Abstract
Energy poverty is a serious social problem with well-known adverse health consequences. This problem has been addressed mainly through improvements in the energy efficiency of housing. Still, little is known about the effects of information-based measures on energy poverty and their impacts on health. A quasi-experimental study was implemented to assess the effectiveness of an energy-counseling home visit intervention targeting the vulnerable population in a southern European city, Barcelona, in alleviating energy poverty and improving health. The intervention had beneficial impacts on keeping homes at an adequate indoor temperature and reducing primary care visits. No effects were found on self-perceived health or self-reported anxiety and depression. After the intervention, participants reported a decrease in arrears on utility bills, but less pronounced than in the comparison group. In conclusion, the study showed that information-based measures lead to psychosocial gains and reduced healthcare use. Nevertheless, the impact of these measures could be enhanced by combining them with policies and programmes that address the structural determinants of energy poverty.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11524-022-00642-6.
Keywords: Energy poverty, Fuel poverty, Counseling intervention, Impact evaluation, Health, Difference-in-differences
Introduction
Abundant evidence has shown that energy poverty (EP) produces a range of adverse effects on health and well-being. The most extreme health consequence is excess seasonal mortality, [1, 2] which is higher in winter than in summer, [3] as well as the acknowledged increase in morbidity rates in cardiovascular, cerebrovascular and respiratory disorders and exacerbations of existing health problems such as diabetes, arthritis and rheumatism. [3–5] In addition, EP negatively affects mental health by increasing stress regarding debt and affordability, thermal discomfort and worry about the health consequences of cold and dampness. [6] These effects have been mostly studied during wintertime, whereas the relationship between energy poverty and health during summertime remains relatively underexplored. [7, 8]
EP is a pervasive problem across the European Union (EU), showing an unequally distributed geographical pattern. More than 50 million people in Europe suffered it, [9] being particularly intense in post-socialist countries in eastern and central Europe and southern European countries. [10] And, it is likely to further increase in the coming years due to rising energy prices, increasing inequalities and climate change. [5, 10] The high EP vulnerability of southern countries has been associated with the poor quality of the housing stock, the lack of adequate heating/cooling systems and the welfare regimes’ reduced ability to counteract inequitable living conditions. [10, 11]
In the case of Spain, historically, housing regulations have been undemanding. Housing insulation was not mandatory in the building code until 1979. It is estimated that 54% were built before that date, so most of them have thermal deficiencies. [12] As a result, most Spanish residencies have poor thermal insulation. Therefore, their inhabitants are exposed to cold and damp homes in winter, despite a warm climate and hot indoor ambient temperatures in summer. In addition, the Spanish welfare state regime, which is described as fragmented and ‘rudimentary’, [13] has been unable to protect the population in need from adverse situations, such as the previous economic recession, which led to an increase in EP. [14] Not only does EP affect a considerable share of the population, but the vulnerable population experience it more intensely, widening social and health inequalities. [15] This situation is one of the determinants of the known excess winter death paradox [2, 16] whereby levels of excess winter dearth are higher in the more temperate southern European countries than in the cooler northern ones.
The response of the Spanish state to this challenge has been initially limited and fragmented, resulting in unequal regional policies. [17] The region of Catalonia has taken specific steps to tackle the phenomenon, such as the regulation (Law 24/2015) that prohibits disconnecting basic supplies for economic reasons in vulnerable populations. This legislation has meant that EP in this region is no longer invisible on the political agenda. Subsequently, in 2019, 4 years later, the Spanish Government approved the National Strategy against EP, thus boosting the level of visibility and political interest towards this problem. [18]
Measures to tackle EP amongst southern EU countries have mainly focused on consumer protection according to EU guidelines, financial support and the provision of energy-efficiency information. [19] This contrasts with the many housing improvement policies applied in the UK, Ireland and other northern countries to overcome the problem. [20–24] Several reviews and syntheses have suggested that housing interventions to improve the energy efficiency of housing lead to significant improvements in health, well-being and psychosocial determinants of health, [4, 25–28] especially when they target vulnerable social groups.
There is, albeit to a lesser extent, evidence that financial support measures to increase household energy affordability reduce the adverse health effects of EP. [29, 30] Increasing the affordability of energy reduced food shortages and child malnutrition. [31] There are indications that excess winter mortality has decreased amongst the elderly population receiving financial support in the UK. [29] However, they increase CO2 emissions, which will handicap the future generations in the current climate crisis. [29]
Comparatively, little is known about the effects of information-based measures on EP and health. Such interventions can help to raise awareness of measures to save energy and energy rights and improve the way people keep their homes warm or cool. [32] A few empirical data have shown that these interventions could have positive effects on EP and health outcomes, but the evidence is inconclusive. [33, 34] Studies performed to date, which have been mainly qualitative, report that such measures could potentially stimulate monetary savings, [33] boost knowledge on energy rights, improve thermal comfort and increase perception of social support. [34] Nevertheless, it has been observed that this type of measure is less likely to increase thermal comfort in poor-quality dwellings. [35]
‘Energia, la justa’ (EJUSTA) was an energy-counseling home visit pilot intervention performed in Barcelona in 2016 through an information-based measure. Despite relatively mild winters, Barcelona is a southern EU city where 10.6% of households suffered EP in 2016 and 23% are in more disadvantaged social classes. [36] The programme aimed to improve household thermal comfort, reduce affordability problems to ensure energy supply and improve well-being, targeting vulnerable populations. The intervention, directed through public social services offices, sought to overcome the ‘inverse care law’, [37] according to which availability of medical or social care varies inversely with need; i.e. those most in need of an intervention are often those who experience the most significant difficulty in benefiting from it.
The present study aimed to investigate the effectiveness of this energy-counseling home visit intervention targeting vulnerable populations in alleviating EP and improving health. The study examined the effect of this intervention on (1) the ability to keep the home adequately warm in winter and cool in summer; (2) difficulties in coping with energy expenditure; and (3) self-perceived health, self-reported mental health and the use of primary health services.
Methods
Design, Intervention, Study Population and Sampling
A quasi-experimental design was conducted to study the effect of the EJUSTA intervention on the EP and health outcomes 1 year after the implementation of the intervention amongst participants compared with a convenience comparison group not receiving the intervention.
The intervention consisted of energy-counseling home visits that included the following four actions: (1) legal action to protect people’s energy rights and avoid disconnections of supplies; (2) promotion of energy-saving behaviours to achieve savings and awareness of the thermal comfort required in the home; (3) if necessary, optimisation of energy services through a change of provider and/or tariffs to obtain cost savings or invoice discounts through government aid; (4) if necessary, installation of micro-efficiency measures, such as plug-in timers and energy-saving light bulbs, amongst others. Participants were recruited at public social service offices amongst applicants for welfare benefits over the 5-month duration of the programme. All measures were free for targeted participants.
The study population was vulnerable populations affected by EP living in Barcelona. The intervention group was selected amongst recipients of the EJUSTA programme who met the following three requirements: (1) Barcelona residents aged 18 years or older, willing to participate and provide signed informed consent; (2) people who were energy poor, defined as those who are unable to ensure socially and materially required levels of domestic energy services [38] measured as the self-reported inability to keep the home warm, or inability to pay utility bills on time, or the presence of damp and/or mould in the dwelling; [39] (3) people who received the intervention during the 2016 spring period. The comparison group was recruited taking advantage of the co-occurrence in time of the Barcelona Public Health Survey (BPHS), which is carried out every 5 years in the general non-institutionalised population of Barcelona city. [40] Participants recruited from the BPHS were 18 years or older, reported being energy poor (met the same EP criteria as the intervention population) and were surveyed in the same spring period as the intervention participants under study. Additionally, we excluded participants recruited from the BPHS who received services or benefits related to their EP situation during the year following the intervention to avoid a potential confounder.
The sample size needed for the study was 348. It was estimated according to a significance level of alpha risk at 0.05, a beta risk below 0.2 in a bilateral contrast and an effect size of 0.10 in a pre-post paired categorical test. Accounting for significant dropouts in hard-to-reach populations, like the intervened population, we calculated the effect size based on a high dropout rate of 30%. The effect size was based on the observed change in thermal comfort of an intervention performed in the UK, the Warm Front intervention, [41] applying a conservative scenario.
Data Source and Study Variables
Two data sources were used in the study: the EJUSTA database containing data from the intervention group and the BPHS database containing data from the comparison group. Participants in the study (only one member per household) completed a questionnaire administered by trained interviewers before and 1 year after the intervention. The questionnaire design was adapted from the BPHS using the same validated items, [40] and the same survey was used in the pre- and the post-test. Both databases contained information on demographic, socioeconomic, housing and EP characteristics, and health outcomes. The socioeconomic, housing and EP profiles of the participants and their physical and mental health status have been described in detailed in a previous paper. [15]
The outcome variables were EP variables and health outcomes which consisted of 3 variables of physical and mental health status and one related to the use of primary health services. EP was self-assessed by the participants with 2 widely used questions: [39] ‘Could your household afford to keep the dwelling heated at an appropriate temperature during the winter months?’ (yes/no); ‘Has your household been in arrears on utility and community bills in the past 12 months?’ (yes/no). In addition, we explored the effect on thermal comfort during summertime, an issue which has been less explored, using the question ‘Could your household afford to keep the dwelling cooled at an appropriate temperature during the summer months?’ (yes/no). The health outcomes included were fair or poor self-reported health, an indicator that has proven to be a good indicator of health status. [42] Mental health was assessed by the self-reported presence or absence of depression and/or anxiety in the previous 12 months and self-reported use of medications for depression and anxiety in the last 2 days. Both indicators are notable for the high concordance between the clinical diagnosis and the self-reported values. [43] Finally, healthcare utilisation was assessed through self-reported use of primary care in the previous 12 months, dichotomised using the median value (3 times or less/more than 3 times).
The main independent variables were the status of the intervention group (comparison group; intervention group) and period (baseline; follow-up). The other covariates included were age; sex (male, female); place of birth (Spain and EU-15; outside the EU-15); household composition (household with children; household without children; single-person household); educational level (primary or less; secondary or higher); employment status (employed; unemployed; inactive); ability to face an unexpected financial expense of €750 or more (yes; no); and tenure status (owner, tenant, other).
The Clinical Research Ethics Committee of Parc de Salut Mar approved the study protocol (Number 2016/6681/I) and was conducted following the principles of the Declaration of Helsinki. All participants provided signed informed consent.
Statistical Analysis
Participants’ basic characteristics were compared between the intervention and comparison groups at baseline and follow-up. The existence of significant differences was tested using the chi-square test for categorical variables and the two-sample t test for continuous variables. We also examined the differences between follow-up and dropouts at baseline within groups.
Given the existence of significant differences in the composition of the groups, propensity scores for treatment at baseline were calculated by means of a binary logistic regression with adjustment by age, sex, place of birth, household composition, educational level, employment status, ability to face an unexpected expense of €750 or more and tenant status at baseline. Scores were later used to estimate inverse probability score treatment weights (IPTW) [44]. IPTW are defined as the conditional probability of being exposed to a particular treatment given the values of measured covariates and are used to achieve greater balance on observed covariates, thus creating a more appropriate comparison group. The balance achieved in observed covariates was assessed using standardised differences across intervention group status. [45] All subsequent analyses were reported weighted by IPTW.
Within-group changes between baseline and follow-up in the dichotomised outcome measures for treatment and control groups were tested using the McNemar test. Then, the significance of the difference-in-differences between the intervention and comparison groups on the outcomes was tested by adjusting several multilevel logistic regressions with random intercepts, in which the interaction between intervention status and period allowed estimation of the net effect of the intervention. Average adjusted predictions with random intercepts were calculated. From these, the average marginal effects of the intervention were estimated for each outcome, [46] with the advantage that average marginal effects can be interpreted as the effect of the intervention in terms of probability.
All statistical analyses were performed with STATA (version 15.0). The syntax used in the analysis can be consulted in the supplementary material for one of the indicators studied, and the same procedure was followed regarding the other indicators.
Results
Study Population and Baseline Characteristics
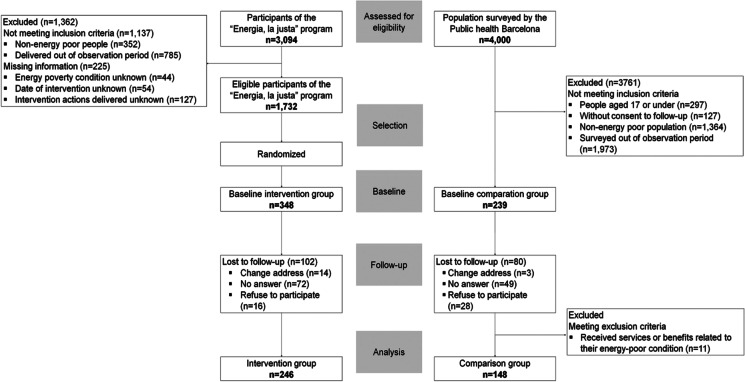
Of 3094 individuals undergoing the EJUSTA programme, 1732 met the eligibility criteria (Fig. 1). These individuals were randomised to obtain a sample of 348 in the intervention group at baseline. A total of 102 (29.3%) participants were lost to follow-up. Of 4000 potential individuals for inclusion in the comparison group, 239 persons consented to be re-contacted and met the eligibility criteria. In all, 80 (33.5%) participants were lost to follow-up and 11 (4.6%) participants excluded after the follow-up due to exclusion criteria. The sample analysed 246 and 148 people from the intervention and the comparison group, respectively. No significant differences were found within either group between participants and losses at baseline.
Fig. 1.
CONSORT chart diagram of individuals studied. EJUSTA, a quasi-experimental pre-post study of home energy-counseling visit intervention. Barcelona 2016
The intervention group were mostly female and middle-aged; half were born outside the EU-15, and most lived in households with children (Table 1). The intervened population reported high unemployment rates, low educational levels and difficulties in facing unexpected expenses. They lived mostly in rentals. The intervention and comparison groups differed significantly in all the observed characteristics. After the IPTW application, none of the characteristics showed significant differences between groups, except for the ability to face an unexpected expense of €750 or more. The mean stabilised weight was equal to 0.0026, whilst the standard deviation of the stabilised weights was equal to 0.0033. The standardised mean differences of covariates below 0.150 after IPTW confirmed the similarity between groups, except for the ability to face an unexpected expense of €750 or more (0.154).
Table 1.
Baseline characteristics for intervention and comparison group, (a) unweighted and (b) weighted by stabilised inverse probability treatment weights (IPTW)
| Unweighted | IPTW | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention group, n=246 | Comparison group, n=148 | p value | Intervention group, n=191 | Comparison group, n=194 | p value | |||||
| Sex | ||||||||||
| Women, n (%) | 177 | (72.0) | 79 | (53.5) | <0.001 | 123 | (64.6) | 116 | (59.8) | 0.170 |
| Men, n (%) | 69 | (28.1) | 69 | (46.5) | 68 | (35.4) | 78 | (40.2) | ||
| Missing | ||||||||||
| Year of birth, yyyy | ||||||||||
| Mean, (SD) | 1965 | (15.9) | 1969 | (15.9) | 0.022 | 1965 | (16.0) | 1966 | (17.1) | 0.166 |
| Range | 1917 | 1995 | 1927 | 1998 | 1917 | 1995 | 1927 | 1998 | ||
| Missing | ||||||||||
| Place of birth | ||||||||||
| Spain and EU-15, n (%) | 122 | (49.6) | 100 | (67.6) | <0.001 | 107 | (55.9) | 117 | (60.5) | 0.188 |
| Outside the EU-15, n (%) | 124 | (50.4) | 48 | (32.4) | 84 | (44.1) | 77 | (39.5) | ||
| Missing | ||||||||||
| Household composition | ||||||||||
| Household without children, n (%) | 51 | (20.7) | 54 | (36.5) | <0.001 | 56 | (29.0) | 53 | (27.3) | 0.495 |
| Household with children, n (%) | 135 | (54.9) | 81 | (54.7) | 98 | (51.5) | 96 | (49.7) | ||
| One-person household, n (%) | 60 | (24.4) | 13 | (8.8) | 37 | (19.5) | 45 | (23.0) | ||
| Missing | ||||||||||
| Educational level | ||||||||||
| Primary or less, n (%) | 157 | (63.8) | 49 | (33.1) | <0.001 | 103 | (53.7) | 97 | (50.0) | 0.283 |
| Secondary or more, n (%) | 89 | (36.2) | 99 | (66.9) | 88 | (46.3) | 97 | (50.0) | ||
| Missing | ||||||||||
| Employment status | ||||||||||
| Employed, n (%) | 56 | (23.4) | 86 | (58.1) | <0.001 | 56 | (29.5) | 68 | (34.9) | 0.191 |
| Unemployed, n (%) | 115 | (48.1) | 28 | (18.9) | 74 | (38.7) | 70 | (36.0) | ||
| Retirees and pensioners, n (%) | 39 | (16.3) | 15 | (10.1) | 39 | (20.3) | 31 | (15.9) | ||
| Others, n (%) | 29 | (12.1) | 19 | (12.8) | 22 | (11.5) | 26 | (13.2) | ||
| Missing | 7 | |||||||||
| Face unexpected expenses above 750€ | ||||||||||
| Capable, n (%) | 11 | (4.3) | 75 | (51.7) | <0.001 | 159 | (83.3) | 150 | (77.1) | 0.041 |
| Incapable, n (%) | 235 | (95.7) | 70 | (48.3) | 32 | (16.7) | 44 | (22.9) | ||
| Missing | ||||||||||
| Tenure status | ||||||||||
| Owner, n (%) | 44 | (17.9) | 68 | (47.2) | <0.001 | 54 | (28.5) | 64 | (33.0) | 0.345 |
| Tenant, n (%) | 193 | (78.5) | 76 | (52.8) | 132 | (78.9) | 127 | (65.8) | ||
| Other, n (%) | 9 | (3.7) | 4 | (2.7) | 5 | (2.6) | 3 | (1.2) | ||
| Missing | ||||||||||
All p values were derived from chi-square tests for categorical variables, except tenure statuses that were derived from the Fisher exact test, and two-sample t test for age
IPTW (inverse probability treatment weights) were estimated by logistic regression adjusted by age, sex, place of birth, household composition educational level, employment status, face unexpected expenses above 750€ and tenure status
Within-Group Changes in Energy Poverty and Health Outcomes
One year after the intervention, all 3 EP outcomes showed statistically significant improvements in the intervention group, with decreases in the inability to keep the home adequately warm in wintertime (p value < 0.001) and cool in summertime (p value < 0.001) and arrears in utility bills (p value = 0.014). In the comparison group, the only improvement was a decrease in arrears in utility bills (p value < 0.001). Health outcomes were significantly worse in both groups, although they were more severe in the intervention group, except for the frequency of use of primary care services which declined in the intervention group (p value = 0.035) but increased in the comparison group (p value < 0.001) (Table 2).
Table 2.
Changes in energy poverty and health outcomes between baseline and follow-up for the intervention and comparison groups; participants were weighted by stabilised inverse probability treatment weights (IPTW)
| Intervention group | Comparison group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Var %1 | p value2 | Baseline | Follow-up | Var %1 | p value2 | |||||
| n | % | n | % | n | % | n | % | |||||
| Energy poverty outcomes | ||||||||||||
| Inability to keep home adequately warm | 158 | 82.5 | 98 | 51.1 | 3-38.1 | < 0.001 | 90 | 46.5 | 88 | 45.5 | − 2.2 | 0.913 |
| Inability to keep home adequately cool | 129 | 67.7 | 81 | 42.2 | -37.7 | < 0.001 | 97 | 50.2 | 105 | 54.4 | 8.4 | 0.405 |
| Arrears utility bills | 120 | 62.6 | 104 | 54.2 | -13.5 | 0.014 | 108 | 56.0 | 49 | 25.4 | − 54.6 | < 0.001 |
| Health outcomes | ||||||||||||
| Self-perceived poor health | 87 | 45.7 | 102 | 53.2 | 16.4 | 0.027 | 76 | 39.4 | 90 | 46.9 | 19.1 | 0.028 |
| Depression and/or anxiety | 97 | 51.9 | 87 | 45.7 | − 11.9 | 0.096 | 58 | 30.2 | 43 | 22.8 | − 24.5 | 0.086 |
| Use of anxiolytics, antidepressants or sleeping in the last 2 days | 48 | 26.7 | 82 | 43.0 | 61.1 | < 0.001 | 37 | 18.3 | 43 | 22.6 | 23.0 | 0.035 |
| More than 3 primary care visits a year | 135 | 70.6 | 122 | 63.7 | 9-9.7 | 0.035 | 71 | 36.8 | 111 | 57.2 | 55.5 | <0.001 |
1Var%, percentage of variation=[(%Post-%Pre) / %Pre]
2The McNemar test was used
IPTW (inverse probability treatment weights) were estimated by logistic regression adjusted by age, sex, place of birth, household composition educational level, employment status, face unexpected expenses above 750€ and tenure status
Impacts of the Intervention on Energy Poverty and Health Outcomes
The difference-in-difference analysis revealed a moderate benefit in EP outcomes. The average marginal effect of the intervention increased the ability to keep warm in winter by 30.4% (95%CI: 5.8%; 55.0%) and cool in summer by 27.3% (95%CI: 8.2%; 46.4%). Although utility bill arrears decreased, the reduction was more pronounced in the comparison group, resulting in overall net effect of − 21.5% (95%CI: 2.3%; 40.7%). The impact of the intervention showed no effect on poor self-perceived health and self-reported depression and/or anxiety, and a quasi-significant modest increase of 8.6% (95%CI: − 0.1%; 17.3%) in consumption of anti-anxiety, antidepressant or sleeping pills. In contrast, the frequency of use of primary care services decreased by 27.3% (95%CI: 12.6%; 42.0%) in the intervention group compared with the comparison group 1 year after the intervention (Fig. 2).
Fig. 2.
Percentual average marginal effect estimation of the intervention and the comparison for energy poverty and health outcomes, and percentual difference-in-difference average marginal effect, weighted by stabilised inverse probability treatment weights (IPTW)
Discussion
This study provides evidence on the positive effect of information-based energy interventions on keeping homes at an adequate temperature not only in winter but also in summer in a southern city of the EU country. Moreover, the intervened population reported decreased arrears on utility bills, although it was less pronounced than the comparison group. The home energy-counseling visit had no impact on self-perceived health or self-reported anxiety or depression. However, it certainly had an effect on the reduction in visits to healthcare facilities.
The counseling intervention reduced the number of people suffering from cold homes in winter and hot homes in summer. These results may be attributable to heightened awareness of the healthy temperature required at home or legal training in energy rights, such as protection against energy supply disruptions amongst vulnerable consumers. The findings of this study support evidence from previous research, both quantitative [24, 47] and qualitative, [34, 48, 49] and provide new insights on how to reduce EP through interventions not based on improving housing energy efficiency. Thermal comfort is not simply enhanced satisfaction with ambient temperature. It also implies that households have a reduced risk of adverse physical and mental health effects. However, the study did not detect physical and psychological health improvements. In contrast, evidence was found on less frequent primary care services use, suggesting that the intervention may play a beneficial role in reducing avoidable visits to healthcare facilities, such as lowering colds, coughs and flu, [50] and dehydration and food poisoning in summer [3].
A noteworthy finding is the impact of the counseling intervention on reducing the number of households having difficulty in keeping the adequate indoor temperature in the summer. Amongst Mediterranean regions, the inability to maintain indoor thermal comfort in summer is a growing problem due to climate change. The frequency and duration of heat and its associated adverse health effects are expected to increase in both the southern and northern areas of Europe [51]. This problem is influenced by the level of income and urbanisation, with households in cities and lower income population facing the most significant issues in keeping their homes cool. [52] Information-based interventions could contribute to reducing both the inability to keep home cool and the morbidity burden associated with indoor heat. However, this effect could be more prominent if combined with other interventions. The World Health Organization has recently advocated the adoption of passive cooling measures in buildings or the use of energy-efficient active cooling systems, or other measures at the city level to reduce the heat island effect. [53]
The study revealed that the intervention decreased delays in paying basic services to a lesser extent than the non-intervened population. The results obtained show certain coherence with the findings obtained in other previous evaluations based on housing efficiency improvement interventions. [22, 24, 50, 54–58] These investigations suggested that the improvement in the energy affordability of households is not so evident, leading to reductions, [22, 24, 50, 54] although sometimes less than expected [55, 56] and even increases. [57, 58] Results could be explained by the empowerment actions in Law 24/2015, which guarantees access to energy supply to consumers at risk of residential exclusion. This law (Law 24/2015) guarantees energy supplies by preventing vulnerable consumers from being disconnected, although they accumulate an energy debt. Vulnerable consumers, such as the intervention recipients, often experienced EP along with other vital insecurities, such as housing, employment and food insecurity. [59, 60] Therefore, we cannot exclude the possibility that households surviving on limited domestic budgets may cope with the coexistence of day-to-day difficulties by adopting an energy debt accumulation strategy that enables them to allocate resources for other basic needs. Furthermore, energy rights empowerment amongst the intervened population and enhanced awareness of a healthy level of thermal comfort may influence decisions, abilities and behaviours to address EP through indebtedness. For example, there is evidence that households with children [48, 61] or chronically ill members [62] adopt practices that prioritise thermal comfort over payment of bills. This strategy may have spread to other vulnerable groups.
The study found no physical or mental health gains, except for healthcare use. Previous studies found that housing energy-efficiency interventions led to modest improvements in general health, respiratory symptoms, mental health and well-being. [4, 25–28] Further research on this type of intervention should investigate other non-life-threatening morbidity outcomes such as those noted above. In addition, future evaluations should consider assessing psychosocial factors. A previous study has suggested that improving living conditions related to EP could enhance people’s emotional state by, for example, raising the social meaning of the home [63] or encouraging greater social integration. [21, 64] Psychosocial factors could improve mental health and reduce social isolation. This issue has been previously highlighted in housing efficiency interventions [24, 27, 28] and demonstrated in the qualitative evaluation of this type of intervention. [35].
Regarding the evidence of decreased visits to primary care services, previous studies found mixed effects, ranging from no significant impacts [23, 65] to unclear results [50] or a positive reduction in the demand for medical care. [22] Reducing the number of people affected by EP is an incentive in itself. However, the evidence on reducing medical care and its associated cost may be useful for political decision-making. Therefore, further research is needed to understand mixed results and unanswered questions for different countries, regions and cities.
Limitations and Strengths
The main limitation of this study is the selection bias affecting the study population. The use of a convenience comparison group that differs considerably could affect the study’s internal validity. We used the propensity score technique to reduce these differences by equating groups based on covariates. Instead of matching in the propensity score, the IPTW strategy allowed balancing of the groups without losing information from the comparison group. [66, 67] However, a limitation is unmeasured confounding due to our inability to account for all potential variables. In addition, the sample size was insufficient to study the effectiveness of the intervention considering a possible heterogeneity in the implementation process. Likewise, a larger sample would also have allowed examining the effect of the intervention by social inequality axes such as gender, age and ethnic group, amongst others.
Another limitation to highlight is the sensitivity of the self-reported health outcomes used. Although the mental health disorder indicators employed are notable for the high concordance between the clinical diagnosis and the self-reported values, they could be less sensitive to changes than other mental health scales. The study assessed a small number of health outcomes. We did not include other outcomes, such as exacerbations of respiratory diseases (e.g. asthma or chronic bronchitis) or common illnesses (e.g. coughs, colds or influenza), although the primary care proxy used may be indicative of these outcomes.
Despite these limitations, this study provides an important contribution to public health and social policies because, to the best of our knowledge, it is the first study contextualised in the southern EU that rigorously examines the effect of information-based interventions on health, as well as on EP. The quasi-experimental study with a comparison group used confers greater realism and ecological validity to the results obtained. [44, 68]
Conclusion
The results suggest the intervention successfully reduced EP in the short term amongst vulnerable populations. The long-term impact of the intervention has been unexplored but is undoubtedly limited since it does not modify the structural factors underlying the phenomenon. However, compared to other housing energy-efficiency improvement measures, it can be applied quickly, easily and economically.
From a public health perspective, two main general approaches can be followed to reduce the impacts of energy poverty on health: (1) a high-risk strategy in which the population experiencing fuel poverty is addressed; (2) a population strategy that intends to improve conditions related to housing, energy access and quality, and material living conditions in the whole population to ‘shift the curve’ and prevent EP from happening from the beginning. [69, 70]. We believe that both are needed to reduce the EP’s significant impacts on health and health inequalities. Given the magnitude of PE in Spain and other southern European countries, housing energy-efficiency improvement programmes are necessary. However, because of the need to intervene urgently on vulnerable populations, it should be combined with information-based energy programmes to be responsive in the short term, whilst the former are being implemented.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank the Associació Benestar i Desenvolupament and the Associació Ecoserveis for their support, particularly to Mònica Plana Izquierdo.
Funding
The study was partly funded by a research grant from the Carlos III Institute of Health, Ministry of Economy and Competitiveness (Spain), awarded on the 2015 call under the Health Strategy Action 2013-2016, within the National Research Programme oriented to Societal Challenges, within the Technical, Scientific and Innovation Research National Plan 2013-2016, with reference PI15/02006, co-funded with European Union ERDF funds (European Regional Development Fund).
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Liddell C, Morris C, Thomson H, Guiney C. Excess winter deaths in 30 European countries 1980–2013: a critical review of methods. Journal of Public Health. 2015;38(4):fdv184. doi: 10.1093/pubmed/fdv184. [DOI] [PubMed] [Google Scholar]
- 2.Healy J. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Community Health. 2003;57(10):784–789. doi: 10.1136/jech.57.10.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jessel S, Sawyer S, Hernández D. Energy, poverty, and health in climate change: a comprehensive review of an emerging literature. Front Pub Health. 2019;7. 10.3389/fpubh.2019.00357. [DOI] [PMC free article] [PubMed]
- 4.Liddell C, Morris C. Fuel poverty and human health: a review of recent evidence. Energy Policy. 2010;38(6):2987–2997. doi: 10.1016/j.enpol.2010.01.037. [DOI] [Google Scholar]
- 5.Marmot Review Team. The health impacts of cold homes and fuel poverty. Vol. 342. Friends of the Earth & the Marmot Review Team; 2011. http://www.instituteofhealthequity.org/projects/the-health-impacts-of-cold-homes-and-fuel-poverty/the-health-impacts-of-cold-homes-and-fuel-poverty-fullreport.pdf. Accessed 17 Apr 2020.
- 6.Liddell C, Guiney C. Living in a cold and damp home: frameworks for understanding impacts on mental well-being. Public Health. 2015;129(3):191–199. doi: 10.1016/j.puhe.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 7.Kovats RS, Ebi KL. Heatwaves and public health in Europe. Eur J Pub Health. 2006;16(6):592–599. doi: 10.1093/eurpub/ckl049. [DOI] [PubMed] [Google Scholar]
- 8.Thomson H, Simcock N, Bouzarovski S, Petrova S. Energy poverty and indoor cooling: an overlooked issue in Europe. Energy and Buildings. 2019;196:21–29. doi: 10.1016/j.enbuild.2019.05.014. [DOI] [Google Scholar]
- 9.Pye S, Dobbins A. Energy poverty and vulnerable consumers in the energy sector across the EU : analysis of policies and measures. 2015
- 10.Bouzarovski S. Energy poverty in the European Union: landscapes of vulnerability. Wiley Interdis Rev: Energy Environ. 2014;3(3):276–289. doi: 10.1002/wene.89. [DOI] [Google Scholar]
- 11.Recalde M, Peralta A, Oliveras L, et al. Structural energy poverty vulnerability and excess winter mortality in the European Union: exploring the association between structural determinants and health. Energy Policy. 2019;133:110869. doi: 10.1016/j.enpol.2019.07.005. [DOI] [Google Scholar]
- 12.Institute for Energy Diversification and Saving - IDAE. Project Sech-Spahousec, Analysis of the energetic consumption of the residential sector in Spain (Proyecto Sech-Spahousec, Análisis del consumo energético del sector residencial en España). Idae. Published online 2016:76.
- 13.Leibfried S. Towards a European welfare state. In: Jones C, ed. New perspectives on the welfare state in Europe. 133. Routledge London; 1993. 10.4324/9780203415863
- 14.Tirado S, Jiménez L. Energy poverty, crisis and austerity in Spain. People Place and Policy Online. 2016;10(1):42–56. doi: 10.3351/ppp.0010.0001.0004. [DOI] [Google Scholar]
- 15.Carrere J, Peralta A, Oliveras L, López MJ, Marí-Dell’Olmo M, Benach J, Novoa AM. Energy poverty, its intensity and health in vulnerable populations in a Southern European city. Gaceta Sanitaria. 2021;35(5):438–444. doi: 10.1016/j.gaceta.2020.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Fowler T, Southgate RJ, Waite T, et al. Excess winter deaths in Europe: a multi-country descriptive analysis. Eur J Pub Health. 2015;25(2):339–345. doi: 10.1093/eurpub/cku073. [DOI] [PubMed] [Google Scholar]
- 17.Creutzfeldt N, Gill C, McPherson R, Cornelis M. The social and local dimensions of governance of energy poverty: adaptive responses to state remoteness. J Consum Policy. 2020:1–24. 10.1007/s10603-019-09442-z.
- 18.Ministerio para la Transición Ecológica. Estrategia Nacional Contra La Pobreza Energética 2019–2024. 2019. https://www.diba.cat/documents/14465/91063194/20190405+estrategianacionalcontralapobrezaenergetica2019-2024_tcm37-496282.pdf/99c07ec6-a72d-4949-b7d2-0d874ce6a347. Accessed 23 May 2020.
- 19.Kyprianou I, Serghides DK, Varo A, Gouveia JP, Kopeva D, Murauskaite L. Energy poverty policies and measures in 5 EU countries: a comparative study. Energy Build. 2019;196:46–60. doi: 10.1016/j.enbuild.2019.05.003. [DOI] [Google Scholar]
- 20.Critchley R, Gilbertson J, Grimsley M, Green G. Living in cold homes after heating improvements: evidence from Warm-Front, England’s Home Energy Efficiency Scheme. Appl Energy. 2007;84(2):147–158. doi: 10.1016/j.apenergy.2006.06.001. [DOI] [Google Scholar]
- 21.Gilbertson J, Stevens M, Stiell B, Thorogood N. Home is where the hearth is: grant recipients’ views of England’s home energy efficiency scheme (Warm Front) Soc Sci Med. 2006;63(4):946–956. doi: 10.1016/j.socscimed.2006.02.021. [DOI] [PubMed] [Google Scholar]
- 22.Gilbertson J, Grimsley M, Green G. Psychosocial routes from housing investment to health: evidence from England’s home energy efficiency scheme. Energy Policy. 2012;49:122–133. doi: 10.1016/j.enpol.2012.01.053. [DOI] [Google Scholar]
- 23.Heyman B, Harrington B, Heyman A. A randomised controlled trial of an energy efficiency intervention for families living in fuel poverty. Hous Stud. 2011;26(1):117–132. doi: 10.1080/02673037.2010.512787. [DOI] [Google Scholar]
- 24.Grey C, Jiang S, Nascimento C, et al. The short-term health and psychosocial impacts of domestic energy efficiency investments in low-income areas: a controlled before and after study. BMC Public Health. 2017;17(1):1–10. doi: 10.1186/s12889-017-4075-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thomson H, Petticrew M, Morrison D. Health effects of housing improvement: systematic review of intervention studies. BMJ (Clin Res ed) 2001;323(7306):187–190. doi: 10.1136/bmj.323.7306.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomson H, Thomas S, Sellstrom E, Petticrew M. The health impacts of housing improvement: a systematic review of intervention studies from 1887 to 2007. Am J Public Health. 2009;99(Suppl 3):S681–S692. doi: 10.2105/AJPH.2008.143909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thomson H, Thomas S, Sellstrom E, Petticrew M. Housing improvements for health and associated socio-economic outcomes. Thomson H, ed. The Cochrane database of systematic reviews. 2013;2(3):CD008657. 10.1002/14651858.CD008657.pub2 [DOI] [PubMed]
- 28.Maidment CD, Jones CR, Webb TL, Hathway EA, Gilbertson JM. The impact of household energy efficiency measures on health: a meta-analysis. Energy Policy. 2014;65:583–593. doi: 10.1016/j.enpol.2013.10.054. [DOI] [Google Scholar]
- 29.Armstrong B, Bonnington O, Chalabi Z, et al. The impact of home energy efficiency interventions and winter fuel payments on winter- and cold-related mortality and morbidity in England: a natural equipment mixed-methods study. 2018;6. 10.3310/phr06110 [PubMed]
- 30.Iparraguirre J. Have winter fuel payments reduced excess winter mortality in England and Wales? J Public Health (Oxf) 2015;37(1):26–33. doi: 10.1093/pubmed/fdu063. [DOI] [PubMed] [Google Scholar]
- 31.Frank D, Neault N, Skalicky A, et al. Heat or eat: the Low Income Home Energy Assistance Program and nutritional and health risks among children less than 3 years of age. Pediatrics. 2006;118(5). 10.1542/peds.2005-2943 [DOI] [PubMed]
- 32.Reeves A. Exploring local and community capacity to reduce fuel poverty: the case of home energy advice visits in the UK. Energies. 2016;9(4). 10.3390/en9040276
- 33.Lorenc A, Pedro L, Badesha B, Dize C, Fernow I, Dias L. Tackling fuel poverty through facilitating energy tariff switching: a participatory action research study in vulnerable groups. Public Health. 2013;127(10):894–901. doi: 10.1016/j.puhe.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 34.Jacques-Aviñó C, Dvorzak JL, Marí-Dell’Olmo M, et al. Qualitative evaluation of an intervention to reduce energy poverty. Rev Saude Publica. 2019;53:62. 10.11606/s1518-8787.2019053001212. [DOI] [PMC free article] [PubMed]
- 35.Boardman B, Darby S. Effective advice: energy efficiency and the disadvantaged. Oxford: Environmental Change Institute: University of Oxford; 2000. [Google Scholar]
- 36.Barcelona Public Health Agency. La Salut a Barcelona 2016.; 2016.
- 37.Tudor J. The inverse care law. The Lancet. 1971;297(7696):405–412. doi: 10.1016/S0140-6736(71)92410-X. [DOI] [PubMed] [Google Scholar]
- 38.Bouzarovski S, Petrova S. A global perspective on domestic energy deprivation: overcoming the energy poverty-fuel poverty binary. Energy Res Soc Sci. 2015;10:31–40. doi: 10.1016/j.erss.2015.06.007. [DOI] [Google Scholar]
- 39.Healy J. Housing, fuel poverty and health: a pan-European analysis. London: Ashgate Publishers; 2004.
- 40.Bartoll X, Baranda L, González JM, et al. Manual Metodològic de l’Enquesta de Salut de Barcelona 2016/17. Barcelona: ASPB Publisher; 2018.
- 41.Gilbertson J, Green G. Warm front - better health: health impact evaluation of the Warm Front Scheme. Sheffield: Sheffield Hallam University; 2008.
- 42.Quesnel-Vallée A. Self-rated health: caught in the crossfire of the quest for “true” health? Int J Epidemiol. 2007;36(6):1161–1164. doi: 10.1093/ije/dym236. [DOI] [PubMed] [Google Scholar]
- 43.De Sanjosé S, Antó J, Alonso J. Comparación de la información obtenida en una encuesta de salud por entrevista con los registros de Atención Primaria. Gac Sanit. 1991;27:260–264. doi: 10.1016/s0213-9111(91)71078-9. [DOI] [PubMed] [Google Scholar]
- 44.D’Agostino R. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17(19):2265–2281. doi: 10.1002/(SICI)1097-0258(19981015)17:19<2265::AID-SIM918>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 45.Carroll M, Sutherland G, Kemp-Casey A, Kinner SA. Agreement between self-reported healthcare service use and administrative records in a longitudinal study of adults recently released from prison. Health and Justice. 2016;4(1). 10.1186/s40352-016-0042-x [DOI] [PMC free article] [PubMed]
- 46.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J:Promot Commu Stat Stata. 2012;12(2):308–331. doi: 10.1177/1536867X1201200209. [DOI] [Google Scholar]
- 47.Howden-Chapman PL, Chandola T, Stafford M, Marmot M. The effect of housing on the mental health of older people: the impact of lifetime housing history in Whitehall II. BMC Public Health. 2011;11(1):682. doi: 10.1186/1471-2458-11-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harrington B, Heyman B, Merleau-Ponty N, Stockton H, Ritchie N, Heyman A. Keeping warm and staying well: findings from the qualitative arm of the Warm Homes Project. Health Soc Care Community. 2005;13(3):259–267. doi: 10.1111/j.1365-2524.2005.00558.x. [DOI] [PubMed] [Google Scholar]
- 49.Grey C, Schmieder-Gaite T, Jiang S, Nascimento C, Poortinga W. Cold homes, fuel poverty and energy efficiency improvements: a longitudinal focus group approach. Indoor and Built Environ. 2017;26(7):1420326X1770345. doi: 10.1177/1420326X17703450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Howden-Chapman P, Matheson A, Crane J, et al. Effect of insulating existing houses on health inequality: cluster randomised study in the community. BMJ (Clin Res ed) 2007;334(7591):460. doi: 10.1136/bmj.39070.573032.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gasparrini A, Guo Y, Sera F, et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health. 2017;1(9):e360–e367. doi: 10.1016/S2542-5196(17)30156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Braubach M, Fairburn J. Social inequities in environmental risks associated with housing and residential location–a review of evidence. Eur J Pub Health. 2010;20(1):36–42. doi: 10.1093/eurpub/ckp221. [DOI] [PubMed] [Google Scholar]
- 53.WHO Regional Office for Europe. Environmental Health Inequalities in Europe. Second Assessment Report. Copenhagen: WHO Regional. Office for Europe; 2019.
- 54.Howden-Chapman P, Crane J, Matheson A, et al. Retrofitting houses with insulation to reduce health inequalities: aims and methods of a clustered, randomised community-based trial. Soc Sci Med (1982) 2005;61(12):2600–2610. doi: 10.1016/j.socscimed.2005.04.049. [DOI] [PubMed] [Google Scholar]
- 55.Green G, Ormandy D, Brazier J, Gilbertson J. Tolerant buildings: the impact of energy efficiency measures on living conditions and health status. In: Cutting the cost of cold: affordable warmth for healthier homes. London: E & FN Spon: 2000. pp. 87–103.
- 56.Lloyd CR, Callau MF, Bishop T, Smith IJ. The efficacy of an energy efficient upgrade program in New Zealand. Energy and Buildings. 2008;40(7):1228–1239. doi: 10.1016/j.enbuild.2007.11.006. [DOI] [Google Scholar]
- 57.Shortt N, Rugkåsa J. “The walls were so damp and cold” fuel poverty and ill health in Northern Ireland: results from a housing intervention. Health Place. 2007;13(1):99–110. doi: 10.1016/j.healthplace.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 58.Pretlove S, Critchley R, Howard R, Oreszczyn T. The Nottingham energy, health and housing study: reducing relative humidity, dust mites and asthma. Build Serv Eng Res Technol. 2002;23(1):43–55. doi: 10.1191/0143624402bt030oa. [DOI] [Google Scholar]
- 59.Hulse K, Saugeres L. Housing insecurity and precarious living: an Australian exploration. AHURI Final Report. 2008;124:1–51. [Google Scholar]
- 60.Hernandez D, Phillips D, Siegel EL. Exploring the housing and household energy pathways to stress: a mixed methods study. Int J Environ Res Pub Health. 2016;13(9). 10.3390/ijerph13090916 [DOI] [PMC free article] [PubMed]
- 61.Tod AM, Nelson P, De Chavez AC, Homer C, Powell-Hoyland V, Stocks A. Understanding influences and decisions of households with children with asthma regarding temperature and humidity in the home in winter: a qualitative study. BMJ Open. 2016;6(1):9636. doi: 10.1136/bmjopen-2015-009636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wright F. Old and cold: older people and policies failing to address fuel poverty. Soc Policy Admin. 2004;38(5):488–503. doi: 10.1111/j.1467-9515.2004.00403.x. [DOI] [Google Scholar]
- 63.Bonnefoy X. Inadequate housing and health: an overview. Int J Environ Pollut. 2007;30(3/4):411–429. doi: 10.1504/IJEP.2007.014819. [DOI] [Google Scholar]
- 64.Willand N, Ridley I, Maller C. Towards explaining the health impacts of residential energy efficiency interventions - a realist review. Part 1: Pathways. Soc Sci Med. 2015;133:191–201. doi: 10.1016/j.socscimed.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 65.Walker J, Mitchell R, Petticrew M, Platt S. The effects on health of a publicly funded domestic heating programme: a prospective controlled study. J Epidemiol Commun Health. 2009;63(1):12–17. doi: 10.1136/jech.2008.074096. [DOI] [PubMed] [Google Scholar]
- 66.Austin P, Stuart E. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–3679. doi: 10.1002/sim.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stuart E, Huskamp H, Duckworth K, et al. Using propensity scores in difference-in-differences models to estimate the effects of a policy change Blue Cross Blue Shield of Massachusetts Blue Cross Blue Shield of Massachusetts. Health Services Outcomes Res Methodol. 2015;14(4):166–182. doi: 10.1007/s10742-014-0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wing C, Simon K, Bello-Gomez RA. Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health. 2018;39(1):453–469. doi: 10.1146/annurev-publhealth-040617-013507. [DOI] [PubMed] [Google Scholar]
- 69.Benach J, Malmusi D, Yasui Y, Martínez JM. A new typology of policies to tackle health inequalities and scenarios of impact based on Rose’s population approach. J Epidemiol Commun Health. 2013;67(3):286–291. doi: 10.1136/jech-2011-200363. [DOI] [PubMed] [Google Scholar]
- 70.McLaren L, McIntyre L, Kirkpatrick S. Rose’s population strategy of prevention need not increase social inequalities in health. Int J Epidemiol. 2010;39(2):372–377. doi: 10.1093/ije/dyp315. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.