Abstract
Background
Patients with chronic hepatitis C virus (HCV) infection are at greater risk of developing metabolic disorders. Obesity is a major risk factor for these disorders, and therefore, managing body weight is crucial. Cannabis use, which is common in these patients, has been associated with lower corpulence in various populations. However, this relationship has not yet been studied in persons with chronic HCV infection.
Methods
Using baseline data from the French ANRS CO22 Hepather cohort, we used binary logistic and multinomial logistic regression models to test for an inverse relationship between cannabis use (former/current) and (i) central obesity (i.e., large waist circumference) and (ii) overweight and obesity (i.e., elevated body mass index (BMI)) in patients from the cohort who had chronic HCV infection. We also tested for relationships between cannabis use and both waist circumference and BMI as continuous variables, using linear regression models.
Results
Among the 6348 participants in the study population, 55% had central obesity, 13.7% had obesity according to their BMI, and 12.4% were current cannabis users. After multivariable adjustment, current cannabis use was associated with lower risk of central obesity (adjusted odds ratio, aOR [95% confidence interval, CI]: 0.45 [0.37–0.55]), BMI-based obesity (adjusted relative risk ratio (aRRR) [95% CI]: 0.27 [0.19–0.39]), and overweight (aRRR [95% CI]: 0.47 [0.38–0.59]). This was also true for former use, but to a lesser extent. Former and current cannabis use were inversely associated with waist circumference and BMI.
Conclusions
We found that former and, to a greater extent, current cannabis use were consistently associated with smaller waist circumference, lower BMI, and lower risks of overweight, obesity, and central obesity in patients with chronic HCV infection. Longitudinal studies are needed to confirm these relationships and to assess the effect of cannabis use on corpulence and liver outcomes after HCV cure.
Trial registration
ClinicalTrials.gov identifier: NCT01953458.
Keywords: Cannabis; Marijuana; Hepatitis C, Chronic; Obesity; Body weight; Fibrosis; Behaviors; Δ9-Tetrahydrocannabinol; Corpulence; Endocannabinoid system
Introduction
Patients with chronic hepatitis C virus (HCV) infection are at greater risk of metabolic disorders such as hyperlipidemia, hepatic steatosis, insulin resistance, metabolic syndrome, and diabetes mellitus (Chaudhari et al. 2021). Direct acting antivirals (DAA) can now cure HCV, leading to liver fibrosis regression, less liver necroinflammation, a lower risk of hepatic decompensation, amelioration of glycemic control, and lower liver-related and overall mortality (Kang et al. 2021; Roche et al. 2018; Huang et al. 2021; Cacciola et al. 2021). However, for patients with diabetes and/or cirrhosis, the benefits in terms of glycemic control and the lower risks of hepatocellular carcinoma (HCC) and mortality are not as strong (Cacciola et al. 2021; Váncsa et al. 2021; Benhammou et al. 2021). Moreover, obesity and hepatic steatosis are risk factors for HCC development after HCV cure (Minami et al. 2021; Ji et al. 2021).
Therefore, for patients with chronic HCV infection, managing metabolic disorders is crucial, both before and after HCV cure. In this population, elevated body weight and/or obesity are associated with hepatic steatosis (Younossi et al. 2004), insulin resistance (Delgado-Borrego et al. 2011), and type 2 diabetes mellitus (Wang et al. 2007). Accordingly, body weight management would appear to be a strong lever to prevent the development of metabolic disorders.
Studies in the general population have shown that cannabis use is inversely associated with body weight, body mass index (BMI), and the risk of both obesity and weight gain (Meier et al. 2019; Alshaarawy and Anthony 2019; Sidney 2016; Ngueta et al. 2015; Clark et al. 2018). However, apart from data on oral cannabinoid-containing medications against interferon and ribavirin-induced weight loss (Costiniuk et al. 2008), no data on the impact of real-life cannabis use on body weight in people with chronic HCV infection have been published. As HCV interacts with host lipid metabolism through several mechanisms (Serfaty 2017), and given that HCV infection is associated with higher levels of plasma endocannabinoids (Patsenker et al. 2015), the relationship between cannabis use and body weight may differ between patients with chronic HCV infection and the general population.
Using data from the French ANRS CO22 Hepather cohort, we aimed to identify clinical and socio-behavioral (including cannabis use) risk factors for obesity and overweight in people with chronic HCV-infection, a population where cannabis use prevalence is high (Barré et al. 2020).
Material and methods
Design and participants
ANRS CO22 Hepather is an ongoing French, national, multicenter, prospective cohort study of patients with chronic active or inactive HCV or HBV infection, which started in August 2012 (Pol et al. 2017). Eligible patients were invited to participate in the cohort during a medical visit in their hepatitis healthcare center. Thirty-two expert centers are involved throughout France. Sociodemographic, clinical, and biological data were collected at the enrolment visit. Patients are followed-up on a yearly basis, and supplemental data are collected during visits related to particular events (e.g., HCV or HBV therapy initiation). Written informed consent was obtained from each cohort participant before enrolment. The Hepather protocol was written in accordance with the Declaration of Helsinki and French law for biomedical research. It was approved by the “Comité de Protection des Personnes (CPP) Ile de France 3” Ethics Committee (Paris, France) and the French Regulatory Authority (ANSM).
Study population
The present study population comprised patients with chronic HCV infection (defined as positive HCV-RNA and anti-HCV antibodies) at cohort enrolment. HCV-cured patients were therefore not included. Cohort exclusion criteria were HIV co-infection, receiving HCV treatment, and having stopped HCV treatment for less than 3 months at enrolment. For the present study, we also excluded patients co-infected with hepatitis B, those with no data for cannabis use, and patients with unavailable data for either waist circumference or BMI.
Data collection
At the cohort enrolment visit, patients completed a face-to-face interview with their physician based on a structured questionnaire. Anthropological measurements and urine and blood samples were also taken.
The questionnaire collected clinical and sociodemographic data including sex, age, country of birth, educational level, average monthly household income, employment status (employed or not), time since HCV diagnosis, HCV treatment status, lifetime and current cannabis use, tobacco use, current and past alcohol consumption (number of standard drinks per day), and current coffee consumption (number of cups per day). Body height, weight, and waist circumference were measured. Data derived from blood samples included platelet count (109/L), and aspartate aminotransferase (AST, IU/L) and alanine aminotransferase (ALT, IU/L) levels.
Outcomes
There were two study outcomes, assessed according to waist circumference and BMI. The first was “central” obesity, defined as having a waist circumference ≥ 94 cm for men (except for men born in Asia, and Central or South America, for whom the cut-off was set at 90 cm) and ≥ 80 cm for women (Grundy et al. 2005). The second outcome was a three-category BMI-status variable. Participants with obesity (defined as a BMI ≥ 30 kg/m2), and those with overweight (defined as a BMI between 25 and 30 kg/m2), were compared with participants without obesity or overweight (World Health Organization 2019).
Explanatory variables
In terms of cannabis use, people who answered “yes” to the question concerning current use were classified in the “current use” category. Among people who answered “no,” those who reported “yes” to the subsequent lifetime cannabis use question were classified in the “former use” category. Finally, people who answered “no” to both questions (current/lifetime use) were classified into the “never” category. Similarly, tobacco use was divided into “current use,” “former use,” and “never.” Coffee consumption was defined as none (0 cups per day), moderate (1–2 cups per day), or elevated (≥ 3 cups per day). The 3 cups/day threshold was chosen based on previous results showing a potential protective effect of coffee consumption on liver stiffness and mortality in patients likely to develop liver disease (Carrieri et al. 2018; 2017a; Protopopescu et al. 2018). Alcohol consumption was classified into the following three categories based on the threshold for unhealthy alcohol use (defined as > 2 and > 3 standard drinks per day for women and men, respectively, in accordance with the French National Authority for Health (Haute Autorité de Santé (French National Authority for Health) 2014)): (i) abstinent with no history of unhealthy use, (ii) current moderate alcohol use (i.e., non-abstinent and non-unhealthy use), and (iii) unhealthy alcohol use (past or current).
As self-reported ethnicity was not collected in the cohort, countries of birth were aggregated into groups as a proxy. France was taken as the reference. The four other groups were “Europe + North America + Latin America + Australia,” “North Africa + Middle East,” “Sub-Saharan Africa + the Caribbean,” and “Asia.” Living in poverty was defined as a standard of living lower than the 2015 French poverty threshold (1 015€ per month) (Institut National de la Statistique et des Etudes Economiques 2021). Standard of living was calculated as the disposable income divided by the number of consumption units in the household. Educational level was dichotomized into having an upper secondary school certificate or not, and employment status as having a job or not.
Liver fibrosis was assessed using the FIB-4 index, a non-invasive marker of fibrosis calculated using age, AST level, ALT level, and platelet count with the following formula: age [years] * AST [IU/L])/(platelet count [109/L] * (ALT [IU/L])1/2. Advanced liver fibrosis was defined as an FIB-4 index >3.25 (Sterling et al. 2006; Vallet-Pichard et al. 2007). History of HCV treatment was classified into “never” (treatment naive), “interferon-based” (with or without ribavirin), “1st or 2nd generation DAA” (i.e., telaprevir, ribavirine, asunaprevir, daclatasvir, boceprevir, ledispavir, simeprevir, sofosbuvir, dasabuvir, ombitasvir, paritaprevir, ritonavir, mericitabine, velpatasvir, grazoprevir, elbasvir, paritaprevir, glecaprevir, and pibrentasvir), and “other” (e.g., ribavirin alone).
Statistical analyses
Study sample characteristics were compared according to (i) central obesity status and (ii) the three-category BMI status variable (participants with obesity, those with overweight, and those without obesity or overweight). Characteristics of excluded patients because of missing data on cannabis use, waist circumference, or BMI were compared with those of included patients. The Chi-squared and Student’s t tests were used in these comparisons for categorical and continuous variables, respectively.
Two separate analyses were performed to test the hypothesis that cannabis use is associated with lower corpulence. First, we estimated a binary logistic regression model with central obesity as the outcome. Second, we estimated a multinomial logistic regression model with the three-category BMI-status outcome (with “underweight or normal weight” as the reference). Associations were assessed by odds ratios (OR) for the logistic regression and by relative risk ratios (RRR) for the multinomial regression. Only variables with a liberal p-value < 0.20 in the univariable analyses were considered eligible for the multivariable models (Hosmer and Lemeshow 2000). Given the large number of explanatory variables and their potential multicollinearity, the final multivariable models were built using a backward stepwise selection procedure. This procedure removes one-by-one insignificant variables from the set of eligible variables based on the significance of their associations with the outcome. The likelihood ratio test (p< 0.05) was used to define the variables to keep in the final multivariable model. Subsequently, variables which were eligible for multivariable analyses but not retained in the final models (i.e., discarded during the backward stepwise procedure) were separately reintroduced in the latter to test for potential changes in terms of the level of significance of the associations and of changes in OR or RRR estimates, with a change-in-estimates threshold of 0.05 (Dunkler et al. 2014). Based on the same selection procedure and using linear regression models, we also tested whether cannabis use was associated with waist circumference and BMI as continuous variables.
To test for potential bias arising from the exclusion of participants with missing waist circumference measures, we performed a sensitivity analysis by including them in the analysis with the three-category BMI-status outcome, and compared the results with those of the main analysis.
All analyses were performed with Stata software version 16.1 for Windows (StataCorp LP, College Station, TX).
Results
Study population characteristics
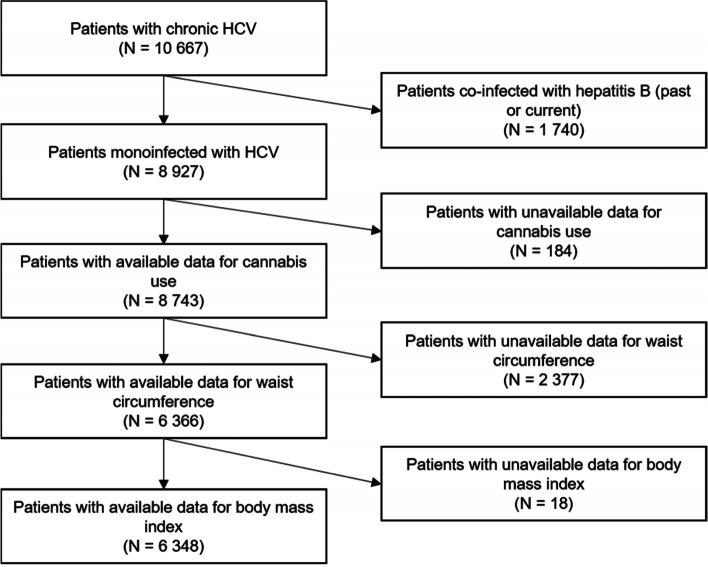
The study population comprised 6348 participants (Fig. 1) whose characteristics are presented in Table 1. They were mainly male (53.8%), with a median age of 56 years (interquartile range [50-64]). Fifty-five percent had central obesity and 13.7% were obese according to their BMI. Thirteen percent had obesity according to both definitions. Current cannabis users represented 12.4% of the study population.
Fig. 1.
Flow chart of the study population (ANRS CO22 Hepather cohort)
Table 1.
Study population characteristics according to obesity status (ANRS CO22 Hepather cohort, N = 6348)
| Variable (% of missing values) | Central obesitya | Underweight or normal weight | Overweight | Obesity | ||||
|---|---|---|---|---|---|---|---|---|
| Study population (N = 6348) | No (N = 2832) | Yes (N = 3516) | P-valueb | BMI < 25 kg/m2 (N = 3443) | 25 ≤ BMI < 30 kg/m2 (N = 2038) | BMI ≥ 30 kg/m2 (N = 867) | P-value | |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |||
| Sex | ||||||||
| Male | 3418 (53.8) | 1744 (61.6) | 1674 (47.6) | < 10−3 | 1708 (49.6) | 1288 (63.2) | 422 (48.7) | < 10−3 |
| Female | 2930 (46.2) | 1088 (38.4) | 1842 (52.4) | 1735 (50.4) | 750 (36.8) | 445 (51.3) | ||
| Age at baseline (years) | ||||||||
| Median [IQR] | 56 [50–64] | 53 [48–61] | 58 [51–66] | < 10−3 | 55 [49–63] | 57 [50–65] | 57 [50–65] | < 10−3 |
| Place of birth (0.1) | ||||||||
| France | 4673 (73.6) | 2188 (77.3) | 2485 (70.7) | < 10−3 | 2671 (77.6) | 1460 (71.7) | 542 (62.6) | < 10−3 |
| Europe + North America + Latin America + Australiac | 486 (7.7) | 221 (7.8) | 265 (7.5) | 246 (7.1) | 160 (7.9) | 80 (9.2) | ||
| North Africa + Middle East | 576 (9.1) | 212 (7.5) | 364 (10.4) | 259 (7.5) | 207 (10.2) | 110 (12.7) | ||
| Sub-Saharan Africa + the Caribbeand | 412 (6.5) | 117 (4.1) | 295 (8.4) | 153 (4.4) | 157 (7.7) | 102 (11.8) | ||
| Asia | 198 (3.1) | 93 (3.3) | 105 (3.0) | 113 (3.3) | 53 (2.6) | 32 (3.7) | ||
| Coffee consumption (0.7) | ||||||||
| 0 cups/day | 1795 (28.5) | 733 (26.1) | 1062 (30.4) | < 10−3 | 915 (26.8) | 594 (29.3) | 286 (33.3) | 0.002 |
| 1–2 cups/day | 2531 (40.2) | 1087 (38.7) | 1444 (41.4) | 1 391 (40.7) | 806 (39.8) | 334 (38.9) | ||
| ≥ 3 cups/day | 1977 (31.4) | 991 (35.3) | 986 (28.2) | 1112 (32.5) | 627 (30.9) | 238 (27.7) | ||
| Cannabis use | ||||||||
| Never | 4271 (67.3) | 1632 (57.6) | 2639 (75.1) | < 10−3 | 2131 (61.9) | 1446 (71.0) | 694 (80.0) | < 10−3 |
| Former | 1292 (20.4) | 680 (24.0) | 612 (17.4) | 753 (21.9) | 410 (20.1) | 129 (14.9) | ||
| Current | 785 (12.4) | 520 (18.4) | 265 (7.5) | 559 (16.2) | 182 (8.9) | 44 (5.1) | ||
| Tobacco smoking | ||||||||
| Never | 2390 (37.7) | 861 (30.4) | 1529 (43.5) | < 10−3 | 1200 (34.9) | 795 (39.0) | 395 (45.6) | < 10−3 |
| Former | 1747 (27.5) | 730 (25.8) | 1017 (28.9) | 866 (25.2) | 616 (30.2) | 265 (30.6) | ||
| Current | 2210 (34.8) | 1241 (43.8) | 969 (27.6) | 1377 (40.0) | 627 (30.8) | 206 (23.8) | ||
| Alcohol consumption (0.4) | ||||||||
| Abstinent without past unhealthy use | 2723 (43.1) | 1084 (38.4) | 1639 (46.8) | < 10−3 | 1401 (40.8) | 888 (43.8) | 434 (50.4) | < 10−3 |
| Moderate use | 2521 (39.9) | 1241 (44.0) | 1280 (36.6) | 1448 (42.2) | 786 (38.7) | 287 (33.3) | ||
| Unhealthy use (past or current) | 1077 (17.0) | 496 (17.6) | 581 (16.6) | 582 (17.0) | 355 (17.5) | 140 (16.3) | ||
| Living in poverty (2.6) | ||||||||
| No | 4303 (69.6) | 1974 (71.6) | 2329 (67.9) | 0.002 | 2411 (72.0) | 1372 (68.8) | 520 (61.7) | < 10−3 |
| Yes | 1883 (30.4) | 782 (28.4) | 1101 (32.1) | 939 (28.0) | 621 (31.2) | 323 (38.3) | ||
| Education level (1.1) | ||||||||
| < upper secondary school certificate | 3396 (54.1) | 1359 (48.5) | 2037 (58.6) | < 10−3 | 1710 (50.3) | 1148 (56.7) | 538 (63.0) | < 10−3 |
| ≥ upper secondary school certificate | 2883 (45.9) | 1443 (51.5) | 1440 (41.4) | 1692 (49.7) | 875 (43.3) | 316 (37.0) | ||
| Employed (0.4) | ||||||||
| No | 3518 (55.6) | 1308 (46.4) | 2210 (63.1) | < 10−3 | 1797 (52.4) | 1146 (56.4) | 575 (66.7) | < 10−3 |
| Yes | 2807 (44.4) | 1513 (53.6) | 1294 (36.9) | 1633 (47.6) | 887 (43.6) | 287 (33.3) | ||
| Advanced liver fibrosise (6.6) | ||||||||
| No | 4391 (74.0) | 2049 (78.4) | 2342 (70.6) | < 10−3 | 2429 (75.9) | 1387 (72.3) | 575 (70.8) | 0.001 |
| Yes | 1541 (26.0) | 566 (21.6) | 975 (29.4) | 772 (24.1) | 532 (27.7) | 237 (29.2) | ||
| Time since HCV diagnosis (years) (2.0) | ||||||||
| Median [IQR] | 14.0 [6.7–19.8] | 14.4 [6.8–19.9] | 13.7 [6.7–19.7] | 0.126 | 14.4 [7.2–20.0] | 13.8 [6.8–19.6] | 12.7 [6.0–19.1] | 0.002 |
| HCV treatment history | ||||||||
| Never | 3289 (51.8) | 1586 (56.0) | 1703 (48.4) | < 10−3 | 1938 (56.3) | 960 (47.1) | 391 (45.1) | < 10−3 |
| Interferon-based | 2278 (35.9) | 947 (33.4) | 1331 (37.9) | 1146 (33.3) | 794 (39.0) | 338 (39.0) | ||
| 1st or 2nd generation DAA | 616 (9.7) | 226 (8.0) | 390 (11.1) | 267 (7.8) | 231 (11.3) | 118 (13.6) | ||
| Other | 165 (2.6) | 73 (2.6) | 92 (2.6) | 92 (2.7) | 53 (2.6) | 20 (2.3) | ||
BMI body mass index, DAA direct-acting antiviral, HCV hepatitis C virus, IQR interquartile range
aCentral obesity was defined as having a waist circumference ≥ 94 cm for men (except for men born in Asia, Central or South America, for whom the cut-off was set at 90 cm) and ≥ 80 cm for women (World Health Organization 2019)
bThe chi-squared and Student’s t tests were used in these comparisons for categorical and continuous variables, respectively
c23 participants were born in Latin America, 15 in the USA, and 2 in Australia
d10 participants were born in the Caribbean
eAdvanced liver fibrosis was defined as an FIB-4 score >3.25 (Sterling et al. 2006)
Excluded cohort patients differed from those included in the present study in terms of sex, place of birth, cannabis use (15.8% of excluded participants were current users), alcohol consumption, living in poverty, employment status, and time since HCV diagnosis (data not shown).
Factors associated with central obesity
In the multivariable analysis, former (adjusted OR (aOR) [95% confidence interval (CI)]: 0.75 [0.64–0.88], p<0.001) and current (aOR [95% CI]: 0.45 [0.37–0.55], p<0.001) cannabis use were associated with a lower risk of central obesity (Table 2). Other protective factors included male sex, younger age, current tobacco use, having an upper secondary school certificate, and having a job. Conversely, risk factors included being born in “North Africa + Middle East” or in “Sub-Saharan Africa + the Caribbean,” unhealthy alcohol use (past or current), living in poverty, having advanced liver fibrosis, and previous HCV treatment with interferon or 1st or 2nd generation DAA (Table 2).
Table 2.
Factors associated with central obesity in univariable and multivariable analyses (logistic regression, ANRS CO22 Hepather cohort, N = 6348)
| Variables | Univariable analysis (N = 6348) | Multivariable analysis (N = 5742) | ||
|---|---|---|---|---|
| OR [95% CI] | P-value | aOR [95% CI] | P-value | |
| Sex | ||||
| Male (ref.) | 1 | 1 | ||
| Female | 1.76 [1.60–1.95] | < 10−3 | 1.49 [1.31–1.67] | < 10−3 |
| Age at baseline (years) | 1.04 [1.03–1.04] | < 10−3 | 1.02 [1.01–1.02] | < 10−3 |
| Place of birth | < 10−3 | < 10−3 | ||
| France (ref.) | 1 | 1 | ||
| Europe + North America + Latin America + Australia | 1.06 [0.88–1.27] | 0.571 | 1.03 [0.83–1.27] | 0.804 |
| North Africa + Middle East | 1.51 [1.26–1.81] | < 10−3 | 1.28 [1.04–1.57] | 0.022 |
| Sub-Saharan Africa + the Caribbean | 2.22 [1.78–2.77] | < 10−3 | 1.90 [1.48–2.44] | < 10−3 |
| Asia | 0.99 [0.75–1.32] | 0.967 | 1.02 [0.74–1.42] | 0.890 |
| Coffee consumption | < 10−3 | |||
| 0 cups/day (ref.) | 1 | |||
| 1–2 cups/day | 0.92 [0.81–1.04] | 0.166 | ||
| ≥ 3 cups/day | 0.69 [0.60–0.78] | < 10−3 | ||
| Cannabis use | < 10−3 | < 10−3 | ||
| Never (ref.) | 1 | 1 | ||
| Former | 0.56 [0.49–0.63] | < 10−3 | 0.75 [0.64–0.88] | < 10−3 |
| Current | 0.32 [0.27–0.37] | < 10−3 | 0.45 [0.37–0.55] | < 10−3 |
| Tobacco smoking | < 10−3 | 0.001 | ||
| Never (ref.) | 1 | 1 | ||
| Former | 0.78 [0.69–0.89] | < 10−3 | 1.08 [0.93–1.26] | 0.327 |
| Current | 0.44 [0.39–0.49] | < 10−3 | 0.81 [0.69–0.95] | 0.009 |
| Alcohol consumption | < 10−3 | 0.002 | ||
| Abstinent without past unhealthy use (ref.) | 1 | 1 | ||
| Moderate use | 0.68 [0.61–0.76] | < 10−3 | 1.04 [0.91–1.18] | 0.583 |
| Unhealthy use (past or current) | 0.77 [0.67–0.89] | < 10−3 | 1.35 [1.13–1.61] | 0.001 |
| Living in poverty | ||||
| No (ref.) | 1 | 1 | ||
| Yes | 1.19 [1.07–1.33] | 0.002 | 1.18 [1.03–1.35] | 0.019 |
| Education level | ||||
| < upper secondary school certificate (ref.) | 1 | 1 | ||
| ≥ upper secondary school certificate | 0.67 [0.60–0.74] | < 10−3 | 0.71 [0.63–0.80] | < 10−3 |
| Employment status | ||||
| No (ref.) | 1 | 1 | ||
| Yes | 0.51 [0.46–0.56] | < 10−3 | 0.78 [0.69–0.89] | < 10−3 |
| Advanced liver fibrosisa | ||||
| No (ref.) | 1 | 1 | ||
| Yes | 1.51 [1.34–1.70] | < 10−3 | 1.15 [1.00–1.31] | 0.044 |
| Time since HCV diagnosis (years) | 1.00 [0.99–1.00] | 0.250 | ||
| HCV treatment history | < 10−3 | 0.001 | ||
| None (ref) | 1 | 1 | ||
| Interferon-based | 1.31 [1.18–1.46] | < 10−3 | 1.15 [1.02–1.30] | 0.026 |
| 1st or 2nd generation DAA | 1.61 [1.35–1.92] | < 10−3 | 1.49 [1.23–1.82] | < 10−3 |
| Other | 1.17 [0.86–1.61] | 0.319 | 0.98 [0.68–1.42] | 0.931 |
aOR adjusted odds ratio, CI confidence interval, DAA direct-acting antivirals, OR odds ratio, ref. reference group, HCV hepatitis C virus
aAdvanced liver fibrosis was defined as an FIB-4 score >3.25 (Sterling et al. 2006)
Former and current cannabis use were also associated with a lower waist circumference after multivariable adjustment (linear regression coefficient (coef.) [95% CI]: −2.00 [−3.01; −1.00], p<0.001, and −5.43 [−6.66; −4.20], p<0.001, respectively) (data not shown).
Factors associated with overweight and obesity as measured by BMI
In the multivariable analysis, both former and current cannabis uses were associated with a lower risk of both overweight and obesity (Table 3). Specifically, current cannabis use was associated with a 53% and 73% lower risk of overweight and obesity, respectively (p<0.001), versus no lifetime cannabis use. Former cannabis use was associated with a 22% and 42% lower risk of overweight and obesity (p=0.003 and p<0.001, respectively), versus no lifetime use.
Table 3.
Factors associated with overweight and obesity in multivariable analyses (multinomial logistic regression, ANRS CO22 Hepather cohort, N = 6049)
| Variables | Overweight (25 ≤ BMI < 30 kg/m2) | Obesity (BMI ≥ 30 kg/m2) | ||
|---|---|---|---|---|
| aRRR [95% CI] | P-value | aRRR [95% CI] | P-value | |
| Sex | ||||
| Male (ref.) | 1 | 1 | ||
| Female | 0.46 [0.41–0.53] | < 10−3 | 0.86 [0.73–1.03] | 0.094 |
| Age at baseline (years) | 1.01 [1.00–1.02] | 0.002 | 0.99 [0.98–1.00] | 0.062 |
| Place of birth | < 10−3 | < 10−3 | ||
| France (ref.) | 1 | 1 | ||
| Europe + North America + Latin America + Australia | 1.10 [0.88–1.37] | 0.397 | 1.39 [1.04–1.84] | 0.024 |
| North Africa + Middle East | 1.20 [0.97–1.48] | 0.093 | 1.67 [1.28–2.18] | < 10−3 |
| Sub-Saharan Africa + the Caribbean | 1.75 [1.35–2.28] | < 10−3 | 2.61 [1.93–3.53] | < 10−3 |
| Asia | 0.76 [0.53–1.08] | 0.122 | 1.14 [0.74–1.75] | 0.550 |
| Cannabis use | < 10−3 | < 10−3 | ||
| Never (ref.) | 1 | 1 | ||
| Former | 0.78 [0.66–0.92] | 0.003 | 0.58 [0.46–0.74] | < 10−3 |
| Current | 0.47 [0.38–0.59] | < 10−3 | 0.27 [0.19–0.39] | < 10−3 |
| Tobacco smoking | 0.004 | < 10−3 | ||
| Never (ref.) | 1 | 1 | ||
| Former | 1.02 [0.87–1.20] | 0.773 | 1.38 [1.12–1.69] | 0.002 |
| Current | 0.79 [0.66–0.94] | 0.007 | 0.82 [0.65–1.03] | 0.093 |
| Living in poverty | ||||
| No (ref.) | 1 | 1 | ||
| Yes | 1.21 [1.05–1.40] | 0.008 | 1.34 [1.11–1.62] | 0.003 |
| Education level | ||||
| < upper secondary school certificate (ref.) | 1 | 1 | ||
| > upper secondary school certificate | 0.81 [0.72–0.92] | 0.001 | 0.61 [0.52–0.73] | < 10−3 |
| Employment status | ||||
| No (ref.) | 1 | 1 | ||
| Yes | 1.02 [0.89–1.17] | 0.769 | 0.69 [0.57–0.83] | < 10−3 |
| Time since HCV diagnosis (years) | 0.99 [0.98–1.00] | 0.033 | 0.99 [0.98–1.00] | 0.052 |
| HCV treatment history | < 10−3 | < 10−3 | ||
| None (ref.) | 1 | 1 | ||
| Interferon-based | 1.33 [1.16–1.51] | < 10−3 | 1.46 [1.22–1.74] | < 10−3 |
| 1st or 2nd generation DAA | 1.60 [1.30–1.96] | < 10−3 | 2.13 [1.64–2.76] | < 10−3 |
| Other | 1.20 [0.83–1.72] | 0.338 | 1.02 [0.60–1.73] | 0.948 |
aRRR adjusted relative risk ratio, BMI body mass index, CI confidence interval, DAA direct-acting antivirals, ref. reference group, HCV hepatitis C virus
Former and current cannabis use were also associated with a lower BMI level after multivariable adjustment (coef. [95% CI]: −0.77 [−1.07; −0.47], p<0.001, and −1.88, [−2.25; −1.51], p<0.001, respectively) (data not shown).
The following variables were associated with both definitions of obesity in multivariable analyses (Tables 2 and 3): cannabis use, living in poverty, education level, employment status, being born in “North Africa and Middle East” or “Sub-Saharan Africa,” and history of HCV treatment.
None of the reintroductions of excluded explanatory variables in the final models had a relevant impact on the model estimates. Sensitivity analyses, performed on the population that included participants with no data on waist circumference, led to similar results to those found in the main analysis in terms of significance level and adjusted RRR magnitude (data not shown).
Discussion
Using cross-sectional data from 6348 chronically infected HCV patients, we found that current cannabis use was associated with a 55% lower likelihood of central obesity (elevated waist circumference), a 73% lower likelihood of obesity (BMI ≥ 30 kg/m2), and a 53% lower likelihood of overweight (BMI between 25 and 30 kg/m2), when compared with no lifetime cannabis use. To our knowledge, this is the first time that such associations have been highlighted for HCV-infected patients.
Our results are in line with those found in general populations in different countries (Meier et al. 2019; Alshaarawy and Anthony 2019; Sidney 2016; Ngueta et al. 2015; Clark et al. 2018). For instance, Ngueta et al., among Inuit adults, found an OR of 0.56 for obesity (BMI ≥ 30 kg/m2) for past-year cannabis use as compared to non-users (Ngueta et al. 2015). They also found a similar association between frequent cannabis use (but not former nor infrequent use) and concurrent elevated triglycerides and waist circumference (Ngueta 2020). However, causal association was not found in a recent Mendelian randomization study (Alayash et al. 2021). Our results are also in line with what we found in a previous study for patients with chronic hepatitis B virus from the same cohort (Barré et al. 2021a).
One possible explanation for the relationship between cannabis use and corpulence is that such frequent use may downregulate cannabinoid receptor 1 (CB1)—which regulates appetite and body weight, thereby reducing energy storage and increasing metabolic rates (Clark et al. 2018; Spindle et al. 2021). In two preclinical studies, CB1 antagonists and peripherally restricted CB1 antagonists (i.e., with no effect on the central nervous system) showed some efficacy on obesity and metabolic syndrome (O’Sullivan et al. 2021; Lopez Trinidad et al. 2021).
However, assuming that the effects of cannabis are solely attributable to the most abundant phytocannabinoid Δ9-tetrahydrocannabinol (THC) (Cluny et al. 2015) and/or are only mediated through CB1 may be reductive. Cannabis exposes users to a large number of phytocannabinoids, as well as to non-cannabinoid molecules, such as terpenoids (Russo 2018). The most abundant phytocannabinoids in cannabis are THC, cannabidiol (CBD), and Δ9-tetrahydrocannabivarin (THCV). Beside their varying affinity for CB1 and CB2, these cannabinoids also interact with other targets such as transient receptor potential channels, GPR55 receptor, or peroxisome proliferator activated receptors, which in turn may impact energy metabolism (Bielawiec et al. 2020; Abioye et al. 2020). Moreover, cannabis compounds may have anti-oxidant and anti-inflammatory properties (Atalay et al. 2019; Bielawiec et al. 2021; Henshaw et al. 2021; Graczyk et al. 2021), inflammation being a major element in chronic diseases, especially metabolic and obesity-related disorders (Cavalheiro et al. 2022; Ellulu et al. 2017). Non-cannabinoid cannabis compounds such as limonene, β-caryophyllene, and other terpenes may also play a role in the corpulence lowering effect of cannabis use (Hashiesh et al. 2021; Jing et al. 2013; Scandiffio et al. 2020). Finally, a synergetic effect, resulting from the interactions between those compounds, cannot be excluded (Russo 2018).
By lowering body weight, cannabis use may have an indirect beneficial effect on liver disease and metabolic disorders in patients with chronic HCV infection. Cannabis and/or cannabis compounds may also have a direct beneficial effect on these problems. More specifically, a growing body of research, including observational, preclinical, and clinical data, suggests that phytocannabinoids may play a role in the prevention or treatment of hepatic steatosis (Berk et al. 2021; Barré et al. 2021b). As modulators of the endocannabinoid system, which is a main therapeutic target for treating diabetes mellitus (Veilleux et al. 2019), cannabis compounds may exert a beneficial role on the development of diabetes in different populations (Bielawiec et al. 2020; Wargent et al. 2013; Jadoon et al. 2016; Meah et al. 2021), including HCV-infected people (Barré et al. 2020). Observational studies have also highlighted a potential role of cannabis compounds in liver disease prevention in this population (Adejumo et al. 2018; Santos et al. 2020).
We adjusted our analyses for tobacco use, which is common in European cannabis users (Hindocha et al. 2016) and is associated with lower body weight (Audrain-McGovern and Benowitz 2011). Accordingly, the effect of cannabis use we found cannot be imputed to tobacco use.
The other factors associated with both definitions of obesity in our study were socioeconomic status, African origin, and history of HCV treatment. The inverse relationship between socioeconomic status and elevated body weight/obesity is multifactorial and has been widely documented (Newton et al. 2017; Vieira et al. 2019; Wang and Beydoun 2007; Pigeyre et al. 2016; Hruby et al. 2016). A higher BMI and/or risk of obesity in African-Americans, as well as immigrants from Africa in Europe, has also been reported (Shai et al. 2006; Agyemang et al. 2016; Toselli et al. 2014; Min et al. 2021; Abraham et al. 2013). This is a complex phenomenon and involves socio-cultural, economic, and genetic factors.
We found that a history of HCV treatment (interferon-based and 1st/2nd generation DAA) was associated with a higher risk of obesity. This may seem counter-intuitive given the documented weight loss-inducing effect of interferon (Alam et al. 2013). Elsewhere, elevated BMI/obesity was an independent risk factor for nonresponse to previous antiviral treatment (Bressler et al. 2003; Asselah et al. 2010). Therefore, as HCV-cured patients were not included in our analyses, participants with a history of HCV treatment were more likely to have risk factors for nonresponses (i.e., obesity) than those with no such history.
The main strength of the present study is its large sample size. The inclusion of socio-behavioral factors is another strength, as it is widely recognized that these factors greatly impact body weight. The assessment of corpulence through two distinct markers (waist circumference and BMI) and the consistency of our results across the different models suggest they are robust. It has previously been highlighted that a measure of waist circumference provides both independent and complementary information to the BMI value when predicting morbidity and mortality. This is likely to be at least partly due to its ability to identify adults with increased visceral adipose tissue mass (Ross et al. 2020).
Some study limitations need to be acknowledged. First, cannabis use was self-declared, and we therefore cannot exclude potential desirability bias, which was however equally likely in people with and without obesity. Second, data on frequency of cannabis use were not collected, preventing the possibility of conducting dose-response analyses. Similarly, cannabinoid content of cannabis products was unknown. However, most recent data indicated that THC levels are increasing in both herb and resin in France and other European countries, reaching around 11 and 18% THC in France, respectively (Freeman et al. 2021; Gandilhon et al. 2019). Third, data for some of the most important determinants of elevated body weight (i.e., dietary intakes and physical activity) were not available. However, we can assume that socioeconomic variables captured part of these effects.
Conclusions
To conclude, we found that both former and, to a greater extent, current cannabis use were consistently associated with lower waist circumference, lower BMI values, and lower risks of overweight, obesity, and central obesity in patients with chronic HCV infection. Longitudinal studies are needed to confirm those relationships and assess the effect of cannabis use on corpulence and on liver outcomes after HCV cure.
Acknowledgements
We would like to thank the participating patients and clinicians at each site. We also thank INSERM-ANRS MIE for sponsoring, funding and conducting the ANRS CO22 Hepather cohort in collaboration with the French Association for the Study of the Liver (Association Française pour l’Etude du Foie: AFEF). Finally, our thanks to Jude Sweeney (Milan, Italy) for the English revision and copyediting of our manuscript.
ANRS/AFEF Hepather study group
Investigators:
Laurent Alric, Delphine Bonnet, Virginie Payssan-Sicart, Chloe Pomes (CHU Purpan, Toulouse, France), Fabien Zoulim, Marianne Maynard, Roxane Bai, Lucie Hucault, François Bailly (Hospices Civils de Lyon, Lyon, France), François Raffi, Eric Billaud, David Boutoille, Maeva Lefebvre, Elisabeth André-Garnier (Hôpital Hôtel-Dieu, Nantes, France), Paul Cales, Isabelle Hubert, Adrien Lannes, Françoise Lunel, Jérôme Boursier (CHU Angers, Angers, France), Tarik Asselah, Nathalie Boyer, Nathalie Giuily, Corinne Castelnau, Giovanna Scoazec (Hôpital Beaujon, Clichy, France), Stanislas Pol, Hélène Fontaine, Emilie Rousseaud, Anaïs Vallet-Pichard, Philippe Sogni (Hôpital Cochin, Paris, France), Victor de Ledinghen, Juliette Foucher, Jean-Baptiste Hiriart, Jancell M’Bouyou, Marie Irlès-Depé (Hôpital Haut-Lévêque, Pessac, Bordeaux, France), Marc Bourlière, Si Nafa Si Ahmed, Valérie Oules (Hôpital Saint Joseph, Marseille, France), Albert Tran, Rodolphe Anty, Eve Gelsi, Régine Truchi (CHU de Nice, Nice, France), Dominique Thabut, Saloua Hammeche, Joseph Moussali (Hôpital de la Pitié Salptétrière, Paris, France), Xavier Causse, Barbara De Dieuleveult, Brahim Ouarani, Damien Labarrière (CHR La Source, Orléans, France), Nathalie Ganne, Véronique Grando-Lemaire, Pierre Nahon, Séverine Brulé, Betul ULKER (Hôpital Jean Verdier, Bondy, France), Dominique Guyader, Caroline Jezequel, Audrey Brener, Anne Laligant, Aline Rabot, Isabelle Renard (CHU Rennes, Rennes, France), François Habersetzer, Thomas F. Baumert, Michel Doffoel, Catherine Mutter, Pauline Simo-Noumbissie, Esma Razi (Hôpitaux Universitaires de Strasbourg, Strasbourg, France), Jean-Pierre Bronowicki, Hélène Barraud, Mouni Bensenane, Abdelbasset Nani, Sarah Hassani-Nani, Marie-Albertine Bernard (CHU de Nancy, Nancy, France), Georges-Philippe Pageaux, Dominique Larrey, Magda Meszaros (Hôpital Saint Eloi, Montpellier, France), Sophie Metivier, Christophe Bureau, Thibault Morales, Jean Marie Peron, Marie Angèle Robic (CHU Purpan, Toulouse, France), Thomas Decaens, Marine Faure, Bruno Froissart, Marie-Noelle Hilleret, Jean-Pierre Zarski (CHU de Grenoble, Grenoble, France), Ghassan Riachi, Odile Goria, Fatima Paris, Hélène Montialoux (CHU Charles Nicolle, Rouen, France), Vincent Leroy, Giuliana Amaddeo, Anne Varaut, Mélanie Simoes, Rachida Amzal (Hôpital Henri Mondor, Créteil, France), Olivier Chazouillières, Tony Andreani, Bénédicte Angoulevant, Azeline Chevance, Lawrence Serfaty (Hôpital Saint-Antoine, Paris, France), Didier Samuel, Teresa Antonini, Audrey Coilly, Jean-Charles Duclos Vallée, Mariagrazia Tateo (Hôpital Paul Brousse, Villejuif, France), Armand Abergel, Maud Reymond, Chanteranne Brigitte, Buchard Benjamin, Léon Muti (Hôpital Estaing, Clermont-Ferrand, France), Claire Geist, Guillaume Conroy, Raphaëlle Riffault (Centre Hospitalier Régional, Metz, France), Isabelle Rosa, Camille Barrault, Laurent Costes, Hervé Hagège (Centre Hospitalier Intercommunal, Créteil, France), Véronique Loustaud-Ratti, Paul Carrier, Maryline Debette-Gratien, (CHU Limoges, Limoges, France), Philippe Mathurin, Guillaume Lassailly, Elise Lemaitre, Valérie Canva, Sébastien Dharancy, Alexandre Louvet (CHRU Claude Huriez, Lille, France), Anne Minello, Marianne Latournerie, Marc Bardou, Thomas Mouillot (Dijon University Hospital, Dijon, France), Louis D’Alteroche, Didier Barbereau, Charlotte Nicolas, Laure Elkrief, Anaïs Jaillais (CHU Trousseau, 37044 Tours, France), Jérôme Gournay, Caroline Chevalier, Isabelle Archambeaud, Sarah Habes (CHU de Nantes, Nantes, France), Isabelle Portal (CHU Timone, Marseille, France), Moana Gelu-Simeon, Eric Saillard, Marie-Josée Lafrance, Lucie Catherine (CHU de Pointe-à-Pitre, Pointe-à-Pitre, Guadeloupe).
Methodology and Coordinating Center:
Fabrice Carrat (coordinator), Frederic Chau, Céline Dorival, Isabelle Goderel, Clovis Lusivika-Nzinga, Marc-Antoine Bellance, Jonathan Bellet, Priscilla Monfalet, Jessica Chane-Teng, Sephora Bijaoui, Grégory Pannetier, François Téoulé, Jérôme Nicol, Florian Sebal, Rafika Bekhti (Sorbonne University & INSERM U1136 - IPLESP, Paris, France).
Sponsor:
Carole Cagnot, Anaïs Boston, Laura Nailler, Guillaume Le Meut (INSERM-ANRS-MIE, Paris, France), Alpha Diallo (Pharmacovigilance coordinator), Ventzislava Petrov-Sanchez (coordinator).
Scientific Committee
- Voting members:
Marc Bourlière (Hôpital St Joseph, Marseille), Jérôme Boursier (CHU Angers, Angers, France), Fabrice Carrat (Scientific Coordinator, Hôpital Saint-Antoine, Paris, France), Patrizia Carrieri (INSERM U912, Marseille, France), Elisabeth Delarocque-Astagneau (Inserm UMR1181, Paris), Victor De Ledinghen (Hôpital Haut-Lévêque, Pessac, Bordeaux, France), Céline Dorival (UPMC & INSERM U1136, Paris, France), Hélène Fontaine (Hôpital Cochin, Paris, France), Slim Fourati (Hôpital Henri Mondor, Créteil, France), Chantal Housset (Inserm UMR-S938 1 IFR65, Paris), Dominique Larrey (Hôpital Saint Eloi, Montpellier, France), Pierre Nahon (Hôpital Jean Verdier, Bondy, France), Georges-Philippe Pageaux (Hôpital Saint Eloi, Montpellier, France), Ventzislava Petrov-Sanchez (ANRS, Paris, France), Stanislas Pol (Principal Investigator, Hôpital Cochin, Paris, France), Mathias Bruyand (Agence Nationale de Santé Publique, Saint Maurice, France), Linda Wittkop (ISPED-INSERM U897, Bordeaux, France), Fabien Zoulim (Hospices Civils de Lyon, Lyon, France), Jessica Zucman-Rossi (Inserm U674/1162, Paris).
- Non-voting members:
Marianne L’hennaff (ARCAT-TRT-5-CHV, France), Michèle Sizorn (SOS hépatites, France); one representative of INSERM-ANRS-MIE Pharmacovigilance team, Paris, France (Anaïs Boston, Alpha Diallo), Carole Cagnot (INSERM-ANRS-MIE, Paris, France), one member of Inserm Transfert, Paris, France (Alice Bousselet, Mireille Caralp), and one representative of each pharmaceutical company (MSD, Gilead, Abbvie).
Abbreviations
- ALT
Alanine aminotransferase
- aOR
Adjusted odds ratio
- aRRR
Adjusted relative risk ratio
- AST
Aspartate aminotransferase
- BMI
Body mass index
- CB1
Cannabinoid receptor 1
- CBD
Cannabidiol
- DAA
Direct-acting antiviral
- HCV
Hepatitis C virus
- HBV
Hepatitis B virus
- IQR
Interquartile range
- THC
Δ9-Tetrahydrocannabinol
- THCV
Δ9-Tetrahydrocannabivarin
Authors’ contributions
TB, CP, PC, and FM: conceptualization, methodology, and validation. VDB: data curation. CR: formal analysis. SP, FC, HF, DL, EDA, PM, and CD: conceptualization, investigation. SP, FC, HF, CD, and VPS: project administration and funding acquisition. TB: writing—original draft preparation. All authors: writing—review and editing. All authors approved the final version of the article, including the authorship list.
Funding
The Hepather cohort is funded by INSERM-ANRS MIE (France REcherche Nord&sud Sida-vih Hepatites | Maladies Infectieuses Emergentes), ANR Equipex and Cohort (Agence Nationale de la Recherche), DGS (Direction Générale de la Santé) and MSD, Janssen, Gilead, Abbvie, BMS, and Roche. These funding sources had no role in the writing of the manuscript or the decision to submit it for publication.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to ongoing data treatment; however, they are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Written informed consent was obtained from each cohort participant before enrolment in Hepather. The cohort protocol was designed in accordance with the Declaration of Helsinki and French law for biomedical research. It was approved by the “Comité de Protection des Personnes (CPP) Ile de France 3” Ethics Committee (Paris, France) and the French Regulatory Authority (ANSM).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Patrizia Carrieri, Email: pmcarrieri@aol.com.
the ANRS/AFEF Hepather study group:
Laurent Alric, Chloe Pomes, Fabien Zoulim, Marianne Maynard, Roxane Bai, Lucie Hucault, François Bailly, François Raffi, Eric Billaud, David Boutoille, Maeva Lefebvre, Elisabeth André-Garnier, Paul Cales, Isabelle Hubert, Adrien Lannes, Françoise Lunel, Jérôme Boursier, Tarik Asselah, Nathalie Boyer, Nathalie Giuily, Corinne Castelnau, Giovanna Scoazec, Stanislas Pol, Hélène Fontaine, Emilie Rousseaud, Anaïs Vallet-Pichard, Philippe Sogni, Victor de Ledinghen, Juliette Foucher, Jean-Baptiste Hiriart, Jancell M’Bouyou, Marie Irlès-Depé, Marc Bourlière, Si Nafa Si Ahmed, Valérie Oules, Albert Tran, Rodolphe Anty, Eve Gelsi, Régine Truchi, Dominique Thabut, Saloua Hammeche, Joseph Moussali, Xavier Causse, Barbara De Dieuleveult, Brahim Ouarani, Damien Labarrière, Nathalie Ganne, Véronique Grando-Lemaire, Pierre Nahon, Séverine Brulé, Betul Ulker, Dominique Guyader, Caroline Jezequel, Audrey Brener, Anne Laligant, Aline Rabot, Isabelle Renard, François Habersetzer, Thomas F. Baumert, Michel Doffoel, Catherine Mutter, Pauline Simo-Noumbissie, Esma Razi, Jean-Pierre Bronowicki, Hélène Barraud, Mouni Bensenane, Abdelbasset Nani, Sarah Hassani-Nani, Marie-Albertine Bernard, Georges-Philippe Pageaux, Dominique Larrey, Magda Meszaros, Sophie Metivier, Christophe Bureau, Thibault Morales, Jean Marie Peron, Marie Angèle Robic, Thomas Decaens, Marine Faure, Bruno Froissart, Marie-Noelle Hilleret, Jean-Pierre Zarski, Ghassan Riachi, Odile Goria, Fatima Paris, Hélène Montialoux, Vincent Leroy, Giuliana Amaddeo, Anne Varaut, Mélanie Simoes, Rachida Amzal, Olivier Chazouillières, Tony Andreani, Bénédicte Angoulevant, Azeline Chevance, Lawrence Serfaty, Didier Samuel, Teresa Antonini, Audrey Coilly, Jean-Charles Duclos-Vallée, Mariagrazia Tateo, Armand Abergel, Maud Reymond, Chanteranne Brigitte, Buchard Benjamin, Léon Muti, Claire Geist, Guillaume Conroy, Raphaëlle Riffault, Isabelle Rosa, Camille Barrault, Laurent Costes, Hervé Hagège, Véronique Loustaud-Ratti, Paul Carrier, Maryline Debette-Gratien, Philippe Mathurin, Guillaume Lassailly, Elise Lemaitre, Valérie Canva, Sébastien Dharancy, Alexandre Louvet, Anne Minello, Marianne Latournerie, Marc Bardou, Thomas Mouillot, Louis D’Alteroche, Didier Barbereau, Charlotte Nicolas, Laure Elkrief, Anaïs Jaillais, Jérôme Gournay, Caroline Chevalier, Isabelle Archambeaud, Sarah Habes, Isabelle Portal, Moana Gelu-Simeon, Eric Saillard, Marie-Josée Lafrance, Lucie Catherine, Fabrice Carrat, Frederic Chau, Céline Dorival, Isabelle Goderel, Clovis Lusivika-Nzinga, Marc-Antoine Bellance, Jonathan Bellet, Priscilla Monfalet, Jessica Chane-Teng, Sephora Bijaoui, Grégory Pannetier, François Téoulé, Jérôme Nicol, Florian Sebal, Rafika Bekhti, Carole Cagnot, Anaïs Boston, Laura Nailler, Guillaume Le Meut, Alpha Diallo, Ventzislava Petrov-Sanchez, Marc Bourlière, Jérôme Boursier, Fabrice Carrat, Patrizia Carrieri, Elisabeth Delarocque-Astagneau, Victor De Ledinghen, Céline Dorival, Hélène Fontaine, Slim Fourati, Chantal Housset, Dominique Larrey, Pierre Nahon, Georges-Philippe Pageaux, Ventzislava Petrov-Sanchez, Stanislas Pol, Mathias Bruyand, Linda Wittkop, Fabien Zoulim, Jessica Zucman-Rossi, Marianne L’hennaff, Michèle Sizorn, and Carole Cagnot
References
- Abioye A, Ayodele O, Marinkovic A, Patidar R, Akinwekomi A, Sanyaolu A. Δ9-Tetrahydrocannabivarin (THCV): a commentary on potential therapeutic benefit for the management of obesity and diabetes. J Cannabis Res. 2020;2(1):6. doi: 10.1186/s42238-020-0016-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraham PA, Kazman JB, Zeno SA, Deuster PA. Obesity and African Americans: physiologic and behavioral pathways. ISRN Obes. 2013;2013:314295. doi: 10.1155/2013/314295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adejumo AC, Adegbala OM, Adejumo KL, Bukong TN. Reduced incidence and better liver disease outcomes among chronic HCV infected patients who consume cannabis. Can J Gastroenterol Hepatol. 2018;2018:9430953. doi: 10.1155/2018/9430953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agyemang C, Meeks K, Beune E, Owusu-Dabo E, Mockenhaupt FP, Addo J, et al. Obesity and type 2 diabetes in sub-Saharan Africans - is the burden in today’s Africa similar to African migrants in Europe? The RODAM study. BMC Med. 2016;14(1):166. doi: 10.1186/s12916-016-0709-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alam I, Ullah N, Alam I, Ali I. The effects and underlying mechanism of interferon therapy on body weight and body composition. Pak J Pharm Sci. 2013;26(6):1251–1257. [PubMed] [Google Scholar]
- Alayash Z, Nolde M, Meisinger C, Baurecht H, Baumeister SE. Cannabis use and obesity-traits: a Mendelian randomization study. Drug Alcohol Depend. 2021;226:108863. doi: 10.1016/j.drugalcdep.2021.108863. [DOI] [PubMed] [Google Scholar]
- Alshaarawy O, Anthony JC. Are cannabis users less likely to gain weight? Results from a national 3-year prospective study. Int J Epidemiol. 2019;48(5):1695–1700. doi: 10.1093/ije/dyz044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asselah T, Estrabaud E, Bieche I, Lapalus M, De Muynck S, Vidaud M, et al. Hepatitis C: viral and host factors associated with non-response to pegylated interferon plus ribavirin. Liver Int. 2010;30(9):1259–1269. doi: 10.1111/j.1478-3231.2010.02283.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atalay S, Jarocka-Karpowicz I, Skrzydlewska E. Antioxidative and anti-inflammatory properties of cannabidiol. Antioxidants (Basel). 2019;9(1) [cited 2021 Feb 2]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7023045/. [DOI] [PMC free article] [PubMed]
- Audrain-McGovern J, Benowitz NL. Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther. 2011;90(1):164–168. doi: 10.1038/clpt.2011.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barré T, Nishimwe ML, Protopopescu C, Marcellin F, Carrat F, Dorival C, et al. Cannabis use is associated with a lower risk of diabetes in chronic hepatitis C-infected patients (ANRS CO22 Hepather cohort) J Viral Hepat. 2020;27(12):1473–1483. doi: 10.1111/jvh.13380. [DOI] [PubMed] [Google Scholar]
- Barré T, Pol S, Ramier C, Di Beo V, Carrat F, Bureau M, et al. Cannabis use is inversely associated with overweight and obesity in hepatitis B virus-infected patients (ANRS CO22 Hepather Cohort). Cannabis Cannabinoid Res. 2021a. 10.1089/can.2021.0094. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- Barré T, Rojas Rojas T, Lacombe K, Protopopescu C, Poizot-Martin I, Nishimwe M, et al. Cannabis use and reduced risk of elevated fatty liver index in HIV-HCV co-infected patients: a longitudinal analysis (ANRS CO13 HEPAVIH) Expert Rev Anti Infect Ther. 2021;19(9):1147–1156. doi: 10.1080/14787210.2021.1884545. [DOI] [PubMed] [Google Scholar]
- Benhammou JN, Moon AM, Pisegna JR, Su F, Vutien P, Moylan CA, et al. Nonalcoholic fatty liver disease risk factors affect liver-related outcomes after direct-acting antiviral treatment for hepatitis C. Dig Dis Sci. 2021;66(7):2394–2406. doi: 10.1007/s10620-020-06457-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berk K, Bzdega W, Konstantynowicz-Nowicka K, Charytoniuk T, Zywno H, Chabowski A. Phytocannabinoids-a green approach toward non-alcoholic fatty liver disease treatment. J Clin Med. 2021;10(3):393. doi: 10.3390/jcm10030393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bielawiec P, Harasim-Symbor E, Chabowski A. Phytocannabinoids: useful drugs for the treatment of obesity? Special focus on cannabidiol. Front Endocrinol (Lausanne) 2020;11:114. doi: 10.3389/fendo.2020.00114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bielawiec P, Harasim-Symbor E, Sztolsztener K, Konstantynowicz-Nowicka K, Chabowski A. Attenuation of oxidative stress and inflammatory response by chronic cannabidiol administration is associated with improved n-6/n-3 PUFA ratio in the white and red skeletal muscle in a rat model of high-fat diet-induced obesity. Nutrients. 2021;13(5):1603. doi: 10.3390/nu13051603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bressler BL, Guindi M, Tomlinson G, Heathcote J. High body mass index is an independent risk factor for nonresponse to antiviral treatment in chronic hepatitis C. Hepatology. 2003;38(3):639–644. doi: 10.1053/jhep.2003.50350. [DOI] [PubMed] [Google Scholar]
- Cacciola I, Russo G, Filomia R, Pitrone C, Caccamo G, Giandalia A, et al. Over time evaluation of glycaemic control in direct-acting-antiviral treated HCV/diabetic individuals with chronic hepatitis or with cirrhosis. Liver Int. 2021;41(9):2059–2067. doi: 10.1111/liv.14905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrieri MP, Protopopescu C, Marcellin F, Rosellini S, Wittkop L, Esterle L, et al. Protective effect of coffee consumption on all-cause mortality of French HIV-HCV co-infected patients. J Hepatol. 2017;67(6):1157–1167. doi: 10.1016/j.jhep.2017.08.005. [DOI] [PubMed] [Google Scholar]
- Carrieri MP, Protopopescu C, Marcellin F, Wittkop L, Lacombe K, Esterle L, et al. The impact of coffee consumption on fibrosis and steatosis in HIV-HCV co-infected patients. J Hepatol. 2018;68(4):845–847. doi: 10.1016/j.jhep.2017.10.025. [DOI] [PubMed] [Google Scholar]
- Cavalheiro EKFF, Costa AB, Salla DH, da Silva MR, Mendes TF, da Silva LE, et al. Cannabis sativa as a treatment for obesity: from anti-inflammatory indirect support to a promising metabolic re-establishment target. Cannabis Cannabinoid Res. 2022;7(2):135–151. doi: 10.1089/can.2021.0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhari R, Fouda S, Sainu A, Pappachan JM. Metabolic complications of hepatitis C virus infection. World J Gastroenterol. 2021;27(13):1267–1282. doi: 10.3748/wjg.v27.i13.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark TM, Jones JM, Hall AG, Tabner SA, Kmiec RL. Theoretical explanation for reduced body mass index and obesity rates in cannabis users. Cannabis Cannabinoid Res. 2018;3(1):259–271. doi: 10.1089/can.2018.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cluny NL, Keenan CM, Reimer RA, Le Foll B, Sharkey KA. Prevention of diet-induced obesity effects on body weight and gut microbiota in mice treated chronically with Δ9-tetrahydrocannabinol. PLoS One. 2015;10(12):e0144270. doi: 10.1371/journal.pone.0144270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costiniuk CT, Mills E, Cooper CL. Evaluation of oral cannabinoid-containing medications for the management of interferon and ribavirin-induced anorexia, nausea and weight loss in patients treated for chronic hepatitis C virus. Can J Gastroenterol. 2008;22(4):376–380. doi: 10.1155/2008/725702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delgado-Borrego A, Kamegaya Y, Jordan SH, Agrawal S, Valim C, Chung RT. HCV synergizes with body weight in the promotion of insulin resistance. J Viral Hepat. 2011;18(2):135–141. doi: 10.1111/j.1365-2893.2010.01291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkler D, Plischke M, Leffondré K, Heinze G. Augmented backward elimination: a pragmatic and purposeful way to develop statistical models. PLoS One. 2014;9(11):e113677. doi: 10.1371/journal.pone.0113677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. 2017;13(4):851–863. doi: 10.5114/aoms.2016.58928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman TP, Craft S, Wilson J, Stylianou S, ElSohly M, Di Forti M, et al. Changes in delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) concentrations in cannabis over time: systematic review and meta-analysis. Addiction. 2021;116(5):1000–1010. doi: 10.1111/add.15253. [DOI] [PubMed] [Google Scholar]
- Gandilhon M, Spilka S, Masson C. Les mutations du marché du cannabis en France (transformations of French cannabis market). Paris: OFDT; 2019. Available from: https://www.ofdt.fr/publications/collections/rapports/thema/les-mutations-du-marche-du-cannabis-en-france-thema/.
- Graczyk M, Lewandowska AA, Dzierżanowski T. The therapeutic potential of cannabis in counteracting oxidative stress and inflammation. Molecules. 2021;26(15):4551. doi: 10.3390/molecules26154551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- Hashiesh HM, Sharma C, Goyal SN, Sadek B, Jha NK, Kaabi JA, et al. A focused review on CB2 receptor-selective pharmacological properties and therapeutic potential of β-caryophyllene, a dietary cannabinoid. Biomed Pharmacother. 2021;140:111639. doi: 10.1016/j.biopha.2021.111639. [DOI] [PubMed] [Google Scholar]
- Haute Autorité de Santé (French National Authority for Health) Screening tool for early detection and brief intervention (Outil d’aide au repérage précoce et à l’intervention brève) 2014. [Google Scholar]
- Henshaw FR, Dewsbury LS, Lim CK, Steiner GZ. The effects of cannabinoids on pro- and anti-inflammatory cytokines: a systematic review of in vivo studies. Cannabis Cannabinoid Res. 2021;6(3):177–195. doi: 10.1089/can.2020.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindocha C, Freeman TP, Ferris JA, Lynskey MT, Winstock AR. No smoke without tobacco: a global overview of cannabis and tobacco routes of administration and their association with intention to quit. Front Psychiatry. 2016;7 [cited 2020 May 22]. Available from: https://www.frontiersin.org/articles/10.3389/fpsyt.2016.00104/full. [DOI] [PMC free article] [PubMed]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. Wiley; 2000 [cited 2019 Oct 8]. Available from: https://onlinelibrary.wiley.com/doi/book/10.1002/0471722146.
- Hruby A, Manson JE, Qi L, Malik VS, Rimm EB, Sun Q, et al. Determinants and consequences of obesity. Am J Public Health. 2016;106(9):1656–1662. doi: 10.2105/AJPH.2016.303326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang R, Rao HY, Yang M, Gao YH, Wang J, Jin Q, et al. Histopathology and the predominantly progressive, indeterminate and predominately regressive score in hepatitis C virus patients after direct-acting antivirals therapy. World J Gastroenterol. 2021;27(5):404–415. doi: 10.3748/wjg.v27.i5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institut National de la Statistique et des Etudes Economiques. Définition - Pauvreté monétaire / Seuil de pauvreté / Seuil de pauvreté | Insee. [cited 2021 Dec 10]. Available from: https://www.insee.fr/fr/metadonnees/definition/c1653.
- Jadoon KA, Ratcliffe SH, Barrett DA, Thomas EL, Stott C, Bell JD, et al. Efficacy and safety of cannabidiol and tetrahydrocannabivarin on glycemic and lipid parameters in patients with type 2 diabetes: a randomized, double-blind, placebo-controlled, parallel group pilot study. Diabetes Care. 2016;39(10):1777–1786. doi: 10.2337/dc16-0650. [DOI] [PubMed] [Google Scholar]
- Ji D, Chen GF, Niu XX, Zhang M, Wang C, Shao Q, et al. Non-alcoholic fatty liver disease is a risk factor for occurrence of hepatocellular carcinoma after sustained virologic response in chronic hepatitis C patients: a prospective four-years follow-up study. Metabol Open. 2021;10:100090. doi: 10.1016/j.metop.2021.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jing L, Zhang Y, Fan S, Gu M, Guan Y, Lu X, et al. Preventive and ameliorating effects of citrus D-limonene on dyslipidemia and hyperglycemia in mice with high-fat diet-induced obesity. Eur J Pharmacol. 2013;715(1–3):46–55. doi: 10.1016/j.ejphar.2013.06.022. [DOI] [PubMed] [Google Scholar]
- Kang Q, Xu J, Luo H, Tan N, Chen H, Cheng R, et al. Direct antiviral agent treatment leads to rapid and significant fibrosis regression after HCV eradication. J Viral Hepat. 2021;28(9):1284–1292. doi: 10.1111/jvh.13558. [DOI] [PubMed] [Google Scholar]
- Lopez Trinidad LM, Martinez R, Kapravelou G, Galisteo M, Aranda P, Porres JM, et al. Caloric restriction, physical exercise, and CB1 receptor blockade as an efficient combined strategy for bodyweight control and cardiometabolic status improvement in male rats. Sci Rep. 2021;11(1):4286. doi: 10.1038/s41598-021-83709-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meah F, Lundholm M, Emanuele N, Amjed H, Poku C, Agrawal L, et al. The effects of cannabis and cannabinoids on the endocrine system. Rev Endocr Metab Disord. 2022;23(3):401–420. doi: 10.1007/s11154-021-09682-w. [DOI] [PubMed] [Google Scholar]
- Meier MH, Pardini D, Beardslee J, Matthews KA. Associations between cannabis use and cardiometabolic risk factors: a longitudinal study of men. Psychosom Med. 2019;81(3):281–288. doi: 10.1097/PSY.0000000000000665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min J, Goodale H, Xue H, Brey R, Wang Y. Racial-ethnic disparities in obesity and biological, behavioral, and sociocultural influences in the United States: a systematic review. Adv Nutr. 2021;12(4):1137–1148. doi: 10.1093/advances/nmaa162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minami T, Tateishi R, Fujiwara N, Nakagomi R, Nakatsuka T, Sato M, et al. Impact of obesity and heavy alcohol consumption on hepatocellular carcinoma development after HCV eradication with antivirals. Liver Cancer. 2021;10(4):309–319. doi: 10.1159/000513705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton S, Braithwaite D, Akinyemiju TF. Socio-economic status over the life course and obesity: systematic review and meta-analysis. PLoS One. 2017;12(5):e0177151. doi: 10.1371/journal.pone.0177151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngueta G, Bélanger RE, Laouan-Sidi EA, Lucas M. Cannabis use in relation to obesity and insulin resistance in the Inuit population. Obesity (Silver Spring) 2015;23(2):290–295. doi: 10.1002/oby.20973. [DOI] [PubMed] [Google Scholar]
- Ngueta G. Lifetime average cannabis use in relation to hypertriglyceridemic waist phenotype in U.S. adults: a population-based cross-sectional study. Cannabis Cannabinoid Res. 2020;5(3):246–254. doi: 10.1089/can.2019.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Sullivan SE, Yates AS, Porter RK. The peripheral cannabinoid receptor type 1 (CB1) as a molecular target for modulating body weight in man. Molecules. 2021;26(20):6178. doi: 10.3390/molecules26206178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patsenker E, Sachse P, Chicca A, Gachet MS, Schneider V, Mattsson J, et al. Elevated levels of endocannabinoids in chronic hepatitis C may modulate cellular immune response and hepatic stellate cell activation. Int J Mol Sci. 2015;16(4):7057–7076. doi: 10.3390/ijms16047057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pigeyre M, Rousseaux J, Trouiller P, Dumont J, Goumidi L, Bonte D, et al. How obesity relates to socio-economic status: identification of eating behavior mediators. Int J Obes (Lond) 2016;40(11):1794–1801. doi: 10.1038/ijo.2016.109. [DOI] [PubMed] [Google Scholar]
- Pol S, Bourliere M, Lucier S, Hezode C, Dorival C, Larrey D, et al. Safety and efficacy of daclatasvir-sofosbuvir in HCV genotype 1-mono-infected patients. J Hepatol. 2017;66(1):39–47. doi: 10.1016/j.jhep.2016.08.021. [DOI] [PubMed] [Google Scholar]
- Protopopescu C, Santos ME, Sogni P, Marcellin F, Esterle L, Wittkop L, et al. Protective effect of cannabis and coffee consumption on HCV-related mortality in French HIV-HCV co-infected patients (ANRS CO13 HEPAVIH cohort) J Hepatol. 2018;68:S142–S143. doi: 10.1016/S0168-8278(18)30501-4. [DOI] [Google Scholar]
- Roche B, Coilly A, Duclos-Vallee JC, Samuel D. The impact of treatment of hepatitis C with DAAs on the occurrence of HCC. Liver Int. 2018;38(Suppl 1):139–145. doi: 10.1111/liv.13659. [DOI] [PubMed] [Google Scholar]
- Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16(3):177–189. doi: 10.1038/s41574-019-0310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo EB. The case for the entourage effect and conventional breeding of clinical cannabis: no ‘strain,’ no gain. Front Plant Sci. 2018;9:1969. doi: 10.3389/fpls.2018.01969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos ME, Protopopescu C, Zucman D, Marcellin F, Wittkop L, Miailhes P, et al. Benefits of cannabis use for metabolic disorders and survival in people living with HIV with or without hepatitis C co-infection. AIDS. 2020;34(6):953–954. doi: 10.1097/QAD.0000000000002480. [DOI] [PubMed] [Google Scholar]
- Scandiffio R, Geddo F, Cottone E, Querio G, Antoniotti S, Gallo MP, et al. Protective effects of (E)-β-caryophyllene (BCP) in chronic inflammation. Nutrients. 2020;12(11) [cited 2021 May 17]. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7692661/. [DOI] [PMC free article] [PubMed]
- Serfaty L. Metabolic manifestations of hepatitis C virus: diabetes mellitus, dyslipidemia. Clin Liver Dis. 2017;21(3):475–486. doi: 10.1016/j.cld.2017.03.004. [DOI] [PubMed] [Google Scholar]
- Shai I, Jiang R, Manson JE, Stampfer MJ, Willett WC, Colditz GA, et al. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care. 2006;29(7):1585–1590. doi: 10.2337/dc06-0057. [DOI] [PubMed] [Google Scholar]
- Sidney S. Marijuana use and type 2 diabetes mellitus: a review. Curr Diab Rep. 2016;16(11):117. doi: 10.1007/s11892-016-0795-6. [DOI] [PubMed] [Google Scholar]
- Spindle TR, Kuwabara H, Eversole A, Nandi A, Vandrey R, Antoine DG, et al. Brain imaging of cannabinoid type I (CB1 ) receptors in women with cannabis use disorder and male and female healthy controls. Addict Biol. 2021;26(6):e13061. doi: 10.1111/adb.13061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling RK, Eduardo L, Nathan C, Ricard S, Cassia CM, Julio M, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43(6):1317–1325. doi: 10.1002/hep.21178. [DOI] [PubMed] [Google Scholar]
- Toselli S, Gualdi-Russo E, Boulos DNK, Anwar WA, Lakhoua C, Jaouadi I, et al. Prevalence of overweight and obesity in adults from North Africa. Eur J Public Health. 2014;24(Suppl 1):31–39. doi: 10.1093/eurpub/cku103. [DOI] [PubMed] [Google Scholar]
- Vallet-Pichard A, Mallet V, Nalpas B, Verkarre V, Nalpas A, Dhalluin-Venier V, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. Comparison with liver biopsy and fibrotest. Hepatology. 2007;46(1):32–36. doi: 10.1002/hep.21669. [DOI] [PubMed] [Google Scholar]
- Váncsa S, Németh D, Hegyi P, Szakács Z, Farkas Á, Kiss S, et al. Diabetes mellitus increases the risk of hepatocellular carcinoma after direct-acting antiviral therapy: systematic review and meta-analysis. Front Med (Lausanne) 2021;8:744512. doi: 10.3389/fmed.2021.744512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veilleux A, Di Marzo V, Silvestri C. The expanded endocannabinoid system/endocannabinoidome as a potential target for treating diabetes mellitus. Curr Diab Rep. 2019;19(11):117. doi: 10.1007/s11892-019-1248-9. [DOI] [PubMed] [Google Scholar]
- Vieira LS, Bierhals IO, Vaz JDS, Meller FDO, Wehrmeister FC, Assunção MCF. Socioeconomic status throughout life and body mass index: a systematic review and meta-analysis. Cad Saude Publica. 2019;35(10):e00125518. doi: 10.1590/0102-311x00125518. [DOI] [PubMed] [Google Scholar]
- Wang CS, Wang ST, Yao WJ, Chang TT, Chou P. Hepatitis C virus infection and the development of type 2 diabetes in a community-based longitudinal study. Am J Epidemiol. 2007;166(2):196–203. doi: 10.1093/aje/kwm061. [DOI] [PubMed] [Google Scholar]
- Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Wargent ET, Zaibi MS, Silvestri C, Hislop DC, Stocker CJ, Stott CG, et al. The cannabinoid Δ9-tetrahydrocannabivarin (THCV) ameliorates insulin sensitivity in two mouse models of obesity. Nutr Diabetes. 2013;3(5):e68. doi: 10.1038/nutd.2013.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . Body mass index - BMI. 2019. [Google Scholar]
- Younossi ZM, McCullough AJ, Ong JP, Barnes DS, Post A, Tavill A, et al. Obesity and non-alcoholic fatty liver disease in chronic hepatitis C. J Clin Gastroenterol. 2004;38(8):705–709. doi: 10.1097/01.mcg.0000135372.10846.2a. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to ongoing data treatment; however, they are available from the corresponding author upon reasonable request.