Abstract
Adults with cardiac implantable electronic devices (CIEDs) implanted at an early age constitute a specific group of patients undergoing transvenous lead extraction (TLE). The aim of this study is to assess safety and effectiveness of TLE in young adults. A comparative analysis of two groups of patients undergoing transvenous lead extraction was performed: 126 adults who were 19–29 years old at their first CIED implantation (early adulthood) and 2659 adults who were > 40 years of age at first CIED implantation and < 80 years of age at the time of TLE (middle-age/older adulthood). CIED-dependent risk factors were more common in young adults, especially longer implant duration (169.7 vs. 94.0 months). Moreover younger age of patients at first implantation, regardless of the dwell lead time, is a factor contributing to the greater development of connective tissue proliferation on the leads (OR 2.587; p < 0.001) and adhesions of the leads with the heart structures (OR 3.322; p < 0.001), which translates into worse TLE results in this group of patients. The complexity of procedures and major complications were more common in younger group (7.1 vs. 2.0%; p < 0.001), including hemopericardium (4.8 vs 1.3; p = 0.006) and TLE-induced tricuspid valve damage (3.2 vs.0.3%; p < 0.001). Among middle-aged/older adults, there were 7 periprocedural deaths: 6 related to the TLE procedure and one associated with indications for lead removal. No fatal complications of TLE were reported in young adults despite the above-mentioned differences (periprocedural mortality rate was comparable in study groups 0.3% vs 0.0%; p = 0.739). Predictors of TLE-associated major complications and procedure complexity were more likely in young adults compared with patients aged > 40 to < 80 years. In younger aged patients prolonged extraction duration and higher procedure complexity were combined with a greater need for second line tools. Both major and minor complications were more frequent in young adults, with hemopericardium and tricuspid valve damage being predominant.
Subject terms: Cardiology, Medical research, Risk factors
Introduction
Permanent cardiac pacing therapy (PM, ICD/CRT) is prescribed predominantly to older patients. Only a small proportion of cardiac implantable electronic devices (CIED) are implanted in subjects aged less than 40 years. Children and juveniles with leads implanted in childhood form a specific group of patients from the viewpoint of lead management and lead extraction in particular. Based on previous reports, the importance of rapid lead-induced tissue scarring and calcification has been emphasized1–7. The formation of this fibrous capsule in combination with somatic growth is a common source of mechanical lead damage and more difficult extraction in children than in adults5–10. To the best of our knowledge there is only one study addressing the peculiarities of lead extraction in young adults (< 40 years) compared with patients ≥ 40 years10. In the recent guidelines older age is considered as a risk factor for TLE-associated major complications and periprocedural mortality11–13. Life expectancy in young CIED carriers is long or very long and the guidelines recommend avoiding lead abandonment in this age group11–13.
The problem of lead extraction in young patients or older adults with CIED implanted in childhood is relatively unknown, and therefore requires detailed research. The purpose of the study was to compare effectiveness, complexity and major complications of transvenous lead extraction in patients aged 19–29 at the time of lead implantation and in subjects aged 40–80 at lead implantation/extraction. Patients with leads implanted in childhood and patients with TLE performed after the age of 80 were not included in this study because of age-specific differences.
Methods
Study population
This post-hoc analysis used clinical data of 3344 patients who underwent transvenous lead extraction between March, 2006 and September, 2020. All information relating to patients and procedures was entered into the computer on an ongoing basis. For the purposes of comparison the cohort was divided into two groups: group A consisting of 126 adult patients who were 19–29 years old, mean age 23.6 ± 3.1, at their first CIED implantation (mean age at extraction 37.9 ± 9.2) and group B comprised of 2659 adults who were > 40 years of age, mean age 58.4 ± 11.5, at the time of their CIED implantation and < 80 years of age, mean age 66.5 ± 9.4, at the time of transvenous lead extraction. No other patient exclusion criteria were used. Some patients with very old leads or abnormal lead route (strained, looped) were referred for elective system replacement at our tertiary reference care center.
This study analyzed demographic, clinical, CIED-related and procedure-related (including success and complications) data. The SAFeTY TLE score was used to predict the risk of major complications14, with an online calculator available at http://alamay2.linuxpl.info/kalkulator/.
Lead extraction procedure
Lead extraction procedures were performed using mechanical systems such as polypropylene Byrd dilator sheaths (Cook® Medical, Leechburg, PA, USA), mainly via the implant vein. If technical difficulties arose, alternative venous approaches and/or additional tools such as Evolution (Cook® Medical, USA), TightRail (Spectranetix, USA) sheaths, lassos, basket catheters were utilized. Laser cutting sheaths were not used. In both groups lead extraction was performed by a team consisting of the same experienced operator, a second operator having experience with pacing therapy and a cardiac surgeon, whereas an anesthesiologist and echocardiographer were often but not always present during the procedure.
Definitions
Indications for TLE and type of periprocedural complications were defined according to the 2017 HRS Expert Consensus Statement on Cardiovascular Implantable Electronic Device Lead Management and Extraction12.
Extraction procedures of lead(s) older than one year were defined according to the guidelines on management of lead-related complications (HRS 2009 and 2017, and EHRA 201811–13.
Procedural success was defined as removal of all targeted leads and all lead material from the vascular space, without any permanently disabling complication or procedure-related death11–13.
Clinical success was defined as removal of all targeted leads or retention of a small (< 4 cm) portion of the lead that did not negatively impact the outcome goals of the procedure or permanently disabled the patient (only in patients with noninfectious indications for TLE)11–13.
Partial radiographic success was defined as leaving a lead tip or a fragment of lead less than 4 cm11–13.
Statistical analysis
The Shapiro–Wilk test showed that most continuous variables were normally distributed. For uniformity, all continuous variables are presented as the mean ± standard deviation. The categorical variables are presented as numbers and percentages. The significance of differences between groups was determined using the nonparametric Chi2 test with Yates correction or because of the large disproportion in the size of the compared groups with the Mann–Whitney U test, as appropriate.
To determine which parameters have impact on the major complications (MC) occurrence and clinical and procedural success the following variables were included in the regression analysis of risk factors of major complication and prognostic factors of clinical and procedural success: patient’s age during the first CIED implantation, patients age during TLE, gender, value of left ventricle ejection fraction, cteatinine level, body mass index, Charlson’s comorbidity index, indications for TLE (infectious vs non-infectious), kind of CIED system (conventional, or with HV lead), presence/extraction of abandoned leads, number of leads in the heart (number of leads in the system + number of abandoned leads), number of CIED—related procedures before TLE and dwell time of the oldest extracted lead.
The variables with p < 0.1 in the one-variable regression analysis are presented in Table 5 and were included in the multivariate analysis. Due to the small number of major complications (n = 9), in group A, a two-variable analysis was performed comparing the dwell time of the oldest extracted leads with other variables, which achieved statistical significance (p < 0.1) under univariable analysis.
Table 5.
Risk factors of major complication and prognostic factors of clinical and procedural success. Results of uni- and multi-variable regression.
| Group A | Univariable model regression | Multivariable model regression | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Major complications | ||||||
| Patient age during TLE [year] | 1.124 | 1.045–1.210 | P < 0.001 | 1.053 (1) | 0.864–1.283 | P = 0.605 |
| Female | 4.375 | 0.858–22.31 | P = 0.073 | 3.862 (2) | 0.681–21.91 | P = 0.123 |
| Creatinine concentration [mg %] | 0.021 | 0.000–1.505 | P = 0.073 | 0.028 (3) | 0.003–2.596 | P = 0.118 |
| Extraction of abandoned lead | 5.050 | 1.208–21.11 | P = 0.025 | 1.449 (4) | 0.244–8.612 | P = 0.680 |
| Dwell time of the oldest extracted lead [year] | 1.136 | 1.049–1.230 | P = 0.002 |
1.078 (1) 1.137 (2) 1.136 (3) 1.124 (4) |
0.871–1.334 1.044–1.236 1.045–1.236 1.025–1.234 |
P = 0.485 P = 0.003 P = 0.002 P = 0.012 |
| Group B | Univariable regression | Multivariable regression | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Patient’s age at first CIED implantation [year] | 0.949 | 0.916–0.983 | P = 0.004 | 0.992 | 0.949–1.038 | P = 0.740 |
| Female gender | 4.314 | 2.130–8.740 | P < 0.001 | 3.361 | 1.618–6.984 | P < 0.001 |
| Extraction of HV lead | 0.257 | 0.091–0.728 | P = 0.011 | 0.561 | 0.186–1.687 | P = 0.303 |
| Presence of abandoned lead | 4.001 | 2.016–7.942 | P < 0.001 | 1.308 | 0.498–3.439 | P = 0.586 |
| Number of leads in the heart before TLE | 1.670 | 1.166–2.392 | P = 0.005 | 1.148 | 0.716–1.838 | P = 0.567 |
| Number of previously CIED- related procedures before TLE | 1.770 | 1.469–2.132 | P < 0.001 | 1.303 | 0.977–1.736 | P = 0.071 |
| Dwell time of the oldest extracted lead [year] | 1.157 | 1.111–1.205 | P < 0.001 | 1.092 | 1.026–1.162 | P = 0.006 |
| Group A | Univariable regression | Multivariable regression | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Clinical success | ||||||
| Patient’s age during TLE | 0.922 | 0.859–0.990 | P = 0.024 | 0.955 | 0.747–1.220 | P = 0.708 |
| Creatinine concentration [mg %] | 48.91 | 0.535–4474 | P = 0.088 | 3.137 | 0.019–521.1 | P = 0.658 |
| Infective TLE indications | 0.253 | 0.058–1.099 | P = 0.064 | 0.426 | 0.045–4.053 | P = 0.453 |
| Presence of abandoned leads | 0.155 | 0.035–0.694 | P = 0.014 | 0.342 | 0.011–10.70 | P = 0.537 |
| Number of the leads in the heart | 0.359 | 0.155–0.834 | P = 0.016 | 2.276 | 0.395–13.12 | P = 0.353 |
| Number of previously CIED related procedures | 0.408 | 0.246–0.675 | P < 0.001 | 0.328 | 0.119–0.907 | P = 0.030 |
| Dwell time of the oldest extracted lead [year] | 0.923 | 0.856–0.955 | P = 0.035 | 1.107 | 0.851–1.440 | P = 0.443 |
| Group B | Univariable regression | Multivariable regression | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Patient’s age at first CIED implantation [year] | 1.043 | 1.011–1.075 | P = 0.008 | 1.015 | 0.978–1.054 | P = 0.425 |
| Left ventricle ejection fraction | 0.978 | 0.959–0.998 | P = 0.029 | 0.988 | 0.964–1.013 | P = 0.359 |
| Infectious indications for TLE | 0.121 | 0.060–0.244 | P < 0.001 | 0.119 | 0.057–0.250 | P < 0.001 |
| Extraction of HV lead | 3.015 | 1.348–6.742 | P = 0.007 | 1.706 | 0.646–4.505 | P = 0.281 |
| Presence of abandoned lead | 0.286 | 0.153–0.534 | P < 0.001 | 1.555 | 0.648–3.728 | P = 0.322 |
| Number of leads in the heart before TLE | 0.495 | 0.366–0.669 | P < 0.001 | 0.592 | 0.390–0.899 | P = 0.014 |
| Number of previously CIED—related procedures before TLE | 0.564 | 0.476–0.668 | P < 0.001 | 0.854 | 0.663–1.101 | P = 0.223 |
| Dwell time of the oldest extracted lead [year] | 0.896 | 0.863–0.930 | P < 0.001 | 0.916 | 0.864–0.971 | P = 0.003 |
| Group A | Univariable regression | Multivariable regression | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Procedural success | ||||||
| Patient’s age during TLE | 0.936 | 0.888–0.986 | P = 0.012 | 0.898 | 0.628–1.283 | P = 0.551 |
| Patient’s age at first CIED implantation | 1.189 | 0.998–1.418 | P = 0.051 | 1.353 | 0.888–2.064 | P = 0.156 |
| Pacemaker (AAI, VVI, DDD, VDD, CRT-P) | 0.220 | 0.074–0.645 | P = 0.006 | 0.249 | 0.073–0.854 | P = 0.025 |
| Number of previously CIED—related procedures before TLE | 0.530 | 0.370–0.761 | P < 0.001 | 0.586 | 0.321–1.068 | P = 0.078 |
| Dwell time of the oldest extracted lead [year] | 0.914 | 0.863–0.968 | P = 0.002 | 1.081 | 0.777–1.502 | P = 0.642 |
| Group B | Univariable regression | Multivariable regression | ||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Patient’s age at first CIED implantation | 1.045 | 1.022–1.068 | P < 0.001 | 1.009 | 0.983–1.037 | P = 0.491 |
| Left ventricle ejection fraction [1%] | 0.984 | 0.971–0.998 | P = 0.025 | 0.992 | 0.977–1.007 | P = 0.307 |
| Extraction of HV lead | 2.470 | 1.341–4.548 | P = 0.004 | 1.339 | 0.676–2.653 | P = 0.403 |
| Presence of abandoned lead | 0.310 | 0.195–0.492 | P < 0.001 | 0.980 | 0.511–1.882 | P = 0.953 |
| Number of leads in the heart before TLE | 0.573 | 0.455–0.721 | P < 0.001 | 0.738 | 0.540–1.008 | P = 0.056 |
| Number of procedures before TLE | 0.607 | 0.530–0.695 | P < 0.001 | 0.809 | 0.668–0.981 | P = 0.031 |
| Dwell time of the oldest extracted lead [year] | 0.892 | 0.867–0.917 | P < 0.001 | 0.929 | 0.892–0.976 | P < 0.001 |
TLE transvenous lead extraction, (1), (2), (3), (4)—pairs of variables compared in the two-variable regression analysis, CIED cardiac implantable electronic device, HV defibrillating (high voltage) lead, AAI pacemaker system with the tip of lead in right atrium, VVI pacemaker system with the tip of lead in right ventricle, DDD dual chamber pacemaker system, VDD pacemaker system with the tip of integrated lead in right ventricle, CRT-P cardiac resynchronisation therapy pacemaker.
In order to assess the significance of the influence of the patient's young age during first implantation, and the dwell lead time a binary regression analysis was performed too. To analysis age of patients between 19 and 29 years during first CIED implantation and the dwell lead time above 10 years were included. Impact of above variables on the major complications occurrence, achieving of clinical and total procedural success, presence of connective tissue on the leads and connective tissue adhesions of leads to heart structures were tested.
Statistical analysis was performed with Statistica version 13.3 (TIBCO Software Inc.).
Approval of the Bioethics Committee
All patients gave their informed written consent to undergo TLE. The use of anonymous data from patient’s medical records was approved by the Bioethics Committee at the Regional Chamber of Physicians in Lublin, Poland no. 288/2018/KB/VII.
All methods were performed in accordance with the relevant guidelines and regulations.
Results
The mean difference in age at the time of lead extraction between group A (patients with lead implanted in early adulthood (ages 19–29) and B (patients with lead implanted at age > 40 and TLE performed before the age of 80) was 28.6 years (37.9 vs. 66.5). The mean difference in age at first lead/system implantation was 34.9 years (23.6 vs. 58.4). Compared with “ordinary” adults younger patients were more often women (46.8 vs. 37.4%). In young adults the most common indications for permanent cardiac pacing were congenital heart diseases, channelopathies, neurocardiogenic syncope and complications of cardiac surgery (82.5%), whereas in middle-aged/older adults ischemic heart disease, myocardial infarction (MI) and cardiomyopathies (77.5%). Age and indications for CIED are the indicators of difference in health status between the two groups, expressed as significant differences in average EF (59.2 vs. 47.8%), diabetes (2.4 vs. 21.1%), renal failure (3.2 vs. 20.4%) and Charlson comorbidity index (0.4 vs. 4.7). (Table 1).
Table 1.
Clinical characteristics of the study population.
| Groups of patients | Implantation ages 19–29 | Implantation and TLE ages 40–80 | A vs B | ||
|---|---|---|---|---|---|
| A | B | Mann–Whitney U test, Chi2 P |
|||
| Number of patients | 126 | 2659 | |||
| Data for analysis | Count/average | %/SD | Count/average | %/SD | |
| Patient age during TLE (years) | 37.85 | 9.22 | 66.49 | 9.38 | P < 0.001 |
| Patient age at first CIED implantation (years) | 23.56 | 3.12 | 58.44 | 11.51 | P < 0.001 |
| Female | 59 | 46.83% | 994 | 37.38% | P = 0.041 |
| Etiology of pacing: IHD, MI | 7 | 5.56% | 1636 | 61.53% | P < 0.001 |
| Etiology of pacing: cardiomyopathy | 15 | 11.90% | 425 | 15.98% | P = 0.271 |
| Etiology of pacing: congenital, channelopathies, neurocardiogenic, cardiac surgery | 104 | 82.54% | 598 | 22.49% | P < 0.001 |
| Heart failure NYHA class III & IV | 3 | 2.38% | 401 | 15.08% | P < 0.001 |
| Left ventricular ejection fraction [%] | 59.20 | 9.80 | 47.81 | 15.48 | P < 0.001 |
| Left Ventricular Ejection Fraction < 41% | 12 | 9.52% | 929 | 34.94% | P < 0.001 |
| Diabetes (any) | 3 | 2.38% | 561 | 21.10% | P < 0.001 |
| Renal failure (any) | 4 | 3.17% | 543 | 20.42% | P < 0.001 |
| Creatinine level [mg%] | 0.94 | 0.79 | 1.24 | 1.84 | P < 0.001 |
| BMI (kg/m2) | 25.89 | 4.35 | 28.31 | 5.40 | P < 0.001 |
| Long-term anticoagulation | 23 | 18.25% | 1076 | 40.47% | P < 0.001 |
| Long-term antiplatelet treatment | 10 | 7.94% | 1229 | 46.22% | P < 0.001 |
| Charlson comorbidity index | 0.44 | 1.32 | 4.73 | 3.52 | P < 0.001 |
BMI body mass index, IHD ischaemic heart diseases, MI myocardial infarction, NYHA New York Heart Association class.
Older patients were more likely to have infections compared with younger adults (32.3 vs. 21.4%), with the difference being significant for pocket infection (9.9 vs. 2.4%). Adults aged 19–29 were referred for lead extraction predominantly for noninfectious indications, mainly mechanical lead damage (46.0 vs. 25.7%). Middle-aged/older adults were more likely to have dysfunctional leads (12.5 vs. 5.6%) and system downgrading (0.8 vs. 3.8%), whereas younger aged patients more often underwent extraction of superfluous leads (10.3 vs. 3.2%). There were no differences in the type of CIED, excluding VDD (7.1 vs. 2.0%) and CRT-D (0.0 vs. 8.3%). Patients in group B tended to have more leads in the system than patients in group A (1.6 ± 0.5 vs. 1.8 ± 0.7 p = 0.003). Young adults had more, albeit insignificantly, abandoned leads (15.1 vs. 11.6%). Adults aged 19–29 were more likely to have more than 4 leads in the heart (3.2 vs. 0.4%), two single-coil ICD leads (8.1 vs. 0.6%), leads on both sides of the chest (5.6 vs. 3.0%) and more CIED-related procedures before lead extraction (2.4 vs. 1.9%) compared with patients aged 40–80. Young adults had significantly older leads: dwell time of the oldest extracted lead per patient was 172.1 months vs. 94.0 months in older adults and mean implant duration per patient before TLE was 152.3 vs. 86.8 months (Table 2).
Table 2.
Analysis of risk factors for the difficulty of the procedure and major complications.
| Groups of patients | Implantation ages 19–29 | Implantation and TLE ages 40–80 | A vs B | ||
|---|---|---|---|---|---|
| A | B | Mann–Whitney U test, Chi2 P |
|||
| Number of patients | 126 | 2659 | |||
| Data for analysis | Count/average | %/SD | Count/average | %/SD | |
| Noninfectious indications for TLE | |||||
| Systemic infection | 24 | 19.05% | 595 | 22.38% | P = 0.442 |
| Local (pocket) infection | 3 | 2.38% | 263 | 9.89% | P = 0.008 |
| Mechanical lead damage (electric failure) | 58 | 46.03% | 682 | 25.65% | P < 0.001 |
| Lead dysfunction (exit/entry block, dislodgement, extracardiac pacing) | 7 | 5.56% | 331 | 12.45% | P = 0.030 |
| Other (perforation, upgrading, downgrading, abandoned lead, threatening/potentially threatening lead, MRI indication, cancer, painful pacemaker pocket, loss of indications for pacing, regaining venous access) | 34 | 26.98% | 786 | 29.56% | P = 0.963 |
| The main goal of TLE | |||||
| System removal—infection | 27 | 21.43% | 858 | 32.27% | P = 0.014 |
| Upgrading | 19 | 15.08% | 294 | 11.06% | P = 0.210 |
| Downgrading | 1 | 0.79% | 100 | 3.76% | P < 0.001 |
| Lead replacement | 61 | 48.41% | 1289 | 48.48% | P = 0.939 |
| Superfluous lead extraction | 13 | 10.32% | 86 | 3.23% | P < 0.001 |
| Other noninfectious indications | 5 | 3.96% | 32 | 1.20% | P = 0.020 |
| System and history of pacing | |||||
| Pacemaker (any) | 88 | 69.84% | 1972 | 74.16% | P = 0.282 |
| Pacemaker—VDD system | 9 | 7.14% | 53 | 1.99% | P < 0.001 |
| ICD (VVI, DDD) pacing system | 38 | 30.16% | 638 | 34.93% | P = 0.141 |
| ICD—CRT-D pacing system | 0 | 0.00% | 220 | 8.27% | P < 0.001 |
| Number of leads in the system before TLE | 1.63 | 0.50 | 1.83 | 0.70 | P = 0.003 |
| Presence of abandoned leads before TLE | 19 | 15.08% | 308 | 11.58% | P = 0.249 |
| Multiple abandoned leads before TLE | 7 | 5.56% | 102 | 3.84% | P = 0.661 |
| Number of leads in the heart before TLE | 1.82 | 0.72 | 1.98 | 0.77 | P = 0.037 |
| 4 and > 4 in the heart before TLE | 4 | 3.17% | 11 | 0.41% | P < 0.001 |
| Two single-coil ICD leads before TLE | 3 | 8.11% | 15 | 0.56% | P = 0.056 |
| CS lead before TLE | 1 | 0.79% | 481 | 18.09% | P < 0.001 |
| Leads on both sides of the chest before TLE | 7 | 5.56% | 80 | 3.01% | P = 0.179 |
| Previous TLE | 8 | 6.35% | 126 | 4.74% | P = 0.540 |
| Upgrading or downgrading with lead abandonment | 14 | 11.11% | 163 | 6.13% | P = 0.040 |
| Large lead loop on X-ray before TLE | 11 | 8.80% | 137 | 5.15% | P = 0.122 |
| Number of procedures before lead extraction | 2.38 | 1.30 | 1.87 | 0.07 | P < 0.001 |
| Dwell time of the oldest lead per patient before TLE | 172.1 | 102.2 | 93.95 | 66.44 | P < 0.001 |
| Mean implant duration (per patient) before TLE | 152.3 | 81.80 | 86.78 | 59.11 | P < 0.001 |
CRT cardiac resynchronization therapy, CS coronary sinus, DDD dual chamber system, ICD implantable cardioverter defibrillator, VVI single chamber system, VDD single lead, dual chamber system, TLE transvenous lead extraction.
Extraction of VDD lead (10.3 vs 2.4%) and abandoned lead(s) (13.5 vs. 10.8%) were more frequent in younger than older adults. The average SAFeTY TLE score used to evaluate the risk of TLE-related major complications as the number of points14 was significantly higher in early adulthood (8.7 vs. 5.7 points). Lead extraction in early adulthood was more time and effort consuming: extraction duration, expressed as “skin-to-skin time” (66.9 vs. 60.2 min), “sheath-to-sheath time” (22.3 vs. 14.8 min), and mean extraction time per lead (sheath-to sheath/number of extracted leads) (14.1 vs. 8.7 min) was prolonged in younger adults. Occurrence of any technical problem during TLE (34.1 vs. 19.6%), Byrd dilator collapse/torsion/"fracture" (11.1 vs. 2.9%) and lead fracture/rupture during the extraction (14.3 vs. 5.6%) were significantly more common in younger adults. Lead-to-lead binding (9.5 vs. 6.8%) and the need to use alternative approach (14.7 vs. 1.6%) were markedly but not significantly (lead-to-lead binding) more frequent in early adulthood. Lasso catheters/snares for broken lead fragments were significantly more commonly used in younger patients (12.9 vs. 3.2%). Similarly, Evolution (old and new) or TightRail sheaths (2.4 vs. 1.1%), loops formed with the catheter, guide wire and lasso (to grasp the lead if the proximal end could not be reached) (2.4 vs. 1.8%) were more often required in young adults. Differences were not significant but a marked tendency was clear (Table 3) (Fig. 1).
Table 3.
Detailed analysis of the risk factors associated with the procedure in terms of the complexity of the procedure and major complications.
| System and procedure information | Implantation ages 19–29 | Implantation and TLE ages 40–80 | A vs. B | ||
|---|---|---|---|---|---|
| A | B | Mann–Whitney U test, Chi2 P |
|||
| Number of patients | 126 | 2659 | |||
| Data for analysis | Count/average | %/SD | Count/average | %/SD | |
| Potential risk factors for major complications and technical problems | |||||
| Number of extracted leads per patient | 1.74 | 0.87 | 1.67 | 0.77 | P = 0.384 |
| Need to use alternative approach | 5 | 3.97% | 84 | 3.16% | P = 0.806 |
| Extraction of VDD lead | 13 | 10.32% | 64 | 2.41% | P < 0.001 |
| Extraction of lead with too long loop | 7 | 5.56% | 94 | 3.54% | P = 0.387 |
| Extraction of broken lead with too long loop | 2 | 1.50% | 67 | 0.00% | P = 0.715 |
| Extraction of abandoned lead(s) (any) | 17 | 13.49% | 288 | 10.83% | P = 0.043 |
| HV therapy (ICD) lead was extracted | 38 | 30.16% | 788 | 29.64% | P = 0.979 |
| CS (LV pacing) lead was extracted | 0 | 0.00% | 185 | 6.96% | P = 0.004 |
| Cumulative dwell times of extracted leads (in years) | 22.60 | 16.90 | 13.16 | 12.57 | P < 0.001 |
| SAFETY TLE risk score (number of points) | 8.70 | 5.00 | 5.65 | 4.21 | P < 0.001 |
| TLE procedure duration | |||||
| Procedure duration (skin to skin) (minutes) | 66.90 | 35.46 | 60.18 | 25.87 | P = 0.013 |
| Procedure duration (sheath to sheath) (minutes) | 22.27 | 32.77 | 14.81 | 22.75 | P < 0.001 |
| Mean extraction time per lead (sheath-to sheath/number of extracted leads) (minutes) | 14.10 | 26.60 | 8.65 | 12.24 | P < 0.001 |
| Procedure difficulty | |||||
| Technical problem during TLE (any) | 43 | 34.13% | 521 | 19.59% | P < 0.001 |
| Lead-to-lead binding | 12 | 9.52% | 181 | 6.81% | P = 0.320 |
| Byrd dilator collapse/torsion/"fracture" | 14 | 11.11% | 77 | 2.90% | P < 0.001 |
| Extracted lead fracture/rupture during extraction | 18 | 14.29% | 150 | 5.64% | P < 0.001 |
| Loss of free lead fragment | 1 | 0.79% | 13 | 0.49% | P = 0.864 |
| One technical problem only | 27 | 21.43% | 304 | 11.43% | P < 0.001 |
| Two technical problems | 11 | 8.73% | 74 | 2.78% | P < 0.001 |
| Need to use alternative approach | 18 | 14.329% | 43 | 1.62% | P < 0.001 |
| Use of additional tools | |||||
| Evolution (old and new) or TightRail sheaths | 3 | 2.38% | 30 | 1.13% | P = 0.396 |
| Metal sheaths | 9 | 7.14% | 183 | 6.88% | P = 0.947 |
| Lasso catheter/snare | 15 | 11.90% | 86 | 3.23% | P < 0.001 |
| Loop formed with catheter guide wire and lasso | 3 | 2.38% | 47 | 1.77% | P = 0.870 |
| Temporary pacing during procedure | 21 | 16.70% | 267 | 10.04% | P = 0.025 |
CS coronary sinus, HV high voltage, ICD implantable cardioverter defibrillator, LV left ventricle, TLE transvenous lead extraction.
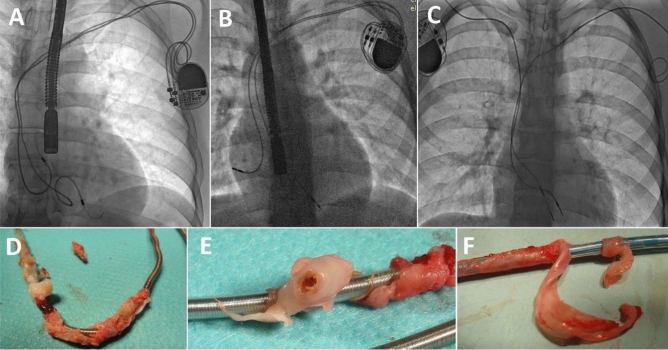
Figure 1.
Several examples of X-ray and view of extracted leads. (A) Planned to long lead loops in the heart implanted 20 years before TLE. (B) Strained (“standing”) 12 y old dysfunctional RV lead due to body growth. RA lead was added 5 year ago during system upgrading. (C) 18-y old VVI pacing system (R) and abandoned 15-y old RV lead. (D) Strong advanced connecting tissue scar surrounding distal part of RAA lead. (E) Extracted in young adult ICD lead; strong massive scar (tunnel form) connecting two of leads before extraction—visible on one of two extracted leads. Such phenomenon make extraction more difficult. (F) Another form of (more floppy) scar on extracted ICD lead in young adult.
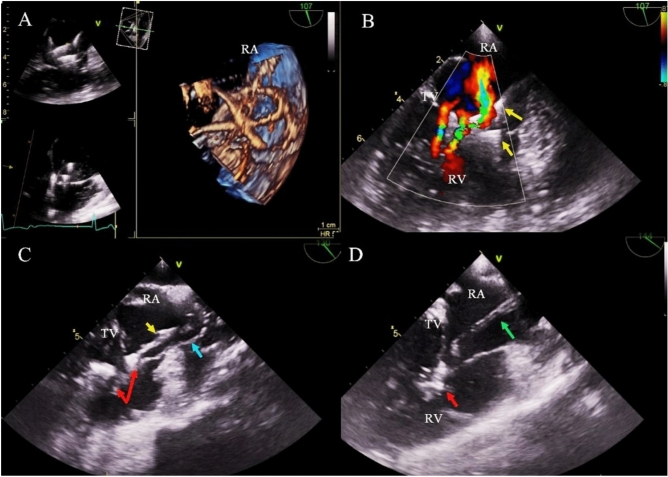
The organizational model plays an important role in extraction procedures. It does not influence the occurrence of major complications but strongly facilitates their proper management and reduces procedure-related mortality. Both groups underwent TLE in the same time interval (selection was done retrospectively). Between 2006 and 2011 extractions were performed in the EP-LAB, between 2012 and 2016 additional precautions (graded approach) were taken and since 2017 all procedures have been performed in the hybrid room or cardiac surgery operating room. Table 4 shows that young adults tended to undergo TLE in cardiac surgical operating rooms or hybrid rooms, with the cardiac surgeon as a co-operator, under general anesthesia and with TEE monitoring of lead extraction when possible (Fig. 2).
Table 4.
Analysis of the effectiveness and complications of TLE.
| Groups of patients | Implantation ages 19–29 | I Implantation and TLE ages 40–80 | A vs. B | ||
|---|---|---|---|---|---|
| A | B | Mann–Whitney U test, Chi2 P |
|||
| Number of patients | 126 | 2659 | |||
| Data for analysis | Count/average | %/SD | Count/average | %/SD | |
| Organizational model of TLE procedure | |||||
| Procedure in cardiac surg. operating room or hybrid room | 70 | 55.55% | 1254 | 47.16% | P = 0.080 |
| Cardiac surgeon as co-operator | 72 | 57.10% | 1262 | 47.46% | P = 0.042 |
| General anesthesia | 64 | 57.10% | 1162 | 43.70% | P = 0.140 |
| Routine TEE monitoring of lead extraction | 59 | 46.80% | 1022 | 38.44% | P = 0.073 |
| Complete radiographic result (only X-ray) | 113 | 89.68% | 2564 | 96.43% | P < 0.001 |
| Partial radiographic result (retained tip of lead) | 5 | 3.97% | 50 | 1.88% | P = 0.202 |
| Partial radiographic result (retained < 4 cm lead fragment) | 7 | 5.56% | 40 | 1.50% | P = 0.003 |
| Lack of radiographic result | 1 | 0.79% | 5 | 0.19% | P = 0.653 |
| Major complications | |||||
| Major complications (all) | 9 | 7.10% | 54 | 2.03% | P < 0.001 |
| Dwell time of extracted lead < 5 years | 0/16 | 0.00% | 6/1036 | 0.579% | P = 0.072 |
| Dwell time of extracted lead 5–9 years | 0/31 | 0.00% | 9/937 | 0.961% | P = 0.384 |
| Dwell time of extracted lead ≥ 10 years | 9/79 | 11.39% | 39/686 | 5.69% | P = 0.083 |
| Hemopericardium | 6 | 4.76% | 35 | 1.32% | P = 0.006 |
| Tricuspid valve damage during TLE (severe) | 4 | 3.14% | 9 | 0.34% | P < 0.001 |
| Other major complications | 0 | 0.00% | 10 | 0.38% | P = 0.572 |
| Rescue cardiac surgery | 4 | 3.17% | 33 | 1.24% | P = 0.150 |
| Minor complications (any) | 16 | 12.70% | 201 | 7.56% | P = 0.053 |
| Procedure-related death (intra-, post-procedural) | 0 | 0.00% | 6 | 0.23% | P = 0.653 |
| Indication-related death (intra-, post-procedural | 0 | 0.00% | 1 | 0.08% | P = 0.876 |
| Radiographic success | |||||
| Complete radiographic success (all material removed) | 109 | 86.51% | 2545 | 95.71% | P < 0.001 |
| Dwell time of extracted lead < 5 years | 16/16 | 100.0% | 1021/1036 | 98.55% | P = 0.564 |
| Dwell time of extracted lead 5–9 years | 30/31 | 96.77% | 904/937 | 96.48% | P = 0.684 |
| Dwell time of extracted lead ≥ 10 years | 63/79 | 79.75% | 620/686 | 90.38% | P = 0.007 |
| Partial radiographic success (retained tip or < 4 cm lead fragment) | 13 | 10.32% | 80 | 3.01% | P < 0.001 |
| Lack of radiographic success (retained lead) | 4 | 3.17% | 34 | 1.28% | P = 0.004 |
| Clinical success | |||||
| Clinical success | 118 | 93.20% | 2611 | 98.12% | P = 0.378 |
| Dwell time of extracted lead < 5 years | 16/16 | 100.0% | 1031/1036 | 99.52% | P = 0.121 |
| Dwell time of extracted lead 5–9 years | 31/31 | 100.0% | 926/937 | 98.83% | P = 0.893 |
| Dwell time of extracted lead ≥ 10 years | 71/79 | 89.87% | 654/686 | 95.33% | P = 0.072 |
| Lack of complete radiographic success in infectious cases | 4 | 3.17% | 28 | 1.28% | P = 0.973 |
| TV damage | 4 | 3.17% | 9 | 0.34% | P < 0.001 |
| Complication—death | 0 | 0.00% | 7 | 0.26% | P = 0.739 |
| Planned cardiac surgery | 0 | 0.00% | 4 | 0.15% | P = 0.175 |
| Procedural success | |||||
| Procedural success | 109 | 86.51% | 2545 | 95.71% | P < 0.001 |
| Dwell time of extracted lead < 5 years | 16/16 | 100.0% | 1021/1036 | 98.55% | P = 0.564 |
| Dwell time of extracted lead 5–9 years | 30/31 | 96.77% | 904/937 | 96.48% | P = 0.684 |
| Dwell time of extracted lead ≥ 10 years | 63/79 | 79.75% | 620/686 | 90.38% | P = 0.007 |
| Lack of complete radiographic success | 13 | 10.32% | 114 | 3.65% | P < 0.001 |
| Permanently disabling complication or death | 4 | 3.178% | 18 | 0.68% | 0. 023 |
| ECHO before and after TLE | |||||
| Tricuspid regurgitation before TLE: moderate/severe | 7 | 5.56% | 362 | 13.61% | P = 0.013 |
| Tricuspid regurgitation before TLE: severe | 2 | 1.59% | 89 | 3.35% | P = 0.407 |
| TLE related TV dysfunction (damage) | |||||
| TR increase by 2 grades | 9 | 7.14% | 40 | 1.50% | P < 0.001 |
| TR increase by 3 grades | 2 | 1.59% | 9 | 0.34% | P = 0.145 |
TEE transesophageal echocardiography, TLE transvenous lead extraction, TV tricuspid valve, TR tricuspid regurgitation.
Figure 2.
TEE images from the monitoring of the extraction of 4 leads in a 24-year-old female patient. (A) In the right atrium, loops of 4 leads fused together, displaced and adhered to the tricuspid apparatus. (B) Color Doppler—multi-flux, moderate tricuspid regurgitation with moderate valve stenosis (V max 1.6 m/s, PG avg. 4 mmHg) resulting from conglomerate of the leads (yellow arrows). (C) Moment of extraction of the lead; one of the ventricular leads is torn and stretched (blue arrow). Pulled up the second of the ventricular leads (yellow arrow) with simultaneous pull-up of the right ventricular wall and elements of the tricuspid apparatus. Red arrows mark massive adhesions of the leads with RV and TV structures. (D) After extraction of the leads, in the RA, a fragment of the silicone insulation was visualized by TEE examination (green arrow). Massive fragments of connective tissue within the sub-valvular apparatus (red arrow), hindering the proper mobility of the valve leaflets.
Major complications were observed more frequently in younger than older adults (7.1 vs. 2.0%), similar to hemopericardium (4.8 vs. 1.3%), need for immediate cardiac surgery (3.2 vs. 1.2%) and severe tricuspid valve damage during TLE (3.2 vs. 0.5%). The differences were significant in all but one variable (immediate cardiac surgery), reflecting well the disparity in TLE safety between the two groups. The comparison of the proportion of major complications depending on lead dwell time showed significantly higher percentage of MC in young adults (with the leads above 10 years old). TLE effectiveness expressed as complete radiographic success (86.5 vs. 95.7) and partial radiographic success (10.3 vs. 3.0%), similar to clinical success (93.2 vs. 98.1%) and procedural success (86.5 vs. 95.7%) was worse in younger than older adults. The relatively low percentage of procedural success was caused mainly by the lack of complete radiographic success (10.3 vs. 3.0%) but also because of the occurrence of permanently disabling complications (3.2 vs. 1.3%). Lead dwell time, number of the leads, presence of abandoned leads and redundant lead loops crossing the tricuspid valve and the occurrence of TLE-related TV dysfunction (increased TR by 2 or 3 degrees) (8.7 vs. 1.8%) were also of more importance in younger than older adults. Clinical success in both groups was comparable, but the rates of complete radiographic and procedural success were lower in younger adults. The relatively low rate of procedural success in both groups was caused mainly by the lack of complete radiographic success and because of the occurrence of permanently disabling complications (TV damage). Procedural and clinical success in young adults with the oldest leads (above 10 years) was significantly lower (Table 4).
Results of multivariable regression analysis
Major complications
In group of younger patients two-variable regression analysis shown that the only higher dwell time of the extracted lead was a risk factor of MC in this group. Probability of MC occurrence increased from 7.8 to 13.7% per one year of dwell time of the oldest extracted lead depending on compared data. The result of the juxtaposition in the two-variable analysis of the patient's age during TLE and the dwell time of the oldest extracted lead does not show statistical significance. This is due to the high correlation coefficient of both variables in this group (Spearman r = 0.888; p < 0.001).
In the group of older patients higher probability of MC occurrence was in patients with older leads—risk increase by 9.2% per one year (OR 1.092; p = 0.006), in female—risk increase by 236% (OR 3.361; p = 0.001) and in patients with higher number of previously CIED related procedures before TLE—risk increase by 30.3% per one procedure (OR 1.303; p = 0.071).
Clinical success
Multivariable regression analysis shown that in the group of younger patients only the number of previously CIED-related procedures had the impact on clinical success achieving, decreasing probability by 67.2% per one procedure (OR 0.328; p = 0.030). In the group of older patients lower probability of achieving of procedural success was in patients with older leads—reduction by 8.4% per one year (OR 0.916; p = 0.003), higher number of leads in the heart—reduction by 40.8% per one lead (OR 0.592; p = 0.014) and in the patients with infectious indications for TLE—reduction by 88.1% (OR 0.119; p < 0.001).
Procedural success
Multivariable regression analysis shown that in the group of younger patients the TLE of conventional pacemaker leads decreased probability of achieving procedural success by 75.1% (OR 0.249; p = 0.025) and each previously CIED—related procedures by 41.4% (OR 0.586; p = 0.078), but this parameter achieving borderline statistically significance. In the group of older patients lower probability of achieving of procedural success was in patients with older leads—reduction by 7.1% per one year (OR 0.929; p < 0.001), higher number of previously CIED—related procedures—reduction by 19.1% per one procedure (OR 0.809; p = 0.031) and in the patients with the higher number of leads—reduction by 26.2% per each lead (OR 0.738; p = 0.056) (Table 5).
The binary regression analysis of the age of patients during the implantation with lead dwell time of the oldest lead in the patient showed that patient’s age during first CIED implantation between 19–29 years (group A) was an independent factor of the occurrence of major complications (OR 4.709; p < 0.001) and the lack of procedural success (OR 0.291; p = 0.002). Younger age of patients at first implantation, regardless of the dwell lead time, is also a factor contributing to the greater development of connective tissue proliferation on the leads (OR 2.587; p < 0.001) and adhesions of the leads with the heart structures (OR 3.322; p < 0.001), which translates into worse TLE results in this group of patients (Table 6).
Table 6.
Binary analysis of impact of patients age during first CIED implantation and dwell time of oldest lead and oldest extracted lead on the major complication, clinical and total procedural success and connective tissue on the leads and connective tissue binding of the leads to the heart structures occurrence.
| Univariable regression analysis | Binary regression analysis | |||||
|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | |
| Major complication | ||||||
| Patient's age during first system implantation: 19–29 vs 40–80 years | 4.709 | 2.265–9.792 | < 0.001 | 2.507 | 1.160–5.421 | 0.019 |
| Dwell time of the oldest lead in the patient before TLE ≥ 10 years | 11.203 | 5.388–23.30 | < 0.001 | 10.035 | 4.776–21.09 | < 0.001 |
| Patient's age during first system implantation: 19–29 vs 40–80 years | 4.709 | 2.265–9.792 | < 0.001 | 2.548 | 1.177–5.515 | 0.018 |
| Dwell time of the oldest extracted lead ≥ 10 years | 10.454 | 5.170–21.14 | < 0.001 | 9.344 | 4.569–19.11 | < 0.001 |
| Clinical success | ||||||
| Patient's age during first system implantation: 19–29 vs 40–80 | 0.291 | 0.135–0.628 | 0.002 | 0.540 | 0.245–1.189 | 0.126 |
| Dwell time of the oldest lead in the patient before TLE ≥ 10 years | 0.147 | 0.082–0.264 | < 0.001 | 0.157 | 0.087–0.284 | < 0.001 |
| Patient's age during first system implantation: 19–29 vs 40–80 | 0.291 | 0.135–0.628 | 0.002 | 0.540 | 0.245–1.189 | 0.126 |
| Dwell time of the oldest extracted lead ≥ 10 years | 0.164 | 0.093–0.288 | < 0.001 | 0.157 | 0.087–0.284 | < 0.001 |
| Procedural success | ||||||
| Patient's age during first system implantation: 19–29 vs 40–80 | 0.291 | 0.135–0.628 | 0.002 | 0.457 | 0.258–0.807 | 0.007 |
| Dwell time of the oldest lead in the patient before TLE ≥ 10 years | 0.147 | 0.082–0.264 | < 0.001 | 0.191 | 0.128–0.287 | < 0.001 |
| Patient's age during first system implantation: 19–29 vs 40–80 | 0.291 | 0.135–0.628 | 0.002 | 0.446 | 0.252–0.790 | 0.006 |
| Dwell time of the oldest extracted lead ≥ 10 years | 0.164 | 0.093–0.288 | < 0.001 | 0.203 | 0.136–0.302 | < 0.001 |
| Fibrous binding of the lead to heart structures | ||||||
| Patient's age during first system implantation: 19–29 vs 40–80 | 3.322 | 2.136–5.166 | < 0.001 | 2.073 | 1.305–3.293 | 0.002 |
| Dwell time of the oldest lead in the patient before TLE ≥ 10 years | 3.811 | 2.888–5.031 | < 0.001 | 3.505 | 2.637–4.660 | < 0.001 |
| Patient's age during first system implantation: 19–29 vs 40–80 | 3.322 | 2.136–5.166 | < 0.001 | 2.068 | 1.303–3.283 | 0.002 |
|
Dwell time of the oldest extracted lead ≥ 10 years |
3.818 | 2.899–5.028 | < 0.001 | 3.516 | 2.652–4.662 | < 0.001 |
| Connective tissue on the leads (accretions. lead thickening. fibrous lead-lead binding) | ||||||
| Patient's age during first system implantation: 19–29 vs 40–80 | 2.587 | 1.762–3.798 | < 0.001 | 1.828 | 1.225–2.728 | 0.003 |
| Dwell time of oldest lead in the patient before TLE ≥ 10 years | 2.400 | 1.960–2.938 | < 0.001 | 2.255 | 1.833–2.774 | < 0.001 |
| Patient's age during first system implantation: 19–29 vs 40–80 | 2.587 | 1.762–3.798 | < 0.001 | 1.864 | 1.251–2.777 | 0.002 |
| Dwell time of the oldest extracted lead ≥ 10 years | 2.458 | 2.008–3.009 | < 0.001 | 2.308 | 1.876–2.838 | < 0.001 |
Discussion
Transvenous lead extraction is now an increasingly common procedure used in the therapy of CIED-related complications. The risk assessment of procedure is often difficult and misinterpreted. Knowledge of major complication predictors (long implant duration, female gender, renal failure, multiple leads, anemia, previous CIED-related procedures)11–14 in combination with risk factors for short- and long-term mortality after lead extraction (infections, old age, diabetes, low EF, heart failure)11–13,15,16 often leads to an unjustified overestimation of TLE-related risk.
There are only five reports on lead extraction in children1–5 and three reports on lead extraction in juveniles6–9, all of them confirming the difficulty of lead removal in these age groups1–9. There are also several reports on the expected increase in procedural risk but none of them has considered younger age of patients undergoing TLE as a risk factor for major complications17–21. Only one study uses the SAFeTY TLE score to assess the risk for the occurrence of major complications based on the following parameters: sum of dwell times of extracted leads (threshold value ≥ 16.5 years), hemoglobin concentration (threshold level < 11.5 g/dl), female gender, the number of previous CIED-related procedures and less than 30 years of age at first CIED implantation14. The TLE score calculator is an online tool available at http://alamay2.linuxpl.info/kalkulator/.
The current study shows that young adults were most likely to have congenital heart disease and complications of cardiac surgery. The majority of patients were in very good condition (Charlson comorbidity index 0.44). Noninfectious indications, especially mechanical lead damage were prevalent in young adults. There were no differences in CIED systems, but young adults had more abandoned leads and more leads on both sides of the chest and more previous CIED-related procedures. Currently, in accordance with the 2017 HRS consensus statement12, early removal of potentially dysfunctional leads should be considered in young people. As young patients have a very long life expectancy, abandonment of superfluous functional leads should be avoided, therefore the idea of prophylactic lead extraction needs further discussion.
Multivariable analysis of the risk of major complications in the current study revealed only a few common risk factors for MC in young and older adults. The most important finding in younger adults was longer dwell time of the oldest lead before TLE. As is well known, longer lead dwell time is the main risk factor for complications of TLE12–14,19,20. The present study confirmed that the effectiveness of the procedure was significantly lower in younger patients. Moreover, it has been shown that during lead extraction in young adults, technical problems occurred more frequently. Young adults more often needed the use of alternative approach and the second line tools (lasso catheters, Evolution or TightRail sheaths and loops formed with the catheter, guide wire and lasso). Mean extraction time per lead (sheath-to sheath/number of extracted leads) was longer in young adults (14.10 vs. 8.65 min). Major complications (including hemopericardium, immediate cardiac surgery and TLE-associated tricuspid valve damage) were also more common in young adults (7.10 vs. 2.03%). This finding is consistent with that of El-Chami who compared two groups: < 40 years of age (n = 84) and ≥ 40 (n = 690) and showed that the younger cohort more frequently tended to require the second line tools and techniques despite similar lead dwell times in both groups (5.7 vs. 5.6 years)10. A slightly different result in our study can be accounted for by different implant duration: 172.1 vs. 93.95 months (14.34 vs. 7.83 years) and a very specific group of young adults (ages 19–29 vs. > 40 years) who seem to be nearer to children in terms of scar formation. Similarly, the analysis of the effectiveness of TLE in the population of young adults with congenital heart disease showed slightly better results, however the age of the extracted leads was lower compared to the present study21. As the evidence shows patient age has a significant impact on the severity of scar formation, and in consequence, lead extraction difficulty1–10.
This study aims to remind that in such specific patients lead extraction should be performed by most experienced operators in a high-volume center, as previously suggested by El-Chami10.
Probably age at CIED implantation is a strong, but largely underestimated risk factor for major complications associated with transvenous lead extraction.
Study limitations
There are some limitations in this study. Extractions were performed based on the organizational model evolving from graded safety precautions between 2006 and 2015 to full safety precautions since 2017. All types of mechanical systems but not laser powered sheaths were used. TLE was performed in three centers by the same very experienced first operator. The database was created prospectively, but analysis was performed retrospectively.
Conclusions
Lead extraction in young adults is often more complicated compared to the older population, because younger aged patients have a more pronounced connective tissue reaction to the presence of the lead and a dwell time of the oldest lead before TLE is usually significantly longer. These factors have the greatest impact on the effectiveness and safety of the procedure. In patients with their leads implanted in early adulthood prolonged extraction duration and higher procedure complexity are combined with a greater need for second line tools and clinical and procedural success are lower due to the lack of complete radiographic success. Moreover, both major and minor complications are more frequent in young adults, with hemopericardium and tricuspid valve damage being predominant.
Acknowledgements
Authors express their sincere gratitude to all TLE team for continuous and unconditional help in realising the project.
Author contributions
A.K.: written manuscript, W.J.: statistical study, Ł.T.: material collection, checking paper, M.C.: material collection, D.N.: material collection, P.S.: material collection, K.T.: material collection, A.P.: material collection, checking paper. All authors read and approved the final manuscript.
Data availability
All data generated or analysed during this study are included in this published article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Friedman RA, Van Zandt H, Collins E, LeGras M, Perry J. Lead extraction in young patients with and without congenital heart disease using the subclavian approach. Pacing Clin. Electrophysiol. 1996;19:778–83. doi: 10.1111/j.1540-8159.1996.tb03359.x. [DOI] [PubMed] [Google Scholar]
- 2.Moak JP, Freedenberg V, Ramwell C, Skeete A. Effectiveness of excimer laser-assisted pacing and ICD lead extraction in children and young adults. Pacing Clin. Electrophysiol. 2006;29:461–466. doi: 10.1111/j.1540-8159.2006.00376.x. [DOI] [PubMed] [Google Scholar]
- 3.Dilber E, Karagöz T, Celiker A. Lead extraction in children and young adults using different techniques. Med. Princ. Pract. 2009;18:356–359. doi: 10.1159/000226287. [DOI] [PubMed] [Google Scholar]
- 4.Cecchin F, Atallah J, Walsh EP, Triedman JK, Alexander ME, Berul CI. Lead extraction in pediatric and congenital heart disease patients. Circ. Arrhythm Electrophysiol. 2010;3:437–444. doi: 10.1161/CIRCEP.110.957324. [DOI] [PubMed] [Google Scholar]
- 5.McCanta AC, Schaffer MS, Collins KK. Pediatric and adult congenital endocardial lead extraction or abandonment decision (PACELEAD) survey of lead management. Pacing Clin. Electrophysiol. 2011;34:1621–7. doi: 10.1111/j.1540-8159.2011.03226.x. [DOI] [PubMed] [Google Scholar]
- 6.Zartner PA, Wiebe W, Toussaint-Goetz N, Schneider MB. Lead removal in young patients in view of lifelong pacing. Europace. 2010;12:714–718. doi: 10.1093/europace/euq059. [DOI] [PubMed] [Google Scholar]
- 7.McCanta AC, Tanel RE, Gralla J, Runciman DM, Collins KK. The fate of nontargeted endocardial leads during the extraction of one or more targeted leads in pediatrics and congenital heart disease. Pacing Clin. Electrophysiol. 2014;37:104–108. doi: 10.1111/pace.12282. [DOI] [PubMed] [Google Scholar]
- 8.Atallah J, Erickson CC, Cecchin F, et al. Pediatric and Congenital Electrophysiology Society (PACES). Multi-institutional study of implantable defibrillator lead performance in children and young adults: Results of the Pediatric Lead Extractability and Survival Evaluation (PLEASE) study. Circulation. 2013;127:2393–402. doi: 10.1161/CIRCULATIONAHA.112.001120. [DOI] [PubMed] [Google Scholar]
- 9.Escudero CA, Mah DY, Miyake CY, et al. Riata lead failure in pediatric and congenital heart disease patients. J. Cardiovasc. Electrophysiol. 2019;30:320–325. doi: 10.1111/jce.13812. [DOI] [PubMed] [Google Scholar]
- 10.El-Chami MF, Sayegh MN, Patel A, et al. Outcomes of lead extraction in young adults. Heart Rhythm. 2017;14:537–540. doi: 10.1016/j.hrthm.2017.01.030. [DOI] [PubMed] [Google Scholar]
- 11.Wilkoff BL, Love CJ, Byrd CL, et al. Transvenous lead extraction: Heart Rhythm Society expert consensus on facilities, training, indications, and patient management: This document was endorsed by the American Heart Association (AHA) Heart Rhythm. 2009;6:1085–1104. doi: 10.1016/j.hrthm.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 12.Kusumoto FM, Schoenfeld MH, Wilkoff B, et al. 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm. 2017;14:e503–e551. doi: 10.1016/j.hrthm.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 13.Bongiorni MG, Burri H, Deharo JC, et al. 2018 EHRA expert consensus statement on lead extraction: Recommendations on definitions, endpoints, research trial design, and data collection requirements for clinical scientific studies and registries: Endorsed by APHRS/HRS/LAHRS. Europace. 2018;20:1217. doi: 10.1093/europace/euy050. [DOI] [PubMed] [Google Scholar]
- 14.Jacheć W, Polewczyk A, Polewczyk M, et al. Transvenous lead extraction SAFeTY score for risk stratification and proper patient selection for removal procedures using mechanical tools. J. Clin. Med. 2020;9:356–361. doi: 10.3390/jcm9020361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brunner MP, Yu C, Hussein AA, et al. Nomogram for predicting 30-day all-cause mortality after transvenous pacemaker and defibrillator lead extraction. Heart Rhythm. 2015;12:2381–2386. doi: 10.1016/j.hrthm.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 16.Merchant FM, Levy MR, Kelli HM, et al. Predictors of long-term survival following transvenous extraction of defibrillator leads. Pacing Clin. Electrophysiol. 2015;38:1297–1303. doi: 10.1111/pace.12733. [DOI] [PubMed] [Google Scholar]
- 17.Sidhu BS, Ayis S, Gould J, et al. ELECTRa Investigators. Group Risk stratification of patients undergoing transvenous lead extraction with the ELECTRa Registry Outcome Score (EROS): An ESC EHRA EORP European lead extraction ConTRolled ELECTRa registry analysis. Europace. 2021;22:1718–1728. doi: 10.1093/europace/euaa131. [DOI] [PubMed] [Google Scholar]
- 18.Afzal MR, Daoud EG, Matre N, et al. RIsk Stratification prior to lead Extraction and impact on major intraprocedural complications (RISE protocol) J. Cardiovasc. Electrophysiol. 2019;30:2453–2459. doi: 10.1111/jce.14151. [DOI] [PubMed] [Google Scholar]
- 19.Zucchelli G, Di Cori A, Segreti L, et al. ELECTRa Investigators. Major cardiac and vascular complications after transvenous lead extraction: Acute outcome and predictive factors from the ESC-EHRA ELECTRa (European Lead Extraction ConTRolled) registry. Europace. 2019;21:771–780. doi: 10.1093/europace/euy300. [DOI] [PubMed] [Google Scholar]
- 20.Kancharla K, Acker NG, Li Z, et al. Efficacy and safety of transvenous lead extraction in the device laboratory and operating room guided by a novel risk stratification scheme. JACC Clin. Electrophysiol. 2019;5:174–182. doi: 10.1016/j.jacep.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 21.Gourraud JB, Chaix MA, Shohoudi A, et al. Transvenous lead extraction in adults with congenital heart disease: Insights from a 20-year single-center experience. Circ. Arrhythm Electrophysiol. 2018;11:e005409. doi: 10.1161/CIRCEP.117.005409. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.