Abstract
Background
Large-bore aspiration catheters enabling greater flow rates and suction force for mechanical thrombectomy might improve outcomes in patients with stroke secondary to large-vessel occlusion. Complete or near-complete reperfusion after a single thrombectomy pass (first-pass effect) is associated with improved clinical outcomes. We assessed the efficacy and safety of novel MIVI Q™ aspiration catheters in combination with stent-retriever devices.
Methods
We retrospectively analyzed demographics, procedure characteristics, and clinical data from consecutive patients with acute anterior large-vessel occlusion treated with a combined approach using MIVI Q™ aspiration catheters and stent retrievers. Reperfusion was defined according to the modified thrombolysis in cerebral infarction (mTICI) score. Clinical outcomes were measured by the National Institute of Health Stroke Scale (NIHSS) and modified Rankin scale (mRS) scores.
Results
We included 52 patients (median age, 75 y IQR: 64–83); 31 (59.6%) women; 14 (26.9%) with terminal internal carotid artery occlusions, 26 (50%) middle cerebral artery (MCA) segment M1 occlusions, and 12 (23.1%) MCA segment M2 occlusions; median NIHSS score at admission was 19 (IQR: 13–22). After the first pass, 25 (48%) patients had mTICI ≥ 2c. At the end of the procedure, 47 (90.4%) had mTICI ≥ 2b and 35 (67.3%) had mTICI ≥ 2c. No serious device-related adverse events were observed. Symptomatic intracranial hemorrhage developed in 1 patient. Mean NIHSS score was 13 at 24 h and 5 at discharge. At 90 days, 24 (46.2%) patients were functionally independent (mRS 0–2).
Conclusion
This preliminary study found good efficacy and safety for MIVI Q™ aspiration catheters used in combination with stent-retriever devices.
Supplementary Information
The online version of this article (10.1007/s00062-021-01065-7) contains supplementary material, which is available to authorized users.
Keywords: Brain ischemia, Stroke, Mechanical thrombectomy, Device, Combined approach thrombectomy
Introduction
Randomized clinical trials have demonstrated the efficacy of mechanical thrombectomy for acute ischemic stroke secondary to large-vessel occlusion [1–5]. Mechanical thrombectomy aims to achieve complete reperfusion, ideally after a single pass of the thrombectomy device through the occluded segment (termed the first-pass effect, FPE) [6, 7]. The FPE is an independent predictor of good clinical outcome [8], and the first-pass rate is a metric of technical success. Modern mechanical thrombectomy devices are associated with higher reperfusion rates, shorter procedure times, better clinical outcomes, and lower risk of mortality [8]; however, although the physical properties influencing the effectiveness of different large-bore aspiration catheters have been investigated [9], the superiority of any specific device over another has yet to be demonstrated in clinical trials [10].
The MIVI QTM (MIVI Neuroscience, Eden Prairie, MN, USA) is a novel CE-approved device designed to provide greater suction and flow [11]. We assessed the technical efficacy and safety of this new catheter when used in combination with stent-retriever devices in patients with acute stroke due to anterior circulation large-vessel occlusion.
Methods
Patients
We retrospectively studied consecutive patients with acute ischemic stroke due to large-vessel occlusion in the anterior circulation (terminal internal carotid artery or middle cerebral artery (MCA) segments M1 or M2, excluding those with simultaneous cervical carotid and intracranial tandem occlusions) who were treated with MIVI QTM aspiration catheters in combination with stent retrievers as the first-line treatment in a comprehensive stroke center between June 2019 and May 2020. All thrombectomy procedures were performed by 4 interventional neuroradiologists, all of whom had ≥ 4 years experience in endovascular stroke treatment. The decision to use the MIVI QTM aspiration catheters as well as the type of stent retriever was at the discretion of the operator. Inclusion criteria were age ≥ 18 years, absence of pregnancy, acute ischemic stroke from large-vessel occlusion confirmed by computed tomography angiography or magnetic resonance angiography, premorbid modified Rankin scale (mRS) score ≤ 2, clinically significant neurological deficit, defined as assessed National Institutes of Health Stroke Scale (NIHSS) score ≥ 6 and time from last seen well to treatment ≤ 24 h. Intravenous thrombolysis was administered before mechanical thrombectomy in all eligible patients according to established criteria [12]. The study received institutional review board approval. After mechanical thrombectomy, patients or their representatives provided informed consent for imaging, procedural, analytical, and clinical data to be used in future retrospective studies. Our institution’s ethics committee waived the need for further specific informed consent for the current study.
Data Collection
We prospectively recorded age, sex, comorbidities, NIHSS score at admission and 24 h after mechanical thrombectomy, Alberta stroke program early CT score (ASPECTS) at admission, site of occlusion, timing of medical and interventional treatments, devices used, reperfusion outcomes, intracranial hemorrhage (ICH) and symptomatic ICH (sICH) [13] on 24‑h follow-up imaging, device-related or technique-related adverse events, and modified Rankin scale (mRS) score at day 90.
Outcome Variables
We recorded puncture-to-revascularization time, divided into puncture-to-first-run time and first-run-to-final-revascularization time. To determine procedural efficacy, an independent experienced interventional neuroradiologist blinded to the interventional team’s assessment classified technical success after a single pass according to the modified thrombolysis in cerebral infarction (mTICI) scale as FPE (mTICI ≥ 2c) or true FPE (tFPE = mTICI 3) [14, 15], as well as final reperfusion scores according to the same criteria.
To determine procedural safety, we analyzed ICH according to the European Cooperative Acute Stroke Study-II definition [13] on computed tomography 24 h after the procedure, early neurological deterioration (≥ 4 points from baseline NIHSS 24 h after the procedure), clinical complications deemed procedural by the attending interventionist, and deaths within 30 days attributable to the procedure. Clinical outcomes were assessed by the mRS score at 90 days. Good clinical outcome was defined as mRS ≤ 2.
Thrombectomy Technique
The MIVI QTM is a novel aspiration catheter designed to maximize flow and minimize pressure loss [11]. The proximal three quarters of the catheter shaft have been replaced with a 119 cm 0.020″ stainless steel pusher wire. This innovation allows the full internal area of the guiding catheter to provide a higher aspirated flow rate and suction force than standard tubular catheter designs. The outer diameter (OD) of the proximal segments of the QTM is 0.088″; the length of the catheter and the inner diameter (ID) of the distal catheter segments varies according to the model, being 25 cm and 0.069″ for the Q6, 25 cm and 0.057″ for the Q5, 30 cm and 0.043″ for the Q4, and 43 cm and 0.036″ for the Q3. The aspiration catheter is used with the Super 90 8F guide catheter (MIVI Neuroscience Inc.) (ID 0.090″, length 80 cm, 90 cm, or 95 cm). Pump aspiration is directly applied to the Super 90 guide catheter and the total system length varies as the QTM is extended outward and retracted into the Super 90 guide catheter [11].
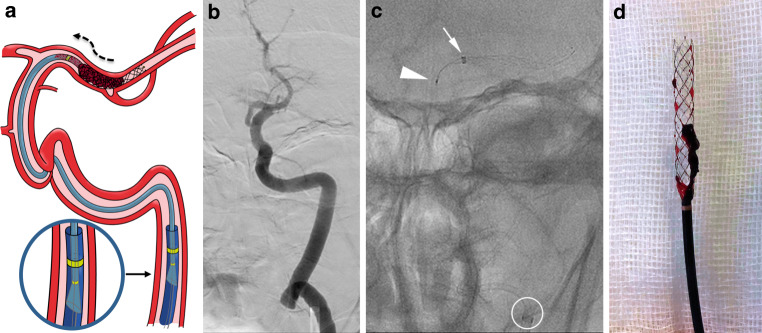
Depending on the patient’s condition, procedures were done with the patient under local anesthesia, conscious sedation or general anesthesia. Through femoral artery access, the guide catheter was placed in the internal carotid artery of the affected side. A RebarTM18 microcatheter (ev3 Inc. Medtronic, Minneapolis, MN, USA) with a Synchro® 0.014″ microwire (Boston Scientific for Stryker Neurovascular, Fremont, CA, USA) was advanced through the arterial occlusion. The largest diameter QTM aspiration catheter that would fit in the affected vessel was advanced to the occlusion over the microcatheter and microwire unit in a monorail fashion. Then a stent retriever was advanced through the microcatheter and deployed at the level of the thrombus using the push-and-fluff technique [16]. To increase the cross-sectional area and flow, the microcatheter was removed [17] and pump aspiration was applied to the guiding catheter. The stent retriever was retracted slightly and the QTM was carefully advanced until no flow was present in the aspiration tubing. After 1 min under occlusive aspiration, both devices were slowly retrieved as a unit inside the guiding catheter and then withdrawn while maintaining aspiration (Fig. 1).
Fig. 1.
a Illustration of the QTM and stent retriever combined approach during the thrombus wedging maneuver. After removing the microcatheter, the stent retriever has been slightly retracted and the QTM catheter carefully advanced under pump aspiration to ensure better engagement of the thrombus. The flared proximal tip of the Q catheter (magnified inset) ensures a tight seal between its outer surface and the Super 90 guiding catheter’s inner surface, enabling increased suction power (curved black dashed arrow) directly through the guide catheter. b Anteroposterior left internal carotid artery (ICA) angiography through the Super 90 guiding catheter showing a terminal ICA occlusion. c Unsubtracted anteroposterior view showing the combined approach thrombectomy: Distal end of the Super 90 Catheter (white circle), distal end of a Q6 aspiration catheter (white arrow), and a fully deployed Aperio® Hybrid stent with its proximal end inside the Q6 (white arrowhead). d Q6 and Aperio® Hybrid with the “pinned” thrombus
Results
During the 10-month study period, a total of 105 patients with acute ischemic stroke underwent mechanical thrombectomy at Hospital Universitari Germans Trias i Pujol comprehensive stroke center. The MIVI QTM aspiration catheter was the first-line treatment in 74 patients with large-vessel occlusion. Of these, 22 were excluded from the analyses (13 had posterior circulation occlusions, 4 had tandem occlusions in the cervical internal carotid and MCA, and 5 had anterior circulation stroke but were treated with first-line contact aspiration only). Thus, 52 patients were analyzed. A flowchart of patient selection is provided in Supplemental Fig. 2. Table 1 summarizes the demographic, clinical, and procedure characteristics of our cohort.
Table 1.
Baseline characteristics of the 52 patients included in the study
| Characteristics | Values |
|---|---|
| Age (years) median (IQR) | 75 (64–83) |
| Female sex, n (%) | 31 (59.6) |
| NIHSS score at admission, median (IQR) | 19 (13–22) |
| Pre-stroke mRS, n (%) | |
| 0 | 44 (84.6) |
| 1 | 4 (7.7) |
| 2 | 4 (7.7) |
| Medical history, n (%) | |
| Hypertension | 34 (65.4) |
| Diabetes mellitus | 15 (28.8) |
| Atrial fibrillation | 13 (25) |
| Dyslipidemia | 28 (53.8) |
| Smoking | 12 (23.1) |
| Obesity | 5 (9.6) |
| Myocardial infarction or coronary artery disease | 13 (25) |
| Previous stroke or TIA | 8 (15.4) |
| Anticoagulation | 13 (25) |
| Antiplatelet | 9 (17.3) |
| ASPECTS at admission, median (IQR) | 9 (8–10) |
| Occlusion site, n (%) | |
| Left side | 30 (57.7) |
| ICA‑T | 14 (26.9) |
| MCA-M1 | 26 (50) |
| MCA-M2 | 12 (23.1) |
| Time from symptom onset or LTSW to arterial puncture (min), median (IQR) | 278 (170–419) |
| Door-to-groin time (min), median (IQR) | 70 (36–96) |
| QTM device used, n (%) | |
| Q3 | 5 (9.6) |
| Q4 | 7 (13.5) |
| Q5 | 19 (36.5) |
| Q6 | 21 (40.4) |
| Stent retriever used, n (%) | |
| Aperio Hybrid® | 27 (51.9) |
| Catch View® | 15 (28.8) |
| Embotrap II® | 5 (9.6) |
| NeVa® | 5 (9.6) |
| IV tPA administered, n (%) | 17 (32.7) |
IQR interquartile range, NIHSS National Institute of Health Stroke Scale score, mRS modified Rankin Scale score, TIA transient ischemic attack, ASPECTS Alberta Stroke Program Early CT Score, MCA-M1 ICA-T: intracranial carotid T occlusion, M1 segment of the middle cerebral artery, MCA-M2 M2 segment of the middle cerebral artery, LTSW last time seen well, QTM (MIVI Neuroscience, Inc., Eden Prairie, MN, USA), Aperio Hybrid® (Acandis company, Pforzheim, Germany), Catch View® (Balt, Montmorency, France), Embotrap II® (Cerenovus, Galway, Ireland), NeVa® (Vesalio, Nashville, TN, USA), IV tPA intravenous tissue plasminogen activator
The QTM aspiration catheter reached the occlusion in all patients, achieving FPE in 48%. Final reperfusion was excellent (mTICI ≥ 2c) in 67.3% and successful (mTICI ≥ 2b) in 90.4%. No device-related adverse events occurred, and no patients required rescue therapy. Table 2 reports procedural variables.
Table 2.
Angiographic outcomes
| Reperfusion and time-metrics | Results |
|---|---|
| Groin-puncture-to-revascularization (min), median (IQR) | 42 (22–66) |
| Time from first angiogram to recanalization (min), median (IQR) | 28 (15–59) |
| QTM tFPE | |
| mTICI 3, n (%) | 22 (42.3) |
| Groin-puncture-to-revascularization (min), median (IQR) | 29 (20–45) |
| Time from first angiogram to recanalization (min), median (IQR) | 15 (11–26) |
| QTM FPE | |
| mTICI 2c‑3, n (%) | 25 (48) |
| Groin-puncture-to-revascularization (min), median (IQR) | 26 (20–39) |
| Time from first angiogram to recanalization (min), median (IQR) | 15 (11–24) |
| QTM mTICI ≥ 2b with a single pass | |
| mTICI ≥ 2b with a single pass, n (%) | 28 (53.8) |
| Groin-puncture-to-revascularization (min), median (IQR) | 26 (20–41) |
| Time from first angiogram to recanalization (min), median (IQR) | 15 (11–26) |
| ≤ 2QTM passes | |
| mTICI ≥ 2b, n (%) | 34 (65.4) |
| mTICI 2c‑3, n (%) | 29 (55.7) |
| Total passes, n (mean) | 40 (1.18) |
| Groin-puncture-to-revascularization (min), median (IQR) | 26 (20–46) |
| Time from first angiogram to recanalization (min), median (IQR) | 15 (11–34) |
| ≤ 3QTM passes | |
| mTICI ≥ 2b, n (%) | 39 (75) |
| mTICI 2c‑3, n (%) | 32 (61.5) |
| Total passes, n (mean) | 55 (1.41) |
| Groin-puncture-to-revascularization (min), median (IQR) | 32 (20–55) |
| Time from first angiogram to recanalization (min), median (IQR) | 18 (14–40) |
| Final Reperfusion | |
| mTICI 3, n (%) | 28 (53.8) |
| mTICI ≥ 2b, n (%) | 47 (90.4) |
| mTICI 2c‑3, n (%) | 35 (67.3) |
| Total passes, mean | 2.46 |
IQR interquartile range, mTICI modified thrombolysis in cerebral ischemia, tFPE mTICI = 3 after a single pass, FPE mTICI ≥ 2c after a single pass
Table 3 reports the clinical outcomes related to safety and efficacy. In one patient with an M1 occlusion, an embolus that had migrated into the A2 segment of the anterior cerebral artery (unaffected territory) during withdrawal was retrieved uneventfully with the same system. A patient in his 40s (admission ASPECTS 5) treated with intravenous thrombolysis who achieved mTICI 2b after 5 passes developed sICH and died. In another patient, microwire vessel perforation during microcatheter advancement (unrelated to the aspiration catheter or the stent retriever) resulted in a parenchymal hematoma (PH1), identified at 24h follow-up, but did not cause any neurological deterioration. Petechial reperfusion hemorrhages (HI1) or minor subarachnoid hemorrhage occurred in 8 patients.
Table 3.
Clinical efficacy and safety outcomes
| Efficacy and safety | Results |
|---|---|
| 24-hour NIHSS, mean (IQR) | 13 (4–18) |
| Early neurological improvement, n (%)a | 28 (53.8) |
| NIHSS at discharge, mean (IQR) | 5 (1–11) |
| mRS at discharge, n (%) | |
| 0–1 | 8 (15.4) |
| 0–2 | 15 (28.8) |
| 3 | 8 (15.4) |
| 4 | 13 (25) |
| 5 | 7 (13.5) |
| 6 | 9 (17.3) |
| mRS at 90 days, n (%) | |
| 0–1 | 20 (38.5) |
| 0–2 | 24 (46.2) |
| 3 | 4 (7.7) |
| 4 | 6 (11.5) |
| 5 | 3 (5.8) |
| 6 | 15 (28.8) |
| Intracranial hemorrhage, n (%) | |
| sICH | 1 (1.9) |
| All ICH | 10 (19.2) |
| Early neurological deterioration, n (%) | 7 (13.5) |
| All-cause mortality at 90 days, n (%) | 15 (28.8) |
| In hospital mortality, n (%) | 9 (17.3) |
| Serious device-related adverse events, n (%) | 0 (0) |
| Serious procedure related adverse events, n (%)b | 1 (1.9) |
NIHSS National Institute of Health Stroke Scale score, IQR interquartile range, mRS modified Rankin Scale score, sICH symptomatic intracranial hemorrhage, ICH intracranial hemorrhage
a Early neurological improvement was defined as a reduction of ≥ 5 points on the NIHSS or an NIHSS score < 4 at 24-hours
b Microwire perforation with contrast extravasation on angiography
Early neurological deterioration developed in 7 (13.5%) patients. A total of 9 (17.3%) patients died before hospital discharge, 2 from malignant edema related to large-volume stroke. At 90 days 24 (46.2%) patients were functionally independent (mRS 0–2).
Discussion
Speed and grade of recanalization are of paramount importance in neurothrombectomy; therefore, choosing a safe and time-efficient strategy is key in stroke treatment.
Final reperfusion rates and functional outcomes after thromboaspiration and stent-retriever thrombectomy are similar [18]. Used as a stand-alone first-line technique, stent retrievers achieve better reperfusion with less need for rescue devices but require longer groin-to-reperfusion times [18]. Recently introduced approaches combining stent retrievers and large-bore aspiration catheters trap the thrombus between the catheter tip and the stent retriever while maintaining local aspiration [19, 20], a change from earlier combined approaches (e.g., Solumbra) where the stent retriever was retracted into the aspiration catheter [21]. Combined approaches have shown improved reperfusion rates and FPE [22]; however, there remains considerable room for improvement in achieving an early and complete reperfusion [23].
Successful thromboaspiration requires using the largest catheter that the vessel can accommodate [24–26]. The MIVI Q™ aspiration catheter is designed to maximize lumen size, increasing flow rates and tip suction force [11]. Both properties combined have been shown to be necessary to effectively extract the clot, but in vitro experiments indicated that suction force is more relevant than aspiration flow in terms of efficacy, particularly in hard clots [27]. The MIVI QTM exhibits these two physical properties, and especially the aspiration flow rate benefits from a dynamic effect as in vitro testing has demonstrated that it increases as the QTM is retracted inside the guiding catheter [11]. It can be used alone or combined with a stent retriever, as in our cohort. In this preliminary clinical experience, there were no device-related adverse events, and the angiographic, time-metric, and clinical outcomes were similar to those in other studies using combined mechanical thrombectomy approaches [20, 28–30].
Delivering large-bore aspiration catheters intracranially to the thrombus is not always easy [31] because of vessel tortuosity, underlying intracranial atherosclerosis, or even the anatomical position where the ophthalmic artery originates from the carotid siphon [32]. The soft and flexible design of the MIVI Q™ aspiration catheter resulted in excellent trackability; in all patients, the catheter was navigated to the occlusion uneventfully. These results compare favorably with those reported in an initial experience with the Sofia catheter (MicroVention, Tustin, CA, USA), where the occlusion was reached uneventfully in 96% of cases [33]. The Q™ catheter was coaxially advanced over the RebarTM18 microcatheter, and no stent anchoring [34] or “blind exchange” maneuvers [35] were needed to navigate the Q™ catheter, even when using larger caliber catheters and when the arterial anatomy was tortuous. Avoiding anchoring and exchange maneuver eliminates a theoretical risk of vascular injury.
The Q™ catheter design takes advantage of fluid mechanics theory so that the suction force in the tip of the Q™ catheter increases when it is retrieved inside the guiding catheter, potentially diminishing the risk of distal emboli migrating during system retrieval [11]. This may explain the low rate of complications related to emboli migrating to previously unaffected territories (1.9%) in our series.
Another potential advantage of the MIVI Q™ aspiration catheter design is that it does not require a rotating hemostatic valve connected to a saline flush line, thus enabling faster preprocedural preparation and faster purging after its retrieval when additional passes are necessary and thereby improving the efficiency of interventions.
Our successful reperfusion rate (90.4%) is in line with those reported by Hesse et al. [30] in the primary combined approach (PCA) group (86%), CAPTIVE (100%) [20], and SAVE (95%) [28]. Likewise, our rate of final TICI 3 (53.8%) is in line with those reported in PCA (37.5%), CAPTIVE (33%), and SAVE (56%). The proportion of procedures that achieved mTICI ≥ 2b with a single pass (53.8%) is in line with rates reported in CAPTIVE (59%) and SAVE (74%). Our rate of tFPE (42.3%) is similar to that reported in SAVE (45%), but higher than that reported by Hesse et al. [30] (26%), who used the Solumbra technique [21] for most cases in the PCA group.
Median groin-to-recanalization time was 42 min, similar to that reported in SAVE (34 min) [28] and PCA (51 min) [30], but longer than in CAPTIVE (14 min) [20].
Lastly, 46.2% of patients in our cohort had good clinical outcomes (mRS ≤ 2) at 90-days, comparable to the 49% reported in CAPTIVE [20].
In summary, the procedure times and proportion of patients achieving FPE, tFPE, excellent and successful final reperfusion and good clinical outcomes at 3 months, were in line with those reported in other cohorts where combined approaches were used.
Limitations
This retrospective, non-randomized study included relatively few patients at a single center with no control group, and reperfusion and clinical outcomes were local operator-measured; thus, caution is essential in extrapolating the results. Nevertheless, our preliminary results include the learning curve inherent in using new devices and merit further studies with larger samples to determine the efficacy of this approach compared to other devices and approaches.
Conclusion
This preliminary study suggests that the MIVI QTM aspiration catheter has a good efficacy and safety profile when used in combination with stent retrievers, achieving high reperfusion rates and favorable clinical outcomes.
Supplementary Information
Supplemental Fig. 2. Flowchart of subjects with acute ischemic stroke caused by a large-vessel occlusion selected for analysis. LVO large-vessel occlusion, MT mechanical thrombectomy, SR stent-retriever
Acknowledgments
Acknowledgements
The authors thank Raquel Pujana and Ana Pujana for the graphic illustration.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Abbreviations
- ASPECTS
Alberta stroke program early CT score
- CAPTIVE
Continuous aspiration prior to intracranial vascular embolectomy
- CT
Computed tomography
- FPE
First-pass effect
- ICH
Intracranial hemorrhage
- IQR
Interquartile range
- LTSW
Last time seen well
- LVO
Large-vessel occlusion
- MCA
Middle cerebral artery
- MRS
Modified Rankin scale
- MTICI
Modified thrombolysis in cerebral infarction scale
- NIHSS
National Institutes of Health Stroke Scale
- PCA
Primary combined approach
- SAVE
Stent-retriever assisted vacuum-locked extraction
- SICH
Symptomatic intracranial hemorrhage
- TFPE
True first-pass effect
- TIA
Transient ischemic attack
- TPA
Tissue plasminogen activator
Author Contribution
S. Remollo: Conceptualization, methodology, formal analysis, resources, data curation, writing-original draft, writing—review and editing, visualization, supervision, project administration; M. Terceño: Resources, data curation, writing—review and editing; M. Werner: Resources, data curation, writing—review and editing; C. Castaño: Resources, data curation, writing—review and editing; M. Hernández-Pérez: Resources, data curation, writing—review and editing; J. Blasco: Writing—review and editing; L. San Román: Writing—review and editing; P. Daunis-i-Estadella: Formal analysis, writing—review and editing; S. Thió-Henestrosa: Formal analysis, writing—review and editing; V. Cuba: Writing—review and editing; A. Gimeno: Writing—review and editing; J. Puig: Formal analysis, writing—original draft, writing—review and editing, visualization, supervision.
Declarations
Conflict of interest
S. Remollo, M. Terceño, M. Werner, C. Castaño, M. Hernández-Pérez, J. Blasco, L. San Román, P. Daunis-i-Estadella, S. Thió-Henestrosa, V. Cuba, A. Gimeno and J. Puig declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional (Ethics Committee of Hospital Universitari Germans Trias i Pujol) and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Footnotes
Availability of Data and Material (data transparency)
Data are available from the corresponding author upon reasonable request.
References
- 1.Berkhemer OA, Fransen PSS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Albert J, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJH, van Walderveen MAA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PLM, van Rooij WJJ, van den Berg JSP, van Hasselt BAAM, Aerden LAM, Dallinga RJ, Visser MC, Bot JCJ, Vroomen PC, Eshghi O, Schreuder THCML, Heijboer RJJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg-Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers MES, Jenniskens SFM, Beenen LFM, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YBWEM, van der Lugt A, van Oostenbrugge RJ, Majoie CBLM, Dippel DWJ. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 2.Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, San Román L, Serena J, Abilleira S, Ribó M, Millán M, Urra X, Cardona P, López-Cancio E, Tomasello A, Castaño C, Blasco J, Aja L, Dorado L, Quesada H, Rubiera M, Hernandez-Pérez M, Goyal M, Demchuk AM, von Kummer R, Gallofré M, Dávalos A. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–2306. doi: 10.1056/NEJMoa1503780. [DOI] [PubMed] [Google Scholar]
- 3.Saver JL, Goyal M, Bonafe A, Diener H-C, Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, Jansen O, Jovin TG, Mattle HP, Nogueira RG, Siddiqui AH, Yavagal DR, Baxter BW, Devlin TG, Lopes DK, Reddy VK, du Mesnil de Rochemont R, Singer OC, Jahan R. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372:2285–2295. doi: 10.1056/NEJMoa1415061. [DOI] [PubMed] [Google Scholar]
- 4.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn S-I, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–1030. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 5.Campbell BCV, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, Ang T, Scroop R, Barber PA, McGuinness B, Wijeratne T, Phan TG, Chong W, Chandra RV, Bladin CF, Badve M, Rice H, de Villiers L, Ma H, Desmond PM, Donnan GA, Davis SM. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–1018. doi: 10.1056/NEJMoa1414792. [DOI] [PubMed] [Google Scholar]
- 6.Linfante I, Starosciak AK, Walker GR, Dabus G, Castonguay AC, Gupta R, Sun CHJ, Martin C, Holloway WE, Mueller-Kronast N, English JD, Malisch TW, Marden FA, Bozorgchami H, Xavier A, Rai AT, Froehler MT, Badruddin A, Nguyen TN, Taqi MA, Abraham MG, Janardhan V, Shaltoni H, Novakovic R, Yoo AJ, Abou-Chebl A, Chen PR, Britz GW, Kaushal R, Nanda A, Issa MA, Nogueira RG, Zaidat OO. Predictors of poor outcome despite recanalization: a multiple regression analysis of the NASA registry. J Neurointerv Surg. 2016;8:224–229. doi: 10.1136/neurintsurg-2014-011525. [DOI] [PubMed] [Google Scholar]
- 7.Kharouba R, Gavriliuc P, Yaghmour NE, Gomori JM, Cohen JE, Leker RR. Number of stentriever passes and outcome after thrombectomy in stroke. J Neuroradiol. 2019;46:327–330. doi: 10.1016/j.neurad.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE, Mueller-Kronast N, English JD, Dabus G, Malisch TW, Marden FA, Bozorgchami H, Xavier A, Rai AT, Froehler MT, Badruddin A, Nguyen TN, Taqi MA, Abraham MG, Yoo AJ, Janardhan V, Shaltoni H, Novakovic R, Abou-Chebl A, Chen PR, Britz GW, Sun CHJ, Bansal V, Kaushal R, Nanda A, Nogueira RG. First pass effect. Stroke. 2018;49:660–666. doi: 10.1161/STROKEAHA.117.020315. [DOI] [PubMed] [Google Scholar]
- 9.Froehler MT. Comparison of vacuum pressures and forces generated by different catheters and pumps for aspiration thrombectomy in acute ischemic stroke. Interv Neurol. 2017;6:199–206. doi: 10.1159/000475478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yaeger K, Iserson A, Singh P, Wolf J, Vidal E, Oxley T, Costa AB, Fifi JT. A technical comparison of thrombectomy vacuum aspiration systems. J Neurointerv Surg. 2020;12:72–76. doi: 10.1136/neurintsurg-2019-014929. [DOI] [PubMed] [Google Scholar]
- 11.Long TD, Kallmes DF, Hanel R, Shigematsu T, Halaszyn AM, Wolter J, Berenstein A. Novel aspiration catheter design for acute stroke thrombectomy. J Neurointerv Surg. 2019;11:179–183. doi: 10.1136/neurintsurg-2017-013702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adams HP, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C, Lyden PD, Morgenstern LB, Qureshi AI, Rosenwasser RH, Scott PA, Wijdicks EFM. Guidelines for the early management of adults with ischemic stroke. Stroke. 2007;38:1655–1711. doi: 10.1161/STROKEAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- 13.Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, Larrue V, Bluhmki E, Davis S, Donnan G, Schneider D, Diez-Tejedor E, Trouillas P. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II) Lancet. 1998;352:1245–1251. doi: 10.1016/S0140-6736(98)08020-9.. [DOI] [PubMed] [Google Scholar]
- 14.Dargazanli C, Fahed R, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, Saleme S, Costalat V, Bracard S, Desal H, Mazighi M, Consoli A, Piotin M, Lapergue B, Redjem H, Ciccio G, Smajda S, Desilles JP, Rodesch G, Coskun O, Di Maria F, Bourdain F, Decroix JP, Wang A, Tchikviladze M, Evrard S, Eker O, Turjman F, Labeyrie PE, Riva R, Mounayer C, Saleme S, Bonafé A, Gascou G, Tonnelet R, Derelle AL, Anxionnat R, Bourcier R, Daumas-Duport B, Berge J, Barreau X, Djemmane L. Modified thrombolysis in cerebral infarction 2C/thrombolysis in cerebral infarction 3 reperfusion should be the aim of mechanical thrombectomy. Stroke. 2018;49:1189–1196. doi: 10.1161/STROKEAHA.118.020700. [DOI] [PubMed] [Google Scholar]
- 15.Almekhlafi MA, Mishra S, Desai JA, Nambiar V, Volny O, Goel A, Eesa M, Demchuk AM, Menon BK, Goyal M. Not all “successful” angiographic reperfusion patients are an equal validation of a modified TICI scoring system. Interv Neuroradiol. 2014;20:21–27. doi: 10.15274/INR-2014-10004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haussen DC, Rebello LC, Nogueira RG. Optimizating clot retrieval in acute stroke. Stroke. 2015;46:2838–2842. doi: 10.1161/STROKEAHA.115.010044. [DOI] [PubMed] [Google Scholar]
- 17.Nikoubashman O, Alt JP, Nikoubashman A, Büsen M, Heringer S, Brockmann C, Brockmann MA, Müller M, Reich A, Wiesmann M. Optimizing endovascular stroke treatment: removing the microcatheter before clot retrieval with stent-retrievers increases aspiration flow. J Neurointerv Surg. 2017;9:459–462. doi: 10.1136/neurintsurg-2016-012319. [DOI] [PubMed] [Google Scholar]
- 18.Tsang COA, Cheung IHW, Lau KK, Brinjikji W, Kallmes DF, Krings T. Outcomes of stent retriever versus aspiration-first thrombectomy in ischemic stroke: a systematic review and meta-analysis. Am J Neuroradiol. 2018;39:2070–2076. doi: 10.3174/ajnr.A5825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maus V, Behme D, Kabbasch C, Borggrefe J, Tsogkas I, Nikoubashman O, Wiesmann M, Knauth M, Mpotsaris A, Psychogios MN. Maximizing first-pass complete reperfusion with SAVE. Clin Neuroradiol. 2018;28:327–338. doi: 10.1007/s00062-017-0566-z. [DOI] [PubMed] [Google Scholar]
- 20.McTaggart RA, Tung EL, Yaghi S, Cutting SM, Hemendinger M, Gale HI, Baird GL, Haas RA, Jayaraman MV. Continuous aspiration prior to intracranial vascular embolectomy (CAPTIVE): a technique which improves outcomes. J Neurointerv Surg. 2017 doi: 10.1136/neurintsurg-2016-012838. [DOI] [PubMed] [Google Scholar]
- 21.Delgado Almandoz JE, Kayan Y, Young ML, Fease JL, Scholz JM, Milner AM, Hehr TH, Roohani P, Mulder M, Tarrel RM. Comparison of clinical outcomes in patients with acute ischemic strokes treated with mechanical thrombectomy using either Solumbra or ADAPT techniques. J Neurointerv Surg. 2016;8:1123–1128. doi: 10.1136/neurintsurg-2015-012122. [DOI] [PubMed] [Google Scholar]
- 22.Ospel JM, McTaggart R, Kashani N, Psychogios M, Almekhlafi M, Goyal M. Evolution of stroke thrombectomy techniques to optimize first-pass complete reperfusion. Semin intervent Radiol. 2020;37:119–131. doi: 10.1055/s-0040-1709153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goyal M, Menon BK, van Zwam WH, Dippel DWJ, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CBLM, van der Lugt A, de Miquel MA, Donnan GA, Roos YBWEM, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millán M, Davis SM, Roy D, Thornton J, San Román L, Ribó M, Beumer D, Stouch B, Brown S, Campbell BCV, van Oostenbrugge R, Saver JL, Hill MD, Jovin TG. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 24.Lapergue B, Blanc R, Guedin P, Decroix JP, Labreuche J, Preda C, Bartolini B, Coskun O, Redjem H, Mazighi M, Bourdain F, Rodesch G, Piotin M. A direct aspiration, first pass technique (ADAPT) versus stent retrievers for acute stroke therapy: an observational comparative study. Am J Neuroradiol. 2016;37:1860–1865. doi: 10.3174/ajnr.A4840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Romano DG, Cioni S, Vinci SL, Pero G, Comelli C, Comai A, Peschillo S, Mardighian D, Castellan L, Resta F, Piano MG, Comelli S, Barletta L, Puliti A, Leonini S, Bracco S. Thromboaspiration technique as first approach for endovascular treatment of acute ischemic stroke: initial experience at nine Italian stroke centers. J Neurointerv Surg. 2017;9:6–10. doi: 10.1136/neurintsurg-2016-012298. [DOI] [PubMed] [Google Scholar]
- 26.Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, Saleme S, Costalat V, Bracard S, Desal H, Mazighi M, Consoli A, Piotin M. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion. JAMA. 2017;318:443. doi: 10.1001/jama.2017.9644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fernandez-Sanchez D, Garcia-Sabido D, Jovin TG, Villanova H, Andersson T, Nogueira RG, Cognard C, Ribo M, Siddiqui AH, Galve I, Arad O, Salmon F. Suction force rather than aspiration flow correlates with recanalization in hard clots: an in vitro study model. J Neurointerv Surg. 2021 doi: 10.1136/neurintsurg-2020-017242. [DOI] [PubMed] [Google Scholar]
- 28.Maus V, Henkel S, Riabikin A, Riedel C, Behme D, Tsogkas I, Hesse AC, Abdullayev N, Jansen O, Wiesmann M, Mpotsaris A, Psychogios MN. The SAVE technique: large-scale experience for treatment of Intracranial large vessel occlusions. Clin Neuroradiol. 2019;29:669–676. doi: 10.1007/s00062-018-0702-4. [DOI] [PubMed] [Google Scholar]
- 29.Brehm A, Maus V, Tsogkas I, Colla R, Hesse AC, Gera RG, Psychogios MN. Stent-retriever assisted vacuum-locked extraction (SAVE) versus a direct aspiration first pass technique (ADAPT) for acute stroke: data from the real-world. BMC Neurol. 2019;19:65. doi: 10.1186/s12883-019-1291-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hesse AC, Behme D, Kemmling A, Zapf A, Hokamp NG, Frischmuth I, Maier I, Liman J, Tsogkas I, Buhk JH, Tran J, Fiehler J, Mpotsaris A, Schramm P, Berlis A, Knauth M, Psychogios MN. Comparing different thrombectomy techniques in five large-volume centers: a ‘real world’ observational study. J Neurointerv Surg. 2018;10:525–529. doi: 10.1136/neurintsurg-2017-013394. [DOI] [PubMed] [Google Scholar]
- 31.Spiotta AM, Chaudry MI, Hui FK, Turner RD, Kellogg RT, Turk AS. Evolution of thrombectomy approaches and devices for acute stroke: a technical review. J Neurointerv Surg. 2015;7(1):2–7. doi: 10.1136/neurintsurg-2013-011022. [DOI] [PubMed] [Google Scholar]
- 32.Kang DH, Hwang YH. Frontline contact aspiration treatment for emergent large vessel occlusion: a review focused on practical techniques. J Stroke. 2019;21(1):10–22. doi: 10.5853/jos.2018.03076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stampfl S, Kabbasch C, Müller M, Mpotsaris A, Brockmann M, Liebig T, Wiesmann M, Bendszus M, Möhlenbruch MA. Initial experience with a new distal intermediate and aspiration catheter in the treatment of acute ischemic stroke: clinical safety and efficacy. J Neurointerv Surg. 2016;8(7):714–718. doi: 10.1136/neurintsurg-2015-011801. [DOI] [PubMed] [Google Scholar]
- 34.Singh J, Wolfe SQ, Janjua RM, Hedayat H, Burnette C. Anchor technique: use of stent retrievers as an anchor to advance thrombectomy catheters in internal carotid artery occlusions. Interv Neuroradiol. 2015;21(6):707–709. doi: 10.1177/1591019915609170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haussen DC, Al-Bayati AR, Eby B, Ravindran K, Rodrigues GM, Frankel MR, Nogueira RG. Blind exchange with mini-pinning technique for distal occlusion thrombectomy. J Neurointerv Surg. 2020;12(4):392–395. doi: 10.1136/neurintsurg-2019-015205. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Fig. 2. Flowchart of subjects with acute ischemic stroke caused by a large-vessel occlusion selected for analysis. LVO large-vessel occlusion, MT mechanical thrombectomy, SR stent-retriever