Background:
Positional plagiocephaly has garnered increased research interest since the introduction of the Back to Sleep campaign in the 1990s, and the subsequent increase in infants with cranial deformity. Research has focused on treatment outcomes and developing new modalities to address asymmetric heads. Little attention has been given to the cost of treatment and diagnosis. This study aimed to summarize the literature and provide an overview of the costs associated with a diagnosis of positional plagiocephaly.
Methods:
A literature review was performed by searching PubMed and Ovid Embase to identify studies pertaining to the “cost” of plagiocephaly diagnosis or treatment through direct financial factors, disturbance to daily routines (ie, through treatment prolongation), or related stress.
Results:
Twenty-nine peer-reviewed studies were included. Treatment options for plagiocephaly are stratified by severity and age of diagnosis, with different pathways available to treat different stages of asymmetry. The common factor across all treatment modalities is that earlier diagnosis unequivocally leads to better aesthetic outcomes and shorter treatment times. This leads to lower costs for treatment, a lower stress burden for parents, and lower costs for the healthcare system in the future through reduction of long-term effects. Our theoretical cost model suggests that early diagnosis at 4 months can lead to a treatment cost of $1495, when compared with $5195 for detection of deformity at or after 6 months.
Conclusion:
The dramatic cost disparity between early and late diagnosis highlights the need for reliable methods to accurately detect cranial deformity early in an infant’s life.
Takeaways
Question: What is the cost burden of a positional plagiocephaly diagnosis in infants, and can it be lowered through earlier diagnosis?
Findings: We conducted a literature review of studies pertaining to the cost of a plagiocephaly diagnosis and subsequent treatment. Significant evidence was found to suggest that earlier diagnosis lowered the financial cost of treatment, decreased the emotional and logistical burden on parents, and improved clinical outcomes.
Meaning: Developing new tools to support earlier diagnosis of positional plagiocephaly in infants would allow us to reduce the cost of the diagnosis and the burden placed on parents and the healthcare system.
INTRODUCTION
It is well established that humans have an aesthetic preference for symmetry.1 Unsurprisingly then, parents express concern over perceived asymmetry in their children’s heads. Unfortunately, the incidence of such asymmetries has been on the rise since the 1990s. Following the introduction of the Back to Sleep campaign, designed to combat sudden infant death syndrome, the prevalence of positional plagiocephaly in infants has risen to above 40%.2–4 Caused primarily by prolonged external force to the developing skull, positional plagiocephaly is characterized by visible cranial deformity and associated facial asymmetry.5 Cranial shape can be affected along a spectrum of locations and severities; in the case of the Back to Sleep campaign, infants spend too much time in the supine position, leading to occipital flattening and frontal bossing.6,7 Mild plagiocephaly will typically present as a slight occipital flattening, while moderate and severe deformities progressively lead to more pronounced occipital flattening (localized to one side or bioccipitaly), the addition of frontal bossing, and ipsilateral ear shift as the head takes on a more “parallelogram” like shape. Additional risk factors for positional plagiocephaly include prolonged/frequent time in swings or car seats, delayed motor development, and obesity; asymmetric cranial molding can also occur in utero or during birth.8–12
Independent pathologies may accelerate the development of positional preferences and resultant plagiocephaly; one study reported torticollis as a clinical finding in more than 90% of infants diagnosed with positional plagiocephaly.13 Despite the primary concern with positional plagiocephaly being aesthetic, there are concerns for long-term effects when the condition is left untreated. These include orthodontic problems in permanent dentition, visual field restriction, jaw asymmetry, muscular problems, and stigma later in life.11,14 Positional plagiocephaly is not traditionally thought to affect cognitive development, though studies have shown that it can be associated with decreased cognitive and academic measures as severity increases.15
Infantile screening for cranial deformity is a standard part of well-baby check-ups to ensure healthy development. In many cases, no intervention is needed to correct the deformity; as infants gain control of head movement, cranial shape often normalizes.16–18 The clinical treatment pathways to manage plagiocephaly are the source of considerable debate, but the value of early diagnosis in managing the condition is well accepted. Cranial sutures start to fuse at 6 months of age, and initiation of treatment before this milestone is crucial to obtaining good clinical outcomes.19 Despite acceptance of early diagnosis as an important clinical goal, little research has been done to evaluate the cost benefit of an early plagiocephaly diagnosis. This review aimed to summarize the evidence for a reduced cost burden when positional plagiocephaly is diagnosed and treated earlier in life.
METHODS
A literature review was performed by searching PubMed and Ovid Embase for relevant studies using the search terms “plagiocephaly” AND (“treatment” OR “diagnosis” OR “cost”). Article titles and abstracts were reviewed to ensure they provided information pertaining to the “cost” of plagiocephaly diagnosis or treatment through direct financial factors, disturbance to daily routines (ie, through treatment prolongation), or related stress. Additional articles were screened from cited references. Only English language articles were included.
RESULTS
The search returned 636 results. Following individual title and abstract review, 29 articles were included in the review and analyzed for relevant content. Collected data were synthesized into dominant themes to present a comprehensive review of the literature and to compile evidence on the benefits of earlier diagnosis in plagiocephaly patients.
CLINICAL MANAGEMENT
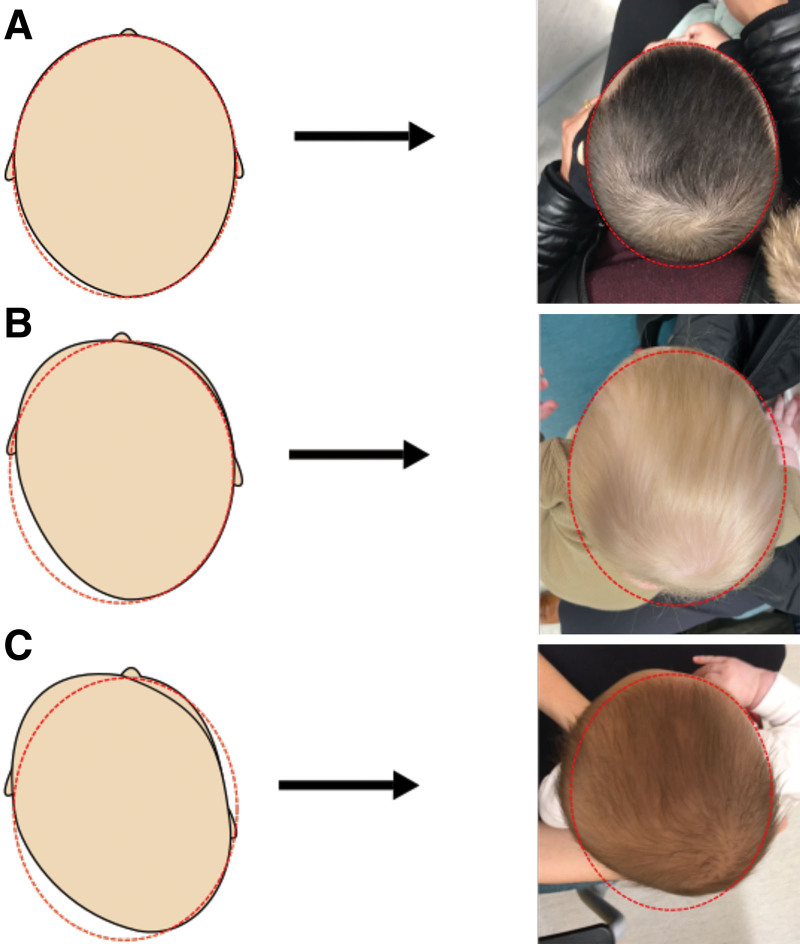
Clinical management of cranial deformity is typically stratified by severity, with multiple modalities available to treat varying degrees of plagiocephaly. Treatment strategies are further broken down into passive (repositioning) and active (physiotherapy, cranial remolding therapy, and surgery) modalities. Upon initial observation of asymmetry or deformity by the parents or the pediatrician, the first-line treatment plan is simple repositioning and an increase in tummy time for the infant to decrease pressure on the affected side of the skull.11,20,21 As plagiocephaly is often accompanied by congenital muscular torticollis, physical therapy is also indicated, with a focus on supporting musculoskeletal development and manipulating tissue to relieve strains causing cranial deformity.11,22,23 Surgery for release of muscular torticollis is occasionally indicated for cases resistant to physical therapy, and generally only after 12 months of age. From the age of 4–6 months, treatment is guided by severity. Infants affected by mild-to-moderate plagiocephaly (Fig. 1A, B) will be treated with repositioning and/or physical therapy, whereas infants showing severe positional plagiocephaly (Fig. 1C) will often be referred to an orthotic specialist or a craniofacial team to initiate helmet therapy.5,11,24 Although its use is not universally accepted in the literature, helmet therapy has been shown to correct asymmetry more efficiently than repositioning alone.10 By the age of 6 months, children with persistent, significant plagiocephaly that did not respond to conservative treatments are frequently sent for helmet therapy, as well as moderate-to-severe cases that present late (at or after 6 months).5,11,25 Later initiation of helmet therapy treatment generally decreases the improvement in cranial symmetry. Although helmet therapy can have some beneficial effects even at advanced ages (eg, after 10 months), substantial decreases in cranium and cranial suture plasticity, as well as the decreased rate of brain growth after 12 months of age, lead to much poorer treatment outcomes than in those who initiate treatment early.5,26,27
Fig. 1.
Occipital flattening, frontal bossing, and ipsilateral ear shift are the hallmark manifestations of deformational plagiocephaly, becoming more pronounced as severity increases. Clinically, this progression is divisible into mild (A), moderate (B) and severe (C) plagiocephaly.
TREATMENT BURDEN
Cohort data for repositioning therapy recommend that infants get at least 10–15 minutes of supervised tummy time three times per day.28 As the definite first-line treatment for cranial deformity, repositioning has the potential to significantly improve head shape without resorting to active treatment.11,20,21 Repositioning redistributes the repetitive forces that may be applied to an infant’s head while they sleep to encourage natural correction of the asymmetry. Repositioning can be prescribed by pediatricians and family physicians while requiring minimal effort on behalf of the infant’s caretakers. It is preferable to “watchful waiting” and does not require additional specialist follow-up, which can be inconvenient and costly to the family.29
Physical therapy treatment approaches to plagiocephaly are still heavily debated. Although its effectiveness at correcting cranial deformity is well documented, there is a lack of consensus for a singular effective treatment.30 One study by Di Chiara et al saw success with a standardized regimen of 16 weekly 40-minute physical therapy sessions.22 With the US national cost of physical therapy averaging to $75, Di Chiara’s standardized treatment plan would entail a cost of approximately $1200, of which a variable amount may be covered depending on the type of insurance coverage a family has. Thus, the out-of-pocket cost borne by patients and their families can vary widely.31
The American Association of Physical Therapy recommends that patients fitted with cranial orthoses receive follow-up 1 week after fitting and every 2 weeks thereafter.32 Certain orthotics, such as the DOC Band, require adjustment every week.33 Usually ranging from $1500 to $3000, the cost of the cranial orthotic typically includes the helmet and required follow-ups for helmet adjustments. Most cranial orthotics “grow” with the infant, thanks to progressive and planned removal of the foam lining the orthotic.34 However, significant cranial growth can necessitate the need for a second, and sometimes third, orthotic.35 As with physical therapy, insurance coverage for helmet therapy is variable; the true cost of treatment will need to be assessed on a case-by-case basis.11 In the United States, caregivers for affected infants had to cover costs themselves in 45.1% of cases. Of those that could submit the costs of helmet therapy to health insurance, 36.1% reported conflicts with the health insurance company regarding the refund of costs.36 Third party insurance companies often refuse to cover treatment for positional plagiocephaly, arguing that the deformity is purely cosmetic and that active treatments (like helmet therapy) are not substantially better than parental repositioning.11,37 One study by Lam et al analyzed the degree of treatment compliance according to patient subgroups and found that families with public insurance were less likely to adhere to the recommended treatment than families with private insurance (80.2% versus 89.6%).38 The authors do not discuss the cause, but one possibility is a lack of coverage for required follow-ups. The consensus is that coverage for low-income Americans is insufficient to support multivisit treatment plans, which considerably affects treatment accessibility and can lead to the development of more severe deformities in low-income households.31 This phenomenon has previously been well documented for medication nonadherence in low-income uninsured patients with chronic conditions.39 Furthermore, Junn et al recently reported that patients on Medicaid were 1.30 times more likely to have delayed presentation for helmet therapy consultation than those with commercial insurance, whereas patients in the highest and second highest income quartiles were respectively 1.55 and 1.45 times more likely to receive helmet therapy following consultation.40 These findings further highlight the clear diagnosis and treatment discrepancies found in different socioeconomic strata.
EMOTIONAL TOLL
Initial detection of cranial deformity is usually noted in the third or fourth month of life by the child’s parents or pediatrician. A conclusive diagnosis can be expected to be made within a month of the initial detection, with rapid initiation of preclinical passive treatment measures (ie, repositioning). Initial presentation of infants with a cranial deformity to craniofacial specialists is not until almost six months of age (average 5.8 month), with an average delay of 3.33 months between the initial recognition of deformity and first specialist presentation.41 Kluba et al suggest that this places increased pressure on parents to make an immediate decision, as the outcomes of treatment modalities such as helmet therapy are heavily reliant on early initiation of a treatment regimen.41 Personal strain on caregivers is rarely considered in the literature, but represents an important component of the burden of diagnosis. Increased caregiver stress levels can play a significant role in the degree of treatment compliance (and thereby treatment efficacy). A distinct study by Kluba et al evaluated factors related to poor treatment compliance.36 They discovered that more than 80% of parents had been affected by treatment related issues; the most commonly cited were financial cost, disputes with health insurance, concern for the child, time spent bringing the child to and from the clinic, and social conflicts.36 Martiniuk et al reported that in their survey, parents of a child with moderate-to-severe plagiocephaly expressed sadness that they had not addressed the flat head sooner and felt sorry for their child when they were forced to wear an orthotic helmet around the clock; typical regimens require the child to wear the helmet 23 hours a day, every day, for months at a time.42,43 Importantly, helmet therapy has been shown to not affect infant quality of life.42 Discrepant and unclear clinical pathways for plagiocephaly form an additional source of parental emotional burden. As physicians are not in agreement on the most appropriate treatment paths for cranial deformity, parents can be confused by potentially contradicting information.
THE BENEFIT OF EARLY DIAGNOSIS
The true cost of a diagnosis is measured by a combination of financial factors, disturbance to daily routines, and related stress. Prolonged treatments cause greater upset in the lives of patients’ families as they continue to bear the burden of care. As the numbers of plagiocephaly patients rise, it becomes ever more important to optimize the treatment pathway for these patients.5 Table 1 illustrates the theoretical financial and clinical outcome disparity between early diagnosis with successful physical therapy treatment and late diagnosis with unsuccessful physical therapy requiring subsequent conversion to helmet therapy.22,35,44,45
Table 1.
Cost Model of Early versus Late Diagnosis of Positional Plagiocephaly
| Age (Mo) | 4 | 4.5 | 6 | 6.5 | 7 | 8 | 15 | Final Cost |
|---|---|---|---|---|---|---|---|---|
| Early diagnosis | Confirmation of moderate plagiocephaly by pediatrician at well-baby visit, initiation of repositioning | Initiation of physical therapy (16 weekly sessions of 40 min) | Physical therapy is improving cranial deformity | — | Craniofacial specialist confirms plagiocephaly, physical therapy is improving cranial deformity | Physical therapy treatment completed with acceptable correction of deformity | — | — |
| Cost | $95 | $1200 | — | — | $200 | — | — | $1495 |
| Late diagnosis | — | — | Confirmation of moderate plagiocephaly by pediatrician at well baby visit, initiation of repositioning | Initiation of physical therapy (12 weekly sessions of 40 min) | Craniofacial specialist confirms plagiocephaly, physical therapy is unsuccessful, recommends helmet therapy | Helmet therapy initiated; average treatment requires 2 helmets | Conclusion of helmet therapy, <20% chance for complete correction of deformity | — |
| Cost | — | — | $95 | $900 | $200 | $2000 × 2 helmets | — | $5195 |
Research into effective physical therapy programs is crucial to the optimization of multidisciplinary treatment. The literature shows that age and degree of severity are essential factors in determining treatment duration and outcomes for patients diagnosed with plagiocephaly. Di Chiara et al reported that their physical therapy program led to positive improvements in 58.3% of the population for the Cranial Proportional Index/Cephalic Ratio and 70.8% for the cranial vault asymmetry index (CVAI), with the highest rate of improvement found in infants under the age of 8 months.22 Specifically, they noted that almost all reference measurements were most improved in infants aged 5–8 months, with no significant difference in treatment efficacy between infants aged 1–4 months and 5–8 months.22 Van Vlimmeren et al’s randomized control trial returned similar results; the occurrence of severe deformational plagiocephaly in infants that underwent physical therapy was reduced by 46% and 57% at 6 and 12 months of age, respectively.28
Physical therapy plays a further role supplementing less conservative techniques. In a study by Steinberg et al, complete correction of cranial deformity was achieved in 77.1% of conservative treatment patients (repositioning ± physical therapy); 15.8% required transition to helmet therapy, and 7.1% ultimately had incomplete correction.45 Furthermore, complete correction was achieved in 94.4% of patients treated with helmet therapy as first-line therapy and in 96.1% of infants who received helmets after failed conservative therapy.45 The authors found that the risk of failure for both conservative and helmet molding therapies increased with age; the younger than 3 month, 3–6 month, 6–9 month, and older than 12 month age categories demonstrated progressively increasing failure rates.45 Conservative therapy was two times more likely to fail at older than 12 months when compared with younger than 3 months, and helmet therapy was greater than three times more likely to fail with the same age groups.45
Several studies have made recommendations for an ideal helmet therapy start date for plagiocephaly patients. Han et al found that initiation of helmet molding therapy between the ages of 3–5 months yielded consistent results, but that initiation beyond 6 months led to significantly decreased rates of CVAI improvement and significant increases in duration of therapy.44 Han et al further demonstrated that starting helmet therapy at 3 months could as much as halve treatment times compared with their 8-month-old initiation group.44 In a study by Hinken et al, the average CVAI improvement with helmet therapy decreased by 36% between the 4–6 month group and the 7–9 month group.26 Graham et al concurred reporting that both treatment duration and treatment outcomes were improved by earlier initiation of cranial molding therapy.46 Finally, Kluba et al’s study resulted in infants less than 6 months old having 4 week shorter helmet therapy treatment time and greater reduction of asymmetry than those in the more than 6 months group.47 Furthermore, the average infant in the more than 6 month group was not able to achieve normal values for CVAI, which were attained by the younger group.47 Importantly, decreased effectiveness does not invalidate the commencement of therapy at an advanced age. Several studies have shown that although failure rates are higher and treatment duration increases, therapy can still have a positive effect on head shape.26,27
In addition to early diagnosis, a high degree of treatment compliance is essential to obtaining positive clinical outcomes. For infants undergoing orthotic helmet therapy, this can mean wearing the helmet up to 23 hours per day, while patients prescribed active repositioning depend on a high degree of treatment compliance for parents following standard instructions.48 Physiotherapy also typically requires multiple visits, requiring commitment from the parents to bring their children to and from appointments.22
CONCLUSIONS
Early identification of positional plagiocephaly plays an important role in lowering the monetary and intangible costs of the diagnosis. Earlier diagnosis has been proven to lead to better outcomes and reduced treatment times, as well as an increased likelihood of compliance with the treatment regimen. Furthermore, the intangible implications of prolonged treatment time due to delayed diagnosis significantly increases the burden on parents, through an increased number of specialist visits, increased likelihood of helmeting, and prolonged emotional strain from caring for the child. The resultant financial and resource burden placed on caregivers and/or the healthcare system is demonstrated in our modeled early versus late diagnosis treatment pathways. In the future, research should be directed at accessible tools that may facilitate early diagnosis of plagiocephaly across all socioeconomic demographics to mitigate the avoidable consequences of late detection.
Footnotes
Published online 16 May 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Huang Y, Xue X, Spelke E, et al. The aesthetic preference for symmetry dissociates from early-emerging attention to symmetry. Sci Rep. 2018;8:6263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collett B, Breiger D, King D, et al. Neurodevelopmental implications of “deformational” plagiocephaly. J Dev Behav Pediatr. 2005;26:379–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sidebotham P, Bates F, Ellis C, Lyus L. Preventive strategies for sudden infant death syndrome. In: Duncan JR, Byard RW, eds. SIDS Sudden Infant and Early Childhood Death: The Past, the Present and the Future. South Australia: University of Adelaide Press; 2018. [PubMed] [Google Scholar]
- 4.Di Rocco F, Ble V, Beuriat PA, et al. Prevalence and severity of positional plagiocephaly in children and adolescents. Acta Neurochir (Wien). 2019;161:1095–1098. [DOI] [PubMed] [Google Scholar]
- 5.Jung BK, Yun IS. Diagnosis and treatment of positional plagiocephaly. Arch Craniofac Surg. 2020;21:80–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Vlimmeren LA, van der Graaf Y, Boere-Boonekamp MM, et al. Risk factors for deformational plagiocephaly at birth and at 7 weeks of age: a prospective cohort study. Pediatrics. 2007;119:e408–e418. [DOI] [PubMed] [Google Scholar]
- 7.Feijen M, Franssen B, Vincken N, et al. Prevalence and consequences of positional plagiocephaly and brachycephaly. J Craniofac Surg. 2015;26:e770–e773. [DOI] [PubMed] [Google Scholar]
- 8.Mawji A, Vollman AR, Fung T, et al. Risk factors for positional plagiocephaly and appropriate time frames for prevention messaging. Paediatr Child Health. 2014;19:423–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Littlefield T, Kelly K, Reiff J, et al. Car seats, infant carriers, and swings: their role in deformational plagiocephaly. J Prosthet Orthot. 2003;15:102–106. [Google Scholar]
- 10.Paquereau J. Non-surgical management of posterior positional plagiocephaly: orthotics versus repositioning. Ann Phys Rehabil Med. 2013;56:231–249. [DOI] [PubMed] [Google Scholar]
- 11.Shenandoah R, Mark P. Diagnosis and management of deformational plagiocephaly. J Neurosurg Pediatrics PED. 2009;3:284–295. [DOI] [PubMed] [Google Scholar]
- 12.Kim EH, Kim KE, Jeon J, et al. Delayed motor development and infant obesity as risk factors for severe deformational plagiocephaly: a matched case-control study. Front Pediatr. 2020;8:582360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rogers GF, Oh AK, Mulliken JB. The role of congenital muscular torticollis in the development of deformational plagiocephaly. Plast Reconstr Surg. 2009;123:643–652. [DOI] [PubMed] [Google Scholar]
- 14.Kunz F, Schweitzer T, Große S, et al. Head orthosis therapy in positional plagiocephaly: longitudinal 3D-investigation of long-term outcomes, compared with untreated infants and with a control group. Eur J Orthod. 2019;41:29–37. [DOI] [PubMed] [Google Scholar]
- 15.Collett BR, Wallace ER, Kartin D, et al. Cognitive outcomes and positional plagiocephaly. Pediatrics. 2019;143:e20182373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bialocerkowski AE, Vladusic SL, Wei Ng C. Prevalence, risk factors, and natural history of positional plagiocephaly: a systematic review. Dev Med Child Neurol. 2008;50:577–586. [DOI] [PubMed] [Google Scholar]
- 17.Losee JE, Mason AC, Dudas J, et al. Nonsynostotic occipital plagiocephaly: factors impacting onset, treatment, and outcomes. Plast Reconstr Surg. 2007;119:1866–1873. [DOI] [PubMed] [Google Scholar]
- 18.Rogers GF. Deformational plagiocephaly, brachycephaly, and scaphocephaly. Part II: prevention and treatment. J Craniofac Surg. 2011;22:17–23. [DOI] [PubMed] [Google Scholar]
- 19.Beuriat PA, Szathmari A, Di Rocco F, et al. Deformational plagiocephaly: state of the art and review of the literature. Neurochirurgie. 2019;65:322–329. [DOI] [PubMed] [Google Scholar]
- 20.Graham JM, Jr, Gomez M, Halberg A, et al. Management of deformational plagiocephaly: repositioning versus orthotic therapy. J Pediatr. 2005;146:258–262. [DOI] [PubMed] [Google Scholar]
- 21.Rogers GF, Miller J, Mulliken JB. Comparison of a modifiable cranial cup versus repositioning and cervical stretching for the early correction of deformational posterior plagiocephaly. Plast Reconstr Surg. 2008;121:941–947. [DOI] [PubMed] [Google Scholar]
- 22.Di Chiara A, La Rosa E, Ramieri V, et al. Treatment of deformational plagiocephaly with physiotherapy. J Craniofac Surg. 2019;30:2008–2013. [DOI] [PubMed] [Google Scholar]
- 23.Kuo AA, Tritasavit S, Graham JM, Jr. Congenital muscular torticollis and positional plagiocephaly. Pediatr Rev. 2014;35:79–87; quiz 87. [DOI] [PubMed] [Google Scholar]
- 24.Kim SY, Park MS, Yang JI, et al. Comparison of helmet therapy and counter positioning for deformational plagiocephaly. Ann Rehabil Med. 2013;37:785–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Loveday BP, de Chalain TB. Active counterpositioning or orthotic device to treat positional plagiocephaly? J Craniofac Surg. 2001;12:308–313. [DOI] [PubMed] [Google Scholar]
- 26.Hinken L, Willenborg H, Dávila LA, et al. Outcome analysis of molding helmet therapy using a classification for differentiation between plagiocephaly, brachycephaly and combination of both. J Craniomaxillofac Surg. 2019;47:720–725. [DOI] [PubMed] [Google Scholar]
- 27.Seruya M, Oh AK, Taylor JH, et al. Helmet treatment of deformational plagiocephaly: the relationship between age at initiation and rate of correction. Plast Reconstr Surg. 2013;131:55e–61e. [DOI] [PubMed] [Google Scholar]
- 28.van Vlimmeren LA, van der Graaf Y, Boere-Boonekamp MM, et al. Effect of pediatric physical therapy on deformational plagiocephaly in children with positional preference: a randomized controlled trial. Arch Pediatr Adolesc Med. 2008;162:712–718. [DOI] [PubMed] [Google Scholar]
- 29.Cummings C. Positional plagiocephaly. Paediatr Child Health. 2011;16:493–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baird LC, Klimo P, Jr, Flannery AM, et al. Congress of Neurological Surgeons systematic review and evidence-based guideline for the management of patients with positional plagiocephaly: the role of physical therapy. Neurosurgery. 2016;79:E630–E631. [DOI] [PubMed] [Google Scholar]
- 31.Carvalho E, Bettger JP, Goode AP. Insurance coverage, costs, and barriers to care for outpatient musculoskeletal therapy and rehabilitation services. N C Med J. 2017;78:312–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Physical Therapy Association. Deformational plagiocephaly & cranial remolding in infants. Available at https://pediatricapta.org/includes/fact-sheets/pdfs/Plagiocephaly.pdf. Published 2007. Accessed March 20, 2021. [Google Scholar]
- 33.Price AV. Positional Plagiocephaly. American Association of Neurological Surgeons. Available at https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Positional-Plagiocephaly. Published 2021. Accessed March 20, 2021. [Google Scholar]
- 34.Naidoo SD, Skolnick GB, Patel KB, et al. Long-term outcomes in treatment of deformational plagiocephaly and brachycephaly using helmet therapy and repositioning: a longitudinal cohort study. Childs Nerv Syst. 2015;31:1547–1552. [DOI] [PubMed] [Google Scholar]
- 35.Timothy WV, Albert SW, et al. A comparison of costs associated with endoscope-assisted craniectomy versus open cranial vault repair for infants with sagittal synostosis. J Neurosurg Pediatrics PED. 2014;13:324–331. [DOI] [PubMed] [Google Scholar]
- 36.Kluba S, Lypke J, Kraut W, et al. Positional cranial deformity—the parents’ point of view. Int J Oral Maxillofac Surg. 2015;44:57–62. [DOI] [PubMed] [Google Scholar]
- 37.Littlefield TR, Kelly KM. Deformational plagiocephaly: recommendations for future research. J Prosthet Orthot. 2004;16:59-62. [Google Scholar]
- 38.Lam S, Luerssen TG, Hadley C, et al. The health belief model and factors associated with adherence to treatment recommendations for positional plagiocephaly. J Neurosurg Pediatr. 2017;19:282–288. [DOI] [PubMed] [Google Scholar]
- 39.Fernandez-Lazaro CI, Adams DP, Fernandez-Lazaro D, et al. Medication adherence and barriers among low-income, uninsured patients with multiple chronic conditions. Res Social Adm Pharm. 2019;15:744–753. [DOI] [PubMed] [Google Scholar]
- 40.Junn A, Dinis J, Long A, et al. Disparities in access to cranial remodeling orthosis for deformational plagiocephaly [Published online ahead of print Dec 30, 2021]. Cleft Palate Craniofac J. [DOI] [PubMed] [Google Scholar]
- 41.Kluba S, Lypke J, Kraut W, et al. Preclinical pathways to treatment in infants with positional cranial deformity. Int J Oral Maxillofac Surg. 2014;43:1171–1175. [DOI] [PubMed] [Google Scholar]
- 42.Martiniuk A, Jacob J, Faruqui N, et al. Positional plagiocephaly reduces parental adherence to SIDS Guidelines and inundates the health system. Child Care Health Dev. 2016;42:941–950. [DOI] [PubMed] [Google Scholar]
- 43.Ryall JJ, Xue Y, Turner KD, et al. Assessing the quality of life in infants with deformational plagiocephaly. J Craniomaxillofac Surg. 2021;49:29–33. [DOI] [PubMed] [Google Scholar]
- 44.Han MH, Kang JY, Han HY, et al. Relationship between starting age of cranial-remolding-orthosis therapy and effectiveness of treatment in children with deformational plagiocephaly. Childs Nerv Syst. 2017;33:1349–1356. [DOI] [PubMed] [Google Scholar]
- 45.Steinberg JP, Rawlani R, Humphries LS, et al. Effectiveness of conservative therapy and helmet therapy for positional cranial deformation. Plast Reconstr Surg. 2015;135:833–842. [DOI] [PubMed] [Google Scholar]
- 46.Graham T, Adams-Huet B, Gilbert N, et al. Effects of initial age and severity on cranial remolding orthotic treatment for infants with deformational plagiocephaly. J Clin Med. 2019;8:E1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kluba S, Kraut W, Reinert S, et al. What is the optimal time to start helmet therapy in positional plagiocephaly? Plast Reconstr Surg. 2011;128:492–498. [DOI] [PubMed] [Google Scholar]
- 48.Lipira AB, Gordon S, Darvann TA, et al. Helmet versus active repositioning for plagiocephaly: a three-dimensional analysis. Pediatrics. 2010;126:e936–e945. [DOI] [PubMed] [Google Scholar]