |
| 2nd Generation | 0.21 (−1.62, 2.03) | −0.02 (−1.83, 1.80) | 0.38 (−1.49, 2.25) |
| 3rd Generation | −0.27 (−2.25, 1.70) | −1.89 (−3.98, 0.20) | −1.39 (−3.55, 0.77) |
| Acculturation index | |||
| Low | Ref | Ref | Ref |
| Medium | −1.81 (−3.27, −0.34) | −1.83 (−3.32, −0.33) | −1.54 (−3.08, 0.00) |
| High | −2.14 (−3.64, −0.64) | −3.59 (−5.27, −1.90) | −3.23 (−5.03, −1.44) |
Model 1 adjusted for age sex, child’s Latino subgroup, controller medication use, Native and African ancestry, and study site
Model 2: Model 1 additionally adjusted for maternal education, maternal age at birth, insurance status, in utero tobacco exposure, current smokers in household, breastfeeding, birthweight, and report of mold, and report of cockroaches
DISCUSSION
Our findings show that regardless of acculturation definition, we consistently observed that higher acculturation (i.e., U.S. born, moving to U.S. at an earlier age, English language preference, and third generation in the U.S.) was associated with higher odds of asthma. These findings remained robust even after adjusting for social (socioeconomic status, history of breastfeeding, birthweight), environmental (in utero tobacco and reported mold and cockroach exposure), and genetic factors that have been postulated to explain this association. Our findings are consistent with past research examining the role of acculturation in Mexican Americans [17–19] and in other ethnic groups [14,42], as well as builds upon the findings demonstrating that with increased length of stay in the U.S., the odds of asthma in Latino populations also increases.
Low acculturation in Latino populations has been consistently associated with better health for several outcomes [11,60], suggesting certain cultural and behavioral practices, community networks, leading to increased disease risk. For instance, obesity, low birth weight, smoking, and reduction in breastfeeding are more common among highly acculturated individuals compared with recent immigrant individuals [25,26,60–62], each of these factors being an independent risk factor for asthma [48,49,51,52,63].
This study is one of few studies to examine the association between acculturation and pulmonary function measurements in Latinos. Across most measures of acculturation, we did not observe a significant association with bronchodilator response or FEV1. An exception was with language preference, where we observed that higher levels of language acculturation were associated lower bronchodilator response and higher FEV1. These findings raise two potential hypotheses: The first, aligning with our findings that higher levels of acculturation were associated with higher odds of asthma, is that the psychosocial stress related to acculturation may not only increase risk for disease but also may decrease drug response to traditional asthma therapies. Language preference may better reflect the cultural and behavioral aspects of acculturation than the other measures used in this study. Past research suggests that acculturative stress may manifest physiologically with psychosomatic symptoms [64]. This finding of lower bronchodilator response is consistent with previous research associating high stress levels with lower bronchodilator response [65]. However, this would not account for the finding of higher FEV1 in the more acculturated groups. A second hypothesis, contrary to our case-control findings, is that English language preference results in improved asthma control manifesting as decreased bronchodilator response [66] (already at personal best) and higher FEV1 compared with children with low language acculturation. This is consistent with previous studies demonstrating that high language concurrence with medical provider results in improved asthma control in Latinos [67,68]. However, these findings warrant further investigation.
Our study has several limitations and the results should be interpreted within the context of these limitations. The sample sizes for non-Mexican American populations in our study are small. While we did not observe an interaction, the overall results should be interpreted with caution. Second, is the lack of consideration of obesity as a potential explanatory pathway for the association between asthma and higher acculturation [60,69]. We were unable to assess this relationship as body mass index information was missing on over 40% of healthy controls. The lack of controlling for BMI may have attenuated our results. We were also unable to account for air pollution effects due to a lack of accurate estimates for participants born outside of the U.S. (in total, missing data for 35% of study population). However, we were able to account for indoor air pollutant sources including reports of mold, cockroaches, and in-utero tobacco smoke exposure.
Another limitation may be under-diagnosis among our healthy control population. Individuals with low educational attainment, especially immigrant Latinos, have a poor rate of enrollment in insurance programs [70]. The Latino population is underinsured compared to other racial/ethnic groups. For example, Mexican American children age 18 or younger have a 16% uninsured rate compared to the national average of 10% [71]. Because minority health is often shaped by language barriers, access to preventive care, and lack of health insurance, limiting ability to navigate the healthcare system and poor patient-provider communication, underdiagnoses cannot be ruled out in this population [37,72]. Outcome misclassification was minimized in our study by carefully screening healthy controls for any asthma-related symptoms using the questions following the International Study of Asthma and Allergies in Childhood (ISAAC) screening tool; however, we acknowledge that terms such as “wheezing” and “whistling” may get lost in translation.
Conclusion
We found that the odds of asthma increase as acculturation increases for Latino children, regardless of how acculturation was defined. The direction of this association remained robust for all national subgroups, raising its importance as a risk factor that necessitates future study to identify important, modifiable risks for asthma in this high-risk population.
Supplementary Material
Key Messages:
Regardless of acculturation measure, we observed lower odds of asthma with lower acculturation (i.e., born outside the U.S., moving to U.S. at an older age, language preference, and first generation in the U.S.), even after adjustment for important socio-environmental factors.
Among children with asthma, Spanish language preference was associated with lower forced expiratory volume in one second and increased bronchodilator response, an important indicator of asthma control.
Acknowledgements
The authors acknowledge the families and patients for their participation and thank the numerous health care providers and community clinics for their support and participation in GALA II. In particular, the authors thank the study coordinator Sandra Salazar; the recruiters who obtained the data: Duanny Alva, MD, Gaby Ayala-Rodriguez, Ulysses Burley, Lisa Caine, Elizabeth Castellanos, Jaime Colon, Denise DeJesus, Iliana Flexas, Blanca Lopez, Brenda Lopez, MD, Louis Martos, Vivian Medina, Juana Olivo, Mario Peralta, Esther Pomares, MD, Jihan Quraishi, Johanna Rodriguez, Shahdad Saeedi, Dean Soto, Ana Taveras, Emmanuel Viera.
Sources of Funding:
This work was supported in part by the Sandler Family Foundation, the American Asthma Foundation, the RWJF Amos Medical Faculty Development Program, Harry Wm. and Diana V. Hind Distinguished Professor in Pharmaceutical Sciences II, National Institutes of Health 1R01HL117004, R01Hl128439, R01HL135156, 1X01HL134589, National Institute of Health and Environmental Health Sciences R01ES015794, R21ES24844, the National Institute on Minority Health and Health Disparities 1P60MD006902, U54MD009523, 1R01MD010443 and the Tobacco-Related Disease Research Program under Award Number 24RT-0025. M01-RR00188 to H.J.F. N.T. was supported by institutional training grant from the NIGMS (T32-GM007546) and career development awards from the NHLBI (K12-HL119997 and K23- HL125551-01A1), Parker B. Francis Fellowship Program, and the American Thoracic Society. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations:
- GALA II
Genes-Environment & Admixture in Latino Americans
- FEV1
Forced Expiratory Volume in one second
- SES
Socioeconomic Status
Footnotes
COI Statement: The authors declare that there are no conflict of interests.
***This article has a data supplement
References:
- 1.Acevedo-Garcia D, Bates LM. Latino health paradoxes: Empirical evidence, explanations, future research, and implications. In: Latinas/os in the United States: Changing the Face of América. Boston, MA: Springer US; 2008. p. 101–13. [Google Scholar]
- 2.Jacobs DE. Environmental health disparities in housing. Am J Public Health. 2011. Dec 28;101(SUPPL. 1):S115–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clark LP, Millet DB, Marshall JD. Changes in transportation-related air pollution exposures by race-ethnicity and socioeconomic status: Outdoor nitrogen dioxide in the United States in 2000 and 2010. Environ Health Perspect. 2017;125(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crespo NC, Ayala GX, Vercammen-Grandjean CD, Slymen DJ, Elder JP. Socio-demographic disparities of childhood asthma. J Child Heal Care. 2011. Dec 12;15(4):358–69. [DOI] [PubMed] [Google Scholar]
- 5.Coker TR, Kaplan RM, Chung PJ. The association of health insurance and disease impairment with reported asthma prevalence in U.S. children. Health Serv Res. 2012. Feb 1;47(1 PART 2):431–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zahran HS, Bailey CM, Damon SA, Garbe PL, Breysse PN. Vital Signs : Asthma in Children — United States, 2001–2016. MMWR Morb Mortal Wkly Rep. 2018. Feb 9;67(5):149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abraído-Lanza AF, Echeverría SE, Flórez KR. Latino Immigrants, Acculturation, and Health: Promising New Directions in Research. Annu Rev Public Health. 2016;37(1):219–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Heal. 1999/10/08. 1999;89(10):1543–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gallo LC, Penedo FJ, Espinosa de los Monteros K, Arguelles W. Resiliency in the face of disadvantage: do Hispanic cultural characteristics protect health outcomes? J Pers. 2009/10/03. 2009;77(6):1707–46. [DOI] [PubMed] [Google Scholar]
- 10.Turra CM, Goldman N. Socioeconomic Differences in Mortality Among U.S. Adults: Insights Into the Hispanic Paradox. Journals Gerontol Ser B Psychol Sci Soc Sci. 2007. May 1;62(3):S184–92. [DOI] [PubMed] [Google Scholar]
- 11.Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Heal. 2005;26:367–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics. 2006/01/07. 2006;117(1):43–53. [DOI] [PubMed] [Google Scholar]
- 13.Akinbami LJ, Bailey CM, Johnson CA, King ME, Liu X, Moorman JE, et al. National surveillance of asthma: United states, 2001–2010. Natl Cent Heal Stat Vital Heal Stat. 2012;3:35. [PubMed] [Google Scholar]
- 14.Barr RG, Aviles-Santa L, Davis SM, Aldrich TK, Gonzalez F 2nd, Henderson AG, et al. Pulmonary Disease and Age at Immigration among Hispanics. Results from the Hispanic Community Health Study/Study of Latinos. Am J Respir Crit Care Med. 2016;193(4):386–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burchard EG, Borrell LN, Choudhry S, Naqvi M, Tsai H-J, Rodriguez-Santana JR, et al. Latino populations: a unique opportunity for the study of race, genetics, and social environment in epidemiological research. J Inf. 2005;95(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koinis-Mitchell D, Sato AF, Kopel SJ, McQuaid EL, Seifer R, Klein R, et al. Immigration and acculturation-related factors and asthma morbidity in Latino children. J Pediatr Psychol. 2011;36(10):1130–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eldeirawi K, McConnell R, Freels S, Persky VW. Associations of place of birth with asthma and wheezing in Mexican American children. J Allergy Clin Immunol. 2005. Jul 1;116(1):42–8. [DOI] [PubMed] [Google Scholar]
- 18.Holguin F, Mannino DM, Antó J, Mott J, Ford ES, Teague WG, et al. Country of birth as a risk factor for asthma among Mexican Americans. Am J Respir Crit Care Med. 2005. Jan 15;171(2):103–8. [DOI] [PubMed] [Google Scholar]
- 19.Martin MA, Shalowitz MU, Mijanovich T, Clark-Kauffman E, Perez E, Berry CA. The effects of acculturation on asthma burden in a community sample of Mexican American schoolchildren. Am J Public Heal. 2007;97(7):1290–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jerschow E, Strizich G, Xue X, Hudes G, Spivack S, Persky V, et al. Effect of Relocation to the U.S. on Asthma Risk Among Hispanics. Am J Prev Med. 2017. May 1;52(5):579–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abraído-Lanza AF, Armbrister AN, Flórez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. Am J Public Health. 2006;96(8):1342–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saad NJ, Patel J, Minelli C, Burney PGJ. Explaining ethnic disparities in lung function among young adults: A pilot investigation. PLoS One. 2017;12(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rode A, Shephard RJ. Acculturation and the Growth of Lung Function: Three Cross-Sectional Surveys of an Inuit Community. Respiration. 1994;61(4):187–94. [DOI] [PubMed] [Google Scholar]
- 24.Stocks J, Hislop A, Sonnappa S. Early lung development: Lifelong effect on respiratory health and disease. Vol. 1, The Lancet Respiratory Medicine. Elsevier; 2013. p. 728–42. [DOI] [PubMed] [Google Scholar]
- 25.Acevedo-Garcia D, Pan J, Jun HJ, Osypuk TL, Emmons KM. The effect of immigrant generation on smoking. Soc Sci Med. 2005. Sep 1;61(6):1223–42. [DOI] [PubMed] [Google Scholar]
- 26.Bandoli G, von Ehrenstein OS, Flores MES, Ritz B. Breastfeeding and Asthmatic Symptoms in The Offspring of Latinas: The Role of Maternal Nativity. J Immigr Minor Heal. 2015;17(6):1739–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cabieses B, Uphoff E, Pinart M, Antó JM, Wright J. A systematic review on the development of asthma and allergic diseases in relation to international immigration: The leading role of the environment confirmed. PLoS One. 2014;9(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eldeirawi K, McConnell R, Furner S, Freels S, Stayner L, Hernandez E, et al. Associations of doctor-diagnosed asthma with immigration status, age at immigration, and length of residence in the United States in a sample of Mexican American school children in Chicago. J Asthma. 2009. Oct;46(8):796–802. [PubMed] [Google Scholar]
- 29.Eldeirawi K, McConnell R, Freels S, Persky VW. Associations of place of birth with asthma and wheezing in Mexican American children. J Allergy Clin Immunol. 2005/07/02. 2005;116(1):42–8. [DOI] [PubMed] [Google Scholar]
- 30.Dumanovsky T, Matte TD. Variation in adult asthma prevalence in hispanic subpopulations in New York City. J Asthma. 2007. Jan 2;44(4):297–303. [DOI] [PubMed] [Google Scholar]
- 31.Huh J, Prause JA, Dooley CD. The impact of nativity on chronic diseases, self-rated health and comorbidity status of Asian and hispanic immigrants. J Immigr Minor Heal. 2008;10(2):103–18. [DOI] [PubMed] [Google Scholar]
- 32.Klinnert MD, Price MR, Liu AH, Robinson JL. Morbidity patterns among low-income wheezing infants. Pediatrics. 2003;112(1 Pt 1):49–57. [DOI] [PubMed] [Google Scholar]
- 33.Svendsen ER, Gonzales M, Ross M, Neas LM. Variability in childhood allergy and asthma across ethnicity, language, and residency duration in El Paso, Texas: a cross-sectional study. Env Heal. 2009/12/10. 2009;8:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thakur N, Oh SS, Nguyen EA, Martin M, Roth LA, Galanter J, et al. Socioeconomic Status and Childhood Asthma in Urban Minority Youths. The GALA II and SAGE II Studies. Am J Respir Crit Care Med. 2013;188(10):1202–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chavez-Payan P, Grineski SE, Collins TW. Early Life and Environmental Risk Factors Modify the Effect of Acculturation on Hispanic Children’s Asthma. Hisp Heal Care Int. 2015;13(3):119–30. [DOI] [PubMed] [Google Scholar]
- 36.Grineski SE, Collins TW, Kim YA. Contributions of individual acculturation and neighborhood ethnic density to variations in Hispanic children’s respiratory health in a US-Mexican border metropolis. J Public Heal (United Kingdom). 2016;38(3):441–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Siañez M, Highfield L, Balcazar H, Collins T, Grineski S. An Examination of the Association of Multiple Acculturation Measures with Asthma Status Among Elementary School Students in El Paso, Texas. J Immigr Minor Heal. 2018;20(4):884–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salam MT, Avoundjian T, Knight WM, Gilliland FD. Genetic ancestry and asthma and rhinitis occurrence in Hispanic children: Findings from the southern California Children’s Health Study. PLoS One. 2015;10(8):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pino-Yanes M, Thakur N, Gignoux CR, Galanter JM, Roth LA, Eng C, et al. Genetic ancestry influences asthma susceptibility and lung function among Latinos. J Allergy Clin Immunol. 2015;135(1):228–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.American_Thoracic_Society. Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med. 1995/09/01. 1995;152(3):1107–36. [DOI] [PubMed] [Google Scholar]
- 41.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999/01/05. 1999;159(1):179–87. [DOI] [PubMed] [Google Scholar]
- 42.Iqbal S, Oraka E, Chew GL, Flanders WD. Association between birthplace and current asthma: The role of environment and acculturation. Am J Public Health. 2014. Feb;104(SUPPL. 1):S175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abid Z, Oh SS, Hu D, Sen S, Huntsman S, Eng C, et al. Maternal age and asthma in Latino populations. Clin Exp Allergy. 2016;46(11):1398–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Almqvist C, Worm M, Leynaert B. Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy. 2007/09/08. 2008;63(1):47–57. [DOI] [PubMed] [Google Scholar]
- 45.Forno E, Celedon JC. Asthma and ethnic minorities: socioeconomic status and beyond. Curr Opin Allergy Clin Immunol. 2009/03/28. 2009;9(2):154–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nishimura KK, Galanter JM, Roth LA, Oh SS, Thakur N, Nguyen EA, et al. Early-Life air pollution and asthma risk in minority children the GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013;188(3):309–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gent JF, Kezik JM, Hill ME, Tsai E, Li D-W, Leaderer BP. Household mold and dust allergens: exposure, sensitization and childhood asthma morbidity. Environ Res. 2012;118:86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oh SS, Tcheurekdjian H, Roth L a, Nguyen E a, Sen S, Galanter JM, et al. Effect of secondhand smoke on asthma control among black and Latino children. J Allergy Clin Immunol. 2012. Jun;129(6d):1478–83.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gilliland FD, Li Y-F, Peters JM. Effects of maternal smoking during pregnancy and environmental tobacco smoke on asthma and wheezing in children. Am J Respir Crit Care Med. 2001;163(2):429–36. [DOI] [PubMed] [Google Scholar]
- 50.Gilliland FD, Berhane K, Li Y-F, Rappaport EB, Peters JM. Effects of early onset asthma and in utero exposure to maternal smoking on childhood lung function. Am J Respir Crit Care Med. 2003;167(6):917–24. [DOI] [PubMed] [Google Scholar]
- 51.Villamor E, Iliadou A, Cnattingius S. Is the association between low birth weight and asthma independent of genetic and shared environmental factors? Am J Epidemiol. 2009;169(11):1337–43. [DOI] [PubMed] [Google Scholar]
- 52.Brooks AM, Byrd RS, Weitzman M, Auinger P, McBride JT. Impact of low birth weight on early childhood asthma in the United States. Arch Pediatr Adolesc Med. 2001/03/20. 2001;155(3):401–6. [DOI] [PubMed] [Google Scholar]
- 53.Pino-Yanes M, Thakur N, Gignoux CR, Galanter JM, Roth LA, Eng C, et al. Genetic ancestry influences asthma susceptibility and lung function among Latinos. J Allergy Clin Immunol. 2015;135(1):228–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kumar R, Seibold MA, Aldrich MC, Williams LK, Reiner AP, Colangelo L, et al. Genetic Ancestry in Lung-Function Predictions. N Engl J Med. 2010;363(4):321–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Williams DR, Collins C. Us Socioeconomic and Racial-Differences in Health - Patterns and Explanations. Annu Rev Sociol. 1995;21:349–86. [Google Scholar]
- 56.Devoe JE, Tillotson CJ, Wallace LS, Lesko SE, Angier H. The effects of health insurance and a usual source of care on a child’s receipt of health care. J Pediatr Heal Care. 2012/08/28. 2012;26(5):e25–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wardlaw TM. Low birthweight: country, regional and global estimates. UNICEF; 2004. [Google Scholar]
- 58.Svarstad BL, Chewning BA, Sleath BL, Claesson C. The Brief Medication Questionnaire: a tool for screening patient adherence and barriers to adherence. Patient Educ Couns. 1999;37(2):113–24. [DOI] [PubMed] [Google Scholar]
- 59.RCoreTeam. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. [Google Scholar]
- 60.Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int J Epidemiol. 2000/06/28. 2000;29(3):470–7. [PubMed] [Google Scholar]
- 61.Callister LC, Birkhead A. Acculturation and perinatal outcomes in Mexican immigrant childbearing women: an integrative review. J Perinat Neonatal Nurs. 2002;16(3):22–38. [DOI] [PubMed] [Google Scholar]
- 62.Gibson MV, Diaz VA, Mainous AG, Geesey ME. Prevalence of breastfeeding and acculturation in Hispanics: results from NHANES 1999–2000 study. Birth. 2005;32(2):93–8. [DOI] [PubMed] [Google Scholar]
- 63.Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007;175(7):661–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Constructs Rudmin F., measurements and models of acculturation and acculturative stress. Int J Intercult Relations. 2009;33(2):106–23. [Google Scholar]
- 65.Brehm JM, Ramratnam SK, Tse SM, Croteau-Chonka DC, Pino-Yanes M, Rosas-Salazar C, et al. Stress and bronchodilator response in children with asthma. Am J Respir Crit Care Med. 2015;192(1):47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Heffler E, Crimi C, Campisi R, Sichili S, Nicolosi G, Porto M, et al. Bronchodilator response as a marker of poor asthma control. Respir Med. 2016;112:45–50. [DOI] [PubMed] [Google Scholar]
- 67.Chan KS, Keeler E, Schonlau M, Rosen M, Mangione-Smith R. How do ethnicity and primary language spoken at home affect management practices and outcomes in children and adolescents with asthma? Arch Pediatr Adolesc Med. 2005. Mar 1;159(3):283–9. [DOI] [PubMed] [Google Scholar]
- 68.Wisnivesky JP, Kattan M, Evans D, Leventhal H, Musumeci-Szabó TJ, McGinn T, et al. Assessing the relationship between language proficiency and asthma morbidity among inner-city asthmatics. Med Care. 2009. Feb;47(2):243–9. [DOI] [PubMed] [Google Scholar]
- 69.Farah CS, Salome CM. Asthma and obesity: a known association but unknown mechanism. Respirology. 2011/10/14. 2012;17(3):412–21. [DOI] [PubMed] [Google Scholar]
- 70.Kandula NR, Grogan CM, Rathouz PJ, Lauderdale DS. The unintended impact of welfare reform on the Medicaid enrollment of eligible immigrants. Health Serv Res. 2004;39(5):1509–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Motel S and EP. The 10 Largest HIspanic Orgin Groups: Characteristics, Rankings, Top Counties. 2012; [Google Scholar]
- 72.Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Heal Care Poor Underserved. 2002/11/01. 2002;13(4):477–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


