Abstract
Intravascular leiomyomatosis is a rare disease characterized by extension of benign smooth muscle proliferation into uterine and pelvic vessels. The involved vessels are almost always veins and rarely lymphatics. Intraarterial growth has not been described. Intravascular leiomyomatosis can show different morphologic features that are commonly described in leiomyomas. The differential diagnosis includes endometrial stromal sarcoma, lymphangioleiomyomatosis and leiomyosarcoma. Immunohistochemistry is helpful to establish a correct diagnosis. The condition is histologically benign; however, these lesions can spread by the venous system into the inferior vena cava, heart, and lungs. Treatment of this condition is surgical. The spread of intravenous leiomyomatosis exclusively by uterine lymphatics to the pelvic lymph nodes has not been previously reported.
Keywords: Intravascular leiomyomatosis, lymphatic metastasis, lymphangioleiomyomatosis, endometrial stromal sarcoma
Introduction
Intravascular leiomyomatosis, also known as intravenous leiomyomatosis, is characterized by presence of smooth muscle within venous spaces in the myometrium, usually in conjunction with a leiomyoma [1,2]. Although presence of tumor within lymphatics in addition to veins is alluded to in literature, exclusive lymphatic spread with lymph node metastases has not been previously reported.
Case report
A 50-year-old woman presented with left flank pain. CT scan of the pelvis showed an enlarged uterus with multiple large leiomyomata as well as pelvic lymph node enlargement. Hysterectomy with bilateral salpingo-oophorectomy and pelvic lymph node dissection was performed. Gross examination revealed a multifibroid uterus. Separately sent pelvic lymph nodes showed well-circumscribed, whorled lesions resembling leiomyomata. Microscopically, in addition to typical leiomyomata, a 11.5 cm intramural tumor with epithelioid cells, very rare mitosis and no necrosis was identified (Figure 1A and 1B). Adjacent to as well as away from this mass, several large endothelial-lined spaces with intravascular extension of the same epithelioid tumor were noted. The endothelial cells were positive for D2-40 and negative for CD31, confirming that they are lymphatic and not venous channels (Figure 1C and 1D). All the pelvic lymph nodes were replaced by tumor (Figure 1E and 1F). Due to the unusual morphology and pattern of spread, immunohistochemical stains were performed to rule out endometrial stromal sarcoma and lymphangioleiomyomatosis. The lesion was positive for desmin (Figure 1G), caldesmon, and negative for CD10 and HMB45 (Figure 1H). Proliferative index was extremely low (<1%). Based on the morphology and immunophenotype, the tumor was consistent with an epithelioid leiomyoma with a highly unusual pattern of spread through myometrial lymphatics to regional lymph nodes.
Figure 1.
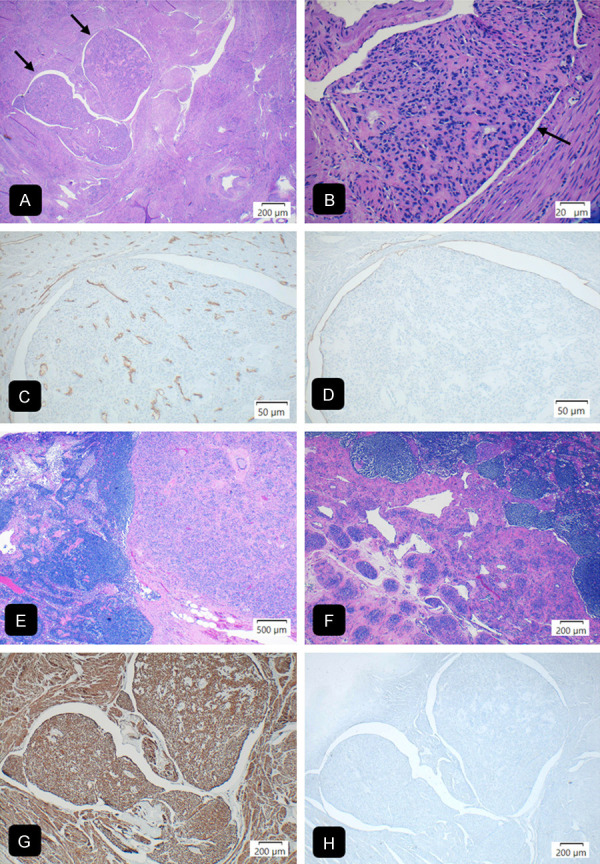
Uterine intravascular leiomyomatosis with lymphatic spread to pelvic lymph nodes. (A) Myometrium with intravascular proliferation of benign smooth muscle (H&E, ×40). (B) Epithelioid smooth muscle cells with mild atypia identical in appearance to epithelioid leiomyoma (H&E, ×400). (C, D) Tumor within lymphatic vessels. CD31 immunostain (C) highlights endothelial lining of blood vessels and is negative in the lymphatic endothelium. D2-40 immunostain (D) is positive in the lymphatic vessel endothelium (×200). (E, F) Pelvic lymph node with benign epithelioid smooth muscle proliferation (×20 and ×40 respectively) identical to the intravascular proliferation (G). Desmin immunostain diffusely positive in the tumor cells and myometrium (×40). (H) Negative HMB45 immunostain (×40) performed to rule out lymphangioleiomyomatosis in the lymph node.
Appropriate consent was signed by the patient to participate in this study.
Discussion
Intravascular leiomyomatosis (IVL) is an uncommon phenomenon characterized by an extension of benign smooth muscle into uterine and pelvic veins and rarely lymphatics, typically associated with uterine leiomyomas. The disease affects predominantly patients of reproductive age and occasionally older women [1,2]. Clinically, it mimics symptoms of leiomyomas and they often coexist [1,2]. Most common complaints include pelvic pain and abnormal uterine bleeding; often patients have a history of recurrent leiomyomas with repeated myomectomies [1,2]. Rarely IVL can be associated with benign metastasizing leiomyoma and can metastasize by pelvic veins into inferior vena cava and the right heart and subsequently into the lungs forming a mass or causing pulmonary embolism [1,2]. Grossly, the uteri are usually enlarged with wormlike plugs of smooth muscle proliferation in the myometrial veins [2]. These plugs can also be seen in pelvic veins within the broad ligament adjacent to ovaries and vagina [1]. The tumor cut surface can vary from soft to firm and rubbery, sometimes gelatinous, or translucent and occasionally hemorrhagic and/or calcified with degenerative features [1]. Extrauterine extension has been reported in approximately 30% of cases [1,3]. Ordinary leiomyomas often coexist as in our case and the IVL is found often at the periphery of the leiomyomas [1]. IVL can be also associated with adenomyosis, or both adenomyosis and leiomyomas [3].
Microscopically, the IVL can resemble any leiomyoma variant and is usually composed of bland spindle cells surrounded by endothelial cells. Other morphologic subtypes described in ILV include cellular leiomyomas, leiomyomas with bizarre nuclei, lipoleiomyomas, and leiomyomas with myxoid or epithelioid features. Rarely intravascular endometrial tissue can be also seen [1-3]. The differential diagnosis includes endometrial stromal sarcoma (ESS), lymphangioleiomyomatosis, and leiomyosarcoma [1-3].
IVL is composed of spindle or epithelioid smooth muscle cells usually with thick-walled variably-sized blood vessels in contrast to the spiral arteriole-like vessels characteristic of ESS. In addition, the irregular tongues of myometrial invasion, small round blue cells of endometrial stroma, and increased mitotic activity seen in ESS are all absent in IVL [1,4]. Lastly, an immunohistochemical panel can be helpful to differentiate ESS and IVL with CD10 positive in ESS and smooth muscle markers positive in IVL.
Uterine lymphangioleiomyomatosis is an extremely rare lesion in the PEComa category. It can be sporadic or associated with tuberous sclerosis [1,5,6]. Lymphangioleiomyomatosis is characterized by a tongue-like intravascular growth pattern of bland spindle cells resembling IVL and distinguishing between the two can be challenging [1,3,5]. HMB-45 immunostain is typically positive in lymphangioleiomyomatosis and negative in IVL [1,5,6]. IVL with an epithelioid or myxoid morphology can mimic leiomyosarcoma; however high-grade nuclear features, increased mitotic activity and tumor necrosis are not seen in IVL [1].
In IVL, spread by venous channels into inferior vena cava, heart, and lung has been well-described in the literature. However, spread to lymph nodes exclusively through lymphatic vessels is very unusual [7]. Pelvic lymph nodes have been reported as an unusual site of metastases in patients who have benign metastasizing leiomyomas involving IVC, heart, and lungs but not as an exclusive site of metastasis in IVL [8].
Conclusion
Intravascular leiomyomatosis is a rare condition with no reported progression to malignancy. Typically, benign smooth muscle is present within venous channels of the myometrium of a leiomyomatous uterus. We present a rare case of intravascular leiomyomatosis with spread exclusively by lymphatics to pelvic lymph nodes.
Disclosure of conflict of interest
None.
References
- 1.Ip PP, Tse KY, Tam KF. Uterine smooth muscle tumors other than the ordinary leiomyomas and leiomyosarcomas: a review of selected variants with emphasis on recent advances and unusual morphology that may cause concern for malignancy. Adv Anat Pathol. 2010;17:91–112. doi: 10.1097/PAP.0b013e3181cfb901. [DOI] [PubMed] [Google Scholar]
- 2.Clement PB, Young RH, Scully RE. Intravenous leiomyomatosis of the uterus. A clinicopathological analysis of 16 cases with unusual histologic features. Am J Surg Pathol. 1988;12:932–945. [PubMed] [Google Scholar]
- 3.Hirschowitz L, Mayall FG, Ganesan R, McCluggage WG. Intravascular adenomyomatosis: expanding the morphologic spectrum of intravascular leiomyomatosis. Am J Surg Pathol. 2013;37:1395–1400. doi: 10.1097/PAS.0b013e31828b2c99. [DOI] [PubMed] [Google Scholar]
- 4.Norris HJ, Parmley T. Mesenchymal tumors of the uterus. V. Intravenous leiomyomatosis. A clinical and pathologic study of 14 cases. Cancer. 1975;36:2164–2178. doi: 10.1002/cncr.2820360935. [DOI] [PubMed] [Google Scholar]
- 5.Szpurek D, Szubert S, Zielinski P, Frankowski A, Sajdak S, Moszynski R. Malignant presentation of uterine lymphangioleiomyomatosis. Taiwan J Obstet Gynecol. 2015;54:603–607. doi: 10.1016/j.tjog.2015.08.015. [DOI] [PubMed] [Google Scholar]
- 6.Clay MR, Gibson P, Lowell J, Cooper K. Microscopic uterine lymphangioleiomyomatosis perivascular epithelioid cell neoplasm: a case report with the earliest manifestation of this enigmatic neoplasm. Int J Gynecol Pathol. 2011;30:71–75. doi: 10.1097/PGP.0b013e3181efe08d. [DOI] [PubMed] [Google Scholar]
- 7.Lin J, Song X, Liu C. Pelvic intravascular leiomyomatosis associated with benign pulmonary metastasizing leiomyoma: clinicopathologic, clonality, and copy number variance analysis. Int J Gynecol Pathol. 2014;33:140–145. doi: 10.1097/PGP.0b013e31828def26. [DOI] [PubMed] [Google Scholar]
- 8.Yoon G, Kim TJ, Sung CO, Choi CH, Lee JW, Lee JH, Bae DS, Kim BG. Benign metastasizing leiomyoma with multiple lymph node metastasis: a case report. Cancer Res Treat. 2011;43:131–133. doi: 10.4143/crt.2011.43.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]


