Abstract
Vegetation may influence asthma exacerbation through effects on aeroallergens, localized climates, air pollution, or children’s behaviors and stress levels. We investigated the association between residential vegetation and asthma exacerbation by conducting a matched case–control study based on electronic health records of asthma patients, from the Children’s Hospital of Philadelphia (CHOP). Our study included 17,639 exacerbation case events and 34,681 controls selected from non-exacerbation clinical visits for asthma, matched to cases by age, sex, race/ethnicity, public payment source, and residential proximity to the CHOP main campus ED and hospital. Overall greenness, tree canopy, grass/shrub cover, and impervious surface were assessed near children’s homes (250 m) using satellite imagery and high-resolution landcover data. We used generalized estimating equations to estimate odds ratios (OR) and 95% confidence intervals (CI) for associations between each vegetation/landcover measure and asthma exacerbation, with adjustment for seasonal and sociodemographic factors—for all cases, and for cases defined by diagnosis setting and exacerbation frequency. Lower odds of asthma exacerbation were observed in association with greater levels of tree canopy near the home, but only for children who experienced multiple exacerbations in a year (OR = 0.94 per 10.2% greater tree canopy coverage, 95% CI = 0.90–0.99). Our findings suggest possible protection for asthma patients from tree canopy, but differing results by case frequency suggest that potential benefits may be specific to certain subpopulations of asthmatic children.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11524-022-00633-7.
Keywords: Pediatric asthma, Greenspace, Trees, Built environment
Introduction
Asthma, one of the most common chronic conditions in children, is among the top contributors to childhood disability and a major cause of pediatric hospitalization [1–3]. There are large disparities associated with asthma. Black children and those living in poverty are more likely to have prevalent asthma and experience asthma morbidity, as reflected in emergency department (ED) visits and hospitalizations [1, 4]. Acute care visits for asthma are also more frequent among children living in urban areas compared to suburbs, particularly in urban neighborhoods with high poverty rates [5]. The influence of urban neighborhood environments on asthma morbidity has been little studied, with the exception of studies linking air pollution levels to asthma exacerbation [6]. Identification of built environment characteristics that influence asthma symptoms may present tangible intervention opportunities by targeting modifiable features of neighborhoods.
Trees and other vegetation (i.e., greenspace) may affect asthma symptoms—either positively or negatively—through effects on aeroallergen levels, localized climates (e.g., heat islands), or air pollution concentrations, or by reducing stress and promoting outdoor activity, among other possible pathways [7]. Depending on the underlying pathways, an effect of vegetation on asthma symptoms may also differ by biological host factors that affect the child’s responsiveness/susceptibility to potential protection or risks conferred by vegetation. For instance, our own prior research found strong associations between tree pollen and higher odds of asthma exacerbation among asthma patients who also had allergic rhinitis [8]. Research on the effect of residential vegetation on asthma exacerbation has produced mixed results to date [9–16], likely due to widely different greenspace exposure measures and definitions of asthma exacerbation/symptoms across the studies. Further research on this topic is warranted, given strong findings of both harms and benefits from vegetation that require clarification—especially given high prevalence of childhood asthma and the corresponding potential for considerable public health impact from this knowledge. If living near a certain amount or type of vegetation is protective against asthma exacerbation, this information may be useful for supporting widespread greening efforts in cities. It is furthermore important to understand whether any influence of vegetation differs by race/ethnicity or socioeconomic status, as such information may inform on whether interventions could reduce disparities in asthma morbidity.
We studied the association between neighborhood vegetation and contemporaneous odds of exacerbation among children with diagnosed asthma living in the City of Philadelphia, who were treated in a large pediatric health system. Philadelphia is an important setting for our study, as a major metropolitan area with among the highest rates of childhood asthma in the USA [17, 18], vast disparities in asthma prevalence across neighborhoods [19], and considerable variability in greenspace [20]. We assessed several vegetation and landcover measures near children’s homes, including overall greenness, tree canopy, grass/shrub vegetation, and impervious surface, and estimated associations of the vegetation measures with asthma exacerbation events from different treatment settings and by exacerbation frequency. We also explored possible modification of associations by children’s characteristics including age, sex, and comorbidities, as well as social determinants such as race/ethnicity and neighborhood sociodemographics.
Methods
Study Population
We conducted a matched case–control study of residential neighborhood vegetation in relation to odds of asthma exacerbation among children (< 18 years old) with diagnosed asthma living in the City of Philadelphia, using electronic health records (EHR) from the Children’s Hospital of Philadelphia (CHOP), from 2011 through 2016. The study population was selected from patients who utilized the CHOP system for regular asthma care; within each calendar year, children were eligible if they had at least 1 non-exacerbation asthma diagnosis from a visit to one of the 31 CHOP primary care practices during the year. Case and control visits were selected from these eligible children within each year, as follows (Fig. 1):
Fig. 1.
Selection of case and control visits for study of neighborhood environmental risk factors for asthma exacerbation in Philadelphia children
Cases
An asthma exacerbation case was defined as a face-to-face physician visit (outpatient, ED, or inpatient) in a CHOP facility with a diagnosis code for asthma and a linked prescription of systemic steroid [21]. The full set of asthma diagnosis codes we used has been reported previously [22]. Cases were selected from three different treatment settings: outpatient, ED, and inpatient. If a child had more than one case visit within 7 days, only one visit was retained (with prioritization of inpatient > ED > outpatient visits), to ensure that the cases were independent exacerbation events. If a child had more than one case visit within the same treatment setting during the calendar year, we randomly selected one encounter from that treatment setting. The same child could be counted as a case up to three times per calendar year, once for each of the treatment setting case types.
Controls
Controls were selected from non-exacerbation clinical visits (visits resulting in an asthma diagnosis but no systemic steroid prescription). A separate set of control visits was selected for each treatment setting case type, but a child with a case event during the year was not eligible to also be selected as a control for that case type. For each case type within each year, all eligible control visits were randomly narrowed to one per patient; then, we selected 2 control visits per case, without replacement. Control visits were matched to cases by age (2-year categories), sex (female, male), race/ethnicity (Hispanic, non-Hispanic Black, non-Hispanic white, other), payment source (Medicaid/sCHIP vs. private/self-pay/other), and a measure for census tract-level probability of using the CHOP main campus ED/hospital [23] (categorized by cutpoints at the tenths decimal place, with low-frequency categories combined: 0 to < 0.3, 0.3 to < 0.4, 0.4 to < 0.6, 0.6 to < 0.7, 0.7 to < 0.8, 0.8 to < 1.0). These matching factors were chosen primarily to enhance comparability of controls to cases with regard to clinical care utilization (frequency and clinical setting).
We restricted our study to children living in Philadelphia. The residential address of the child, recorded for each clinical encounter, was geocoded and assigned to a 30-m × 30-m grid and to a 2010 census tract. These geographic assignments were used to link spatial information to the case and control visits.
Vegetation Measures
We characterized several vegetation and landcover measures, linked to children’s residential locations at the time of their clinical encounters. We hypothesized that vegetation near the home would have more of an impact on asthma exacerbation than vegetation at a greater distance, so we summarized each vegetation variable within a 250-m-radius (approximate) circular buffer around the home—the smallest spatial resolution common to the vegetation variables in our database.
Overall Greenness
Overall greenness was characterized by the normalized difference vegetation index (NDVI), a measure of the density (or intensity) of vegetation within an areal unit, calculated based on reflectance properties of vegetation. Values range from − 1 (water) to 1 (highest vegetation density). NDVI was derived from images of the Moderate-Resolution Imaging Spectroradiometer of NASA’s Terra satellite (MOD13Q1, version 6 product) [24]. The MOD13Q1 provides 250-m-resolution 16-day composite images, which we used to calculate the seasonal median NDVI value within a 250-m buffer.
Tree Canopy and Grass/Shrub Cover
Different types of vegetated landcover were characterized using high-resolution data (1 m) from the University of Vermont Spatial Analysis Laboratory [25, 26]. These data were derived from Light Detection and Ranging (LiDAR) data and orthoimagery, using object-based image analysis (OBIA). The assessment assigned each 1-m pixel to 1 of 12 mutually exclusive landcover categories, based on “leaf-on” imagery for 2013. We used these data to calculate the percentage of land area within a 250-m buffer that was covered by tree canopy, and separately for low vegetation, scrub/shrub, and emergent wetlands (shortened as “grass/shrub”).
Impervious Surface
Landcover with impervious surface was used to represent lack of vegetation or other natural landcover (e.g., soil). This variable was calculated using 30-m grid classification of impervious surface from the National Land Cover Database for the year 2011 [27], summarized as the percentage impervious surface in an approximate 250-m buffer area.
Covariates
Patient and Clinical Data
We obtained children’s sociodemographic and clinical data from the EHR, including sex and race/Hispanic ethnicity, and encounter-specific variables for age and payment source/insurance. Information was also available on patient’s medical history, including comorbidities and asthma medications.
Census Tract Sociodemographics
Data from the U.S. Census (5-year estimates of the American Community Survey (ACS) for each year of the study) [28] were used to indicate neighborhood sociodemographics, including tract-level population density and racial composition (% Hispanic, % non-Hispanic Black). We also used a variable to represent census tract-level socioeconomic status (SES), created as an index from variables representing education, occupation, income, interest/dividend income, and median housing value [29].
Air Pollution
Census tract-level estimates of daily PM2.5 were obtained from EPA’s Downscaler model [30, 31].
Climate
Meteorological data from NOAA [32] included daily values for mean temperature and total precipitation. We assigned to each case the data from the monitor closest to their address.
Statistical Analysis
We used generalized estimating equations (GEE) to fit marginal models that accounted for repeated visits within patients. GEE with a logit link and independent correlation matrix were used to estimate odds ratios (OR) and 95% confidence intervals (CI) for associations between vegetation measures and odds of asthma exacerbation (proc GENMOD in SAS v. 9.4). Associations were estimated for all cases combined, as well as for each treatment setting case type (outpatient, ED, inpatient). We also classified asthma exacerbation cases by the child’s number of exacerbation events (of any type) during the calendar year, as infrequent (only 1) or frequent (> 1), and conducted analyses of these two separate case groups with their matched controls. Each vegetation measure was modeled separately as categories split by quartiles (with lowest category as referent) and as a continuous measure. The models included variables defining each matching stratum (indicator variables for each matching variable category and terms for multiplicative interactions between all matching variables), as well as covariates selected a priori as potential confounders: calendar month and day-of-week of the clinical visit, and census tract-level population density and SES index (each categorized by percentiles (p) among all cases and controls as ≤ 25p, > 25p to < 50p, > 50 to 75p, > 75 to 90p, > 90p). In a sensitivity analysis, we also evaluated confounding by ambient environmental factors which are closely intertwined with urban vegetation including daily mean temperature, total precipitation, and fine particulate matter air pollution (PM2.5). These exposures were each evaluated as short-term (average of the value on the exacerbation date and 1-day prior) and seasonal measures (average of the daily values within each season of each calendar year).
Effect modification was evaluated among all cases and controls by estimating the vegetation-exacerbation association within each category of the potential modifier variable. We tested the statistical significance of effect modification by the p-value for an interaction term between the continuous vegetation measure and the covariate level (vs. the association within the lowest covariate category). Potential effect modifiers considered were children’s characteristics we hypothesized to be related to biological responsiveness/susceptibility to vegetation because of their influence on exacerbation rates (age, sex, allergic rhinitis, eczema, inhaled steroid prescription) and sociodemographics including child’s race/ethnicity, public payer for clinical visit, and census tract-level population density, % Hispanic, % non-Hispanic Black, and SES index.
Results
Our study of neighborhood vegetation in relation to asthma exacerbation included 17,639 total cases from outpatient (N = 7853 visits, 5344 children), ED (N = 5522 visits, 3881 children), and inpatient (N = 4264 admissions, 3098 children) clinical settings (Table 1). Due to matching, case visits (all combined) were similar to controls in distributions of age, sex, race/ethnicity, public payment source, and probability of using the CHOP main campus. On average, ED and inpatient cases were younger and more likely to use the CHOP main campus than were outpatient cases, and higher proportions were non-Hispanic Black or had a public payer for the clinical visit. Despite differences, all three treatment setting case types were closely matched to their own control groups (not shown).
Table 1.
Characteristics of case and control visits (median (75th–25th percentile) or N (%))
| Characteristic | All controls (N = 34,681) |
All cases (N = 17,639) |
Outpatient cases (N = 7853) |
ED cases (N = 5522) |
Inpatient cases (N = 4264) |
Matched factor, modeling covariate, or main exposure |
|---|---|---|---|---|---|---|
| Child’s age | 5.85 (6.02) | 5.81 (5.98) | 6.34 (6.07) | 5.65 (5.83) | 5.01 (5.88) | Matched |
| Child’s sex | Matched | |||||
| Female | 13,964 (40.3) | 7102 (40.3) | 3229 (41.1) | 2177 (39.4) | 1696 (39.8) | |
| Male | 20,717 (59.7) | 10,537 (59.7) | 4624 (58.9) | 3345 (60.6) | 2568 (60.2) | |
| Child’s race/ethnicity | Matched | |||||
| Hispanic/Latinx | 1487 (4.3) | 835 (4.7) | 438 (5.6) | 226 (4.1) | 171 (4.0) | |
| Black, non-Hispanic | 29,711 (85.7) | 14,915 (84.6) | 6249 (79.6) | 4915 (89.0) | 3751 (88.0) | |
| White, non-Hispanic | 2013 (5.8) | 1085 (6.1) | 715 (9.1) | 197 (4.6) | 173 (4.0) | |
| Other/multiple/unknown | 1470 (4.2) | 804 (4.6) | 451 (5.7) | 184 (3.3) | 169 (4.0) | |
| Public payment source | Matched | |||||
| No | 8451 (24.4) | 4371 (24.8) | 2176 (27.7) | 1231 (22.3) | 964 (22.6) | |
| Yes | 26,230 (75.6) | 13,268 (75.2) | 5677 (72.3) | 4291 (77.7) | 3300 (77.4) | |
| Probability of using CHOP main campus | 0.72 (0.29) | 0.72 (0.29) | 0.70 (0.37) | 0.73 (0.18) | 0.73 (0.21) | Matched |
| Month of clinical visit | Covariate | |||||
| January | 2953 (8.5) | 1549 (8.8) | 764 (9.7) | 441 (8.0) | 344 (8.1) | |
| February | 2806 (8.1) | 1462 (8.3) | 726 (9.2) | 416 (7.5) | 320 (7.5) | |
| March | 2942 (8.5) | 1833 (10.4) | 774 (9.9) | 612 (11.1) | 447 (10.5) | |
| April | 2907 (8.4) | 1681 (9.5) | 716 (9.1) | 537 (9.7) | 428 (10.0) | |
| May | 2832 (8.2) | 1690 (9.6) | 742 (9.4) | 522 (9.4) | 426 (10.0) | |
| June | 2600 (7.5) | 907 (5.1) | 397 (5.1) | 294 (5.3) | 216 (5.1) | |
| July | 2322 (6.7) | 703 (4.0) | 287 (3.7) | 222 (4.0) | 194 (4.6) | |
| August | 2771 (8.0) | 867 (4.9) | 361 (4.6) | 263 (4.8) | 243 (5.7) | |
| September | 2996 (8.6) | 1474 (8.4) | 597 (7.6) | 471 (8.5) | 406 (9.5) | |
| October | 3383 (9.7) | 1677 (9.5) | 774 (9.9) | 540 (9.8) | 363 (8.5) | |
| November | 3201 (9.2) | 1808 (10.2) | 771 (9.8) | 605 (11.0) | 432 (10.1) | |
| December | 2968 (8.6) | 1988 (11.3) | 944 (12.0) | 599 (10.9) | 445 (10.4) | |
| Day-of-week | Covariate | |||||
| Monday | 6681 (19.2) | 3273 (18.6) | 1641 (20.9) | 938 (17.0) | 694 (16.3) | |
| Tuesday | 7148 (20.6) | 3197 (18.1) | 1622 (20.7) | 880 (16.0) | 695 (16.3) | |
| Wednesday | 6650 (19.2) | 2866 (16.2) | 1459 (18.6) | 786 (14.2) | 621 (14.6) | |
| Thursday | 6655 (19.2) | 2646 (15.0) | 1383 (17.6) | 709 (12.8) | 554 (13.0) | |
| Friday | 5743 (16.6) | 2345 (13.3) | 1149 (14.6) | 661 (12.0) | 535 (12.5) | |
| Saturday or Sunday | 1804 (5.2) | 3312 (18.8) | 599 (7.6) | 1548 (28.0) | 1165 (27.3) | |
| Census tract population density (per km2) | Covariate | |||||
| ≤ 6399 | 8707 (25.1) | 4489 (25.5) | 2148 (27.4) | 1289 (23.3) | 1052 (24.7) | |
| > 6399 to 8360 | 8662 (25.0) | 4365 (24.7) | 1852 (23.6) | 1433 (26.0) | 1080 (25.3) | |
| > 8360 to 10,284 | 8597 (24.8) | 4433 (25.1) | 1839 (23.4) | 1476 (26.7) | 1118 (26.2) | |
| > 10,284 to 13,353 | 5148 (14.8) | 2694 (15.3) | 1165 (14.8) | 877 (15.9) | 652 (15.3) | |
| > 13,353 | 3567 (10.3) | 1658 (9.4) | 849 (10.8) | 447 (8.1) | 362 (8.5) | |
| Census tract SES index (percentile) | Covariate | |||||
| ≤ 25th | 8727 (25.2) | 4486 (25.4) | 1831 (23.3) | 1516 (27.4) | 1139 (26.7) | |
| > 25th to ≤ 50th | 8354 (24.1) | 4634 (26.3) | 1870 (23.8) | 1540 (27.9) | 1224 (28.7) | |
| > 50th to ≤ 75th | 8830 (25.4) | 4273 (24.2) | 1929 (24.6) | 1335 (24.2) | 1009 (23.7) | |
| > 75th to ≤ 90th | 5275 (15.2) | 2509 (14.2) | 1299 (16.5) | 693 (12.6) | 517 (12.1) | |
| > 90th | 3495 (10.1) | 1737 (9.9) | 924 (11.8) | 438 (7.9) | 375 (8.8) | |
| Overall greenness (NDVI) | 0.24 (0.16) | 0.24 (0.16) | 0.23 (0.17) | 0.24 (0.15) | 0.24 (0.15) | Main exposure |
| Tree canopy cover (%) | 12.7 (10.2) | 12.7 (10.2) | 12.7 (11.2) | 12.7 (9.1) | 12.7 (9.6) | Main exposure |
| Grass/shrub cover (%) | 10.7 (6.6) | 11.2 (6.1) | 11.1 (6.6) | 11.2 (5.6) | 11.2 (6.1) | Main exposure |
| Impervious surface (%) | 73.0 (15.0) | 72.9 (14.8) | 72.6 (16.6) | 73.2 (13.3) | 73.1 (14.2) | Main exposure |
ED, emergency department; CHOP, Children’s Hospital of Philadelphia; SES, socioeconomic status
Numbers included in modeling of vegetation measures, after excluding observations with missing values for census tract SES index (39 case visits (0.22%) and 91 control visits (0.26%))
Asthma exacerbation occurred most frequently during the winter months (November, December)—most notably for outpatient cases—and ED and inpatient cases also had another peak in the spring (March). Cases were more likely than controls to occur on weekend days, mostly due to large proportions of ED and inpatient cases on weekends. ED and inpatient cases generally lived in census tracts with higher population density and lower SES than controls, whereas outpatient cases lived in higher-SES tracts than controls. The distributions of overall greenness and tree canopy cover (median and interquartile range (75th–25th percentiles)) were nearly identical between cases and controls, whereas grass/shrub cover was higher among cases than among controls. Impervious surface coverage was similar between all cases and all controls, but was lower among outpatient cases, and slightly higher among ED and inpatient cases, compared to all controls.
Vegetation levels near children’s Philadelphia residences (within 250-m buffer) varied considerably by child- and neighborhood-level sociodemographic characteristics (shown in Table 2 for all controls). Overall greenness and tree cover trended higher for non-Hispanic white children than for other race/ethnicity groups (e.g., tree cover 75p: 29.4% in non-Hispanic Whites, 18.8% in non-Hispanic Blacks, 15.2% in Hispanics). In contrast, levels of grass/shrub cover were generally highest for non-Hispanic Black children. Impervious landcover was somewhat paradoxically highest among non-Hispanic White children for the 75th percentile level and above. Distributions of all the vegetation measures were lower among children with a public payer for their clinical visit and those living in high population density census tracts, with an opposite distribution for impervious landcover. Overall greenness and tree cover trended lower in low SES compared to high SES census tracts (e.g., tree cover 75p: 37.1% in high SES tracts, 17.3% in low SES tracts), whereas little difference was seen for grass/shrub cover by SES (e.g., grass/shrub cover 75p: 14.7% in both high and low SES tracts).
Table 2.
Distributions of vegetation measures (250-m buffer) among controls, by child and census tract sociodemographic characteristics
| Vegetation measure percentiles | ||||
|---|---|---|---|---|
| 25th | 50th | 75th | 90th | |
| Overall greenness (NDVI) | ||||
| Black, non-Hispanic | 0.17 | 0.25 | 0.32 | 0.41 |
| White, non-Hispanic | 0.10 | 0.18 | 0.35 | 0.52 |
| Hispanic | 0.11 | 0.19 | 0.28 | 0.37 |
| Public payment source—no | 0.17 | 0.26 | 0.36 | 0.47 |
| Public payment source—yes | 0.16 | 0.24 | 0.31 | 0.39 |
| Census tract population density—lowa | 0.22 | 0.31 | 0.42 | 0.52 |
| Census tract population density—higha | 0.08 | 0.13 | 0.18 | 0.23 |
| Census tract SES index—lowa | 0.18 | 0.26 | 0.32 | 0.38 |
| Census tract SES index—higha | 0.15 | 0.25 | 0.41 | 0.53 |
| Tree canopy cover (%) | ||||
| Black, non-Hispanic | 9.1 | 13.2 | 18.8 | 27.9 |
| White, non-Hispanic | 5.6 | 11.7 | 29.4 | 48.2 |
| Hispanic | 5.1 | 9.6 | 15.2 | 24.4 |
| Public payment source—no | 9.6 | 15.2 | 24.4 | 37.6 |
| Public payment source—yes | 8.1 | 12.2 | 17.8 | 26.4 |
| Census tract population density—lowa | 12.2 | 18.8 | 30.5 | 44.2 |
| Census tract population density—higha | 3.0 | 5.1 | 8.1 | 11.2 |
| Census tract SES index—lowa | 9.6 | 12.7 | 17.3 | 22.8 |
| Census tract SES index—higha | 9.6 | 22.3 | 37.1 | 49.7 |
| Grass/shrub cover (%) | ||||
| Black, non-Hispanic | 8.6 | 11.2 | 14.7 | 19.3 |
| White, non-Hispanic | 2.5 | 7.1 | 13.7 | 21.3 |
| Hispanic | 3.6 | 8.1 | 12.7 | 17.3 |
| Public payment source—no | 8.1 | 11.2 | 15.7 | 20.8 |
| Public payment source—yes | 7.6 | 10.7 | 13.7 | 18.3 |
| Census tract population density—lowa | 9.6 | 13.2 | 18.3 | 24.4 |
| Census tract population density—higha | 3.0 | 4.1 | 6.6 | 8.1 |
| Census tract SES index—lowa | 9.1 | 11.7 | 14.7 | 18.3 |
| Census tract SES index—higha | 6.1 | 9.6 | 14.7 | 20.3 |
| Impervious surface (%) | ||||
| Black, non-Hispanic | 64.5 | 72.5 | 78.6 | 82.8 |
| White, non-Hispanic | 48.3 | 77.7 | 85.5 | 91.1 |
| Hispanic | 70.0 | 78.3 | 84.0 | 89.2 |
| Public payment source—no | 55.5 | 70.0 | 78.3 | 83.8 |
| Public payment source—yes | 66.6 | 73.6 | 79.8 | 84.0 |
| Census tract population density—lowa | 47.8 | 62.6 | 72.7 | 80.6 |
| Census tract population density—higha | 80.0 | 84.2 | 88.2 | 90.9 |
| Census tract SES index—lowa | 68.0 | 72.5 | 77.2 | 82.9 |
| Census tract SES index—higha | 41.8 | 68.9 | 82.0 | 87.2 |
NDVI, normalized difference vegetation index; SES, socioeconomic status
a “low” indicates variable values ≤ 25th percentile; “high” indicates variable values > 90th percentile
Neighborhood vegetation measures were not associated with odds of asthma exacerbation for all cases combined (Table 3 for continuous measure ORs per interquartile range (IQR) increase; results for quartile analyses shown as Supplemental Table 1). In analyses considering each treatment setting case type separately, higher overall greenness was associated with lower odds of ED exacerbation (OR = 0.92, 95% CI: 0.85–0.99), but with higher odds of inpatient exacerbation (OR = 1.08, 95% CI: 0.99–1.17). In analyses of cases classified by patient exacerbation frequency, an inverse association was found between tree canopy cover and frequent exacerbations (> 1/year). For example, 10.2% higher tree canopy coverage was associated with 6% lower odds of frequent exacerbation (OR = 0.94, 95% CI = 0.90–0.99), whereas there was no significant association with infrequent exacerbation (1/year) (OR = 1.03, 95% CI = 0.99–1.06). Likewise, 14.9% higher impervious surface coverage near the home was associated with 5% higher odds of frequent exacerbation, with borderline significance. These associations with frequent exacerbation were consistent across outpatient, ED, and inpatient cases (not shown, tree canopy ORs = 0.94–0.95, impervious surface ORs = 1.03–1.09). There was also a suggestion of lower odds of frequent exacerbation with higher overall greenness, but there was no association with grass/shrub vegetation. These results persisted after adjustment for short-term or seasonal mean temperature, precipitation, or PM2.5 air pollution (Supplemental Table 2).
Table 3.
Associations between greenspace measures and odds of asthma exacerbation, by case type (odds ratios (OR) and 95% confidence intervals (CI) for interquartile-range (IQR) increase)
| N controls | N cases | Overall greenness (NDVI) | Tree canopy cover (%) | Grass/shrub cover (%) | Impervious surface (%) | |
|---|---|---|---|---|---|---|
| IQR = 0.16 | IQR = 10.2% | IQR = 6.1% | IQR = 14.9% | |||
| All cases | 34,681 | 17,639 | 0.98 (0.93–1.03) | 0.98 (0.95–1.02) | 0.99 (0.96–1.02) | 1.02 (0.98–1.06) |
| Outpatient cases | 15,346 | 7853 | 0.98 (0.92–1.04) | 1.00 (0.96–1.04) | 0.98 (0.94–1.02) | 1.00 (0.95–1.04) |
| ED cases | 10,922 | 5522 | 0.92 (0.85–0.99) | 0.97 (0.93–1.02) | 0.97 (0.92–1.01) | 1.05 (0.99–1.12) |
| Inpatient cases | 8413 | 4264 | 1.08 (0.99–1.17) | 0.96 (0.91–1.02) | 1.02 (0.97–1.08) | 1.02 (0.96–1.10) |
| Not frequent (1/year) | 16,327 | 8323 | 1.02 (0.97–1.08) | 1.03 (0.99–1.06) | 0.99 (0.96–1.03) | 0.98 (0.94–1.03) |
| Frequent (> 1/year) | 18,354 | 9316 | 0.94 (0.88–1.01) | 0.94 (0.90–0.99) | 0.98 (0.94–1.02) | 1.05 (1.00–1.12) |
OR, odds ratio; CI, confidence interval; IQR, interquartile range; NDVI, normalized difference vegetation index
All associations adjusted for calendar month, day-of-week, census tract population density, and census tract SES index
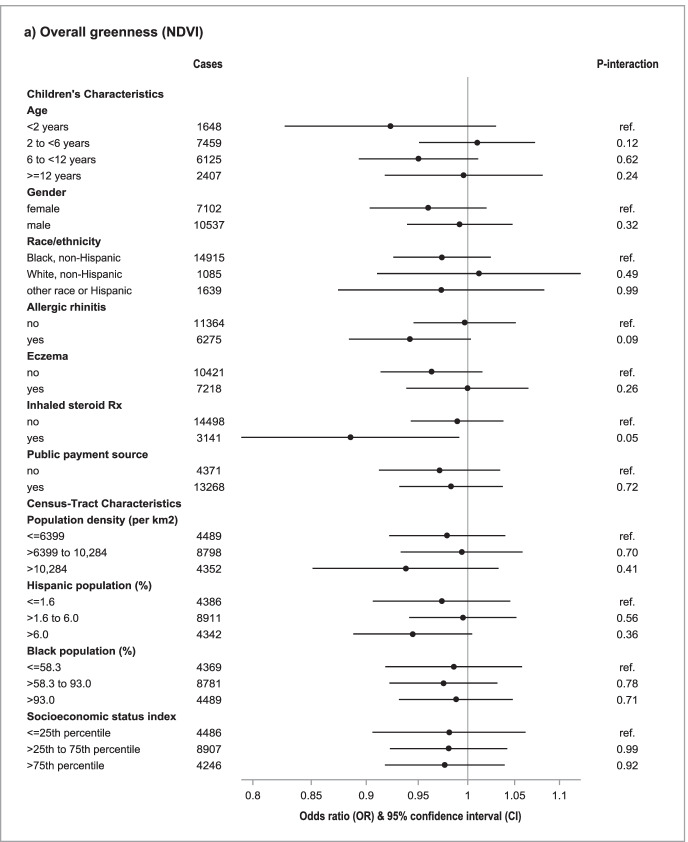
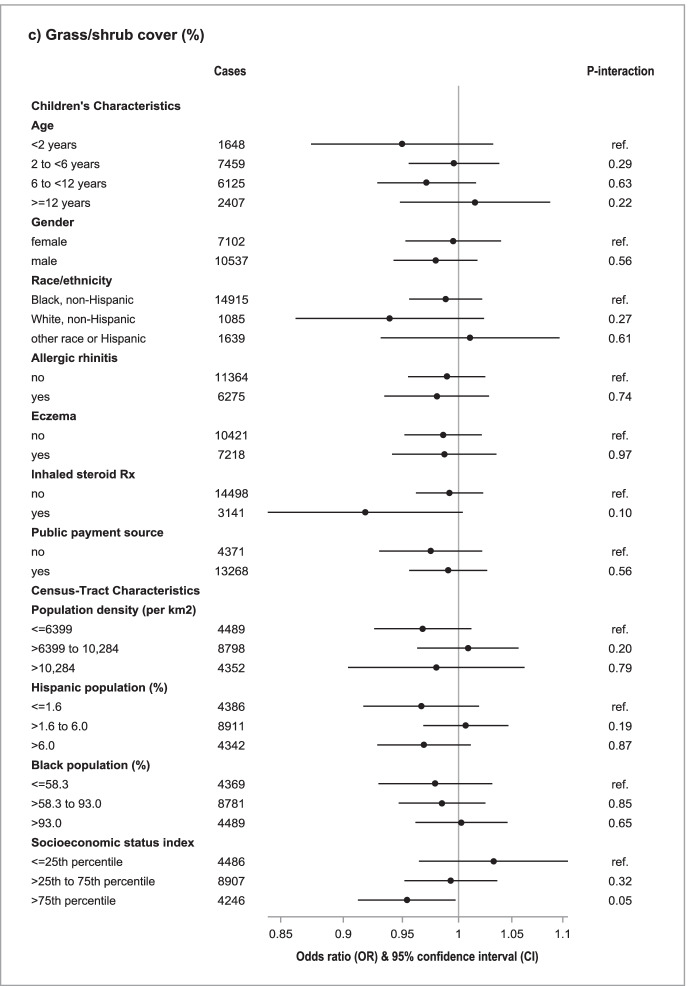
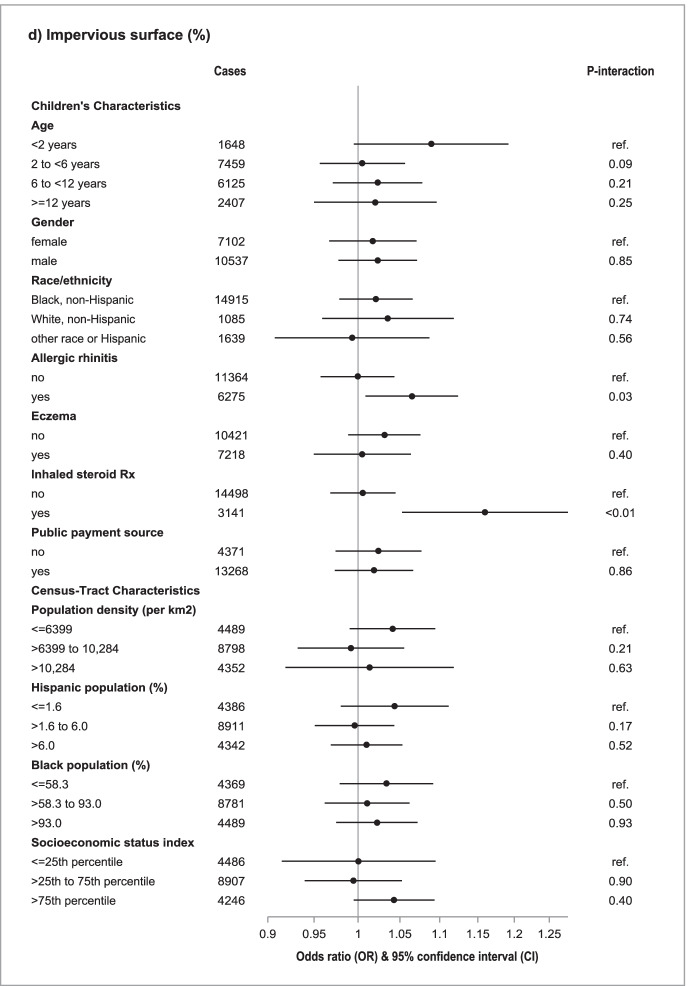
Figure 2 shows associations between vegetation measures (per IQR increase) and odds of asthma exacerbation, within strata of potential effect modifier variables (ORs and CIs are provided as Supplemental Table 3). The strongest associations (albeit imprecise) were found in children with a prescription for inhaled steroids, and there was evidence that these estimates differed from the associations in children without a prescription, for overall greenness (Rx: OR = 0.89, 95% CI: 0.79–0.99; no Rx: OR = 0.99, 95% CI = 0.94–1.04; p-value for interaction (P-int) = 0.05), tree cover (Rx: OR = 0.91, 95% CI = 0.84–0.99; no Rx: OR = 0.99, 95% CI = 0.96–1.02; P-int = 0.04), and impervious surface (Rx: OR = 1.16, 95% CI = 1.05–1.28; no Rx: OR = 1.01, 95% CI = 0.97–1.04; P-int < 0.01). Associations between vegetation measures and odds of asthma exacerbation were stronger in children with an allergic rhinitis diagnosis than in those without, notably for impervious surface (allergic rhinitis: OR = 1.06, 95% CI = 1.01–1.12; no allergic rhinitis: OR = 1.00, 95% CI = 0.96–1.04; P-int = 0.03). No similar modification was seen by eczema diagnosis. There was no significant modification by categories of children’s age, sex, race/ethnicity, or payment source, nor by census tract-level population density or race/ethnic composition variables. Although we found no association with grass/shrub cover in our main analysis, lower odds of exacerbation in association with grass/shrub cover were differentially seen among children living in census tracts with high SES index levels (> 75p SES index: OR = 0.95, 95% CI = 0.91–1.00; ≤ 25p SES index: OR = 1.03, 95% CI = 0.96–1.11; P-int = 0.05).
Fig. 2.
Associations of vegetation measures with odds of asthma exacerbation, by potential effect modifiers. Odds ratio (OR) and 95% confidence interval (CI). a Overall greenness (NDVI). b Tree canopy cover (%). c Grass/shrub cover (%). d Impervious surface (%)
Discussion
In our study of pediatric asthma patients in Philadelphia, we observed lower odds of asthma exacerbation for children living near greater amounts of vegetation, but these associations were only found with frequent exacerbations (case events that were one of multiple exacerbations that a child experienced during the year). Odds of frequent exacerbation were lower in association with greater tree canopy cover and higher with greater impervious surface, but we found no consistent associations with overall greenness or grass/shrub vegetation.
Proposed pathways by which living near vegetation may protect against asthma exacerbation center largely on the influence of trees on the local physical environment (such as through effects on temperature, air pollution, and stormwater control) and on psychosocial health (such as by stress reduction due to neighborhood beautification and/or increased outdoor activity). It is likely that the physical and psychosocial impacts differ between tree canopy and grass/shrub vegetation, thus leading to different magnitudes of effect. Furthermore, the grass/shrub landcover data we used was assessed with exclusion of tree canopy—thus indicating vegetation with lack of tree canopy and its related benefits. As overall greenness (NDVI) is not specific to the type of vegetation, it makes sense that these results reflect a mix of the results for tree canopy and grass/shrub vegetation, without a clear picture of the direction of association. Our results suggest the importance of assessing the potential benefits of the tree canopy separately from other types of vegetation.
We investigated person-level relationships between vegetation near children’s homes in relation to asthma exacerbation. Several ecologic studies with area-level measures of both vegetation and exacerbation rates have reported mixed results. A small-area study conducted in England [12] found lower asthma hospitalization rates (all ages) in postal codes with greater tree canopy coverage, public green spaces, and gardens. Tree canopy was similarly associated with lower asthma-related ED visits in a census tract-level analysis in Los Angeles County [16]. An earlier study of health service catchment areas in New York City [9] found no association between street tree density and asthma hospitalization rates; however, street trees represent only a fraction of the total tree canopy and this metric is not comparable to the tree measure used in our study. Several additional studies of exacerbation-related measures such as wheeze and “asthma control” have also reported mixed results, such as no association with residential greenness measured as the NDVI [10–12], and imprecise decreases of asthma-related symptoms with greater NDVI (OR = 0.80, 95% CI: 0.63, 1.02) and tree canopy (OR = 0.86, 95% CI = 0.66, 1.12) within 500 m of children’s homes [14]. A pooled cohort study found significant increases in “current” wheeze and asthma in association with vegetated landcover within 500 m; these associations were particularly prominent with residential proximity to coniferous (but not deciduous or mixed) forests [15]. This study was strong based on its large sample size of children with individual survey data and detailed landcover measures, but the vague definition of “current” asthma (current medication use and/or asthma attack in last 12 months) limits comparability to our study of clinically identified and temporally resolved asthma exacerbation events.
There was little evidence from our study that the main hypothesized effect of residential vegetation on asthma exacerbation differed systematically by the clinical treatment setting. The lower odds of ED exacerbation and higher odds of inpatient exacerbation that we observed in relation to overall greenness may reflect residual confounding by factors related to the treatment setting. It has been documented that Black children who are insured by Medicaid are more likely to have ED visits and less likely to make routine primary care visits [1], and such preference/access may partially account for the strength of the associations seen for ED exacerbations. We restricted our study to children who utilized the CHOP system for regular asthma care, and we matched cases to controls on Medicaid/sCHIP payment and residential proximity to the CHOP main campus, as well as race/ethnicity and other demographic variables possibly related to clinical care utilization. These design features likely diminished confounding, but residual confounding remains a possibility. We have the most confidence in findings that were consistent across all three case types—such as an inverse association between tree canopy and frequent exacerbation—particularly because we would expect little selection difference between cases and controls in the outpatient clinic setting.
Several of our results suggest specificity in the types of asthma patients who may benefit from neighborhood greening. Findings of potentially protective effects of residential vegetation were found for frequent exacerbations and among children with a prescription for inhaled steroid—both indicators of more severe asthma. These consistent findings are novel and potentially important, as such categorizations represent clinically distinct subgroups of children based on risk of future exacerbation and persistent (versus intermittent) disease [33]. We utilized allergic rhinitis diagnosis as a crude indicator of sensitization to allergens (including but not limited to those from vegetation, like pollen) and counter to our hypothesis, found a positive association between impervious surface (less vegetation) and odds of asthma exacerbation, only among asthma patients with allergic rhinitis. We hesitate to interpret this finding without further information on sensitization, because in the context of our other findings, this association might simply result from more severe asthma in this subgroup (including more frequent exacerbations). Regardless, if potential benefits of neighborhood vegetation are specific to certain case groups, then differing definitions of asthma exacerbation and related symptoms in previous research may have contributed to the mixed evidence to date.
An inverse association (a possible “protective effect”) of grass/shrub vegetation was found only among children living in areas with relatively high SES. If causal, this might reflect greater benefits from vegetation for populations with fewer socioeconomic stressors that cause vulnerability. Another possibility is that the quality of green spaces across Philadelphia may differ by neighborhood SES [20, 34], and potential benefits of residential vegetation may be related to its qualities—such as the attractiveness of the greenspace (e.g., due to design, maintenance) and species composition (which encompasses allergenicity of the vegetation). We did not have information on quality-related characteristics of green spaces in our study. However, the fact that the interaction with SES was found primarily for grass/shrub vegetation may suggest that quality is a contributor to potential benefits from these types of green spaces that lack tree canopy.
Our study had considerable strengths, including a large database of pediatric asthma patients’ clinical encounters that enabled direct comparison of exacerbation events to non-exacerbation care visits, allowing investigation of risk factors for asthma exacerbation that avoided conflation of estimates by correlates of prevalent asthma. We investigated several different high-resolution vegetation-related measures, enabling interpretation of potential benefits from different types and characteristics of vegetation near children’s homes. Given the size of our database and the rich array of measures, we were able to adjust for critical individual-level and spatiotemporal confounders and assess modification of vegetation effects by children’s and neighborhood characteristics. Nevertheless, there are important limitations of our study. We lacked information from children’s home environments, such as indoor smoking and mold, which are known triggers of asthma exacerbation [35] that likely vary by neighborhood. We were also unable to account for time spent in green spaces outside the immediate home environment, such as in parks and forests; thus, inference from our study is limited to possible benefits of living near vegetation.
In conclusion, we found lower odds of asthma exacerbation among children living near greater amounts of vegetation, and in particular, tree canopy. These associations were only found for frequent exacerbations. Further investigation of mechanisms underlying modification of effects by asthma case characteristics and neighborhood SES may inform about the potential benefits of greening efforts across patient subgroups and neighborhoods in Philadelphia.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This study is part of the Pediatric Big Health Data initiative funded by the State of Pennsylvania and led by the Children’s Hospital of Philadelphia, University of Pennsylvania, and the Urban Health Collaborative at Drexel University. We would like to thank the investigators of the Pediatric Big Health Data initiative for their contributions. These individuals include the following: Christopher B. Forrest, MD, PhD; L. Charles Bailey, MD, PhD; Shweta P. Chavan, MSEE; Rahul A. Darwar, MPH; Jillian Benedetti, MPH; Daniel Forsyth; Chén C. Kenyon, MD, MSHP; Ritu Khare, PhD; Mitchell G. Maltenfort, PhD; Aaron J. Masino, PhD, ME; Xueqin Pang, PhD; Ting Qian, PhD; Hanieh Razzaghi, MPH; Justine Shults, PhD; Levon H. Utidjian, MD, MBI from the Children’s Hospital of Philadelphia; Ana V. Diez Roux, MD, PhD, MPH; Amy H. Auchincloss, PhD, MPH; Elizabeth A. Campbell, MSPH; Kimberly Daniels, MS; Anneclaire J. De Roos, PhD, MPH; J. Felipe Garcia-Espana, MS, PhD; Irene Headen, PhD, MS; Félice Lê-Scherban, PhD, MPH; Steven Melly, MS, MA; Yvonne L. Michael, ScD, SM; Jeffrey Moore, MS; Kari Moore, MS; Abigail E. Mudd, MPH; Leah Schinasi, PhD, MSPH; and Yuzhe Zhao, MS from Drexel University and, Yong Chen, PhD; John H. Holmes, PhD; Rebecca A. Hubbard, PhD; A. Russell Localio, JD, MPH, PhD from the University of Pennsylvania.
This work was supported by a grant from the Commonwealth Universal Research Enhancement (C.U.R.E) program funded by the Pennsylvania Department of Health—2015 Formula award—SAP #4100072543.
Anneclaire J. De Roos would like to acknowledge the Whiteley Center at the University of Washington Friday Harbor Laboratories for providing a peaceful and inspirational setting in which to complete the bulk of this research.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bryant-Stephens T. Asthma disparities in urban environments. J Allergy Clinical Immunol. 2009;123(6):1199–1206. doi: 10.1016/j.jaci.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 2.Ferrante G, La Grutta S. The burden of pediatric asthma (editorial) Front Pediatr. 2018;6:186. doi: 10.3389/fped.2018.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nunes C, Pereira AM, Morais-Almeida M. Asthma costs and social impact. Asthma Res Pract. 2017;3:1. doi: 10.1186/s40733-016-0029-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perry R, Braileanu G, Palmer T, Stevens P. The economic burden of pediatric asthma in the United States: literature review of current evidence. Pharmacoeconom. 2019;37(2):155–167. doi: 10.1007/s40273-018-0726-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keet CA, Matsui EC, McCormack MC, Peng RD. Urban residence, neighborhood poverty, race/ethnicity, and asthma morbidity among children on Medicaid. J Allergy Clin Immunol. 2017;140(3):822–827. doi: 10.1016/j.jaci.2017.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng XY, Ding H, Jiang LN, et al. 2015 Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. PLoS One;10(9):e0138146. [DOI] [PMC free article] [PubMed]
- 7.Markevych I, Schoierer J, Hartig T, et al. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ Res. 2017;158:301–317. doi: 10.1016/j.envres.2017.06.028. [DOI] [PubMed] [Google Scholar]
- 8.De Roos AJ, Kenyon CC, Zhao Y, et al. 2020 Ambient daily pollen levels in association with asthma exacerbation among children in Philadelphia, Pennsylvania. Environ Int.;145:106138. [DOI] [PubMed]
- 9.Lovasi GS, Quinn JW, Neckerman KM, Perzanowski MS, Rundle A. Children living in areas with more street trees have lower prevalence of asthma. J Epidemiol Community Health. 2008;62(7):647–649. doi: 10.1136/jech.2007.071894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen E, Miller GE, Shalowitz MU, et al. 2017 Difficult family relationships, residential greenspace, and childhood asthma. Pediatrics.;139(4):e20163056. [DOI] [PMC free article] [PubMed]
- 11.Tischer C, Gascon M, Fernández-Somoano A, et al. Urban green and grey space in relation to respiratory health in children. Eur Respir J. 2017;49(6):1502112. doi: 10.1183/13993003.02112-2015. [DOI] [PubMed] [Google Scholar]
- 12.Alcock I, White M, Cherrie M, et al. Land cover and air pollution are associated with asthma hospitalisations: a cross-sectional study. Environ Int. 2017;109:29–41. doi: 10.1016/j.envint.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 13.DePriest K, Butz A, Curriero FC, Perrin N, Gross D. Associations among neighborhood greenspace, neighborhood violence, and children’s asthma control in an urban city. Ann Allergy Asthma Immunol. 2019;123(6):608–610. doi: 10.1016/j.anai.2019.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dzhambov AM, Lercher P, Rüdisser J, Browning MHEM, Markevych I. 2021 Allergic symptoms in association with naturalness, greenness, and greyness: a cross-sectional study in schoolchildren in the Alps. Environ Res.;198:110456. [DOI] [PubMed]
- 15.Parmes E, Pesce G, Sabel CE, et al. 2020 Influence of residential land cover on childhood allergic and respiratory symptoms and diseases: evidence from 9 European cohorts. Environ Res.;183:108953. [DOI] [PubMed]
- 16.Kim D, Ahn Y. The contribution of neighborhood tree and greenspace to asthma emergency room visits: an application of advanced spatial data in Los Angeles County. Int J Environ Res Public Health. 2021;18(7):3487. doi: 10.3390/ijerph18073487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pennsylvania Department of Health. Pennsylvania Asthma Burden Report (2012). http://www.paasthma.org/images/docs/2012_asthma_burden_report.pdf. Accessed March 14, 2021.
- 18.Asthma and Allergy Foundation of America (AAFA). Asthma Capitals 2019: the most challenging places to live with asthma. https://www.aafa.org/asthma-capitals/. Accessed March 14, 2021.
- 19.Delaware Valley Regional Planning Commission (DVRPC). Health Data Snapshot. https://www.dvrpc.org/health/PASnapshot/. Accessed March 14, 2021.
- 20.Nowak DJ, Bodine AR, Hoehn R, et al. The urban forests of Philadelphia. Resource Bulletin NRS-106. Newtown Square, PA: US Department of Agriculture, Forest Service, Northern Research Station. 2016;106:1–80.
- 21.Fuhlbrigge A, Peden D, Apter AJ, et al. Asthma outcomes: exacerbations. J Allergy Clin Immunol. 2012;129(3 Suppl):S34–48. doi: 10.1016/j.jaci.2011.12.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kenyon CC, Maltenfort MG, Hubbard RA, et al. Variability in diagnosed asthma in young children in a large pediatric primary care network. Acad Pediatr. 2020;20(7):958–966. doi: 10.1016/j.acap.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mudd AE, Michael YL, Diez-Roux AV, et al. Primary care accessibility effects on health care utilization among urban children. Acad Pediatr. 2020;20(6):871–878. doi: 10.1016/j.acap.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carroll ML, DiMiceli CM, Sohlberg RA, Townshend JR. 250m MODIS normalized difference vegetation index. College Park, MD: University of Maryland; 2004. [Google Scholar]
- 25.O’Neil-Dunne JP, Grove JM. A report on the City of Philadelphia’s existing and possible tree canopy. Washington, DC: USDA Forest Service; 2011. [Google Scholar]
- 26.Philadelphia Land Cover Raster 2018. University of Vermont Spatial Analysis Laboratory. http://www.pasda.psu.edu/uci/DataSummary.aspx?dataset=3193. Accessed November 7, 2016.
- 27.National Land Cover Database. www.mrlc.gov. Accessed April 19, 2016.
- 28.American Community Survey (ACS0509 & ACS1216). U.S. Census. https://www.census.gov/programs-surveys/acs. Accessed 2018
- 29.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. New Engl Journal Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 30.Berrocal VJ, Gelfand AE, Holland DM. A spatio-temporal downscaler for output from numerical models. J Agric Biol Environ Stat. 2010;15(2):176–197. doi: 10.1007/s13253-009-0004-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berrocal VJ, Gelfand AE, Holland DM. Space-time data fusion under error in computer model output: an application to modeling air quality. Biometrics. 2012;68(3):837–848. doi: 10.1111/j.1541-0420.2011.01725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.NOAA, National Centers for Environmental Information. https://www.ncdc.noaa.gov/cdo-web/datatools/lcd. Accessed 2017–2018.
- 33.National Asthma Education and Prevention Program. Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel Report 3: guidelines for the diagnosis and management of asthma. Bethesda, MD: National Heart Lung and Blood Institute. 2007. Available from https://www.ncbi.nml.gov/books/NBK7232/. Accessed October 2021
- 34.Pearsall H, De Roos AJ, Dickinson S, et al. The benefits and costs of urban public spaces. Philadelphia, PA: William Penn Foundation, 2020. https://williampennfoundation.org/what-we-are-learning/benefits-and-costs-urban-public-spaces. Accessed November 3, 2021.
- 35.Kanchongkittiphon W, Mendell MJ, Gaffin JM, Wang G, Phipatanakul W. Indoor environmental exposures and exacerbation of asthma: an update to the 2000 review by the Institute of Medicine. Environ Health Perspect. 2015;123(1):6–20. doi: 10.1289/ehp.1307922. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.