Abstract
Background
Food insecurity is a critical public health problem in the United States that has been associated with poor diet quality. Cooking dinner more frequently is associated with better diet quality.
Objective
This study aimed to examine how food insecurity and dinner cooking frequency are associated with diet quality during the initial months of the coronavirus disease 2019 pandemic.
Design
This cross-sectional study analyzed data from a national web-based survey (June 23 to July 1, 2020).
Participants/setting
Participants were 1,739 low-income (<250% of the federal poverty level) adults in the United States.
Main outcome measures
The outcome was diet quality, measured by the Prime Diet Quality Score (PDQS-30D). The PDQS-30D is a food frequency questionnaire-based, 22-component diet quality index.
Statistical analyses performed
Food security status (high, marginal, low, or very low) and frequency of cooking dinner (7, 5 to 6, 3 to 4, or 0 to 2 times/week) were evaluated in relation to PDQS-30D scores (possible range = zero to 126) in age- and sex and gender-, and fully adjusted linear regression models. Postestimation margins were used to predict mean PDQS-30D score by food security status and dinner cooking frequency. The interaction between food security status and frequency of cooking dinner was also tested.
Results
Overall, the mean PDQS-30D score was 51.9 ± 11 points (possible range = zero to 126). The prevalence of food insecurity (low/very low) was 43%, 37% of the sample cooked 7 times/week and 15% cooked 0 to 2 times/week. Lower food security and less frequent cooking dinner were both associated with lower diet quality. Very low food security was associated with a 3.2-point lower PDQS-30D score (95% CI –4.6 to –1.8) compared with those with high food security. Cooking dinner 0 to 2 times/week was associated with a 4.4-point lower PDQS-30D score (95% CI –6.0 to –2.8) compared with cooking 7 times/week. The relationship between food insecurity and diet quality did not differ based on cooking dinner frequency.
Conclusions
During the initial months of the coronavirus disease 2019 pandemic food insecurity and less frequently cooking dinner at home were both associated with lower diet quality among low-income Americans. More research is needed to identify and address barriers to low-income households’ ability to access, afford and prepare enough nutritious food for a healthy diet.
Key words: Food insecurity, Cooking frequency, Diet quality, COVID-19
Research Snapshot.
Research Question: How were food insecurity and frequency of cooking dinner associated with diet quality during the initial months of the coronavirus disease 2019 pandemic among low-income adults in the United States?
Key Findings: In this large, national survey of low-income adults in the United States, overall diet quality was poor. Food insecurity and frequency of cooking dinner were independently associated with lower diet quality. The relationship between food insecurity and diet quality did not differ based on frequency of cooking dinner.
Food insecurity, a condition of limited or uncertain access to sufficient and nutritionally adequate food, is a critical public health problem in the United States that contributes to poor diet quality and other health disparities.1, 2, 3, 4, 5 In 2019, approximately 10.5% (or 13.7 million) US households experienced food insecurity6; however, in the early months of the coronavirus disease 2019 (COVID-19) pandemic approximately one-quarter to one-third of all Americans, and 44% of low-income Americans, were estimated to experience food insecurity.7, 8, 9 If accompanied by reductions in diet quality, as has been previously documented,2 , 3 food insecurity during the pandemic, particularly among low-income Americans, may contribute to long-lasting health consequences among groups that have been historically economically and socially marginalized.1 , 6 , 10
During the initial months of the COVID-19 pandemic, early reports indicated that food insecurity rose due to economic disruptions related to the pandemic.7 , 10 , 11 However, annual estimates of food insecurity from the US Department of Agriculture using the Current Population Survey Food Security Supplement indicate that the overall level of food insecurity remained stable in 2020 compared with 2019 though disparities in food security rates did widen for some groups.12 Questions arose about whether or not more people staying home would lead to improvements in diet quality due to more frequent cooking at home and less frequent eating out.13 Prior evidence suggests that cooking at home is associated with better diet quality,14, 15, 16, 17 but that diet quality is lower among low-income groups even when they cook frequently.18 During the pandemic, the limited emerging evidence regarding the relationship between food insecurity, cooking frequency, and diet quality has been mixed.19, 20, 21, 22, 23, 24 Food insecurity has been associated with lower fruit and vegetable consumption,23 higher energy intake,22 and lower diet quality.21 In a cohort study, diet quality and food security status improved compared with prepandemic levels, and eating out frequency decreased.19 In a cross-country comparisons from June 2020, the United States had the least change in cooking frequency compared to other countries and all countries saw no significant change in fruit or vegetable consumption compared with prepandemic levels.20 No study during the COVID-19 pandemic has examined the relationships between food insecurity, cooking frequency, and diet quality, which all could have been affected by the societal, economic, and supply chain disruptions during the early months of the pandemic.20 , 25 , 26
The objective of this study was to examine how food insecurity and frequency of cooking dinner were associated with diet quality during the initial months of the COVID-19 pandemic among a large sample of low-income adults in the United States. A second objective was to examine whether or not dinner cooking frequency modified the relationship between food security status and diet quality. Food insecurity was hypothesized to be associated with lower diet quality and cooking dinner more frequently at home was hypothesized to be associated with better diet quality, particularly among food-secure adults.
Methods
This cross-sectional study analyzed data from a web-based survey, designed using Qualtrics software,27 to assess food choices and behaviors, food security, and health during the initial months of the COVID-19 pandemic. Developed by the study investigators, the survey included previously validated measures wherever possible (eg, food security status,12 food agency,28 diet quality,29 , 30 cooking behavior,31 anxiety and depression,32 and diabetes distress33), and was pilot tested for clarity before rollout. The survey was fielded using CloudResearch, formerly TurkPrime, an online crowdsourcing platform designed to be used for academic research across multiple disciplines.34 The survey was fielded on Prime Panels. Prime Panels aggregates several market research panels and allows researchers to employ census matching and other targeted recruitment strategies to enable large samples that are more representative of the US population than microtask sites such as MTurk.35 This study used a census-matched panel of US adults aged 18 years or older (matched on age, sex, and race and ethnicity to the overall population) while also limiting the sample to adults with annual household income <250% of the 2020 federal poverty level (based on household size and annual household income).36
The survey was open to participants from June 23, 2020, to July 1, 2020, via an advertisement inviting eligible Prime Panel members to complete the survey. The survey opportunity was displayed to potential participants using a generic survey name (eg, “New Survey Opportunity” or “New Survey”). Data collection was ongoing until the target sample size for all demographic targets was reached. Participants provided informed consent at the start of the survey after reading a brief description of the survey. The survey was described as “a research study assessing your experience and views during a COVID-19 outbreak. The purpose of the study is to understand the effect of the outbreak on the health and wellbeing of adults in the United States.” Participants who completed the survey received a small monetary compensation set by the survey platform through which they were recruited. In total, 2,307 complete survey responses were received. Participants who indicated they did not live in the United States (n = 2), completed the survey unrealistically quickly (<10 minutes) (n = 240), were missing information on food security status (n = 17) or who failed to answer attention check questions correctly (n = 309) were excluded resulting in a final analytic sample of 1,739. The final sample included participants in all 50 states and the District of Columbia, and American citizenship was not a requirement to participate (citizenship was not measured). This study was determined to be exempt by the University of Michigan School of Public Health Institutional Review Board.
Measures
Diet quality, as measured by the Prime Diet Quality Score 30-day screener (PDQS-30D) was the outcome for all analyses.29 A 24-hour recall period and a 30-day recall period version of the PDQS exist; the 30-day version was used for this survey. The PDQS-30D is a food-based diet quality index that includes 22 components (14 healthy, seven unhealthy, and one neutral in a high-income country setting).29 The PDQS-30D measures frequency of intake of the 22 component foods/food groups over the past 30 days via a food frequency questionnaire with seven possible responses for each component: less than once/month, 2 to 3 times/month, 1 to 2 times/week, 3 to 4 times/week, 5 to 6 times/week, once a day, or 2 or more times/day.29 Responses are coded from zero to six with unhealthy components scored in reverse and the neutral component not scored. Scores are then summed to create a PDQS-30D total diet quality score (possible score zero to 126) with higher scores indicating a healthier diet. More information about the development and validation of the PDQS diet quality index and its associated data collection tool (PDQS-30D) is available elsewhere.29 , 37 , 38 Briefly, the PDQS-30D was developed to be used as a short-form screener and global diet quality assessment tool and has been shown to be strongly correlated with usual nutrient intakes as measured by the Automated Self-Administered 24-hour (ASA24) Dietary Assessment Tool,29 and compares favorably with the Healthy Eating Index-2015.29 , 30 In the PDQS-30D validation study there was a statistically significant association between total Healthy Eating Index-2015 score and PDQS-30D score (r = 0.60) as well as generally consistent results comparing PDQS-30D results with usual nutrient intakes as measured by the ASA24.29
Household food security during the past 30 days was measured using the 18-item US Household Food Security Survey Module.39 Questions were ordered by severity and included three levels of screening for adults and one additional level of questions for households with children. Affirmative responses were summed to create a total food security score (out of 10 for household with only adults and out of 18 for households with children). Food security categories (high, marginal, low, and very low) were assigned according to the US Department of Agriculture scoring guidelines.40 Food insecurity refers to both categories of low and very low food security.
Household frequency of cooking dinner was based on the question “In the past 7 days, how many days did you or someone else cook food for dinner or supper at home?” This question was based on the cooking frequency measure included in the 2007-2010 National Health and Nutrition Examination Survey and was asked of all survey respondents.31 Following prior literature,18 a four category measure of dinner cooking frequency was created: 7 days/week, 5 to 6 days/week, 3 to 4 days/week, and 0 to 2 days/week.
Covariates were measured using multiple choice questions and included age (18 to 39 years, 40 to 59 years, and ≥60 years), sex and gender (male, female, or transgender/nonbinary/other), race and ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, or other), education (high school degree/GED or less, some college, or college degree or higher), student status (yes or no), marital status (single, married, divorced/separated/widowed, or living with a partner), annual household income (<$35,000 or ≥$35,000), Supplemental Nutrition Assistance Program (SNAP) participation (yes/no), household size (1 to 3 people or ≥4 people), presence of children younger than age 18 years old in the household (yes/no), and employment status (full time, part time, unemployed/looking for work, or out of the labor force).
Analysis
First, descriptive statistics were used to examine mean PDQS-30D scores by each study covariate. Simple linear regressions were used to evaluate unadjusted differences in PDQS-30D scores across sample characteristics. Then, associations of food security status and dinner cooking frequency with PDQS-30D scores were examined in age- and sex and gender-adjusted linear regression models. Next, separate linear regression models for food security and dinner cooking frequency adjusted for the full set of covariates described above were used to calculate predicted PDQS-30D scores while holding all other covariates at their means. Trend tests across categories of food security status and dinner cooking frequency were calculated using Stata’s contrast command. Finally, differences in the association of food security with diet quality by frequency of cooking dinner was investigated by including an interaction term (the product of categorical variables for food security and cooking dinner frequency) in the fully adjusted model. The significance of the interaction was tested using a likelihood ratio test. In addition, to account for the ordinal nature of the food security and cooking frequency variables, a likelihood ratio test with one degree of freedom using the ‘c.’ prefix in Stata for both measures was also estimated. All analyses were conducted in Stata version 15.0,41 all tests were two-sided and significance was considered at P < 0.05.
Results
Characteristics of the study sample and unadjusted mean PDQS-30D scores across socio-demographic characteristics are presented in Table 1 . The mean PDQS-30D score was 51.9 ± 11.4 points (of possible 0 to 126 points). Compared with non-Hispanic White participants, Hispanic participants (53.2 ± 11.3 vs 50.8 ± 11.1; P = 0.002) and Asian participants (58.2 ± 12.0 vs 50.8 ± 11.1; P < 0.0001) had higher PDQS-30D scores. Higher educational attainment (some college [P = 0.001] and college degree or higher [P < 0.0001]) and higher income was also associated with higher PDQS-30D scores (P < 0.0001).
Table 1.
Characteristics and unadjusted diet quality score (Prime Diet Quality Screener [PDQS-30D]) of the sample of low-income adults in the United States between June 23 and July 1, 2020 (N = 1,739)
| n | % | PDQS-30D |
|||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mina | Maxa | P valueb | |||
| Total | 1,739 | 100 | 51.9 | 11.4 | 21 | 97 | N/Ac |
| Sex and genderd | |||||||
| Male | 838 | 48.2 | 52.2 | 11.5 | 24 | 97 | Refe |
| Female | 885 | 50.9 | 51.6 | 11.1 | 21 | 92 | 0.232 |
| Transgender/non-binary/other | 16 | 0.9 | 54.5 | 16.7 | 34 | 90 | 0.430 |
| Age (y) | |||||||
| 18-39 | 790 | 45.4 | 52.4 | 11.4 | 24 | 97 | Ref |
| 40-59 | 493 | 28.4 | 50.3 | 11.2 | 21 | 97 | 0.001 |
| 60+ | 456 | 26.2 | 52.9 | 11.4 | 25 | 92 | 0.491 |
| Race and ethnicity | |||||||
| Non-Hispanic White | 1,109 | 63.8 | 50.8 | 11.1 | 21 | 92 | Ref |
| Non-Hispanic Black | 193 | 11.1 | 52.3 | 10.8 | 28 | 97 | 0.092 |
| Hispanic | 250 | 14.4 | 53.2 | 11.3 | 30 | 88 | 0.002 |
| Asian | 114 | 6.6 | 58.2 | 12.0 | 29 | 97 | < 0.0001 |
| Otherf | 73 | 4.2 | 53.8 | 12.7 | 33 | 92 | 0.043 |
| Education | |||||||
| High school, GED or less | 561 | 32.3 | 49.5 | 10.6 | 24 | 84 | Ref |
| Some college | 583 | 33.5 | 51.7 | 11.5 | 25 | 97 | 0.001 |
| College degree or higher | 595 | 34.2 | 54.4 | 11.4 | 21 | 97 | < 0.0001 |
| Employment | |||||||
| Full time | 470 | 27.0 | 52.4 | 11.1 | 21 | 97 | Ref |
| Part time | 242 | 13.9 | 52.8 | 10.7 | 27 | 88 | 0.647 |
| Unemployed, looking for work | 285 | 16.4 | 51.7 | 11.6 | 29 | 97 | 0.434 |
| Out of the labor force | 742 | 42.7 | 51.5 | 11.6 | 21 | 92 | 0.189 |
| College student | |||||||
| Yes | 111 | 6.4 | 53. | 11. | 29 | 87 | 0.083 |
| No | 1,628 | 93.6 | 51.8 | 11.3 | 21 | 97 | Ref |
| Annual household income | |||||||
| <$35,000 | 1,055 | 60.7 | 50.5 | 11.4 | 21 | 92 | Ref |
| ≥$35,000 | 684 | 39.3 | 54.1 | 10.9 | 26 | 97 | < 0.0001 |
| SNAP participation | |||||||
| Yes | 522 | 30.0 | 49.5 | 10.4 | 21 | 84 | < 0.0001 |
| No | 1,217 | 70.0 | 53.0 | 11.6 | 21 | 97 | Ref |
| Marital status | |||||||
| Single | 664 | 38.3 | 51.5 | 11.9 | 21 | 97 | Ref |
| Married | 534 | 30.8 | 53.6 | 11.4 | 27 | 97 | 0.002 |
| Divorced, separated, widowed | 352 | 20.3 | 51.3 | 10.7 | 21 | 85 | 0.846 |
| Living with a partner | 184 | 10.6 | 50.0 | 10.0 | 27 | 78 | 0.116 |
| Household size | |||||||
| 1-3 people | 1,272 | 73.2 | 51.4 | 11.4 | 21 | 97 | Ref |
| 4 or more people | 467 | 26.9 | 53.4 | 11.1 | 24 | 97 | 0.001 |
| Children younger than 18 years in household | |||||||
| Yes | 523 | 30.1 | 53.5 | 11.0 | 24 | 97 | Ref |
| No | 1,216 | 69.9 | 51.3 | 11.4 | 21 | 92 | < 0.0001 |
| Food security status | |||||||
| High | 722 | 41.5 | 53.4 | 12.2 | 21 | 97 | Ref |
| Marginal | 266 | 15.3 | 52.3 | 11.4 | 26 | 87 | 0.183 |
| Low | 302 | 17.4 | 51.7 | 10.5 | 21 | 82 | 0.028 |
| Very low | 449 | 25.8 | 49.6 | 10.1 | 25 | 97 | < 0.0001 |
| Cooking dinner frequency (times/wk) | |||||||
| 7 | 637 | 36.6 | 53.9 | 12.2 | 21 | 97 | Ref |
| 5-6 | 510 | 29.3 | 52.5 | 10.4 | 27 | 90 | 0.027 |
| 3-4 | 340 | 19.6 | 49.4 | 9.9 | 24 | 97 | < 0.0001 |
| 0-2 | 252 | 14.5 | 49.2 | 11.5 | 21 | 86 | < 0.0001 |
Possible range of scores for the PDQS-30D is 0 to 126. Higher scores indicate better diet quality.
P values from separate simple linear regressions with each categorical variable as the predictor and PDQS-30D score as the outcome.
N/A = not available.
Sex and gender response options were included in the same survey question.
Ref = reference category.
Other race and ethnicity category included Native American (n = 27), Pacific Islander (n = 3), Middle Eastern or North African (n = 8), or participants who entered text in the open response ‘Other’ category (n = 35). ‘Other’ included a variety of responses from participants primarily, but not exclusively, indicating multiple identities, including “mixed,” “multiethnic,” and “multiracial.” Text entries also included responses such as “Latin” or “Israelite,” “human,” or “Lebanese American.”
Overall, 41.5% of the sample experienced high food security (Table 1). In bivariate associations, those with high food security had the highest PDQS-30D score (53.4 ± 12.2) across all food security levels. Individuals experiencing food insecurity comprised 43.2% of the sample (17.4% low food security and 25.8% very low food security) and had lower PDQS-30D scores compared with those with high food security (low vs high: 51.7 ± 10.5 vs 53.4 ± 12.2; P = 0.028; very low vs high: 49.6 ± 10.1 vs 53.4 ± 12.2; P < 0.0001). More than one-third (36.6%) of low-income Americans cooked dinner 7 times/week and had the highest PDQS-30D scores (53.9 ± 12.2) compared with less frequent cooks. The least frequent cooks (0 to 2 times/week) had the lowest mean PDQS-30D score (49.2 ± 11.5; P < 0.0001 [difference from cooking dinner 7 times/week]).
Age- and sex and gender-adjusted associations between food security status and diet quality (PDQS-30D score) are presented in Table 2 . Greater food insecurity was associated with worse PDQS-30D score (P for trend < 0.0001). Compared with individuals with high food security, low food security (β = –1.7, 95% CI –3.2 to –0.1) and very low food security (β = –3.9, 95% CI –5.3 to –2.5) were both significantly associated with lower diet quality. These associations persisted in the fully adjusted models: low food security was associated with a 1.9-point lower PDQS-30D score (95% CI –3.4 to –0.4) and very low food security was associated with a 3.2-point lower PDQS-30D score (95% CI –4.6 to –1.8) compared with high food security.
Table 2.
Food insecurity and cooking dinner frequency associations with diet quality among low-income adults in the United States between June 23 and July 1, 2020 (N = 1,739)
| Variable | Model 1a |
Model 2b |
||
|---|---|---|---|---|
| β | 95% CI | β | 95% CI | |
| Panel A | ||||
| Food security status | ||||
| High | Refc | Ref | ||
| Marginal | –1.1 | –2.7 to 0.5 | –0.9 | –2.5 to 0.6 |
| Low | –1.7 | –3.2 to –0.1 | –1.9 | –3.4 to –0.4 |
| Very low | –3.9 | –5.3 to –2.5 | –3.2 | –4.6 to –1.8 |
| P for trendd | < 0.0001 | < 0.0001 | ||
| Panel B | ||||
| Cooking dinner frequency | ||||
| 7 times/week | Ref | Ref | ||
| 5-6 times/week | –1.5 | –2.8 to –0.2 | –1.59 | –2.9 to –0.3 |
| 3-4 times/week | –4.8 | –6.3 to –3.3 | –4.69 | –6.1 to –3.3 |
| 0-2 times/week | –4.8 | –6.5 to –3.2 | –4.42 | –6.0 to –2.8 |
| P for trend | < 0.0001 | < 0.0001 | ||
Model 1 is an age- and gender-adjusted ordinary least squares regression model (separate models for food security and cooking frequency).
Model 2 is an ordinary least squares model (separate models for food security and cooking frequency) adjusted for age, sex and gender, race and ethnicity, education, income, marital status, household size, presence of children aged younger than 18 years in the household, employment, Supplemental Nutrition Assistance Program participation, and student status.
Ref = reference category.
P for trend obtained using the postestimation contrast command in Stata41 to test whether or not the linear trend across categories is significant.
In age- and sex and gender-adjusted models cooking dinner less frequently was also associated with lower PDQS-30D scores (P for trend < 0.0001) (Table 2). Compared with individuals who cooked dinner at home 7 times/week, cooking dinner 5 to 6 times/week (β = –1.5, 95% CI –2.8 to –0.2), 3 to 4 times/week (β = –4.8, 95% CI –6.3 to, –3.3), and 0 to 2 times/week (β = –4.8, 95% CI –6.5 to –3.2) were all significantly associated with lower diet quality. These associations persisted in the fully adjusted models: cooking 0 to 2 times/week was associated with a 4.4-point lower PDQS-30D score (95% CI –6.0 to –2.8) compared with cooking 7 times/week.
In fully adjusted models that mutually adjusted for food security status and cooking dinner frequency, the significant inverse associations with diet quality for both exposures remained but were slightly attenuated (see Table 3, available at www.jandonline.org). However, there was no evidence that the association between food insecurity and PDQS-30D scores differed based on frequency of cooking dinner (effect modification) based on likelihood ratio tests with multiple degrees of freedom or one degree of freedom (P values > 0.05) (data not shown).
Differences in the frequency of consumption of PDQS-30D components by food security status are available in Table 4 (available at www.jandonline.org ). Lower PDQS-30D scores related to more severe food insecurity were largely accounted for by lower frequency of consumption of several healthy PDQS-30D components (ie, dark green leafy vegetables, cruciferous vegetables, other vegetables, other fruits, nuts and seeds, fish, whole grains, low-fat dairy, and liquid vegetable oils) and higher frequency of consumption of unhealthy PDQS-30D components (ie, processed meats, sugar-sweetened beverages, and fried foods away from home) (all P values < 0.05). Similarly, lower diet quality among those who cooked dinner less frequently (see Table 5, available at www.jandonline.org) was accounted for by lower frequency of consumption of all healthy PDQS-30D components (with the exception of fish) and higher frequency of consumption of some unhealthy components (ie, sugar-sweetened beverages and fried foods away from home all P values < 0.05).
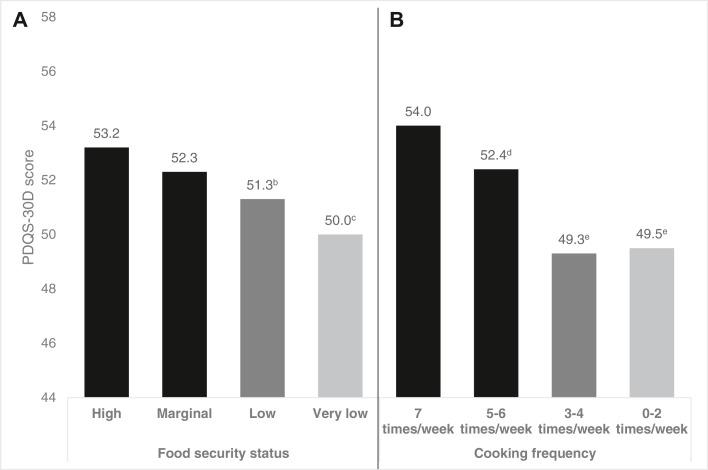
The Figure displays the predicted mean PDQS-30D scores by food security status (Panel A) and frequency of cooking dinner at home (Panel B) based on separate fully adjusted models. Individuals with high food security were expected to have PDQS-30D scores of 53.2 points, which were significantly higher than expected PDQS-30D scores of individuals with low (51.3 points) and very low (50.0 points) food security. Individuals who cooked dinner 7 times/week had the highest expected PDQS-30D scores (54.0 points), which were significantly higher those individuals cooking dinner 5 to 6 times/week (52.4 points), 3 to 4 times/week (49.3 points), and 0 to 2 times/week (49.5 points).
Figure.
Predicted mean Prime Diet Quality Screener (PDQS-30D) scorea by food insecurity (Panel A) and frequency of cooking dinner (Panel B) among low-income adults in the United States between June 23 and July 1, 2020 (N = 1,739). aResults from ordinary least squares regression models (separate models for food security and cooking frequency) adjusted for age, sex and gender, race and ethnicity, education, income, marital status, household size, presence of children younger than age 18 years in the household, employment, Supplemental Nutrition Assistance Program participation, and student status. bDifference from high food security significant at P < 0.05. cDifference from high food security significant at P < 0.001. dDifference from cooking 7 times/week significant at P < 0.05. eDifference from cooking 7 times/week significant at P < 0.001.
Discussion
In this national survey of low-income Americans during the COVID-19 pandemic results show that overall diet quality was poor (mean scores less than half of the possible PDQS-30D score), and that after adjusting for sociodemographic characteristics, both greater food insecurity and less frequent cooking dinner at home were associated with lower diet quality as measured by the PDQS-30D. Contrary to our hypothesis, the relationship between food insecurity and diet quality did not differ by frequency of cooking dinner; in this sample, food insecurity was associated with lower diet quality regardless of how frequently people cooked dinner. Given the high levels of food insecurity observed during the early months of the pandemic from this study and others,7, 8, 9 , 42 and the widening disparities documented in US Department of Agriculture annual food security estimates,12 and prior evidence regarding associations between food insecurity and health,43, 44, 45, 46, 47, 48 findings from this study suggest that adverse diet-related health outcomes may follow.
These findings are consistent with prior evidence showing that food insecurity is associated with poor diet quality, and that these findings are robust across dietary assessment methods and diet quality indexes.1, 2, 3, 4 , 49, 50, 51, 52 PDQS-30D scores were also low for all demographic groups (mean scores were all below 50% of possible scores), which is consistent with prior evidence of poor diet quality among Americans with low income.53 , 54 PDQS-30D scores in this sample were also lower than prior estimates among US women (mean score = 56 points).29 Also consistent with prior research,2 , 3 , 23 , 51 , 52 lower diet quality among those experiencing food insecurity was due to lower consumption of some fruits and vegetables, whole grains, and healthy fats; and higher consumption of highly palatable and highly processed foods such as processed meat, fried foods, and sweetened beverages. These known associations between food insecurity and diet quality not only persisted for low-income Americans during the COVID-19 pandemic, but may have also been exacerbated because food-insecure households faced unique challenges in acquiring necessary food items during the early months of the pandemic.7
Notably, the mean frequency of cooking dinner (5.0 times/week) in the current study is consistent with the prepandemic mean frequency of cooking dinner as measured in multiple US national samples.17 , 55 , 56 This suggests that although some people may have been cooking more frequently in the early months of the pandemic, on average, overall cooking dinner frequency did not increase. It is also notable that even within a low-income sample, higher cooking dinner frequency was still associated with better diet quality, even after adjusting for sociodemographic measures that contrasts with prior evidence.18 The fact that the relationship between food insecurity and diet quality did not differ by cooking dinner frequency is also striking. Although cooking is a modifiable behavior that can improve diet quality, our findings suggest that other policy interventions are needed to improve food access and availability, both key dimensions of food insecurity,57 , 58 to influence diet quality in food-insecure populations.
During the COVID-19 pandemic numerous policy interventions, including stimulus payments and unemployment insurance program expansions, aimed to blunt the economic influence of the pandemic for US households, particularly those at risk for food insecurity.59, 60, 61 SNAP, the largest federal nutrition assistance program, expanded rapidly growing by 17% in the early months of the pandemic.62 Later Congressional relief bills further modified the program to, among other things, ease enrollment and recertification requirements and increase benefits by 15%.59, 60, 61 The present findings underscore that though those efforts likely contributed to overall estimates of food insecurity remaining stable from 2019 to 2020,12 many households still experienced food insecurity, which was associated with poor diet quality even when people cooked at home frequently. Due to the positive association between cooking frequency and diet quality, more efforts and continued support is needed to help households at risk for food insecurity both procure and prepare enough nutritious food to support a healthy diet.63, 64, 65, 66, 67, 68 The recent changes to the Thrifty Food Plan, which SNAP benefits are based on, will increase SNAP benefits by 21% and are an important step that may help food insecure households afford the true cost of a healthy diet.69 It will be important for future research to investigate whether or not/how these benefit increases influence cooking behaviors and diet quality.
Limitations
This study should be considered in light of several limitations. Primarily, the cross-sectional nature of the data precludes making any causal inferences about food insecurity, cooking and diet quality. Measures of prepandemic food security status or cooking frequency were also not included, which precludes examination of pandemic related changes in food security or cooking. Second, all data are self-reported which can lead to social desirability and recall bias.70 This may be particularly relevant when it comes to the PDQS-30D data. The PDQS-30D requires participants to recall and estimate usual frequency of consumption over the past 30 days, which could be more vulnerable to recall bias than a shorter timeframe or 24-hour recall. Relatedly, selection bias could also be present if Prime Panel members who participated in the survey systematically differed from those who did not participate or from the general population. The use of quotas to match the sample with US Census demographic characteristics mitigates some of this concern (see Table 6, available at www.jand.online), but unmeasured differences could still be present, which could limit generalizability. Another potential limitation related to the survey platform used is satisficing,71 in which respondents rush through a survey and do not provide thoughtful or true answers. To address this possibility participants who completed the survey unreasonably quickly or who failed attention checks embedded in the survey were excluded. Furthermore, the survey was fielded with PrimePanels, which employs their own quality checks for participants who are part of the panel. Third, the survey was fielded in English only, and its web-based nature required participants to have Internet access. This could limit the representativeness of the data to some subpopulations that are particularly vulnerable to food insecurity (ie, those with very low incomes, without high school degrees, or without Internet access) and could limit the generalizability of the results to non-English–speaking populations. Fourth, the PDQS-30D is a short form dietary screener that does not fully capture every food or beverage a person could consume, but rather focuses on a limited number of food and beverage groups. However, the PDQS-30D has compared well against an open-ended dietary assessment method, specifically the ASA24.29 Fifth, the observed differences in dietary quality measured in this study were relatively small and how sustained such differences would be over time or how likely they are to contribute to differences in health outcomes over the long term is unknown. In addition, the way sex was measured in the survey included both biological sex and gender identity response options within the same question, which could have caused confusion among some participants about how to respond. Finally, the cooking frequency measure used in this study focused on only frequency of cooking dinner, rather than other meals, and did not further define what types of food preparation should be included in the definition of cooking, which prior research shows varies considerably and can influence how individuals report how frequently they cook at home.55 , 72 Although frequency of cooking dinner was chosen because it is a widely used measure of cooking frequency,17 , 31 , 55 , 56 , 73 , 74 and because, in the United States, dinner is the most frequently cooked meal,55 it is possible that, particularly during the COVID-19 pandemic, other meals were cooked at home more frequently, which could also influence diet quality. Relatedly, cooking skill levels, motivation for cooking, or other factors that could influence the relationship between cooking frequency and diet quality were not investigated in this study.
Conclusions
During the COVID-19 pandemic, overall diet quality in this sample of low-income Americans was poor and low food security and less frequent cooking dinner at home were both associated with lower diet quality. However, the relationship between food security and diet quality did not differ based on frequency of cooking dinner, indicating that food insecurity in the present sample was associated with lower diet quality regardless of how frequently people cooked dinner at home. More research is needed to identify and address barriers to low-income households’ ability to access, afford, and prepare enough nutritious food for a healthy diet.
Biographies
J. Wolfson is an assistant professor, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD.
H. Posluszny is a master’s degree student, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD.
S. Kronsteiner-Gicevic is a visiting researcher, Harvard T.H. Chan School of Public Health, Boston, MA.
W. Willet is a professor, Harvard T.H. Chan School of Public Health, Boston, MA.
C. Leung is an assistant professor, University of Michigan School of Public Health, Ann Arbor, MI.
Footnotes
Supplementary materials:Table 3, Table 4, Table 5, Table 6 are available at www.jandonline.org
STATEMENT OF POTENTIAL CONFLICT OF INTEREST No potential conflict of interest was reported by the authors.
FUNDING/SUPPORT Funding for this study was provided by a Faculty Research Grant from the University of Michigan Poverty Solutions. J. Wolfson was supported by the National Institutes of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (award #K01DK119166) and C. Leung was supported by the Eunice Kennedy Shriver National Institute for Child Health and Human Development (award #4R00HD084758). The funders had no role in the design of the study, analysis, or interpretation of the data or in writing the manuscript.
AUTHOR CONTRIBUTIONS J. Wolfson and C. Leung designed the study and developed and fielded the survey. J. Wolfson and C. Leung developed the study hypotheses. J. Wolfson conducted the analyses and wrote the first draft of the manuscript. All authors critically reviewed and approved the manuscript as submitted.
Supplementary Materials
Table 3.
Food security and cooking dinner frequency associations with diet quality among low-income adults in the United States between June 23 and July 1, 2020 (N = 1,739)
| Variable | Model 3a |
|
|---|---|---|
| β | 95% CI | |
| Food security status | ||
| High | Refb | |
| Marginal | –0.8 | –2.3 to 0.7 |
| Low | –1.6 | –3.1 to –0.2 |
| Very low | –2.8 | –4.1 to –1.4 |
| P for trendc | 0.0001 | |
| Cooking dinner frequency (times/wk) | ||
| 7 | Ref | |
| 5-6 | –1.7 | –2.9 to –0.3 |
| 3-4 | –4.5 | –5.9 to –3.0 |
| 0-2 | –4.2 | –5.8 to –2.6 |
| P for trendc | < 0.0001 | |
Model 3 is an ordinary least squares model that included food insecurity, cooking frequency (both exposures simultaneously in the model), age, sex and gender, race and ethnicity, education, income, marital status, household size, presence of children younger than age 18 years in the household, employment, Supplemental Nutrition Assistance Program participation, and student status.
Ref = reference category.
P value for trend obtained by using the postestimation contrast command in Stata41 to test whether or not the linear trend across categories is significant.
Table 4.
Differences in Prime Diet Quality Screener (PDQS-30D) component consumption frequency (%) by food security status among low-income adults in the United States between June 23 and July 1, 2020 (N = 1,739)
| Component | Food Security Status |
P valuea | |||
|---|---|---|---|---|---|
| High (n = 722) |
Marginal (n = 266) |
Low (n = 302) |
Very Low (n = 449) |
||
| ←%→ | |||||
| Healthy | |||||
| Dark green leafy vegetables | |||||
| ≤ once/mo | 26.9 | 27.8 | 29.5 | 34.3 | < 0.001 |
| 2-3 times/mo | 18.1 | 18.4 | 22.2 | 27.2 | |
| 1-2 times/wk | 24.9 | 25.9 | 28.5 | 18.9 | |
| 3-4 times/wk | 16.5 | 15.8 | 12.6 | 12.9 | |
| 5-6 times/wk | 5.8 | 6.0 | 4.0 | 2.9 | |
| Once a day | 5.3 | 4.9 | 2.7 | 2.9 | |
| ≥2 times/d | 2.5 | 1.1 | 0.6 | 0.9 | |
| Cruciferous vegetables | |||||
| ≤ once/mo | 26 | 29.7 | 26.5 | 35.9 | 0.002 |
| 2-3 times/mo | 21.3 | 19.9 | 28.2 | 23.4 | |
| 1-2 times/wk | 26.3 | 24.4 | 24.2 | 23.6 | |
| 3-4 times/wk | 14.8 | 18.1 | 12.3 | 12.3 | |
| 5-6 times/wk | 5.7 | 4.1 | 5.6 | 2.2 | |
| Once a day | 4.7 | 3.0 | 3.3 | 1.8 | |
| ≥2 times/d | 1.1 | 0.8 | 0 | 0.9 | |
| Deep orange vegetables | |||||
| ≤ once/mo | 35 | 35.3 | 36.1 | 42.1 | 0.312 |
| 2-3 times/mo | 24.5 | 25.9 | 28.8 | 26.5 | |
| 1-2 times/wk | 25.1 | 25.6 | 21.2 | 17.2 | |
| 3-4 times/wk | 8.3 | 7.5 | 8.6 | 9.6 | |
| 5-6 times/wk | 4.4 | 2.6 | 3.0 | 2.9 | |
| Once a day | 1.8 | 2.3 | 1.7 | 1.3 | |
| ≥2 times/d | 0.8 | 0.8 | 0.7 | 0.5 | |
| Other vegetables | |||||
| ≤ once/mo | 16.9 | 19.9 | 17.6 | 27.4 | <0.001 |
| 2-3 times/mo | 17.0 | 22.2 | 25.5 | 23.2 | |
| 1-2 times/wk | 28.0 | 29.7 | 27.5 | 23.6 | |
| 3-4 times/wk | 21.9 | 18.8 | 20.5 | 16.7 | |
| 5-6 times/wk | 10.7 | 4.4 | 6.0 | 5.6 | |
| Once a day | 4.3 | 3.4 | 2.0 | 2.2 | |
| ≥2 times/d | 1.3 | 1.9 | 1.0 | 1.3 | |
| Citrus fruits | |||||
| ≤ once/mo | 32.7 | 36.1 | 26.2 | 33.6 | 0.105 |
| 2-3 times/mo | 22.0 | 19.6 | 24.5 | 28.3 | |
| 1-2 times/wk | 20.2 | 21.1 | 20.5 | 18.0 | |
| 3-4 times/wk | 12.5 | 10.9 | 16.2 | 10.7 | |
| 5-6 times/wk | 4.9 | 4.9 | 6.6 | 4.9 | |
| Once a day | 6.0 | 5.3 | 4.6 | 2.9 | |
| ≥2 times/d | 1.8 | 2.3 | 1.3 | 1.6 | |
| Deep orange fruits | |||||
| ≤ once/mo | 58.3 | 54.5 | 49.7 | 56.4 | 0.472 |
| 2-3 times/mo | 18.0 | 22.2 | 21.5 | 19.8 | |
| 1-2 times/wk | 13.6 | 13.9 | 15.9 | 13.1 | |
| 3-4 times/wk | 6.2 | 4.9 | 8.3 | 5.1 | |
| 5-6 times/wk | 1.5 | 1.5 | 3.0 | 2.9 | |
| Once a day | 1.9 | 2.3 | 1.3 | 1.6 | |
| ≥2 times/d | 0.4 | 0.8 | 0.3 | 1.1 | |
| Other fruits | |||||
| ≤ once/mo | 16.2 | 16.9 | 18.2 | 24.1 | <0.001 |
| 2-3 times/mo | 23.3 | 25.2 | 27.5 | 28.1 | |
| 1-2 times/wk | 22.0 | 25.2 | 23.2 | 26.7 | |
| 3-4 times/wk | 18.8 | 15.8 | 18.5 | 13.1 | |
| 5-6 times/wk | 10.0 | 7.1 | 7.6 | 3.6 | |
| Once a day | 7.3 | 7.9 | 4.3 | 2.9 | |
| ≥2 times/d | 2.4 | 1.9 | 0.7 | 1.6 | |
| Legumes | |||||
| ≤ once/mo | 27.8 | 22.9 | 23.5 | 25.8 | 0.119 |
| 2-3 times/mo | 24.8 | 30.1 | 27.5 | 26.7 | |
| 1-2 times/wk | 26.5 | 29.7 | 32.5 | 22.3 | |
| 3-4 times/wk | 13.3 | 10.9 | 11.6 | 14.7 | |
| 5-6 times/wk | 4.7 | 3.8 | 3.6 | 6.0 | |
| Once a day | 1.9 | 1.9 | 1.3 | 2.9 | |
| ≥2 times/d | 1.0 | 0.8 | 0 | 1.6 | |
| Nuts and seeds | |||||
| ≤ once/mo | 30.3 | 28.2 | 32.8 | 42.5 | <0.001 |
| 2-3 times/mo | 20.8 | 27.4 | 26.2 | 21.8 | |
| 1-2 times/wk | 21.2 | 20.3 | 22.5 | 17.8 | |
| 3-4 times/wk | 13.9 | 12.0 | 9.9 | 11.8 | |
| 5-6 times/wk | 6.9 | 6.4 | 4.3 | 3.6 | |
| Once a day | 6.0 | 3.4 | 2.7 | 1.3 | |
| ≥2 times/d | 1.0 | 2.3 | 1.7 | 1.1 | |
| Poultry | |||||
| ≤ once/mo | 9.6 | 11.3 | 11.3 | 15.1 | 0.068 |
| 2-3 times/mo | 18 | 16.5 | 19.9 | 22.5 | |
| 1-2 times/wk | 36.1 | 29.0 | 30.5 | 31.2 | |
| 3-4 times/wk | 24.1 | 29.0 | 25.8 | 20.3 | |
| 5-6 times/wk | 7.8 | 10.5 | 8.0 | 6.9 | |
| Once a day | 3.5 | 3 | 3.3 | 2.2 | |
| ≥2 times/d | 1.1 | 0.8 | 1.3 | 1.8 | |
| Fish | |||||
| ≤ once/mo | 41.1 | 39.5 | 40.1 | 52.3 | <0.001 |
| 2-3 times/mo | 26.6 | 30.8 | 27.8 | 22.9 | |
| 1-2 times/wk | 25.2 | 22.2 | 20.2 | 15.1 | |
| 3-4 times/wk | 5.1 | 5.9 | 8.9 | 5.4 | |
| 5-6 times/wk | 1.7 | 2.6 | 2.0 | 2.5 | |
| Once a day | 0.3 | 0 | 0.7 | 0.7 | |
| ≥2 times/d | 0 | 0 | 0.3 | 1.1 | |
| Whole grains | |||||
| ≤ once/mo | 15.7 | 18.4 | 15.6 | 19.2 | 0.001 |
| 2-3 times/mo | 14.1 | 14.3 | 24.5 | 16.3 | |
| 1-2 times/wk | 24.2 | 24.4 | 23.8 | 27.6 | |
| 3-4 times/wk | 19.4 | 20.3 | 19.2 | 19.6 | |
| 5-6 times/wk | 12.3 | 13.5 | 10.3 | 9.1 | |
| Once a day | 11.8 | 7.1 | 5.6 | 5.8 | |
| ≥2 times/d | 2.5 | 1.9 | 1.0 | 2.5 | |
| Low fat dairy | |||||
| ≤ once/mo | 34.6 | 35.7 | 25.5 | 26.1 | <0.001 |
| 2-3 times/mo | 12.3 | 14.7 | 16.9 | 16.7 | |
| 1-2 times/wk | 13.2 | 16.2 | 27.2 | 23.8 | |
| 3-4 times/wk | 14.4 | 12.0 | 13.6 | 18.5 | |
| 5-6 times/wk | 9.8 | 8.7 | 7.6 | 4.9 | |
| Once a day | 11.9 | 9.4 | 7.3 | 7.4 | |
| ≥2 times/d | 3.7 | 3.4 | 2.0 | 2.7 | |
| Liquid vegetable oils | |||||
| ≤ once/mo | 27.6 | 31.2 | 23.5 | 31.6 | 0.013 |
| 2-3 times/mo | 19.1 | 17.3 | 17.6 | 22.3 | |
| 1-2 times/wk | 21.5 | 22.6 | 28.5 | 20.5 | |
| 3-4 times/wk | 14.8 | 13.2 | 16.2 | 14.0 | |
| 5-6 times/wk | 10.7 | 6.8 | 8.6 | 5.8 | |
| Once a day | 4.0 | 6.4 | 5.3 | 4.7 | |
| ≥2 times/d | 2.4 | 2.6 | 0.3 | 1.1 | |
| UNHEALTHY | % | % | % | % | |
| Red meat as a main dish | |||||
| ≤ once/mo | 16.2 | 18.4 | 22.5 | 21.6 | 0.063 |
| 2-3 times/mo | 21.2 | 18.1 | 22.5 | 24.7 | |
| 1-2 times/wk | 35.2 | 36.8 | 29.1 | 29.6 | |
| 3-4 times/wk | 20.5 | 20.3 | 20.5 | 16.1 | |
| 5-6 times/wk | 5.4 | 4.9 | 3.0 | 5.8 | |
| Once a day | 1.3 | 1.5 | 1.7 | 1.1 | |
| ≥2 times/d | 0.3 | 0 | 0.7 | 1.1 | |
| Processed meat | |||||
| ≤ once/mo | 23.8 | 21.4 | 20.5 | 21.4 | 0.003 |
| 2-3 times/mo | 25.5 | 27.1 | 24.8 | 20.9 | |
| 1-2 times/wk | 30.6 | 25.9 | 33.1 | 25.6 | |
| 3-4 times/wk | 14.7 | 18.4 | 13.6 | 19.8 | |
| 5-6 times/wk | 3.6 | 4.1 | 4.6 | 8.2 | |
| Once a day | 1.3 | 2.6 | 3.3 | 2.9 | |
| ≥2 times/d | 0.6 | 0.4 | 0 | 1.1 | |
| Potatoes | |||||
| ≤ once/mo | 20.5 | 21.8 | 21.5 | 27.6 | 0.009 |
| 2-3 times/mo | 14.5 | 16.5 | 22.2 | 18.5 | |
| 1-2 times/wk | 29.0 | 29.0 | 27.8 | 20.7 | |
| 3-4 times/wk | 24.2 | 21.8 | 18.2 | 22.5 | |
| 5-6 times/wk | 7.6 | 7.5 | 7.3 | 6.9 | |
| Once a day | 3.6 | 1.5 | 2.3 | 2.2 | |
| ≥2 times/d | 0.6 | 1.9 | 0.7 | 1.6 | |
| Refined grains and baked goods | |||||
| ≤ once/mo | 11.6 | 12.4 | 13.6 | 14.0 | 0.025 |
| 2-3 times/mo | 18.1 | 17.7 | 23.5 | 14.9 | |
| 1-2 times/wk | 28.5 | 28.2 | 28.5 | 25.9 | |
| 3-4 times/wk | 20.2 | 21.1 | 22.2 | 26.1 | |
| 5-6 times/wk | 10.4 | 11.3 | 7.6 | 9.6 | |
| Once a day | 9.0 | 7.9 | 4.0 | 6.2 | |
| ≥2 times/d | 2.1 | 1.5 | 0.7 | 3.3 | |
| Sugar-sweetened beverages | |||||
| ≤ once/mo | 39.6 | 36.1 | 25.5 | 26.1 | <0.001 |
| 2-3 times/mo | 12.2 | 17.7 | 12.3 | 15.6 | |
| 1-2 times/wk | 16.8 | 12.4 | 20.5 | 16.5 | |
| 3-4 times/wk | 10.0 | 11.7 | 12.3 | 14.5 | |
| 5-6 times/wk | 6.1 | 6.0 | 11.9 | 7.4 | |
| Once a day | 7.9 | 9.0 | 9.6 | 8.4 | |
| ≥2 times/d | 7.5 | 7.1 | 8.0 | 11.8 | |
| Fried foods away from home | |||||
| ≤ once/mo | 39.8 | 35.7 | 30.1 | 36.5 | <0.001 |
| 2-3 times/mo | 25.6 | 27.1 | 27.8 | 22.5 | |
| 1-2 times/wk | 24.8 | 25.2 | 22.5 | 21.2 | |
| 3-4 times/wk | 7.3 | 7.9 | 13.3 | 11.6 | |
| 5-6 times/wk | 1.5 | 3.0 | 4.3 | 3.8 | |
| Once a day | 0.8 | 1.1 | 1.3 | 1.8 | |
| ≥2 times/d | 0.1 | 0 | 0.7 | 2.7 | |
| Sweets and ice cream | |||||
| ≤ once/mo | 15.1 | 17.7 | 19.2 | 28.5 | <0.001 |
| 2-3 times/mo | 21.2 | 24.4 | 20.9 | 24.9 | |
| 1-2 times/wk | 25.2 | 22.2 | 27.2 | 22.3 | |
| 3-4 times/wk | 18.8 | 20.7 | 18.2 | 12.7 | |
| 5-6 times/wk | 9.4 | 6.8 | 5.0 | 5.8 | |
| Once a day | 7.2 | 6.8 | 6.0 | 2.9 | |
| ≥2 times/d | 3.1 | 1.5 | 3.6 | 2.9 | |
| NEUTRAL | % | % | % | % | |
| Eggs | |||||
| ≤ once/mo | 16.2 | 19.2 | 10.3 | 17.6 | 0.150 |
| 2-3 times/mo | 17.5 | 16.9 | 20.2 | 18.5 | |
| 1-2 times/wk | 28.1 | 24.4 | 31.8 | 25.8 | |
| 3-4 times/wk | 19.5 | 18.8 | 22.9 | 20.5 | |
| 5-6 times/wk | 9.1 | 10.2 | 6.6 | 9.4 | |
| Once a day | 9.0 | 9.4 | 7.3 | 6.5 | |
| ≥2 times/d | 0.6 | 1.3 | 2.0 | 1.8 | |
Bold values are statistically significant (P < .05).
P values from Pearson’s χ2 test.
Table 5.
Differences in Prime Diet Quality Screener (PDQS-30D) component consumption frequency by frequency of cooking dinner among low-income adults in the United States between June 23 and July 1, 2020 (N = 1,739)
| Component | Dinner cooking frequency (times/wk) |
P valuea | |||
|---|---|---|---|---|---|
| 7 (n = 637) |
5-6 (n = 510) |
3-4 (n = 340) |
0-2 (n = 252) |
||
| Healthy | |||||
| Dark green leafy vegetables | |||||
| ≤ once/mo | 29.0 | 22.4 | 31.5 | 41.7 | < 0.001 |
| 2-3 times/mo | 16.8 | 23.7 | 24.4 | 23.0 | |
| 1-2 times/wk | 23.4 | 27.7 | 25.0 | 17.9 | |
| 3-4 times/wk | 17.1 | 15.1 | 14.1 | 9.1 | |
| 5-6 times/wk | 6.6 | 5.1 | 2.1 | 3.2 | |
| Once a day | 4.9 | 5.3 | 1.5 | 3.6 | |
| ≥2 times/d | 2.2 | 0.8 | 1.5 | 1.6 | |
| Cruciferous vegetables | |||||
| ≤ once/mo | 27.5 | 24.7 | 30.6 | 40.9 | < 0.001 |
| 2-3 times/mo | 21.4 | 23.3 | 24.7 | 23.0 | |
| 1-2 times/wk | 23.9 | 27.1 | 27.9 | 19.4 | |
| 3-4 times/wk | 14.4 | 18.4 | 10.9 | 9.5 | |
| 5-6 times/wk | 6.8 | 3.3 | 3.8 | 2.4 | |
| Once a day | 5.0 | 2.6 | 1.8 | 3.6 | |
| ≥2 times/d | 1.1 | 0.6 | 0.3 | 1.2 | |
| Deep orange vegetables | |||||
| ≤ once/mo | 36.4 | 29.4 | 41.5 | 48.4 | < 0.001 |
| 2-3 times/mo | 23.7 | 32.0 | 24.4 | 21.8 | |
| 1-2 times/wk | 25.1 | 22.9 | 21.2 | 16.3 | |
| 3-4 times/wk | 8.8 | 9.4 | 7.4 | 7.9 | |
| 5-6 times/wk | 2.8 | 4.3 | 4.4 | 2.4 | |
| Once a day | 2.2 | 1.4 | 0.6 | 2.8 | |
| ≥2 times/d | 0.9 | 0.6 | 0.6 | 0.4 | |
| Other vegetables | |||||
| ≤ once/mo | 18.7 | 13.9 | 24.1 | 31.4 | < 0.001 |
| 2-3 times/mo | 20.7 | 18.6 | 23.2 | 22.6 | |
| 1-2 times/wk | 24.8 | 31.0 | 27.9 | 23.4 | |
| 3-4 times/wk | 19.0 | 26.1 | 16.5 | 13.9 | |
| 5-6 times/wk | 10.4 | 6.9 | 5.6 | 4.4 | |
| Once a day | 5.0 | 2.4 | 1.2 | 3.2 | |
| ≥2 times/d | 1.4 | 1.2 | 1.5 | 1.2 | |
| Citrus fruits | |||||
| ≤ once/mo | 34.9 | 25.3 | 32.4 | 40.1 | < 0.001 |
| 2-3 times/mo | 21.5 | 23.9 | 28.5 | 22.2 | |
| 1-2 times/wk | 18.4 | 22.6 | 19.4 | 18.7 | |
| 3-4 times/wk | 11.5 | 13.5 | 13.8 | 10.7 | |
| 5-6 times/wk | 5.2 | 7.8 | 2.7 | 3.2 | |
| Once a day | 6.1 | 5.7 | 1.8 | 4.0 | |
| ≥2 times/d | 2.5 | 1.2 | 1.5 | 1.2 | |
| Deep orange fruits | |||||
| ≤ once/mo | 60.2 | 50.8 | 54.7 | 56.0 | 0.012 |
| 2-3 times/mo | 16.5 | 21.6 | 22.1 | 21.0 | |
| 1-2 times/wk | 12.6 | 16.7 | 12.4 | 13.9 | |
| 3-4 times/wk | 6.0 | 4.5 | 7.4 | 7.9 | |
| 5-6 times/wk | 1.7 | 3.5 | 2.1 | 0.4 | |
| Once a day | 2.5 | 2.2 | 0.9 | 0.4 | |
| ≥2 times/d | 0.6 | 0.8 | 0.6 | 0.4 | |
| Other fruits | |||||
| ≤ once/mo | 20.7 | 11.4 | 20.3 | 26.2 | < 0.001 |
| 2-3 times/mo | 24.3 | 23.5 | 29.7 | 27.0 | |
| 1-2 times/wk | 22.0 | 24.7 | 25.3 | 25.4 | |
| 3-4 times/wk | 15.2 | 22.0 | 16.5 | 11.1 | |
| 5-6 times/wk | 7.4 | 9.6 | 5.6 | 5.6 | |
| Once a day | 7.5 | 6.7 | 2.7 | 3.6 | |
| ≥2 times/d | 2.8 | 2.2 | 0.0 | 0.8 | |
| Legumes | |||||
| ≤ once/mo | 23.4 | 20.6 | 32.1 | 34.1 | < 0.001 |
| 2-3 times/mo | 23.7 | 28.0 | 28.2 | 28.6 | |
| 1-2 times/wk | 26.7 | 32.0 | 22.4 | 23.4 | |
| 3-4 times/wk | 15.4 | 13.5 | 11.8 | 7.5 | |
| 5-6 times/wk | 5.7 | 3.9 | 3.8 | 5.2 | |
| Once a day | 3.1 | 1.8 | 1.2 | 1.2 | |
| ≥2 times/d | 2.0 | 0.2 | 0.6 | 0.0 | |
| Nuts and seeds | |||||
| ≤ once/mo | 34.2 | 29.6 | 34.1 | 39.3 | < 0.001 |
| 2-3 times/mo | 19.3 | 24.3 | 25.3 | 26.6 | |
| 1-2 times/wk | 19.5 | 24.5 | 20.0 | 15.1 | |
| 3-4 times/wk | 11.5 | 11.6 | 16.5 | 10.7 | |
| 5-6 times/wk | 7.5 | 5.3 | 2.9 | 4.4 | |
| Once a day | 5.8 | 3.9 | 0.9 | 2.4 | |
| ≥2 times/d | 2.2 | 0.8 | 0.3 | 1.6 | |
| Poultry | |||||
| ≤ once/mo | 13.3 | 7.5 | 10.9 | 16.3 | 0.001 |
| 2-3 times/mo | 17.4 | 16.5 | 22.1 | 25.8 | |
| 1-2 times/wk | 31.4 | 35.5 | 35.3 | 27.0 | |
| 3-4 times/wk | 24.2 | 27.8 | 21.8 | 19.8 | |
| 5-6 times/wk | 8.8 | 8.6 | 7.4. | 5.6 | |
| Once a day | 3.5 | 2.8 | 2.1 | 4.0 | |
| ≥2 times/d | 1.4 | 1.4 | 0.6 | 1.6 | |
| Fish | |||||
| ≤ once/mo | 42.7 | 40.6 | 45.9 | 48.8 | 0.217 |
| 2-3 times/mo | 24.8 | 27.7 | 27.1 | 27.8 | |
| 1-2 times/wk | 24.3 | 23.3 | 17.4 | 14.7 | |
| 3-4 times/wk | 5.3 | 5.9 | 6.2 | 6.4 | |
| 5-6 times/wk | 2.0 | 2.2 | 2.4 | 1.6 | |
| Once a day | 0.5 | 0.2 | 0.3 | 0.8 | |
| ≥2 times/d | 0.3 | 0.2 | 0.9 | 0.0 | |
| Whole grains | |||||
| ≤ once/mo | 17.4 | 15.5 | 14.4 | 22.2 | < 0.001 |
| 2-3 times/mo | 15.4 | 14.1 | 21.2 | 17.9 | |
| 1-2 times/wk | 21.5 | 26.9 | 26.8 | 28.2 | |
| 3-4 times/wk | 19.0 | 22.4 | 20.3 | 14.3 | |
| 5-6 times/wk | 12.6 | 11.4 | 10.9 | 8.7 | |
| Once a day | 10.4 | 8.8 | 5.0 | 7.5 | |
| ≥2 times/d | 3.8 | 1.0 | 1.5 | 1.2 | |
| Low-fat dairy | |||||
| ≤ once/mo | 32.8 | 27.1 | 29.7 | 36.1 | < 0.001 |
| 2-3 times/mo | 11.99 | 13.1 | 19.4 | 17.9 | |
| 1-2 times/wk | 16.5 | 21.6 | 22.4 | 14.3 | |
| 3-4 times/wk | 13.8 | 17.7 | 14.1 | 13.5 | |
| 5-6 times/wk | 7.9 | 7.8 | 6.5 | 10.7 | |
| Once a day | 12.1 | 11.4 | 4.4 | 6.4 | |
| ≥2 times/d | 5.0 | 1.4 | 3.5 | 1.2 | |
| Liquid vegetable oils | |||||
| ≤ once/mo | 28.4 | 19.4 | 27.9 | 47.6 | < 0.001 |
| 2-3 times/mo | 18.8 | 17.5 | 22.7 | 20.2 | |
| 1-2 times/wk | 20.1 | 28.2 | 24.7 | 14.7 | |
| 3-4 times/wk | 13.5 | 18.0 | 15.3 | 9.5 | |
| 5-6 times/wk | 9.4 | 10.4 | 6.2 | 5.2 | |
| Once a day | 6.8 | 5.1 | 2.4 | 2.4 | |
| ≥2 times/d | 3.0 | 1.4 | 0.9 | 0.4 | |
| UNHEALTHY | |||||
| Red meat as a main dish | |||||
| ≤ once/mo | 21.5 | 13.3 | 17.7 | 26.2 | < 0.001 |
| 2-3 times/mo | 19.5 | 18.6 | 24.4 | 31.0 | |
| 1-2 times/wk | 32.5 | 35.1 | 35.9 | 25.8 | |
| 3-4 times/wk | 18.8 | 25.3 | 15.6 | 13.5 | |
| 5-6 times/wk | 6.1 | 5.3 | 4.7 | 2.0 | |
| Once a day | 1.1 | 2.0 | 0.9 | 1.2 | |
| ≥2 times/d | 0.5 | 0.4 | 0.9 | 0.4 | |
| Processed meat | |||||
| ≤ once/mo | 26.2 | 17.8 | 18.8 | 25.8 | 0.009 |
| 2-3 times/mo | 22.9 | 22.4 | 29.4 | 25.8 | |
| 1-2 times/wk | 27.0 | 32.9 | 26.2 | 30.2 | |
| 3-4 times/wk | 14.8 | 18.8 | 18.8 | 12.3 | |
| 5-6 times/wk | 5.3 | 5.3 | 5.0 | 4.0 | |
| Once a day | 3.0 | 2.2 | 1.8 | 1.2 | |
| ≥2 times/d | 0.8 | 0.6 | 0.0 | 0.8 | |
| Potatoes | |||||
| ≤ once/mo | 22.9 | 16.1 | 24.1 | 33.7 | < 0.001 |
| 2-3 times/mo | 18.2 | 15.7 | 14.4 | 21.4 | |
| 1-2 times/wk | 25.0 | 30.4 | 30.3 | 18.3 | |
| 3-4 times/wk | 21.7 | 26.5 | 22.7 | 15.5 | |
| 5-6 times/wk | 7.4 | 8.0 | 6.5 | 7.1 | |
| Once a day | 3.1 | 2.9 | 1.2 | 3.2 | |
| ≥2 times/d | 1.7 | 0.4 | 0.9 | 0.8 | |
| Refined grains and baked goods | |||||
| ≤ once/mo | 14.3 | 7.8 | 12.7 | 18.7 | < 0.001 |
| 2-3 times/mo | 16.2 | 16.7 | 20.3 | 23.4 | |
| 1-2 times/wk | 27.9 | 29.4 | 28.8 | 22.6 | |
| 3-4 times/wk | 18.4 | 28.8 | 21.7 | 19.1 | |
| 5-6 times/wk | 11.0 | 9.8 | 9.1 | 7.9 | |
| Once a day | 9.6 | 5.7 | 5.6 | 6.8 | |
| ≥2 times/d | 2.7 | 1.8 | 1.8 | 1.6 | |
| Sugar-sweetened beverages | |||||
| ≤ once/mo | 42.2 | 27.3 | 26.2 | 31.4 | < 0.001 |
| 2-3 times/mo | 12.1 | 13.7 | 15.6 | 16.7 | |
| 1-2 times/wk | 14.0 | 18.2 | 20.3 | 15.5 | |
| 3-4 times/wk | 8.2 | 15.1 | 15.0 | 9.9 | |
| 5-6 times/wk | 6.8 | 8.4 | 7.7 | 6.8 | |
| Once a day | 7.8 | 9.2 | 7.9 | 9.5 | |
| ≥2 times/d | 9.1 | 8.0 | 7.1 | 10.3 | |
| Fried foods away from home | |||||
| ≤ once/mo | 52.6 | 27.1 | 22.1 | 35.3 | <0.001 |
| 2-3 times/mo | 22.5 | 29.4 | 24.7 | 25.8 | |
| 1-2 times/wk | 15.9 | 30.2 | 28.8 | 22.2 | |
| 3-4 times/wk | 5.2 | 9.8 | 16.8 | 10.3 | |
| 5-6 times/wk | 2.2 | 1.8 | 5.6 | 2.8 | |
| Once a day | 1.1 | 0.8 | 1.2 | 2.4 | |
| ≥2 times/d | 0.6 | 1.0 | 0.9 | 1.2 | |
| Sweets and ice cream | |||||
| ≤ once/mo | 25.6 | 12.0 | 15.6 | 25.8 | < 0.001 |
| 2-3 times/mo | 22.9 | 19.6 | 22.9 | 27.4 | |
| 1-2 times/wk | 21.0 | 28.6 | 26.8 | 20.6 | |
| 3-4 times/wk | 13.8 | 22.9 | 20.3 | 11.5 | |
| 5-6 times/wk | 7.9 | 7.1 | 7.7 | 6.0 | |
| Once a day | 5.6 | 7.5 | 4.4 | 5.2 | |
| ≥2 times/d | 3.3 | 2.4 | 2.4 | 3.6 | |
| Neutral | |||||
| Eggs | |||||
| ≤ once/month | 17.0 | 10.4 | 16.2 | 24.6 | < 0.001 |
| 2-3 times/month | 14.4 | 17.7 | 22.4 | 22.6 | |
| 1-2 times/week | 25.1 | 28.4 | 30.6 | 28.2 | |
| 3-4 times/week | 19.6 | 25.1 | 17.9 | 15.1 | |
| 5-6 times/week | 10.8 | 9.4 | 7.9 | 4.4 | |
| Once a day | 11.5 | 8.4 | 3.8 | 4.8 | |
| ≥2 times/d | 1.6 | 0.6 | 1.2 | 0.4 | |
Bold values are statistically significant (P < .05).
P values from Pearson χ2 tests.
Table 6.
Sampling quotas, distribution of the final sample, and census demographic estimatesa
| Characteristic | Quota name | Field Target | Final Sample | 2019 ACSb |
|---|---|---|---|---|
| ←%→ | ||||
| Agec | 18 to 24 years old | 13 | – | 12 |
| 25 to 44 years old | 41 | – | 34 | |
| 45 to 64 years old | 30 | – | 33 | |
| Over 65 years old | 16 | – | 21 | |
| 18-29 years old | – | 25 | 21 | |
| 30-39 years old | – | 20 | 17 | |
| 40-49 years old | – | 14 | 16 | |
| 50-59 years old | – | 14 | 16 | |
| 60-69 years old | – | 18 | 15 | |
| 70-79 years old | – | 7 | 9 | |
| 80+ years old | – | 1 | 5 | |
| Sexd | Male | 50 | 48 | 49 |
| Female | 50 | 51 | 51 | |
| Ethnicity | Hispanic | 11 | 14 | 18 |
| Not Hispanic | 89 | 86 | 82 | |
| Race | Black | 12 | 12 | 13 |
| White | 70 | 72 | 72 | |
| Other race | 18 | 16 | 17 | |
| Region | Midwest | 22 | 22 | 21 |
| Northeast | 18 | 19 | 17 | |
| South | 37 | 37 | 38 | |
| West | 23 | 22 | 23 | |
| Household size | Household Size 1 and maximum annual household income $31,900 | 25 | 23 | 26 |
| Household Size 2 and maximum annual household income $43,100 | 32 | 30 | 33 | |
| Household Size 3 and maximum annual household income $54,300 | 18 | 20 | 17 | |
| Household Size 4 and maximum annual household income $65,500 | 16 | 16 | 14 | |
| Household Size 5 and maximum annual household income $76,700 | 6 | 7 | 7 | |
| Household Size 6 and maximum annual household income $87,900 | 2 | 4 | 3 | |
| Household Size 7 and maximum annual household income $110,000 | 1 | 2 | ||
This study used a census-matched panel of US adults aged 18 years or older (matched on age, sex, and race and ethnicity to the overall US population. The sample was limited to adults with annual household income <250% of the 2020 federal poverty level. This table shows the quotas used to recruit participants with CloudResearch (Quota), the actual sample recruited (Field Sample), in comparison to demographics of the US population based on the American Community Survey.
ACS = American Community Survey 2019 1-year estimates.
Age categories the study collected did not align completely with the target sampling age categories.
Gender identity was not included as a criteria for sampling (the census-matched panel was based on sex not gender) and is therefore not included as a point of comparison here.
References
- 1.Gundersen C., Ziliak J.P. Food insecurity and health outcomes. Health affairs (Project Hope) 2015;34(11):1830–1839. doi: 10.1377/hlthaff.2015.0645. [DOI] [PubMed] [Google Scholar]
- 2.Leung C.W., Epel E.S., Ritchie L.D., Crawford P.B., Laraia B.A. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet. 2014;114(12):1943–1953.e2. doi: 10.1016/j.jand.2014.06.353. [DOI] [PubMed] [Google Scholar]
- 3.Hanson K.L., Connor L.M. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr. 2014;100(2):684–692. doi: 10.3945/ajcn.114.084525. [DOI] [PubMed] [Google Scholar]
- 4.Larson N., Laska M.N., Neumark-Sztainer D. Food insecurity, diet quality, home food availability, and health risk behaviors among emerging adults: findings from the EAT 2010-2018 study. Am J Public Health. 2020;110(9):1422–1428. doi: 10.2105/ajph.2020.305783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagata J.M., Ganson K.T., Whittle H.J., et al. Food insufficiency and mental health in the U.S. during the COVID-19 pandemic. Am J Prev Med. 2021;60(4):453–461. doi: 10.1016/j.amepre.2020.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coleman-Jensen A., Rabbitt M.P., Gregory C., Singh A. Household food security in the United States in 2019. https://www.ers.usda.gov/publications/pub-details/?pubid=99281
- 7.Wolfson J.A., Leung C.W. Food insecurity and COVID-19: disparities in early effects for US adults. Nutrients. 2020;12(6):1648. doi: 10.3390/nu12061648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fitzpatrick K., Harris C., Drawve G. Assessing U.S. food insecurity in the United States during COVID-19 pandemic. https://fulbright.uark.edu/departments/sociology/research-centers/community-family-institute/_resources/community-and-family-institute/revised-assessing-food-insecurity-brief.pdf
- 9.Schanzenbach D., Pitts A. How much has food insecurity risen? Evidence from the Census Household Pulse Survey. 2020. https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-10-june-2020.pdf
- 10.Leddy A.M., Weiser S.D., Palar K., Seligman H. A conceptual model for understanding the rapid COVID-19-related increase in food insecurity and its impact on health and healthcare. Am J Clin Nutr. 2020;112(5):1162–1169. doi: 10.1093/ajcn/nqaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ziliak JP. Food hardship during the COVID-19 pandemic and great recession. Appl Econ Perspect Policy. October 2, 2020. [Epub ahead of print]. https://doi.org/10.1002/aepp.13099 [DOI] [PMC free article] [PubMed]
- 12.Coleman-Jensen A., Rabbitt M.P., Gregory C.A., Singh A. 2021. Household Food Security in the United States in 2020.https://www.ers.usda.gov/publications/pub-details/?pubid=102075 [Google Scholar]
- 13.Oaklander M. Our diets are changing because of the coronavirus pandemic. Is it for the better? https://time.com/5827315/coronavirus-diet/
- 14.Hagmann D., Siegrist M., Hartmann C. Acquisition of cooking skills and associations with healthy eating in Swiss adults. J Nutr Educ Behav. 2020;52(5):483–491. doi: 10.1016/j.jneb.2019.12.016. [DOI] [PubMed] [Google Scholar]
- 15.Mills S., White M., Brown H., et al. Health and social determinants and outcomes of home cooking: a systematic review of observational studies. Appetite. 2017;111:116–134. doi: 10.1016/j.appet.2016.12.022. [DOI] [PubMed] [Google Scholar]
- 16.Mills S., Brown H., Wrieden W., White M., Adams J. Frequency of eating home cooked meals and potential benefits for diet and health: cross-sectional analysis of a population-based cohort study. Int J Behav Nutr Phys Activity. 2017;14(1):109. doi: 10.1186/s12966-017-0567-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wolfson J.A., Bleich S.N. Is cooking at home associated with better diet quality or weight-loss intention? Public Health Nutr. 2015;18:1397–1406. doi: 10.1017/S1368980014001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wolfson J.A., Leung C.W., Richardson C.R. More frequent cooking at home is associated with higher Healthy Eating Index-2015 score. Public Health Nutr. 2020;23(13):2384–2394. doi: 10.1017/s1368980019003549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lamarche B., Brassard D., Lapointe A., et al. Changes in diet quality and food security among adults during the COVID-19-related early lockdown: results from NutriQuébec. Am J Clin Nutr. 2021;113(4):984–992. doi: 10.1093/ajcn/nqaa363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murphy B., Benson T., McCloat A., et al. Changes in consumers' food practices during the COVID-19 lockdown, implications for diet quality and the food system: a cross-continental comparison. Nutrients. 2020;13(1) doi: 10.3390/nu13010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robinson E., Boyland E., Chisholm A., et al. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. 2020;13(1):20. doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Batlle-Bayer L., Aldaco R., Bala A., et al. Environmental and nutritional impacts of dietary changes in Spain during the COVID-19 lockdown. Sci Total Environment. 2020;748:141410. doi: 10.1016/j.scitotenv.2020.141410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Litton M.M., Beavers A.W. The relationship between food security status and fruit and vegetable intake during the COVID-19 pandemic. Nutrients. 2021;13(3):712. doi: 10.3390/nu13030712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cummings J.R., Wolfson J.A., Gearhardt A.N. Health-promoting behaviors in the United States during the early stages of the COVID-19 pandemic. Appetite. 2022;168:105659. doi: 10.1016/j.appet.2021.105659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Organisation for economic co-operation and development food supply chains and COVID-19: impacts and policy lessons. https://www.oecd.org/coronavirus/policy-responses/food-supply-chains-and-covid-19-impacts-and-policy-lessons-71b57aea/
- 26.US Bureau of Labor Statistics Civilian unemployment rate. https://www.bls.gov/charts/employment-situation/civilian-unemployment-rate.htm
- 27.Qualtrics. Version June 2020. www.qualtrics.com
- 28.Lahne J., Wolfson J.A., Trubek A. Development of the Cooking and Food Provisioning Action Scale (CAFPAS): a new measurement tool for individual cooking practice. Food Qual Pref. 2017;62:96–105. doi: 10.1016/j.foodqual.2017.06.022. [DOI] [Google Scholar]
- 29.Gicevic S., Mou Y., Bromage S., Fung T.T., Willett W. Development of a diet quality screener for global use: evaluation in a sample of US women. J Acad Nutr Diet. 2021;121(5):854–871 e6. doi: 10.1016/j.jand.2020.12.024. [DOI] [PubMed] [Google Scholar]
- 30.Gicevic S., Tahirovic E., Bromage S., Willett W. Diet quality and all-cause mortality among U.S. adults, estimated from NHANES, 2003-2008. Public Health Nutr. 2021:1–25. doi: 10.1017/S1368980021000859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control National Health and Nutrition Examination Survey 2007-2008 data documentation, codebook, and frequencies. https://wwwn.cdc.gov/Nchs/Nhanes/2007-2008/CBQ_E.htm
- 32.Löwe B., Wahl I., Rose M., et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1-2):86–95. doi: 10.1016/j.jad.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 33.Polonsky W.H., Fisher L., Earles J., et al. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2005;28(3):626–631. doi: 10.2337/diacare.28.3.626. [DOI] [PubMed] [Google Scholar]
- 34.Litman L., Robinson J., Abberbock T. TurkPrime.com: a versatile crowdsourcing data acquisition platform for the behavioral sciences. Behav Res Methods. 2017;49(2):433–442. doi: 10.3758/s13428-016-0727-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chandler J., Rosenzweig C., Moss A.J., Robinson J., Litman L. Online panels in social science research: expanding sampling methods beyond Mechanical Turk. Behav Res Methods. 2019;51(5):2022–2038. doi: 10.3758/s13428-019-01273-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Office of the Assistant Secretary for Planning and Evaluation, US Department of Health and Human Services. 2020 Percentage Poverty Tool. https://aspe.hhs.gov/sites/default/files/migrated_legacy_files//194391/2020-percentage-poverty-tool.pdf
- 37.Fung T.T., Isanaka S., Hu F.B., Willett W.C. International food group-based diet quality and risk of coronary heart disease in men and women. Am J Clin Nutr. 2018;107(1):120–129. doi: 10.1093/ajcn/nqx015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gicevic S., Gaskins A.J., Fung T.T., et al. Evaluating pre-pregnancy dietary diversity vs. dietary quality scores as predictors of gestational diabetes and hypertensive disorders of pregnancy. PloS One. 2018;13(4) doi: 10.1371/journal.pone.0195103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bickel G.W. Guide to measuring household food security (revised 2000). May 19, 2022. https://fns-prod.azureedge.us/sites/default/files/FSGuide.pdf
- 40.US Dept of Agriculture, Economic Research Service Definition of food insecurity. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/measurement.aspx#
- 41.Stata Statistical Software. Release 15. StataCorp LLC; 2017. www.stata.com
- 42.Vandevijvere S., De Ridder K., Drieskens S., Charafeddine R., Berete F., Demarest S. Food insecurity and its association with changes in nutritional habits among adults during the COVID-19 confinement measures in Belgium. Public Health Nutr. 2021;24(5):950–956. doi: 10.1017/s1368980020005005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jia J., Fung V., Meigs J.B., Thorndike A.N. Food insecurity, dietary quality, and health care utilization in lower-income adults: a cross-sectional study. J Acad Nutr Diet. 2021;121(11):2177–2186 e3. doi: 10.1016/j.jand.2021.06.001. [DOI] [PubMed] [Google Scholar]
- 44.Berkowitz S.A., Basu S., Meigs J.B., Seligman H.K. Food insecurity and health care expenditures in the United States, 2011-2013. Health Serv Res. 2018;53(3):1600–1620. doi: 10.1111/1475-6773.12730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Berkowitz S.A., Gao X., Tucker K.L. Food-insecure dietary patterns are associated with poor longitudinal glycemic control in diabetes: results from the Boston Puerto Rican Health study. Diabetes Care. 2014;37(9):2587–2592. doi: 10.2337/dc14-0753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Berkowitz S.A., Seligman H.K., Choudhry N.K. Treat or eat: food insecurity, cost-related medication underuse, and unmet needs. Am J Med. 2014;127(4):303–310.e3. doi: 10.1016/j.amjmed.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 47.Seligman H.K., Jacobs E.A., López A., Tschann J., Fernandez A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35(2):233. doi: 10.2337/dc11-1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seligman H.K., Laraia B.A., Kushel M.B. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2009;140(2):304–310. doi: 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leung C.W., Wolfson J.A. Food insecurity among older adults: 10-year national trends and associations with diet quality. J Am Geriatr Soc. 2021;69(4):964–971. doi: 10.1111/jgs.16971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leung C.W., Wolfson J.A., Lahne J., Barry M.R., Kasper N., Cohen A.J. Associations between food security status and diet-related outcomes among students at a large, public midwestern university. J Nutr Diet. 2019;119(10):1623–1631. doi: 10.1016/j.jand.2019.06.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wright B.N., Tooze J.A., Bailey R.L., et al. Dietary quality and usual intake of underconsumed nutrients and related food groups differ by food security status for rural, midwestern food pantry clients. J Acad Nutr Diet. 2020;120(9):1457–1468. doi: 10.1016/j.jand.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rivera R.L., Zhang Y., Wang Q., et al. Diet quality and associations with food security among women eligible for Indiana Supplemental Nutrition Assistance Program-Education. J Nutr. 2020;150(8):2191–2198. doi: 10.1093/jn/nxaa171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang D.D., Leung C.W., Li Y., et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174(10):1587–1595. doi: 10.1001/jamainternmed.2014.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hartman TJ, Haardörfer R, Whitaker LL, et al. Dietary and behavioral factors associated with diet quality among low-income overweight and obese African American women. J Am Coll Nutr. 2015/09/03 2015;34(5):416-424. https://doi.org/10.1080/07315724.2014.982305 [DOI] [PubMed]
- 55.Wolfson J.A., Smith K.C., Frattaroli S., Bleich S.N. Public perceptions of cooking and the implications for cooking behaviour in the USA. Public Health Nutr. 2016;19(9):1606–1615. doi: 10.1017/s1368980015003778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wolfson J.A., Lahne J., Raj M., Insolera N., Lavelle F., Dean M. Food agency in the United States: associations with cooking behavior and dietary intake. Nutrients. 2020;12(3):877. doi: 10.3390/nu12030877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.US Dept of Agriculture, Economic Research Service Definition of food insecurity. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security/
- 58.Gupta N.R., Freedman D.A. Food security moderates relationship between perceived food environment and diet quality among adults in communities with low access to healthy food retail. Public Health Nutr. 2021;24(10):2975–2986. doi: 10.1017/s1368980020001317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Families First Coronavirus Response Act. https://www.dol.gov/agencies/whd/ffcra
- 60.Coronavirus Aid, Relief, and Economic Security (CARES) Act. 2020. https://www.congress.gov/bill/116th-congress/house-bill/748 [DOI] [PubMed]
- 61.Consolidated Appropriations Act. HR 133. 2021. https://www.congress.gov/bill/116th-congress/house-bill/133
- 62.Rosenbaum D. Boost SNAP to capitalize on program’s effectiveness and ability to respond to need. https://www.cbpp.org/research/food-assistance/boost-snap-to-capitalize-on-programs-effectiveness-and-ability-to-respond
- 63.Rivera R.L., Maulding M.K., Abbott A.R., Craig B.A., Eicher-Miller H.A. SNAP-Ed (Supplemental Nutrition Assistance Program-Education) increases long-term food security among Indiana households with children in a randomized controlled study. J Nutr. 2016;146(11):2375–2382. doi: 10.3945/jn.116.231373. [DOI] [PubMed] [Google Scholar]
- 64.Rivera R.L., Maulding M.K., Eicher-Miller H.A. Effect of Supplemental Nutrition Assistance Program–Education (SNAP-Ed) on food security and dietary outcomes. Nutr Rev. 2019;77(12):903–921. doi: 10.1093/nutrit/nuz013. [DOI] [PubMed] [Google Scholar]
- 65.Eicher-Miller H.A., Rivera R.L., Sun H., Zhang Y., Maulding M.K., Abbott A.R. Supplemental Nutrition Assistance Program-Education improves food security independent of food assistance and program characteristics. Nutrients. 2020;12(9):2636. doi: 10.3390/nu12092636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rivera R.L., Dunne J., Maulding M.K., et al. Exploring the association of urban or rural county status and environmental, nutrition- and lifestyle-related resources with the efficacy of SNAP-Ed (Supplemental Nutrition Assistance Program-Education) to improve food security. Public Health Nutrition. 2018;21(5):957–966. doi: 10.1017/s1368980017003391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Slagel N., Newman T., Sanville L., et al. A Pilot Fruit and Vegetable Prescription (FVRx) program improves local fruit and vegetable consumption, nutrition knowledge, and food purchasing practices. Health Promot Pract. 2021 doi: 10.1177/15248399211018169. [DOI] [PubMed] [Google Scholar]
- 68.Kaiser L., Chaidez V., Algert S., et al. Food resource management education with SNAP participation improves food security. J Nutr Educ Behav. 2015;47(4):374–378.e1. doi: 10.1016/j.jneb.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 69.Llobrera J. Modernizing SNAP benefits will help millions of families afford healthy, nutritious diet. https://www.cbpp.org/blog/modernizing-snap-benefits-will-help-millions-of-families-afford-healthy-nutritious-diet
- 70.Fowler F.J., Jr. Sage Publications; 2013. Survey Research Methods. [Google Scholar]
- 71.Beto J.A., Metallinos-Katsaras E., Leung C. Crowdsourcing: a critical reflection on this new frontier of participant recruiting in nutrition and dietetics research. J Acad Nutr Diet. 2020;120(2):193–196. doi: 10.1016/j.jand.2019.10.018. [DOI] [PubMed] [Google Scholar]
- 72.Wolfson JA, Bleich SN, Clegg Smith K, Frattaroli S. What does cooking mean to you?: Perceptions of cooking and factors related to cooking behavior. Appetite. 2016;97(February 2016):146-154. doi: 10.1016/j.appet.2015.11.030 [DOI] [PubMed]
- 73.Virudachalam S., Long J.A., Harhay M.O., Polsky D.E., Feudtner C. Prevalence and patterns of cooking dinner at home in the USA: National Health and Nutrition Examination Survey (NHANES) 2007–2008. Public Health Nutrition. 2014;17(5):1022–1030. doi: 10.1017/S1368980013002589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tiwari A., Aggarwal A., Tang W., Drewnowski A. Cooking at home: a strategy to comply with U.S. dietary guidelines at no extra cost. Am J Prev Med. 2017;52(5):616–624. doi: 10.1016/j.amepre.2017.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]