Abstract
Background
A prospective randomised trial was conducted to compare the results of conservative management of middle-third clavicular fracture using the figure of 8 bandage and broad-arm sling.
Methods
296 patients with middle-third clavicle fracture were included in the study conducted between March 2017 and January 2020. 152 patients were managed with figure of 8 bandage and 144 patients were managed with a broad arm sling. Results were evaluated based on clinical, radiological and functional outcomes. Visual analogue scale (VAS) for pain was used to evaluate the clinical outcomes, whereas radiological outcomes were assessed with non-union, malunion, clavicle shortening and time to union. Disability of Arm, Shoulder and Hand score (DASH), Constant score and Nottingham Clavicle Score were used to assess functional outcomes.
Results
The broad arm sling group showed a significantly better VAS score in the first 4 weeks. DASH score was significantly superior in the broad arm sling group in the initial 4 weeks, but with similar outcome thereafter. Constant scores showed a good outcome for both groups at the final follow-up, whereas the Nottingham Clavicle Score was significantly superior in the broad arm sling group at the 2 year follow-up. A satisfactory outcome was achieved with respect to the radiological parameters, without any significant difference between the 2 groups. Incidence of malunion was significantly higher in figure of 8 bandage group.
Conclusions
Broad-arm sling proves to be a better modality of management for middle-third clavicular fractures in terms of ease of application, pain relief, incidence of malunion, and functional outcomes.
Keywords: Clavicle, Figure of 8 bandage, Broad arm sling, Conservative management, Fracture, DASH score, Nottingham Clavicle Score, Constant score, Middle-third, VAS score
Introduction
Traumatic clavicle injuries account for 2.6–4% of all fractures, 44% of injuries to the shoulder girdle and are one of the most common fractures [1]. Overall incidence is 36.5–64 per 100,000 per year [2]. Epidemiology data indicates a bimodal distribution with a male predominance in the young and female predominance (7:1) in later life [3].
Clavicle fractures are most commonly seen in the midshaft, also known as middle third fractures comprising 82% of cases, whereas 12% occur in the lateral third of the clavicle and least commonly in medial third comprising 6% of the cases [3].
Non-displaced clavicle fractures, irrespective of their location are usually managed non-operatively, whereas rare open fractures, fractures associated with neurovascular complications and suspicion of imminent skin lesion produced by sharp clavicle fracture edges, are usually managed surgically [2].
Non-operative management ranges from spica casting, figure of 8 bandaging, broad arm sling to benign neglect, and principally involves immobilisation of the clavicle [4]. Operative management is principally done with open reduction and internal fixation with plates or nail, with or without bone grafting [2].
The available evidence from current literature is limited regarding the effectiveness of the different methods of conservative interventions and the best conservative treatment for middle-third clavicle fractures in adults is controversial [2]. In addition, to the best of our knowledge, we haven’t come across any Indian study comparing these two conservative treatment options.
Hence, we decided to conduct a study and evaluate the effects of the two commonly used conservative interventions (figure of 8 bandage and broad arm sling) and investigate which of these two methodologies would be better to manage the middle-third clavicle fracture based on functional, radiological and clinical outcomes.
Materials and Methods
A prospective study was conducted at a tertiary care hospital in Mumbai from March 2017 to January 2020. All patients with middle third clavicular fracture who met with the inclusion criteria and gave a written informed consent were included in the study.
Inclusion criteria
Patients between the age of 18 and 60.
Acute middle third clavicular fracture of less than 10 days
No medical contraindication to the above-mentioned conservative management method.
Patients who gave a written informed consent.
Patients who followed-up for 2 years at least
Exclusion criteria
Open fracture
Fracture involving neurovascular complications or skin tenting.
Pathological fracture.
History of frozen shoulder or any pre-existing limb disease which could influence the result.
Ipsilateral upper limb fractures and/or dislocation
Randomisation was done in a non-stratified manner in blocks of two, using sealed envelope method, in which one person chooses one sealed envelope and the next patient is allocated to the other group according to the remaining envelope of the pair.
Group 1—Figure of 8 bandage was to be used for 4 weeks and was applied with proper tightening. Patients and relatives were educated regarding regular tightening of the brace. The figure of 8 bandage needs to be adjusted, so that the shoulder is pressed back in an arched position, such as a back-stretch. Figure of 8 bandage allowed the dominant hand to remain free and simple activities were allowed (Fig. 1).
Fig. 1.
Clinical picture showing a figure of 8 bandage (left) and broad arm sling (right)
Group 2—A standard broad arm sling was given for 4 weeks. Upper limb was immobilised with a sling in internal rotation and patients were advised to flex and extend the elbows four times a day for 10 min to prevent elbow stiffness (Fig. 1).
The only analgesia permitted in both groups was paracetamol and those who could not comply and required further analgesia were excluded.
Follow-up of patients was done at 1 week and thereafter every 4 weeks for 6 months, and then at 6 monthly intervals. Outcomes measured at each of the follow-up visits are mentioned below:
Pain was assessed using Visual Analogue Scale from 1 to 10 (best to worst) [5]. This outcome was measured at 1, 4, 8, 24 weeks, 1 year and 2 years.
Radiological outcome—Radiographs were obtained for patients in both groups at 4, 8, 24 weeks, 1 year and 2 years. Time to union, incidence of malunion, nonunion and shortening were recorded. Measurement was done using AP radiographs with 20 degree cephalic tilt. Malunion, nonunion and shortening comparison was done at the final 2 year follow-up and the worst measurement was recorded.
Malunion was defined if one of the following criteria were met [6]:
Angulation > 15 degrees
Shortening more than 1.5 cm
Displacement more than 1.5 cm
Nonunion definition
We defined fracture union as the absence of pain or mobility on stressing the site of the fracture and presence of bridging callus on radiographs. For the purposes of this study, we defined nonunion as a fracture that remained unhealed according to these criteria at the 24 week follow-up [7].
Shortening of the clavicle was measured using antero-posterior radiographs of both clavicles. The length of both clavicles was measured from centre of sternoclavicular joint to centre of acromioclavicular joint [8]. Literature has shown that a shortening of more than 1.5–2 cm is associated with worse functional outcomes and non-union [1, 9].
Functional outcomes were measured with the Disability of Arm, Shoulder and Hand questionnaire (DASH), Constant score and Nottingham Clavicle Score [10–12].
-
The DASH consists of a 30-item disability/symptom scale, scored 0 (no disability) to 100 [13]. The final score of the DASH questionnaire was converted to a percentage via the following formula:
where n is the number of complete answers. At least 27 of the 30 items needed to be completed for a score to be calculated. The value was then transformed to a score out of 100. DASH score was assessed at weeks 1, 4, 8, 24, 1 year and 2 years.
Constant scores were used for assessment at the last follow-up (2 years). The method recorded individual parameters and provided an overall clinical functional assessment [11].
Nottingham Clavicle score is a 10-item patient reported outcome measure (PROM) with a maximum score of 100 (least difficulties) and a minimum score of 20 (most difficulties). 1 to 4 items measures pain, 5 and 6 measure strength, item 7 measures cosmetic satisfaction with the shoulder, item 8 asses clicking sounds within the shoulder and item 9 and item 10 have a component measuring sensations, such as tingling and dragging sensations, respectively. The unique feature of this scoring system is that it is a valid and reliable score with an extra component of cosmesis which is not seen in the other scoring systems [12].
Paired t test was used for statistical analysis with significance set a p value < 0.05. Statistical analyses were performed using MedCalc for Windows, version 19.1.7 (MedCalc Software, Ostend, Belgium).
Results
308 patients with middle third clavicular fractures initially enrolled in the study.
5 patients declined to continue participation, 3 patients were lost to follow up after the second follow-up because of death due to Covid-19 virus and 4 patients took painkillers apart from paracetamol.
296 patients were finally included in the analysis, of which 152 were managed with figure of 8 bandage (Group 1) and 144 patients were managed with broad arm sling (Group 2).
In Group 1 mean age was 26.2 (SD 2.5) years, 53% of patients were males and 58% had a displaced fracture. In Group 2, the mean age was 29.6 (SD 1.8) years, 49% were males and 67% had a displaced fracture.
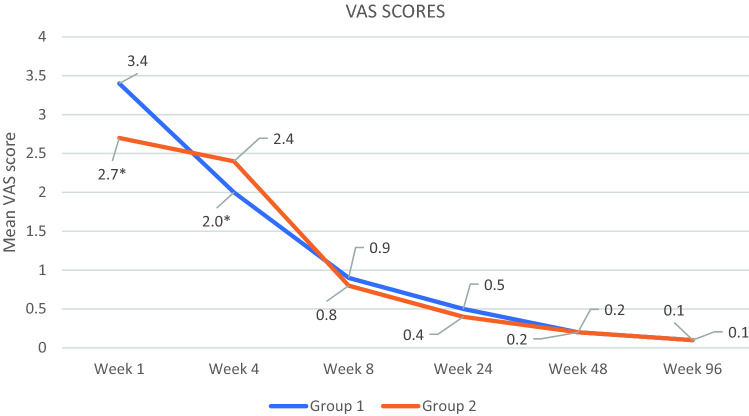
The mean VAS at week 1 and week 4 was significantly lower in Group 2 as compared to Group 1. From weeks 8 to 2 years, there was no significant difference in the pain scores between the two groups (Fig. 2).
Fig. 2.
VAS (Visual Analogue Scale) scores. *p < 0.05 between group 1 and 2 at week 1 and week 4
Mean time to union in Group 1 was 7.4 (SD 1.3) weeks and in Group 2 was 7.0 (SD 1.5) weeks which turned out to be statistically insignificant (p = 0.0665).
Malunion was compared at the final visit (2 years) and the results are shown in Table 1.
Table 1.
Radiologic assessment for malunion, nonunion and shortening
| Values at week 96(2 years) | Group 1 (n = 152) | Group 2 (n = 144) |
|---|---|---|
| Number of patients who developed malunion | 18 | 4 |
| Total number of patients | 152 | 144 |
| Proportion of patients who developed malunion (%) | 11.84 | 2.77 |
| p value for malunion | 0.0030 | |
| Number of patients who developed nonunion | 27 | 20 |
| Total number of patients | 152 | 144 |
| Proportion of patients who developed nonunion (%) | 17.76 | 13.88 |
| p value for nonunion | 0.3620 | |
| Mean shortening(in mm) | 8.5 (SD 3.2) | 7.8 (SD 3.4) |
| Total number of patients | 152 | 144 |
| p value for shortening | 0.0691 |
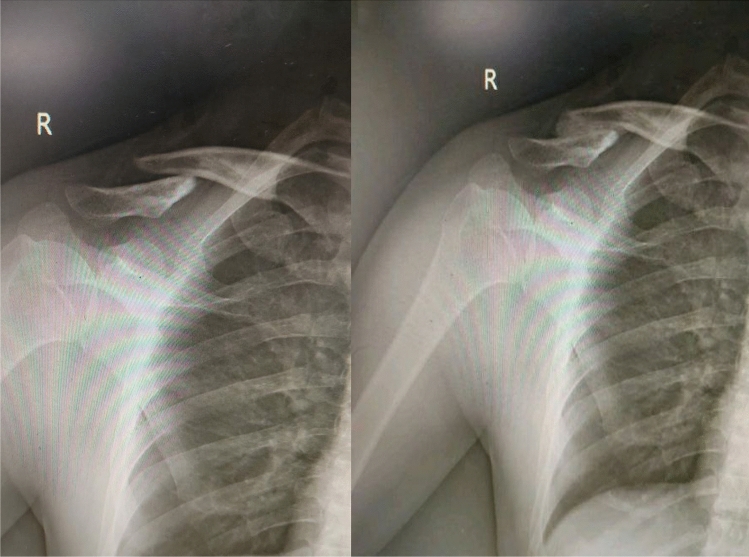
Figure 3 shows radiographs of a patient with middle third clavicular fracture treated with figure of 8 bandage which resulted in malunion.
Fig. 3.
Radiograph of a patient showing a middle third clavicular fracture before treatment (left) and a middle third clavicular fracture managed with figure of 8 brace resulting in malunion (right)
Nonunion and shortening of the clavicle was compared at the last follow-up (2 years) and the results are shown in Table 1. Out of 27 patients in group 1 who developed non-union, 6 patients were smoker, 3 were diabetic, and out of 20 patients of non-union in group 2, 3 patients were diabetic and 5 were smokers.
Patients who developed malunion and nonunion were offered operative management. 4 out of 22 malunion patients and 22 out of 47 non-union patients were subsequently operated upon. Rest of the patients refused operative intervention as they were either satisfied with the outcome or were not willing to get operated.
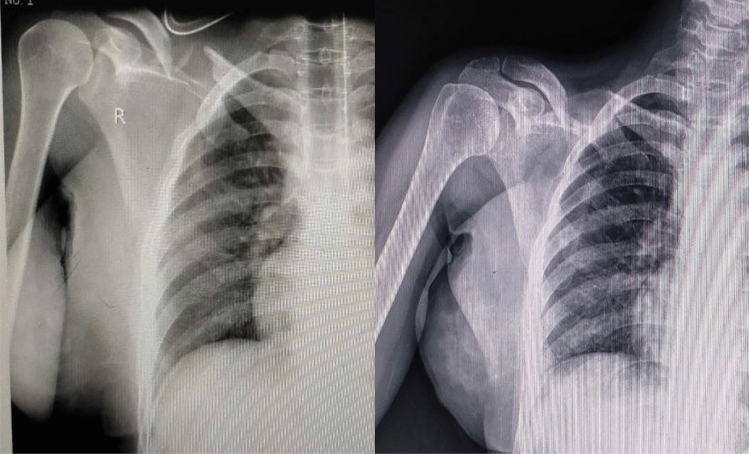
Figure 4 shows radiographs of a patient with middle third clavicular fracture treated with figure of 8 bandage which resulted in nonunion.
Fig. 4.
Radiograph of a patient showing a middle third clavicular fracture before treatment (left) and a middle third clavicular fracture managed with figure of 8 brace resulting in nonunion (right)
The DASH score at week 1 and week 4 was significantly lower in Group 2 as compared to Group 1. From week 8 to week 48 (1 year) there was no significant difference in the DASH scores. The DASH scores were less than 5 at the final follow-up of 96 weeks (2 years).
High Constant scores in both the treatment groups denoted good functional recovery. The mean Constant scores were 95 (SD 6.7) in group 1 and 97 (SD 6.8) in group 2 (p = 0.0736) at the end of 2 year follow-up.
Nottingham score questionnaire was given to patients in both groups. Group 1 showed an average score of 88.6 (SD 3.2) and group 2 showed an average score of 89.8(SD 3.4) with statistical significance (p = 0.0019). Highest Nottingham score of 96 was found in one of the patients in the broad arm sling group.
Discussion
The main aim of treatment of clavicular fractures is to restore the function of shoulder joint and allow the clavicle to heal with minimum pain, deformity and good range of motion for daily range of activities [14].
The various options for non-operative management include spica casting, figure of 8 bandaging, broad arm sling and neglect [15]. The figure of 8 brace is reported to be associated with more discomfort and pain and nerve compression with temporary brachial plexus palsies and restriction of venous blood return. The broad arm sling is associated with elbow stiffness [16].
The figure of 8 bandage and the broad arm sling are most commonly used and, despite their wide use, very few randomised studies have compared the two. The midshaft part of the clavicle is the thinnest and least medullous area of the clavicle, and lacks muscular and ligamentous attachments. These factors make the midshaft of the clavicle, most vulnerable to fractures [17]. The medial segment gets pulled superiorly due to the pull of sternocleidomastoid, with a counterforce from the trapezius. The lateral segment gets displaced inferomedially due to the pull of pectoralis major and latissimus dorsi which at times, results in consequent shortening [17]. The figure of 8 brace presses the medial fragment downwards to enable reduction and aligns the fragments. The broad arm sling gives support at the elbow, which counteracts the gravity forces. This counterbalances the inferior pull of the lateral fragment due to gravity, and achieves alignment of the two fragments.
Our study compares the two conservative methods of non-operative management in terms of clinical, radiological and functional outcomes.
Ersen et al. in their study, reported that pain measured by visual analogue scale on the first day after treatment in broad arm sling group was 5.5 (SD 1.8) and in the figure of 8 group it was 6.8 (SD 1.7) with statistical significance (p = 0.034). After day 1, the mean VAS score was statistically insignificant (p > 0.05) with complete resolution of pain on day 14 [4]. Faldini et al. reported good pain relief with figure of 8 bandage in 72 out of 100 patients [18]. A study by Hoofwijk and van der Werken reported a statistically significant difference in favour of the broad arm sling in terms of pain after 15 days (mean difference 0.80, 95% CI 0.34–1.26) [19].
Our findings echoed the above mentioned study with statistical significance in pain seen in favour of broad arm sling till 4 weeks. At week 8 and thereafter, mean VAS score was < 1 and was statistically insignificant.
We found that despite a shorter time to union in the broad arm sling group as compared to figure of 8 bandage, (7.0 weeks vs 7.4 weeks, respectively) it was statistically not significant (p = 0.0665). On reviewing the study done by Ersen et al., a similar finding of insignificance with respect to time to union was observed [6]. Kelly et al.` in their study on operative vs non-operative treatment of midshaft clavicle fracture showed that mean time to union was 7.4 weeks and 8.7 weeks, respectively (p = 0.02) [20].
An important clinical outcome in our study was the significant difference in incidence of malunion between the two groups, in favour of broad arm sling group. On comparison of proportions of malunion amongst the two groups, we found a significant statistical difference (p = 0.0030) showing less incidence of malunion in patients managed with broad arm sling as compared to figure of 8 bandage. After a thorough review of literature, to the best of our knowledge, we found no literature to support the comparison of malunion between the two conservative management groups.
On comparison of nonunion and shortening of the clavicle amongst the two groups, we found no statistical significance (p = 0.3620 and 0.0691). The mean shortening in the figure of 8 brace group was 8.5 mm, whereas it was 7.8 mm in the broad arm sling group compared to the contralateral normal clavicle (p = 0.0691). Ersen et al. found a mean shortening of 9 mm and 7.7 mm in the figure of 8 bandage and broad arm sling group, respectively, with no statistical significance between the two (p = 0.30) [4]. Faldini et al., evaluated 100 patients of midshaft clavicle fractures managed with figure of 8 bandage and found 3 patients to have a nonunion [18]. Gustavo et al., studied the outcome of clavicle midshaft fractures treated with figure of 8 bandage and found a mean shortening of 92 mm [8]. Bharadwaj et al. compared plate fixation vs broad arm sling for midshaft clavicle fractures and found 6 percent of patients in the broad arm sling group to have a nonunion at the last follow-up, whereas patients treated operatively did not show nonunion [21].
Ersen et al. evaluated functional outcomes on the basis of Constant and ASES (American Shoulder and Elbow Surgeons) scores. The mean Constant score was better in the broad arm sling group (96.75 with the range being 80–100) as compared to the figure of 8 bandage group (96 with range being 80–100) but showed no statistical significance (p = 0.676). The mean ASES scores were 94.5 (82–100) in the figure of 8 group and 96.15 (73.3–100) in the broad arm sling group but did not show any significance in the functional outcome, either (p = 0.873) [4].
Comparison of the mean DASH scores of the two groups at week 1 and week 4 showed statistical significance in favour of the broad arm sling group with p ≤ 0.0001 (week 1) and p = 0.013 (week 4). Mean DASH scores measured thereafter were statistically insignificant and were less than 5 by week 96 (2 years). Gustavo et al., in his study on management of midshaft clavicle fractures with figure of 8 bandage found DASH scores to be 28.84 and 8.18 at the 6 weeks and 1 year follow-up, respectively [8]. Faldini et al., found majority of the patients treated by figure of 8 bandage to have an excellent outcome with respect to DASH scores [18].
The Constant score comparison was done at the end of 2 years and did not reveal any statistical significance with score being 96 in the figure of 8 bandage group and 97 in the broad arm sling group (p = 0.0736). In a study by Bhardwaj et al., which compared broad arm sling management vs plate fixation, there was a statistical significance of difference in favour of the plate fixation method [21].
Nottingham scores showed a good outcome at the final follow-up. Group 1 showed an average score of 88.6(SD 3.2) and Group 2 showed an average score of 89.8 (SD 3.4) with statistical significance on comparison of the two means (p = 0.0019). Kamaci et al., in their study on midshaft clavicle fractures in adolescents, treated with plate osteosynthesis showed an excellent outcome with mean Nottingham score of 91.8 (85–98) [22].
A review of literature of management of midshaft clavicle fractures has been shown in Table 2. The major drawback of our study was the number of patients which significantly reduced due to the COVID-19 pandemic which coincided with our study period, and the lack of a control group. Another limitation to the study was the patient selection with a wide range of age. Patients of different ages would have different healing rates and different functional requirements which could have affected the outcomes of our study.
Table 2.
Review of literature on management of midshaft clavicle fractures
| Name of author | Year of publication | Title | Number of Patients | Results |
|---|---|---|---|---|
| Anderson et al. [23] | 1987 | Treatment of clavicular fractures: Figure-of-eight bandage versus a simple sling | 61 | Treatment with a simple sling was identical to figure of 8 bandage in terms of functional and cosmetic results. Simple sling caused lesser discomfort than figure of 8 bandage |
| Liu et al. [24] | 2010 | Comparison of Plates versus Intramedullary Nails for Fixation of Displaced Midshaft Clavicular Fractures | 110 | No significant difference in function outcomes and non-union rates between the two groups |
| Mohammed et al. [25] | 2013 | Functional Outcome of Midclavicular Fracture Fixation Utilising a Reconstruction Plate | 34 | Plate fixation provides a stable fixation with good functional outcomes |
| Althausen et al. [26] | 2013 | Clinical and financial comparison of operative and nonoperative treatment of displaced clavicle fractures | 149 | Patients with displaced clavicle fractures benefit clinically and financially with operative stabilisation inspite of the initial hospital charges due to surgery |
| Ersen et al. [4] | 2015 | Comparison of simple arm sling and figure of eight clavicular bandage for midshaft clavicular fractures | 60 | Figure of 8 bandage causes more discomfort than broad arm sling with more pain experienced initially with the former group |
| Tagliapietra et al. [27] | 2020 | Midshaft Clavicle Fractures Treated Nonoperatively Using Figure-of-Eight Bandage | 122 | This study pointed out the effectiveness of the figure of eight bandage in reducing fracture fragments and restoring clavicular length. On the contrary, residual displacement has been shown as the most likely predictor of both delayed union and non-union |
| Murray NJ et al. [28] | 2021 | Reducing unnecessary fixation of midshaft clavicle fractures | 613 | A protocol for managing clavicle fractures has demonstrated an effective management of these injuries. It is cost-effective reducing the number of patients with displaced fractures requiring fixation with a fixation rate of 21% whilst reducing the rate of symptomatic non- and malunion (3.2%). The management pathway is simple and could be introduced into any orthopaedic outpatient department with ease |
| Ali Sisman et al. [29] | 2021 | Are there any differences between the shoulder–arm sling and figure-of-eight bandage in the conservative treatment of paediatric clavicle fractures? | 41 | In the paediatric age group, there was no significant difference between shoulder–arm sling and figure-of-eight bandage in the conservative treatment of clavicle fractures. Since the shoulder–arm sling is more suitable for treatment, it may be the primary preference |
Conclusions
With better pain relief, faster functional recovery, fewer union related complications and overall better patient compliance, we found broad arm sling to be a better modality of conservative management of middle third clavicle fractures, and thus strongly advocate its use over figure of 8 brace. Our study is the first to have comprehensively demonstrated superiority of broad arm sling over figure of 8 brace in the Indian population to the best of our knowledge.
Declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. Journal of Shoulder and Elbow Surgery. 2002;11(5):452–456. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 2.Lenza M, Taniguchi LF, Ferretti M. Figure-of-eight bandage versus arm sling for treating middle-third clavicle fractures in adults: Study protocol for a randomised controlled trial. Trials. 2016;17(1):229. doi: 10.1186/s13063-016-1355-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 4.Ersen A, Atalar AC, Birisik F, Saglam Y, Demirhan M. Comparison of simple arm sling and figure of eight clavicular bandage for midshaft clavicular fractures: a randomised controlled study. The Bone & Joint Journal. 2015;97-B(11):1562–1565. doi: 10.1302/0301-620X.97B11.35588. [DOI] [PubMed] [Google Scholar]
- 5.Flandry F, Hunt JP, Terry GC, Hughston JC. Analysis of subjective knee complaints using visual analog scales. The American Journal of Sports Medicine. 1991;19(2):112–118. doi: 10.1177/036354659101900204. [DOI] [PubMed] [Google Scholar]
- 6.Lazarides S, Zafiropoulos G. Conservative treatment of fractures at the middle third of the clavicle: the relevance of shortening and clinical outcome. Journal of Shoulder and Elbow Surgery. 2006;15(2):191–194. doi: 10.1016/j.jse.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. Journal of Bone and Joint Surgery. American Volume. 2004;86(7):1359–1365. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Figueiredo GS, Tamaoki MJ, Dragone B, Utino AY, Netto NA, Matsumoto MH, Matsunaga FT. Correlation of the degree of clavicle shortening after non-surgical treatment of midshaft fractures with upper limb function. BMC Musculoskeletal Disorders. 2015;17(16):151. doi: 10.1186/s12891-015-0585-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. Journal of Bone and Joint Surgery. British Volume. 1997;79(4):537–539. doi: 10.1302/0301-620X.79B4.0790537. [DOI] [PubMed] [Google Scholar]
- 10.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) American Journal of Industrial Medicine. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 11.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clinical Orthopaedics and Related Research. 1987;214:160–164. doi: 10.1097/00003086-198701000-00023. [DOI] [PubMed] [Google Scholar]
- 12.Charles ER, Kumar V, Blacknall J, Edwards K, Geoghegan JM, Manning PA, Wallace WA. A validation of the Nottingham Clavicle Score: A clavicle, acromioclavicular joint and sternoclavicular joint-specific patient-reported outcome measure. Journal of Shoulder and Elbow Surgery. 2017;26(10):1732–1739. doi: 10.1016/j.jse.2017.03.036. [DOI] [PubMed] [Google Scholar]
- 13.Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: Longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskeletal Disorders. 2003;16(4):11. doi: 10.1186/1471-2474-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeray KJ. Acute midshaft clavicular fracture. Journal of American Academy of Orthopaedic Surgeons. 2007;15(4):239–248. doi: 10.5435/00124635-200704000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Neer CS., 2nd Nonunion of the clavicle. Journal of the American Medical Association. 1960;5(172):1006–1011. doi: 10.1001/jama.1960.03020100014003. [DOI] [PubMed] [Google Scholar]
- 16.Waldmann S, Benninger E, Meier C. Nonoperative treatment of midshaft clavicle fractures in adults. Open Orthop J. 2018;17(12):1–6. doi: 10.2174/1874325001812010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pecci M, Kreher JB. Clavicle fractures. American Family Physician. 2008;77(1):65–70. [PubMed] [Google Scholar]
- 18.Faldini C, Nanni M, Leonetti D, Acri F, Galante C, Luciani D, Giannini S. Nonoperative treatment of closed displaced midshaft clavicle fractures. Journal of Orthopaedics and Traumatology. 2010;11(4):229–236. doi: 10.1007/s10195-010-0113-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoofwijk AG, van der Werken C. Konservative Behandlung der Claviculafrakturen; eine prospektive Studie [Conservative treatment of clavicular fractures] Zeitschrift für Unfallchirurgie, Versicherungsmedizin und Berufskrankheiten. 1988;81(3):151–156. [PubMed] [Google Scholar]
- 20.Vander Have KL, Perdue AM, Caird MS, Farley FA. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. Journal of Pediatric Orthopedics. 2010;30(4):307–312. doi: 10.1097/BPO.0b013e3181db3227. [DOI] [PubMed] [Google Scholar]
- 21.Bhardwaj A, Sharma G, Patil A, Rahate V. Comparison of plate osteosynthesis versus non-operative management for mid-shaft clavicle fractures—A prospective study. Injury. 2018;49(6):1104–1107. doi: 10.1016/j.injury.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 22.Kamaci S, Bess L, Glogovac G, Colosimo AJ. Plate osteosynthesis of midshaft clavicle fractures in adolescent contact sports athletes—Adolescent clavicle fracture. Journal of Pediatric Orthopedics. Part B. 2022;31(1):1–6. doi: 10.1097/BPB.0000000000000810. [DOI] [PubMed] [Google Scholar]
- 23.Andersen K, Jensen PO, Lauritzen J. Treatment of clavicular fractures. Figure-of-eight bandage versus a simple sling. Acta Orthopaedica Scandinavica. 1987;58(1):71–74. doi: 10.3109/17453678709146346. [DOI] [PubMed] [Google Scholar]
- 24.Liu HH, Chang CH, Chia WT, Chen CH, Tarng YW, Wong CY. Comparison of plates versus intramedullary nails for fixation of displaced midshaft clavicular fractures. Journal of Trauma. 2010;69(6):E82–E87. doi: 10.1097/TA.0b013e3181e03d81. [DOI] [PubMed] [Google Scholar]
- 25.Mohammed E, Mahadane H, Mechchat A, Shimi M, Elibrahimi A, Elmrini A. Functional outcome of midclavicular fracture fixation utilising a reconstruction plate. Malaysian Orthopaedic Journal. 2013;7(3):6–9. doi: 10.5704/MOJ.1311.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Althausen PL, Shannon S, Lu M, O'Mara TJ, Bray TJ. Clinical and financial comparison of operative and nonoperative treatment of displaced clavicle fractures. Journal of Shoulder and Elbow Surgery. 2013;22(5):608–611. doi: 10.1016/j.jse.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 27.Tagliapietra J, Belluzzi E, Biz C, Angelini A, Fantoni I, Scioni M, Bolzan M, Berizzi A, Ruggieri P. Midshaft clavicle fractures treated nonoperatively using figure-of-eight bandage: Are fracture type, shortening, and displacement radiographic predictors of failure? Diagnostics (Basel). 2020;10(10):788. doi: 10.3390/diagnostics10100788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murray NJ, Johnson T, Packham IN, Crowther MAA, Chesser TJS. Reducing unnecessary fixation of midshaft clavicle fractures. European Journal of Orthopaedic Surgery & Traumatology. 2021 doi: 10.1007/s00590-021-03107-9. [DOI] [PubMed] [Google Scholar]
- 29.Sisman A, Poyraz C, Cicek AC, Kor S, Cullu E. Are there any differences between the shoulder-arm sling and figure-of-eight bandage in the conservative treatment of paediatric clavicle fractures? Journal of Children's Orthopaedics. 2021;15(6):540–545. doi: 10.1302/1863-2548.15.210139. [DOI] [PMC free article] [PubMed] [Google Scholar]