Abstract
Background and Purpose
A Thrombolysis in Cerebral Infarction (TICI) score of 3 has been established as therapeutic goal in endovascular therapy (EVT) for acute ischemic stroke; however, in the case of early TICI2b reperfusion, the question remains whether to stop the procedure or to continue in the pursuit of perfection (i.e., TICI 2c/3).
Methods
A total of 6635 patients were screened from the German Stroke Registry. Patients who underwent EVT for occlusion of the middle cerebral artery (M1 segment), with final TICI score of 2b/3 were included. Multivariable logistic regression was performed with functional independence (modified Rankin Scale, mRS at day 90 of 0–2) as the dependent variable.
Results
Of 1497 patients, 586 (39.1%) met inclusion criteria with a final TICI score of 2b and 911 (60.9%) with a TICI score of 3. Patients who achieved first-pass TICI3 showed highest odds of functional independence (Odds ratio [OR] 1.71, 95% confidence interval [95% CI] 1.18–2.47). Patients who achieved TICI2b with the second pass (OR 0.53, 95% CI 0.31–0.89) or with three or more passes (OR 0.44, 95% CI 0.27–0.70) had significantly worse clinical outcomes compared to first-pass TICI2b. TICI3 at the second pass was by trend better than first-pass TICI2b (OR 1.55, 95% CI 0.98–2.45), but TICI3 after 3 or more passes (OR 0.93, 95% CI 0.57–1.50) was not significantly different from first-pass TICI2b.
Conclusion
First-pass TICI2b was superior to TICI2b after ≥ 2 retrievals and comparable to TICI3 at ≥ 3 retrievals. The potential benefit in outcome after achieving TICI3 following further retrieval attempts after first-pass TICI2b need to be weighed against the risks.
Supplementary Information
The online version of this article (10.1007/s00062-021-01048-8) contains supplementary material, which is available to authorized users.
Keywords: Ischemic stroke, Thrombectomy, Endovascular therapy, Retrievals, Prognostic factors
Introduction
Endovascular therapy (EVT) has been established as the standard of care for acute large-vessel occlusion (LVO) in the anterior circulation ischemic stroke [1]. In the past, procedural success of EVT had been defined by a final thrombolysis in cerebral infarction (TICI) score of 2b and 3 [2]; however, several studies have reported improved clinical outcome in patients with a final TICI score of 3 vs. those with a final score of 2b [3–5]. Furthermore, a TICI score of 2c has been defined as nearly complete reperfusion [6]. The clinical importance of achieving at least this level of reperfusion has been illustrated in a recent study by Dargazanli et al., which showed that patients with a TICI score of 2c/3 had a superior outcome compared to those with a TICI score of 2b [7]. As a result, the current ESO/ESMINT guidelines recommend TICI 3 reperfusion to be the therapeutic goal of EVT, if reasonably and safely achievable [8].
In the case of early TICI 2b reperfusion, the practical question remains whether to stop or continue the procedure, with the goal of achieving TICI 3. Barring any potential risks associated with increasing retrieval count, one could perform as many attempts as needed to achieve the TICI 2c/3 reperfusion goal; however, multiple retrieval attempts have been associated with worse clinical outcome following EVT [9–11], as well as with an increased risk of intracranial hemorrhage [12, 13].
For the present study, we included only patients with occlusions of the M1 segment of the MCA from a large multicenter registry, in an effort to rule out differing locations of occlusion as a confounding factor of reperfusion success [14, 15]. Our aim was to compare outcomes of patients with a final TICI score of 3 with a final TICI score of 2b, stratified by the number of retrieval attempts required.
We hypothesized that patients with a final TICI score of 2b during the first attempt have the same or superior odds of good clinical outcome compared to patients who achieve TICI 3 after more than one attempt.
Methods
Patient Selection
A total of 6635 patients were initially analyzed from the German Stroke Registry—Endovascular Treatment database (GSR-ET 07/2015–04/2018; ClinicalTrials.gov Identifier: NCT03356392). Patients who were treated between June 2015 and December 2019 were included. The GSR-ET is an ongoing, open-label, prospective, multicenter registry of consecutively recruited EVT patients, with 25 participating stroke centers in Germany [16].
The inclusion criteria were: 1. acute ischemic stroke due to large-vessel occlusion in patients aged ≥ 18 years, 2. decision to perform EVT, 3. occlusion of the M1 segment of the middle cerebral artery (MCA), confirmed on digital subtraction angiography (DSA), and documented location of occlusion, 4. a final TICI score of 2b or 3 following EVT, 5. documented age, admission National Institutes of Health Stroke Scale (NIHSS) score, Alberta stroke program early CT score (ASPECTS), reported number of retrieval attempts in EVT, modified Rankin Scale (mRS) score at 90 days (mRS90), and available information on the administration or withdrawal of intravenous recombinant tissue plasminogen activator (iv-thrombolysis). Patients with spontaneous reperfusion before EVT were excluded from the analysis.
Study protocols and procedures were in accordance with the ethical guidelines of the leading ethics committee with additional approval from the local ethics committees of the participating hospitals. The study was conducted in compliance with the Declaration of Helsinki.
Data Acquisition and Management
Data acquisition was performed according to the previously described protocol of the GSR-ET [16, 17]. All data were collected by the local neurointerventionalists and neurologists and underwent standardized quality checks to control for consistency, plausibility, and completeness.
The ASPECTS was determined on admission nonenhanced computed tomography (CT) scans or diffusion-weighted imaging (in the case of magnetic resonance imaging, MRI). The TICI score was assessed on the final angiographic series by the treating neurointerventionalist. The number of retrieval attempts was documented following intervention by the neurointerventionalist and included both retrieval attempts with stent retriever devices as well as direct thrombus aspiration attempts. The modified Rankin Scale (mRS) score was assessed at 90 days. Good clinical outcome was defined as an mRS score at day 90 of 2 and was assessed as the primary outcome.
Statistical Analysis
All analyses were performed with the R statistics program (v. 3.6.3, R Core Team 2019, Vienna, Austria; RStudio IDE v. 1.1.463, Boston, MA, USA) [18]. Normally distributed variables are reported as mean and standard deviation (SD). Non-normally distributed data are reported as median and interquartile range (IQR). Categorical variables are reported as proportions. We performed multivariable logistic regression analysis with good clinical outcome (mRS score at day 90 of 2) as the dependent variable, adjusted for age, NIHSS and ASPECTS on admission, administration of iv thrombolysis, and the location of occlusion (occlusion of the proximal vs. distal M1 segment). The final TICI score and number of retrieval attempts were stratified into TICI 2b or TICI 3 following the first, second or ≥ third retrieval attempt. Figures were created using ggplot2 (R statistics program). P-values < 0.05 were considered significant.
Results
Baseline Characteristics
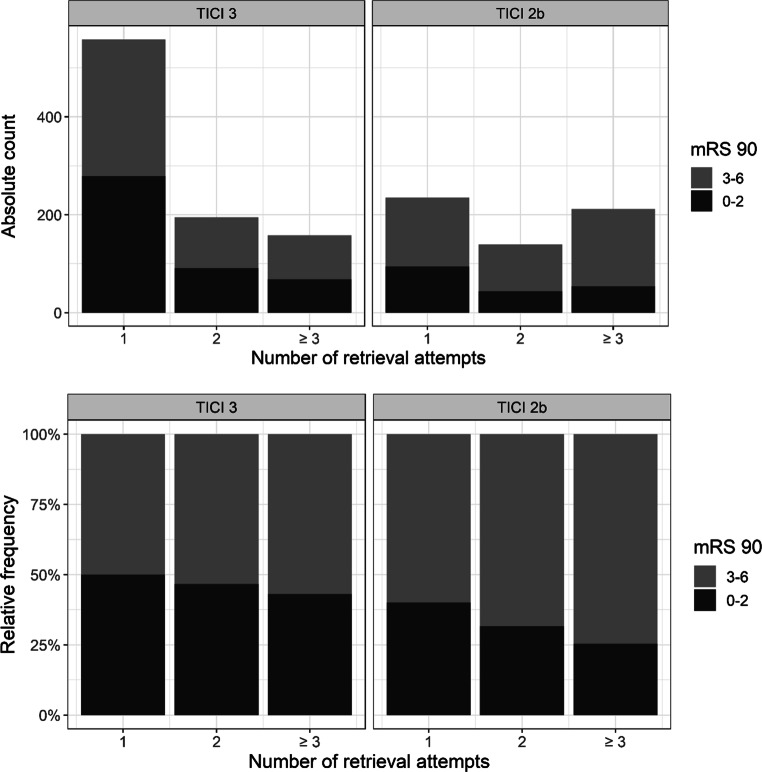
Basic characteristics, procedural and clinical outcome are displayed in Table 1. Of 6635 screened patients, 1497 fulfilled the inclusion criteria (Fig. 1). Of these, 808 patients (54.0%) were female. The mean age was 73.6 years (±13.3). The median NIHSS score on admission was 15 [11–18] and the median ASPECTS score on admission imaging was 9 [7–10]. The median number of device passes was 1 [1, 2]. Concomitant stenting of the cervical ICA was performed in 4.6% of patients. The median mRS at day 90 was 3 [1–5]. A good clinical outcome was observed in 629 (42%) patients. Mortality rate at day 90 was 24%. A final TICI score of 3 was observed in 911 patients (60.9%), and the remaining 586 patients had final TICI score of 2b (39.1%).
Table 1.
Basic characteristics, procedural and clinical outcome
| Variable | TICI 2b (N = 586) | TICI 3 (N = 911) |
|---|---|---|
| Age, years (mean, SD) | 72.8 (13.9) | 74.1 (12.9) |
| Female sex (%) | 318 (54.3%) | 491 (53.9%) |
| Hypertension (%) | 437 (74.8%) | 703 (77.5%) |
| Diabetes mellitus (%) | 124 (21.2%) | 192 (21.1%) |
| Dyslipidemia (%) | 198 (33.8%) | 378 (41.6%) |
| Atrial fibrillation (%) | 241 (41.3%) | 414 (45.5%) |
| Initial NIHSS score (median, Q1–Q3) | 15 [11–18] | 15 [10–18] |
| Pre-Stroke mRS score (median, Q1–Q3) | 0 [0–1] | 0 [0–1] |
| Initial ASPECTS (median, Q1–Q3) | 8 [7–10] | 9 [8–10] |
| Initial occlusion site (%) | ||
| Left hemisphere | 300 (51.3%) | 462 (50.8%) |
| Location of vessel occlusion (%) | ||
| M1 proximal | 355 (60.6%) | 572 (62.8%) |
| M1 distal | 234 (39.9%) | 346 (38%) |
| Intravenous tPA, n (%) | 317 (54.1%) | 464 (50.9%) |
| Onset to admission, min (median, Q1–Q3, n = 868 reported values) | 135 [62–201] | 105 [56.5–190] |
| Stroke etiology | ||
| Cardioembolism | 314 (54%) | 526 (58.1%) |
| Dissection | 2 (0.3%) | 9 (1%) |
| Atherosclerosis | 115 (19.8) | 174 (19.2%) |
| Other determined etiology | 28 (4.8%) | 36 (4%) |
| Unknown etiology | 123 (21.1%) | 160 (17.7%) |
| Onset to groin puncture, min (median, Q1–Q3, n = 861) | 195 [140–260] | 175 [126–246] |
| Groin puncture to final TICI, min (median, Q1–Q3, n = 1451) | 42 [26–67] | 33 [22–52] |
| Onset to reperfusion, min (median, Q1–Q3, n = 848) | 253 [188–320] | 219 [162–298] |
| Number of retrieval attempts (%) | ||
| 1 | 235 (40.1%) | 558 (61.2%) |
| 2 | 139 (23.7%) | 195 (21.4%) |
| 3 | 85 (14.5%) | 99 (10.9%) |
| 4 | 55 (9.4%) | 25 (2.7%) |
| 5 | 35 (6.0%) | 17 (1.9%) |
| 6 or more | 37 (6.3%) | 17 (1.9%) |
| Dissection/Perforation | 10 (1.7%) | 15 (1.7%) |
| Intracranial hemorrhage (ICH) | 16 (2.7%) | 12 (1.3%) |
| Modified Rankin Scale (mRS) score at 90 days (median, Q1–Q3) | 4 [2–6] | 3 [1–5] |
| Mortality (mRS = 6) | 109 (23%) | 145 (18.1%) |
| Functional independence (mRS ≤ 2) | 192 (32.8%) | 438 (48.1%) |
NIHSS National Institutes of Health Stroke Scale; mRS modified Rankin scale; ASPECTS Alberta Stroke Programme Early CT Score; M1 first middle cerebral artery segement; M2 second middle cerebral artery segment; tPA tissue Plasminogen Activator; TICI Thrombolysis in Cerebral Infarction score
Fig. 1.
Patient selection flowchart. LVO Large Vessel Occlusion, MT Mechanical Thrombectomy, M1 first middle cerebral artery segement, TICI Thrombolysis in Cerebral Infarction score, NIHSS National Institutes of Health Stroke Scale, rtPA recombinant tissue Plasminogen Activator, ASPECTS Alberta Stroke Programme Early CT Score, mRS90 modified Rankin scale at 90 days
Proportion of TICI 3 Reperfusions and Good Clinical Outcome by Retrieval Attempt
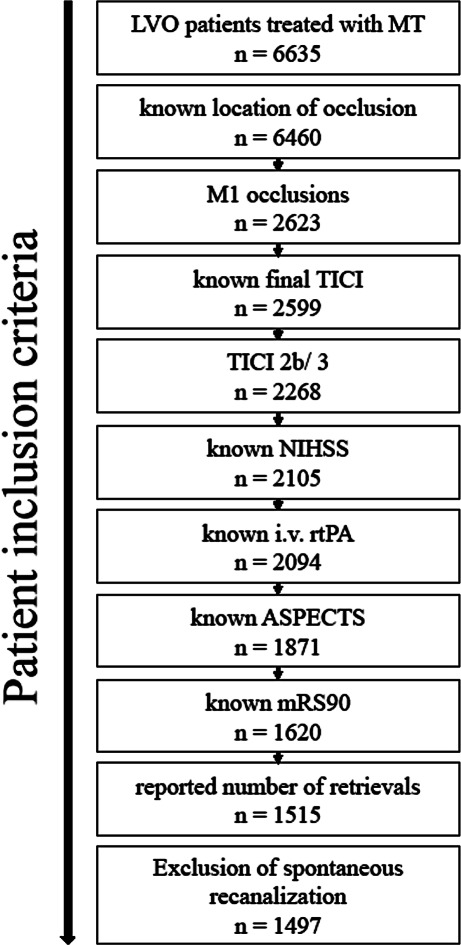
Of those patients who only underwent 1 retrieval attempt, a final TICI score of 3 was observed in 558 (70%) patients (Table 2). Of those who underwent 4 or more retrieval attempts, the rate of a final TICI 3 score declined to 31.3–32.6%. Fig. 2 depicts the rate of good clinical outcome by final TICI score and the total number of retrieval attempts performed. Of 558 patients with first pass TICI 3, 279 (50%) achieved a good clinical outcome. Of 235 patients with first pass TICI 2b, 94 (40%) achieved a good clinical outcome.
Table 2.
TICI grade and clinical outcome by number of retrievals
| Number of retrievals | 1 pass (n = 793) | 2 passes (n = 334) | ≥ 3 passes (n = 370) | |||
|---|---|---|---|---|---|---|
| Final TICI | TICI 2b | TICI 3 | TICI 2b | TICI 3 | TICI 2b | TICI 3 |
| n | 235 | 558 | 139 | 195 | 212 | 158 |
| % per pass | 29.7% | 70.3% | 41.6% | 58.4% | 57.3% | 42.7% |
| Functional independence n, (%) | 94 (40) | 279 (50) | 44 (32) | 91 (47) | 54 (26) | 68 (43) |
| Mortality n, (%) | 53 (23) | 118 (21) | 40 (29) | 43 (22) | 78 (37) | 33 (21) |
TICI Thrombolysis in Cerebral Infarction score
Fig. 2.
Rate of good clinical outcome (defined as mRS of 0–2 at day 90) by final TICI score and number of retrieval attempts. mRS 90 modified Rankin scale at day 90, TICI thrombolysis in cerebral iInfarction
Multivariable Analysis
The multivariable logistic regression analysis (adjusted for predictors, Table 3) revealed a negative association of older age (per-year increase OR 0.93, 95% CI 0.92–0.94, p < 2 × 10−16) and higher NIHSS score on admission (per-point increase OR 0.89, 95% CI 0.87–0.91, p < 2 × 10−16) with good clinical outcome. Furthermore, distal M1 occlusions were associated with a better outcome compared to proximal M1 occlusions (OR 1.54, 95% CI 1.19–1.98, p = 0.0008), as was iv-thrombolysis (OR 1.76, 95% CI 1.37–2.26, p = 8.72 × 10−6), and an ASPECTS of 10 (OR 2.42, 95% CI 1.46–4.10, p = 0.0007) or 8–9 (OR 2.07, 95% CI 1.26–3.47, p = 0.0047).
Table 3.
Summary table of the logistic regression model with good clinical outcome (mRS at day 90 of 0–2) as the dependent variable
| Predictor variable | OR (95% CI) | Coefficientb | P-value |
|---|---|---|---|
| Agea | 0.93 (0.92–0.94) | −0.07 | < 2 × 10−16 |
| NIHSSa | 0.89 (0.87–0.91) | −0.12 | < 2 × 10−16 |
| ASPECTS 0–5 | – | Ref | – |
| ASPECTS 6–7 | 1.43 (0.83–2.49) | 0.36 | 0.20 |
| ASPECTS 8–9 | 2.07 (1.26–3.47) | 0.73 | 0.0047 |
| ASPECTS 10 | 2.42 (1.46–4.10) | 0.89 | 0.0007 |
| Proximal M1 occlusion | – | Ref.- | – |
| Distal M1 occlusion | 1.54 (1.19–1.98) | 0.43 | 0.0008 |
| Iv-Thrombolysis | 1.76 (1.37–2.26) | 0.57 | 8.72 × 10−6 |
| TICI 2b at first pass | – | Ref.- | – |
| TICI 3 at first pass | 1.71 (1.18–2.47) | 0.53 | 0.0046 |
| TICI 2b at 2nd pass | 0.53 (0.31–0.89) | −0.63 | 0.017 |
| TICI 3 at 2nd pass | 1.55 (0.98–2.45) | 0.44 | 0.06 |
| TICI 2b at 3rd or more passes | 0.44 (0.27–0.70) | −0.82 | 0.0006 |
| TICI 3 at 3rd or more passes | 0.93 (0.57–1.50) | −0.07 | 0.76 |
| (Intercept) | 94.26 (36.36–249.61) | 4.55 | < 2 × 10−16 |
NIHSS National Institutes of Health Stroke Scale, ASPECTS Alberta stroke programme early CT score, TICI Thrombolysis in Cerebral Infarction score
aAge and NIHSS were treated as continuous variables; ASPECTS and TICI at the nth retrieval were treated as factors
bCoefficients are reported on the logit scale
First-pass TICI 2b patients comprised the reference group (Fig. 3). Patients with first-pass TICI 3 reperfusion had the highest odds of a good clinical outcome (OR 1.71, 95% CI 1.18–2.47, p = 0.0046). Second-pass TICI 2b had a significantly worse clinical outcome than first-pass TICI 2b (OR 0.53, 95% CI 0.31–0.89, p = 0.017), whereas second-pass TICI 3 was by trend better than first-pass TICI 2b with a borderline result (OR 1.55, 95% CI 0.98–2.45, p = 0.06). When examining patients who underwent ≥ 3 retrieval attempts, it was found that those who thus achieved TICI 2b had a significantly worse clinical outcome compared to first-pass TICI 2b (OR 0.44, 95% CI 0.27–0.70, p = 0.0006), whereas those who thus achieved TICI 3 had outcomes comparable to first-pass TICI 2b (OR 0.93, 95% CI 0.57–1.50, p = 0.76).
Fig. 3.
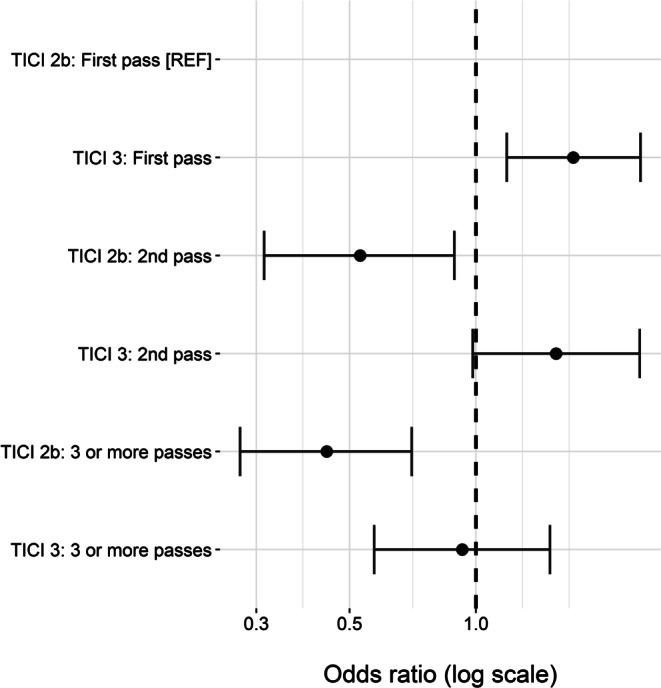
Odds ratio of good clinical outcome (defined as mRS of 0–2 at day 90) by final TICI score and number of retrieval attempts, adjusted for age, NIHSS score on admission, location of occlusion (proximal vs. distal segment of the MCA), ASPECTS on admission and iv-thrombolysis. mRS modified Rankin scale, TICI thrombolysis in cerebral infarction, MCA middle cerebral artery, ASPECTS Alberta stroke programme early CT score
Discussion
In the present study, we observed two effects: first, a final TICI score of 3 outperformed a final TICI score of 2b within each group of patients who underwent a certain number of retrieval attempts. Second, both TICI 3 and TICI 2b showed decreasing odds of good clinical outcome with increasing number of retrieval attempts. Hence, patients with late TICI 3 reperfusion (after 3 or more retrievals) and patients with early TICI 2b reperfusion (after the first retrieval) showed comparable odds of good clinical outcome. Furthermore, the rate of TICI 3 was ~70% in patients who underwent 1 attempt and decreased to ~30% for patients who underwent 4 or more retrieval attempts.
In our patient cohort, the proportion of TICI 3 amongst all patients with sufficient reperfusion (TICI 2b–3) was 61%, which is slightly higher than in the ESCAPE-NA 1 trial control group (259/480 patients, 54%) [19]. The difference could be explained by the fact that ESCAPE-NA 1 had a central imaging core laboratory, while our registry used self-reported final TICI scores, which are potentially subject to bias [17]. Furthermore, we only included occlusions of the M1 segment of the MCA, which showed higher rates of reperfusion than occlusions of the ICA [15].
An improved clinical outcome after TICI 3 vs. TICI 2b reperfusion has been previously described [3, 4], as has decreased infarct growth after TICI 3 reperfusion [20]. Dargazanli et al. reported rates of functional independence of 71.7% vs. 50.5% for TICI 3 vs. TICI 2b [4], while Chamorro et al. reported rates of functional independence of 67.6% vs. 56.8% [20]. In this study, we observed rates of 48.1% vs. 32.8% for TICI 3 and 2b, respectively. Furthermore, as previously described [22], patients treated with intravenous thrombolysis (rtPA) prior to mechanical thrombectomy were more likely to achieve higher reperfusion rates and subsequently favorable outcome as demonstrated in Table 1, [21] while a recently conducted meta-analysis pooling 20 studies with more than 5000 patients conducted by Kaesmacher et al. favored neither treatment approach [22]. The overall comparatively lower rates of good clinical outcome in our GSR-ET cohort have been previously described and discussed [17]. Despite this, we found a similar reduction in the rate of good clinical outcome in patients with TICI 2b compared to TICI 3.
In a large multicenter cohort of patients with M1 occlusions, we observed the highest odds of good clinical outcome in patients with TICI 3 reperfusion following a single retrieval, confirming the previously described first-pass effect [23, 24]. Furthermore, when comparing patients who underwent a certain number of retrieval attempts, we found higher odds of good clinical outcome after TICI 3 reperfusion compared to TICI 2b. García-Tornel et al. analyzed the association of final TICI score and number of retrieval attempts in detail [25]. They also observed an overall superior clinical outcome after TICI 3 compared to TICI 2b. In contrast to our findings, they reported comparable rates of good clinical outcome in patients who achieved TICI 3 during the first three passes, with declining odds only being observed following the fourth retrieval attempt. On the other hand, they reported a negative impact of each retrieval attempt on outcome, beginning with the second pass in patients who achieved TICI 2b, which we were able to confirm; however, this part of their analysis was not adjusted for confounders and included a comparatively small number of patients. In our study the odds for a good clinical outcome decreased with the second pass in patients with TICI 2b reperfusion and with the third pass in patients with TICI 3 reperfusion. Due to this effect, the odds of good clinical outcome were comparable between late TICI 3 and early TICI 2b reperfusion.
Our analysis suffers from an important limitation. García-Tornel et al. described the phenomenon of sudden recanalization, defined as a variation of TICI score from 0–1 to 2b–3 in a single pass, and demonstrated that sudden recanalization is associated with superior clinical outcome, even when achieved after multiple retrieval attempts [26]. In the present study recanalization success of each retrieval attempt could not be evaluated due to limitations of data collection, and we therefore cannot differentiate between sudden and stepwise recanalization. Perhaps most importantly, we were unable to further differentiate if patients with late TICI 2b/3 had TICI 0–2a or TICI 2b during the first retrieval attempts. Furthermore, due to the retrospective design of this data collection, TICI 2c was not evaluated separately but is included in the TICI 2b classification.
Other limitations are as follows: the number of retrieval attempts, as well as the final TICI score, was reported by the treating neurointerventionalist and was not validated by a central imaging core laboratory [6]; the technical approaches differed according to the local standard of clinical routine at the different centers and a substantial proportion of patients (1108 of 2623 patients with M1 occlusions, 42.2%) had to be excluded from the analysis due to missing data.
From a practical point of view, the most important question is whether or not to continue with mechanical thrombectomy in the case of TICI 2b reperfusion, especially after the first pass. One could argue that if late TICI 3 is as good as early TICI 2b, the former should always be strived for; however, we describe declining rates of TICI 3 reperfusion with subsequent attempts, as has also been previously reported [26]. Furthermore, while TICI 3 after the second pass showed a tendency towards better outcome compared to first-pass TICI 2b (marginally missing the significance threshold), TICI 3 after 3 or more passes was comparable to first-pass TICI 2b. In addition, with each further retrieval attempt, the patient has an increasing risk of a late TICI 2b result, which was associated with inferior clinical outcome compared to first-pass TICI 2b. Hence, perfect could indeed be the enemy of good. However, due to the beforementioned limitations, a thorough documentation of TICI grade after each retrieval attempt in a large patient cohort would be needed to investigate whether or not there is a significant benefit of further thrombectomy attempts after first-pass TICI 2b has been achieved. Albeit technically challenging, a randomized controlled trial would be needed to ultimately clarify this question.
Our data suggest that each additional retrieval attempt has to be undertaken with caution, taking into account a variety of factors, including the size of the perfusion deficit, eligibility of iv thrombolysis, and the location of the persisting occlusion [27].
Conclusion
First-pass TICI 2b was superior to TICI 2b after ≥ 2 retrievals and comparable to TICI 3 at ≥ 3 retrievals. Therefore, the negative effects of further retrieval attempts, such as declining odds of good outcome in late TICI 2b, have to be considered.
Coinvestigators
List of all coinvestigators of the German Stroke Registry Steering Committee was blinded for review.
Supplementary Information
Fig. 4: Rate of TICI 3 reperfusions stratified by total of retrieval attempts (dark gray: final TICI score of 3, light grey: final TICI score of 2b)
Funding
Open Access funding enabled and organized by Projekt DEAL.
Conflict of interest
G. Thomalla: unrelated consultancy for Acandis, Stryker; payment for lectures including service on “speakers bureaus”: Bayer, Bristol Myers Squibb, Boehringer Ingelheim, Daiichi Sankyo. J. Fiehler: unrelated consultancy for Acandis, Boehringer Ingelheim, Cerenovus, Covidien, Evasc Neurovascular, MD-Clinicals, Medtronic, Medina, MicroVention, Penumbra, Route 92 Medical, Stryker, Transverse Medical; grants/grants pending: MicroVention, Medtronic, Stryker, Cerenovus. M.E. Maros: funding from the German Federal Ministry for Economic Affairs and Energy within the scope of Zentrales Innovationsprogramm Mittelstand (ZF 4514602TS8). Unrelated consultancy for Smart Reporting and Siemens Healthineers. F. Flottmann, N. van Horn, R. McDonough, M. Deb-Chatterji, A. Alegiani, U. Hanning and C. Brekenfeld declare that they have no competing interests.
Footnotes
The authors F. Flottmann and N. van Horn contributed equally to the manuscript.
References
- 1.Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Dávalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millán M, Davis SM, Roy D, Thornton J, Román LS, Ribó M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG, HERMES collaborators Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 2.Yoo AJ, Simonsen CZ, Prabhakaran S, Chaudhry ZA, Issa MA, Fugate JE, Linfante I, Liebeskind DS, Khatri P, Jovin TG, Kallmes DF, Dabus G, Zaidat OO. Cerebral Angiographic Revascularization Grading Collaborators. Refining angiographic biomarkers of revascularization: improving outcome prediction after intra-arterial therapy. Stroke. 2013;44:2509–2512. doi: 10.1161/STROKEAHA.113.001990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kleine JF, Wunderlich S, Zimmer C, Kaesmacher J. Time to redefine success? TICI 3 versus TICI 2b recanalization in middle cerebral artery occlusion treated with thrombectomy. J Neurointerv Surg. 2017;9:117–121. doi: 10.1136/neurintsurg-2015-012218. [DOI] [PubMed] [Google Scholar]
- 4.Dargazanli C, Consoli A, Barral M, Labreuche J, Redjem H, Ciccio G, Smajda S, Desilles JP, Taylor G, Preda C, Coskun O, Rodesch G, Piotin M, Blanc R, Lapergue B. Impact of Modified TICI 3 versus Modified TICI 2b Reperfusion Score to Predict Good Outcome following Endovascular Therapy. AJNR Am J Neuroradiol. 2017;38:90–96. doi: 10.3174/ajnr.A4968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu X, Khunte M, Gandhi D, Matouk C, Hughes DR, Sanelli P, Malhotra A. Implications of achieving TICI 2b vs TICI 3 reperfusion in patients with ischemic stroke: a cost-effectiveness analysis. J Neurointerv Surg. 2020;12:1161–1165. doi: 10.1136/neurintsurg-2020-015873. [DOI] [PubMed] [Google Scholar]
- 6.Goyal M, Fargen KM, Turk AS, Mocco J, Liebeskind DS, Frei D, Demchuk AM. 2C or not 2C: defining an improved revascularization grading scale and the need for standardization of angiography outcomes in stroke trials. J Neurointerv Surg. 2014;6:83–86. doi: 10.1136/neurintsurg-2013-010665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dargazanli C, Fahed R, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, Saleme S, Costalat V, Bracard S, Desal H, Mazighi M, Consoli A, Piotin M, Lapergue B, ASTER Trial Investigators Modified Thrombolysis in Cerebral Infarction 2C/Thrombolysis in Cerebral Infarction 3 Reperfusion Should Be the Aim of Mechanical Thrombectomy. Insights From the ASTER Trial (Contact Aspiration Versus Stent Retriever for Successful Revascularization) Stroke. 2018;49:1189–1196. doi: 10.1161/STROKEAHA.118.020700. [DOI] [PubMed] [Google Scholar]
- 8.Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, Schellinger PD, Toni D, de Vries J, White P. European Stroke Organisation (ESO) – European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. 2019;11:535–538. doi: 10.1136/neurintsurg-2018-014568. [DOI] [PubMed] [Google Scholar]
- 9.Seker F, Pfaff J, Wolf M, Ringleb PA, Nagel S, Schönenberger S, Herweh C, Möhlenbruch MA, Bendszus M, Pham M. Correlation of Thrombectomy Maneuver Count with Recanalization Success and Clinical Outcome in Patients with Ischemic Stroke. AJNR Am J Neuroradiol. 2017;38:1368–1371. doi: 10.3174/ajnr.A5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flottmann F, Leischner H, Broocks G, Nawabi J, Bernhardt M, Faizy TD, Deb-Chatterji M, Thomalla G, Fiehler J, Brekenfeld C. Recanalization Rate per Retrieval Attempt in Mechanical Thrombectomy for Acute Ischemic Stroke. Stroke. 2018;49:2523–2525. doi: 10.1161/STROKEAHA.118.022737. [DOI] [PubMed] [Google Scholar]
- 11.Baek JH, Kim BM, Heo JH, Nam HS, Kim YD, Park H, Bang OY, Yoo J, Kim DJ, Jeon P, Baik SK, Suh SH, Lee KY, Kwak HS, Roh HG, Lee YJ, Kim SH, Ryu CW, Ihn YK, Kim B, Jeon HJ, Kim JW, Byun JS, Suh S, Park JJ, Lee WJ, Roh J, Shin BS. Number of Stent Retriever Passes Associated With Futile Recanalization in Acute Stroke. Stroke. 2018;49:2088–2095. doi: 10.1161/STROKEAHA.118.021320. [DOI] [PubMed] [Google Scholar]
- 12.Bai Y, Pu J, Wang H, Yang D, Hao Y, Xu H, Zhang M, Geng Y, Wan Y, Wang W, Zhang H, Zi W, Liu X, Xu G, ACTUAL Investigators Impact of Retriever Passes on Efficacy and Safety Outcomes of Acute Ischemic Stroke Treated with Mechanical Thrombectomy. Cardiovasc Intervent Radiol. 2018;41:1909–1916. doi: 10.1007/s00270-018-2022-0. [DOI] [PubMed] [Google Scholar]
- 13.Bourcier R, Saleme S, Labreuche J, Mazighi M, Fahed R, Blanc R, Gory B, Kyheng M, Marnat G, Bracard S, Desal H, Consoli A, Piotin M, Lapergue B, ASTER Trial Investigators More than three passes of stent retriever is an independent predictor of parenchymal hematoma in acute ischemic stroke. J Neurointerv Surg. 2019;11:625–629. doi: 10.1136/neurintsurg-2018-014380. [DOI] [PubMed] [Google Scholar]
- 14.Yeo LLL, Bhogal P, Gopinathan A, Cunli Y, Tan B, Andersson T. Why Does Mechanical Thrombectomy in Large Vessel Occlusion Sometimes Fail? : A Review of the Literature. Clin Neuroradiol. 2019;29:401–414. doi: 10.1007/s00062-019-00777-1. [DOI] [PubMed] [Google Scholar]
- 15.Flottmann F, Broocks G, Faizy TD, McDonough R, Watermann L, Deb-Chatterji M, Thomalla G, Herzberg M, Nolte CH, Fiehler J, Leischner H, Brekenfeld C, GSR investigators Factors Associated with Failure of Reperfusion in Endovascular Therapy for Acute Ischemic Stroke: A Multicenter Analysis. Clin Neuroradiol. 2021;31:197–205. doi: 10.1007/s00062-020-00880-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alegiani AC, Dorn F, Herzberg M, Wollenweber FA, Kellert L, Siebert E, Nolte CH, von Rennenberg R, Hattingen E, Petzold GC, Bode FJ, Pfeilschifter W, Schäfer JH, Wagner M, Röther J, Eckert B, Kraft P, Pham M, Boeckh-Behrens T, Wunderlich S, Bernkopf K, Reich A, Wiesmann M, Mpotsaris A, Psychogios M, Liman J, Maier I, Berrouschot J, Bormann A, Limmroth V, Spreer J, Petersen M, Krause L, Lowens S, Kraemer C, Zweynert S, Lange KS, Thonke S, Kastrup A, Papanagiotou P, Alber B, Braun M, Fiehler J, Gerloff C, Dichgans M, Thomalla G. Systematic evaluation of stroke thrombectomy in clinical practice: The German Stroke Registry Endovascular Treatment. Int J Stroke. 2019;14:372–380. doi: 10.1177/1747493018806199. [DOI] [PubMed] [Google Scholar]
- 17.Wollenweber FA, Tiedt S, Alegiani A, Alber B, Bangard C, Berrouschot J, Bode FJ, Boeckh-Behrens T, Bohner G, Bormann A, Braun M, Dorn F, Eckert B, Flottmann F, Hamann GF, Henn KH, Herzberg M, Kastrup A, Kellert L, Kraemer C, Krause L, Lehm M, Liman J, Lowens S, Mpotsaris A, Papanagiotou P, Petersen M, Petzold GC, Pfeilschifter W, Psychogios MN, Reich A, von Rennenberg R, Röther J, Schäfer JH, Siebert E, Siedow A, Solymosi L, Thonke S, Wagner M, Wunderlich S, Zweynert S, Nolte CH, Gerloff C, Thomalla G, Dichgans M, Fiehler J. Functional Outcome Following Stroke Thrombectomy in Clinical Practice. Stroke. 2019;50:2500–2506. doi: 10.1161/STROKEAHA.119.026005. [DOI] [PubMed] [Google Scholar]
- 18.R Core Team . A language and environment for statistical computing. 2020. [Google Scholar]
- 19.Hill MD, Goyal M, Menon BK, Nogueira RG, McTaggart RA, Demchuk AM, Poppe AY, Buck BH, Field TS, Dowlatshahi D, van Adel BA, Swartz RH, Shah RA, Sauvageau E, Zerna C, Ospel JM, Joshi M, Almekhlafi MA, Ryckborst KJ, Lowerison MW, Heard K, Garman D, Haussen D, Cutting SM, Coutts SB, Roy D, Rempel JL, Rohr AC, Iancu D, Sahlas DJ, Yu AYX, Devlin TG, Hanel RA, Puetz V, Silver FL, Campbell BCV, Chapot R, Teitelbaum J, Mandzia JL, Kleinig TJ, Turkel-Parrella D, Heck D, Kelly ME, Bharatha A, Bang OY, Jadhav A, Gupta R, Frei DF, Tarpley JW, McDougall CG, Holmin S, Rha JH, Puri AS, Camden MC, Thomalla G, Choe H, Phillips SJ, Schindler JL, Thornton J, Nagel S, Heo JH, Sohn SI, Psychogios MN, Budzik RF, Starkman S, Martin CO, Burns PA, Murphy S, Lopez GA, English J, Tymianski M, ESCAPE-NA1 Investigators Efficacy and safety of nerinetide for the treatment of acute ischaemic stroke (ESCAPE-NA1): a multicentre, double-blind, randomised controlled trial. Lancet. 2020;395:878–887. doi: 10.1016/S0140-6736(20)30258-0. [DOI] [PubMed] [Google Scholar]
- 20.Chamorro Á, Blasco J, López A, Amaro S, Román LS, Llull L, Renú A, Rudilosso S, Laredo C, Obach V, Urra X, Planas AM, Leira EC, Macho J. Complete reperfusion is required for maximal benefits of mechanical thrombectomy in stroke patients. Sci Rep. 2017;7:11636. doi: 10.1038/s41598-017-11946-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Maria F, Mazighi M, Kyheng M, Labreuche J, Rodesch G, Consoli A, Coskun O, Gory B, Lapergue B. Intravenous Thrombolysis Prior to Mechanical Thrombectomy in Acute Ischemic Stroke: Silver Bullet or Useless Bystander? J Stroke. 2018;20:385–393. doi: 10.5853/jos.2018.01543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaesmacher J, Mordasini P, Arnold M, López-Cancio E, Cerdá N, Boeckh-Behrens T, Kleine JF, Goyal M, Hill MD, Pereira VM, Saver JL, Gralla J, Fischer U. Direct mechanical thrombectomy in tPA-ineligible and -eligible patients versus the bridging approach: a meta-analysis. J Neurointerv Surg. 2019;11:20–27. doi: 10.1136/neurintsurg-2018-013834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE, Mueller-Kronast N, English JD, Dabus G, Malisch TW, Marden FA, Bozorgchami H, Xavier A, Rai AT, Froehler MT, Badruddin A, Nguyen TN, Taqi MA, Abraham MG, Yoo AJ, Janardhan V, Shaltoni H, Novakovic R, Abou-Chebl A, Chen PR, Britz GW, Sun CJ, Bansal V, Kaushal R, Nanda A, Nogueira RG. First Pass Effect: A New Measure for Stroke Thrombectomy Devices. Stroke. 2018;49:660–666. doi: 10.1161/STROKEAHA.117.020315. [DOI] [PubMed] [Google Scholar]
- 24.Nikoubashman O, Dekeyzer S, Riabikin A, Keulers A, Reich A, Mpotsaris A, Wiesmann M. True First-Pass Effect. Stroke. 2019;50:2140–2146. doi: 10.1161/STROKEAHA.119.025148. [DOI] [PubMed] [Google Scholar]
- 25.García-Tornel Á, Requena M, Rubiera M, Muchada M, Pagola J, Rodriguez-Luna D, Deck M, Juega J, Rodríguez-Villatoro N, Boned S, Olivé-Gadea M, Tomasello A, Hernández D, Molina CA, Ribo M. When to Stop. Stroke. 2019;50:1781–1788. doi: 10.1161/STROKEAHA.119.025088. [DOI] [PubMed] [Google Scholar]
- 26.García-Tornel Á, Rubiera M, Requena M, Muchada M, Pagola J, Rodriguez-Luna D, Deck M, Juega J, Rodríguez-Villatoro N, Boned S, Olivé-Gadea M, Tomasello A, Piñana C, Hernández D, Molina CA, Ribo M. Sudden Recanalization: A Game-Changing Factor in Endovascular Treatment of Large Vessel Occlusion Strokes. Stroke. 2020;51:1313–1316. doi: 10.1161/STROKEAHA.119.028787. [DOI] [PubMed] [Google Scholar]
- 27.Goyal M, Ospel JM, Menon BK, Hill MD. MeVO: the next frontier? J Neurointerv Surg. 2020;12:545–547. doi: 10.1136/neurintsurg-2020-015807. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig. 4: Rate of TICI 3 reperfusions stratified by total of retrieval attempts (dark gray: final TICI score of 3, light grey: final TICI score of 2b)