Abstract
Infants born with low or high (“at-risk”) birthweights are at greater risk of adverse health outcomes across the life course. Our objective was to examine whether geographic hotspots of low and high birthweight prevalence in New York City had different patterns of neighborhood risk factors. We performed census tract–level geospatial clustering analyses using (1) birthweight prevalence and maternal residential address from an all-payer claims database and (2) domains of neighborhood risk factors (socioeconomic and food environment) from national and local datasets. We then used logistic regression analysis to identify specific neighborhood risk factors associated with low and high birthweight hotspots. This study examined 2088 census tracts representing 419,025 infants. We found almost no overlap (1.5%) between low and high birthweight hotspots. The majority of low birthweight hotspots (87.2%) overlapped with a socioeconomic risk factor and 95.7% overlapped with a food environment risk factor. Half of high birthweight hotspots (50.0%) overlapped with a socioeconomic risk factor and 48.8% overlapped with a food environment risk factor. Low birthweight hotspots were associated with high prevalence of excessive housing cost, unemployment, and poor food environment. High birthweight hotspots were associated with high prevalence of uninsured persons and convenience stores. Programs and policies that aim to prevent disparities in infant birthweight should examine the broader context by which hotspots of at-risk birthweight overlap with neighborhood risk factors. Multi-level strategies that include the neighborhood context are needed to address prenatal pathways leading to low and high birthweight outcomes.
Introduction
Infants born with low (less than 2500 g) or high (greater than 4000 g) birthweights are at greater risk for adverse health outcomes at birth and across the life course (e.g., neonatal hypoglycemia, obesity, and cardiometabolic disease in children and adults) [1–3]. Low infant birthweight is thought to be driven by individual-level prenatal risk factors such as prematurity or hypertension, which are exacerbated by parent-/family-level racial/socioeconomic disparities and chronic stress [4]. At a neighborhood level, low infant birthweight has been associated with poor neighborhood housing conditions and lower neighborhood support [5, 6]. Neighborhood factors associated with high infant birthweight have received less attention. Individual-level prenatal risk factors for high infant birthweight include increased maternal body mass index, gestational diabetes, and excessive gestational weight gain [7]. Neighborhood fast food access, neighborhood overcrowding, and unemployment are all associated with maternal risk factors for high birthweight, such as excessive gestational weight gain [8, 9]. Past studies have missed opportunities to look at neighborhood risk factors with low and high birthweight together as potential “at-risk” birthweights to disentangle whether different prenatal neighborhood environments are associated with low and high birthweight outcomes.
In New York City (NYC), racial/socioeconomic disparities in low birthweight are well documented [10], as are NYC-specific geographic disparities in weight outcomes across the life course [11–13]. Less is known about whether there are high-risk geographic clusters of where mothers who deliver infants with at-risk birthweights live, and whether these areas overlap with socioeconomic and food environment risk factors at a neighborhood level. Domains of neighborhood risk factors previously associated with prenatal and cardiovascular outcomes [14–18] include (1) socioeconomic conditions, which include social (e.g., overcrowding, stable housing) and economic (e.g., unemployment, lack of health insurance) conditions and (2) food environment (e.g., fast food restaurants, convenience stores). To understand how the prenatal neighborhood environment may play a role in birthweight outcomes, we conducted an ecological study to assess relationships between hotspot distributions of at-risk birthweight prevalence, socioeconomic conditions, and the food environment in NYC. We then assessed which individual neighborhood risk factors (e.g., unemployment rates, fast food restaurants) predicted hotspots of low or high birthweight. We hypothesized that (1) hotspot distribution of at-risk birthweights would overlap with the hotspot distribution of neighborhood risk factors (socioeconomic conditions and food environment) and (2) low and high birthweight hotspots would be associated with different prenatal neighborhood risk factors.
Methods
Study Design
Our target population included single livebirths born in NYC. We assessed distribution of hotspots (statistically significant geospatial clustering) of at-risk birthweight prevalence (low and high) by geocoded residential census tract, socioeconomic conditions, and food environment. Prenatal neighborhood environment was assessed at the domain level (socioeconomic conditions, food environment) and at the individual risk factor level (e.g., excessive housing cost, fast food restaurants—definitions below). We then built multivariable logistic regression models to examine if high prevalence of neighborhood risk factors were associated with hotspots of low and high birthweights, adjusting for sociodemographic covariates.
Target Population and Data Sources
We obtained data from the Statewide Planning and Research Cooperative System (2011–2014), an all-payer claims database administered by the New York State Department of Health [19]. The database contains infant birthweight and each patient’s home address, which we geocoded to census tract. We performed a sensitivity analysis comparing all single live births with a subsample excluding premature live births with similar results. We included all single live births without exclusions for prematurity.
We obtained socioeconomic conditions and demographic covariate variables using data from the American Community Survey (2009–2013) provided by City Health Dashboard, which compiles neighborhood data from multiple national and state sources [20, 21]. We obtained food environment data using inspection records (2009–2013) from the NYC Department of Health and Mental Hygiene and the New York State Department of Agriculture and Markets. [13, 22].
Low and High Birthweights
The main outcomes were low and high birthweight prevalence, calculated by dividing the number of low or high birthweight newborns by the total number of newborns per census tract. Low birthweight, as defined by the World Health Organization, was defined as a birthweight below 2500 g. [23] High birthweight, as defined by prior literature, was defined as a birthweight greater than 4000 g. [7] We excluded likely erroneous birthweights of above 5000 g and below 500 g as per prior birthweight literature. [24].
Socioeconomic Conditions
We included the following 4 census tract–level socioeconomic risk factors: excessive housing cost, crowded housing, unemployment, and uninsured persons. As defined by the American Community Survey [21] and as examined in previous literature [6], the following definitions were used: (1) excessive housing cost was defined by a percentage estimate of households where over 30% of household income was spent on housing costs; (2) crowded housing was defined by a percentage estimate of households with more than one person per room; (3) unemployment was defined by a percentage estimate of the population ≥ 16 years old unemployed but seeking work; (4) uninsured persons was defined by a percentage estimate of lack of health insurance among people aged 0–64 years.
Food Environment
We included 2 census tract–level food environment risk factors: prevalence of fast food restaurants and convenience food stores. We used the New York State Department of Agriculture and Markets licensing and inspection data to characterize the food environment. After excluding non-restaurants and collapsing observations to unique restaurants by name and location, fast food restaurants were defined as venues marked as “fast food,” “take-out,” or “counter service only.” Fast food prevalence was defined as the percentage of these venues categorized as fast food in a census tract as per prior literature [12, 13]. Similarly, we calculated the prevalence of convenience stores as the percentage of retail food stores categorized as small convenience stores as per prior literature. [12, 13].
Neighborhood Demographic Covariates
We assessed basic demographic covariates from the American Community Survey [21]: % Hispanic, % non-Hispanic Black, % female, % children under the age of 18, and median household income.
Statistical Analysis
We used the Getis-Ord Gi-star statistic [25] to identify hotspots where variable prevalence demonstrated statistically significant geospatial clustering. We chose this statistical method because it quantifies geospatial patterns by analyzing each geographic unit in relation to its neighboring areas to identify statistically significant clusters of high or low values. In our analysis, we used a distance band of 1 mile to define neighboring features, a confidence level of 95%, and a false discovery rate correction to account for multiple comparisons. We defined overlap as when one census tract was a hotspot for multiple variables. To identify areas of increased socioeconomic risk factors, we counted the number of overlapping socioeconomic risk factor hotspots for each census tract from 0 (no risk factor hotspots) to 4 (census tract a hotspot for all 4 risk factors). To identify areas of increased food environment risk factors, we counted the number of overlapping food environment hotspots for each census tract from 0 (no risk factor hotspots) to 2 (census tract a hotspot for both fast food and convenience stores).
We performed logistic regressions to identify predictors of low and high birthweight hotspots. To represent high prevalence and to focus on areas with significant disparities, we dichotomized neighborhood risk factors at the highest prevalence quartile (e.g., above 75th percentile for prevalence of excessive housing cost). Selecting our demographic covariates a priori, we tested factors for multicollinearity prior to inclusion in our model.
Of the 2167 census tracts in NYC, we excluded tracts deemed inappropriate for analysis, such as those with no population (e.g., airports and parks—40 tracts) and those with less than 30 births between 2011 and 2014 (30 tracts) or missing information (9 tracts). Our final sample included 2088 census tracts (96% of total).
We used ArcGIS Desktop 10.3.1 (ESRI, Redlands, Calif, 2015) to perform geographic analyses and Stata/SE version 15.1 (Stata Corp, College Station, TX) to perform statistical analyses. This study protocol was approved by the Institutional Review Board at NYU Grossman School of Medicine.
Results
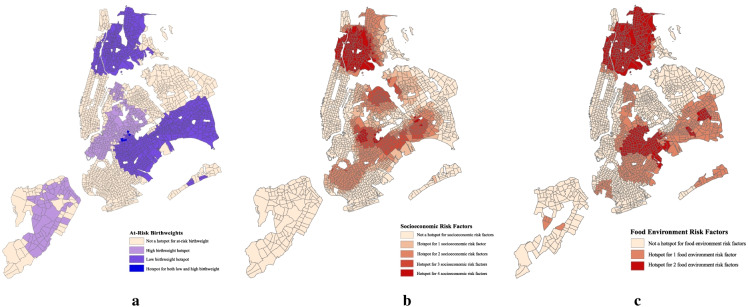
This study included 419,025 single live infants. Table 1 is a descriptive summary of NYC census tracts. Mean prevalence of low and high birthweight were similar (6.3% vs. 6.8%, respectively). The prevalence of infants born premature was 6.0% (n = 25,012). Figure 1 displays overlap of risk factors by domain with at-risk birthweight hotspots. Table 2 displays overlap of individual risk factors with at-risk birthweight hotspots. In NYC, we identified hotspots of low and high birthweight in 38.1% and 16.0% of total census tracts, respectively. Low and high birthweight hotspots had minimal overlap (1.5%).
Table 1.
Descriptive summary of New York City census tracts (n = 2088)
| Birthweight outcomes, mean prevalence (median, IQR) | |
| Low birthweight (< 2500 g) | 6.3% (6.2%, 4.5–7.9%) |
| High birthweight (≥ 4000 g) | 6.8% (6.6%, 5.3–8.1%) |
| At-risk birthweight1 | 13.1% (13.1%, 11.1–15.1%) |
| Socioeconomic conditions, mean prevalence (median, IQR) | |
| Excessive housing cost2 | 49.1% (49.2%, 41.6–56.6%) |
| Crowded housing3 | 9.2% (7.6%, 3.7–13.1%) |
| Unemployment4 | 10.9% (9.8%, 6.9–13.8%) |
| Uninsured5 | 15.4% (14.7%, 9.4–20.1%) |
| Food Environment, mean prevalence (median, IQR) | |
| Fast food restaurants6 | 70.3% (71.4%, 58.9–81.8%) |
| Convenience stores7 | 80.0% (82.2%, 74.3–88.1%) |
| Demographic covariates, mean prevalence (median, IQR) | |
| Hispanic persons | 26.6% (18.0%, 8.9–39.7%) |
| Black, non Hispanic persons | 26.3% (10.0%, 1.8–45.1%) |
| Female sex | 52.3% (52.3%, 49.5–55.0%) |
| Children8 | 21.6% (21.4%, 16.8–26.0%) |
| Median income9 | 57,392 (52,769, 37,931–71,612) |
1Prevalence of high or low birthweight
2Households where ≥ 30% of household income is spent on housing costs
3More than 1 persons per room
4Persons aged ≥ 16 years unemployed but seeking work
5Current lack of health insurance among people aged 0–64 years
6Proportion of restaurants within census tract categorized as fast food
7Proportion of retail food stores within census tract categorized as convenience stores
8Persons aged ≤ 18 years old
9Census tract median income in US dollars
Fig. 1.
New York City census tract map of birthweight and prenatal neighborhood environment. Hotspots where prevalence estimates cluster at a confidence level of 95%. a 1Hotspots of high birthweight (> 4000 g) or low birthweight (< 2500 g); b 2Hotspots of socioeconomic risk factors: excessive housing cost (> 30% income), crowded (> 1 person/ room), unemployment (> 16 years old seeking work), uninsured (between 0 and 64 years old); c 3Hotspots of food environment risk factors: fast food restaurants, convenience stores
Table 2.
Overlap of neighborhood risk factors and at-risk birthweight hotspots
| All census tracts (%) |
Low birthweight hotspots1 (% overlap) |
High birthweight hotspots2 (% overlap) |
|
|---|---|---|---|
| Socioeconomic conditions | |||
| Excessive housing cost3 | 42.8 | 77.5 | 17.7 |
| Crowded housing4 | 33.6 | 40.7 | 21.0 |
| Unemployment5 | 32.5 | 75.8 | 12.9 |
| Uninsured6 | 31.9 | 40.5 | 47.6 |
| Food environment | |||
| Fast food7 | 44.7 | 94.1 | 16.1 |
| Convenience stores8 | 35.4 | 61.3 | 46.0 |
Geographic hotspots identified using the Getis-Ord Gi-star statistic where prevalence estimates demonstrated statistically significant clustering at a confidence level of 95%
1Infants born < 2500 g
2Infants born ≥ 4000 g
3Households where ≥ 30% of household income is spent on housing costs
4More than 1 persons per room
5Persons aged ≥ 16 years unemployed but seeking work
6Current lack of health insurance among people aged 0–64 years
7Proportion of restaurants within census tract categorized as fast food
8Proportion of retail food stores within census tract categorized as convenience stores
Low Birthweight Hotspots
The majority of low birthweight hotspots (87.2%) overlapped with a hotspot for at least 1 socioeconomic risk factor, and 73.5% overlapped with at least 2 risk factors. Almost all low birthweight hotspots (95.7%) overlapped with a hotspot for at least 1 food environment risk factor, and 59.7% overlapped with both risk factors. In decreasing order (Table 2), low birthweight hotspots had highest overlap with hotspots of fast food restaurants (94.1%), excessive housing cost (77.5%), and unemployment (75.8%).
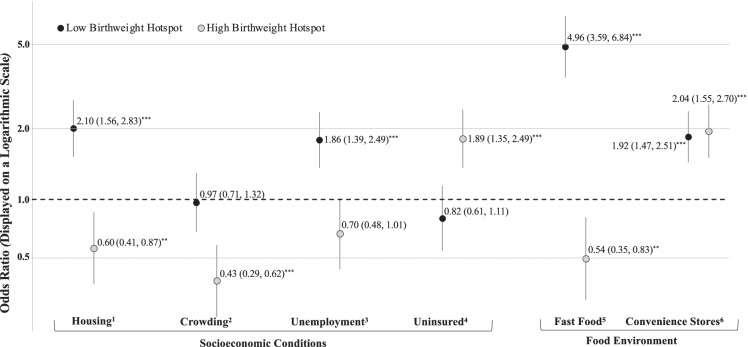
In our logistic regression model (Fig. 2), consistent with neighborhood risk factors with high overlap, we found that among socioeconomic risk factors, census tracts with the highest quartile prevalence of excessive housing cost and unemployment had 2.10 (95% CI 1.56, 2.83) and 1.86 (95% 1.39, 2.49), respectively, increased odds of being a low birthweight hotspot. Among food environment risk factors, census tracts with the highest quartile prevalence of fast food restaurants and convenience stores had 4.96 (95% CI 3.59, 6.84) and 1.92 (95% CI 1.47, 2.51) increased odds of being a low birthweight hotspot. Among our covariates, census tracts with the highest quartile prevalence of Hispanic and Black persons had increased odds of being a low birthweight hotspot (4.79 [95% CI 3.46, 6.63] and 7.07 [95% CI 5.01, 9.97], respectively).
Fig. 2.
Neighborhood risk factors associated with hotspots of at-risk birthweights. Y-axis depicted on a logarithmic scale for visual accuracy; Logistic regression [aOR (95% CI), *p < 0.05; **p < 0.01; ***p < 0.001]; factors dichotomized at highest quartile prevalence, model also includes age, sex, race/ethnicity, income; 1% excessive housing cost (> 30% income); 2% crowded (> 1 person/ room); 3% unemployment (> 16 years old seeking work); 4% uninsured (between 0 and 64 years old)
High Birthweight Hotspots
Compared to 87.2% of low birthweight hotspots, half of high birthweight hotspots (50.0%) overlapped with hotspots for at least 1 socioeconomic risk factor, and 27.0% overlapped with at least 2 risk factors. Almost half of high birthweight hotspots (48.8%) overlapped with at least 1 food environment risk factor, and 14.4% overlapped with both risk factors. High birthweight hotspots had highest overlap (Table 2) with neighborhood risk factors distinct from the low birthweight hotspots: uninsured persons (47.6%) and convenience stores (46.0%).
In our logistic regression model (Fig. 2), among socioeconomic risk factors, we found census tracts with highest quartile prevalence of uninsured persons had 1.89 (95% CI 1.39, 2.56) increased odds of being a high birthweight hotspot, while excessive housing cost and crowded housing did not increase odds of being a high birthweight hotspot. Among food environment risk factors, we found Census tracts with the highest quartile prevalence of convenience stores had 2.04 (95% CI 1.55, 2.70) increased odds of being a high birthweight hotspot while fast food restaurants did not increase odds of being a high birthweight hotspot. Among our covariates, census tracts with the highest quartile prevalence of Black persons had decreased odds of being a high birthweight hotspot (0.46 [95% CI 0.29, 0.74]).
Discussion
In this study, we examined geographic patterns in the prenatal neighborhood environment and prevalence of at-risk birthweights. We found that low and high birthweight hotspots had minimal overlap, consistent with previous knowledge describing different prenatal low and high birthweight individual-/family-level risk factors [2]. Our study expands these findings to show that these pathways extend to different distinguishable geographic distributions. The vast majority of low birthweight hotspots overlapped with neighborhood risk factors, specifically excessive housing cost, unemployment, fast food restaurants, and convenience stores. Prior studies have shown that higher stress cortisol levels [26] are associated with lower birthweight, and perhaps multiple neighborhood risk factors synergistically increase population stress levels, increasing low birthweight prevalence.
Associations between high birthweight hotspots and neighborhood risk factors were less consistent. Only about half of high birthweights hotspots overlapped with neighborhood risk factors in either domain, including specific associations with uninsured persons and convenience stores. These findings are different from prior literature identifying associations between neighborhood fast food access and gestational weight gain [18], which may reflect unmeasured sociocultural differences that drive both high birthweight and where people live in NYC. Overall, we found that distinct prenatal neighborhood environments are associated with low and high birthweight hotspots, suggesting that influencing the neighborhood context of at-risk birthweights may require examination of specific risk factors with specific birthweight outcomes.
We found associations between low birthweight, housing, and unemployment, confirming associations previously found on the individual level [15, 27]. Excessive housing cost likely leads to housing instability, well documented in the longstanding housing crisis in NYC [28]. A community with high levels of housing instability and high resident turnover may decrease opportunities to create mutually supportive social networks that can mitigate psychological stressors during pregnancy. Future studies should incorporate a multi-level design to examine relationships between housing instability, social support, and birthweight outcomes to inform prenatal interventions designed to stabilize social support networks as well as policy agendas to increase stable housing during critical developmental periods. Prior studies have described associations between preterm births, another reflection of at-risk prenatal conditions, and state-level unemployment [15]. Our findings expand descriptions of the impact of neighborhood-level unemployment to include clustering of low birthweight prevalence. As economic factors such as unemployment tend to fluctuate, future studies may consider a longitudinal design to capture relationships between shifting prenatal neighborhood economic disparities and birthweight outcomes.
We found that census tracts with high prevalence of uninsured persons were associated with being a high birthweight hotspot. While being uninsured on an individual level conveys more than double the odds of delayed prenatal care [17], this would perpetuate both low and high birthweight outcomes. Rather, our neighborhood findings may highlight a specific socioeconomic threshold where family incomes are too high to qualify for Medicaid but not stable enough for secure health coverage, resulting in an insurance coverage gap. Prior work shows that uninsured populations are largely young, without access to insurance through work (e.g., self-employed), and Hispanic [29]. Future studies may consider geographically targeted qualitative analysis to understand unmeasured sociocultural differences in prenatal dietary practices in high birthweight hotspots. Pregnant mothers with similar income levels, shared sociocultural backgrounds, and practices may be more likely to live close to one another. Gaining a detailed understanding of prenatal dietary practices that influence high birthweight in the context of a shared neighborhood and community setting would inform home-based strategies to optimize healthy prenatal dietary practices.
Our findings in the food environment also show differences between low and high birthweight prenatal neighborhood environments. High prevalence of fast food restaurants was associated with low birthweight hotspots and inversely related to high birthweight hotspots. In contrast, while low birthweight and fast food intake has not been studied, prior work has shown that individual fast food intake is associated with maternal gestational weight gain, a risk factor for high birthweight [9]. Rather than capture individual-level behaviors, our findings may reflect how racial and income segregation influences fast food restaurant placement [30, 31]. Both low and high birthweight hotspots were associated with convenience stores, supporting previous work that convenience store density reflects neighborhood-level poverty [32]. In NYC in particular, investments into local convenience stores to promote healthy foods have demonstrated early success in promoting healthier purchases [33]. Given that increased prevalence of convenience stores may be in hotspots of at-risk birthweights, neighborhood programs may consider using convenience stores as a setting for neighborhood interventions to improve healthy practices during pregnancy.
Our models also showed that race/ethnicity prevalence is associated with birthweight outcomes, aligning with well-established evidence around racial/ethnic disparities in birthweight [6, 10, 11]. Given that prior work has identified geospatial racial segregation as potential trigger for increased fast food density [30, 31], future study design should consider investigating how structural inequalities in the neighborhood built environment may contribute to birthweight outcomes.
Barker proposed 35 years ago that adverse birthweight outcomes increase susceptibility to cardiometabolic syndromes [34]. Our findings meaningfully expand this body of work by suggesting that prenatal neighborhood risk factors play a role in adverse cardiometabolic programming by contributing to adverse birthweight outcomes. To date, interventions addressing cardiometabolic outcomes by preventing child obesity have largely focused on a parent-/family-level interventions to improve parenting behaviors, without fully integrating neighborhood risk factors [35]. A multi-level approach is needed to integrate the work of geospatial epidemiology and clinical interventional work to integrate parent-level with neighborhood-level strategies to reduce the impact of socioeconomic disparities. For example, primary care may integrate social needs screening programs to connect parents to neighborhood social services, or to identify families who need intensified programming during key developmental periods to buffer neighborhood stressors. On a policy level, geographic analyses such as ours could be used to direct programs such as the NYC “Food Retail Expansion to Support Health” intervention [36], which offer incentives to food retailers that lower the cost of maintaining retail supermarket space and to develop neighborhood partnerships targeting patients who are at greatest risk.
Key limitations to the interpretation of our findings include the ecological nature of the study, unclear duration of residence in census tracts, potential bias in spatial clustering, and unmeasured variables. Associations were conducted on the census tract level, and no conclusions can be drawn at the individual level nor can directionality be assessed. We also do not know how long families have lived at the address we used for analysis, but research thus far reflects that when individuals are displaced due to a lack of affordable housing, they tend to move to similar neighborhoods [37]. Our analysis was limited by potential bias from spatial clustering across census tracts meaning that similar exposures tend to cluster spatially, which can affect assumptions of independence among observations. Other unmeasured factors may also confound the associations that we identified. However, our conceptual model was grounded in selected variables with prior evidence relevant to our study. This study draws from data of over 400,000 newborn infants with rich neighborhood data, providing an important framework to conduct future multi-level studies that integrate data on the individual, family, and neighborhood level. Our findings can be used to guide future cohort studies to delineate causal pathways between salient variables and multi-level mechanisms around high and low birthweight within the context of the prenatal neighborhood environment.
Conclusion
In NYC, the geographic distributions of low and high birthweights have different patterns of overlap with neighborhood risk factors. Low birthweight hotspots have a higher overall concentration of overlap with neighborhood risk factor hotspots and associations with excessive housing cost, unemployment, and poor food environment. High birthweight hotspots were associated with high prevalence of uninsured persons and convenience stores. These findings reflect different prenatal neighborhood environments for low and high birthweight hotspots. Interventions to prevent adverse health outcomes that originate in at-risk birthweights should address both overall level of prenatal neighborhood risk as well as target-specific risk factors to address low and high birthweight outcomes.
Acknowledgements
This work was supported by a training grant by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health 2KL2TR001446-06 and grants from the National Institutes of Diabetes and Digestive and Kidney Diseases R01DK097347 and R01DK108682 to study the impact of the food and built environment on childhood obesity. These funding sources had no involvement in conducting the research or in preparing this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Holtrop PC. The frequency of hypoglycemia in full-term large and small for gestational age newborns. Am J Perinatol. 1993;10(2):150–154. doi: 10.1055/s-2007-994649. [DOI] [PubMed] [Google Scholar]
- 2.Cnattingius S, Villamor E, Lagerros YT, Wikström AK, Granath F. High birth weight and obesity—a vicious circle across generations. Int J Obes. 2012;36(10):1320–1324. doi: 10.1038/ijo.2011.248. [DOI] [PubMed] [Google Scholar]
- 3.Ligi I, Grandvuillemin I, Andres V, Dignat-George F, Simeoni U. Low Birth weight infants and the developmental programming of hypertension: a focus on vascular factors. Semin Perinatol. 2010;34(3):188–192. doi: 10.1053/j.semperi.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Krans EE, Davis MM. Preventing low birthweight: 25 years, prenatal risk, and the failure to reinvent prenatal care. Am J Obstet Gynecol. 2012;206(5):398–403. doi: 10.1016/j.ajog.2011.06.082. [DOI] [PubMed] [Google Scholar]
- 5.Buka SL, Brennan RT, Rich-Edwards JW, Raudenbush SW, Earls F. Neighborhood support and the birth weight of urban infants. Am J Epidemiol. 2003;157(1):1–8. doi: 10.1093/aje/kwf170. [DOI] [PubMed] [Google Scholar]
- 6.Zuberi A, Duck W, Gradeck B, Hopkinson R. Neighborhoods, race, and health: examining the relationship between neighborhood distress and birth outcomes in Pittsburgh. J Urban Aff. 2016;38(4):546–563. doi: 10.1111/juaf.12261. [DOI] [Google Scholar]
- 7.Ouzounian JG, Hernandez GD, Korst LM, et al. Pre-pregnancy weight and excess weight gain are risk factors for macrosomia in women with gestational diabetes. J Perinatol. 2011;31(11):717–721. doi: 10.1038/jp.2011.15. [DOI] [PubMed] [Google Scholar]
- 8.Headen I, Mujahid M, Deardorff J, Rehkopf DH, Abrams B. Associations between cumulative neighborhood deprivation, long-term mobility trajectories, and gestational weight gain. Health Place. 2018;52:101–109. doi: 10.1016/j.healthplace.2018.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu ZM, Van Blyderveen S, Schmidt L, et al. Predictors of gestational weight gain examined as a continuous outcome: a prospective analysis. Journal of Women’s Health. Published online January 13, 2021. doi:10.1089/jwh.2020.8799 [DOI] [PubMed]
- 10.Howell EA, Hebert P, Chatterjee S, Kleinman LC, Chassin MR. Black/white differences in very low birth weight neonatal mortality rates among New York City hospitals. Pediatrics. 2008;121(3):e407–415. doi: 10.1542/peds.2007-0910. [DOI] [PubMed] [Google Scholar]
- 11.Grady SC. Racial disparities in low birthweight and the contribution of residential segregation: a multilevel analysis. Soc Sci Med. 2006;63(12):3013–3029. doi: 10.1016/j.socscimed.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 12.Osorio M, Koziatek CA, Gallagher MP, et al. Concordance and discordance in the geographic distribution of childhood obesity and pediatric type 2 diabetes in New York City. Acad Pediatr. 2020;20(6):809–815. doi: 10.1016/j.acap.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elbel B, Tamura K, McDermott ZT, Wu E, Schwartz AE. Childhood obesity and the food environment: a population-based sample of public school children in New York City. Obesity. 2020;28(1):65–72. doi: 10.1002/oby.22663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, et al. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med. 2013;95:106–114. doi: 10.1016/j.socscimed.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cole TJ, Donnet ML, Stanfield JP. Unemployment, birthweight, and growth in the first year. Arch Dis Child. 1983;58(9):717–721. doi: 10.1136/adc.58.9.717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Melki IS, Beydoun HA, Khogali M, Tamim H, Yunis KA. Household crowding index: a correlate of socioeconomic status and inter-pregnancy spacing in an urban setting. J Epidemiol Community Health. 2004;58(6):476–480. doi: 10.1136/jech.2003.012690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenberg D, Handler A, Rankin KM, Zimbeck M, Adams EK. Prenatal care initiation among very low-income women in the aftermath of welfare reform: does pre-pregnancy Medicaid coverage make a difference? Matern Child Health J. 2007;11(1):11–17. doi: 10.1007/s10995-006-0077-z. [DOI] [PubMed] [Google Scholar]
- 18.Phelan S, Marquez F, Redman LM, et al. The moderating role of the built environment in prenatal lifestyle interventions. International Journal of Obesity. Published online February 26, 2021:1–5. 10.1038/s41366-021-00782-w [DOI] [PMC free article] [PubMed]
- 19.Statewide Planning and Research Cooperative System. Accessed May 1, 2021. https://www.health.ny.gov/statistics/sparcs/
- 20.Gourevitch MN, Athens JK, Levine SE, Kleiman N, Thorpe LE. City-level measures of health, health determinants, and equity to foster population health improvement: the city health dashboard. Am J Public Health. 2019;109(4):585–592. doi: 10.2105/AJPH.2018.304903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bureau UC. 2009–2013 ACS 5-year estimates. The United States Census Bureau. Accessed May 1, 2021. https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2013/5-year.html
- 22.New York State Department of Agriculture and Markets Bureau of Community Environmental Health and Food Protection. Food Service Establishment: Last Inspection. Accessed September 12, 2019. https://data.ny.gov/ Economic-Development/Retail-Food-Stores/9a8c-vfzj
- 23.Cutland CL, Lackritz EM, Mallett-Moore T, et al. Low birth weight: case definition & guidelines for data collection, analysis, and presentation of maternal immunization safety data. Vaccine. 2017;35(48Part A):6492–6500. doi:10.1016/j.vaccine.2017.01.049 [DOI] [PMC free article] [PubMed]
- 24.Savitz DA, Bobb JF, Carr JL, et al. Ambient fine particulate matter, nitrogen dioxide, and term birth weight in New York. New York Am J Epidemiol. 2014;179(4):457–466. doi: 10.1093/aje/kwt268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Getis A, Ord JK. The analysis of spatial association by use of distance statistics. Geogr Anal. 1992;24(3):189–206. doi: 10.1111/j.1538-4632.1992.tb00261.x. [DOI] [Google Scholar]
- 26.Bolten MI, Wurmser H, Buske-Kirschbaum A, Papoušek M, Pirke KM, Hellhammer D. Cortisol levels in pregnancy as a psychobiological predictor for birth weight. Arch Womens Ment Health. 2011;14(1):33–41. doi: 10.1007/s00737-010-0183-1. [DOI] [PubMed] [Google Scholar]
- 27.Carrion BV, Earnshaw VA, Kershaw T, et al. Housing instability and birth weight among young urban mothers. J Urban Health. 2015;92(1):1–9. doi: 10.1007/s11524-014-9913-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Plunz R. A history of housing in New York City. Columbia University Press; 2018. Accessed May 29, 2021. http://www.degruyter.com/document/doi/10.7312/plun17834/html
- 29.Tolbert J, Orgera K, Damico, Anthony. Key Facts about the uninsured population. Kaiser Family Foundation; 2020. Accessed August 12, 2021. https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population/
- 30.Kwate NOA. Fried chicken and fresh apples: racial segregation as a fundamental cause of fast food density in black neighborhoods. Health Place. 2008;14(1):32–44. doi: 10.1016/j.healthplace.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 31.Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. Am J Prev Med. 2004;27(3):211–217. doi: 10.1016/j.amepre.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 32.Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007;44(3):189–195. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 33.Dannefer R, Williams DA, Baronberg S, Silver L. Healthy bodegas: increasing and promoting healthy foods at corner stores in New York City. Am J Public Health. 2012;102(10):e27–e31. doi: 10.2105/AJPH.2011.300615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barker D, Osmond C. Infant mortality, childhood nutrition, ischaemic heart disease in England and Wales. The Lancet. 1986;327(8489):1077–1081. doi: 10.1016/S0140-6736(86)91340-1. [DOI] [PubMed] [Google Scholar]
- 35.Dietz WH. We need a new approach to prevent obesity in low-income minority populations. Pediatrics. 2019;143(6). doi:10.1542/peds.2019-0839 [DOI] [PubMed]
- 36.Cohen N. REFRESH: modifying the food retail expansion to support health program to improve healthy food access. CUNY Urban Food Policy Institute; 2018. Accessed September 1, 2021. https://www.cunyurbanfoodpolicy.org/news/2018/7/16/refesh-policy-brief
- 37.Desmond M, Shollenberger T. Forced displacement from rental housing: prevalence and neighborhood consequences. Demography. 2015;52(5):1751–1772. doi: 10.1007/s13524-015-0419-9. [DOI] [PubMed] [Google Scholar]