Abstract
Superior mesenteric artery (SMA) and superior mesenteric vein (SMV) thrombotic occlusion is a rare but potentially fatal condition. Though isolated mesenteric arterial occlusion associated with COVID-19 has been reported in literature, combined superior mesenteric arterial and venous thrombosis is very rare. We report the case of an 88-years-old woman with a combined superior mesenteric arterial and venous thrombotic occlusion with a previous COVID-19 pneumonia of about 15 days before, diagnosed at computed tomography angiography (CTA) scan. CTA had an important key-role for the diagnosis and evaluation of the severity of the mesenteric venous and arterious thrombosis.
Keywords: Mesenteric venous thrombosis, Mesenteric arterial thrombosis, Computed tomography angiography, Simultaneous, COVID-19 pneumonia
Introduction
Coronavirus disease 2019 (COVID-19) caused by the novel severe acute respiratory syndrome coronavirus 2 had caused a devastating pandemic in all over the world. Patients with COVID-19 common present with fever, constitutional symptoms, and respiratory symptoms. However, atypical presentations are well known, particularly arterial or venous occlusion including stroke, myocardial infarction, acute limb ischemia, mesenteric ischemia, deep venous thrombosis, and pulmonary embolism. We report an unusual combination of superior mesenteric artery (SMA) and superior mesenteric vein (SMV) occlusion in a patient with a previous COVID-19 pneumonia.
Case presentation
An 88-year-old woman was admitted to the emergency department of our hospital with a 4-day history of progressively worsening upper abdominal pain located in the epigastric area associated with diarrhea over the previous 8 days, and deterioration of her general clinical conditions. About 15 days ago, she was finally negative at oropharyngeal swab for SARS-CoV-2 by RT-PCR (about 25 days of hospitalization). She vomited once and the vomitus was unremarkable. There was no fever, loose stools, hematemesis, melena, or bleeding per rectum. She had atrial fibrillation and deep vein thrombosis, under drug treatment. Her vital signs at emergency room were stable, with a pulse rate of 70 beats/min, blood pressure of 140/90 mmHg, a respiratory rate of 20 breaths/min, and oxygen saturation of 96%. Her abdomen was globose, and so a drug therapy was immediately started.
The first radiological exam carried out in emergency was an abdomen radiography, which had documented a distension of the intestinal loops (Fig. 1).
Fig. 1.
Abdomen radiography had documented a distension of the intestinal loops, without any signs of subdiaphragmatic free air.
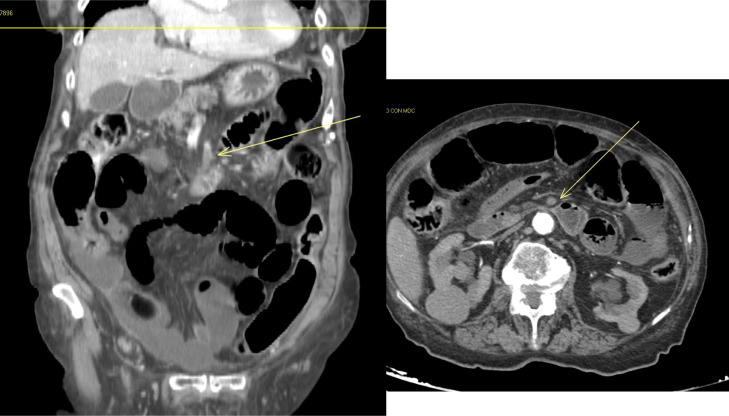
Given his persistent pain, which was out of proportion to the examination findings, mesenteric ischemia was suspected, and the patient underwent an emergency at computed tomography angiography (CTA) scan of the abdomen, that we had made with a 64 ms multidetector scanner, and the images so obtained were analyzed with a slice-thickness of 1.2 mm and MPR reconstructions (axial, sagittal, and coronal). With great our surprise, CTA had documented (Figs. 2A and B) the presence of a simultaneous superior mesenteric arterial (SMA) and venous (SMV) thrombosis. In the arterial phase, we had documented, about 6 cm from its origin, a complete occlusion of the SMA (evidence of an endoluminal thrombotic/hypodense apposition), with some small branches, although just slightly perfused, more distally. Filiform was the caliber of the spleno-mesenteric-portal venous axis. We had also documented an obstruction of the SMV, also thrombosed by hypodense endoluminal apposition, at the level of a plane adjacent to the site of the arterial (SMA) thrombosis. Furthermore, there were minimal signs of perfusion of some small distal branches for the jejunal loops; while the walls of the ileal loops appeared hypoperfused.
Fig. 2.
(A, B): Computed tomography angiography of the abdomen (MPR reconstructions – axial/coronal) had documented the presence of a simultaneous superior mesenteric arterial and venous thrombosis. In the arterial phase (upper image), there is, at about 6 cm from its origin, a complete occlusion of the superior mesenteric arterial, with evidence of an endoluminal thrombotic/hypodense apposition. In the venous phase (image below), there is an obstruction of the superior mesenteric vein, thrombosed by hypodense endoluminal apposition, at the level of a plane adjacent to the site of the same arterial thrombosis.
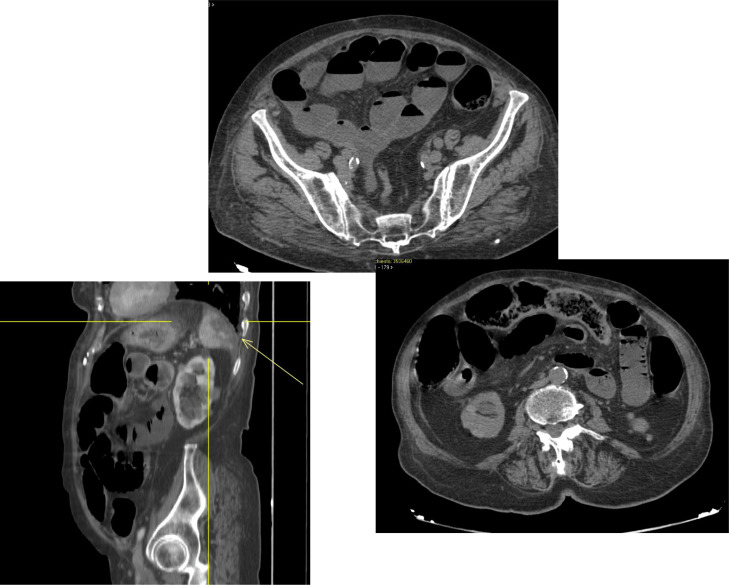
We had also documented other important CTA signs (Figs. 3A-C): the presence of concentric parietal thickening of some intestinal loops of the small intestine (distal ileal), with fluid repletion of some loops, and a significant alteration in the density of the adjacent adipose tissue, imbibed; the presence of numerous endoluminal air bubbles of some intestinal loops, mainly in the periphery, as for an initial parietal pneumatosis. In the venous phase, the spleen had multiple hypodense areas of the parenchymal, referred to the vascular nature (multiple splenic venous infarcts).
Fig. 3.
(A-C): Computed tomography angiography of the abdomen (MPR coronal reconstructions – axial/sagittal/axial) had also documented the presence of concentric parietal thickening of some intestinal loops, with fluid repletion of some of them (upper image), and a significant alteration in the density of the adjacent adipose tissue, imbibed; the presence in the venous phase of multiple hypodense areas of the spleen parenchymal, referred to the vascular nature (multiple splenic venous infarcts) – (image on the left); the presence of numerous endoluminal air bubbles, as for an initial parietal pneumatosis (image on the right).
The patient (and her family) had refused hospitalization; so we had no further informations about her clinical situation.
Discussion
SMA occlusion most commonly results from thrombosis based on atherosclerotic disease, or embolism where the embolus originates from the left atrium as a consequence of atrial fibrillation [1,2]. Interestingly, in our literature review, SMA occlusion also occurred in COVID-19 patients, with risk factors for thromboembolic diseases [3]. The mechanisms of arterial occlusion in patients with COVID-19 are still unclear. Emerging evidence suggests that COVID-19 is associated with endothelitis by diffuse endothelial damage and infiltration of inflammatory cells, and a systemic hypercoagulable state caused by hyperinflammation and hypercytokinemia. These factors of COVID-19 patients can provide a plausible explanation for the mechanisms of arterial occlusion; highlighting the impact of COVID-19 infection on both thrombosis and embolism. A SMV thrombotic occlusion, chronic, accounts for about 20%-40% of all cases of SMV, may be detected incidentally on abdominal imaging, and is differentiated from acute SMV occlusion by the presence of an extensive collateral circulation. The diagnosis of chronic SMV thrombosis is usually made on CT. Extensive thrombosis involving the portal vein, SMV, splenic vein, and IMV results in extensive bowel edema, with sequelae being persistent abdominal pain, small-bowel structures, and inability to meet nutritional needs via the gastrointestinal tract [4], [5]–6]. In our case, we reasonably suppose that it is a simultaneous arterial and mesenteric venous thrombosis, which was accentuated and made evident because it was "unmasked" by the previous COVID-19 disease (for which the patient had already been Hospitalized), concomitant with the thrombotic situation (deep vein thrombosis), which the patient had already suffering from. This had also caused multiple splenic venous infarcts. CTA is the diagnostic modality of choice. The diagnostic finding for SMV thrombosis is the presence of thrombus (hypodense), with an accuracy of about 90% for the diagnosis [7,8]. Findings of intestinal ischemia such as bowel wall thickening of greater than 3 mm, thickened mesentery, indistinct bowel margins, and ascites may also be noted. Similarly, the same diagnostic accuracy is provided by CTA for the diagnosis of mesenteric arterial thrombosis (acute or chronic).
Conclusions
This is a case of simultaneous superior mesenteric venous and arterious thrombosis that had required an urgent imaging diagnosis and clinical management of the elderly patient. Early diagnosis requires a high index of clinical suspicion. Computed tomography had an important key-role for the diagnosis and evaluation of the severity of the mesenteric venous and arterious thrombosis, and for the best management of the patients.
Patient consent
The patient confirmed the consent for publication of our case report.
Footnotes
Competing Interests: The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
References
- 1.Chou EL, Wang LJ, McLellan RM, Feldman ZM, Latz CA, LaMuraglia GM, et al. Evolution in the presentation, treatment, and outcomes of patients with acute mesenteric ischemia. Ann Vasc Surg. 2021;74:53–62. doi: 10.1016/j.avsg.2021.01.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Florim S, Almeida A, Rocha D, Portugal P. Acute mesenteric ischaemia: a pictorial review. Insights Imaging. 2018;9(5):673–682. doi: 10.1007/s13244-018-0641-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheruiyot I, Kipkorir V, Ngure B, Misiani M, Munguti J, Ogeng'o J. Arterial thrombosis in coronavirus disease 2019 patients: a rapid systematic review. Ann Vasc Surg. 2021;70:273–281. doi: 10.1016/j.avsg.2020.08.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar S, Kamath PS. Acute superior mesenteric venous thrombosis: one disease or two? Am J Gastroenterol. 2003;98(6):1299–1304. doi: 10.1111/j.1572-0241.2003.07338.x. [DOI] [PubMed] [Google Scholar]
- 5.Thatipelli MR, McBane RD, Hodge DO, Wysokinski WE. Survival and recurrence in patients with splanchnic vein thromboses. Clin Gastroenterol Hepatol. 2010;8(2):200–205. doi: 10.1016/j.cgh.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 6.Abu-Daff S, Abu-Daff N, Al-Shahed M. Mesenteric venous thrombosis and factors associated with mortality: a statistical analysis with five-year follow-up. J Gastrointest Surg. 2009;13(7):1245–1250. doi: 10.1007/s11605-009-0833-7. [DOI] [PubMed] [Google Scholar]
- 7.Acosta S, Alhadad A, Ekberg O. Findings in multi-detector row CT with portal phase enhancement in patients with mesenteric venous thrombosis. Emerg Radiol. 2009;16(6):477–482. doi: 10.1007/s10140-009-0807-9. [DOI] [PubMed] [Google Scholar]
- 8.Furukawa A., Kanasaki S., Kono N., Wakamiya M., Tanaka T., Takahashi M., et al. CT diagnosis of acute mesenteric ischemia from various causes. Am J Roentgenol. 2009;192(2):408–416. doi: 10.2214/AJR.08.1138. [DOI] [PubMed] [Google Scholar]