Abstract
Background
The World Health Organization recommends that abortion can be provided at the lowest level of the healthcare system. Training mid‐level providers, such as midwives, nurses and other non‐physician providers, to conduct first trimester aspiration abortions and manage medical abortions has been proposed as a way to increase women's access to safe abortion procedures.
Objectives
To assess the safety and effectiveness of abortion procedures administered by mid‐level providers compared to doctors.
Search methods
We searched the CENTRAL Issue 7, MEDLINE and POPLINE databases for comparative studies of doctor and mid‐level providers of abortion services. We searched for studies published in any language from January 1980 until 15 August 2014.
Selection criteria
Randomised controlled trials (RCTs) (clustered or not clustered), prospective cohort studies or observational studies that compared the safety or effectiveness (or both) of any type of first trimester abortion procedure, administered by any type of mid‐level provider or doctors, were eligible for inclusion in the review.
Data collection and analysis
Two independent review authors screened abstracts for eligibility and double‐extracted data from the included studies using a pre‐tested form. We meta‐analysed primary outcome data using both fixed‐effect and random‐effects models to obtain pooled risk ratios (RR) with 95% confidence intervals (CIs). We carried out separate analyses by study design (RCT or cohort) and type of abortion procedure (medical versus surgical).
Main results
Eight studies involving 22,018 participants met our eligibility criteria. Five studies (n = 18,962) assessed the safety and effectiveness of surgical abortion procedures administered by mid‐level providers compared to doctors. Three studies (n = 3056) assessed the safety and effectiveness of medical abortion procedures. The surgical abortion studies (one RCT and four cohort studies) were carried out in the United States, India, South Africa and Vietnam. The medical abortion studies (two RCTs and one cohort study) were carried out in India, Sweden and Nepal. The studies included women with gestational ages up to 14 weeks for surgical abortion and nine weeks for medical abortion.
Risk of selection bias was considered to be low in the three RCTs, unclear in four observational studies and high in one observational study. Concealment bias was considered to be low in the three RCTs and high in all five observational studies. Although none of the eight studies performed blinding of the participants to the provider type, we considered the performance bias to be low as this is part of the intervention. Detection bias was considered to be high in all eight studies as none of the eight studies preformed blinding of the outcome assessment. Attrition bias was low in seven studies and high in one, with over 20% attrition. We considered six studies to have unclear risk of selective reporting bias as their protocols had not been published. The remaining two studies had published their protocols. Few other sources of bias were found.
Based on an analysis of three cohort studies, the risk of surgical abortion failure was significantly higher when provided by mid‐level providers than when procedures were administered by doctors (RR 2.25, 95% CI 1.38 to 3.68), however the quality of evidence for this outcome was deemed to be very low. For surgical abortion procedures, we found no significant differences in the risk of complications between mid‐level providers and doctors (RR 0.99, 95% CI 0.17 to 5.70 from RCTs; RR 1.38, 95% CI 0.70 to 2.72 from observational studies). When we combined the data for failure and complications for surgical abortion we found no significant differences between mid‐level providers and doctors in both the observational study analysis (RR 1.36, 95% CI 0.86 to 2.14) and the RCT analysis (RR 3.07, 95% CI 0.16 to 59.08). The quality of evidence of the outcome for RCT studies was considered to be low and for observational studies very low. For medical abortion procedures the risk of failure was not different for mid‐level providers or doctors (RR 0.81, 95% CI 0.48 to 1.36 from RCTs; RR 1.09, 95% CI 0.63 to 1.88 from observational studies). The quality of evidence of this outcome for the RCT analysis was considered to be high, although the quality of evidence of the observational studies was considered to be very low. There were no complications reported in the three medical abortion studies.
Authors' conclusions
There was no statistically significant difference in the risk of failure for medical abortions performed by mid‐level providers compared with doctors. Observational data indicate that there may be a higher risk of abortion failure for surgical abortion procedures administered by mid‐level providers, but the number of studies is small and more robust data from controlled trials are needed. There were no statistically significant differences in the risk of complications for first trimester surgical abortions performed by mid‐level providers compared with doctors.
Plain language summary
Can health care providers who are not doctors perform abortions as well as doctors?
Unsafe abortion causes death and disability and remains a major public health concern in developing countries. Most of these deaths and disabilities could be prevented if safe and legal abortion were provided by trained people. This review looked at whether using mid‐level providers (health care providers who are not doctors) to perform abortions is safe. It also looked at whether the abortions provided by mid‐level providers worked as well as those provided by doctors.
We carried out searches for studies that compared medical abortion (using pills) or surgical abortion provided by either mid‐level providers or doctors. We also wrote to researchers to find more studies. The studies could compare how safe the abortions were or how effective they were (whether they actually worked). The evidence we found is up to date as of the 15th of August 2014.
We found eight studies with a total of 22,018 participants. Five studies compared surgical abortion provided by doctors or mid‐level providers and three studies compared medical abortion provided by doctors or mid‐level providers. Of the five surgical abortion studies only one had a high‐quality study design. Of the three medical abortion studies, two had a high‐quality study design. Three of these studies were carried out in America, two in India, one in was carried out in both South Africa and Vietnam the remaining two were from Sweden and Nepal.
The results from the analyses of the medical abortion studies showed that there does not seem to be an advantage when these are provided by doctors. The results from most of the analyses of the surgical abortion studies showed that we cannot be sure that there is a difference in how safe and how effective mid‐level providers are compared to doctors. One analysis of three low‐quality studies of surgical abortion showed that there was more chance of the abortion being ineffective if it was provided by mid‐level providers.
Most of the studies did not show a difference between mid‐level providers and doctors in how safe the abortions were and how well they worked. Training mid‐level providers to give medical or surgical abortions could reduce the number of deaths and the disability caused by unsafe abortion. Studies in the future should focus on what types of mid‐level providers can provide safe and effective abortions. They should also look at whether mid‐level providers are as safe and effective as doctors for providing abortions in rural developing country settings.
Summary of findings
Background
Description of the condition
Unsafe abortion remains a major public health concern in developing countries. Despite the existence of safe and effective surgical methods (Kulier 2009), and medical methods to induce abortion (Kulier 2011), an estimated 22 million unsafe abortions are performed each year, resulting in the deaths of 47,000 women and disabilities for an additional five million women (Sedgh 2012). Most of these deaths and disabilities could be prevented through the provision of safe and legal induced abortion by qualified providers.
To ensure that women living in developing countries can readily access safe termination procedures, the World Health Organization (WHO) recommends that abortion can be provided at the lowest level of the healthcare system (WHO 2008). However, in many developing countries, even in settings where abortion is legal, access to abortion remains limited due to a shortage of trained physicians.
Irrespective of legal conditions, in settings where access to safe abortion care is lacking, women often obtain termination services from unqualified or unskilled providers (WHO 2012). Therefore, training mid‐level providers (midwives, nurses and other non‐physician providers) to conduct first‐trimester aspiration abortions and manage medical abortions has been proposed as a way to increase women's access to safe abortion procedures (Berer 2009).
Description of the intervention
In order to address the shortage of human resources for abortion services, mid‐level providers have been used in a number of settings. Mid‐level providers are midwives or any other healthcare worker who has less training than doctors and provides clinical care. There are two methods of abortion: medical and surgical. Medical abortion is the use of drugs to induce abortion. The gold standard for this therapy is a combination of mifepristone and misoprostol. Surgical abortion uses transcervical procedures to terminate the pregnancy, including manual vacuum aspiration (MVA) and dilation and evacuation. Both are safe and effective methods for abortion that are recommended by the World Health Organization (WHO 2012).
How the intervention might work
Authorising and training mid‐level providers to provide abortion could reduce the number of unsafe procedures and alleviate the burden on healthcare systems. A review of medical abortion service delivery has suggested that the provision and management of medical abortion by mid‐level providers is cost‐effective in resource‐limited settings due to salary costs and the scarcity of physicians (Berer 2009). However, not all countries across the world adopt this practice. In many developed country settings, including France and the UK (Jones 2000), nurses and midwives are not permitted to manage and administer abortion procedures independently. Only a handful of countries in the developing world permit midwives to perform aspiration abortion (Cambodia (Long 2001) and South Africa) or paramedics to carry out 'menstrual regulation' procedures (Bangladesh). In many countries, national policies limit access to medical abortion by restricting its prescription and provision to certified physicians (Yarnall 2009).
Why it is important to do this review
Training mid‐level providers to conduct aspiration abortions and manage medical abortions has been proposed as a way to increase women's access to safe abortion. However, only a few countries across the world have adopted this practice. Restrictions on mid‐level provision are mainly due to concerns about the standard of care and safety of the abortions provided. In order to inform clinical practice and policy regarding abortion provision, a review of the evidence on the effectiveness and safety of abortion procedures performed by mid‐level providers compared with doctors is therefore needed. This review aims to update a previous systematic review published in 2012 (Ngo 2013). This review included published studies assessing the effectiveness or safety (or both) of abortion provided by mid‐level providers compared with procedures provided by doctors. For the purposes of this review, we will define mid‐level providers as any trained health professionals who are not physicians (WHO 2010).
Objectives
To assess the safety and effectiveness of abortion procedures administered by mid‐level providers compared to doctors.
Methods
Criteria for considering studies for this review
Types of studies
We included RCTs and cohort studies that assessed the safety and effectiveness of surgical or medical abortion procedures administered by mid‐level providers compared to doctors.
Types of participants
We included women of any age, in any setting who were seeking abortion procedures (gestational age less than 14 weeks for surgical abortion and less than nine weeks for medical abortion).
Types of interventions
We included any type of abortion procedure provided by either doctors or mid‐level providers in any setting. Mid‐level providers included nurses, nurse practitioners, ayurvedic practitioners, physician assistants, midwives, auxiliary nurse midwives and certified nurse midwives. Mid‐level providers worked independently when carrying out the abortion procedure.
Types of outcome measures
Primary outcomes
Failure/incomplete abortion, including continuing pregnancy at follow‐up and incomplete abortion.
Complications of abortion, including haematometra, haemorrhage, endocervical injury, anaesthesia‐related reactions, uterine perforation, infection, injury to bowel, any complication requiring blood transfusion and any complication requiring hospitalisation.
Secondary outcomes
Total complications (incomplete or failed abortion and complications).
Search methods for identification of studies
Electronic searches
We carried out a search on the 15th of August 2014. We searched the Cochrane Central Register of Controlled Trials Issue 7, Ovid MEDLINE and POPLINE for studies assessing the effectiveness and safety of mid‐level provision of abortion, using the following terms:
((("Nurses"[Mesh] OR "Physician Assistants"[Mesh] OR "mid‐level provider"[text word] OR "mid‐level providers"[text word] OR nurse*[text word] OR midwife*[text word] OR midwives[text word] OR "nurse practitioner"[text word] OR "nurse practitioners"[text word] OR "physician assistant"[text word] OR "physician assistants"[text word] OR "non‐physician"[text word] OR "non‐physicians"[text word] OR "substitute health worker"[text word] OR "substitute health workers"[text word] OR auxiliar*[text word]) AND ("Abortion, Incomplete"[Mesh] OR "Abortion, Induced"[Mesh:noexp] OR "Abortion, Legal"[Mesh] OR "Abortion, Therapeutic"[Mesh:noexp] OR abortion*[text word]))) AND ("1980"[Date ‐ Publication] : "3000"[Date ‐ Publication])
We restricted the search results to studies published after 1980 through to 15th August 2014 for all databases. We placed no limits on language.
Searching other resources
We handsearched the reference lists of key articles and also contacted investigators in the field to find studies that were not identified in the electronic search, including unpublished reports. We also searched the EU clinical trials register, ICTRP and ISRCTN registers for publications of protocols.
Data collection and analysis
Selection of studies
Two review authors (SB, CK) independently screened the titles and abstracts of studies for eligibility. We retrieved the full text of potentially eligible studies and applied the inclusion criteria to the retrieved publications. We sought further information from the authors where papers contained insufficient information to make a decision about eligibility. There was good inter‐rater agreement (kappa coefficient = 0.619). We resolved disagreements about the inclusion of studies by consensus.
Data extraction and management
Two independent authors (SB, CK) double‐extracted data using a pre‐designed standard form. We checked the extracted data from each review author against each other and, if necessary, made reference to the original paper. We resolved any outstanding discrepancies by consensus. Where necessary, we also contacted study authors twice over a period of two months in an attempt to obtain any missing information. One author (SB) entered the data into Review Manager (RevMan 2014), and another author (CK) checked the entries for accuracy.
Assessment of risk of bias in included studies
Two authors assessed the risk of bias for the included studies in the following domains: selection bias, performance bias, detection bias, attrition bias, reporting bias and other biases and recorded this in the 'Risk of bias' tables. We ranked the studies as 'low risk', 'high risk' or 'unclear risk' using the criteria recommended by theCochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
We used the GRADE approach to assess the quality of the body of evidence used in meta‐analysis (Higgins 2011). Using the GRADE methods we assessed within‐study risk of bias (methodological quality), directness of evidence, heterogeneity, precision of effect estimates and risk of publication bias. We rated the quality of the body of evidence as high, moderate, low or very low.
Measures of treatment effect
The main measures of effect were pooled risk ratios (RRs) of the primary outcomes (failure, complications, failure + complications) for mid‐level providers compared to doctors. Data on the number of events and number of participants assigned to each treatment group were meta‐analysed using Mantel‐Haenszel fixed‐effect and random‐effects models (Higgins 2011; RevMan 2014). For studies that included rates rather than number of events, we contacted study authors for data relating to the number of events. If the study authors did not respond, we calculated the number of events using the rates reported in the study.
Unit of analysis issues
For all included studies, we assessed whether an appropriate analysis had been done that adjusted for clustering by provider in calculating measures of precision. Two studies adjusted for clustering at the design stage (by increasing the sample size) and in analysis (Kopp Kallner 2015; Warriner 2011). Four studies increased the sample size by 10% to 15% in order to adjust for clustering (Jejeebhoy 2011; Jejeebhoy 2012; Warriner 2006; Weitz 2013). Two studies did not mention adjustment for clustering in their methods (Freedman 1986; Goldman 2004). We were unable to adjust for clustering in the meta‐analysis as we were unable to obtain the raw data.
When analysing the data for failure and incomplete abortion for medical abortion RCTs (Kopp Kallner 2015; Warriner 2011), we used the per protocol analysis data from each study.
Dealing with missing data
We attempted to obtain missing data from the authors. If we did not receive a response we did not attempt to impute missing data.
Assessment of heterogeneity
We determined clinical heterogeneity using the I2 statistic and qualitative assessment of forest plots. We used a random‐effects model for meta‐analysis if the I2 statistic was ≥ 50% and we identified heterogeneity qualitatively. We used a fixed‐effect model if the I2 statistic was ≤ 50% and we did not identify heterogeneity qualitatively.
Assessment of reporting biases
We assessed selective outcome reporting as a risk of bias criterion, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). In order to identify differences between outcomes in the study protocol and in the published study we searched databases for publication of protocols and contacted study authors if the protocol was not available. Finally, we compared the outcomes reported between the studies included in the review.
Data synthesis
Over a period of a month we attempted to contact several researchers by email for supplemental data. If we did not receive a response, we did not attempt to impute the data. One author entered the data into Review Manager (RevMan 2014), and another author checked the entries for accuracy.
For the surgical abortion studies, we carried out meta‐analyses for failure (including incomplete abortion), complications and for complications including failure and incomplete abortion. For the medical abortion studies we carried out meta‐analysis for failure, including incomplete abortions. All meta‐analyses used Mantel‐Haenszel models and we used the Review Manager software (RevMan 2014). We analysed and presented RCTs independently of cohort studies. As there was only one cohort study for medical abortion, we carried out no meta‐analysis.
Subgroup analysis and investigation of heterogeneity
No subgroup analyses were conducted. We investigated heterogeneity using both the I2 statistic and visual inspection.
Sensitivity analysis
We separately analysed RCTs and non‐RCTs to assess the effect of study quality on the main outcomes. We performed sensitivity analysis for immediate and delayed complications and developing and developed settings.
Results
Description of studies
Results of the search
There were 1525 citations identified in the search, of which 253 were duplicates. Of the 1273 unique citations, we excluded 1185 citations based on title screening. We identified 87 titles as potentially relevant and screened the abstracts for retrieval. Based on abstract screening, we excluded 73 citations and retrieved full texts for 15 citations. Eight studies met the inclusion criteria; of these, five had been included in the Ngo 2013 review and we identified two more recent studies. We identified an additional study in July 2014. All studies were published in English (Figure 1).
1.
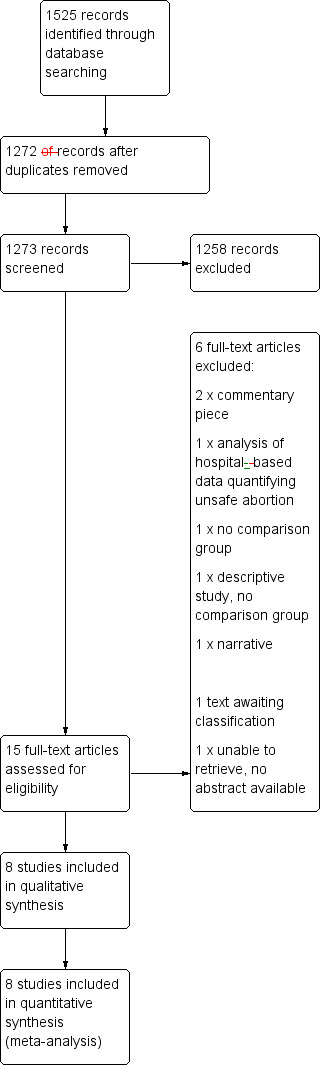
Study flow diagram.
Included studies
We included eight studies in this review (Characteristics of included studies), comprising five prospective cohort studies and three randomised controlled trials (RCTs). A total of 22,018 women were included across the eight studies; of these, 11,091 women underwent a procedure administered by a mid‐level provider (9339 had surgical abortion; 1752 had medical abortion) and 10,927 women underwent a physician‐administered procedure (9623 had surgical abortion; 1304 had medical abortion). All studies took place in either a hospital or a specialist health clinic, such as a women's health centre or sexual and reproductive health clinic. Studies are described in detail in the Characteristics of included studies table. One RCT of manual vacuum aspiration (MVA) procedures administered by mid‐level providers and physicians took place in South Africa (n = 1153) and Vietnam (n = 1636) in 2003 (Warriner 2006). The other RCTs were carried out in Nepal in 2009 (n = 976) (Warriner 2011) and Sweden in 2011 (n = 916) (Kopp Kallner 2015), and compared the outcomes of medical abortion procedures administered by mid‐level providers and physicians. The five prospective cohort studies (n = 7939) assessed surgical abortion procedures conducted in the US in 1981 (Freedman 1986), 1997 (Goldman 2004) and 2012 (Weitz 2013), in India in 2009 (Jejeebhoy 2011), and medical abortion in India in 2010 (Jejeebhoy 2012).
The included studies are described below, by type of abortion (surgical or medical).
Surgical abortion studies
A RCT conducted in South Africa and Vietnam compared the outcomes of MVA procedures for pregnancies up to 12 weeks gestation delivered by mid‐level providers, with government‐accredited training in abortion, and those administered by physicians (Warriner 2006). The number of years of provider experience differed between mid‐level providers and doctors in both countries. In the South African study the median experience for doctors was seven years while for mid‐level providers the median number of years experience was four years. In Vietnam, the mid‐level providers had a median of seven years of experience, while doctors had a median of 10 years of experience. All participants were offered lidocaine and additional oral analgesia; in one of the study locations (South Africa), misoprostol 400 mg was administered two to three hours before the procedure. Women were followed up 10 to 14 days after the procedure. The outcomes of interest were: total complication rates for mid‐level providers and doctors by time of complication; total number of women reporting adverse symptoms at follow‐up interviews for mid‐level providers and doctors.
Four prospective cohort studies used surgical abortion methods (Freedman 1986; Goldman 2004; Jejeebhoy 2011; Weitz 2013).
One study, conducted in the US, used early uterine evacuation or suction curettage (Freedman 1986), delivered by either a physician assistant or a physician; women arriving at the clinic were seen by the next available provider and were followed up within four weeks of the procedure. The outcomes of interest were: total complication rates for physician assistants and physicians by procedure and weeks gestation; total complication rates by procedure and time of complication; distribution of complications by procedure and time of complication.
In another US study (Goldman 2004), physicians with at least five years experience in abortion procedures performed standard vacuum curettage procedures for pregnancies up to 12 weeks gestation, while physician assistants with the same level of experience provided MVA or standard vacuum curettage procedures for pregnancies up to 14 weeks gestation. Follow‐up was within 14 days of the procedure. The outcomes of interest were: total complication rates by site and time of occurrence; procedures with complication by gestational age and abortion method; complication type by site.
A study conducted in India used MVA delivered by nurses or physicians with no previous experience of providing any type of abortion, who underwent 10 days of MVA training as part of the study (Jejeebhoy 2011). All abortion procedures were conducted in the presence of a qualified supervisor. Women were followed up after seven days. The outcomes of interest were: accuracy of assessment of gestational age for nurses and physicians; accuracy of assessment of other criteria relating to eligibility for nurses and physicians; assessment of complete abortion for nurses and physicians; rate of complete abortion by day seven by nurses and physicians; overall complication rate for nurses and physicians; complication rates (not including failure) for nurses and physicians.
The most recent study was conducted in the USA (Weitz 2013), and compared complication rates within four weeks of aspiration abortion for nurse practitioners, certified nurse midwives and physician assistants to those of physicians. Providers were trained to competency in the provision of aspiration abortion and had a California professional license and basic life support. The mean number of years of experience differed between mid‐level providers and physicians. The mean number of years experience of mid‐level providers' was 1.5 years while for physicians it was 14 years. Providers performed aspiration abortion on participants with less than 14 weeks gestation. Follow‐up was within four weeks of the procedure. The outcomes of interest were: incidence of major and minor complications within four weeks of aspiration abortion for nurse practitioners, certified nurse midwives, physician assistants and physicians.
Medical abortion studies
Three studies (two RCTs and one cohort study) assessed the safety and effectiveness of mid‐level providers for medical abortion procedures (Jejeebhoy 2012; Kopp Kallner 2015; Warriner 2011).
The cohort study used a medical abortion regimen of 200 mg of mifepristone orally followed by 400 µg of misoprostol orally two days later for women of up to eight weeks gestation (Jejeebhoy 2012). The regimen was delivered by ayurvedic physicians, nurses and allopathic physicians in abortion clinics in India. Only providers who had never performed surgical or medical abortion, never conducted pelvic examinations or never assessed gestational age were recruited. All underwent identical medical training, which lasted 10 days. Women were followed up after 15 and 21 days (if extended follow‐up was advised). The outcomes of interest were: observed failure rates for ayurvedic physicians, nurses and allopathic physicians; complication rates for ayurvedic physicians, nurses and allopathic physicians; accuracy of eligibility assessment for nurses and allopathic physicians; accuracy of assessment of abortion completeness for nurses and allopathic physicians; acceptability for nurses and allopathic physicians (client satisfaction).
Both RCTs used a medical abortion regimen of 200 mg mifepristone orally followed by 800 mg of misoprostol vaginally one to two days later for pregnancies up to nine weeks of gestational age.
The Nepali study compared the safety and efficacy of staff nurses and auxiliary midwives trained in MVA to doctors (obstetricians, gynaecologists, general practitioners and other doctors) for medical abortion across five district hospitals in Nepal (Warriner 2011). The demographic data for the participants were similar to the socio‐demographic characteristics of women typically seeking abortions in Nepal. Mid‐level providers had a median of 25 years of professional medical practice experience compared to a median of 15 years for doctors. All providers underwent a three‐day training course in medical abortion. Women were followed up 10 to 14 days after the procedure. The outcomes of interest were: failed abortion and continuing pregnancy at 30 days for mid‐level healthcare providers and doctors; the extent to which each group provided medical abortion procedures independently; serious adverse events by provider type.
The Swedish RCT compared the efficacy, safety and acceptability of nurse midwives or doctors providing medical abortion at the outpatient family planning clinic of a university hospital in Stockholm (Kopp Kallner 2015). Two nurse‐midwives who were experienced in medical abortion and contraceptive counselling received theoretical and practical training in vaginal ultrasound examination of early pregnancy. A total of 34 doctors with varying levels of experience and training were involved in the study. Women randomised to the nurse midwife group were examined, counselled, informed and treated by a single nurse‐midwife. Participating nurse midwives did not perform any regular nurse midwife duties during the study period. Women randomised to the doctors group were examined and counselled by a doctor, and then received additional information from a nurse midwife. Follow‐up was at three weeks for failure and six weeks for complications, including incomplete abortion. The outcomes of interest were: efficacy, defined as the need for surgical intervention; safety, defined as no unscheduled visit within six weeks of medical abortion; and acceptability, defined as women preferring their allocated provider.
Excluded studies
We excluded six reports, which we had examined in full text. Two studies did not provide a comparison group and one did not fit the inclusion criteria for this review. Three reports that we retrieved were commentaries or narrative pieces. The remaining title listed no authors and could not be retrieved. This has been classified as 'awaiting classification'. (See table of Characteristics of excluded studies for more details).
Risk of bias in included studies
Allocation
The method of sequence generation was described in all eight studies. We considered selection bias associated with sequence generation to be low in three studies, unclear in four studies and high in one study (Figure 2; Figure 3).
2.
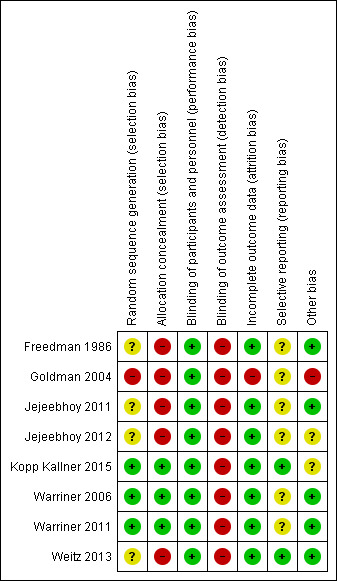
3.
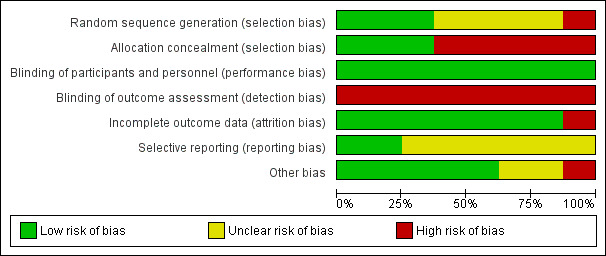
The three randomised trials used a computer‐generated randomisation scheme, giving each study a low risk of bias (Kopp Kallner 2015; Warriner 2006; Warriner 2011).
Although the remaining studies were observational studies, each described their method of allocation sequence generation. Freedman 1986 had the participants seen by the next available provider. Jejeebhoy 2011 described the sequence generation as "naturally random" by having one type of provider at each facility until they had completed the required number of vacuum aspirations. Jejeebhoy 2012 used the same methods, assigning providers to clinics until they had completed a required number of medical abortions. The most recent study, Weitz 2013, observed the outcomes of various providers at several health centres. While these four studies did not carry out random sequence generation, treatment allocation was not dependent on risk of failure or complications, therefore we considered the risk of selection bias to be unclear. Goldman 2004 compared two clinics in different US states, one clinic where the providers were physicians and the other where the providers were physician assistants. We assessed the risk of selection bias in this observational study to be high as the settings differed between states.
We considered allocation concealment bias to be low in three studies and high in five studies. For the three randomised studies, there was adequate allocation concealment. All three studies used sealed, opaque envelopes that contained the random allocation of the provider type. These envelopes were sequentially numbered and opened once written consent was obtained (Kopp Kallner 2015; Warriner 2006; Warriner 2011). There was no allocation concealment in the five observational studies (Freedman 1986; Goldman 2004; Jejeebhoy 2011; Jejeebhoy 2012; Weitz 2013).
Blinding
None of the eight studies performed blinding of participants. The participants' knowledge of the provider type is part of the intervention, therefore it is a better reflection of the real world effectiveness of the intervention. We considered this a low risk of bias as it is part of the intervention.
None of the eight studies performed blinding of outcome assessment. We considered this a high risk of bias.
Incomplete outcome data
We considered attrition bias to be low in seven studies and high in one study. We considered loss to follow‐up of greater than 20% to threaten study validity (Strauss 2005). We noted the Goldman 2004 study to have a loss to follow‐up of 28.5% (Goldman 2004). Another study reported a loss to follow‐up of 30%, however this loss was similar in both provider groups (Weitz 2013). The rest of the studies achieved a low rating for attrition bias due to their minimal loss to follow‐up rate. These six studies had a low loss to follow‐up rate (3% for Freedman 1986, 3.6% for Jejeebhoy 2011, 5% for Jejeebhoy 2012, 3.6% for Warriner 2006, 4% for Warriner 2011 and 12% for Kopp Kallner 2015).
Selective reporting
We considered six studies to have an unclear risk of bias for selective reporting. One study had published their protocol (Weitz 2013). Three studies did not publish their protocol prior to data collection but did make it available (Jejeebhoy 2011; Jejeebhoy 2012; Kopp Kallner 2015). It is unknown whether the protocols are available for the remaining four studies.
Other potential sources of bias
Only one of the eight studies had other sources of bias. Goldman 2004 had varied levels of clinician training between provider type, which introduced a type of performance bias.
In two studies, mid‐level providers and doctors worked from different clinics, therefore reducing the opportunity for mid‐level providers to discuss clinical concerns (Goldman 2004; Jejeebhoy 2011). In one study, although mid‐level providers and doctors were operating from the same site, a separate waiting area and examination rooms were provided to reduce interactions between providers and to act as a surrogate for how providers would manage in an independent setting (Warriner 2011). Four studies had mid‐level providers and doctors operating from the same site with no restrictions on interaction between providers (Freedman 1986; Kopp Kallner 2015; Warriner 2006; Weitz 2013). In two studies, although mid‐level providers worked independently, their assessments of failure were verified by a higher‐level clinician (Jejeebhoy 2011; Jejeebhoy 2012). Heterogeneity between studies makes it difficult to discuss the safety and efficacy of mid‐level providers carrying out abortion procedures independently from doctors.
This review analysed raw unadjusted data in order to make comparisons between studies. As a result we have not been able to control for confounding in non‐randomised studies. The quality of the analyses of non‐randomised studies has been downgraded as a result. Future versions of the review should attempt to analyse adjusted effect estimates when analysing non‐randomised studies.
Effects of interventions
Summary of findings for the main comparison. Surgical abortion procedures: mid‐level providers compared to doctors.
| Surgical abortion procedures: mid‐level providers compared to doctors | ||||||
|
Patient or population: Patients requesting abortion procedures
Settings: Hospital or clinic
Intervention: Surgical abortion administered by mid‐level providers Comparison: Surgical abortion administered by doctors | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Mid‐level providers | |||||
| Failure/incomplete abortion (RCTs) Provider assessment Follow‐up: 10 to 14 days | 6 per 1000 | 17 per 1000 (1 to 241) | RR 2.97 (0.21 to 41.82) | 2789 (2 studies) | ⊕⊕⊝⊝ low3 | — |
| Failure/incomplete abortion (observational studies) Provider or supervisor assessment Follow‐up: 7 to 28 days | 3 per 1000 | 7 per 1000 (4 to 12) | RR 2.2 (1.34 to 3.6) | 13,715 (3 studies) | ⊕⊝⊝⊝ very low1 | — |
| Complications (RCTs) Provider assessment Follow‐up: 10 to 14 days | 1 per 1000 | 1 per 1000 (0 to 8) | RR 0.99 (0.17 to 5.7) | 2789 (2 studies) | ⊕⊕⊝⊝ low3 | — |
| Complications (observational studies) Provider or supervisor assessment Follow‐up: 7 to 28 days | 7 per 1000 | 10 per 1000 (5 to 19) | RR 1.38 (0.7 to 2.72) | 13,715 (3 studies) | ⊕⊝⊝⊝ very low1,2 | — |
| Total complications (RCTs) Provider assessment Follow‐up: 10 to 14 days | 7 per 1000 | 22 per 1000 (1 to 425) | RR 3.07 (0.16 to 59.08) | 2789 (2 studies) | ⊕⊕⊝⊝ low3 | — |
| Total complications (observational studies) Provider or supervisor assessment Follow‐up: 7 to 28 days | 13 per 1000 | 18 per 1000 (11 to 28) | RR 1.36 (0.86 to 2.14) | 16,173 (4 studies) | ⊕⊝⊝⊝ very low1,2 | — |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval;RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Quality of evidence was downgraded from Low to Very Low due to Risk of bias. The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results. All studies are observational studies. Blinding in abortion studies is not feasible (ethical) . 2 Quality of evidence was downgraded from Low to Very Low due to Study Limitations and Imprecision (Wide confidence intervals for Jejeebhoy 2011). 3No events in the doctors group in South Africa.
Summary of findings 2. Medical abortion procedures: mid‐level providers compared to doctors.
| Medical abortion procedures: mid‐level providers compared to doctors | ||||||
|
Patient or population: Patients requesting abortion procedures
Settings: Hospital or clinic
Intervention: Medical abortion administered by mid‐level providers Comparison: Medical abortion administered by doctors | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Mid‐level providers | |||||
| Failure/incomplete abortion (RCTs) Provider assessment Follow‐up: 30 to 42 days | 33 per 1000 | 27 per 1000 (16 to 45) | RR 0.81 (0.48 to 1.36) | 1892 (2 studies) | ⊕⊕⊕⊕ high | — |
| Failure/incomplete abortion (observational studies) Verifier assessment Follow‐up: 15 to 21 days | 46 per 1000 | 50 per 1000 (29 to 87) | RR 1.09 (0.63 to 1.88) | 1164 (1 study) | ⊕⊝⊝⊝ very low1 | — |
|
Complications (RCTs) Provider assessment Follow‐up: 30 to 42 days |
0 per 1000 | 0 per 1000 | ‐ | 1892 (2 studies) |
⊕⊕⊕⊕ high | — |
|
Complications (observational studies) Verifier assessment Follow‐up: 15 to 21 days |
0 per 1000 | 0 per 1000 | ‐ | 1164 (1 study) | ⊕⊝⊝⊝ very low1 | — |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Quality of evidencewas downgraded from Low to Very Low due to Risk of bias. The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results. All studies are observational studies. Blinding in abortion studies is not feasible (ethical).
Surgical abortion
Failure/incomplete abortion
Failure/incomplete abortion included continuing pregnancy at follow‐up and incomplete abortion. Incomplete abortion was defined in four out of five of the surgical abortion studies as retained products of conception necessitating re‐evacuation. One study did not specify the definition of incomplete abortion (Weitz 2013).
In the randomised controlled trial (RCT) of surgical abortion, of the 1400 women who had a procedure provided by a mid‐level provider, 1.1% (n = 16) experienced a failed or incomplete abortion. Among the 1389 women who had an abortion provided by a doctor, 0.6% (n = 8) experienced a failed or incomplete abortion. There was no significant difference in the risk of failure among women who had a procedure provided by a mid‐level provider and those who had a procedure provided by a physician (risk ratio (RR) 2.97, 95% confidence interval (CI) 0.21 to 41.82) (Analysis 1.1).
1.1. Analysis.
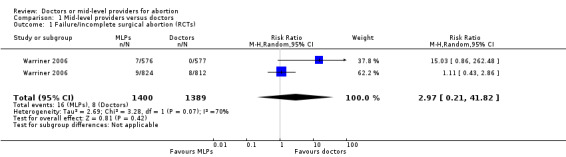
Comparison 1 Mid‐level providers versus doctors, Outcome 1 Failure/incomplete surgical abortion (RCTs).
In the three cohort studies that reported failure/incomplete abortion independently of total complication rates, 6654 women had an abortion procedure provided by a mid‐level provider. Of these women, 0.7% (n = 47) experienced a failed or incomplete abortion. Of the 7061 women who had an abortion provided by a physician, 0.3% (n = 23) experienced a failed or incomplete abortion. The risk of failure or incomplete abortion was higher among women who had a procedure provided by a mid‐level provider (pooled RR 2.25, 95% CI 1.38 to 3.68) (Analysis 1.2; Figure 4 ).
1.2. Analysis.
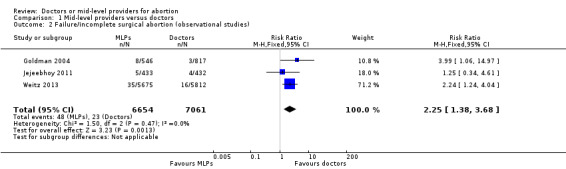
Comparison 1 Mid‐level providers versus doctors, Outcome 2 Failure/incomplete surgical abortion (observational studies).
4.
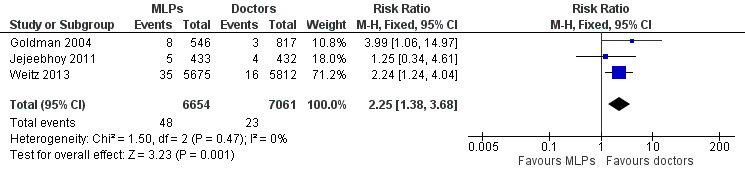
Forest plot of comparison: 1 Mid‐level providers versus doctors, outcome: 1.2 Failure/incomplete surgical abortion (observational studies).
Complications
Complications of abortion included haematometra, haemorrhage, endocervical injury, anaesthesia‐related reactions, uterine perforation, infection, injury to the bowel, any complication requiring blood transfusion and any complication requiring hospitalisation.
The RCT of surgical abortion showed that of the 1400 women who had a procedure delivered by a mid‐level provider, 0.1% (n = 2) experienced a complication. The same proportion of women experienced a complication among the 1389 women who had a procedure provided by a physician (n = 2). There was no difference between provider types in the risk of complications (RR 0.99, 95% CI 0.17 to 5.70) (Analysis 1.3).
1.3. Analysis.
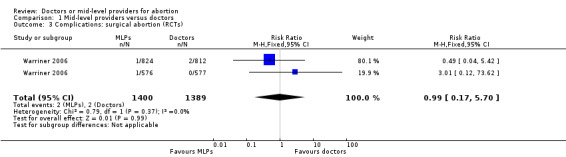
Comparison 1 Mid‐level providers versus doctors, Outcome 3 Complications: surgical abortion (RCTs).
In the three cohort studies that reported complications independently from failure, 6654 women had an abortion procedure provided by a mid‐level provider. The proportion of those who experienced a complication in this group was 1.0% (n = 68). Among the 7061 women who had a procedure provided by a physician, 0.7% (n = 49) experienced a complication. There was no significant difference between procedures provided by mid‐level providers and those provided by doctors in the risk of complications (pooled RR 1.38, 95% CI 0.70 to 2.72) (Analysis 1.4).
1.4. Analysis.
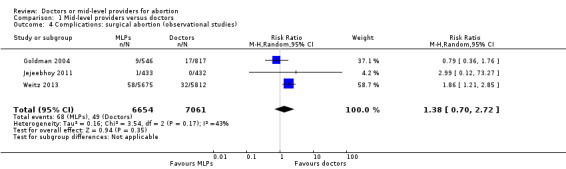
Comparison 1 Mid‐level providers versus doctors, Outcome 4 Complications: surgical abortion (observational studies).
Total complications (incomplete or failed abortion and complications)
Total complications included failure and incomplete abortion, retention of products of pregnancy, haematometra, haemorrhage, endocervical injury, anaesthesia‐related reactions, uterine perforation, infection, injury to the bowel, any complication requiring blood transfusion and any complication requiring hospitalisation.
In the RCT, data for total complications were available for 1400 women who had procedures administered by mid‐level providers. The proportion of total complications among this group was 1.3 % (n = 18) for surgical abortion (Warriner 2006). Among the 1389 women who had abortion procedures provided by physicians in these trials, the proportion of total complications was 0.7% (n = 10) for surgical procedures (RR 3.07, 95% CI 0.16 to 59.08) (Analysis 1.5).
1.5. Analysis.
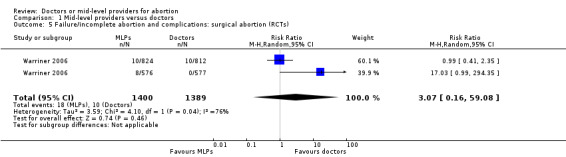
Comparison 1 Mid‐level providers versus doctors, Outcome 5 Failure/incomplete abortion and complications: surgical abortion (RCTs).
In the four cohort studies of surgical abortion, the proportion of total complications among women who had a procedure administered by a mid‐level provider (n = 7939) was 1.9%. Among the 8234 women who had a procedure provided by a physician, the proportion of women who experienced failure or complication was 1.3%. There was no significant difference in the risk of failure or complication among women who had a procedure provided by a mid‐level provider compared with those who had a procedure administered by a physician (pooled RR 1.36, 95% CI 0.86 to 2.14) (Analysis 1.6).
1.6. Analysis.
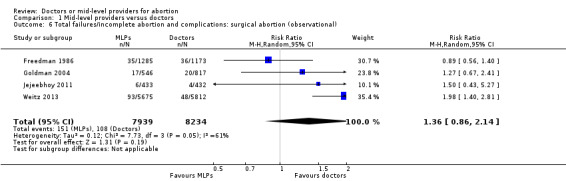
Comparison 1 Mid‐level providers versus doctors, Outcome 6 Total failures/incomplete abortion and complications: surgical abortion (observational).
Medical abortion
Failure/incomplete abortion
Failure or incomplete abortion was defined by two studies as the need for surgical evacuation. One study defined failure as urinary human chorionic gonadotropin (hCG) greater than 500 IU/ml three weeks following medical abortion (Kopp Kallner 2015).
RCT data for failure of medical abortion or incomplete abortion were derived from two studies (Kopp Kallner 2015; Warriner 2011). Among the 977 women who had a medical abortion administered by a mid‐level provider, 2.7% (n = 26) experienced failed/incomlpete abortion. Among the 915 women who had a medical abortion administered by a physician, 3.3% (n = 30) experienced failure or incomplete abortion. There was no significant difference in the risk of failure or incomplete abortion between mid‐level provider and physician‐administered procedures (pooled RR 0.81, 95% CI 0.48 to 1.36) (Analysis 1.7).
1.7. Analysis.
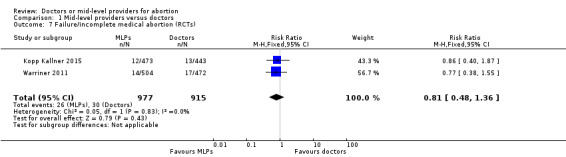
Comparison 1 Mid‐level providers versus doctors, Outcome 7 Failure/incomplete medical abortion (RCTs).
One cohort study reported data for failure of medical abortion (Jejeebhoy 2012). Among the 775 women who had a mid‐level provider‐administered medical abortion, 5.0% (n = 39) experienced failure. Among the 389 women who had a physician‐administered procedure, 4.6% (n = 18) experienced failureor incomplete abotion. There was no significant difference between mid‐level provider and physician‐administered procedures in the risk of failure or incomplete abortion (RR 1.09, 95% CI 0.63 to 1.88) (Analysis 1.8).
1.8. Analysis.
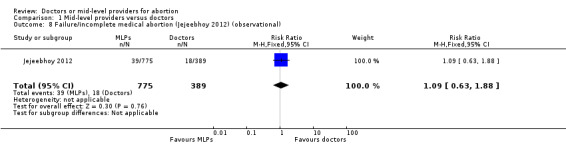
Comparison 1 Mid‐level providers versus doctors, Outcome 8 Failure/incomplete medical abortion (Jejeebhoy 2012) (observational).
Complications
Complications of abortion included haematometra, haemorrhage, endocervical injury, anaesthesia‐related reactions, uterine perforation, infection, injury to the bowel, any complication requiring blood transfusion and any complication requiring hospitalisation. For all three medical abortion studies, there were no reported complications for either mid‐level provider administered or physician administered medical abortions.
Discussion
Summary of main results
There is some evidence of an increase in the risk of failure or incomplete abortion for surgical abortion procedures provided by mid‐level providers (pooled risk ratio (RR) 2.25, 95% confidence interval CI 1.38 to 3.68), however the absolute risk is small and the data come from only three cohort studies. We rated the quality of the body of evidence as very low. There is no evidence of a statistically significant difference in the risk of total complications (which includes abortion failure, complications alone, immediate complications or delayed complications) when surgical abortion is provided by mid‐level providers. There is no statistically significant evidence of a difference in the risk of failure of medical abortion between mid‐level providers and physicians. Our results suggest that medical abortion can be carried out safely and effectively by mid‐level providers.
Overall completeness and applicability of evidence
The findings from this review are only applicable to pregnancies up to nine weeks for medical abortion and up to 14 weeks for surgical procedures. The findings from the medical abortion studies cannot be generalised to settings where a misoprostol‐only regimen is used to induce abortion and is limited to settings involving the specific regimens used in these studies. This review focuses on clinical measures of effectiveness and safety as the outcomes. Assessment of feasibility and acceptability, and barriers to the use of mid‐level provision, were beyond the scope of this review, however recent findings from India and Nepal suggest that mid‐level providers found task‐shifting of medical abortion provision to mid‐level providers to be acceptable (Acharya 2014), and women are happy with the service provided (Puri 2014).
'Mid‐level provider' is a broad term that is currently used by the World Health Organization (WHO) to describe any trained practitioner who is not a physician (Brown 2011). We recognise that concerns have been raised that the term 'mid‐level' implies that these clinicians provide a lower level of service to physicians; however, to be consistent with the WHO terminology, we have used the term when referring to these providers collectively.
We were unable to perform an analysis of subtypes of mid‐level providers due to the heterogeneity of the training for provider types in different settings (Mullan 2007). In addition, the role that mid‐level providers played in the intervention varied between studies. By including a broad range of mid‐level providers in our review, we may be masking important differences between provider types by lumping them together. We recommend that future studies are carried out to establish the safety and effectiveness of subtypes of mid‐level providers performing all aspects of the abortion procedure. An addition, the minimum required training and clinical experience for each subtype of mid‐level provider should be established to enable better informed policy.
Although a large number of women were included in these studies, relatively few providers have been included. In order to improve the evidence base for the provision of abortion procedures by mid‐level providers, future studies should endeavour to include larger numbers of providers.
Half of the studies included in the review were carried out in developing country settings (Jejeebhoy 2011; Jejeebhoy 2012; Warriner 2006; Warriner 2011); however, only one trial was carried out in a rural developing country setting (Warriner 2011). The surgical trial conducted in South Africa and Vietnam took place in Marie Stopes International (MSI) clinics, which serve a population that is slightly more educated and well‐off than clients in the public sector (Warriner 2006). Both of the Indian studies took place in urban settings in non‐governmental organisation (NGO) clinics (Jejeebhoy 2011; Jejeebhoy 2012). As a result of this, women in these studies may not be representative of women who attend public clinics in developing country settings or rural women in these countries. Only the Nepali medical abortion trial was carried out in rural areas in a developing country setting (Warriner 2011). The training of mid‐level providers to provide abortion procedures aims to address shortages of trained physicians, particularly in rural areas (Berer 2009). As rural settings may pose different challenges for mid‐level providers carrying out abortion procedures, such as a lack of access to primary care facilities for the management of complications, we recommend that future studies investigate the safety and effectiveness of the provision of surgical abortion procedures by mid‐level providers and doctors in rural developing country settings.
In the Nepali medical abortion study, the participants' demographic data were similar to the socio‐demographic characteristics of women typically seeking abortions in Nepal, suggesting that the data are generalisable to Nepal. In addition, the trial was carried out in low‐resource settings in rural areas where mid‐level providers are more numerous and available than physicians (Warriner 2011). These results suggest that the training of mid‐level providers for medical abortion could be scaled up in Nepal in order to address shortages in the provision of safe abortion. However, caution should be applied in the interpretation of data that come from trial conditions, therefore scaling up should be closely monitored for safety and effectiveness.
Due to the shortage of physicians, mid‐level providers are often the only health professionals available in many settings. Given the potential to expand women's access to safe abortion in underserved areas, mid‐level provision has been widely advocated (Chong 2006; IPAS 2002; Samora 2007). Training mid‐level providers to provide first‐trimester medical abortion and surgical abortion up to 12 weeks could facilitate widened access to safe termination, with the potential to reduce the number of unsafe abortions and related deaths and disabilities.
There is a significant difference in the risk of failure/incomplete abortion(P value = 0.002) between mid‐level providers and physicians for surgical abortion, but the effect is small. The results suggest that for every 1000 procedures administered by a mid‐level provider, an additional four women (95% confidence interval (CI) 1 to 9) will experience abortion failure or incomplete abortion. However, in the context of settings with a shortage of physicians and a high incidence of unsafe abortion procedures, the potential health gains associated with mid‐level provision of abortion are substantial. The current WHO unsafe abortion statistics estimate that 22 million unsafe abortions take place every year, resulting in five million complications (a 23% complication rate) and 47,000 deaths (Sedgh 2012). Even based on the assumption (from surgical abortion randomised controlled trials (RCTs)) that the total complication rate for procedures carried out by mid‐level providers is as high as 22/1000, if all unsafe abortions were carried out by mid‐level providers, there could be a 90% reduction in complications and far fewer deaths (Chong 2006). A change in policy that allows mid‐level providers to carry out abortion procedures may not achieve the theoretical reduction of 90% of complications, but it will contribute to a reduction in the number of complications and deaths caused by a lack of access to safe abortion. Compared to the other potential complications that can occur, abortion failure is not life‐threatening in the majority of cases and its treatment and management falls within the scope of the same providers.
There is no significant difference in the risk of immediate complications between abortion procedures provided by mid‐level providers and those provided by physicians. In the context of a developing country setting, where mid‐level providers are likely to be operating with limited support, these results are encouraging.
Adequate training and infrastructure are likely to be central to the delivery of effective and safe abortion. The mid‐level providers in the studies included in this review were trained nurses, physician assistants and midwives, who had experience in abortion procedures or who were supervised by a qualified provider. National reproductive health programmes need to evaluate how training should be structured and implemented. Additionally, operational research studies are needed to identify other types of mid‐level provider and to assess the feasibility and acceptability of rolling out mid‐level provision. Evaluations should also consider the structure of the wider healthcare system and the availability of personnel, to identify which mid‐level providers are best placed to provide abortion procedures and should also consider how the process from pre‐ to post‐abortion care is managed.
Quality of the evidence
According to the GRADE system (Higgins 2011), the majority of the evidence is of low or very low quality. This is due to the majority of data being derived from non‐randomised, observational studies. We considered the body of evidence derived from RCTs of surgical abortion to be of low quality due to inconsistencies between results across studies. We considered the body of evidence on medical abortion, which was derived from RCTs, to be of high quality. However, these data come from a single study, therefore assessment of inconsistency was not possible (Table 1; Table 2).
A concern from the body of evidence derived from the cohort studies is selection bias due to unconcealed allocation or different eligibility criteria in study arms, which could lead to systematic differences in participant characteristics in the intervention groups. This is problematic when these participant characteristics may be associated with abortion outcomes, leading to differences between the two groups that cannot be attributed solely to the intervention. These differences were only reported in one of the observational studies, where participants were from different US states (Goldman 2004). The remaining four observational studies reported similarities between the two groups of participants.
The studies included in this review did not blind either participants or outcome assessors. Although the reasons for this were not explicitly stated we expect that this results in increased validity of the body of evidence as this is consistent with non‐trial conditions.
This review assesses the safety and efficacy of mid‐level provision of abortion services. Efficacy is reflected in the number of complete abortions, therefore the primary outcome is defined as ongoing pregnancy or incomplete abortion at follow‐up. Further sub‐analysis of ongoing pregnancy was not possible for surgical abortion studies as only two studies separately reported ongoing pregnancy and incomplete abortion in their results (Goldman 2004; Weitz 2013). In the medical abortion studies included in this review, efficacy was reflected by the number of complete abortions. These studies counted incomplete abortion and ongoing pregnancy as failures. Therefore, we used the same definitions to align with these studies when pooling the results to determine efficacy.
Potential biases in the review process
We minimised bias by conducting a thorough search in the databases and by contacting the authors of studies for further information. Our search process was able to identify foreign language studies that were indexed in English; however, we did not search any foreign language databases.
The review was limited due to having only eight included studies, only three of which were randomised controlled trials. As a result of the different study designs, we carried out analysis of RCTs independently of cohort studies.
Agreements and disagreements with other studies or reviews
The systematic review that this Cochrane review updates reported similar results (Ngo 2013), as did a similar review published in 2012 (Renner 2012). The present study has expanded on this published review by including more recent findings from settings where there is a shortage of providers and a high incidence of unsafe abortions. These are the settings in which the implementation of mid‐level provision of abortion is likely to be a priority. Future studies should also evaluate the feasibility of introducing mid‐level provision in these settings.
Authors' conclusions
Implications for practice.
Our findings suggest that mid‐level providers can provide medical abortion safely and effectively. Based on a small number of studies, there may be some difference in the effectiveness of surgical abortion procedures performed by mid‐level providers compared with physicians, however we cannot be sure. Observational data indicate that there may be a higher risk of abortion failure for surgical abortion procedures administered by mid‐level providers, but the number of studies is small and more robust data from controlled trials are needed. There is no significant difference in the risk of complications when surgical abortions are provided by mid‐level providers. If these findings are confirmed in further studies, in settings with a shortage of trained providers coupled with a high incidence of unsafe abortion, mid‐level provision of terminations could potentially reduce complications and death related to unsafe abortion.
Implications for research.
Further studies are required to establish the minimum level of provider training and experience required for safe and effective abortion procedures in both low and high‐resource settings.
Acknowledgements
This protocol was reviewed by three editors of the Cochrane Fertility Regulation Group as part of the peer review process.
The authors acknowledge funding support from the STEP UP (Strengthening Evidence for Programming on Unintended Pregnancy) Research Programme Consortium. STEP UP is funded by UK aid from the Department for International Development.
Appendices
Appendix 1. MEDLINE via Pubmed search strategy
Search 1
All fields: (Nurses"[Mesh] OR "Physician Assistants"[Mesh] OR "mid‐level provider"[text word] OR "mid‐level providers"[text word] OR nurse*[text word] OR midwife*[text word] OR midwives[text word] OR "nurse practitioner"[text word] OR "nurse practitioners"[text word] OR "physician assistant"[text word] OR "physician assistants"[text word] OR "non‐physician"[text word] OR "non‐physicians"[text word] OR "substitute health worker"[text word] OR "substitute health workers"[text word] OR auxiliar*[text word]) AND ("Abortion, Incomplete"[Mesh] OR "Abortion, Induced"[Mesh:noexp] OR "Abortion, Legal"[Mesh] OR "Abortion, Therapeutic"[Mesh:noexp] OR abortion*[text word])
Search results were restricted to studies published after 1980 through to August 15 2014.
We placed no limits on language.
Replicated PubMed Strategy in Cochrane CENTRAL: 24 unique citations
Appendix 2. POPLINE search strategy
Search 1: 193
All fields: ("mid‐level provider" OR "mid‐level providers" OR nurse* OR midwife* OR midwives OR "nurse practitioner" OR "nurse practitioners" OR "physician assistant" OR "physician assistants" OR "non‐physician" OR "non‐physicians" OR "substitute health worker" OR "substitute health workers"OR auxiliar*) AND abortion*
Search 2: 141 citations
All fields: "mid‐level provider" OR "mid‐level providers" OR nurse* OR midwife* OR midwives OR "nurse practitioner" OR "nurse practitioners" OR "physician assistant" OR "physician assistants" OR "non‐physician" OR "non‐physicians" OR "substitute health worker" OR "substitute health workers"OR auxiliar*
AND
Keywords: abortion
Search 3: 79 citations
All Fields: abortion*
AND
Keywords (MIDWIVES AND MIDWIFERY OR Traditional Birth Attendants OR PARAMEDICAL PERSONNEL OR Nurses and Nursing OR Nurse‐Midwives)
Unique citations from Popline from 1980 through to August 15 2014
We deleted duplicated using EndNote and then removed citations older than 1980.
Data and analyses
Comparison 1. Mid‐level providers versus doctors.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Failure/incomplete surgical abortion (RCTs) | 1 | 2789 | Risk Ratio (M‐H, Random, 95% CI) | 2.97 [0.21, 41.82] |
| 2 Failure/incomplete surgical abortion (observational studies) | 3 | 13715 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.25 [1.38, 3.68] |
| 3 Complications: surgical abortion (RCTs) | 1 | 2789 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.17, 5.70] |
| 4 Complications: surgical abortion (observational studies) | 3 | 13715 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [0.70, 2.72] |
| 5 Failure/incomplete abortion and complications: surgical abortion (RCTs) | 1 | 2789 | Risk Ratio (M‐H, Random, 95% CI) | 3.07 [0.16, 59.08] |
| 6 Total failures/incomplete abortion and complications: surgical abortion (observational) | 4 | 16173 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.86, 2.14] |
| 7 Failure/incomplete medical abortion (RCTs) | 2 | 1892 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.48, 1.36] |
| 8 Failure/incomplete medical abortion (Jejeebhoy 2012) (observational) | 1 | 1164 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.63, 1.88] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Freedman 1986.
| Methods | 24‐month cohort study There was no differential allocation of patients between provider types. A patient could request a particular provider if she desired. Less than 5% of clinic patients availed themselves of this option |
|
| Participants | 2458 participants completed the study All women who obtained abortions from a physician or a physician assistant at the Vermont Women's Health Center during the 2‐year period from1 January 1981 through 31 December 1982 Gestation assessed by pelvic estimate Contraindications included uterine sizing beyond 12 weeks gestation, current use of anticoagulants, haematocrit less than 30%, prolonged bleeding time and active pelvic inflammatory disease. Only procedures utilising local anaesthetics were performed at this clinic |
|
| Interventions | Physicians and physician assistants performed early uterine evacuation or suction curettage at a Women's Health Center in Vermont Women arriving at the clinic were seen by the next available provider and were followed up within 4 weeks of the procedure MLPs worked independently to carry out abortions within the same site where physicians were working |
|
| Outcomes | Complication rates Complications were placed into 1 of 7 categories: ‐ Uterine haemorrhage or "excessive bleeding", as determined by patient estimate (soaking 2 or more pads per hour for 4 to 6 hours) ‐ Uterine perforation ‐ Cervical laceration ‐ Incomplete abortion or retained products of conception ‐ Infection (fever 100.4 °F or higher on 2 readings and definite uterine tenderness) ‐ Post‐abortion syndrome ‐ Vagal reaction (rapid drop in blood pressure followed by a short loss of consciousness) Each complication was further classified as either immediate or delayed Immediate complications were defined as those evident before the patient was discharged from the clinic on the day of her procedure, while delayed complications were those noted within the 4‐week post‐abortion period |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No random sequence generation. Women were seen by the next available provider. However, only 5% of women opted for a physician. The author states that randomisation could have been natural |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The participant was aware of the provider type. We do not consider this to be a bias because this is part of the intervention. If MLPs are to perform abortion procedures outside of study conditions, we would expect patients to be aware of the provider type. We therefore do not consider the lack of blinding to provider type to bias the results of the study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 96% follow‐up – no difference stated between groups |
| Selective reporting (reporting bias) | Unclear risk | Not available |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Goldman 2004.
| Methods | 2‐year cohort study of women undergoing surgically induced abortion in 2 clinics | |
| Participants | 1393 women completed the study The study was carried out in the USA – in New Hampshire and Vermont clinic facilities All women who underwent an outpatient surgical abortion performed by a physician at the Feminist Health Center of Portsmouth, New Hampshire, or by a physician assistant at the Vermont Women's Health Center in Burlington, Vermont, between July 1996 and October 1997 were eligible There were no restrictions on gestational age but the majority were in the 1st trimester |
|
| Interventions | Physicians with at least 5 years experience in abortion procedures performed standard vacuum curettage procedures for pregnancies up to 12 weeks gestation at a clinic in New Hampshire Physician assistants with the same level of experience provided MVA or standard vacuum curettage procedures for pregnancies up to 14 weeks gestation at a clinic in Vermont Follow‐up was within 14 days of the procedure |
|
| Outcomes | Complications: Complications were defined according to National Abortion Federation guidelines as follows: ‐ Incomplete abortion, in which tissue from the pregnancy remains in the uterus, requiring a repeat abortion ‐ Failed abortion (continued pregnancy), in which the abortion does not end the pregnancy, requiring a repeat abortion ‐ Ectopic/extrauterine pregnancy, in which the signs and symptoms of pregnancy continue after abortion but no intrauterine pregnancy is detected ‐ Perforation, a condition in which a puncture or tear in the wall of the uterus or other organ is present ‐ Cervical laceration, a condition in which a tear in the cervix is present, requiring either sutures or vaginal packing ‐ Infection, which is detected by a temperature elevated to 100.4 °F or 38.0 °C, lower abdominal pain or tenderness, and abnormal cervical discharge ‐ Haemorrhage, defined as blood loss estimated as 500 cc or greater (defined as bleeding that was heavier than the heaviest day of a normal menstrual period or that soaked through more than 1 sanitary pad per hour), which is caused by failure of the uterus to contract and may require a blood transfusion ‐ Other complications, including shock, coma, amniotic fluid embolism, anaesthesia‐related Complications were further classified as either immediate or delayed Immediate complications were defined as those that occurred during the procedure or before discharge from the clinic. Delayed complications were those that occurred up to 2 weeks after discharge difficulties, and death |
|
| Notes | All procedures performed by the physicians in New Hampshire were standard vacuum curettage, whereas more than half of the physician assistant procedures (virtually all of those performed at 8 weeks gestation or earlier) were manual vacuum curettage The cannula sizes used by the 2 clinics differed. In Vermont, 95% of the manual vacuum curettage procedures performed at 8 weeks gestation or earlier were performed with a 5 mm or 6 mm cannula. By contrast, in New Hampshire 96% of the standard vacuum curettage procedures performed at 8 weeks gestation or earlier were performed with a 7 mm, 8 mm or 9 mm cannula |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | None. 2 clinics in 2 different US states: providers in New Hampshire were physicians, providers in Vermont were physician assistants. Characteristics of the participants differed between the 2 settings |
| Allocation concealment (selection bias) | High risk | None |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The participant was aware of the provider type. We do not consider this to be a bias because this is part of the intervention. If MLPs are to perform abortion procedures outside of study conditions, we would expect patients to be aware of the provider type. We therefore do not consider the lack of blinding to provider type to bias the results of the study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | None |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 28.5% loss to follow‐up – delayed complication data are likely to be affected |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | High risk | Physician assistants and physicians differed in the methods of abortion used Clinician training varied between clinics |
Jejeebhoy 2011.
| Methods | Cohort study The study was located in 5 clinics in Bihar and Jharkhand, 2 poorly developed states of India, in which access to health services is limited |
|
| Participants | 865 women completed the study Eligibility: Positive uterine pregnancy of ≤ 10 weeks gestational age; no attempts in the previous week to terminate the current pregnancy; resided within an hour of the study; willing to return 7 days later (day 7) for a follow‐up check‐up and undergo 2 pelvic examinations (by the study provider and supervisor); indicated no other contraindications for abortion as per the Government of India guidelines |
|
| Interventions | MVA delivered by nurses or physicians with no previous experience of providing any type of abortion, who underwent MVA training as part of the study All abortion procedures were conducted in the presence of a qualified supervisor Women were followed up after 7 days |
|
| Outcomes | Provider assessment of gestational age Provider assessment of other criteria relating to eligibility Provider assessment of complete abortion Efficacy: complete abortion at day 7 Overall complication rate: including failure (failed abortion and adverse events ‐ blood transfusion, cervical injury, perforation, bowl injury, infection, hospitalisation) |
|
| Notes | Supervisor assessment of outcomes Women attending the clinics were unaware of the type of provider prior to attending the clinic. The authors state that recruitment was naturally random |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No random sequence generation. Providers were assigned to a facility for a certain period of time. Clients who came for an abortion were unaware of the type of clinician who would be providing services on the day of the visit |
| Allocation concealment (selection bias) | High risk | None specified |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The participant was aware of the provider type. We do not consider this to be a bias because this is part of the intervention. If MLPs are to perform abortion procedures outside of study conditions, we would expect patients to be aware of the provider type. We therefore do not consider the lack of blinding to provider type to bias the results of the study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | None specified |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data are balanced in numbers across intervention groups, with similar reasons for missing data across groups |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available – the report alludes to a protocol and summarises it in the methods but there is no published protocol |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Jejeebhoy 2012.
| Methods | Cohort study Carried out over 17 months in 2008‐2010 in Bihar and Jharkhand, India. The study was conducted in 5 NGO clinics |
|
| Participants | 1164 women completed the study Eligibility criteria: The client needed to have a haemoglobin level of at least 9 g/dL, undergo 2 pelvic examinations (by the study provider and verifier) and reside within an hour of the study site; she would be ineligible if, during the past week, she had tried to terminate the pregnancy using medication obtained from a chemist without a prescription. No contraindications to medical abortion regimen |
|
| Interventions | Medical abortion regimen of 200 mg mifepristone orally followed by 400 µg misoprostol orally 2 days later for women up to 8 weeks gestation. The regimen was delivered by ayurvedic physicians, nurses and allopathic physicians in abortion clinics in India. Only providers who had never performed surgical or medical abortion, never conducted pelvic examinations or assessed gestational age were recruited. All underwent identical medical training, which lasted 10 days. Women were followed up after 15 and 21 days (if extended follow‐up was advised) MLPs worked independently, though assessment was verified by a higher level clinician |
|
| Outcomes | Complications: the percentage of women who experienced serious complications or required a blood transfusion or hospitalisation Incomplete abortion on day 15 or 21 The proportion of clients whose eligibility had been incorrectly assessed by their provider (as compared with the verifier), including those who would have wrongly been denied entry into the study and those who would have been wrongly recruited. The proportion of study participants whose abortion completeness status was incorrectly assessed by the study provider |
|
| Notes | Supervisors assessed providers' accuracy of assessing eligibility and abortion completeness | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study was not a randomised controlled trial, as clients were not randomly assigned to a particular type of provider. Providers were assigned to a facility for a certain period of time. Clients who came for an abortion were unaware of the type of clinician who would be providing services on the day of the visit or the type of physicians who would succeed the current provider, as there was no particular sequence |
| Allocation concealment (selection bias) | High risk | None |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The participant was aware of the provider type. We do not consider this to be a bias because this is part of the intervention. If MLPs are to perform abortion procedures outside of study conditions, we would expect patients to be aware of the provider type. We therefore do not consider the lack of blinding to provider type to bias the results of the study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | None |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The confidence intervals for the differences in loss to follow‐up fell within the predetermined margin of statistical equivalence for each provider type, both for day 3 and for day 15 or 21 |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Unclear risk | A break in recruitment due to unavailable study providers produced a long study period |
Kopp Kallner 2015.
| Methods | Randomised controlled trail Carried out in 2011‐2012 in Sweden in an outpatient family planning clinic Women who made an appointment by calling the clinic by telephone were informed about the study and invited to participate |
|
| Participants | Women were eligible to participate if they: had a gestation of 63 days or less according to their last menstrual period; were 18 years or older; had no contraindication for medical abortion; were in good general health; were not taking any continuing medication for chronic disease | |
| Interventions | 2 nurse midwives experienced in medical abortion and contraceptive counselling received theoretical and practical training in vaginal ultrasound examination of early pregnancy These nurse midwives were the sole providers in the nurse midwife arm There were a total of 34 doctors with varying levels of training and experience in the standard care arm Women randomised to the nurse‐midwife arm were counselled, examined, informed and treated by a single nurse midwife. Nurse‐midwives in this arm did not perform any other tasks during the study period Women randomised to the standard care arm were examined and counselled by the doctor and then received additional information about the practical details and medication from a nurse midwife, according to clinical routine All women received 200 mg of mifepristone in the clinic Women then had the choice of receiving 800 µg of misoprostol vaginally at home or in the clinic 24 to 48 hours after mifepristone administration. If no bleeding occurred within 3 hours, women were instructed to take an additional dose of 400 µg of misoprostol orally Women were followed up after 3 weeks and given a urinary hCG test. If the results were positive a serum hCG test was performed and they were referred for evaluation with vaginal ultrasound Complications were followed up for 6 weeks MLPs and doctors worked at the same site |
|
| Outcomes | The primary outcome was efficacy, defined as the need for surgical intervention Secondary outcomes: Safety, defined as no complications up to 6 weeks after the procedure Hospitalisation or blood transfusion Acceptability, defined as women preferring their allocated provider Outcomes were assessed by questionnaires at follow‐up visit |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The participant was aware of the provider type. We do not consider this to be a bias because this is part of the intervention. If MLPs are to perform abortion procedures outside of study conditions, we would expect patients to be aware of the provider type. We therefore do not consider the lack of blinding to provider type to bias the results of the study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low loss to follow‐up, similar in each group |
| Selective reporting (reporting bias) | Low risk | Protocol made available prior to study |
| Other bias | Unclear risk | No other bias detected |
Warriner 2006.
| Methods | Randomised controlled trial The study was carried out in South Africa from September 2003 to June 2004 and in Vietnam from May to December 2003 Randomisation was done separately for each clinic using a block design with about 600 women in each centre and a ratio of 1:1 for doctors and MLPs. The random allocation sequence was generated using SAS by a data management team at WHO in Geneva, Switzerland Sealed, opaque envelopes containing the random allocation of the type of provider were sequentially numbered and were opened when written informed consent had been provided Women were not blinded to their provider type |
|
| Participants | 1153 women completed the study in South Africa. All women presenting for an abortion at 2 MSI clinics in the Western Cape Province and 2 MSI clinics in KwaZulu Natal province were invited to take part if they met the eligibility criteria 1636 women completed the study in Vietnam. All women presenting for an abortion at 4 MSI clinics in Ha Tinh, Ho Chi Minh City, Nghe An and Thai Binh were invited to take part in the study if they met the eligibility criteria Clinics in both countries were located in urban and peri‐urban areas and served mainly lower middle‐class women Eligibility criteria: All women who presented for a first‐trimester abortion during the study period were informed of the study and invited to participate Women met medical eligibility criteria if they were: at least 18 years old; the gestational age of the pregnancy was less than 12 completed weeks as estimated by pelvic examination and date of last menstrual period Data from ultrasound examinations, done routinely at MSI clinics, were also obtained to ensure that eligibility criteria were met Additional eligibility criteria were: residence within a specified geographical area; willingness to be randomly assigned to a provider; willingness to return to the clinic for follow‐up or to be interviewed at home (or another mutually agreed upon location) or by telephone, 10 to 14 days after the abortion. Additionally, women were required to provide written informed consent Gestation < 12 weeks assessed by ultrasound |
|
| Interventions | MVA delivered by MLPs with government‐accredited training in abortion, and those administered by physicians. All participants were offered lidocaine and additional oral analgesia; in one of the study locations (South Africa), misoprostol 400 mg was administered 2 to 3 hours before the procedure (reference). Women were followed up 10 to 14 days after the procedure MLPs and doctors worked at the same site |
|
| Outcomes | Compared outcomes of MVA procedures for pregnancies up to 12 weeks gestation delivered by MLPs with government‐accredited training in abortion and those procedures administered by physicians Abortion complications (i) Collected at the time of abortion/before leaving clinic and at follow‐up 10 to 14 days later (ii) Reported: at follow‐up interviews Immediate complications: excess bleeding (> 500 cc) after abortion, cervical injury, confirmed/suspected perforation, adverse drug reaction Delayed complication: retained POC needing re‐evacuation, haematometra, post‐abortion pelvic infection, excessive post‐abortion bleeding (> 500 cc), abortion‐related death Percentage of complication types per group |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate randomisation: "computer generated randomisation list" |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes; opened once written informed consent obtained |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The participant was aware of the provider type. We do not consider this to be a bias because this is part of the intervention. If MLPs are to perform abortion procedures outside of study conditions, we would expect patients to be aware of the provider type. We therefore do not consider the lack of blinding to provider type to bias the results of the studys |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Interviewer was a 3rd party, however they were not blinded to the provider type |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low |
| Selective reporting (reporting bias) | Unclear risk | Pre‐specified outcomes were reported; protocol not published |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Warriner 2011.
| Methods | Randomised controlled trial. Multicentre randomised controlled equivalence trial, which took place over 11 months Sequence generation: Computer‐generated randomisation scheme stratified by study centre with a block size of 6. The random allocation sequence was generated by the use of SAS software (SAS Institute, Cary, NC, USA) Allocation sequence concealment: Sealed, opaque envelopes containing the random allocation were consecutively numbered and were opened and assigned sequentially to women by a research assistant once written informed consent had been obtained Blinding: blinded to research assistant |
|
| Participants | 1032 women completed the study in 5 rural district hospitals in Nepal. Data were collected between 15 April 2009 and 17 March 2010 Eligibility: Providers: only providers trained in manual vacuum aspiration were eligible for medical abortion training Patients: less than 9 weeks (≤ 63 days) of gestation according to date of last menstrual period and as estimated by bimanual pelvic examination, older than 16 years, resided no more than 90 minutes journey from the study clinic and willing to be randomly assigned to a provider, to return to the clinic 10 to 14 days after the start of treatment and to provide written informed consent |
|
| Interventions | Medical abortion regimen of 200 mg mifepristone orally followed by 800 mg of misoprostol vaginally 1 to 2 days later, delivered by MLPs (staff nurses and auxiliary midwives) trained in MVA, or doctors (obstetricians, gynaecologists, general practitioners and other doctors) across 5 district hospitals in Nepal. Women were followed up 10 to 14 days after the procedure MLPs and doctors worked from the same site, though waiting areas and examination rooms were separated to reduce interaction between providers |
|
| Outcomes | The primary endpoint was complete abortion without manual vacuum aspiration within 30 days of treatment Failed abortion (continuing pregnancy) was recorded when clinical examination indicated continuing symptoms of pregnancy and manual vacuum aspiration was needed to terminate the pregnancy Incomplete abortion was defined as products of conception remaining in the uterus with continued bleeding, bulky uterus and open cervix at examination, possibly necessitating surgical evacuation at the discretion of the provider or at the woman's request Women were also asked whether they had visited any non‐study hospital, clinic or provider during the study The secondary endpoint measured case management decisions by recording case management discussion and referrals between providers to assess the extent to which each group provided medical abortion services independently Serious adverse events (haemorrhage necessitating blood transfusion, conditions necessitating hospitalisation) were recorded |
|
| Notes | A limitation of the study is that although separate waiting and examination rooms for the 2 groups were set up for the duration of the study, both types of providers worked in the same hospital and in the same environment. Although this controlled environment optimised comparison, it might have led to a convergence of outcomes that would not have happened if the women had been assigned to providers at different clinics | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generation using SAS |
| Allocation concealment (selection bias) | Low risk | Sequential, sealed, opaque envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The participant was aware of the provider type. We do not consider this to be a bias because this is part of the intervention. If MLPs are to perform abortion procedures outside of study conditions, we would expect patients to be aware of the provider type. We therefore do not consider the lack of blinding to provider type to bias the results of the study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding Outcome was assessed by the same provider type that carried out the abortion – potentially the same provider Observer bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up of women receiving treatment was 24 of 542 (4%) in the mid‐level health care providers group and 19 of 535 (4%) in the doctors group. Women lost to follow‐up were, on average, less educated than those followed up. Two women in the doctors group were excluded from the analysis because at follow‐up they were shown not to have been pregnant: one was a long‐time user of a 3‐monthly injectable contraceptive, and the other one had had a manual vacuum aspiration 37 days before |
| Selective reporting (reporting bias) | Unclear risk | Protocol not published |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Weitz 2013.
| Methods | Cohort study carried out over 4 years in California, USA | |
| Participants | 11,487 women completed the study. The study was carried out in a private facility hospital and private clinic in California, USA between August 2007 and August 2011 Eligibility: Aged 16 years or older (18 years at Planned Parenthood affiliates), seeking a first trimester aspiration abortion (facilities self defined this as < 12 or < 14 weeks gestation by ultrasound), could speak English or Spanish Patients were excluded if they requested general anaesthesia or did not meet the health‐related criteria (unexplained historical, physical or laboratory findings or known or suspected cervical or uterine abnormalities) |
|
| Interventions | In this prospective, observational cohort study, NPs, CNMs and PAs from 5 partner organisations (4 Planned Parenthood affiliates and KPNC) The study compared complication rates within 4 weeks of aspiration abortion for nurse practitioners, certified nurse midwives and physician assistants to those of physicians. Providers were trained to competency in the provision of aspiration abortion (a minimum of 40 procedures over 6 clinical days, with competence assessed by an authorised physician trainer) and had a California professional licence and basic life support. Providers performed aspiration abortion on participants with < 14 weeks gestation. Follow‐up was within 4 weeks of procedure MLPs and doctors worked from the same site |
|
| Outcomes | The primary outcome was the difference in the incidence of complications within 4 weeks of the aspiration abortion between NPs, CNMs and PAs and physicians Complications were categorised as immediate (occurring before leaving the facility) and delayed (occurring < 4 weeks after the procedure) Complications were classified as major if the patient required hospital admission, surgery or a blood transfusion and minor if they were treated at home or in an outpatient setting |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No random sequence generation, however a lack of randomisation was adjusted for in analysis using propensity score matching |
| Allocation concealment (selection bias) | High risk | None |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The participant was aware of the provider type. We do not consider this to be a bias because this is part of the intervention. If MLPs are to perform abortion procedures outside of study conditions, we would expect patients to be aware of the provider type. We therefore do not consider the lack of blinding to provider type to bias the results of the study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | A further limitation of the study is that the health care provider who initially identified a complication was not blinded to the type of provider who performed the abortion |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 30% loss to follow‐up Complications between groups compared "Although postprocedure complications may have been missed among patients for whom we did not have follow‐up data, given the nondifferential follow‐up rates between provider groups, we would expect unidentified complications to be equally distributed between groups, leaving the risk difference unaffected." |
| Selective reporting (reporting bias) | Low risk | Protocol published |
| Other bias | Low risk | The study appears to be free of other sources of bias |
CNM: certified nurse midwife hCG: human chorionic gonadotropin KPNC: Kaiser Permanente of Northern California MLP: mid‐level provider MSI: Marie Stopes International MVA: manual vacuum aspiration NGO: non‐governmental organisation NP: nurse practitioner PA: physician assistant POC: products of conception WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Donovan 1992 | Narrative piece on physician assistants performing abortions and training residents |
| Igberase 2008 | Descriptive study of complications of abortion; no comparison group |
| IPPF 2001 | No comparison group |
| Neustatter 1980 | No comparison group |
| Shaikh 2010 | Analysis of hospital‐based data quantifying unsafe abortion |
| Shamash 2002 | Commentary piece |
Characteristics of studies awaiting assessment [ordered by study ID]
Safe Motherhood 1992.
| Methods | Title could not be retrieved |
| Participants | Title could not be retrieved |
| Interventions | Title could not be retrieved |
| Outcomes | Title could not be retrieved |
| Notes | Title could not be retrieved |
Differences between protocol and review
Types of Participants, was amended to state that women seeking abortions should be "gestational age less than 14 weeks for surgical abortion and less than nine weeks for medical abortion".
Types of Intervention, was amended to provide the following specific description of mid‐level providers; "Mid‐level providers included nurses, nurse practitioners, ayurvedic practitioners, physician assistants, midwives, auxiliary nurse midwives and certified nurse midwives. Mid‐level providers worked independently when carrying out the abortion procedure".
Types of Outcome Measures was amended to include a new ‘secondary outcome’:“Total complications (incomplete or failed abortion and complications)”.
Subgroup analysis’: Not all subgroup analyses were performed. Subgroup analysis of MLP type could not be performed due to heterogeneity between MLP types. Subgroup analysis of healthcare setting was not carried out due to heterogenity between healthcare settings.
Contributions of authors
Drafting the protocol: Sharmani Barnard (SB), Caron Kim (CK). Study selection: SB, CK. Extracting data from studies: SB, CK. Entering data into Review Manager: SB, CK. Carrying out the analysis: SB, CK. Interpreting the analysis: SB, CK, Min Hae Park (MHP), Thoai Ngo (TN). Drafting the final review: SB, CK. Disagreement resolution: MHP, TN. Updating the review SB, CK.
Sources of support
Internal sources
-
Marie Stopes International, UK.
Funding of the study and administrative support
External sources
-
David Geffen School of Medicine UCLA, USA.
Provision of literature
-
STEP UP (Strengthening Evidence for Programming on Unintended Pregnancy) Research Programme Consortium , Other.
The authors acknowledge funding support from the STEP UP (Strengthening Evidence for Programming on Unintended Pregnancy) Research Programme Consortium. STEP UP is funded by UK aid from the Department for International Development
Declarations of interest
Sharmani Barnard: nothing to declare. Caron Kim: nothing to declare. Min Hae Park: nothing to declare. Thoai D. Ngo: nothing to declare.
New
References
References to studies included in this review
Freedman 1986 {published data only}
- Freedman MA, Jillson DA, Coffin RR, Novick LF. Comparison of complication rates in first trimester abortions performed by physician assistants and physicians. American Journal of Public Health 1986;76(5):550‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goldman 2004 {published data only}
- Goldman MB, Occhiuto JS, Peterson LE, Zapka JG, Palmer RH. Physician assistants as providers of surgically induced abortion services. Research and Practice 2004;94(8):1352‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jejeebhoy 2011 {published data only}
- Jejeebhoy SJ, Kalyanwalaa S, Zaviera AJF, Kumara R, Mundleb S, Tankc J, et al. Can nurses perform manual vacuum aspiration (MVA) as safely and effectively as physicians? Evidence from India. Contraception 2011;84:615–21. [DOI] [PubMed] [Google Scholar]
Jejeebhoy 2012 {published data only}
- Jejeebhoy SJ, Kalyanwalaa S, Zaviera AJF, Kumara R, Mundleb S, Tankc J, et al. Feasibility of expanding the medication abortion provider base in India to include ayurvedic physicians and nurses. International Perspectives on Sexual and Reproductive Health 2012;38(3):133‐42. [DOI] [PubMed] [Google Scholar]
Kopp Kallner 2015 {published data only}
- Kopp Kallner H, Gomperts R, Salomonsson E, Johansson M, Marions L, Gemzell‐Danielsson K. The efficacy, safety and acceptability of medical termination of pregnancy provided by standard care by doctors or by nurse midwives: a randomised controlled equivalence trial. BJOG 2015 ; 122 ( 4 ):510‐7. [DOI: 10.1111/1471-0528.12982] [DOI] [PubMed] [Google Scholar]
Warriner 2006 {published data only}
- Warriner IK, Meirik O, Hoffman M, Morroni C, Harries J, My Huong NT, et al. Rates of complication in first‐trimester manual vacuum aspiration abortion done by doctors and mid‐level providers in South Africa and Vietnam: a randomised controlled equivalence trial. Lancet 2006;368:1965‐72. [DOI: 10.1016/S0140-6736(06)69742-0] [DOI] [PubMed] [Google Scholar]
Warriner 2011 {published data only}
- Warriner IK, Wang D, My Huong NT, Thapa K, Tamang A, Shah I, et al. Can midlevel health‐care providers administer early medical abortion as safely and effectively as doctors? A randomised controlled equivalence trial in Nepal. Lancet 2011;377:1155–61. [DOI] [PubMed] [Google Scholar]
Weitz 2013 {published data only}
- Weitz TA, Taylor D, Desai S, Upadhyay UD, Waldman J, Battistelli MF, et al. Safety of aspiration abortion performed by nurse practitioners, certified nurse midwives, and physician assistants under a California legal waiver. Research and Practice 2013;103(3):454‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Donovan 1992 {published data only}
- Donovan P. Vermont physician assistants perform abortions, train residents. Family Planning Perspectives 1992;24(5):225. [PubMed] [Google Scholar]
Igberase 2008 {published data only}
- Igberase GO, Ebeigbe PN. Exploring the pattern of complications of induced abortion in a rural mission tertiary hospital in the Niger Delta, Nigeria. Tropical Doctor 2008;38(3):146‐8. [DOI] [PubMed] [Google Scholar]
IPPF 2001 {published data only}
- International Planned Parenthood Federation (IPPF), South Asia Region. Expanding the role of traditional birth attendants: experiences from South Asia. IPPF, South Asia Region: London, England 2001:44.
Neustatter 1980 {published data only}
- Neustatter PL. Participation of nurses in abortions . Lancet 1980;2(8205):1199‐200. [DOI] [PubMed] [Google Scholar]
Shaikh 2010 {published data only}
- Shaikh Z, Abbassi RM, Rizwan N, Abbasi S. Morbidity and mortality due to unsafe abortion in Pakistan. International Journal of Gynaecology and Obstetrics 2010;110(1):47‐9. [DOI] [PubMed] [Google Scholar]
Shamash 2002 {published data only}
- Shamash J. Abortion: is it a step too far for nurses?. Nursing Times 2002;98(28):12. [PubMed] [Google Scholar]
References to studies awaiting assessment
Safe Motherhood 1992 {published data only}
Additional references
Acharya 2014
- Acharya R, Kalyanwala S. Physicians' and non‐physicians' views about provision of medical abortion by nurses and AYUSH physicians in Maharashtra and Bihar, India. Reproductive Health Matters 2014;Suppl(43):1‐11. [DOI] [PubMed] [Google Scholar]
Berer 2009
- Berer M. Provision of abortion by mid‐level providers: international policy, practice and perspectives. Bulletin of the World Health Organization 2009;87(1):58‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2011
- Brown A, Cometto G, Cumbi A, Pinho H, Kamwendo F, Lehmann U, et al. Mid‐level health providers: a promising resource to achieve the health Millennium Development Goals. Revista P eruana de M edicina Experimental y S alud Pública 2011;28(2):308‐15. [PubMed] [Google Scholar]
Chong 2006
- Chong YS, Mattar CN. Midlevel providers: a safe solution for unsafe abortion. Lancet 2006;368(9551):1939‐40. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
IPAS 2002
- Ipas, IHCAR. Deciding women's lives are worth saving: expanding the role of midlevel providers in safe abortion care. Ipas. Chapel Hill, 2002. [1‐882220‐33‐1]
Jones 2000
- Jones RK, Henshaw SK. Mifepristone for early medical abortion: experiences in France, Great Britain and Sweden. Perspectives on Sexual and Reproductive Health 2000;34(3):154‐61. [PubMed] [Google Scholar]
Kulier 2009
- Kulier R, Cheng L, Fekih A, Hofmeyr GJ, Campana A. Surgical methods for first trimester termination of pregnancy. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD002900] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kulier 2011
- Kulier R, Kapp N, Gülmezoglu AM, Hofmeyr GJ, Cheng L, Campana A. Medical methods for first trimester abortion. Cochrane Database of Systematic Reviews 2011, Issue 11. [DOI: 10.1002/14651858.CD002855.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Long 2001
- Long C, Ren N. Abortion in Cambodia: country report. Expanding Access: Midlevel Providers in Menstrual Regulation and Elective Abortion Care; 2001 Dec 3‐6; South Africa. 2001.
Mullan 2007
- Mullan F, Frehywot S. Non‐physician clinicians in 47 sub‐Saharan African countries. Lancet 2007;370(9605):2158‐65. [DOI] [PubMed] [Google Scholar]
Puri 2014
- Puri M, Tamang A, Shrestha P, Joshi D. The role of auxiliary nurse‐midwives and community health volunteers in expanding access to medical abortion in rural Nepal. Reproductive Health Matters 2014;Suppl (43):1–10. [DOI] [PubMed] [Google Scholar]
Renner 2012
- Renner RM, Brahmi D, Knapp N. Who can provide effective and safe termination of pregnancy care? A systematic review. BJOG 2013;120(1):23‐31. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3 . Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014 .
Samora 2007
- Samora JB, Leslie N. The role of advanced practice clinicians in the availability of abortion services in the United States. Journal of Obstetric, Gynecologic, and Neonatal Nursing 2007;36(7):471‐6. [DOI] [PubMed] [Google Scholar]
Sedgh 2012
- Sedgh G, Singh S, Shah IH, Ahman E, Henshaw SK, Bankole A. Induced abortion: incidence and trends worldwide from 1995 to 2008. Lancet 2012;379(9816):625‐32. [DOI] [PubMed] [Google Scholar]
Strauss 2005
- Strauss SE, Richardson WS, Glasziou P, Haynes RB. Evidence‐based Medicine: How to Practice and Teach EBM. 3rd Edition. Vol. 1, New York : Churchill Livingstone, 2005. [Google Scholar]
WHO 2008
- World Health Organi zation. Task shifting: rational redistribution of tasks among health workforce teams. Global recommendations and guidelines. WHO Press 2008.
WHO 2010
- World Health Organi zation. Mid‐level health providers a promising resource to achieve the health Millennium Development Goals. WHO Press 2010.
WHO 2012
- World Health Organization, Department of Reproductive Health and Research. Safe Abortion: Technical and Policy Guidance for Health Systems. 2nd Edition. Geneva: World Health Organization, 2012. [Google Scholar]
Yarnall 2009
- Yarnall J, Swica Y, Winikoff B. Non‐physician clinicians can safely provide first trimester medical abortion. Reproductive Health Matters 2009;17(33):61‐9. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Barnard 2014
- Barnard S, Kim C, Park MH, Ngo TD. Doctors or Mid‐Level Providers for Abortion. Cochrane Database of Systematic Reviews 2014, Issue 7. [DOI: 10.1002/14651858.CD011242] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ngo 2013
- Ngo TD, Park MH, Free C. Safety and effectiveness of termination services performed by doctors versus midlevel providers: a systematic review and analysis. International Journal of Women's Health 2013;5:9‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]


