Abstract
Background
The Million Hearts Cardiovascular Disease Risk Reduction Model provides financial incentives for practices to lower 10-year atherosclerotic cardiovascular disease (ASCVD) risk for high risk (ASCVD >=30%) Medicare patients. To estimate average practice-level ASCVD risk reduction, we applied optimal trial outcomes to a real-world population with high ASCVD risk.
Methods
This study uses observational registry data from the National Cardiovascular Data Registry® PINNACLE Registry® from January 2013 to June 2016. We modeled ASCVD risk reductions using historical clinical trial data (reducing cholesterol by 26.5%, reducing systolic blood pressure by 10.9%, reducing smoking rates by 21.8%) the average reduction in ASCVD risk associated with individual and combined risk factor modifications, and then percentage of practices achieving the various incentive thresholds for the Million Hearts Model.
Results
The final study population included 135,166 patients, with 16,248 (12.0%) with 10-year ASCVD risk of >=30%, but without existing ASCVD. The mean 10-year ASCVD risk was 41.9% (±1 SD of 11.6). Using risk factor reductions from clinical trials, lowering cholesterol, blood pressure and smoking rates reduced 10-year ASCVD risk by 3.3% (±3.1), 6.3% (±1.1) and 0.5% (±1.3), respectively. Combining all 3 reductions resulted in a 9.7% (±3.6) reduction, with 67 (27.0%) of practices achieving a patient-level average 10-year ASCVD risk reduction of ≥10%, 181 (73.0%) achieving a 2 to 10% reduction, and no practice achieving <2% reduction.
Conclusions
In cardiology practices, about one out of eight patients have a 10-year ASCVD risk greater than 30% and qualify as high risk in the Million Hearts model. If practices target the three main modifiable risk factors and achieve reductions similar to clinical trial results, ASCVD risk could be substantially lowered and all practices could receive incentive payments. These findings support the potential benefit of the Million Hearts model and provide guidance to participating practices.
Keywords: Health policy, value-based care, prevention, cardiovascular
Over recent decades, myocardial infarction deaths have decreased substantially due to improvements in both the prevention of and treatment for these coronary events.1 Yet, despite these improvements, cardiovascular disease remains the leading cause of death in the US, and atherosclerotic risk factors remain prevalent.2 The two most recent cholesterol management guidelines focus heavily on an individual’s 10-year atherosclerotic cardiovascular disease (ASCVD) risk as a key factor in deciding whether or not to prescribe a statin.3,4 These guidelines have made an important shift in the clinical mindset toward a focus on ASCVD risk as an indicator of which individuals need the most aggressive risk factor reduction.
Concurrent with these evolving cardiovascular risk reduction recommendations, the Centers for Medicare and Medicaid Services (CMS) have been shifting their payment strategy toward financially rewarding better health outcomes. In 2015, CMS launched their largest test yet of a value-based payment program for prevention aimed specifically at reducing ASCVD risk as defined in the guidelines. This program, entitled the Million Hearts Cardiovascular Risk Reduction Model (MH Model), randomized practices into an intervention or control group, with the intervention group receiving financial incentives linked to lowering practice-level ASCVD risk for those patients whose baseline ASCVD risk is greater than or equal to 30%.5 Bonus payments increased with increasing ASCVD risk reduction, such that a mean practice-level ASCVD risk reduction of two to ten percentage points among high-risk patients resulted in a $5 per member per month cardiovascular care management fee, and a reduction of more than ten percentage points resulted in a $10 per member per month fee.
Practices participating in the MH Model, and providers in general seeking to reduce their population’s ASCVD risk, have several modifiable risk factors to target including blood pressure, cholesterol, and smoking. We sought to use a real-world clinical database to model reductions in ASCVD risk that practices might achieve, the results of which could guide practices in implementing intervention to improve modifiable cardiovascular risk factors.
Methods
Data Source
The study data source was the National Cardiovascular Data Registry NCDR PINNACLE Registry. The PINNACLE Registry is part of a national office-based cardiovascular quality improvement program in which cardiology practices voluntarily participate and submit data.6,7 Most data are obtained through a validated electronic health record mapping algorithm designed to comprehensively capture required data elements, with the data collected at the point of care through a paper chart abstraction form. Abstracted data elements include demographics, insurance status, and detailed clinical information including symptoms, medical conditions, vital signs, medications, and laboratory values. Rigorous data definitions, standard data collection and transmission, and periodic data quality checks are employed to ensure registry data quality.8,9 The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study Population
The study population was generated to match the MH Model. We identified all patients aged 40–79 without ASCVD in the PINNACLE Registry between January 1, 2013, and June 30, 2016. Similar to the MH Model, we excluded patients with end-stage renal disease, or those receiving hospice care. We performed our analysis for all patients regardless of insurance type in the PINNACLE Registry. However, since the MH Model only included Medicare patients, we performed a sensitivity analysis among patients with Medicare only. Additionally, to assess for a reduced treatment effect of lowering cholesterol for patients already on a statin, we performed a sensitivity analysis of patients not on a statin at baseline.
ASCVD Risk Assessment and Modeling
The primary study outcome measure was the percentage reduction in ASCVD risk, amongst patients with a baseline ASCVD risk of at least 30%, associated with various assumed reductions in the individual risk factors. The ASCVD risk calculation requires the parameters of age, sex, race, blood pressure, total cholesterol, HDL cholesterol, diabetes status, smoking status and hypertensive medications status. Among these risk factors, the blood pressure, total cholesterol and smoking status are modifiable. For ASCVD risk estimation, we used any available risk factor values, such as blood pressure measurement and cholesterol. If a patient had risk factor values from multiple visits in the registry, we used values from the most recent patient visit during the study period. Race was self-reported by patients and, when missing, no ASCVD risk score was calculated as race is an input variable required by the ASCVD calculator. We calculated ASCVD risk using the pooled cohort risk equations published with the 2013 ASCVD risk assessment guidelines.10 We attempted to use the The Million Hearts Longitudinal ASCVD Risk Assessment Tool; however, we were unable obtain a detailed formula to apply to our dataset.11,12
To model changes in ASCVD risk, the baseline average values for total cholesterol and systolic blood pressure were reduced by the percentage reductions reported in landmark clinical trials. For cholesterol reduction, we applied a 26.5% reduction in total cholesterol as was realized for LDL-cholesterol using moderate intensity statin therapy in the Heart Outcomes Prevention Evaluation (HOPE)-3 trial of intermediate risk people without cardiovascular disease.13 For systolic blood pressure lowering, we assumed a 10.9% reduction as was obtained in the Systolic Blood Pressure Intervention Trial (SPRINT) of patients at increased cardiovascular risk.14 To model smoking cessation rates, data were taken from a randomized controlled trial comparing smoking cessation medications, which showed smoking cessation success rates at 9 to 24 weeks of 21.8% with varenicline.15 If a patient was a smoker (binary variable in the model), their ASCVD risk associated with smoking (the beta coefficient on that variable in the risk score) was multiplied by 0.782, to reduce the risk by 21.8%. Following the Million Heart Model program design, we only applied the improvement in risk factors to those patients with elevated risk at baseline, defined as a baseline 10-year ASCVD risk of greater than or equal to 30%. We compared these modeled average ASCVD risk levels to baseline average ASCVD risk levels. The reductions were applied at the individual level.
Given that real-world performance with risk factor reduction may be less than clinical trials, we performed a sensitivity analysis assuming 60% of the reduction realized in the clinical trials, based on prior work demonstrating gaps between clinical trials and real-world practice patterns.16 Thus, this sensitivity analysis assumes a 15.9% reduction in total cholesterol, a 6.5% reduction in systolic blood pressure, and a 13.1% reduction in smoking rates.
To model potential bonus payments, following CMS program rules, the calculation is of practice-level averages of the ASCVD risk among those patients who are at baseline high risk. The number of patients with ASCVD risk of at least 30% were multiplied by the per beneficiary per month cardiovascular care management fee expected on average by the practice performance, and then annualized by multiplying by 12 months. Practices with a mean practice-level ASCVD risk reduction of two to ten percentage points among high-risk patients would receive a $5 per beneficiary per month cardiovascular care management fee, and practices with a reduction of more than ten percentage points would receive a $10 per beneficiary per month fee.
Statistical Analysis
The patient clinical characteristics were described and baseline ASCVD risk calculated. Practice geographic characteristics were by census region. We then calculated the baseline percentage of patients with elevated total cholesterol of greater than or equal to 200 mg/dL, elevated systolic blood pressure of greater than or equal to 140 mm Hg, and current smoking among all patients and patients with ASCVD risk greater than 30%. To assess the combination of risk factors contributing to overall ASCVD risk, we calculated the baseline percentage of patients with various combinations of high cholesterol, high systolic blood pressure and smoking. We then calculated the baseline individual and average ASCVD risk for all patients with risk of at least 30%. Lastly, we modeled individual and combination risk reductions using evidence-based estimates from randomized clinical trials, as noted above. All analyses were performed with SAS version 9.3 (SAS Institute, Cary, North Carolina). A waiver of written informed consent and authorization for this study was granted by an internal institutional review board, Advarra.
Results
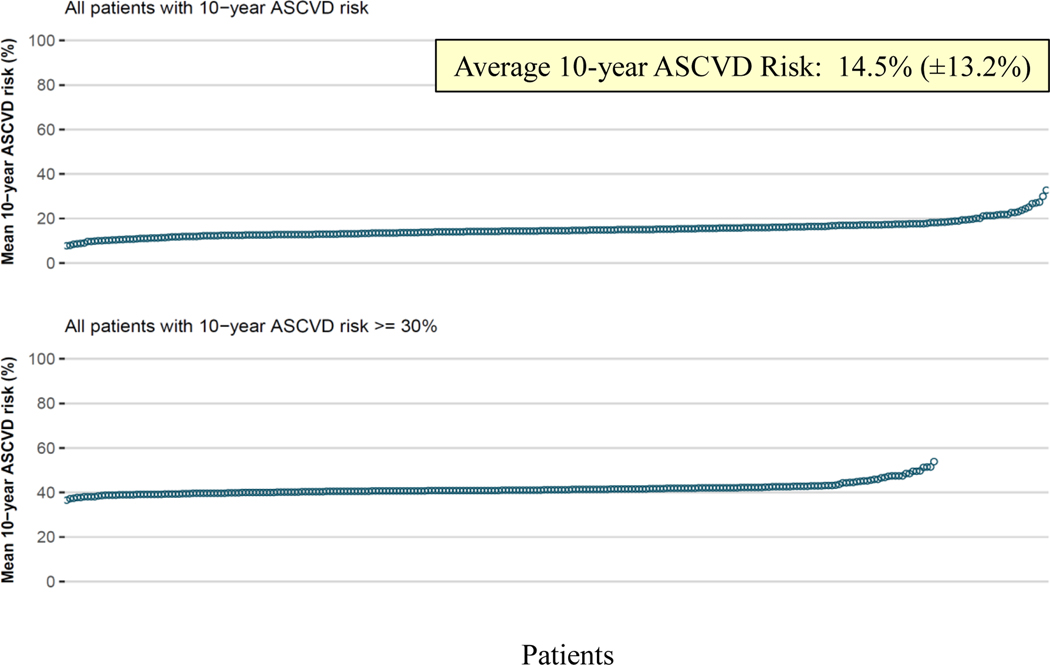
The initial study population of patients without ASCVD included 3,724,991 patients with their most recent encounter. A total of 3,589,825 patients were excluded due to missing at least one data point required for input to calculate the ASCVD risk score. The final study population included 135,166 patients in 280 clinic sites, with an average number of patients per site of 483, of which 248 clinic sites had patients with 10-year ASCVD risk of at least 30%. The practices had an average of 10.3 (± 13.7) physicians, with 46 (16.4%) in the Midwest, 50 (17.9%) in the Northeast, 152 (54.3%) in the South and 32 (11.4%) in the West. The characteristics of the patients are described in Table 1, with 55.4% female, 89.6% white, 65.6% with hypertension and 21.4% with diabetes. In comparing to those patients missing data, the study population was older and with more males, more patient who are white and with private insurance and more comorbidities. (Table 1) Among these patients, the average overall baseline ASCVD risk was 14.5% (± 13.2%), and 16,248 (12.0%) had an ASCVD risk 30% or greater with an average risk of 41.9% (± 11.6) among this high risk group. (Figure 1) These high risk patients included 4,233 (26.1%) with total cholesterol at least 200 mg/dL, 8,342 (51.3%) with systolic blood pressure of 140 mm Hg or greater, and 3,204 (19.1%) who were current smokers. (Table 2)
Table 1.
Baseline Patient Characteristics
| Total Patients (n = 3,724,991) | Patient Missing Data for ASCVD Calculation (n = 3,589,825) | Study Patients (n = 135,166) | |
|---|---|---|---|
| Age (mean ± SD) | 56.9 ± 19.6 | 56.8 ± 19.9 | 61.2 ± 10.2 |
| Sex | |||
| Male | 1,559,473 (42.6%) | 1,499,163 (42.5%) | 60,310 (44.6%) |
| Female | 2,102,712 (57.4%) | 2,027,856 (57.5%) | 74,856 (55.4%) |
| Race | |||
| White | 1,905,291 (86.8%) | 1,784,246 (86.6%) | 121,045 (89.6%) |
| Black | 235,321 (10.7%) | 224,280 (10.9%) | 11,041 (8.2%) |
| Other | 55,493 (2.5%) | 52,413 (2.5%) | 3,080 (2.3%) |
| Insurance | |||
| No insurance | 4,370 (1.3%) | 4,264 (1.4%) | 106 (0.7%) |
| Private | 243,819 (73.9%) | 231,535 (73.6%) | 12,284 (78.5%) |
| Medicare | 64,947 (19.7%) | 62,238 (19.8%) | 2,709 (17.3%) |
| Medicaid | 9,035 (2.7%) | 8,865 (2.8%) | 170 (1.1%) |
| Other | 7,965 (2.4%) | 7,576 (2.4%) | 389 (2.5%) |
| Missing | 1,006,336 | 41,490 | |
| Total cholesterol mg/dl (mean± SD) | 180.9 ± 42.2 | 179.8 ± 42.2 | 185.6 ± 41.9 |
| Tobacco use | |||
| Never | 977,914 (60.7%) | 904,373 (61.1%) | 73,541 (56.1%) |
| Current | 247,370 (15.3%) | 228,107 (15.4%) | 19,263 (14.7%) |
| Quit within past 12 months | 4,159 (0.3%) | 3,632 (0.2%) | 527 (0.4%) |
| Quit more than 12 months | 382,084 (23.7%) | 344,309 (23.3%) | 37,775 (28.8%) |
| Tobacco screening not performed | 6 (0.0%) | 5 (0.0%) | 1 (0.0%) |
| Hypertension | 1,338,502 (48.4%) | 1,256,972 (47.6%) | 81,530 (65.6%) |
| Systolic Blood Pressure, mm Hg mean ±SD |
127.1 ± 17.8 |
127.0 ± 17.8 |
129.1 ± 16.8 |
| Diastolic Blood Pressure, mm Hg, mean ± SD | 76.0 ± 11.2 |
75.9 ± 11.2 |
76.8 ± 10.7 |
| Diabetes Mellitus (any) | 396,489 (12.9%) |
367,518 (12.5%) |
28,971 (21.4%) |
| High Density Lipoprotein (HDL) cholesterol, mg/dl, mean ± SD |
51.8 ± 19.1 |
51.7 ± 19.1 | 52.4 ± 18.9 |
| Low Density Lipoprotein (LDL) cholesterol, mg/dl, mean ± SD |
102.3 ± 37.2 |
101.4 ± 37.1 |
105.9 ± 37.2 |
| Chronic Liver Disease | 24,473 (0.9%) | 23,107 (0.9%) | 1,366 (1.2%) |
| Intracranial Hemorrhage | 19,282 (0.5%) | 18,872 (0.5%) | 410 (0.3%) |
| Dyslipidemia | 1,078,619 (37.9%) | 993,317 (36.4%) | 85,302 (71.6%) |
| Heart Failure | 263,417 (9.0%) | 251,387 (8.9%) | 12,030 (9.3%) |
FIGURE 1:
10-year ASCVD Risk
TABLE 2.
Patients with individual risk factor and combinations of risk factors.
| Cardiac Risk Factors | All Patients (n = 135,166) | Patients with ASCVD ≥ 30% (n = 16,248) |
|---|---|---|
| Total Cholesterol ≥ 200 mg/dL | 46,283 (34.2%) | 4,233 (26.1%) |
| Systolic Blood Pressure ≥ 140 mm Hg | 34,553 (25.6%) | 8,342 (51.3%) |
| Current Smoking | 19,263 (14.7%) | 3,204 (19.1%) |
| Risk Factor Combinations | ||
| Cholesterol + Blood Pressure reduction | 12,118 (9.0%) | 2,421 (14.9%) |
| Cholesterol reduction + Smoking cessation | 6,717 (5.1%) | 903 (5.7%) |
| Blood Pressure reduction + Smoking cessation | 5,089 (3.6%) | 1,525 (9.6%) |
| Cholesterol + Blood Pressure reduction + Smoking cessation | 1,819 (1.4%) | 522 (3.3%) |
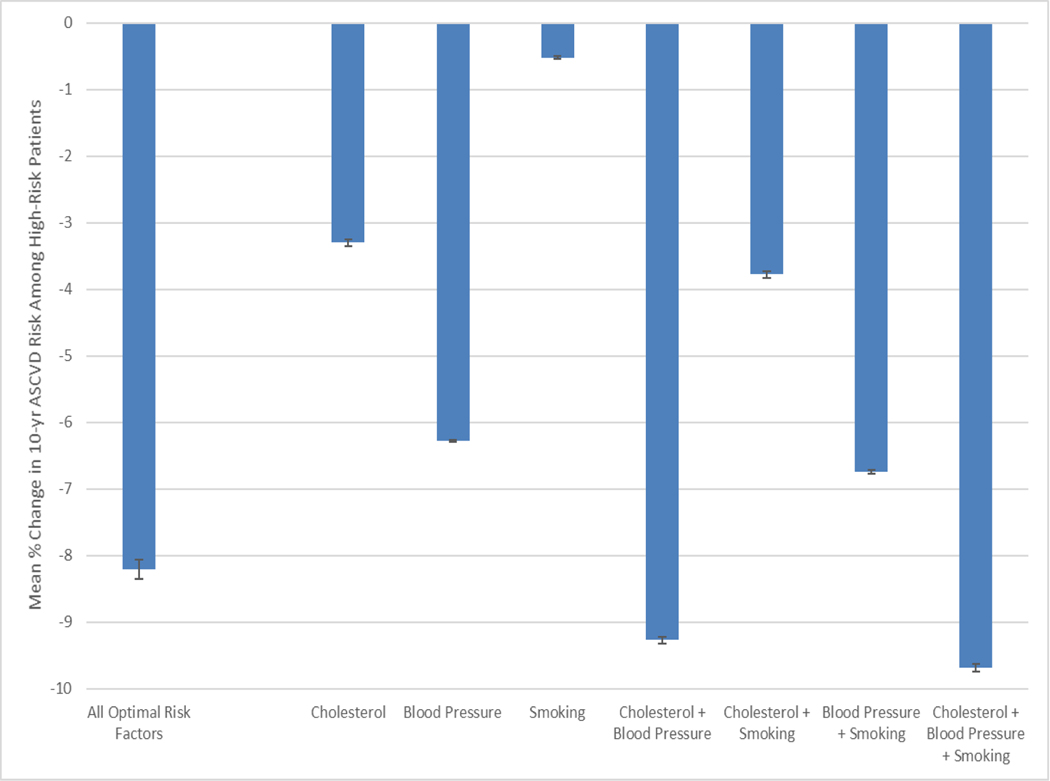
In the modeling analysis using risk factor reductions from clinical trials, lowering cholesterol, blood pressure and smoking rates reduced ASCVD risk by 3.3% (±3.1), 6.3% (±1.1) and 0.5% (±1.3), respectively. Combining all three evidence-based reductions resulted in a 9.7% (±3.6) lower ASCVD risk among high-risk patients, with 67 (27.0%) of practices achieving a ≥10% reduction in ASCVD risk, 181 (73.0%) achieving a 2 to 10% reduction in ASCVD risk, and no practice achieving <2% reduction in ASCVD risk. With all of the modifiable risk factors at goal, the mean ASCVD risk decreased by 8.2% (±9.0). (Figure 2) The results were similar in the sensitivity analysis of only Medicare patients (n = 527) where lowering cholesterol, blood pressure and smoking rates reduced ASCVD risk by 2.3% (±2.4), 6.3% (±1.1) and 0.5% (±1.3), respectively. Combining all three evidence-based reductions resulted in an 8.8% (±2.7) lower ASCVD risk among high-risk patients. In patients not taking a statin at baseline (n = 7,935) lowering cholesterol, blood pressure and smoking rates reduced ASCVD risk by 3.5% (±3.4), 6.3% (±1.1) and 0.5% (±1.2), respectively. Combining all three evidence-based reductions resulted in a 9.9% (±3.9) lower ASCVD risk among high-risk patients.
FIGURE 2:
ASCVD Risk Reduction Modeling Associated with Practice-Level Risk Factor Reductions in High Risk Patients (± 1 Standard Deviation). All Optimal Risk Factors is when total cholesterol is less than 200 mg/dL, systolic blood pressure is less than 140 mm Hg, and the patient is a non-smoker.
In modeling the potential financial implications, a practice in this study with the average number of patients per practice site of 483 and earning the maximum bonus of $10 per beneficiary per month could receive an average $57,960 per year. The same practice earning, on average, the lower bonus of $5 per beneficiary per month could receive an average of $28,980. In our sensitivity analysis assuming 60% of the risk factor reduction realized in clinical trials, only 3 practices would achieve ≥10% reduction in ASCVD risk, compared to 67 practices in the primary analysis. However, all remaining practices would still achieve >2% reduction in ASCVD risk.
Discussion
In cardiology practices, about one in eight patients have a 10-year ASCVD risk greater than 30%. As practices look beyond the individual patient to their entire population to drive reductions in ASCVD risk, those practices will be evaluating the relative merits of quality improvement initiatives targeting particular modifiable risk factors. Practices participating in the MH Model may additionally be interested to know what reductions they can expect with various interventions, and how those reductions can apply to receiving cardiovascular care management fees from Medicare. Our study demonstrated that amongst these high-risk patients, following evidence-based approaches can result in substantial reductions in ASCVD risk. Achieving a combination of trial-based reductions in cholesterol, blood pressure and smoking rates resulted in a nearly 10% lower practice-level ASCVD risk. Following this approach and achieving similar results would lead to all MH Model practices receiving some bonus, and one quarter receiving the maximum bonus.
This analysis of real-world data supports the rationale for Medicare’s testing of the MH Model. Medicare in recent years has begun moving from process measures, such as assessing the provision of heart failure teaching, toward more outcome measures, such as 30-day post-hospital discharge mortality for patients with heart failure. In the ambulatory realm, Medicare assesses intermediate outcome measures, such as diabetes and hypertension control. With the MH Model, Medicare tests the concept that ASCVD risk as a more composite intermediate outcome measure, with clear predictive linkage to clinical endpoints such as myocardial infarction and stroke, can be modified through financial incentives. Moreover, ASCVD risk as a target fits closely with the American College of Cardiology / American Heart Association (ACC/AHA) cholesterol management guidelines. Medicare recently released the third annual evaluation of the MH Model program, which showed improvement in cardiovascular disease preventive care, though without reductions in observed myocardial infarctions or strokes. The intervention group had an average decline of 8 percentage points in ASCVD risk, compared to a 7 percentage point decline in the control group.17 These results align quite closely with our study results, which showed an average 9.7 percentage point decline in ASCVD risk with implementing all evidence-based strategies. With performance period completion at the end of 2021, the final results of the MH Model will ultimately demonstrate whether or not these financial incentives successfully lower ASCVD risk compared to controls.
These study results provide a roadmap for practices on how to succeed in lowering ASCVD risk, and validate the results from Medicare’s third year evaluation. For a practice with limited time and resources, choosing to only focus on one practice-level intervention initially, our results show that focusing on blood pressure control would have the greatest practice-level ASCVD risk lowering impact at over 6%. Cholesterol control would have the next greatest impact at lowering practice-level risk just over 3% and lastly practice-wide reductions in smoking rates lowering overall ASCVD risk by 0.5%. While smoking is clearly a strong risk factor for cardiovascular events and all efforts should be made by clinicians to work with patients on smoking cessation, our study results were likely due to the smaller number of high-risk patients (19.1%) who smoked compared to those high-risk patients who had high blood pressure (51.3%) or high cholesterol (26.1%). The federal Million Hearts initiative, closely related to the MH Model, provides a variety of tools for practices to improve blood pressure and cholesterol control, and reduce smoking rates.18 For example, Million Hearts provides a Hypertension Control Change Package with practice level change management guidance and resources.19
Our study has several limitations, starting with the model assumption of risk factor control rates from randomized-controlled trials. The clinical trial environment is clearly different from real-world practice; however, the trial data show what is possible and it is reasonable to assume that a robust practice-level quality improvement program focused on ASCVD risk factors could achieve similar results. A study of a multimodal blood pressure control program in diverse real-world clinical settings resulted in an 8.7% reduction in systolic blood pressure,20 similar to the 10.9% systolic blood pressure reduction from the SPRINT trial that we used as the blood pressure input in our study model. While our data may over-estimate the actual results that will be realized in the MH Model, our analysis supports that improvements can be made with evidence-based approaches and that practices can succeed financially in the MH Model. In sensitivity analyses, we also provide estimates in practice-level reduction in ASCVD risk if 60% of the risk factor reduction realized in clinical trials is seen in routine clinical practice. Second, we chose seminal clinical trials, and the medications and populations studied may differ from the PINNACLE Registry. However, as a proof of concept, our results demonstrate approximate results that can be expected by practices. Third, practices that participate in the PINNACLE Registry may be more committed to quality improvement, thus the baseline risk factor rates may be lower than in a general population. However, within the PINNACLE Registry of cardiology practices, only 59.6% of patients achieve blood pressure goals16 and only 67.6% of statin-eligible patients were receiving statins.21 Given that ASCVD risk factor modifiers may already be in place, our results may overestimate the impact of the trial-based risk factor reductions on overall ASCVD risk. The combination of risk factor reductions has not been studied, so it is unknown if combining blood pressure, cholesterol and smoking control interventions would have a reduced effect on each component, or potentially even a greater synergistic effect. Baseline case-mix in each practice will likely also factor into the ability to reduce ASCVD risk, and individual risk factor reduction may be less effective if that particular risk factor is already at or below normal values. Moreover, our results assume clinical trial levels of adherence to strategies used to lower blood pressure, cholesterol or medications used to lower smoking rates. In real world-practice, risk factor reductions can vary over time and optimal control of multiple risk factors at once can be challenging22; however, all practices achieved some degree of bonus even with assuming only 60% reduction in risk factors. Actual reduction in ASCVD risk would depend on individual patient adherence to these strategies.
Fourth, our study dataset had a large amount of missing data that precluded calculation of the ASCVD risk score. In comparing the available baseline characteristics, the study population had generally more risk factors suggesting that the population missing complete data would have lower ASCVD risk scores. While this may somewhat lower the potential impact of interventions, among the patients missing data, those with 10-year ASCVD risk included in the MH Model would have had higher risk and with substantial opportunity for improvement. Lastly, and importantly, the study population, with 90% white patients, 79% with private insurance, and with 54% in the South, is not reflective of the United States as a whole. Therefore, the results from this modeling study may not be representative of the performance seen by all practices.
A final consideration is that our study does not evaluate whether the financial incentives in the Million Hearts model are sufficient to change practices’ behavior. For example, a practice that has only 100 patients at high ASCVD risk could earn a maximum of $12,000 if it achieves a >10% reduction in ASCVD risk. It is unknown whether the magnitude and likelihood of financial rewards are sufficient to convince practices to invest in interventions, such as community health workers,23 who might drive risk factor reductions. However, the average practice in our study had approximately 10 physicians and 483 eligible patients and, if that practice were able to achieve >10% reduction in ASCVD risk, it would potentially earn about $58,000 per year. Such an amount could be sufficient to hire a community health worker or develop other risk modification initiatives. While any investment made by a practice would be in advance of knowing or receiving bonus payments or without knowing the payments will come on a recurring basis, and it is unknown if practices would actually make these investments. However, if investment were made in these care improvements, they could potentially also drive better performance on quality measures in programs such as the Medicare Quality Payment Program and the Medicare Shared Savings Program. Our modeling study demonstrates that such improvements are possible; however, the overall Million Hearts model evaluation planned by CMS will answer whether these incentive-driven improvements are achievable in real-world practice.
Our study demonstrates that reducing blood pressure, cholesterol and smoking rates using results from randomized-controlled trials lowers ASCVD risk nearly 10%, with blood pressure lowering having the greatest single impact. Practices participating in the MH Model have a clear path to success in both improving their patients’ ASCVD risk and in the practice achieving financial rewards. While this study is simply a modeling exercise that demonstrates the feasibility and potential results of the program, these findings support the potential benefit of the Million Hearts model, provide guidance to practices seeking to lower ASCVD risk and validate the interim program results. The final MH Model evaluation will provide the definitive results regarding the success of the program and will clarify the road ahead both for practices seeking to improve their population’s health, and for Medicare as it innovates with approaches to reduce cardiovascular events.
Supplementary Material
What is Known
Individual cardiovascular risk factor reductions reduce cardiovascular events
Medicare is testing a payment model to incentivize reducing 10-years atherosclerotic cardiovascular disease (ASCVD) risk
What the Study Adds
Lowering hypertension, high cholesterol and smoking rates with results similar to clinical trials could substantially lower ASCVD risk
Healthcare practices achieving these reduction could receive incentive payments in the Medicare payment model
Acknowledgements
Kensey Gosch from Saint Luke’s Mid America Heart Institute contributed additional statistical analyses during the manuscript revision process.
Disclosures
Dr. Borden led the George Washington University Medical Faculty Associates participation in the Medicare Million Hearts Cardiovascular Disease Risk Reduction Model, randomized into the Control Group. Dr. Virani receives an honorarium from the American College of Cardiology (Associate Editor for Innovations, acc.org). Ms. Tang participated in this research while employed at the Saint Luke’s Mid America Heart Institute).
Sources of Funding
This research was supported by the American College of Cardiology Foundation’s National Cardiovascular Data Registry (NCDR). The views expressed in this article represent those of the authors and do not necessarily represent the official views of the NCDR or its associated professional societies identified at www.ncdr.com. Dr. Daugherty is supported by R01 HL133343 from the National Heart, Lung and Blood Institute and 15SFDRN24470027 from the American Heart Association. Dr. Virani is supported by research funding from the Department of Veterans Affairs, World Heart Federation, and Tahir and Jooma Family. Dr. Wasfy is supported by grants from the American Heart Association (18 CDA 34110215) and National Institutes of Health (R01 AG062282), has received consulting fees from Biotronik and Pfizer, and serves as the vice-chair of the New England Comparative Effectiveness Public Affairs Committee. Dr. Maddox receives grant funding via grant 1U24TR002306-01 from the NIH/NCATS, and consulting revenue from Creative Educational Concepts, Inc.
NON-STANDARD ABBREVIATIONS AND ACRONYMS:
- ACC/AHA
American College of Cardiology / American Heart Association
- ASCVD
atherosclerotic cardiovascular disease
- CMS
Centers for Medicare and Medicaid Services
- HDL
High-density lipoprotein
- HOPE-3
Heart Outcomes Prevention Evaluation
- LDL
Low-density lipoprotein
- MH Model
Million Hearts Cardiovascular Risk Reduction Model
- NCDR
National Cardiovascular Data Registry
- SPRINT
Systolic Blood Pressure Intervention Trial
Contributor Information
William B. Borden, George Washington University, Washington, DC
Jingyan Wang, University of Texas Health Science Center, Houston, TX.
Philip Jones, Saint Luke’s Mid America Heart Institute and University of Missouri-Kansas City School of Medicine, Kansas City, MO.
Yuanyuan Tang, Eli Lilly and Company, Indianapolis, IN.
Johanna Contreras, Mount Sinai, New York, NY.
Stacie L. Daugherty, University of Colorado School of Medicine, Aurora, CO
Nihar R. Desai, Yale University, New Haven, CT
Salim S. Virani, Michael E. DeBakey Veterans Affairs Medical Center & Baylor College of Medicine, Houston, TX
Jason H. Wasfy, Harvard University, Boston, MA
Thomas M. Maddox, Washington University School of Medicine, St. Louis, MO
REFERENCES
- 1.Ford ES, Ajani UA, Croft JB, et al. Explaining the Decrease in U.S. Deaths from Coronary Disease, 1980–2000. N Engl J Med 2007; 356;2388–2398. [DOI] [PubMed] [Google Scholar]
- 2.Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics 2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67–e492. DOI: 10.1161/CIR.0000000000000558 [DOI] [PubMed] [Google Scholar]
- 3.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013. ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. J Am Coll Cardiol. Jul 2014, 63 (25 Part B) 2889–2934; DOI: 10.1016/j.jacc.2013.11.002 [DOI] [PubMed] [Google Scholar]
- 4.Grundy SM, Stone NJ, Bailey AL, et al. 2018. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. J Am Coll Cardiol. Nov 2018, 25709; DOI: 10.1016/j.jacc.2018.11.003 [DOI] [Google Scholar]
- 5.Centers for Medicare and Medicaid Services. Million Hearts®: Cardiovascular Disease Risk Reduction Model. https://innovation.cms.gov/initiatives/Million-Hearts-CVDRRM. Accessed December 27, 2018.
- 6.Chan PS, Oetgen WJ, Buchanan D, et al. Cardiac Performance Measure Compliance in Outpatients. The American College of Cardiology and National Cardiovascular Data Registry’s PINNACLE (Practice Innovation And Clinical Excellence) Program. J Am Coll Cardiol 2010;56:8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan PS, Oetgen WJ, Spertus JA. The Improving Continuous Cardiac Care (IC3) Program and Outpatient Quality Improvement. Am J Med 2010;123:217–219. [DOI] [PubMed] [Google Scholar]
- 8.Messenger JC, Ho KK, Young CH, et al. The National Cardiovascular Data Registry (NCDR) Data Quality Brief: The NCDR Data Quality Program in 2012. J Am Coll Cardiol 2012;60:1484–1488. [DOI] [PubMed] [Google Scholar]
- 9.Masoudi FA, Ponirakis A, Yeh RW, et al. Cardiovascular Care Facts: a Report from the National Cardiovascular Data Registry: 2011. J Am Coll Cardiol 2013;62:1931–47. [DOI] [PubMed] [Google Scholar]
- 10.Goff DC, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014. Jun 24;129(25 Suppl 2):S49–73. doi: 10.1161/01.cir.0000437741.48606.98. Epub 2013 Nov 12. [DOI] [PubMed] [Google Scholar]
- 11.Lloyd-Jones DM, Huffman MD, Karmali KN, et al. Estimating Longitudinal Risks and Benefits From Cardiovascular Preventive Therapies Among Medicare Patients: The Million Hearts Longitudinal ASCVD Risk Assessment Tool: A Special Report From the American Heart Association and American College of Cardiology. J Am Coll Cardiol. 2017. Mar 28;69(12):1617–1636. doi: 10.1016/j.jacc.2016.10.018. Epub 2016 Nov 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American College of Cardiology ASCVD Risk Estimator Plus. https://tools.acc.org/ASCVD-Risk-Estimator-Plus/#!/calculate/estimate/. Accessed December 27, 2018.
- 13.Yusuf S, Lonn E, Pais P, et al. Blood-Pressure and Cholesterol Lowering in Persons without Cardiovascular Disease. N Engl J Med 2016; 374:2032–2043. DOI: 10.1056/NEJMoa1600177 [DOI] [PubMed] [Google Scholar]
- 14.The SPRINT Research Group. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med 2015; 373:2103–2116 DOI: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anthenelli RM, Benowitz NL, West R, et al. Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. Lancet. 2016. Jun 18;387(10037):2507–20. doi: 10.1016/S0140-6736(16)30272-0. Epub 2016 Apr 22. [DOI] [PubMed] [Google Scholar]
- 16.Borden WB, Maddox TM, Tang F, et al. Impact of the 2014 Expert Panel Recommendations for Management of High Blood Pressure on Contemporary Cardiovascular Practice: Insights From the NCDR PINNACLE Registry. J Am Coll Cardiol. 2014. Dec 2; 64(21):2196–203. [DOI] [PubMed] [Google Scholar]
- 17.Blue L, Peterson G, Keith Kranker, et al. Evaluation of the Million Hearts Cardiovascular Disease Risk Reduction Model: Third Annual Report. https://innovation.cms.gov/data-and-reports/2020/mhcvdrrm-thirdannevalrpt. Accessed January 26, 2021.
- 18.Million Hearts. https://millionhearts.hhs.gov/. Accessed December 27, 2018.
- 19.Million Hearts. Hypertension Control Change Package for Clinicians. https://millionhearts.hhs.gov/files/HTN_Change_Package.pdf. Accessed December 27, 2018.
- 20.Magid DJ, Ho PM, Olson KL, et al. A multimodal blood pressure control intervention in 3 healthcare systems. Am J Manag Care. 2011. Apr;17(4):e96–103. [PubMed] [Google Scholar]
- 21.Maddox TM, Borden WB, Tang F, et al. Implications of the 2013 ACC/AHA Cholesterol Guidelines for Adults in Contemporary Cardiovascular Practice: Insights From the NCDR PINNACLE Registry. J Am Coll Cardiol. 2014. Dec 2; 64(21):2183–92. [DOI] [PubMed] [Google Scholar]
- 22.Schroeder EB, Hanratty R, Beaty BL, et al. Simultaneous control of diabetes mellitus, hypertension, and hyperlipidemia in 2 health systems. Circ Cardiovasc Qual Outcomes. 2012. Sep 1;5(5):645–53. Epub 2012 Jul 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adair R, Wholey DR, Christianson J, et al. Improving Chronic Disease Care by Adding Laypersons to the Primary Care Team: A Parallel Randomized Trial. Ann. Intern. Med. 2013;159(3):176–184. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.