Abstract
Background
To assess the effects of policy of selective versus routine episiotomy on mother and baby for women delivering vaginally in Shanghai and whether the hospital type has any effect on the outcomes.
Method
This was a multi-center retrospective cohort study in Shanghai between March 2015 and May 2017. The study population were vaginal births with selective or routine episiotomy (n = 5478) in 20 secondary or tertiary hospitals. Main Outcome Measure was the incidence of severe perineal lacerations. The adjusted odds ratios (aOR) and 95% confidence intervals (CI) were estimated by logistic regression and presented as the effect sizes. All models were stratified by the utilization of level (secondary and tertiary) and type (general and Obstetric) of hospital.
Results
The primary outcome was not significantly different between vaginal births with routine and selective episiotomy. Patients with selective episiotomy had a lower risk of postpartum hemorrhage, and newborns in the selective episiotomy group had a lower risk of shoulder dystocia and Neonatal Ward compared to those with routine episiotomy. Newborns in selective episiotomy group had a lower risk of birth injury in tertiary hospital. However, newborns in selective episiotomy group had a higher risk of birth injury in general hospitals.
Conclusion
Selective episiotomy is safe and can be recommended over routine episiotomy in obstetric and tertiary hospital settings in China.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-022-04790-0.
Keywords: Vaginal delivery, Selective episiotomy, Routine episiotomy, Perineal lacerations, Cohort study
Introduction
Vaginal delivery is considered a preferred method of delivery, although cesarean delivery has been increasing over the recent decades. Compared to cesarean delivery, which may be necessary in order to prevent adverse outcomes or to save life, the primary maternal benefit of vaginal delivery is less anesthetic and surgical complications, including less hemorrhage requiring transfusion or hysterectomy, less bowel or bladder injury, less postoperative ileus, less amniotic fluid embolism, less air embolism and less thromboembolic disease [1, 2]. Other maternal benefit of vaginal delivery is less long-term risks including less uterine rupture, less recurrent cesarean delivery, lower abnormal placentation risks including previa/accreta [3, 4]. Fetal benefits include higher likelihood of breast-feeding, shorter hospital admission, decreased rates of respiratory distress syndrome, and lower risk of respiratory-related NICU admission [2]. While several problems have been reported with vaginal birth. A major problem in vaginal birth is the risk of vagina and perineal tears leading to pain, bleeding, infection, dyspareunia and even a prolonged hospital stay. Subsequently, severe perineal tears increase the risk of prolapse of pelvic organs and fecal incontinence [5].
Episiotomy is a surgical incision performed during the delivery process to expand the vaginal opening in order to reduce the risk of lacerations of the posterior wall and severe perineal lacerations (3rd or 4th degree) to avoid injury to the pelvic floor and facilitate the birth of the baby [6, 7]. It can provide enough space to allow for assisted deliveries with forceps or vacuums to shorten labor and reduce pain [8, 9]. However, with routine use of episiotomy, the rate of unnecessary perineal tear is increased. Studies have shown that the routine use of episiotomy is associated with a higher prevalence of posterior wall perineal tear and severe perineal tear [10–12]. The potential long-term complications of episiotomy include dyspareunia, anorectal dysfunction and sexual dysfunction [13]. Therefore, routine episiotomy rates in Western developed countries have dropped from 70 to 15% since 1983 [14].
To better refine the use of episiotomy, selective use of episiotomy was advocated. Several studies have shown that selective use of episiotomy was preferable to routine episiotomy [15] with respect to the risk of lacerations of the posterior wall and unnecessary perineal lacerations [16]. However, in places where marked reduction in the rate of episiotomy was achieved, there was an increase in the occurrence of severe perineal lacerations [17]. Ethnicity may play a role in the long term effects of perineal injury as described by Abdool [18]. The perineal tear is closely related not only to the size and the position of the fetus, and the size of the pelvis of the woman, but also to the conditions of the perineal-associated muscles and ligaments. Whether selective use of episiotomy is better than routine use of episiotomy has not been systematically assessed in different ethnic groups worldwide.
In China, the rate cesarean increased from 28.8% in 2008 to 34.9% in 2014 [19], a significant proportion of which were without medical indication. However, recent studies have shown that vaginal births have become more frequent in recent since the promulgation of the two-child policy in 2015 [20]. Nowadays, selective episiotomy is preferred over routine episiotomy in most developed countries, However, it is uncertain whether selective episiotomy should be promoted in China considering the differences between ethnic groups concerning the risk of perineal laceration following vaginal delivery [21]. The aim of the present study was to assess the effects of policy of selective versus routine episiotomy on mother and baby for women delivering vaginally in Shanghai and whether the hospital type has any effect on the outcomes.
Methods
Study population
The was a multi-center, retrospective cohort study in Shanghai between March 2015 and May 2017. The participating hospitals were solicited through obstetric conferences and networks. Those that expressed an interest were asked to provide basic information about the hospitals. There was a total of 20 participating hospitals, including 13 secondary and 7 tertiary hospitals (11 general hospitals and 9 obstetric hospitals). Eligible subjects were singleton pregnancies at 34+ weeks of gestation in primiparous women with vaginal deliveries in cephalic presentation. Medical records were retrieved and reviewed, and information was extracted by trained research nurses. Exclusion criteria included multiple pregnancy, non-cephalic pregnancy, gestation weeks > 42, age < 18 or age > 45.This methodology has been used in the WHO Global Survey of Maternal and Perinatal Health and the WHO Multi-Country Survey of Maternal and Newborn Health [22, 23]. A data coordination center was responsible for the management and maintenance of the database and website, coordination among hospitals, investigators’ training, and quality control of the data. A logic check function was programmed in the database for preventing missing items and data entry errors. Data administrators checked the data regularly and contacted the hospital investigators to fill in omissions or correct errors.
Covariates
Individual covariates were maternal characteristics including maternal age, body mass index (BMI), pre-existing medical conditions such as diabetes, cardiac diseases, hyperthyroidism or hypothyroidism, birthweight, thyroid disease, and gestational complications. Institute covariates were the level (secondary vs. tertiary) and type of hospital (general vs. obstetric).
Exposures and outcomes
The exposure variable was the hospital policy for selective vs. routine episiotomy. Selective episiotomy mean episiotomy was done when the obstetrician deems it necessary. Indications of selective episiotomy include the size of fetus, perineal conditions, and the possibility of vaginal assistance. Routine episiotomy mean that all women had an episiotomy. The group was determined by hospital policy. There were 10 hospitals in the group of routine episiotomy and 10 in the group of selective episiotomy.
The primary outcome was severe perineal laceration (3rd or 4th degree) and/or vaginal trauma [24]. Secondary outcomes were major adverse maternal and neonatal outcomes, including meconium-stained amniotic fluid, fetal distress, shoulder dystocia, dehiscence, postpartum hemorrhage, transfusion, puerperal infection, amniotic fluid embolism, maternal thrombosis, admission into intensive care unit, birth injury, 5 min APGAR score ≤ 7, and admission to NICU.
Statistical analysis
To better represent selective episiotomy with routine episiotomy in Shanghai overall, we calculated a weight for each woman in the survey using the number of deliveries in each hospital. Unweighted results were showed in supplementary material.
Hospital level and type was considered as a post stratification factor. Adverse maternal and infant outcomes in routine episiotomy vs. selective episiotomy were compared by chi-square tests. Multivariable logistic regression was used to estimate the effects of selective vs. routine episiotomy on adverse maternal and infant outcomes, adjusting for potential confounders. Potential confounders included maternal age at childbirth, BMI, use of assisted reproductive technology, induced labor, pregnancy-induced hypertension, preexisting diabetes, gestational diabetes and pre-existing cardiac diseases. All analyses were performed using SPSS version 22.0 (IBM, Somers, NY). Two-tailed P values < 0.05 were considered statistically significant.
Funding
This study was funded by the Shanghai Municipal Commission of Health and Family Planning (GWIV-26) and Pudong Commission of Health and Family Planning (PW2019D-13).
Results
A total of 21,360 women gave births in study hospitals between March, 2015 and May, 2017, and 5478 women met the study inclusion criteria and exclusion criteria. Of these, 75.3% patients were assessed with policy of selective episiotomy, 24.7% patients were treated with policy of routine episiotomy (Fig. 1).
Fig. 1.
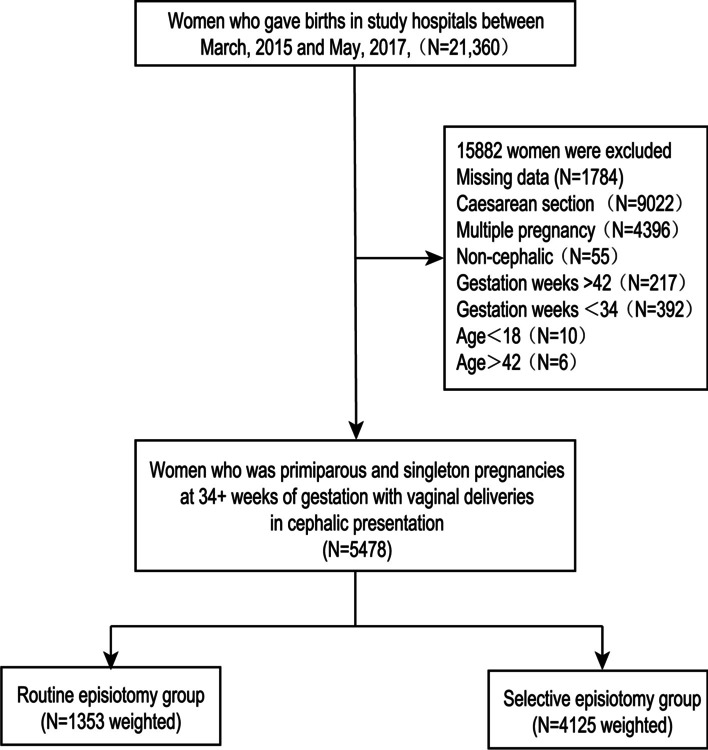
Study flow chart
Demographic and clinical characteristics of study participants are shown in Table 1 and Table S1. The patients with selective episiotomy had advanced age compared to the patients with routine episiotomy (27.10 vs 27.94, P < 0.05). Pre-existing cardiac diseases was more common in women with selective episiotomy (0.55% vs 1.09%, P < 0.05).
Table 1.
Characteristics at baseline (weighted)
| Characteristics | Routine episiotomy (1353) | Selective episiotomy (4125) | P | ||
|---|---|---|---|---|---|
| mean | 95%CI | mean | 95%CI | ||
| age | 27.96 | 27.82–28.11 | 28.32 | 28.22–28.43 | < 0.05 |
| -20 | 33 | 2.44 | 34 | 0.83 | |
| 20–34 | 1283 | 94.86 | 4000 | 96.95 | |
| 35- | 36 | 2.70 | 92 | 2.22 | |
| BMI | 21.22 | 21–21.34 | 21.18 | 21.09–21.27 | 0.60 |
| −18.5 | 206 | 15 | 522 | 12.64 | |
| 18.5–24 | 936 | 69 | 3079 | 74.63 | |
| 24- | 210 | 16 | 525 | 12.73 | |
| Diabetes | 4 | 0.32 | 6 | 0.15 | 0.21 |
| n | % | n | % | P | |
| Pre-existing cardiac diseases | 7 | 0.54 | 73 | 1.77 | < 0.05 |
| Pre-existing renal disease | 3 | 0.21 | 10 | 0.25 | 0.84 |
| Pre-existing autoimmune disease | 2 | 0.16 | 6 | 0.15 | 0.90 |
| Pre-existing hyperthyroidism | 6 | 0.46 | 24 | 0.58 | 0.61 |
| Pre-existing hypothyroidism | 17 | 1.25 | 59 | 1.42 | 0.63 |
BMI Body mass index
The incidences of pregnancy complications are presented in Table 2 and Table S2. More women had hypothyroidism (8.7% vs 5.55%, P < 0.05) and pregnancy-induced hypertension syndrome (14.34% vs 12.14%, P < 0.05) in the routine episiotomy group.
Table 2.
Current pregnancy complications (weighted)
| Characteristics | Routine episiotomy (1353) | Selective episiotomy (4125) | P | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| ART | 19 | 1.38 | 88 | 2.13 | 0.08 |
| Hyperthyroidism | 8 | 0.61 | 26 | 0.63 | 0.96 |
| Hypothyroidism | 99 | 7.29 | 202 | 4.89 | 0.05 |
| Other thyroidism | 14 | 1.03 | 68 | 1.65 | 0.10 |
| PIH | 191 | 14.1 | 496 | 12.02 | < 0.05 |
| GDM | 146 | 10.82 | 415 | 10.05 | 0.42 |
| placental abruption | 1 | 0.05 | 9 | 0.22 | 0.19 |
| PROM | 317 | 23.42 | 1022 | 24.77 | 0.32 |
| Prenatal stillbirth | 0 | 0.05 | 3 | 0.08 | 0.39 |
ART Assisted reproductive technology, PIH Pregnancy-induced hypertension syndrome, GDM Gestational Diabetes Mellitus, PROM Premature rupture of membranes
The incidence rates of adverse maternal and neonatal outcomes are presented in Tables 3, 4 and Table S3. The rate of episiotomy in the selective episiotomy group was 33.55%, and those in routine episiotomy group was 81.84%. The incidence rate of severe perineal laceration was lower in the selective episiotomy, comvs routine episiotomypared to routine episiotomy. Besides, shoulder dystocia, postpartum hemorrhage and neonatal ward were less frequent in newborns and pregnant women in selective episiotomy group. And more women had doula and term labor in the selective episiotomy group.
Table 3.
Selective versus Routine episiotomy: maternal (weighted)
| Characteristics | Routine episiotomy (1353) | Selective episiotomy (4125) | P | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Severe perineal laceration | 3 | 0.23 | 2 | 0.04 | < 0.05 |
| Term labor | 375 | 27.7 | 1462 | 35.43 | < 0.05 |
| Doula | 127 | 9.4 | 2622 | 63.55 | < 0.05 |
| Meconium | 96 | 7.09 | 283 | 6.87 | 0.78 |
| Placenta accreta | 24 | 1.8 | 88 | 2.14 | 0.44 |
| Incompletely uterine rupture | 1 | 0.08 | 7 | 0.17 | 0.44 |
| Episiotomy | 1107 | 81.84 | 1384 | 33.55 | < 0.05 |
| Postpartum hemorrhage | 48 | 3.52 | 68 | 1.65 | < 0.05 |
| Transfusion | 6 | 0.48 | 14 | 0.35 | 0.48 |
| Puerperal infection | 3 | 0.19 | 20 | 0.48 | 0.15 |
| Vacuum or forceps delivery | 66 | 4.90 | 184 | 4.48 | 0.22 |
Table 4.
Selective versus Routine episiotomy: neonatal outcomes (weighted)
| Characteristics | Routine episiotomy (1353) | Selective episiotomy (4125) |
P | ||
|---|---|---|---|---|---|
| mean | 95%CI | mean | 95%CI | ||
| Birthweight | 3277.6 | 3261.8–3293.4 | 3295.9 | 3283.1–3308.6 | 0.12 |
| n | % | n | % | ||
| Fetal distress | 80 | 5.94 | 190 | 4.6 | 0.05 |
| Shoulder dystocia | 13 | 0.97 | 4 | 0.1 | < 0.05 |
| Birthweight | 3277.6 | 3261.8–3293.4 | 3295.9 | 3283.1–3308.6 | 0.12 |
| Apgar≤7 (5 min) | 2 | 0.12 | 11 | 0.28 | 0.29 |
| Birth injury | 243 | 17.96 | 708 | 17.15 | 0.49 |
| Congenital malformation | 30 | 2.19 | 65 | 1.58 | 0.13 |
| Neonatal Ward | 159 | 11.77 | 302 | 7.32 | < 0.05 |
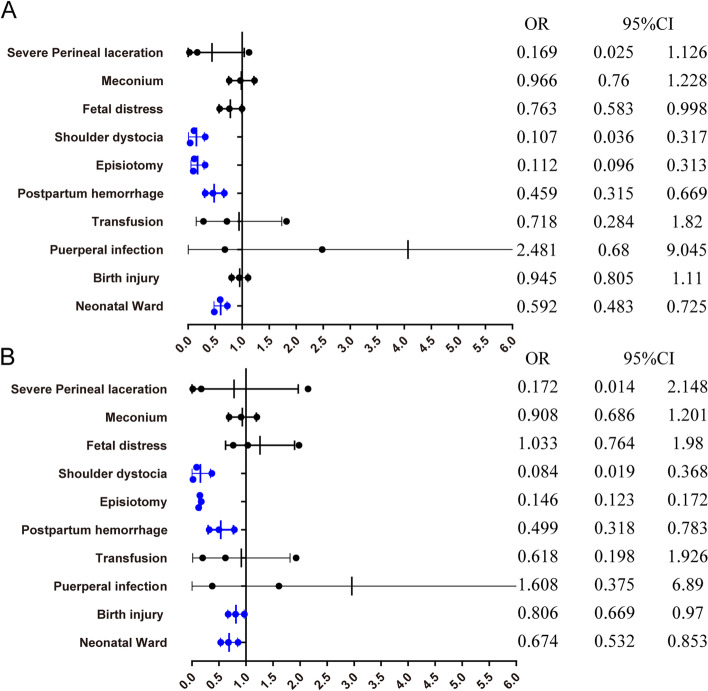
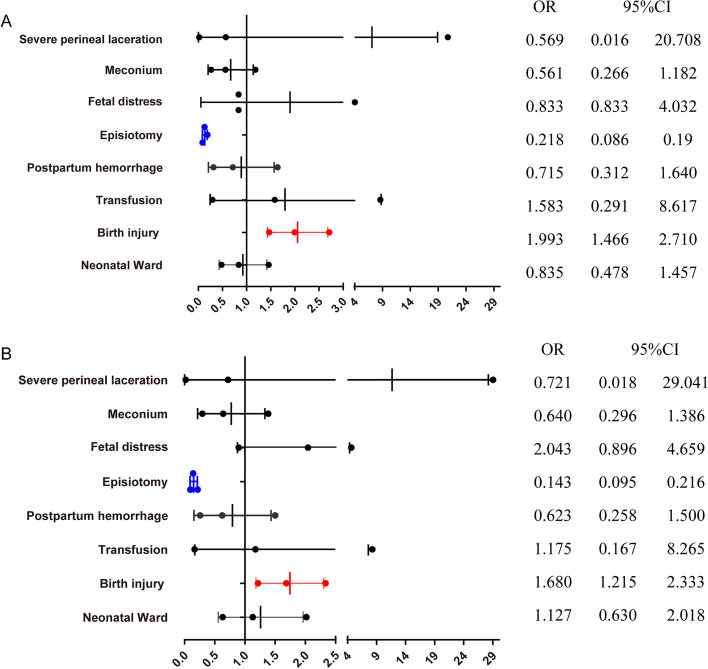
The outcomes comparing selective vs. routine episiotomy are showed in Fig. 2 and Table S4. The risk of severe perineal laceration was not significant different between selective vs. routine episiotomy, but the incidence rates were lower for shoulder dystocia (aOR = 0.084,95%CI:0.059–0.368), postpartum hemorrhage (aOR = 0.499,95%CI:0.318–0.783). And newborns in the selective episiotomy group are at lower risk of neonatal ward admission (aOR = 0.674,95%CI:0.532–0.853).
Fig. 2.
Selective versus Routine episiotomy: maternal and neonatal outcomes (weighted). A. Weighted data, crude ORs. B. Weighted data, adjusted ORs. The ORs were adjusted for maternal age at childbirth, BMI, the use of assisted reproductive technology, induced labor, pregnancy-induced hypertension, preexisting diabetes, hypothyroidism, pre-existing cardiac diseases and Placenta accrete
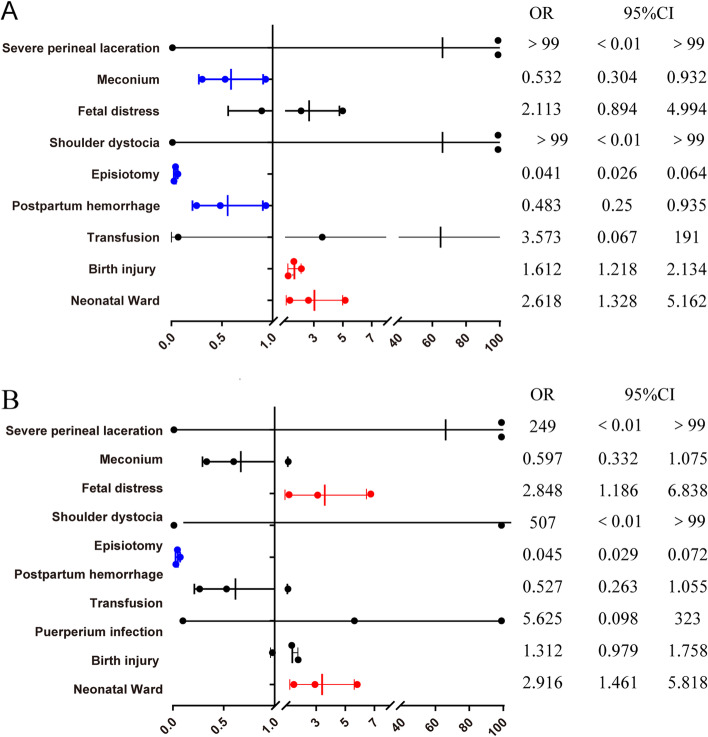
Comparisons of maternal and neonatal outcomes between selective vs routine episiotomy in secondary and tertiary hospitals are presented in Tables 5, 6, Figs. 3, 4, Table S5, and Table S6. In secondary hospitals, the rate of episiotomy in the selective episiotomy group was 38.93%, and those in routine episiotomy group was 94.01%. While in tertiary hospitals, the rate of episiotomy in the selective episiotomy group was 28.24%, and those in routine episiotomy group was 77.69%. The risk of severe perineal laceration was not significant different between selective and routine episiotomy in both secondary and tertiary hospitals. In secondary hospitals, newborns in the selective episiotomy group were at higher risk of neonatal ward admission; but in tertiary hospitals, newborns in the selective episiotomy group were in lower risk of neonatal ward (aOR = 0.462,95%CI:0.335–0.638), birth injury (aOR = 0.357,95%CI:0.258–0.493), postpartum hemorrhage (aOR = 0.328,95%CI:0.157–0.682), and shoulder dystocia (aOR =0.077,95%CI:0.051–0.553).
Table 5.
Selective versus Routine episiotomy in Secondary hospitals and Tertiary hospitals: maternal outcomes (weighted)
| Characteristics | Secondary hospitals (2393) | Tertiary hospitals(3085) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Routine episiotomy(343) | Selective episiotomy (2050) | P | Routine episiotomy(1010) | Routine episiotomy(2075) | P | |||||
| Severe perineal laceration | 0 | 0 | 1 | 0.06 | 0.65 | 4 | 0.31 | 0 | 0 | < 0.05 |
| Term labor | 83 | 24.25 | 630 | 30.72 | < 0.05 | 291 | 28.87 | 832 | 40.09 | < 0.05 |
| Doula | 104 | 30.28 | 1287 | 62.86 | < 0.05 | 23 | 2.28 | 1334 | 64.27 | < 0.05 |
| Meconium | 18 | 4.86 | 52 | 2.65 | 0.03 | 79 | 7.85 | 229 | 11.03 | < 0.05 |
| Placenta accreta | 4 | 1.27 | 38 | 1.83 | 0.46 | 20 | 1.98 | 51 | 2.44 | 0.42 |
| Incompletely uterine rupture | 1 | 0.16 | 3 | 0.13 | 0.89 | 1 | 0.05 | 4 | 0.20 | 0.30 |
| Episiotomy | 323 | 94.01 | 798 | 38.93 | < 0.05 | 784 | 77.69 | 586 | 28.24 | < 0.05 |
| Postpartum hemorrhage | 12 | 3.55 | 36 | 1.75 | < 0.05 | 35 | 3.50 | 32 | 1.54 | < 0.05 |
| Transfusion | 1 | 0.07 | 5 | 0.26 | 0.50 | 6 | 0.62 | 9 | 0.43 | 0.47 |
| Puerperal infection | 1 | 0.20 | 11 | 0.49 | 0.46 | 2 | 0.19 | 10 | 0.46 | 0.24 |
Table 6.
Selective versus Routine episiotomy in Secondary hospitals and Tertiary hospitals: neonatal outcomes (weighted)
| Characteristics | Secondary hospitals (2393) | Tertiary hospitals(3085) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Routine episiotomy(343) | Selective episiotomy (2050) | P | Routine episiotomy(1010) | Routine episiotomy(2075) | P | |||||
| mean | 95%CI | mean | 95%CI | mean | 95%CI | mean | 95%CI | |||
| Birthweight | 3280.5 | 3257.9–3303.2 | 3295.6 | 3278.5–3312.8 | 0.46 | 3276.6 | 3255.6–3297.6 | 3296.1 | 3277.1–3315.0 | 0.20 |
| n | % | n | % | n | % | n | % | n | ||
| Shoulder dystocia | 0 | 0 | 1 | 0.03 | 0.76 | 13 | 1.30 | 4 | 0.18 | < 0.05 |
| Apgar≤7 (5 min) | 0 | 0 | 5 | 0.22 | 0.38 | 2 | 0.15 | 7 | 0.33 | 0.37 |
| Birth injury | 69 | 20.18 | 594 | 28.96 | < 0.05 | 174 | 17.21 | 114 | 5.49 | < 0.05 |
| Congenital malformation | 2 | 0.53 | 22 | 1.08 | 0.34 | 28 | 2.76 | 43 | 2.07 | 0.23 |
| Neonatal Ward | 9 | 2.67 | 137 | 6.69 | < 0.05 | 150 | 14.88 | 165 | 7.94 | < 0.05 |
Fig. 3.
Selective versus Routine episiotomy in secondary hospitals: maternal and neonatal outcomes (weighted). A. Weighted data, crude ORs. B. Weighted data, adjusted ORs. The ORs were adjusted for maternal age at childbirth, BMI, the use of assisted reproductive technology, induced labor, pregnancy-induced hypertension, preexisting diabetes, hypothyroidism, pre-existing cardiac diseases and Placenta accrete
Fig. 4.
Selective versus Routine episiotomy in tertiary hospitals: maternal and neonatal outcomes (weighted). A. Weighted data, crude ORs. B. Weighted data, adjusted ORs. The ORs were adjusted for maternal age at childbirth, BMI, the use of assisted reproductive technology, induced labor, pregnancy-induced hypertension, preexisting diabetes, hypothyroidism, pre-existing cardiac diseases and Placenta accrete
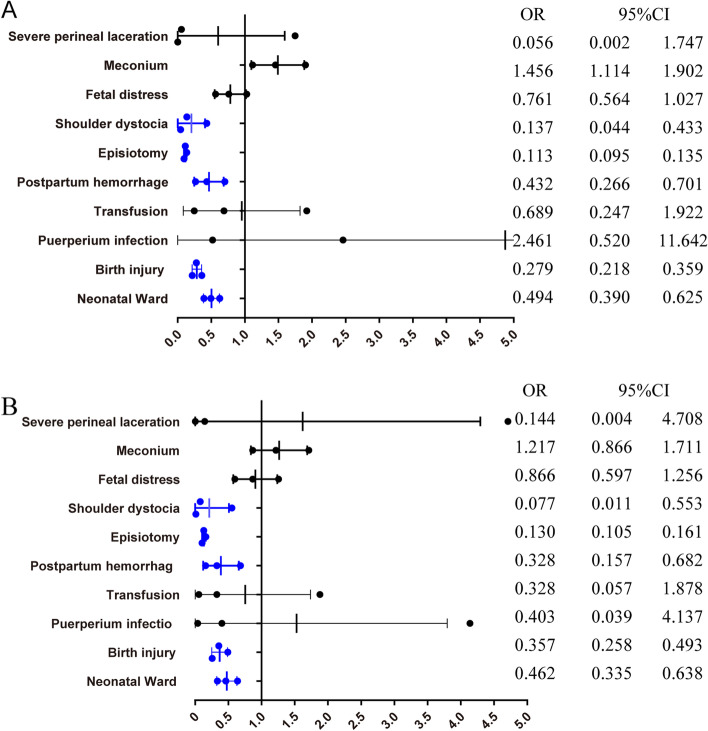
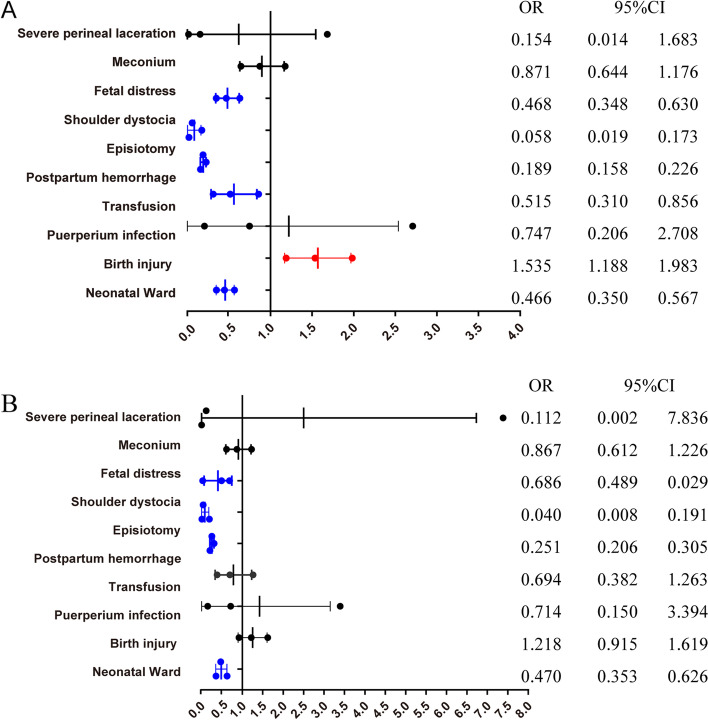
The incidence rates of maternal and neonatal outcomes comparing selective vs routine episiotomy in obstetric and general hospitals are presented in Tables 7, 8, Figs. 5, 6, Table S7, and Table S8. There was no significant difference in the primary outcome (severe perineal/vaginal trauma) between the two groups in both obstetric and general hospitals. In the obstetric hospitals, newborns in the selective episiotomy group had lower risks of neonatal ward (aOR = 0.47,95%CI:0.353–0.626), fetal distress (aOR = 0.686,95%CI:0.489–0.829), and shoulder dystocia (aOR = 0.04,95%CI:0.008–0.191), In contrast, newborns in the selective episiotomy group were in a higher risk of birth injury (aOR = 1.68,95%CI:1.215–2.333) in general hospitals.
Table 7.
Selective versus Routine episiotomy in Obstetric hospitals and General hospitals: maternal outcomes (weighted)
| Characteristics | Obstetric hospitals (4564) | General hospitals (914) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Routine episiotomy (689) | Selective episiotomy (3875) | P | Routine episiotomy (664) | Selective episiotomy (250) | P | |||||
| n | % | n | % | n | % | n | % | |||
| Severe perineal laceration | 1 | 0.21 | 1 | 0.03 | 0.08 | 2 | 0.25 | 1 | 0.14 | 0.76 |
| Term labor | 200 | 29.14 | 1361 | 35.12 | < 0.05 | 174 | 26.21 | 101 | 40.37 | < 0.05 |
| Augment | 229 | 33.27 | 841 | 21.70 | < 0.05 | 94 | 14.12 | 65 | 26.2 | < 0.05 |
| Doula | 40 | 5.89 | 2540 | 65.54 | < 0.05 | 87 | 13.03 | 81 | 32.65 | < 0.05 |
| Meconium | 55 | 8.05 | 275 | 7.08 | 0.37 | 41 | 6.09 | 9 | 3.51 | 0.12 |
| Placenta accreta | 14 | 2 | 83 | 2.15 | 0.80 | 11 | 1.58 | 5 | 1.91 | 0.74 |
| Incompletely uterine rupture | 0 | 0 | 7 | 0.18 | 0.27 | 1 | 0.15 | 0 | 0 | 0.54 |
| Episiotomy | 488 | 70.96 | 1226 | 31.64 | < 0.05 | 619 | 93.09 | 158 | 63.27 | < 0.05 |
| Postpartum hemorrhage | 21 | 2.99 | 61 | 1.56 | < 0.05 | 27 | 4.06 | 7 | 2.94 | 0.43 |
| Transfusion | 3 | 0.42 | 12 | 0.31 | 0.66 | 4 | 0.55 | 2 | 0.86 | 0.59 |
| Puerperal infection | 2 | 0.29 | 19 | 0.49 | 0.47 | 1 | 0.10 | 1 | 0.29 | 0.50 |
Table 8.
Selective versus Routine episiotomy in Obstetric hospitals and General hospitals: neonatal outcomes (weighted)
| Characteristics | Obstetric hospitals (4564) | General hospitals (914) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Routine episiotomy (689) | Selective episiotomy (3875) | P | Routine episiotomy (664) | Selective episiotomy (250) | P | |||||
| mean | 95%CI | mean | 95%CI | mean | 95%CI | mean | 95%CI | |||
| Birthweight | 3281.0 | 3250.7–3311.3 | 3297.7 | 3283.5–3312.0 | 0.36 | 3274.1 | 3255.8–3292.3 | 3266.8 | 3238–3295.6 | 0.68 |
| n | % | n | % | n | % | n | % | n | ||
| Fetal distress | 64 | 9.37 | 179 | 4.62 | < 0.05 | 16 | 2.39 | 11 | 4.30 | 0.13 |
| Shoulder dystocia | 13 | 1.89 | 4 | 0.11 | < 0.05 | 1 | 0.03 | 0 | 0 | 0.80 |
| Apgar≤7 (5 min) | 0 | 0 | 10 | 0.26 | 0.18 | 2 | 0.23 | 1 | 0.52 | 0.49 |
| Birth injury | 74 | 10.78 | 607 | 15.65 | < 0.05 | 169 | 25.39 | 101 | 40.41 | < 0.05 |
| Congenital malformation | 10 | 1.47 | 62 | 1.59 | 0.81 | 20 | 2.94 | 3 | 1.40 | 0.18 |
| Neonatal Ward | 104 | 15.09 | 284 | 7.34 | < 0.05 | 55 | 8.34 | 18 | 7.06 | 0.52 |
Fig. 5.
Selective versus Routine episiotomy in Obstetric hospitals: maternal and neonatal outcomes (weighted). A. Weighted data, crude ORs. B. Weighted data, adjusted ORs. The ORs were adjusted for maternal age at childbirth, BMI, the use of assisted reproductive technology, induced labor, pregnancy-induced hypertension, preexisting diabetes, hypothyroidism, pre-existing cardiac diseases and Placenta accrete
Fig. 6.
Selective versus Routine episiotomy in General hospitals: maternal and neonatal outcomes (weighted). A. Weighted data, crude ORs. B. Weighted data, adjusted ORs. The ORs were adjusted for maternal age at childbirth, BMI, the use of assisted reproductive technology, induced labor, pregnancy-induced hypertension, preexisting diabetes, hypothyroidism, pre-existing cardiac diseases and Placenta accrete
Discussion
Main findings
Vaginal birth, as a preferred delivery method, has many benefits such as less anesthetic and surgical complications, compared to cesarean delivery. While vaginal birth with malpresentation or fetal macrosomia, may cause serious perineal injury which may affect the quality of life. Episiotomy was designed to decrease the rate of serious perineal tears in vaginal deliveries, but routine episiotomy may be unnecessary [25]. For women where a spontaneous vagina birth was anticipated, a policy of selective episiotomy may result in 30% fewer women experiencing severe perineal/vaginal trauma in western country [26–28]. There is a lack of consensus on whether selective or routine episiotomy is preferred in China.
There have been multiple researches comparing selective versus routine episiotomy, they came to conflicting conclusion. Most trials reported no significant difference in the main outcome ‘severe perineal/vaginal trauma’ between the two groups, while some studies suggest a trend toward a greater risk of perineal lacerations in selective episiotomy [26, 29], but a randomized controlled clinical trial by Zuleta found that selective episiotomy reduced the rate of severe perineal lacerations [30]. The effect size was different of in each study, probably owing the differences in the definition and the reference group.
Our large population-based study in Shanghai found that mothers with selective episiotomy had no increased risk of severe perineal/vaginal trauma. The incidence of severe perineal lacerations (selective episiotomy 0.04%, routine episiotomy 0.23%) was similar to western developed countries [26]. Better yet, the mothers with selective episiotomy had a lower risk of postpartum hemorrhage, and newborns in the selective episiotomy group had a lower risk of shoulder dystocia and neonatal ward compared to those with routine episiotomy. Our results did not support the view that routine episiotomy was preferred in Shanghai. This observation is in agreement with several randomized controlled studies in western developed countries [26–28].
We observed that patients in tertiary and secondary hospitals with selective episiotomy were at a similar risk of severe perineal lacerations. In tertiary hospitals, newborns in the selective episiotomy group had lower risk of neonatal ward, but in secondary hospitals, newborns in the selective episiotomy group had higher risk of neonatal ward. This may be due to more experienced physicians and more advanced medical facilities in tertiary hospitals. Moreover, compared to patients with routine episiotomy, there was a lower risk of birth injuries, postpartum hemorrhage and shoulder dystocia with selective episiotomy in tertiary care hospitals where obstetricians could be more experienced in fetal assessment/monitoring might have reduced the risk of inappropriate vaginal delivery [31].
There was no difference in risks of severe perineal lacerations between selective episiotomy policy and routine episiotomy policy in gynecology specialty hospitals compared to general hospitals. But in general hospitals, patients with selective episiotomy policy had higher risk of birth injury. In China, patients are more willing to deliver in obstetric hospitals, so doctors in obstetric hospitals have more experience in handling complicated obstetric patients. We believe that obstetric care providers need more experience in the use of selective episiotomy. The injudicious use of selective episiotomy may decrease the rate of episiotomy but increase the risk of significant perineal lacerations. With more standardized training, patients in all hospitals can be handled appropriately under a policy of selective use of episiotomy.
Strengths
The strengths of this study include a large sample size with the contemporary data on Chinese pregnant women, the use of uniform definitions of study variables collected across all hospitals.
Limitations
There are some limitations in our study. First, we only investigated short-term neonatal outcomes. We have no data on potential long-term maternal and child health outcomes. Second, our conclusions may be applicable to secondary and tertiary care settings in urban areas only in China. More studies are required to understand whether the findings are applicable to other settings in China.
Conclusion
Selective episiotomy is safe and has a similar risk of severe perineal/vaginal trauma compared to routine episiotomy in all types of hospitals in Shanghai, China. Selective episiotomy may be advocated in obstetric and tertiary care settings in urban areas in China.
Supplementary Information
Acknowledgements
Not applicable.
Authors’ contributions
Shengyi Gu and Jindan Pei, Chenchen Zhou participated in interpretation of data and involved in drafting the manuscript. Xiaobo Zhao, and Sheng Wan analyzed the data. Jun Zhang, Adewumi Adanlawo and Zhongcheng Luo critically revised the manuscript. Guizhu Wu and Xiaolin Hua made substantial contributions to conception and design, interpreted the data, and critically revised the manuscript. All authors read and approved the final manuscript.
Funding
This study was funded by the Shanghai Municipal Commission of Health and Family Planning (GWIV-26, 202040128) and Pudong Commission of Health and Family Planning (PW2019D-13).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the research ethics board of Shanghai Xinhua Hospital (Approved number: XHEC-C − 2016-095). All methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects and/or their legal guardian.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shengyi Gu and Jindan Pei contributed equally to this work.
Contributor Information
Guizhu Wu, Email: wugz6666@126.com.
Xiaolin Hua, Email: xiaolin_hua@tongji.edu.cn.
References
- 1.National Institutes of Health Consensus Development conference statement Vaginal birth after cesarean: new insights march 8-10, 2010. Obstet Gynecol. 2010;115(6):1279–1295. doi: 10.1097/AOG.0b013e3181e459e5. [DOI] [PubMed] [Google Scholar]
- 2.Gregory KD, Jackson S, Korst L, Fridman M. Cesarean versus vaginal delivery: whose risks? Whose benefits? Am J Perinatol. 2012;29(1):7–18. doi: 10.1055/s-0031-1285829. [DOI] [PubMed] [Google Scholar]
- 3.Ananth CV, Smulian JC, Vintzileos AM. The association of placenta previa with history of cesarean delivery and abortion: a metaanalysis. Am J Obstet Gynecol. 1997;177(5):1071–1078. doi: 10.1016/S0002-9378(97)70017-6. [DOI] [PubMed] [Google Scholar]
- 4.Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, Moawad AH, Caritis SN, Harper M, Wapner RJ, Sorokin Y, Miodovnik M, Carpenter M, Peaceman AM, O'Sullivan MJ, Sibai B, Langer O, Thorp JM, Ramin SM, Mercer BM. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006;107(6):1226–1232. doi: 10.1097/01.AOG.0000219750.79480.84. [DOI] [PubMed] [Google Scholar]
- 5.Leeman L, Rogers R, Borders N, Teaf D, Qualls C. The effect of perineal lacerations on pelvic floor function and anatomy at 6 months postpartum in a prospective cohort of nulliparous women. Birth. 2016;43(4):293–302. doi: 10.1111/birt.12258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Serati M, Salvatore S, Rizk D. Episiotomy in modern clinical practice: friend or foe? Int Urogynecol J. 2019;30(5):669–671. doi: 10.1007/s00192-019-03912-1. [DOI] [PubMed] [Google Scholar]
- 7.Goueslard K, Cottenet J, Roussot A, Clesse C, Sagot P, Quantin C. How did episiotomy rates change from 2007 to 2014? Population-based study in France. BMC pregnancy and childbirth. 2018;18(1):208. doi: 10.1186/s12884-018-1747-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thacker SB, Banta HD. Benefits and risks of episiotomy: an interpretative review of the English language literature, 1860-1980. Obstet Gynecol Surv. 1983;38(6):322–338. doi: 10.1097/00006254-198306000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Amorim MM, Coutinho IC, Melo I, Katz L. Selective episiotomy vs. implementation of a non-episiotomy protocol: a randomized clinical trial. Reprod Health. 2017;14(1):55. [DOI] [PMC free article] [PubMed]
- 10.Gabbe SG, DeLee JB. The prophylactic forceps operation. 1920. Am J Obstet Gynecol. 2002;187(1):254. doi: 10.1067/mob.2002.123205. [DOI] [PubMed] [Google Scholar]
- 11.Islam A, Hanif A, Ehsan A, Arif S, Niazi SK, Niazi AK. Morbidity from episiotomy. J Pak Med Assoc. 2013;63(6):696–701. [PubMed] [Google Scholar]
- 12.Belihu FB, Small R, Davey M-A. Episiotomy and severe perineal trauma among eastern African immigrant women giving birth in public maternity care: A population based study in Victoria, Australia. Women and Birth. 2017;30(4):282–290. doi: 10.1016/j.wombi.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Gun I, Dogan B, Ozdamar O. Long- and short-term complications of episiotomy. Turk J Obstet Gynecol. 2016;13(3):144–148. doi: 10.4274/tjod.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldberg J, Holtz D, Hyslop T, Tolosa JE. Has the use of routine episiotomy decreased? Examination of episiotomy rates from 1983 to 2000. Obstet Gynecol. 2002;99(3):395–400. doi: 10.1016/s0029-7844(01)01756-2. [DOI] [PubMed] [Google Scholar]
- 15.Correa Junior MD, Passini JR. Selective episiotomy: indications, Techinique, and association with severe perineal lacerations. Rev Bras Ginecol Obstet. 2016;38(6):301–307. doi: 10.1055/s-0036-1584942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):Cd000081. [DOI] [PMC free article] [PubMed]
- 17.Raisanen S, Cartwright R, Gissler M, Kramer MR, Laine K, Jouhki MR, Heinonen S. Changing associations of episiotomy and anal sphincter injury across risk strata: results of a population-based register study in Finland 2004-2011. BMJ Open. 2013;3(8):e003216. doi: 10.1136/bmjopen-2013-003216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abdool Z, Dietz HP, Lindeque BG. Ethnic differences in the levator hiatus and pelvic organ descent: a prospective observational study. Ultrasound Obstet Gynecol. 2017;50(2):242–246. doi: 10.1002/uog.17297. [DOI] [PubMed] [Google Scholar]
- 19.Li HT, Luo S, Trasande L, Hellerstein S, Kang C, Li JX, Zhang Y, Liu JM, Blustein J. Geographic variations and temporal trends in cesarean delivery rates in China, 2008-2014. Jama. 2017;317(1):69–76. doi: 10.1001/jama.2016.18663. [DOI] [PubMed] [Google Scholar]
- 20.Wang E, Hesketh T. Large reductions in cesarean delivery rates in China: a qualitative study on delivery decision-making in the era of the two-child policy. BMC Pregnancy Childbirth. 2017;17(1):405. doi: 10.1186/s12884-017-1597-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grobman WA, Bailit JL, Rice MM, Wapner RJ, Reddy UM, Varner MW, Thorp JM, Jr, Leveno KJ, Caritis SN, Iams JD, Tita AT, Saade G, Rouse DJ, Blackwell SC, Tolosa JE, VanDorsten JP. Racial and ethnic disparities in maternal morbidity and obstetric care. Obstet Gynecol. 2015;125(6):1460–1467. doi: 10.1097/AOG.0000000000000735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shah A, Faundes A, Machoki MI, Bataglia V, Amokrane F, Donner A, Mugerwa K, Carroli G, Fawole B, Langer A, Wolomby JJ, Naravaez A, Nafiou I, Kublickas M, Valladares E, Velasco A, Zavaleta N, Neves I, Villar J. Methodological considerations in implementing the WHO global survey for monitoring maternal and perinatal health. Bull World Health Organ. 2008;86(2):126–131. doi: 10.2471/BLT.06.039842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Souza JP, Gülmezoglu AM, Vogel J, Carroli G, Lumbiganon P, Qureshi Z, Costa MJ, Fawole B, Mugerwa Y, Nafiou I, Neves I, Wolomby-Molondo J-J, Bang HT, Cheang K, Chuyun K, Jayaratne K, Jayathilaka CA, Mazhar SB, Mori R, Mustafa ML, Pathak LR, Perera D, Rathavy T, Recidoro Z, Roy M, Ruyan P, Shrestha N, Taneepanichsku S, Tien NV, Ganchimeg T, Wehbe M, Yadamsuren B, Yan W, Yunis K, Bataglia V, Cecatti JG, Hernandez-Prado B, Nardin JM, Narváez A, Ortiz-Panozo E, Pérez-Cuevas R, Valladares E, Zavaleta N, Armson A, Crowther C, Hogue C, Lindmark G, Mittal S, Pattinson R, Stanton ME, Campodonico L, Cuesta C, Giordano D, Intarut N, Laopaiboon M, Bahl R, Martines J, Mathai M, Merialdi M, Say L. Moving beyond essential interventions for reduction of maternal mortality (the WHO multicountry survey on maternal and newborn health): a cross-sectional study. Lancet (London, England) 2013;381(9879):1747–1755. doi: 10.1016/S0140-6736(13)60686-8. [DOI] [PubMed] [Google Scholar]
- 24.Bradley CS, Richter HE, Gutman RE, Brown MB, Whitehead WE, Fine PM, Hakim C, Harford F, Weber AM. Risk factors for sonographic internal anal sphincter gaps 6-12 months after delivery complicated by anal sphincter tear. Am J Obstet Gynecol. 2007;197(3):310.e311–310.e315. doi: 10.1016/j.ajog.2007.06.034. [DOI] [PubMed] [Google Scholar]
- 25.Corrêa Junior MD, Passini JR. Selective episiotomy: indications, Techinique, and association with severe perineal lacerations. Revista brasileira de ginecologia e obstetricia : revista da Federacao Brasileira das Sociedades de Ginecologia e Obstetricia. 2016;38(6):301–307. doi: 10.1055/s-0036-1584942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jiang H, Qian X, Carroli G, Garner P. Selective versus routine use of episiotomy for vaginal birth. The Cochrane database of systematic reviews. 2017;2:CD000081. doi: 10.1002/14651858.CD000081.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forey P-L, Lallemant M, Bourtembourg-Matras A, Eckman-Lacroix A, Ramanah R, Riethmuller D, et al. Impact of a selective use of episiotomy combined with Couder's maneuver for the perineal protection. Arch Gynecol Obstet. 2020. [DOI] [PubMed]
- 28.Ghulmiyyah L, Sinno S, Mirza F, Finianos E, Nassar AH. Episiotomy: history, present and future - a review. J Matern Fetal Neonatal Med. 2020:1–6. [DOI] [PubMed]
- 29.Macleod M, Goyder K, Howarth L, Bahl R, Strachan B, Murphy DJ. Morbidity experienced by women before and after operative vaginal delivery: prospective cohort study nested within a two-Centre randomised controlled trial of restrictive versus routine use of episiotomy. Bjog. 2013;120(8):1020–1026. doi: 10.1111/1471-0528.12184. [DOI] [PubMed] [Google Scholar]
- 30.Rodriguez A, Arenas EA, Osorio AL, Mendez O, Zuleta JJ. Selective vs routine midline episiotomy for the prevention of third- or fourth-degree lacerations in nulliparous women. Am J Obstet Gynecol. 2008;198(3):285.e281–285.e284. doi: 10.1016/j.ajog.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 31.Maskey S, Bajracharya M, Bhandari S. Prevalence of cesarean section and its indications in A tertiary care hospital. JNMA J Nepal Med Assoc. 2019;57(216):70–73. doi: 10.31729/jnma.4282. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.