Abstract
Over the last year, the coronavirus disease 2019 (COVID-19) pandemic has resulted in profound disruptions across the globe, with school closures, social isolation, job loss, illness, and death affecting the lives of children and families in myriad ways. In an Editors' Note in our June 2020 issue,1 our senior editorial team described this Journal’s role in advancing knowledge in child and adolescent mental health during the pandemic and outlined areas we identified as important for science and practice in our field. Since then, the Journal has published articles on the impacts of the pandemic on child and adolescent mental health and service systems,2, 3, 4, 5 which are available in a special collection accessible through the Journal’s website.6 Alongside many opinion papers, the pace of publication of empirical research in this area is rapidly expanding, covering important issues such as increased frequency of mental health symptoms among children and adolescents3,5,7, 8, 9, 10 and changes in patterns of clinical service use such as emergency department visits.11, 12, 13, 14
As the Senior Editors prepared that Editors’ Note, they were acutely aware that the priorities that they identified were broad and generated by only a small group of scientists and clinicians. Although this had the advantage of enabling us to get this information out to readers quickly, we decided that a more systematic approach to developing recommendations for research priorities would be of greater long-term value. We were particularly influenced by the efforts of the partnership between the UK Academy of Medical Scientists and a UK mental health research charity (MQ: Transforming Mental Health) to detail COVID-19−related research priorities for “Mental Health Science” that was published online by Holmes et al. in The Lancet Psychiatry in April 2020.15 Consistent with its focus on mental health research across the lifespan, several recommendations highlighted child development and children's mental health. However, a more detailed assessment of research priorities related to child and adolescent mental health was beyond the scope of that paper. Furthermore, the publication of that position paper preceded the death of George Floyd at the hands of Minneapolis police on May 25, 2020, which re-energized efforts to acknowledge and to address racism and healthcare disparities in the United States and many other countries.
To build upon the JAACAP Editors’ Note1 and the work of Holmes et al.,15 we conducted an international survey of professionals—practitioners and researchers—working on child and adolescent development and pediatric mental health to identify concerns about the impact of the pandemic on children, adolescents, and their families, as well as what is helping families navigate these impacts, and the specific research topics that are of greatest importance.
Method
Between June 30 and July 26, 2020, participants were recruited through outreach to professional societies, including the American Academy of Child and Adolescent Psychiatry, Royal Australian and New Zealand College of Psychiatry, and social media groups of child development and mental health professionals (eg, The International Association for Child and Adolescent Psychiatry and Allied Professions) around the world to complete a brief online survey. Three open-ended questions covered domains comparable to those in the community survey included in Holmes et al.’s position paper15: 1) what are you most concerned about in terms of the impacts of the COVID-19 pandemic on health, child development, families, and child and adolescent mental health? 2) what do you think has been most helpful to children, adolescents, and families during the course of the pandemic? and 3) what are the top 3 research questions you believe we need to address regarding the pandemic and the mental health of children, adolescents, and their families? The survey also included demographic questions such as age group, gender identity, race, ethnicity, and area of residence. The full survey is included in Supplement 1, available online. This study was determined to be exempt from human subjects regulations by the Colorado Multiple Institutional Review Board.
Responses to the open-ended questions were analyzed using 2 methods. First, we used a commonly used natural language analysis technique, latent Dirichlet allocation-based topic modeling,16 to identify the most common themes for each of the 3 open-ended questions. For the question focused on research priorities, this unsupervised machine learning approach complemented the labor-intensive approach of verifying the most common concerns of our respondents, described below. For each open-ended question, perplexity, a traditional statistic for evaluating topic models, informed the choice of a number of topics, κ. Lower values of perplexity represent a better fit when comparing 2 values of κ. The topics are latent themes that the model estimates best explain all responses to a question. Only topics with a large representation across all responses are reported. For each question, topics are assigned a probability value. This is the likelihood that the topic is represented in responses relative to other topics over the entire response set to a question. All probability values for topics sum to 1, so a probability value for a topic is meaningful only in comparison to all the other topics in the set. For reference, many topics have a probability value near zero (eg, median values ∼.01). Topic modeling was done in MATLAB17 version R2020b using standard procedures in the Text Analytics Toolbox. Code is posted at joelStod/COVIDlda (github.com).
Second, for the open-ended question on research priorities, we identified 7 a priori domains of research (measurement; genetics and epigenetics; biomarkers; neuroscience; prevention, treatment, and service delivery; social determinants of health; and epidemiology). For each of these 7 domains, 2 or more authors conducted a thematic analysis of the open-ended responses to identify specific topics within each domain of research.18, 19, 20 Authors independently coded 50 responses at a time, which they then compared and discussed, building a codebook for each research domain and addressing coding discrepancies. During this coding process, social determinants of health were combined with the epidemiology research domain because of the substantial overlap of identified themes. Biomarkers, genetics, epigenetics, and neuroscience areas were similarly combined. Once agreement was established between coders, the remaining responses were divided across authors, again working in groups of 2 or more to ensure continued discussion and agreement on codes, and coding was completed. There were no responses directly related to measurement.
For both the natural language and thematic analyses, individual participant responses could contribute to more than 1 topic and/or theme. Findings from both analytic approaches are summarized below and include illustrative quotations from survey participants.
Results
A total of 681 participants provided answers to at least 1 of the 3 open-ended questions. Their characteristics are summarized in Table 1 . The majority of participants were between 25 and 50 years old (54%), female (59%), resided in the United States (69%) and in urban areas (54%), and reported that they were completing the survey from the perspective of a mental health care provider (68%). Participant race and ethnicity were queried as open-ended questions, given the international scope of the survey. The majority of participants chose not to respond to the question (65%). Among those who responded, the majority were White (59%).
Table 1.
Participant Characteristics (n = 681)
| Characteristic | Percentage (%) |
|---|---|
| Age (y) | |
| 18-24 | 0.6 |
| 25-50 | 53.5 |
| ≥50 | 46.0 |
| Gender identity | |
| Female | 59.2 |
| Male | 37.0 |
| Non-binary | 0.3 |
| Prefer not to state | 1.9 |
| Race/ethnicity | |
| Black | 1.5 |
| Asian | 6.3 |
| Indigenous | 0.4 |
| White | 18.4 |
| Hispanic | 3.4 |
| Multiracial | 1.0 |
| Arab | 0.1 |
| Not provided | 64.9 |
| Region of residence | |
| North America | 73.9 |
| United States | 69.0 |
| Midwest | 12.9 |
| South | 9.7 |
| Southwest | 4.1 |
| Intermountain West | 2.2 |
| West Coast | 12.2 |
| East Coast | 27.5 |
| Alaska, Puerto Rico, Hawaii | 0.4 |
| Canada | 3.4 |
| Mexico | 1.3 |
| Central America | 0.1 |
| Europe | 10.3 |
| Eastern | 0.3 |
| Northern | 1.0 |
| Southern | 2.5 |
| Western (including United Kingdom) | 5.7 |
| Australasia, New Zealand, Indonesia | 8.1 |
| Asia | 3.8 |
| South America | 2.9 |
| Africa | 1.0 |
| Middle East | 0.7 |
| Urban-rural | |
| Urban | 53.6 |
| Suburban | 36.0 |
| Rural | 8.7 |
| Primary perspective when completing survey | |
| Mental health care provider | 67.7 |
| A researcher focused on child mental illness | 10.3 |
| Health care provider | 9.0 |
| A leader in an organization/foundation focused on child mental illness | 2.6 |
| A member of the public with an interest in child mental health | 1.8 |
| A person with a family member with a mental illness | 0.9 |
| A person involved in child education | 0.9 |
| A parent of a child with a mental illness | 0.9 |
| A decision maker for an organization/foundation involved in funding for research focused on child mental health | 0.4 |
| A person involved in political decision making | 0.4 |
| A person with lived experience of mental illness | 0.3 |
| A member of a support group or network or organization focused on child mental illness | 0.3 |
| A person involved in child protection/child welfare/child maltreatment services | 0.1 |
| Other | 2.1 |
| COVID-19 pandemic status in community of Residence | |
| Almost none or no cases daily | 9.5 |
| Increasing rates of new cases daily | 48.5 |
| About the same number of new cases daily | 19.1 |
| Decreasing rates of new cases daily | 19.4 |
| Don't know | 1.0 |
Note: Includes participants who answered at least 1 of the key survey questions. Not all categories total 100% because of missing values. Race/ethnicity question was open ended, given that the survey was international.
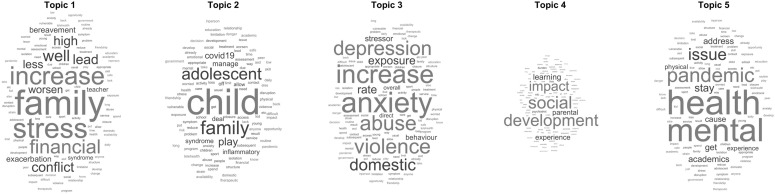
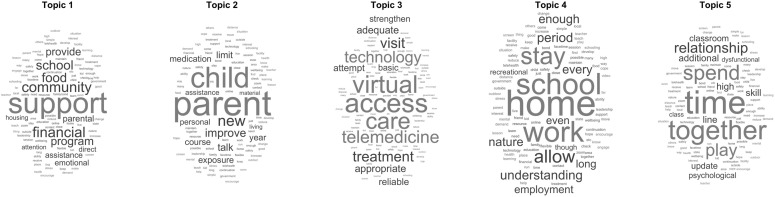
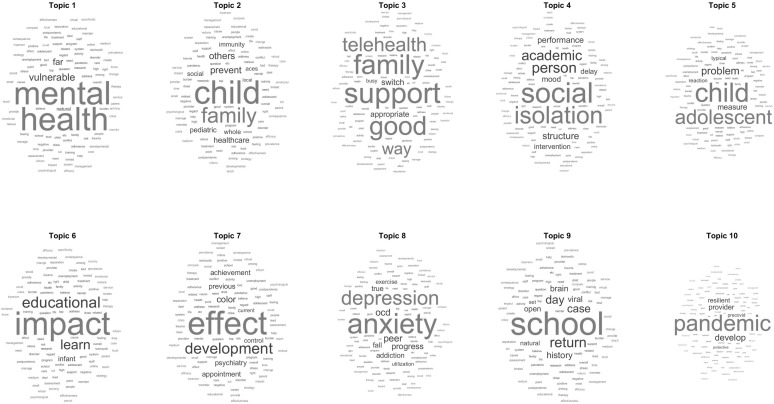
Table 2 summarizes the results of the natural language analyses for the open-ended questions regarding the greatest concerns for children, adolescents, and families, and what has been most helpful for them, respectively. Word clouds for each of these topic areas are reported in Figures S1 and S2 , available online. As reflected in the high κ values, we expected and discovered a high diversity of themes. For the question regarding greatest concerns, κ = 100, with the 5 most probable topics representing 23% of the topic probability and the remaining 77% of topic probability distributed over 95 topics. For the question regarding what has been most helpful, κ = 50, with the 5 most probable topics also accounting for 23% of the topic probability and the remaining 77% of topic probability distributed over 45 topics.
TABLE 2.
Results of Natural Language Analysis (n = 681)
| Question/topic | Probabilitya |
|---|---|
| Concerns about the impacts of the pandemic on children | |
| Increased stress in families | .058 |
| Effects of the pandemic on children | .052 |
| Increased rates of abuse/domestic violence | .051 |
| Impact of the pandemic on child development, especially social development | .045 |
| Impacts on child and adolescent mental health | .028 |
| What is helping children during the pandemic | |
| Material support for families | .057 |
| Parents and children learning more about each other | .054 |
| Access to health care | .046 |
| Flexibility to spend time with family | .041 |
| More quality time for children and their families | .036 |
| Top 3 research questions we need to address | |
| Mental health (vulnerability) | .042 |
| Families and childhood | .032 |
| Service delivery/support | .028 |
| Social isolation | .028 |
| Children and adolescents | .026 |
| Impact on education | .020 |
| Developmental effects | .020 |
| Depression and anxiety | .018 |
| School policy | .017 |
| Pandemic effects | .017 |
Note:
Probability represents the concentration of the topic's representation relative to all the other topics in the whole body of responses for that specific question (also called the “corpus”). In other words, it is the normalized probability that one will see the topic in reading anything from all of the responses together. For each question, all topic probabilities sum to 1.
Figure S1.
Word Clouds for Top 5 Topics in Response to Question “What are you most concerned about in terms of the impacts of the COVID-19 pandemic on health, child development, families, and child and adolescent mental health?”
Figure S2.
Word Clouds for Top 5 Topics in Response to Question “What do you think has been most helpful to children, adolescents, and families during the course of the pandemic?”
What are you most concerned about in terms of the impacts of the COVID-19 pandemic on health, child development, families, and child and adolescent mental health? − Natural Language Analysis
The leading topic was concerns about increased stress in families with a topic probability of 5.8% (Quotation [Q] 1A: The effect on the economy, leading to stress in families, leading to worsening child mental health; Q1B: For families, the lack of childcare is disproportionately impacting women, who are unable to work, and leading to increased financial and emotional stress within the home; Q1C: The impact of parents’ increased stress—this pandemic has stretched everyone's reserve of resilience, energy, and motivation. As parent stress increases, children and youth are increasingly stressed). This was followed by concerns about the effects of the pandemic on children (topic probability of 5.2%; Q1D: My major concern is the further deterioration of children and families in rural areas which are pathetically underserved by C&A Psychiatrists. Included in this group are foster children and adolescents. Many of these children do not have enough nutritious food, basic medical care, or resources for in-home schooling. The devastation to them and their families is very clear; I have significant concerns about children and adolescents with special needs being unable to succeed academically using online schooling; Q1E: Impact of quarantine and ACES [adverse childhood experiences] for children and developmental outcomes), concerns about increased rates of abuse and domestic violence (topic probability of 5.1%; Q1F: More reports of child abuse/domestic violence; Increased exposure to domestic violence due to lockdown) concerns about the impact of the pandemic on child development, especially social development (topic probability of 4.5%; Q1G: The long-term psychological, social, and academic impacts remote and reduced in-person learning will have on child development; Q1H: The impact of social isolation on peer relationships/social development), and impacts on child and adolescent mental health (topic probability of 2.8%; Q1I: The increase in anxiety that the COVID-19 pandemic has caused, which has exacerbated the mental health issues of those already suffering and created new symptoms in those that have not had mental illness).
What do you think has been most helpful to children, adolescents, and families during the course of the pandemic? − Natural Language Analysis
The most commonly endorsed topic was material support for families, with a topic probability of 5.7% (Q2A: Direct financial support to parents. Direct food aid to families who need assistance; Q2B: Government unemployment assistance, school food programs; emotional and financial support for families). This was followed by parents and children learning more about each other (topic probability of 5.4%; Q2C: more personal time with parents, parents learning more about what their children are learning; more time at home with parents and siblings. Parents are getting to see their children in a new light—their strengths and weaknesses in the context of completing school work. Similarly children are getting to see their parents work, which was the case for human history during the agricultural period, and this can increase bidirectional understanding); access to health care (topic probability of 4.6%; Q2D: Reliable access to appropriate services in education, health—including mental health, and social care; Q2E: ability to access MH [mental health] care through telemedicine); flexibility to spend time with family (topic probability of 4.1%; Q2F: Increased time at home for families [eg, caretakers working from home]; When parental employment has been flexible enough to allow parents to be away from work and either facilitate remote learning or just be with their kids, without panic over making ends meet. Too rare, though!); and more quality time for children and their families (topic probability of 3.6%; Q2G: Families who are solid have spent more time together. But families who were struggling do not always benefit from more together time).
Research Priorities—What are the top 3 research questions you believe we need to address regarding the pandemic and the mental health of children, adolescents, and their families?
Thematic Analyses
Results of the thematic analyses are summarized here, with illustrative quotations, and are reported in Table 3 . The most common research priorities were related to epidemiology and social determinants of health, with 80% of participants describing at least 1 such theme, followed by research related to prevention, treatment, and service system response (59%) and research related to biomarkers and neuroscience (30%).
TABLE 3.
Endorsement of Research Priority Themes (n = 643)
| AREA/THEME | PERCENTAGE (%) |
|---|---|
| Epidemiology/social determinants of health | |
| Exposures during the pandemic (factors affecting child) | 54.4 |
| Fear of pandemic/contagion | 1.4 |
| Public health measures | 25.2 |
| School closure/virtual schooling | 16.6 |
| Closure of public spaces | 0.8 |
| Social distancing | 3.6 |
| Screen time | 5.4 |
| Social media | 2.3 |
| Video games | 0.8 |
| Social isolation | 15.6 |
| Parents and families | 28.9 |
| Parental mental health | 8.1 |
| Death of family member/loved one | 2.6 |
| Family relations (including stress and conflict) | 12.0 |
| Family financial stresses | 4.2 |
| Parental unemployment | 1.6 |
| Child abuse/neglect | 7.8 |
| Family/domestic violence | 3.6 |
| Other traumatic experience | 4.7 |
| Impacts on child (child outcomes) | 64.9 |
| Mental health effects on child | 52.7 |
| Suicidality | 4.7 |
| Substance use | 1.2 |
| Anxiety | 12.8 |
| Child development | 13.4 |
| Social−emotional development | 8.2 |
| Adaptive functioning | 1.2 |
| Learning/academic achievement | 13.1 |
| Diminished view of the future | 1.2 |
| Loss of social skills/damage to peer relationships | 8.9 |
| Risk modifiers: social determinants of health | 29.1 |
| Prior mental health problems | 19.1 |
| Vulnerable populations | 4.0 |
| Minoritized groups | 3.3 |
| Black people/people of color | 1.1 |
| Discrimination | 5.0 |
| Poverty | 2.0 |
| Homelessness | 0.8 |
| Risk modifiers: resilience | 12.9 |
| Resilience of child/youth | 11.5 |
| Resilience of family | 3.6 |
| Any epidemiologic theme endorsed | 79.8 |
| Prevention, treatment, and service systems | |
| Service system surveillance | 32.5 |
| Clinical service access/equity | 24.0 |
| Access to mental health services during the pandemic | 9.0 |
| Impact of programmatic changes in inpatient, partial hospitalization, and residential care on quality of services | 1.6 |
| Changes in mental health services to address increased need | 15.1 |
| Clinical service quality and outcomes | 13.7 |
| Effectiveness of TMH | 2.2 |
| Interventions to improve services during the pandemic | 44.8 |
| Prevention and community interventions | 30.9 |
| Direct support to families (eg, financial, rent support, food) | 4.8 |
| Strategies to mitigate impacts of pandemic and societal responses on children | 7.2 |
| Use of electronic means (social media, gaming, video-conferencing) to maintain social connections and to reduce impacts of pandemic on mood | 1.1 |
| Strategies to mitigate the impacts of COVID-19 directly upon neurodevelopment | 3.1 |
| Strategies to increase coping, wellness, and resiliency | 11.2 |
| Prioritizing services for vulnerable populations | 6.4 |
| Services to support parents such as social work and parenting skill development | 3.1 |
| Interventions to ensure the ability of health, education, and human service professionals to identify children at risk for/experiencing child abuse/neglect | 3.1 |
| Interventions in/for schools | 9.6 |
| Interventions to improve online educational engagement and effectiveness | 2.3 |
| Interventions to support the education of children with mental health problems | 4.7 |
| Interventions to bring children back to in-person school safely | 2.5 |
| Clinical and service system interventions | 19.9 |
| TMH services | 10.6 |
| Interventions to ensure quality and accessibility of TMH services | 4.8 |
| Use of health information technology for engagement in mental health treatment | 0.9 |
| Interventions to support valid assessments and evaluations (TMH) | 2.0 |
| Adapting interventions for delivery by TMH | 3.9 |
| Interventions for specific clinical issues | 6.8 |
| Prevention and treatment of OCD | 5.3 |
| Interventions to address impacts of trauma on child mental health | 1.4 |
| Proper use of medication during the pandemic | 0.9 |
| Developing changes to the service system to improve the equity of access to and quality of mental health services | 5.8 |
| Policy changes that support the delivery of quality services in an equitable manner (TMH) | 1.9 |
| Any prevention, treatment, or service system theme endorsed | 59.4 |
| Biomarkers and neuroscience | |
| Cognition and cognitive development | 20.7 |
| SARS-CoV-2 infection | 7.0 |
| Circadian rhythm (sleep physiology) | 1.7 |
| Brain function | 1.6 |
| Immune system function | 1.6 |
| Allostatic load/cortisol | 0.8 |
| Nutritional markers | 0.8 |
| Any biomarker/neuroscience theme endorsed | 29.7 |
Note: Themes listed here were endorsed by 5 or more participants. TMH = tele–mental health.
Epidemiology and Social Determinants of Health
Priorities in this area of research grouped into the following major areas: 1) exposures during the pandemic that might affect children, 2) effects of the pandemic on children and their outcomes, and 3) risk modifiers (both social determinants of health and resilience).
The most common exposure-related themes included the closure of schools and virtual/online schooling (17% of participants; Q3A: 1) Impact of isolation on social/emotional development? 2) Impact of virtual schooling in cognitive development in younger children? 3) Effect of schools being closed on depression and anxiety?), social isolation (16% of participants; Q3B: How has social isolation impacted children and do the effects differ based on socioeconomic factors? The impact of social isolation on normal developmental milestones ie, toddlers, school age, middle school/high school age and college age young adults), and the effects of the pandemic on relationships within families (12% of participants; Q3C: What symptoms are most likely occur in children and youth in relation to the level of caretaker and family stress during this epidemic? Have family attachments improved due to being shut down together?).
Priorities related to the effects of the COVID-19 pandemic on child and adolescent mental health were the most common outcome-related themes (53% of participants; Q3D: Determining rates of depression, anxiety and PTSD across different SE and ethnic groups. Clarifying steps that best correlate with resilience and (+)[positive] outcomes—ie, returning to school, government $ support?). Other outcome-related themes included effects on child development, including social emotional development (13% of participants; Q3E: impact on normal development, especially socialization? How does isolation impact their social development?), learning and academic achievement (13% of participants; Q3F: how much educational ground do kids lose from online schooling? Is the education loss recovered in the following school year or will we face lower scores and abilities?), and effects on social skills and damage to peer relationships (9% of participants; Q3G: To what extent has isolation related to the pandemic negatively impacted social and academic skills?).
The most priorities related to risk modification highlighted social determinants of health for children and adolescents who had mental health problems prior to the pandemic (19% of participants; Q3H: impact of COVID on symptom levels among youth with pre-existing mental health conditions? Impact of loss of schedule/routine on children with ASD/IDD—rates of hospitalization, respite care use, medication changes?). Statements related to other social determinants of health such as discrimination and minoritized groups were less common (5% and 3%; Q3I: experience of Black children and adolescents with the double stressor of the pandemic and George Floyd's murder). Thirteen percent of participants included a focus on resilience, both of the child and the family (13% of participants; Q3J: What makes some at-risk children resilient to the impacts of the pandemic, but not others?).
Prevention, Treatment, and Service Systems. Priorities in this area grouped into 2 major areas: (1) service system surveillance, and (2) interventions to improve services during the pandemic.
In terms of service system surveillance, the most common themes related to access to clinical services in an equitable manner (24% of participants; Q4A: Effectiveness of virtual assessment and intervention with emphasis on those who do not benefit, considering equity, diversity and inclusion factors) and outcomes of clinical care during the pandemic (14% of participants; Q4B: Looking at providing telehealth on a broad scale to compare to care as usual prior to the pandemic. With less regulation and oversight, how did our profession do at taking good care of children/adolescents?).
The most common priorities regarding interventions focused on prevention and community interventions (31% of participants), including strategies to increase coping, wellness, and resilience (11%; Q4C: What are concrete ways to increase resiliency in children and adolescents?), strategies to mitigate the effects of the pandemic and societal responses on children (7%; Q4D: What strategies can be effectively used to mitigate some of the traumatizing nature of learning about the pandemic in the home?), and efforts to prioritize service for vulnerable populations (6%; Q4E: What to prioritize—how to comprehensively organize care for vulnerable families including aspects that affect overall ability to deal with adverse events—how to adapt to virtual care / make accessible for all?). Responses of 10% of participants focused on interventions to and for schools (15% of responses), including interventions to support the education of children with mental health problems (5%; Q4F: How to get remote learning right for kids with ADHD and/or ASD?). Clinical and service system research priorities (20% of participants) most commonly focused on providing effective assessment and treatment services via tele−mental health (13%; Q4G: To test new ways of delivering care, digital care). Other themes included interventions for specific clinical issues such as obsessive-compulsive disorder (5%) and interventions to the service system to improve the equity of access to and quality of mental health care (6%; Q4H: Ways child psychiatrists can reach underserved minority families during a pandemic. How can we improve access to mental health support to all—these are more accessible to affluent people at this time?).
Biomarkers and Neuroscience
Thirty percent of participants identified priorities related to biomarkers and neuroscience in their responses. The most common theme was related to concerns regarding the effect of the pandemic on child and adolescent cognition and cognitive development (21% of participants; Q5A: What impact does a global pandemic or other global event/crisis have [on] a child's neurological development? Q5B: The effect of the solitary use of computer-based learning on achievement and brain development, including the development of oral language skills/social communication [pragmatics, etc.], auditory skills [field/ground, etc]), and the direct impact of the SARS-Cov-2 virus on the brain (7% of participants; Q5C: What are the long-term inflammatory, neurological, and psychological effects on children who have been infected with the virus, if any?).
Natural Language Analysis
Table 2 and Figure S3 , available online, summarizes the results of the natural language analyses for the open-ended question regarding COVID-19 pandemic−related research priorities. As with questions 1 and 2, we expected and discovered a high diversity of themes (κ = 150). Despite the diversity of respondents and our prompt to offer 3 recommendations, there was a remarkable convergence of topics. For example, the top 10 most probable topics represented 25% of topic probability (with the remaining 75% probability distributed over 140 topics). The findings supported the thematic analyses, as indicated by the most probable 10 topics displayed in Table 2. Finally, we used each illustrative quotation provided above to query the model for topics that were most represented by that quotation. The findings of this crosswalk are summarized in Table S1 , available online. Quotations matched well with topics identified in this analysis.
Figure S3.
Word Clouds for Top 10 Topics in Response to Question “What are your top 3 research questions you believe we need to address regarding the pandemic and the mental health of children, adolescents, and their families?”
TABLE S1.
Thematic Analysis to Natural Language Analysis Crosswalk for Research Priorities
| Theme | Illustrative quotation | Top 3 topicsa represented by this quotation |
|---|---|---|
| Epidemiology and social determinants of health | ||
| Closure of schools and virtual/online schooling | Q3A: Impact of isolation on social/emotional development? 2) Impact of virtual schooling in cognitive development in younger children? 3) Effect of schools being closed on depression and anxiety? |
Depression and anxiety (topic 8, p = .09); resilience, minorities, stress (topic 29, p = .07); service delivery and (family) support (topic 3, p = .06) |
| Social isolation | Q3B: How has social isolation impacted children and do the effects differ based on socioeconomic factors? The impact of social isolation on normal developmental milestones, ie, toddlers, school-age, middle school/high school−age, and college-age young adults | Social isolation (topic 4; p = .12); school policy (topic 9; p = .09); age-specific issues (topic 91; p = .08) |
| Effects of the pandemic on relationships within families | Q3C: What symptoms are most likely occur in children and youths in relation to the level of caretaker and family stress during this epidemic? Have family attachments improved due to being shut down together? | Effects of shutting down (topic 33, p = .10); staying home (topic 24, p = .04); family members (topic 47, p = .04) |
| Effects of the COVID-19 pandemic on child and adolescent mental health | Q3D: Determining rates of depression, anxiety and PTSD across different socioeconomic and ethnic groups. Clarifying steps that best correlate with resilience and (+)[positive] outcomes—ie returning to school, government financial support? | Depression and anxiety (topic 8, p = .09); resilience, minorities, stress (topic 29, p = .07); service delivery and (family) support (topic 3, p = .06) |
| Effects on child development, including social−emotional development | Q3E: Impact on normal development, especially socialization? How does isolation impact their social development? | Social isolation (topic 4, p = .09); emotional development (topic 12, p = .07); developmental effects (topic 6, p = .05) |
| Learning and academic achievement | Q3F: How much educational ground do kids lose from online schooling? Is the education loss recovered in the following school year or will we face lower scores and abilities? | Losing ground (topic 34, p = .08); disruption of lost year (topic 82, p = .07); education impact (topic 6, p = .05) |
| Effects on social skills and damage to peer relationships | Q3G: To what extent has isolation related to the pandemic negatively impacted social and academic skills? | Social isolation (topic 4, p = .13); pandemic risks (topic 22, p = .07); screen time/away from people (topic 18, p = .05) |
| Social determinants of health for children and adolescents who had mental health problems prior to the pandemic | Q3H: Impact of COVID on symptom levels among youths with pre-existing mental health conditions? Impact of loss of schedule/routine on children with ASD/IDD—rates of hospitalization, respite care use, medication changes? | Mental health vulnerability (topic 1, p = .09), change/routine disruption (topic 28, p = .07), impact on psychiatric care (topic 57, p = .06) |
| Other social determinants of health such as discrimination and minoritized groups | Q3I: Experience of Black children and adolescents with the double stressor of the pandemic and George Floyd's murder | Screen time/away from people (underserved represented; topic 18, p = .06); pandemic effects (topic 10, p = .05); community stress (topic 90, p = .05)b |
| Resilience, both of the child and of the family | Q3J: What makes some at-risk children resilient to the impacts of the pandemic, but not others? | Pandemic effects (includes resilience; topic 10, p = .11); families and childhood (topic 2, p = .08); mental health vulnerability (topic 1, p = .04) |
| Prevention, treatment, and service systems | ||
| Access to clinical services in an equitable manner | Q4A: Effectiveness of virtual assessment and intervention with emphasis on those who do not benefit, considering equity, diversity, and inclusion factors | Virtual treatment during quarantine (includes ethnic, topic 14, p = .05); intervention effectiveness (topic 19, p = .05); access/resources (includes equity; topic 21, p = .05) |
| Outcomes of clinical care during the pandemic | Q4B: Looking at providing telehealth on a broad scale to compare to care as usual prior to the pandemic. With less regulation and oversight, how did our profession do at taking good care of children/adolescents? | Service delivery/support (topic 3, p = .10); valid care delivery model (topic 67, p = .07); prevention/well child (topic 34, p = .05) |
| Strategies to increase coping, wellness, and resilience | Q4C: What are concrete ways to increase resiliency in children and adolescents? | Impact/resiliency (topic 13, p = .06); mitigate school closure (topic 42, p = .06); modify risk (topic 23, p = .04) |
| Strategies to mitigate the effects of the pandemic and societal responses on children | Q4D: What strategies can be effectively used to mitigate some of the traumatizing nature of learning about the pandemic in the home? | Management of quarantine (topic 14, p = .05); remote learning (topic 25, p = .05); effective assessment/protection/therapy (topic 63, p = .05) |
| Efforts to prioritize service for vulnerable populations | Q4E: What to prioritize—how to comprehensively organize care for vulnerable families including aspects that affect overall ability to deal with adverse events—how to adapt to virtual care / make accessible for all? | Effective/accessible (topic 64, p = .07); mental health vulnerability (topic 1, p = .06); valid care delivery model (topic 67, p = .06) |
| Interventions to support the education of children with mental health problems | Q4F: How to get remote learning right for kids with ADHD and/or ASD? | Remote learning (topic 25, p = .10); ADHD/activity/sleep (topic 78, p = .05); kids (topic 69, p = .04) |
| Providing effective assessment and treatment services via tele−mental health | Q4G: To test new ways of delivering care, digital care | Valid care delivery model (topic 67, p = .08); novel electronic/digital care (topic 73, p = .07); mitigate school closure (topic 42, p = .05) |
| Interventions for specific clinical issues such as obsessive-compulsive disorder; interventions to the service system to improve the equity of access to and quality of mental health care | Q4H: Ways child psychiatrists can reach underserved minority families during a pandemic. How can we improve access to mental health support to all (these are more accessible to affluent people at this time)? | Mental health vulnerability (topic 1, p = .08); screen time/away from people (underserved represented; topic 18, p = .08); equitable access/resources/service (topic 21, p = .05) |
| Biomarkers and Neuroscience | ||
| Effect of the pandemic on child and adolescent cognition and cognitive development | Q5A: What impact does a global pandemic or other global event\crisis have [on] a child's neurological development? | Effect global nature of pandemic (topic 46, p = .10); interventions/crisis (topic 19, p = .04); neurological effects (topic 50, p = .04) |
| Q5B: The effect of the solitary use of computer-based learning on achievement and brain development, including the development of oral language skills/social communication (pragmatics, etc), auditory skills (field/ground, etc) | Developmental effects (topic 7, p = .14); risk (topic 35, p = .06); remote learning (topic 25, p = .04) | |
| Direct impact of the SARS-Cov-2 virus on the brain | Q5C: What are the long-term inflammatory, neurological, and psychological effects on children who have been infected with the virus, if any? | Long-term brain effects (topic 17, p = .09); neurological effects (topic 50, p = .05); psychological effects (topic 93, p = .05) |
Note: ADHD = attention-deficit/hyperactivity disorder; ASD = autism spectrum disorder; IDD = intellectual developmental disorder.
Topic number is the rank order of the topic in terms of its likelihood of appearing anywhere in the total response set, with lesser numbers being more probable. In other words, topic 1 is far more likely to appear relative to topic 150. The p values reflect the topic mixture probabilities, or the probability of the topic being represented by the quotation compared to all other topics. For short, focused quotations, most topic probabilities are small, with a few dominant topics. For lengthy quotations representing many concepts, topic probabilities are spread over many topics.
This quotation was too distinct from other quotations for strong matches to topics.
Discussion
The responses of participants of this survey, conducted in June and July 2020 and, to our knowledge, the first large-scale survey of this type, appear to be prescient, as the pandemic has continued to affect children, adolescents, and their families. Although the scholarly literature is still developing, media around the globe continue to document the ways in which societies have responded to the pandemic to reduce the spread of COVID-19 and how the related morbidity and mortality have affected children and their families.4 , 5 , 9 , 10 , 21, 22, 23, 24 Participants in the present survey emphasized the importance of documenting these effects through research as well as developing and testing interventions to reduce them. Many of the research questions raised by participants, such as the longitudinal effects of the pandemic on vulnerable populations, as well as adjustments to preventive and clinical services, will require ongoing surveillance. The full scope of the developmental and mental health effects of the COVID-19 pandemic will be an important area of research for many years.
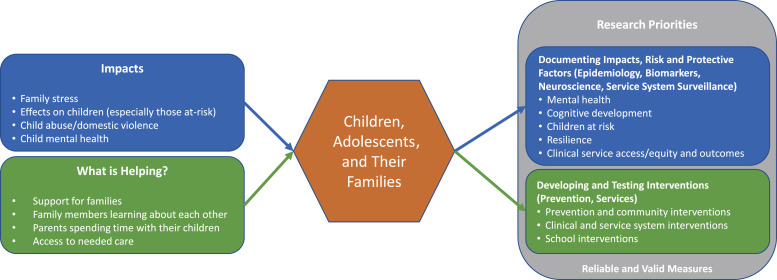
The most frequently described research priorities are consistent with participants’ concerns regarding the impact of the pandemic as well as what they identified as most helpful to families and are summarized in Figure 1 . Given the rationale for the survey and the background of the participants, it is not surprising that the effects of the COVID-19 pandemic on the mental health of children and adolescents was a research priority described by a majority of participants (53%) and was 1 of the 5 most common topics from participant responses regarding the impacts of the pandemic. Similarly, preventive and community interventions, service access, and equity were the most commonly endorsed services and treatment priorities (31% and 24%, respectively) and material support for families and access to health care were among the 5 most common topics regarding what was proving helpful for children and families. Finally, the impacts of the pandemic on cognitive development was the most common biomarker and neuroscience research priority (21%), which was captured by 2 of the 5 most commonly endorsed topics regarding the impacts of the pandemic: specifically, impacts on children and impacts on social development.
FIGURE 1.
Overview of Key Study Findings
For thematic analysis, the topics that included biomarkers, genetics, epigenetics, and neuroscience domains were combined for the purpose of analysis, and responses related to these topics were relatively rare. In particular, there were no responses that directly mentioned genetics or epigenetics, although genetics and epigenetics could potentially be included in research studies of biomarkers and neuroscience, and topics outside of the biomarkers and neuroscience category (social determinants of health, risk and resilience factors, various aspects of mental health) could potentially be influenced by genetics, epigenetics and gene−environment interplay.
Although respondents did not directly raise questions regarding research methods and measures, their responses do have implications for the conduct of research regarding the mental health effects of the COVID-19 pandemic on children and adolescents. First, we need reliable and valid measures that are able to capture the unique challenges that the COVID-19 pandemic has created, such as stress, social isolation, and trauma, as well as the mental health effects of the virus itself on infected children.
The research questions raised by survey participants span a wide variety of important topics, including adherence to public health recommendations, reactions to public health measures, rationale for individual/family behavior, effects of uncertainty around the pandemic itself (eg, when it will end, what behaviors and situations raise the risk of infection, whether the gains of in-person education outweigh the risks of exposure to others infected with COVID-19), the effects of the political environment during the pandemic, and the effects of the pandemic on child/adolescent worldview. Developing new research in these areas will necessitate the development of measures that capture these novel aspects of the pandemic and its effects. In areas where baseline and ongoing measures have already been and continue to be collected, it will be important to scrutinize the ability to capture the experiences of children and families during the pandemic, including social isolation, child development, family cohesion, unemployment, financial stressors, and resilience. Identification and analysis of the effects of the COVID-19 pandemic on vulnerable populations, including children from minoritized groups, who live in poverty, have existing mental health problems, or have experienced loss of special education services, will also need careful scrutiny.
In addition, because the pandemic reduces contact between children and mandated reporters of child abuse, new methods are needed to detect incidents of abuse and neglect. Finally, although research examining the delivery of child and adolescent tele−mental health includes well-established procedures,25, 26, 27 some aspects of service delivery, such as tele−mental health directly into homes, are not well studied and likely require the development of new methods and measures. In sum, studies that assess the psychometric properties of these much-needed measures are foundational for ongoing and future COVID-19−focused research.
This survey and these analyses have a number of limitations. The participants predominantly resided in the United States in urban and suburban areas, even though 31% resided in other countries and 9% in rural areas. This survey focused on recruiting participants in the mental health professions. A survey that captures the perspectives of children and families is also warranted. Although almost two-thirds of participants did not report their race/ethnicity, among those who did the majority (59%) were White. Only 43 participants identified as Asian, 23 participants identified as Hispanic, 10 as Black, 7 as Multiracial, 3 as Indigenous, and 1 as Arab, making it highly likely that we did not capture the perspectives of our Black, Indigenous, and People of Color (BIPOC) colleagues during a time of increased awareness of COVID-19− specific racial disparities, increased racial tensions, civil unrest, and enhanced global awareness of systemic racism. The heterogeneity of the open-ended responses created challenges for both the natural language analysis and the thematic analyses. For the topic modeling, the dataset of 681 participants was relatively small, specifically fitting to brief responses representing a diverse set of topics. This is particularly the case for the item querying research preferences, which prompted 3 ideas per response. In contrast, for the thematic analyses, the dataset was relatively large, making the development of a codebook representative of the diverse themes raised by participants particularly challenging. Furthermore, JAACAP’s June−July 2020 survey preceded the COVID-19 vaccine development and approval of multiple vaccines beginning in December 2020. As the pandemic unfolds and hopefully subsides, vaccine distribution and equity issues and the uncertainty of when and how to return to more in-person activities will affect the mental health of youths and their families. Finally, the survey did not address the effect of the pandemic on research itself, and the challenges in conducting research that is rigorous, reliable, and valid while trying to capture new phenomena and limiting the risk to participants and research staff.
As we write this almost a year after the World Health Organization declared the COVID-19 outbreak a global pandemic, we, as members of the Editorial Board of JAACAP, renew our commitment to maintain our high editorial standards, such that the articles that we publish regarding this pandemic are well designed, carefully conducted, and properly interpreted and… [are] situated within and expand the existing knowledge base. 28 We hope that this survey helps guide the ongoing investigation and analyses of the events that have changed—and will change— the developmental trajectory and mental health of many children and adolescents, and support our work to provide the extraordinary prevention and treatment that they need and deserve.
Footnotes
The authors have reported no funding for this work.
This study was determined to be exempt from human subjects regulations by the Colorado Multiple Institutional Review Board.
Author Contributions
Conceptualization: Novins, Stoddard, Althoff, Charach, Cortese, Cullen, Frazier, Glatt, Henderson, Herringa, Hulvershorn, Kieling, McBride, McCauley, Middeldorp, Reiersen, Rockhill, Sagot, Scahill, Simonoff, Stewart, Szigethy, Taylor, White, Zima
Data curation: Novins
Formal analysis: Novins, Stoddard, Althoff, Charach, Cortese, Cullen, Frazier, Glatt, Henderson, Hulvershorn, Kieling, McBride, McCauley, Middeldorp, Reiersen, Rockhill, Sagot, Scahill, Simonoff, Szigethy, Taylor
Investigation: Novins, Stoddard, Althoff, Charach, Cortese, Cullen, Frazier, Glatt, Henderson, Herringa, Hulvershorn, Kieling, McBride, McCauley, Middeldorp, Reiersen, Rockhill, Sagot, Scahill, Simonoff, Stewart, Szigethy, Taylor, White, Zima
Methodology: Novins, Stoddard, Althoff, Charach, Cortese, Cullen, Frazier, Glatt, Henderson, Herringa, Hulvershorn, Kieling, McBride, McCauley, Middeldorp, Reiersen, Rockhill, Sagot, Scahill, Simonoff, Stewart, Szigethy, Taylor, White, Zima
Project administration: Novins
Resources: Novins, Stoddard
Software: Novins, Stoddard
Supervision: Novins
Validation: Novins, Stoddard, Althoff, Charach, Cortese, Cullen, Frazier, Glatt, Henderson, Hulvershorn, Kieling, McBride, McCauley, Middeldorp, Reiersen, Rockhill, Sagot, Scahill, Simonoff, Szigethy, Taylor
Visualization: Novins
Writing – original draft: Novins, Stoddard
Writing – review and editing: Novins, Stoddard, Althoff, Charach, Cortese, Cullen, Frazier, Glatt, Henderson, Herringa, Hulvershorn, Kieling, McBride, McCauley, Middeldorp, Reiersen, Rockhill, Sagot, Scahill, Simonoff, Stewart, Szigethy, Taylor, White, Zima
ORCID
Douglas K. Novins, MD: https://orcid.org/0000-0003-4475-8596
Joel Stoddard, MD, MAS: https://orcid.org/0000-0003-4070-4566
Robert R. Althoff, MD, PhD: https://orcid.org/0000-0002-5673-7613
Alice Charach, MD, MSc, FRCPC: https://orcid.org/0000-0001-9756-4328
Samuele Cortese, MD, PhD: https://orcid.org/0000-0001-5877-8075
Kathryn Regan Cullen, MD: https://orcid.org/0000-0001-9631-3770
Jean A. Frazier, MD: https://orcid.org/0000-0001-7055-3530
Stephen J. Glatt, PhD: https://orcid.org/0000-0002-0360-7567
Schuyler W. Henderson, MD, MPH: https://orcid.org/0000-0001-9271-2846
Ryan J. Herringa, MD, PhD: https://orcid.org/0000-0002-1936-7959
Leslie Hulvershorn, MD, MSc: https://orcid.org/0000-0001-5827-4889
Christian Kieling, MD, PhD: https://orcid.org/0000-0001-7691-4149
Anne B. McBride, MD: https://orcid.org/0000-0002-6320-4831
Elizabeth McCauley, PhD, ABPP: https://orcid.org/0000-0001-9763-9262
Christel Middeldorp, MD, PhD: https://orcid.org/0000-0002-6218-0428
Angela M. Reiersen, MD, MPE: https://orcid.org/0000-0003-3203-4590
Carol M. Rockhill, MD, PhD, MPH: https://orcid.org/0000-0001-5799-9706
Adam J. Sagot, DO, FAPA: https://orcid.org/0000-0002-4393-5346
Lawrence Scahill, PhD: https://orcid.org/0000-0001-5073-1707
Emily Simonoff, MD, FRCPsych: https://orcid.org/0000-0002-5450-0823
S. Evelyn Stewart, MD: https://orcid.org/0000-0002-0994-6383
Eva Szigethy, MD, PhD: https://orcid.org/0000-0001-6783-581X
Jerome H. Taylor, MD: https://orcid.org/0000-0003-2787-6232
Tonya White, MD, PhD: https://orcid.org/0000-0003-0271-1896
Bonnie T. Zima, MD, PhD: https://orcid.org/0000-0002-5542-1879
The authors consist of members of the Masthead of the Journal of the American Academy of Child and Adolescent Psychiatry and its companion journal, JAACAP Connect. The authors acknowledge the contributions of Nicole King Cotton, MD, of Morehouse School of Medicine, Stacy S. Drury, MD, PhD, of Tulane University, Lesha D. Shah, MD, of Icahn School of Medicine at Mount Sinai, Chad M. Sylvester, MD, PhD, of Washington University School of Medicine, and Peter Szatmari, MD, of University of Toronto, in the design of the survey methods. The authors also acknowledge the contributions of Mary K. Billingsley, ELS, JAACAP Managing Editor, in editing this manuscript and preparing it for publication.
Disclosure: Dr. Novins has received grant or research support from the National Institutes of Health and the Administration for Children and Families. Dr. Stoddard has received grant or research support from the National Institute of Mental Health. He has served as a DSMB committee member: Threat Interpretation Bias as Cognitive Marker and Treatment Target in Pediatric Anxiety (R61 Phase). Dr. Althoff has received grant or research support from the National Institute of Mental Health, the National Institute on Drug Abuse, and the Klingenstein Third Generation Foundation. He has served on the editorial board of Child Psychiatry and Human Development and as consulting editor of the Journal of Clinical Child and Adolescent Psychology. He has received honoraria from Massachusetts General Hospital Psychiatry Academy and Frontline Medical Communications, Inc. He is a partner of WISER Systems, LLC. Dr. Charach has received grants or research funding from the Canadian Institutes of Health Research, the Ontario Ministry of Health, the University of Toronto Department of Psychiatry, the University of Toronto Edwin S.H. Leong Centre for Healthy Children, and SickKids Centre for Brain and Mental Health. Dr. Cortese has served as deputy editor of Evidence-Based Mental Health, associate editor of Child and Adolescent Mental Health, and on the editorial boards of the Journal of Child Psychology and Psychiatry, the Journal of Child and Adolescent Psychopharmacology, and CNS Drugs. He has received honoraria from the Association for Child and Adolescent Mental Health, the British Association for Psychopharmacology, Healthcare Convention, and the Canadian ADHD Resource Alliance. Dr. Cullen has received grants from the National Institute of Health (NIH) and the University of Minnesota. She has served on a grant review committee for NIH and received honoraria. She has received honoraria for serving on an advisory committee for the Food and Drug Administration. Dr. Frazier has received grant or research support from the the National Institute of Mental Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Fulcrum Therapeutics, and Roche. She has served on the editorial board of the Harvard Review of Psychiatry and as associate editor of the Journal of Child and Adolescent Psychopharmacology. Dr. Glatt has received grant or research support from the National Institutes of Health and the National Science Foundation. He has served as a consultant to Cohen Veterans Bioscience. He has received book royalties from Oxford University Press. Dr. Herringa has received grant or research support from the National Institute of Mental Health. Dr. Hulvershorn has received grant or research support from the National Institutes of Health, the Substance Abuse and Mental Health Services Administration, the Indiana Family and Social Services Agency, Merck, and Greenwich Biosciences. Dr. Kieling has received research support from Brazilian governmental research funding agencies: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), and Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (Fapergs); from the UK funding agencies MQ: Transforming Mental Health, the Academy of Medical Sciences, and the Royal Academy of Engineering; and from the US National Institutes of Health. He has served on the editorial boards of Archives of Clinical Psychiatry, Global Mental Health, Jornal Brasileiro de Psiquiatria, and Social Science and Medicine - Mental Health. He has received authorship royalties from Brazilian publishers Artmed and Editora Manole. Dr. McBride has received royalties from American Psychiatric Publishing, Inc. Dr. McCauley has received grant or research support from the National Institute of Mental Health, the Institute of Education Sciences - US Department of Education, the American Foundation for Suicide Prevention, and the Scooty Fund. She has served as a consultant to King County Public Health—School-Based Mental Health Programs and School Mental Health, Ontario. She has received honoraria for trainings for school-based mental health providers on a Brief Intervention for School Clinicians (BRISC). She has received book royalties from Guilford Press for Behavioral Activation with Adolescents: A Clinician's Guide and Academic Media Solutions for a psychology textbook. Dr. Middeldorp has received grant or research support from the National Health and Medical Research Council, the European Union, the National Mental Health Research Committee, and the Australian ADHD Professional Association. She has served as associate editor of the American Journal of Medical Genetics Part B. Dr. Reiersen has received grant or research support from the National Institutes of Health, the McDonnell Center for Systems Neuroscience, the McDonnell Center for Cellular and Molecular Neurobiology, the Taylor Family Institute for Innovative Psychiatric Treatment at Washington University, Fast Grants, and the COVID-19 Early Treatment Fund. Washington University has applied for a patent related to methods of treating COVID-19 invented by Dr. Reiersen. She has received travel support from the Child and Adolescent Psychiatric Department, Region Zealand (Denmark hospital). Dr. Scahill has received grant or research support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the US Department of Defense, and the Marcus Foundation. He is a co-author of the Children's Yale–Brown Obsessive Compulsive Scale (CYBOCS), the Children's Yale–Brown Obsessive Compulsive Scale modified for Autism Spectrum Disorder (CYBOCS-ASD), and the Parent-Rated Anxiety Scale for youth with autism spectrum disorders (PRAS-ASD). He has served as a consultant to Roche, Impel NeuroPharma, Inc., Yamo Pharmaceuticals, and Teva Pharmaceutical Industries. He has served as associate editor of the Journal of Child and Adolescent Psychopharmacology and on the editorial board of the International Journal of Developmental Disabilities. He has received royalties from Guilford Press, Oxford University Press, and American Psychiatric Association Publishing. Dr. Simonoff has received grant or research support from the UK National Institute of Health Research, the European Commission, the UK Economic and Social Research Council, the UK Medical Research Council, the National Institute of Health Research Biomedical Research Centre at South London and Maudsley Foundation, the Psychiatry Research Trust, the Guy's and St. Thomas’ Charitable Foundation Trust, and the Maudsley Charity. She has served on the advisory boards of the European ADHD Guidelines Group, Eunethydis, the Autistica Mental Health Steering Group, the National Autism Project Board, the Medical Research Council Neuroscience and Mental Health Board, the Central Institute for Mental Health, Manheim, Germany, and the Oak Foundation. She is author of the assessment tools Assessment of Consuming Behaviour (copyright, Santosh and Simonoff, manuscript in preparation) and Observation Schedule for Children with Autism (in preparation). She has served on the editorial board of the British Journal of Psychiatry. She has received honoraria from the Royal College of Physicians as Senior Clinical Advisor for the National Institute of Health and Care Excellence. Dr. Stewart has received grant or research support from the Michael Smith Foundation for Health Research, the British Columbia Ministry of Health and the British Columbia Centre for Disease Control. She has served on the Scientific and Clinical Advisory Board of the International OCD Foundation and on the Scientific Advisory Committee of Anxiety Canada. She has served on the editorial boards of the Journal of the Canadian Academy of Child and Adolescent Psychiatry, Annals of Clinical Psychiatry, and the Canadian Journal of Psychiatry. She authored the OCD Family Functioning (OFF) Scale and the Guilford Press book OCD in Children and Adolescents: The OCD is Not the Boss of Me Handbook. She has received honoraria from the University of Colorado for 2019-20 Brewster Visiting Professorship, the Canadian Academy of Child and Adolescent Psychiatry, and Aarhus University, Denmark. She has received anonymous donor funding support. Dr. Szigethy has received grant or research support from the National Institutes of Health and the Patient-Centered Outcomes Research Institute. She has received book royalties from APPI for co-editing Cognitive-Behavior Therapy for Children and Adolescents. She has served on the speakers’ bureau of Janssen. Dr. White has received grant or research support from the Sophia Children's Hospital Foundation, the Dutch Research Council (Nationale wetenschappelijke organisatie; NWO), and the US National Institutes of Health. She has served on the scientific advisory board/DSMB of the University of Bergen Center for Brain Plasticity. She is the Editor-in-Chief of Aperture Neuro and has served on the editorial board of Neuroinformatics. Dr. Zima has received grant or research support from the Substance Abuse and Mental Health Services Administration, the California Mental Health Services Act (SB82-833), and the California Bureau for Cannabis Control. She has served as deputy editor to the Journal of Child and Adolescent Psychopharmacology and as consulting editor to the Journal of Clinical Child and Adolescent Psychology and the Journal of Emotional and Behavioral Disorders. Drs. Henderson, Rockhill, Sagot, and Taylor have reported no biomedical financial interests or potential conflicts of interest.
Supplement 1: JAACAP COVID-19 Survey
Start of Block: Block 1
Preamble. Within the past several months, the emergence of COVID-19 has resulted in widespread changes to our lives and daily routines. Schools, playgrounds, and businesses have been closed, peer interactions curbed. Families may be isolated with limited interactions with extended family and community networks and are facing new financial, educational, and employment challenges. Beyond this, many lives have been lost likely disproportionately impacting our highest-risk populations. As an organization committed to promoting the optimum mental health and well-being in children and families, we at JAACAP are asking you to complete a very short survey to let us know what you believe the most crucial research priorities should be as we work together toward our shared common goal of ensuring the health and well-being of children and families. The survey should take less than 10 minutes and we thank you for your time.
Q1 How old are you?
-
○
17 years old or younger (1)
-
○
18-24 years old (2)
-
○
25-50 years old (3)
-
○
50 years old or older (4)
Skip To: Exit 1 If How old are you? = 17 years old or younger
Exit 1 We appreciate your interest in this survey but you must be 18 years of age or older to participate. We are planning on conducting a similar survey for youths in the coming weeks.
Skip To: End of Survey If We appreciate your interest in this survey but you must be 18 years of age or older to participate... Is Displayed
Q2 Where do you live?
-
○US – Midwest (1)
-
○US – South (2)
-
○US – Southwest (3)
-
○US – Intermountain West (4)
-
○US – West Coast (5)
-
○US – East Coast (6)
-
○US – Alaska, Puerto Rico, Hawaii (7)
-
○Canada (19)
-
○Mexico (20)
-
○Central America (8)
-
○South America (9)
-
○Europe – Eastern (10)
-
○Europe – Northern (11)
-
○Europe – Southern (12)
-
○Europe – Western (including UK) (13)
-
○Middle East (14)
-
○Asia (15)
-
○Australia/New Zealand/Indonesia (16)
-
○Africa (17)
-
○Other location (please specify) (18)______________
-
○
Skip To: GDPR If Where do you live? = Europe – Eastern
Skip To: GDPR If Where do you live? = Europe – Northern
Skip To: GDPR If Where do you live? = Europe – Southern
Skip To: GDPR If Where do you live? = Europe – Western (including UK)
Skip To: Preamble 2 If Where do you live? = US – Midwest
Skip To: Preamble 2 If Where do you live? = US – South
Skip To: Preamble 2 If Where do you live? = US – Intermountain West
Skip To: Preamble 2 If Where do you live? = US – South West
Skip To: Preamble 2 If Where do you live? = US – West Coast
Skip To: Preamble 2 If Where do you live? = US – East Coast
Skip To: Preamble 2 If Where do you live? = US – Alaska, Puerto Rico, Hawaii
Skip To: Preamble 2 If Where do you live? = Central America
Skip To: Preamble 2 If Where do you live? = South America
Skip To: Preamble 2 If Where do you live? = Middle East
Skip To: Preamble 2 If Where do you live? = Asia
Skip To: Preamble 2 If Where do you live? = Australia/New Zealand/Indonesia
Skip To: Preamble 2 If Where do you live? = Africa
Skip To: Preamble 2 If Where do you live? = Other location (please specify)
Skip To: Preamble 2 If Condition: Other location (please spec... Is Not Empty. Skip To: Please do not include any personal in....
Skip To: Preamble 2 If Where do you live? = Canada
Skip To: Preamble 2 If Where do you live? = Mexico
GDPR Addendum for informed consent (for countries adhering to GDPR only)
The researchers will collect Personal Information about you for this study. This includes your responses to this survey. If you withdraw your permission, your participation in the study will end. No new information will be collected about you. Your withdrawal has no effect on the lawfulness of the data processing that occurred prior to your withdrawal. Your Personal Information that has already been collected to the time of your withdrawal will be kept and used to guarantee the integrity of the study and/or for any other purposes permitted under applicable data protection and privacy laws.
Your Personal Information will not be used for further research. However, if permitted by applicable law, your Personal Information may be anonymized so that the information cannot identify you personally, and such anonymized information may be used for further research.
Your Personal Information will be treated in compliance with applicable data protection laws. The researcher is based in the United States. The European Commission has determined that the data protection laws of the United States do not protect Personal Information to the same extent as those of the European Economic Area. By signing this consent form, you consent to the transfer of your information to the United States, and those working with the University will take steps to maintain the confidentiality of your Personal Information.
The University, its IRB, Privacy Officer and Legal Counsel, and other University professional staff are permitted to access and use your Personal Information to conduct and oversee the research and ensure compliance with legal and regulatory requirements, including:
-
×
verify that the study is conducted correctly and that study data are accurate;
-
×
answer questions from IRB, or government or regulatory agencies;
-
×
contact you during and after the study (if necessary); and
-
×
answer your data protection requests (if any).
Your rights related to your Personal Information collected under the study are described below. If you wish to exercise any of these rights, you must contact COMIRB@ucdenver.edu.
-
•
You have the right to see the information being collected about you in the study.
-
•
You have the right to correct or update your Personal Information if it is inaccurate.
-
•
You have the right to limit the collection and use of your Personal Information under certain circumstances (for example, if you think that the information is inaccurate).
-
•
You have the right to receive your Personal Information in a structured, common computer format (for example, in a readable text electronic file or chart) for your own purposes or for giving it to others, as required by applicable data protection laws. You may not have the right to receive your Personal Information that has been used for public interest purposes or in the exercise of official authority vested in The University.
-
•
You have the right to request the deletion of your Personal Information if you are no longer participating in the study. However, there are limits on your ability to request deletion of your Personal Information. The University may keep and use some or all of your Personal Information if deletion would seriously impair the study (for example, if deletion would affect the consistency of study results) or if your Personal Information is needed to comply with legal requirements.
-
•
You have the right to make a complaint to a data protection authority within the EU (http://ec.europa.eu/justice/data-protection/article-29/structure/data-protection-authorities/index_en.htm). Your Personal Information needed for the research will be saved, analyzed and, if necessary, transferred outside of the University. Researchers will not transfer any information that directly identifies you. This is called your “Coded Information” and it is sometimes called “pseudonymized data” by data protection laws. The University and some of the other people using your Personal Information, including your Coded Information, may be based in countries other than your country, including the United States. Data protection and privacy laws in these countries may not offer the same level of protection as those in your own country. The University, your study site, and those working with The University and your Study Site will take steps to maintain the confidentiality of your Personal Information.
If your Personal Information is transferred by the University to other countries data transfer agreements will be used to protect your Personal Information.-
○Your checking this box documents that you have freely given your consent to the use of Personal Information as Idescribed in this GDPR Addendum. (1)
-
○I decline to give my consent to the use of Personal Information as described in GDPR (2)
-
○
Skip To: If GDPR Addendum for informed consent The researchers will collect personal information about you fo... = Your checking this box documents that you have freely given your consent to the use of Personal Information as described in this GDPR Addendum.
Exit 2 We thank you for your interest in our survey; consent to the use of Personal Information as described in this GDPR Addendum is required for participation.
Skip To: End of Survey If We thank you for your interest in our survey; consent to the use of Personal Information as descr... Is Displayed
Preamble 2 Please do not include any personal information that could be used to identify you in your responses to the following 3 questions.
Q3 What are you most concerned about in terms of the impacts of the COVID-19 pandemic on health, child development, families, and child and adolescent mental health?
__________________________________________________________________________________________
Q4 What do you think has been most helpful to children, adolescents, and families during the course of the pandemic?
__________________________________________________________________________________________
Q5 What are your top 3 research questions you believe we need to address regarding the pandemic and the mental health of children, adolescents, and their families?
__________________________________________________________________________________________
Preamble 3. Please tell us more about yourself
Q6 Gender Identity
-
○
Male (1)
-
○
Female (2)
-
○
Non-binary (3)
-
○
Prefer not to state (4)
Q7 To which ethnic/racial group(s) in your country of residence do you belong?
__________________________________________________________________________________________
Q8 Location
-
○
Urban (1)
-
○
Suburban (2)
-
○
Rural (3)
Q9 Over the last week how would you describe your community's COVID-19 current/new infection rates?
-
○
Almost none or no cases daily (1)
-
○
Increasing rates of new cases daily (2)
-
○
Decreasing rates of new cases daily (3)
-
○
About the same number of new cases daily (4)
-
○
Don't know (5)
Q10 Since the onset of the pandemic, how would you describe the total number of COVID-19 cases in your community?
-
○
Low to none (1)
-
○
Moderate (2)
-
○
High (3)
-
○
Very high (4)
-
○
Don't know (5)
Q11 What organization/group would categorize the PRIMARY perspective from which you are answering these questions—pick the one that best applies:
-
○Mental health care provider (1)
-
○Health care provider (2)
-
○A member of the public with in interest in child mental health (3)
-
○A parent of a child with a mental illness (4)
-
○A person with lived experience of mental illness (5)
-
○A person with a family member with a mental illness (6)
-
○A leader in an organization/foundation focused on child mental illness (7)
-
○A decision maker for an organization/foundation involved in funding for research focused on child mental health (8)
-
○A person involved in political decision making (9)
-
○A member of a support group or network or organization focused on child mental illness (10)
-
○A researcher focused on child mental illness (11)
-
○A person involved in child education (12)
-
○A person involved in child protection/child welfare/child maltreatment services (13)
-
○Other (please specify) (14) ____________________
-
○
References
- 1.Novins DK, Althoff RR, Billingsley MK, et al. JAACAP's role in advancing the science of pediatric mental health and promoting the care of youth and families during the COVID-19 pandemic. J Am Acad Child Adolesc Psychiatry. 2020;59:686–688. doi: 10.1016/j.jaac.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zeytinoglu S, Morales S, Lorenzo NE, et al. A developmental pathway from early behavioral inhibition to young adults' anxiety during the COVID-19 pandemic. J Am Acad Child Adolesc Psychiatry. [DOI] [PMC free article] [PubMed]
- 3.Penner F, Ortiz JH, Sharp C. Change in youth mental health during the COVID-19 pandemic in a majority Hispanic/Latinx US sample. J Am Acad Child Adolesc Psychiatry. [DOI] [PubMed]
- 4.Copeland WE, McGinnis E, Bai Y, et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry. 2021;60:134–141. doi: 10.1016/j.jaac.2020.08.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen IH, Chen C-Y, Pakpour AH, Griffiths MD, Lin C-Y. Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. J Am Acad Child Adolesc Psychiatry. 2020;59:1099–1102. doi: 10.1016/j.jaac.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Journal of the American Academy of Child and Adolescent Psychiatry . 2021. COVID-19 Paper Collection.https://www.jaacap.org/covid-19 [Google Scholar]
- 7.Isumi A, Doi S, Yamaoka Y, Takahashi K, Fujiwara T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 2020;110 doi: 10.1016/j.chiabu.2020.104680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patrick SW, Henkhaus LE, Zickafoose JS, et al. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020;146 doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- 9.Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health. 2020;17:8479. doi: 10.3390/ijerph17228479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Czeisler M, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 Pandemic—United States, June 24−30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheek JA, Craig SS, West A, Lewena S, Hiscock H. Emergency department utilisation by vulnerable paediatric populations during the COVID-19 pandemic. Emerg Med Australas. 2020;32:870–871. doi: 10.1111/1742-6723.13598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldman RD, Grafstein E, Barclay N, Irvine MA. Portales-Casamar E. Paediatric patients seen in 18 emergency departments during the COVID-19 pandemic. Emerg Med J. 2020;37:773–777. doi: 10.1136/emermed-2020-210273. [DOI] [PubMed] [Google Scholar]
- 13.Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM. Mental health-related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1−October 17, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1675–1680. doi: 10.15585/mmwr.mm6945a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holland KM, Jones C, Vivolo-Kantor AM, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic [published online ahead of print February 3, 2021]. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2020.4402. [DOI] [PMC free article] [PubMed]
- 15.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blei DM, Ng AY, Jordan MI. Latent dirichlet allocation. J Machine Learn Res. 2003;3:993–1022. [Google Scholar]
- 17.MATLAB. 2021. https://www.mathworks.com/products/matlab.html. Accessed March 7, 2021.
- 18.Chapman AL, Hadfield M, Chapman CJ. Qualitative research in healthcare: an introduction to grounded theory using thematic analysis. J R Coll Physicians Edinb. 2015;45:201–205. doi: 10.4997/JRCPE.2015.305. [DOI] [PubMed] [Google Scholar]
- 19.Strauss A, Corbin JM. Sage Publications; Thousand Oaks, CA: 1990. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. [Google Scholar]
- 20.Flick U. Sage Publications; Thousand Oaks, CA: 2009. An Introduction to Qualitative Research. [Google Scholar]
- 21.Lawson M, Piel MH, Simon M. Child maltreatment during the COVID-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Negl. 2020;110 doi: 10.1016/j.chiabu.2020.104709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grose J. The pandemic is a ‘mental health crisis’ for parents. New York Times. September 9, 2020 https://www.nytimes.com/2020/09/09/parenting/mental-health-parents-coronavirus.html [Google Scholar]
- 23.Goldberg E. Teens in Covid isolation: ‘I felt like I was suffocating. New York Times. November 12, 2020 https://www.nytimes.com/2020/11/12/health/covid-teenagers-mental-health.html [Google Scholar]
- 24.Levin D. How the pandemic has been devastating for children from low-income families. New York Times. December 29, 2020 https://www.nytimes.com/2020/12/29/us/coronavirus-trauma-young-people.html [Google Scholar]
- 25.Myers K, Cain S. Practice parameter for telepsychiatry with children and adolescents. J Am Acad Child Adolesc Psychiatry. 2008;47:1468–1483. doi: 10.1097/CHI.0b013e31818b4e13. [DOI] [PubMed] [Google Scholar]
- 26.Clinical Update: telepsychiatry with children and adolescents. J Am Acad Child Adolesc Psychiatry. 2017;56:875–893. doi: 10.1016/j.jaac.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 27.Myers K, Vander Stoep A, Zhou C, McCarty CA, Katon W. Effectiveness of a telehealth service delivery model for treating attention-deficit/hyperactivity disorder: a community-based randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2015;54:263–274. doi: 10.1016/j.jaac.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Novins DK, Althoff RR, Billingsley MK, et al. Bias, the scientific method, and the journal. J Am Acad Child Adolesc Psychiatry. 2018;57:71. doi: 10.1016/j.jaac.2017.12.006. [DOI] [PubMed] [Google Scholar]