Background:
We transitioned our hand practice from the operating room (OR) to our office-based procedure room (OPR) to offer wide-awake, local anesthesia, no tourniquet (WALANT). We have established that using wide-awake virtual reality improves patient comfort and anxiety during wide-awake procedures and helps facilitate our patients’ choice of venue. We aimed to assess the effect of this transition on infection rates for procedures performed by a single surgeon in the OR versus the OPR.
Methods:
A retrospective chart review was performed on a single surgeon’s adult patients who underwent elective and closed traumatic upper limb surgeries. A surgical site infection was defined as superficial or deep, based on clinical examination conducted by the surgeon, and was treated with antibiotics within a 4-week postoperative window.
Results:
From August 2017 to August 2019, 538 (216 OR and 322 OPR) consecutive cases met inclusion criteria. There were six (2.78%) superficial infections and zero deep space infections in the OR cohort compared with four (1.24%) superficial and zero deep space infections in the OPR cohort with no statistical significance. Two-thirds of cases were converted to WALANT and delivered in the office.
Conclusions:
This narrative study concurs with the current literature that WALANT in the office setting is as safe as the hospital OR-based procedures for selected elective cases. By transitioning suitable cases from the OR to the OPR, a surgeon’s overall infection rate should not change.
Takeaways
Question: Does a hand surgeon’s overall infection rate change as they transition cases from the operating room to the clinic-based procedure room, performing the surgeries via the WALANT technique?
Findings: There is no statistically significant difference between a single surgeon’s infection rates when comparing all elective and closed trauma cases between the operating room and clinic-based procedure room.
Meaning: It is safe in regard to infection rates, to operate via WALANT in a clinic-based procedure room with the assistance of virtual reality for patient comfort.
INTRODUCTION
The engineering required to support sterile technique and general anesthesia first came together in the operating room in the early 20th century, creating the walled garden that enabled the golden age of surgical development to take place.1 This delivery model still dictates the location and method of surgical and anesthesia care while more surgeries than ever before are offered to an aging population of increasingly frail patients. The most routine smaller hand procedures are at the front line in the debate over whether we might be providing overly expensive, environmentally wasteful, and unproven levels of sterile services in addition to unnecessary exposure to anesthesia. (See figure, Supplemental Digital Content 1, which displays the main operating room triad. http://links.lww.com/PRSGO/C11.)
Patient morbidity will be reduced once central nervous anesthesia is truly found to be unnecessary for a large percentage of a hand practice. For example, it is observed that 12% of older patients undergoing a general anesthetic develop cognitive decline in the postoperative period, 40% of whom do not fully recover by 6 months.2 Wide-awake, local anesthesia, no tourniquet (WALANT) has also challenged long-held unproven medical dictums, such as the dangers of epinephrine in the hand, which have been shown to be errors dating back to over 90 years ago.3
WALANT has been gaining international traction over the last decade.4 A recent survey reported that 62% of United States hand surgeons now incorporate some degree of WALANT in their practice.5 Two common barriers to WALANT include the physician’s concern for infection under field sterility and a patient’s concern for the experience during awake surgery. Over the past 20 years, several studies have supported that simplified field sterility alone is suitable for many hand procedures.6–10 To address the patient experience whilst undergoing WALANT, we have applied the developing technology of wide-awake virtual reality.11 Procedures done in the office are also significantly less costly than those performed in the main operating room.12–14
With the original triad in mind, we refocused our hand surgical practice with a new triad utilizing virtual reality (VR) to encourage patient uptake of office-based surgery. (See figure, Supplemental Digital Content 2, which displays the office procedure room triad. http://links.lww.com/PRSGO/C12.)
During this period, we transitioned two-thirds of our suitable cases from the main operating room (OR) to the office-based procedure room (OPR). Prior studies at our institution have already demonstrated the utility of VR in reducing anxiety and pain while increasing patient enjoyment for awake patients undergoing office procedures.15
The objective of this study was to report our narrative of a transition of suitable surgical cases from the main OR to the office. The primary outcome measure was the comparative postoperative infection rates between the operating room and office-based procedure room.
METHODS
We performed a retrospective chart review of a single surgeon’s (senior author JHWC) elective upper limb cases from the OR and OPR. An institutional review board at both centers approved the review. Surgical site infections were identified via chart review by accessing both institutions’ electronic health records. Inclusion criteria encompassed all adults, 18 years or older, with upper limb surgeries at either center between August 2017 to August 2019. Patients were excluded from the study if there was failure to follow up or if the elective surgery took place shortly after an open trauma or recent infection, to eliminate the impact of contamination from the injury on this infection rate study. We define “full sterility” as that found in the main OR and “field sterility” as that which is used in the OPR.
Based on the CDC guidelines,16 a surgical site infection was defined as a surgical site that on clinical examination was deemed to be infected by the senior author, within 30 days of the procedure. This was categorized as any evidence of cellulitis, spreading erythema or presence of purulence. Simple suture abscesses were excluded unless there was evidence of spreading erythema. An infection was classified as a deep infection if it were noted to be tracking below the fascial layer.
The OR surgeries were performed following the hospital’s standard sterile protocol, including upper extremity and full body drapes in an accredited operating room. This location was able to make use of plates and screws not available in the OPR where internal fixation was restricted to k wires. The OPR is a single room that has been set up to perform WALANT surgeries and other minor procedures. A single medical assistant performs circulating and first assistant duties. Between surgeries in the OPR, the medical assistant washes the patient’s chair, surgical table, stools, counter, mayo stand, and VR headset. The VR headset has a silicone elastomer face shield, which facilitates cleaning.
Our OPR protocol has patients first enter an exam room where their vitals are taken, and the surgical site is anesthetized with tumescent local anesthesia described by Lalonde and Wong.17 If patients are needle phobic or anxious, they are offered the use of VR during injection. Patients wait for approximately 30 minutes for maximal effect, and during that time they scrub the surgical site with iodine or chlorhexidine themselves without maintaining sterility. Afterward they are moved to the procedure room where they remain in their street clothing. The patient is then positioned in a sitting or supine position and VR is offered. The limb is prepared with alcohol chlorhexidine (Chloraprep) and draped using sterile towels. The surgeon wears sterile gloves, gown, cap, and mask. We use an autoclave to process towels and instruments.
Descriptive statistics were used for summarizing the data. Pearson’s χ² and Fisher’s exact tests were conducted on categorical variables. A logistic regression was performed on variables pertaining to patient demographics. Patient demographics included sex, age, postoperative antibiotics, smoking status, use of immunosuppressive drugs, use of insulin and a history of diabetes, asthma, chronic obstructive pulmonary disease, cerebral vascular accident, coronary artery disease, hypertension, or chronic kidney disease. Patients were not matched between cohorts.
RESULTS
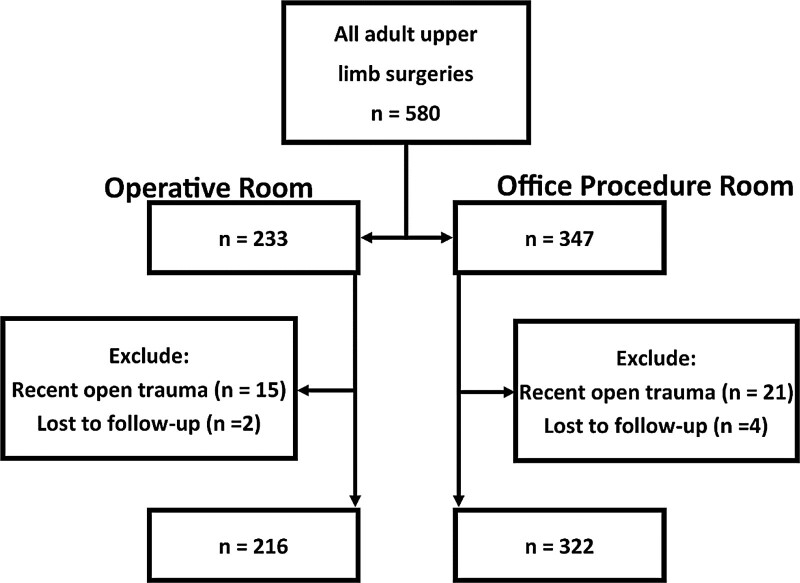
From August 2017 to August 2019, we identified 538 consecutive elective cases that met the inclusion criteria, with 216 cases in the OR and 322 cases in the OPR (Fig. 1). Of all patients receiving surgery over that period, two-thirds of them have converted to WALANT. The average age of the patients in the OPR cohort was greater, with a mean of 54.8 years old, versus the mean of 46.2 years old in the OR cohort. Along with increased age, Table 1 shows that the OPR cohort had a statistically significant increase in the prevalence of comorbid coronary artery disease, diabetes, hypertension, and chronic kidney disease.
Fig. 1.
Breakdown of patients meeting inclusion criteria.
Table 1.
Demographics of the Study Population
| Operating Room | Procedure Room | All Patients | P values | |
|---|---|---|---|---|
| Gender | ||||
| Women | 103 | 204 | 307 | 0.0003 |
| Men | 113 | 118 | 231 | |
| Smoking status | ||||
| Nonsmoker | 170 | 252 | 422 | 0.297 |
| Current smoker | 46 | 54 | 100 | |
| Comorbidities | ||||
| Asthma | 41 | 50 | 91 | 0.42 |
| COPD | 12 | 11 | 23 | 0.35 |
| Previous CVA | 4 | 10 | 14 | 0.476 |
| CAD | 2 | 21 | 23 | 0.005 |
| Diabetes | 24 | 78 | 102 | 0.001 |
| HTN | 64 | 145 | 209 | 0.001 |
| CKD | 2 | 15 | 17 | 0.046 |
| Average age | 46.2 | 54.8 | 51 | <0.0001 |
Bolded P values indicated significance. COPD, chronic obstructive pulmonary disease; CVA, cerebrovascular accident; CAD, coronary artery disease; HTN, hypertension; CKD, chronic kidney disease.
In total, there were six superficial infections and zero deep space infections in the OR cohort compared with four superficial and zero deep space infections in the OPR cohort. The overall infection rate was 1.86%, and infection rates of 2.78% and 1.24% were observed in the OR and OPR, respectively. The difference did not reach statistical significance with Fisher exact test (P = 0.211, Table 2), although it was noted that a higher rate of infection was observed in the main OR.
Table 2.
Infection Breakdown in Each Operative Environment
| Total Cases | Superficial Infection | Deep Infection | Total Infections | Infection Percent | P | |
|---|---|---|---|---|---|---|
| Operating Room | 216 | 6 | 0 | 6 | 2.78 | 0.211 |
| Procedure Room | 322 | 4 | 0 | 4 | 1.24 | |
| All Cases | 538 | 10 | 0 | 10 | 1.86 |
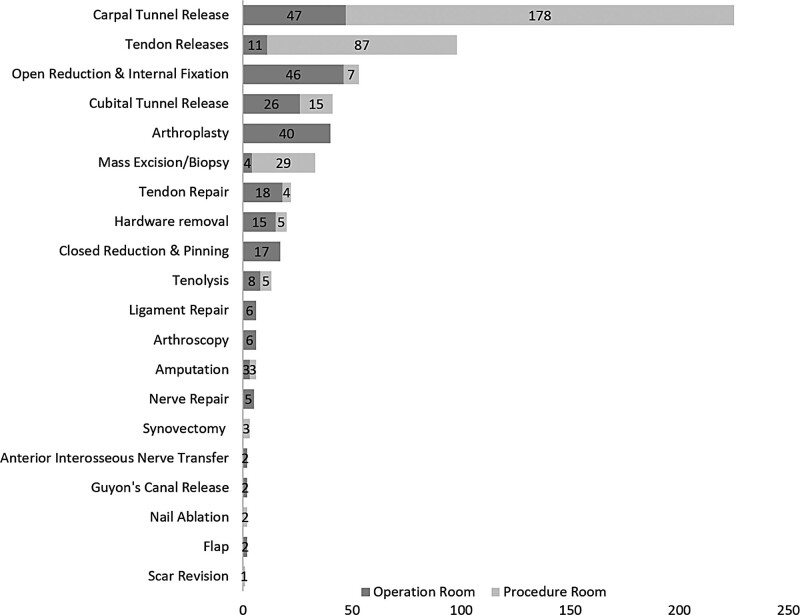
Figure 2 shows the breakdown of surgeries performed over the study period. There were 597 procedures performed on the 538 patients, with 81 of the patients having multiple procedures at the same time. A subanalysis of surgeries involving open carpal tunnel releases (CTRs) was done to further analyze infection rates. A total of 46 CTRs were performed in the OR compared with 178 CTR cases performed in the OPR. There were three incidences of infection in the OR cases (6.7% infection rate) compared with one identified infection in the OPR cases (0.56% infection rate), which was noted to be statistically significant (P = 0.028). However, it should be noted that all three of the patients in the OR underwent multiple procedures and most OPR CTRs were done as standalone procedures.
Fig. 2.
Breakdown of all procedures and the location they were performed. There were 597 total procedures in the 538 cases. Each trigger finger was counted as a separate procedure, and many nerve releases were also performed with other procedures.
DISCUSSION
The infection rate of 1.24% seen in our patients undergoing WALANT hand surgery falls in the reported observed range reported by others who operate in the OPR.7,10 Additionally, our overall average infection rate of 1.86% falls in the reported infection rate range of 1%–11% seen after CTR in the literature.18 When CTR cases were analyzed, they demonstrated even lower infection rates in the office, with an incidence of only 0.56%. This agrees with the multiple other studies that have shown no increase in infection rates when compared with the traditional OR9,19 despite the OPR population being older with more comorbidities.
Our patients undergoing surgeries in the OPR were poorer surgical candidates with an increased prevalence of diabetes (24% in OPR versus 11% in OR), hypertension (44% in OPR versus 30% in OR) and chronic kidney disease (5% in OPR versus 1% in OR). These risk factors have been shown to increase the incidence of surgical site infections following CTR.20 Our OPR patients were also older, which increases the risk of anesthesia-related complications.2,21,22
This is a narrative study comparing the transition period when cases were moving into the office from the main OR; therefore, we recognize that the two groups are not similar, which is a weakness to the study. Once the efficiencies and safety became apparent with office-based WALANT, more cases and procedures were offered in the clinic in accordance with the surgeon’s comfort level. The more complex cases were less likely to transition to the office environment, which is seen in Figure 2. Reasons to retain more complex cases in the main OR were varied, including the need for sophisticated or expensive equipment and implants in addition to the location that the patient was encountered such as the emergency room of the hospital with urgent need for surgery. This comparison demonstrates the current real world constraints of implementing WALANT in an office-based setting.
Although the implication of this study might encourage surgeons to migrate all their hand surgery to the office environment, our study does not include permanent indwelling implants in the office setting. In this study, open reduction and internal fixation were performed in the OPR using buried K wires. The main OR was the setting when an open approach was need using plates and screws. In the face of limited evidence for the benefits of enhanced sterility, we still advocate that where the consequence of deep space infection around an implant would be devastating, it is still common sense to make use of main OR sterility until more data are present.
The use of VR has been well documented during anxiety provoking or painful procedures other than hand surgery. This includes burn dressing changes, dental procedures, and inpatient invasive procedures.23–27 We have previously demonstrated that wide-awake virtual reality reduces anxiety, pain, and increases fun for patients.15 The same study demonstrated the safety of VR use during WALANT procedures.
Many of our patients who were at first hesitant to be alert during the procedure were put at ease when offered the ability to focus their attention elsewhere using VR. In answer to their request “just put me out doc,” we were able to offer to “put them somewhere else” while alert and cooperative during the procedure. Increasing appeal with wide-awake virtual reality allowed the practice to better recruit patients to undergo WALANT. We are currently looking for ways to trial this hypothesis.
The practice of medicine is replete with ritualistic behaviors, which serve other motives in addition to any practical effects.28 Indeed cleansing rituals have been depicted as an example of a “Macbeth effect,” serving both moral and practical purposes.29 As physicians we need to be cognizant of the possibility that behind our behaviors may lie the bones of a more ancient cultural meme that serves to drive these behaviors beyond their practical application. For example, these memes may even predispose us to accept unnecessary regulatory or industrial complexity. To enable this insight, it is helpful to look at the original facts that lie behind them. For hand surgery, we may examine the origins of sterile technique. William Arbuthnot Lane (1856–1943), amongst many things, is acknowledged as Harold Gillies’ greatest political sponsor in the First World War. He was also the first surgeon to introduce the plating of orthopedic fractures. He refined and further engineered the 19th-century work of Lister and Semmelweis with his “no touch technique” and by introducing dry steam sterilization at Guy’s Hospital in London, England, around 1904, after reading of the technology from the Berlin surgeon, Ernst von Bergmann. This involved no more sterile engineering than a “pig” steam sterilizer between the operating rooms, dry sterile towel, sterile instruments, gowns, and gloves. This is closer to our OPR “field sterility” model than the elaborate sterility precautions encountered in a modern 21st-century operating room, and yet it permitted him to commence the first plating of closed orthopedic fractures with close to zero reported infections.1 Although to cut down on a closed fracture was surgical heresy at that time, 120 years of history have proven him right. These are the original facts and yet, over the same period, sterile protocol has become increasingly complex and regulated, increasing the costs associated with hospital and surgery center services despite little evidence that more sterility is better.
Following the current trend toward office-based surgery, hand surgeons and health care systems who primarily operate in the OR can feel comfortable when considering transitioning suitable cases out of the operating room. The evidence from this narrative study suggests that a surgeon should not see their overall infection rate increase when they begin transitioning their practice to the office-based procedure room for smaller cases.
The office-based WALANT literature is rapidly increasing, demonstrating that the technique is a comparable surgical option when compared with the traditional ways of performing hand surgery, such as using a tourniquet, intravenous regional anesthesia, and general anesthesia. Have we “ritualized” sterile technique beyond its practical effects? In Lane’s own words: “If everyone believes a thing, it is probably untrue.”30,31
Supplementary Material
Footnotes
Published online 13 May 2022.
Presented as a poster at the ASSH Annual Meeting, San Antonio, Tex., October 1, 2020.
Disclosure: Dr. Clarkson is the Chief Medical Officer for a Virtual Reality Company “Wide Awake VR”. No funding was received for this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Layton TB. Sir William Arbuthnot Lane, Bt., C.B., M.S. An enquiry into the mind and influence of a surgeon. Proc R Soc Med. 1956;49:959. [Google Scholar]
- 2.Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367:30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomson CJ, Lalonde DH, Denkler KA, et al. A critical look at the evidence for and against elective epinephrine use in the finger. Plast Reconstr Surg. 2007;119:260–266. [DOI] [PubMed] [Google Scholar]
- 4.Lalonde DH. Latest advances in wide awake hand surgery. Hand Clin. 2019;35:1–6. [DOI] [PubMed] [Google Scholar]
- 5.Grandizio LC, Graham J, Klena JC. Current trends in WALANT surgery: a survey of American Society for Surgery of the Hand Members. J Hand Surg Glob Online. 2020;2:186–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu J, Ji TA, Craig M, et al. Evidence-based sterility: the evolving role of field sterility in skin and minor hand surgery. Plast Reconstr Surg Glob Open. 2019;7:e2481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hashemi K, Blakeley CJ. Wound infections in day-case hand surgery: a prospective study. Ann R Coll Surg Engl. 2004;86:449–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jagodzinski NA, Ibish S, Furniss D. Surgical site infection after hand surgery outside the operating theatre: a systematic review. J Hand Surg Eur Vol. 2017;42:289–294. [DOI] [PubMed] [Google Scholar]
- 9.Halvorson AJ, Sechriest VF, II, Gravely A, et al. Risk of surgical site infection after carpal tunnel release performed in an operating room versus a clinic-based procedure room within a veterans affairs medical center. Am J Infect Control. 2020;48:173–177. [DOI] [PubMed] [Google Scholar]
- 10.Leblanc MR, Lalonde DH, Thoma A, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand (N Y). 2011;6:60–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wide Awake Virtual Reality (WAVR). The surgical experience re-imagined. Available at https://wideawakevr.com/. Accessed March 15, 2021.
- 12.Leblanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in Canada. Hand (N Y). 2007;2:173–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rhee PC, Fischer MM, Rhee LS, et al. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: a critical analysis of the first 100 procedures. J Hand Surg Am. 2017;42:e139–e147. [DOI] [PubMed] [Google Scholar]
- 14.Tang JB, Xing SG, Ayhan E, Hediger S, Huang S. Impact of wide-awake local anesthesia no tour niquet on departmental settings, cost, patient and surgeon satisfaction, and beyond. Hand Clin. 2019;35:29–34. [DOI] [PubMed] [Google Scholar]
- 15.Hoxhallari E, Behr IJ, Bradshaw JS, et al. Virtual reality improves the patient experience during wide-awake local anesthesia no tourniquet hand surgery: a single-blind, randomized, prospective study. Plast Reconstr Surg. 2019;144:408–414. [DOI] [PubMed] [Google Scholar]
- 16.National Healthcare Safety Network (NHSN). Surgical site infection event (SSI). Washington, D.C.: Centres for Disese Control and Prevention. 2021;1–39. [Google Scholar]
- 17.Lalonde DH, Wong A. Dosage of local anesthesia in wide awake hand surgery. J Hand Surg Am. 2013;38:2025–2028. [DOI] [PubMed] [Google Scholar]
- 18.Eberlin KR, Ring D. Infection after hand surgery. Hand Clin. 2015;31:355–360. [DOI] [PubMed] [Google Scholar]
- 19.Garon MT, Massey P, Chen A, et al. Cost and complications of percutaneous fixation of hand fractures in a procedure room versus the operating room. Hand (N Y). 2018;13:428–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Werner BC, Teran VA, Deal DN. Patient-related risk factors for infection following open carpal tunnel release: an analysis of over 450,000 medicare patients. J Hand Surg Am. 2018;43:214–219. [DOI] [PubMed] [Google Scholar]
- 21.Aitkenhead AR. Injuries associated with anaesthesia. a global perspective. Br J Anaesth. 2005;95:95–109. [DOI] [PubMed] [Google Scholar]
- 22.Liu LL, Leung JM. Predicting adverse postoperative outcomes in patients aged 80 years or older. J Am Geriatr Soc. 2000;48:405–412. [DOI] [PubMed] [Google Scholar]
- 23.Walker MR, Kallingal GJ, Musser JE, et al. Treatment efficacy of virtual reality distraction in the reduction of pain and anxiety during cystoscopy. Mil Med. 2014;179:891–896. [DOI] [PubMed] [Google Scholar]
- 24.Mosadeghi S, Reid MW, Martinez B, et al. Feasibility of an immersive virtual reality intervention for hospitalized patients: an observational cohort study. JMIR Ment Health. 2016;3:e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morris LD, Louw QA, Grimmer-Somers K. The effectiveness of virtual reality on reducing pain and anxiety in burn injury patients: a systematic review. Clin J Pain. 2009;25:815–826. [DOI] [PubMed] [Google Scholar]
- 26.Furman E, Jasinevicius TR, Bissada NF, et al. Virtual reality distraction for pain control during periodontal scaling and root planing procedures. J Am Dent Assoc. 2009;140:1508–1516. [DOI] [PubMed] [Google Scholar]
- 27.van Twillert B, Bremer M, Faber AW. Computer-generated virtual reality to control pain and anxiety in pediatric and adult burn patients during wound dressing changes. J Burn Care Res. 2007;28:694–702. [DOI] [PubMed] [Google Scholar]
- 28.Arnold MH, Komesaroff P, Kerridge I. Understanding the ethical implications of the rituals of medicine. Intern Med J. 2020;50:1123–1131. [DOI] [PubMed] [Google Scholar]
- 29.Zhong CB, Liljenquist K. Washing away your sins: threatened morality and physical cleansing. Science. 2006;313:1451–1452. [DOI] [PubMed] [Google Scholar]
- 30.Clarkson JHW, Kirkpatrick JJ, Lawrie R. Prevention by organization: the story of no. 4 maxillofacial surgical unit in North Africa and Italy during the Second World War. Plast Reconstr Surg. 2008;121:657–668. [DOI] [PubMed] [Google Scholar]
- 31.Tanner WE. Sir W. Arbuthnot Lane. His Life and Work. London: Bailliere, Tindall and Cox; 1946. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.