ABSTRACT
Background
Nutrition labels on prepackaged foods are an important source of nutrition information; however, differences in comprehension of varying label formats can limit their use and effectiveness.
Objectives
This study examined levels and correlates of consumers’ self-reported understanding of Nutrition Facts tables (NFts) and front-of-package (FOP) labels, as well as functional NFt understanding.
Methods
Adults (≥18 y) in Australia (n = 3901), Canada (n = 4107), Mexico (n = 4012), the United Kingdom (n = 5121), and the United States (n = 4445) completed online surveys in November/December 2018. Descriptive statistics summarized sample profiles by country. Linear regression models examined the association between label understanding (self-reported NFt and FOP, functional NFt) and consumer dietary behaviors, functional nutrition knowledge, and sociodemographic characteristics. NFt understanding was measured in all countries, with FOP labeling assessed only in Mexico, Australia, and the United Kingdom.
Results
Self-reported and functional NFt understanding was significantly higher in the United States and Canada (P < 0.0001). In adjusted analyses, functional NFt understanding was significantly higher among women compared to men (P < 0.0001); respondents from the “majority” ethnic group in their respective countries compared with minority ethnic groups (P < 0.0001); those with higher education levels (P < 0.0001) and functional nutrition knowledge compared with their lower education and nutrition knowledge counterparts (P < 0.0001), respectively; and those making efforts to consume less sodium, sugar, or fat compared with those not reporting dietary efforts (P < 0.0001). Self-reported FOP label understanding was significantly higher for interpretive labeling systems in Australia (health star ratings) and the United Kingdom (traffic lights) compared with Mexico's Guideline Daily Amounts (GDAs) (P < 0.0001).
Conclusions
Nutrition labels requiring greater numeracy skills (i.e., NFts, GDAs) were more difficult for consumers to understand than interpretive FOP labels (i.e., traffic lights). Differences in NFt and FOP label understanding by income adequacy and education suggest potential disparities in labeling policy effects among vulnerable subgroups.
Keywords: nutrition label, nutrition facts table, front-of-package label, food labeling policy, consumer understanding, international
Introduction
Nutrition labels on food packages provide nutrient content information at the point-of-purchase to support consumers in making informed choices (1). Nutrition Facts tables (NFts)—tables in a standard format found on the back or side of packaged foods listing calories per serving and percentage daily value for key nutrients—are one of the most commonly used sources of nutrition information, particularly among consumers trying to modify their dietary intake (2, 3). However, studies have found that consumers generally struggle with interpreting and applying NFt information (4–7).
Poor NFt understanding has been observed across countries, with studies using both self-reported and functional tests of consumer label understanding identifying issues with numeracy (6–10). Indeed, consumers with lower education, income, or literacy are less likely to understand and therefore use NFts (4, 6, 8). These disparities in NFt understanding are troubling given those with lower socioeconomic status are also more vulnerable to poor dietary patterns and nutrition-related chronic disease due to other barriers in accessing healthy foods (11, 12).
In response to concerns about NFts, front-of-package (FOP) labels have been proposed as a policy solution for providing simple and interpretive nutrition information in a noticeable location on food packages (1, 13, 14). Several FOP labeling systems are in use globally and range in presentation (i.e., nutrient-specific compared with summary-indicator labels), design (i.e., various symbols, colours, sizes), and nutrient focus (13, 14). For example, nutrient-specific FOP labels [e.g., Guideline Daily Amounts (GDAs)] display information on specific nutrients from the NFt, often highlighting nutrients of public health concern such as sodium, saturated fats, and sugars (13, 14). Summary-indicator systems [e.g., Health Star Ratings (HSRs), Nutri-Score] summarize nutrient content and product healthfulness using algorithms to provide an overall score for the product (13, 14).
Overall, studies suggest FOP labels are easier for consumers to understand than NFts alone (1, 4, 15, 16). Among consumers with lower self-reported nutrition knowledge, income, and education, the preference for simpler FOP label designs is consistent with better understanding of these labeling systems (4, 17, 18).
Although many studies use self-reported measures of label understanding, consumers tend to overestimate their ability to use and apply label information (6, 10, 19), thereby making functional tests a preferred measure. Functional measures of label understanding, which commonly ask participants to complete a rating task comparing foods based on nutritional profile, have found that FOP labels have higher comprehension, and therefore greater potential to promote healthy food choices compared with numerical label formats such as the NFt or GDA (16–18, 20).
Label understanding is influenced by a variety of factors ranging from individual-level characteristics such as consumer nutrition knowledge and dietary practices, to broader nutrition education policies and national health promotion efforts (2, 3, 21). To date, few cross-country studies have been conducted examining understanding of nutrition labels, including potential disparities among subgroups. Using cross-sectional data from the International Food Policy Study (IFPS), this study aimed to determine levels and correlates of self-reported and functional nutrition label understanding across countries. In particular, 4 research questions were examined: 1) What are the levels of self-reported (NFt and FOP) label and functional NFt understanding across Australia, Canada, Mexico, the United Kingdom, and the United States? 2) Does self-reported FOP label understanding vary by label type (i.e., HSR compared with GDA)? 3) Is self-reported label understanding associated with functional label understanding and nutrition knowledge? and 4) Does label understanding vary by consumers’ dietary behaviors or sociodemographic characteristics?
Methods
Study design and participants
This study used cross-sectional data from the 2018 wave of the IFPS (22). Respondents aged ≥18 y were recruited through Nielsen Consumer Insights Global Panel and their partners’ panels, and completed web-based surveys in November/December 2018. The Nielsen panel is recruited using both probability and nonprobability recruitment methods in each country. After applying age- and sex-based quotas to facilitate recruitment of a diverse sample approximating known proportions in each country, e-mail invitations were sent to a random sample of panelists; panelists known to be ineligible were not invited. Surveys were conducted in English in Australia and the United Kingdom; in Spanish in Mexico; in English or French in Canada; and in English or Spanish in the United States. The median time to complete the survey across all countries was 40 min.
Of the 22,824 respondents who completed the 2018 IFPS survey, a subsample of 21,586 respondents from Australia (n = 3901), Canada (n = 4107), Mexico (n = 4012), the United Kingdom (n = 5121), and the United States (n = 4445) were included in the current study. Those with missing data for self-reported NFt understanding (n = 160), self-reported FOP label understanding (n = 153), functional NFt understanding (n = 29), Food Processing Knowledge (FoodProK) score (n = 17), dietary efforts (n = 122), food shopping role (n = 29), education (n = 69), ethnicity (n = 296), and income adequacy (n = 182) were excluded from analyses. All respondents provided informed consent prior to completing the survey and received remuneration in accordance with the panel's usual incentive structure (e.g., points-based or monetary rewards, chances to win prizes). The study was reviewed by and received ethics clearance through a University of Waterloo Research Ethics Committee (ORE# 21460). More details can be found in the 2018 IFPS Technical Report (22).
Measures
Self-reported understanding of food labels
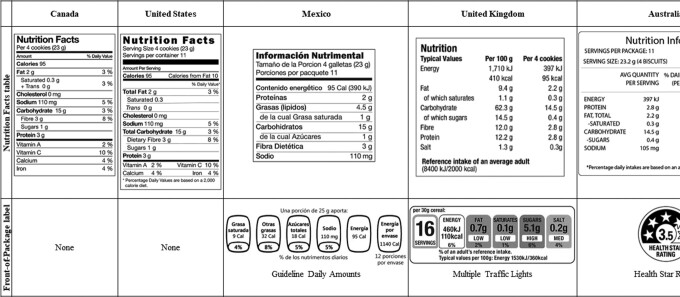
Participants were shown an image of the NFt that appears on packages in their country and asked, “Do you find this information … ‘very hard to understand,’ ‘hard to understand,’ ‘neither hard or easy to understand,’ ‘easy to understand,’ or ‘very easy to understand?’” In addition, participants in Australia, Mexico, and the United Kingdom were then shown an image of an FOP label for their respective countries and asked to respond to the same measure of self-reported understanding (Figure 1). This measure was adapted from the 2014 Food and Drug Agency Health and Diet Survey (23).
FIGURE 1.
Food labels by country in the International Food Policy Study survey.
Functional NFt understanding
Participants completed an online version of the Newest Vital Sign, which consists of 6 questions that test functional ability to use NFts (Supplemental Table 1). The Newest Vital Sign assesses respondents’ ability to make mathematical calculations (numeracy), read and apply label information (prose literacy), and understand the label information (document literacy) (24). It thus serves not only as a proxy measure of health and nutrition literacy (25), but also as a functional measure of consumer NFt understanding. We adapted the Newest Vital Sign tool to the NFt design and layout mandated in each country (Supplemental Table 2). A score between 0 and 6 was calculated based on the number of correct answers, with higher scores corresponding with a higher understanding of NFts.
Correlates of label understanding were selected based on evidence regarding associations between nutrition knowledge, dietary behaviors, and sociodemographic characteristics.
Functional nutrition knowledge
Prior nutrition knowledge can influence consumers’ understanding of nutrition labels (17, 21); hence, this survey assessed consumer nutrition knowledge using the FoodProK score, a functional test of nutrition knowledge based on level of food processing (26). Respondents viewed and rated images of 3 food products within each of 4 categories: fruits (apple, apple juice, apple sauce), meat (chicken breast, deli chicken slices, chicken nuggets), dairy (1% milk, cheese block, processed cheese slices), and grains (oats, cereal, cereal bar). Products in each category were selected based on availability in multiple international contexts, and to represent varied levels of processing according to the NOVA food classification system (27). The 12 product images and corresponding NFts and ingredients lists were displayed 1 at a time, in random order. For each product, respondents were asked, “Overall, how healthy is this food product?” and answered using a scale of 0 to 10, with 0 representing “not healthy at all” to 10 indicating “extremely healthy.” Respondents’ FoodProK scores (ranging from 0 to 8) were calculated based on whether they correctly ordered foods according to the NOVA classification for level of processing, with less-processed foods representing higher healthiness (26, 27).
Consumer dietary behaviors
Dietary modification efforts, another possible predictor of label understanding, were measured by asking, “Have you made an effort to consume more or less of the following in the past year?” Respondents answered, “consume less,” “consume more,” or “no effort made,” to a list of nutrients and food categories. This study focused on efforts in 5 categories that have received increasing attention in policies such as dietary guidelines within the 5 countries: “trans fats,” “sugar/added sugars,” “salt/sodium,” “calories,” and “processed foods” (18, 28–32). A value of −1 was assigned for any responses to “consume less,” +1 for responses to “consume more,” and 0 for “no effort made” in the 5 categories. Dietary modification efforts were recoded into a scale variable, with 5 points added to all responses to create a 0 to 10 scale where 0 represents “consume less” responses to all categories, 10 represents “consume more” responses to all categories, and the range between reflects all other response combinations.
Consumers with specific dietary practices, as well as those with a primary food shopping role in their households, are hypothesized to have greater interest in and exposure to labels. Respondents indicated whether they engaged in any of the following dietary practices: “vegetarian,” “vegan,” “pescatarian,” “following a religious practice for eating (please specify),” or “none of the above.” This variable was recoded as binary (no specific dietary practices = 0; ≥1 dietary practices = 1) (33). Food shopping role was captured using an adapted version of the USDA Eating and Health survey measure: “Do you do most of the food shopping in your household?” with response options “yes,” “no,” or “share equally with other(s)” (34).
Sociodemographic variables and BMI
Nutrition label understanding has been shown to vary by sociodemographic and socioeconomic characteristics, which can contribute to greater disparities in nutrition outcomes (11, 35). Age, sex at birth (female or male), country (Australia, Canada, Mexico, United Kingdom, United States), and derived variables for education and minority race/ethnicity were included in analyses. Less than 1% (n = 113) of IFPS respondents reported a gender different than their biological sex, which was insufficient for providing robust estimates in modeling. Hence, sex at birth was used as a binary covariate. Education level was categorized in accordance with country-specific criteria, with respondents classified as having “low” (high school completion or lower), “medium” (some post–secondary school qualifications, including some university), or “high” (university degree or higher) levels of education (36–39). Ethnicity was assessed using country-specific race/ethnicity categories and analyzed as a derived variable (majority/minority/unstated) to accommodate different measures across countries. To enable cross-country comparisons, respondents were categorized as “majority” in Mexico if they identified themselves as “non-Indigenous,” and “majority” in Australia, Canada, the United Kingdom, and the United States if they identified themselves as “white,” predominantly English-speaking, or non-Indigenous based on country-specific ethnic identity questions (38–41). Income adequacy was assessed by asking, “Thinking about your total monthly income, how difficult or easy is it for you to make ends meet?” with Likert scale response options “very difficult,” “difficult,” “neither easy nor difficult,” “easy,” and “very easy” (42).
Categorization of BMI (kg/m2) followed WHO criteria (43), with self-reported height and weight used to classify respondents based on BMI <18.5, 18.5–24.9, 25.0–29.9, and ≥30. Response options “don't know” and “refuse to answer” were provided for all survey questions and recoded as missing. Given the large number of cases with missing height and weight data—including those who selected “don't know” or “refuse to answer”—a separate category for “missing” was created and retained as a response category for analyses.
Statistical analysis
Descriptive statistics were used to summarize the sample profile and labeling outcomes by country. Analyses were conducted only on respondents who had complete data from all variables, with the exception of BMI, as described above. Hypotheses and the analytic plan were specified before data collection based on current evidence.
Using pooled data from all the countries where the relevant question was asked, 3 multiple linear regression models were fitted to examine self-reported NFt understanding (all countries), FOP label understanding (Australia, United Kingdom, Mexico), and functional NFt understanding (all countries). All models were adjusted for sociodemographic characteristics (age, sex, country, income adequacy, education level, ethnicity), consumer dietary behaviors (food shopping role, dietary efforts and practices), BMI, and functional nutrition knowledge (FoodProK score). Multiple comparisons were conducted to assess all pairwise contrasts for categorical variables. The Benjamini–Hochberg procedure was applied to decrease the false detection rate following multiple exploratory tests (44). All statistically significant pairwise contrasts are reported after applying the Benjamini–Hochberg procedure, assuming a false discovery rate of 10%. Spearman rank correlation tested bivariate associations between self-reported NFt understanding, self-reported FOP understanding, and functional NFt understanding (Newest Vital Sign score).
Statistical analyses were conducted using SAS Studio (SAS Institute). Parameter estimates are reported with 95% CIs. Data were weighted with poststratification sample weights constructed using a raking algorithm with population estimates from respective country-based censuses based on age group, sex at birth, region, ethnicity (except in Canada), and education (except in Mexico) (22). All reported estimates are weighted.
Results
Sample characteristics are presented in Table 1.
TABLE 1.
Sample characteristics (n = 21,586), International Food Policy Study, 20181
| Characteristic | Australia (n = 3901), % (n) | Canada (n = 4107), % (n) | Mexico (n = 4012), % (n) | United Kingdom (n = 5121), % (n) | United States (n = 4445), % (n) |
|---|---|---|---|---|---|
| Age group | |||||
| 18–29 y | 21.3 (831) | 18.9 (777) | 29.8 (1194) | 19.0 (974) | 20.6 (914) |
| 30–44 y | 26.2 (1022) | 24.7 (1014) | 32.3 (1297) | 24.8 (1270) | 25.1 (1115) |
| 45–59 y | 24.7 (963) | 25.8 (1059) | 28.7 (1151) | 25.9 (1327) | 25.7 (1141) |
| ≥60 y | 27.8 (1085) | 30.6 (1257) | 9.2 (370) | 30.3 (1550) | 28.6 (1275) |
| Sex | |||||
| Male | 48.7 (1898) | 49.4 (2028) | 47.6 (1911) | 47.8 (2448) | 48.2 (2141) |
| Female | 51.3 (2003) | 50.6 (2079) | 52.4 (2101) | 52.2 (2673) | 51.8 (2304) |
| Ethnicity2 | |||||
| Majority | 76.1 (2969) | 79.9 (3280) | 78.7 (3156) | 89.1 (4563) | 76.1 (3382) |
| Minority | 23.9 (932) | 20.1 (827) | 21.3 (856) | 10.9 (558) | 23.9 (1063) |
| Education level3 | |||||
| Low | 41.6 (1622) | 41.0 (1683) | 19.5 (782) | 47.6 (2438) | 58.2 (2585) |
| Medium | 32.6 (1272) | 34.1 (1400) | 13.2 (531) | 23.5 (1203) | 10.0 (443) |
| High | 25.8 (1007) | 24.9 (1024) | 67.3 (2699) | 28.9 (1480) | 31.8 (1417) |
| Income adequacy | |||||
| Very difficult to make ends meet | 8.5 (331) | 8.4 (345) | 12.0 (482) | 6.8 (349) | 9.4 (416) |
| Difficult to make ends meet | 19.2 (750) | 19.6 (804) | 31.7 (1273) | 18.5 (949) | 20.3 (902) |
| Neither easy nor difficult to make ends meet | 37.8 (1473) | 36.8 (1511) | 38.9 (1559) | 36.0 (1844) | 33.7 (1497) |
| Easy to make ends meet | 23.6 (921) | 22.5 (927) | 13.9 (557) | 24.7 (1265) | 21.8 (970) |
| Very easy to make ends meet | 10.9 (426) | 12.7 (520) | 3.5 (141) | 14.0 (714) | 14.8 (660) |
| BMI, kg/m2 | |||||
| ≤18.5 | 3.1 (122) | 3.2 (133) | 2.1 (85) | 2.9 (150) | 3.4 (153) |
| 18.5–24.9 | 36.3 (1416) | 33.5 (1376) | 39.6 (1588) | 34.8 (1780) | 31.2 (1385) |
| 25.0–29.9 | 26.6 (1039) | 28.8 (1183) | 30.1 (1208) | 27.0 (1384) | 27.6 (1226) |
| ≥30.0 | 20.9 (815) | 24.7 (1015) | 15.5 (620) | 17.0 (870) | 27.4 (1218) |
| Missing | 13.1 (509) | 9.8 (400) | 12.7 (511) | 18.3 (937) | 10.4 (463) |
| Food shopping role | |||||
| Primary shopper | 71.6 (2792) | 72.0 (2959) | 74.9 (3005) | 74.6 (3820) | 73.2 (3255) |
| Not primary shopper | 6.9 (268) | 5.9 (242) | 5.0 (201) | 4.5 (230) | 6.6 (293) |
| Shared equally with others | 21.5 (841) | 22.1 (906) | 20.1 (806) | 20.9 (1071) | 20.2 (897) |
| Dietary practices | |||||
| No specific dietary practices | 87.1 (3396) | 90.4 (3714) | 88.2 (3539) | 86.8 (4446) | 88.6 (3936) |
| ≥1 dietary practices (i.e., vegetarian, vegan, pescatarian, religious practices) | 12.9 (505) | 9.6 (393) | 11.8 (473) | 13.2 (675) | 11.4 (509) |
| Dietary efforts score4, 5 | 2.7 (2.2) | 2.6 (2.1) | 2.5 (2.3) | 3.0 (2.1) | 2.9 (2.3) |
| FoodProK score5, 6 | 5.0 (1.7) | 5.1 (1.5) | 4.8 (1.5) | 4.9 (1.8) | 4.6 (1.8) |
Data presented have been weighted. FoodProK, Food Processing Knowledge.
“Majority” ethnicity refers to respondents who identified as “white,” “predominantly English-speaking,” or “non-Indigenous” based on country-specific ethnic identity questions.
“Low” education refers to high school completion or lower, “medium” education refers to some post–secondary school qualifications including some university, and “high” refers to respondents who received a university degree or higher.
The dietary efforts score reflects consumers’ efforts to consume more or less of the following nutrient categories: trans fats, sugar/added sugars, salt/sodium, calories, and processed foods. On a scale of 0–10, 0 represents “consume less” responses to all categories, 10 represents “consume more” responses to all categories, and the range in between reflects all other response combinations.
Mean and SD reported for dietary efforts and FoodProK score.
The FoodProK score reflects consumers’ functional nutrition knowledge based on level of food processing. On a scale of 0–8, scores reflect whether respondents correctly ordered foods according to the NOVA classification for level of processing, with higher scores reflecting higher functional nutrition knowledge.
Self-reported and functional label understanding across countries
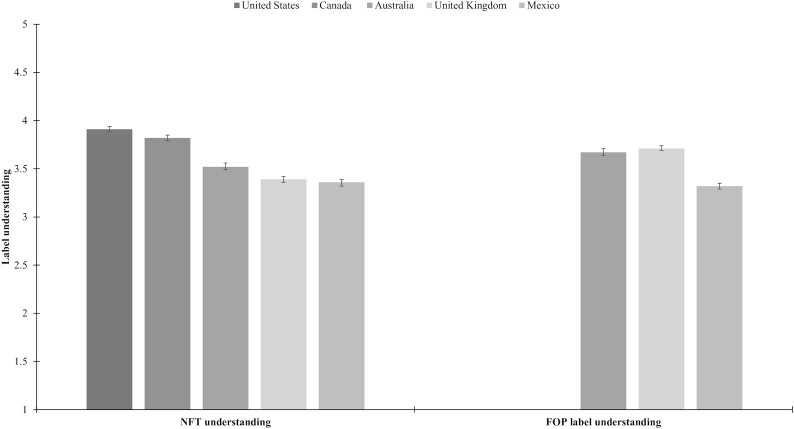
Respondents from the United States self-reported significantly higher NFt understanding than respondents from Canada, Australia, the United Kingdom, and Mexico (Figure 2). All other cross-country differences in means were statistically significant (P < 0.001), with the exception of the United Kingdom compared with Mexico. For FOP labels, the mean level of understanding for traffic lights and HSR labels was higher than GDA labels (P < 0.0001), respectively. When comparing NFt with FOP labels, self-reported FOP label understanding was significantly higher than NFt understanding in Australia and the United Kingdom (P < 0.0001), whereas FOP label understanding was significantly higher than NFt label understanding in Mexico (P < 0.0001).
FIGURE 2.
Self-reported understanding of Nutrition Facts tables (NFts) and front-of-package (FOP) labels, by country. Participants rated their level of label understanding, where 1 = very hard to understand, 2 = hard to understand, 3 = neither hard or easy to understand, 4 = easy to understand, and 5 = very easy to understand. Mean levels of self-reported understanding are shown with 95% CIs. For NFt understanding, all cross-country differences in means are statistically significant (P < 0.001) with the exception of the United Kingdom compared with Mexico. For FOP label understanding, all cross-country differences in means are statistically significant (P < 0.001).
Table 2 shows functional NFt understanding in each of the 5 countries. Respondents in all countries had the highest proportions of correct answers for questions pertaining to nut allergies, and the lowest proportion of correct answers for the question regarding concentrations of saturated fats. A greater number of respondents received full scores for questions requiring minimal or no mathematical calculations [i.e., question (Q) 5 and Q6].
TABLE 2.
Functional understanding of Nutrition Facts tables, by country (n = 21, 586)1
| Newest Vital Sign questions2 | Total score3 (mean ± SD) | ||||||
|---|---|---|---|---|---|---|---|
| Country | Q1: calorie content, % (n) | Q2: carbohydrates, % (n) | Q3: saturated fats, % (n) | Q4: percentage daily value, % (n) | Q5: allergy safety, % (n) | Q6: allergy rationale, % (n) | |
| Mexico (n = 4012) | 41.7 (1675) | 41.5 (1667) | 37.7 (1512) | 44.9 (1803) | 62.0 (2489) | 56.2 (2253) | 2.84 ± 1.99 |
| United Kingdom (n = 5121) | 55.8 (2856) | 53.2 (2726) | 44.0 (2253) | 48.3 (2473) | 61.7 (3161) | 55.8 (2860) | 3.19 ± 2.22 |
| Australia (N = 3901) | 52.6 (2053) | 46.3 (1805) | 41.2 (1618) | 49.6 (1935) | 66.3 (2585) | 60.8 (2373) | 3.23 ± 2.12 |
| United States (n = 4445) | 64.9 (2883) | 55.0 (2444) | 44.9 (1995) | 53.0 (2357) | 68.8 (3057) | 63.1 (2807) | 3.50 ± 2.12 |
| Canada (n = 4107) | 62.7 (2576) | 61.5 (2525) | 45.0 (1848) | 61.0 (2505) | 72.0 (2959) | 67.2 (2762) | 3.69 ± 1.97 |
Data presented have been weighted.
% refers to total percentage of respondents who answered the Newest Vital Sign question correctly in each country, and “n” refers to the total number in the sample.
Scores range from 0 to 6, with higher scores representing greater understanding of Nutrition Facts tables.
In general, self-reported NFt understanding was greater with higher Newest Vital Sign scores (i.e., functional NFt understanding), with a few exceptions in Mexico and the United States (Table 3). Self-reported FOP label understanding similarly was greater with higher Newest Vital Sign scores.
TABLE 3.
Mean self-reported label understanding by Newest Vital Sign score across countries1
| NVS score2 | Self-reported NFt understanding (mean ± SD)3, 4 | Self-reported FOP label understanding (mean ± SD)3, 4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All countries | Canada | United States | Australia | United Kingdom | Mexico | All countries | Australia | United Kingdom | Mexico | |
| 0 | 3.22 ± 1.15 | 3.33 ± 1.06 | 3.74 ± 1.07 | 3.13 ± 1.11 | 2.98 ± 1.14 | 3.13 ± 1.62 | 3.25 ± 1.11 | 3.46 ± 1.04 | 3.22 ± 1.19 | 3.11 ± 1.15 |
| 1 | 3.38 ± 1.11 | 3.55 ± 1.02 | 3.60 ± 1.08 | 3.29 ± 1.15 | 3.18 ± 1.13 | 3.33 ± 1.10 | 3.38 ± 1.07 | 3.49 ± 1.05 | 3.35 ± 1.04 | 3.32 ± 1.12 |
| 2 | 3.44 ± 1.12 | 3.64 ± 1.05 | 3.81 ± 1.02 | 3.34 ± 1.21 | 3.20 ± 1.17 | 3.36 ± 1.03 | 3.42 ± 1.07 | 3.57 ± 1.05 | 3.50 ± 1.05 | 3.26 ± 1.09 |
| 3 | 3.56 ± 1.08 | 3.77 ± 0.96 | 3.86 ± 1.01 | 3.45 ± 1.12 | 3.40 ± 1.14 | 3.34 ± 1.08 | 3.51 ± 1.05 | 3.60 ± 0.94 | 3.72 ± 1.04 | 3.25 ± 1.08 |
| 4 | 3.61 ± 1.04 | 3.82 ± 0.93 | 3.92 ± 0.92 | 3.51 ± 1.12 | 3.41 ± 1.07 | 3.35 ± 1.03 | 3.56 ± 1.02 | 3.64 ± 0.99 | 3.70 ± 0.97 | 3.29 ± 1.08 |
| 5 | 3.73 ± 1.00 | 3.91 ± 0.89 | 3.95 ± 0.86 | 3.73 ± 1.01 | 3.52 ± 1.09 | 3.46 ± 1.06 | 3.73 ± 0.98 | 3.76 ± 0.95 | 3.88 ± 0.90 | 3.44 ± 1.06 |
| 6 | 3.83 ± 0.96 | 4.03 ± 0.83 | 4.07 ± 0.76 | 3.79 ± 1.00 | 3.60 ± 1.09 | 3.49 ± 0.99 | 3.77 ± 0.96 | 3.63 ± 1.03 | 3.97 ± 0.85 | 3.48 ± 1.01 |
Data presented have been weighted. FOP, front-of-package; NFt, Nutrition Facts table; NVS, Newest Vital Sign.
Scores range from 0 to 6, with higher scores representing greater understanding of Nutrition Facts tables.
The 5-country sample size for self-reported NFt understanding was n = 21,586; for self-reported FOP label understanding in 3 countries, n = 12,360.
Self-reported NFt label understanding means reflect 5-country mean (n = 21,586); FOP label means reflect 3-country mean for Australia, Mexico, and the United Kingdom only.
Functional NFt understanding was weakly correlated with self-reported understanding of NFt labels [Spearman's rank correlation coefficient ( rs) = 0.18, P < 0.0001] and self-reported understanding of FOP labels (rs = 0.16, P < 0.0001). Self-reported NFt and FOP understanding were moderately correlated (rs = 0.51, P < 0.0001).
Cross-country differences and correlates of NFt and FOP label understanding
As shown in Table 4, respondents from the United States, Canada, and Australia self-reported significantly higher NFt understanding than respondents from Mexico (P < 0.0001). Additional pairwise contrasts (data not shown) demonstrated that respondents from Australia reported significantly lower NFt understanding than respondents from Canada (β: −0.27; 95% CI: −0.33, −0.22; P < 0.0001) and the United States (β: −0.41; 95% CI: −0.45, −0.35; P < 0.0001), and higher NFt understanding than UK respondents (β: 0.15; 95% CI: 0.10, 0.20; P < 0.0001). Respondents from Canada and the United Kingdom reported lower NFt understanding than those from the United States (β: −0.13; 95% CI: −0.18, −0.01; P < 0.0001; and β: −0.56; 95% CI: −0.61, −0.51; P < .0001, respectively), and respondents in Canada reported higher NFt understanding than UK respondents (β: 0.43; 95% CI: 0.38, 0.48; P < 0.0001). Respondents from Australia and the United Kingdom reported significantly higher FOP label understanding than respondents from Mexico (β: 0.41; 95% CI: 0.35, 0.47; P < 0.0001; and β: 0.38; 95% CI: 0.32, 0.44; P < 0.0001).
TABLE 4.
Sociodemographic and behavioral correlates of self-reported NFt and FOP label understanding1
| NFt understanding, mean ± SD | NFt understanding2 | FOP label understanding, mean ± SD | FOP label understanding2 | |||||
|---|---|---|---|---|---|---|---|---|
| β | 95% CI | P value3 | β | 95% CI | P value | |||
| Country | ||||||||
| Mexico | 3.36 ± 1.07 | Ref | 3.31 ± 1.09 | Ref | ||||
| United Kingdom | 3.36 ± 1.12 | 0.01 | −0.04, 0.07 | 0.6609 | 3.65 ± 1.01 | 0.38 | 0.32, 0.44 | <0.0001* |
| Australia | 3.53 ± 1.11 | 0.16 | 0.10, 0.21 | <0.0001* | 3.68 ± 0.97 | 0.41 | 0.35, 0.47 | <0.0001* |
| Canada | 3.81 ± 0.95 | 0.44 | 0.38, 0.49 | <0.0001* | — | — | — | — |
| United States | 3.90 ± 0.95 | 0.57 | 0.51, 0.62 | <0.0001* | — | — | — | — |
| Age | — | −0.005 | −0.006, −0.004 | <0.0001* | — | −0.006 | −0.008, −0.005 | <0.0001* |
| Sex at birth | ||||||||
| Male | 3.56 ± 1.08 | Ref | 3.55 ± 1.03 | Ref | ||||
| Female | 3.60 ± 1.06 | 0.00 | −0.04, 0.03 | 0.8489 | 3.56 ± 1.05 | −0.04 | −0.08, 0.00 | 0.0589 |
| Ethnicity4 | ||||||||
| Minority | 3.67 ± 1.16 | Ref | 3.55 ± 1.24 | Ref | ||||
| Majority | 3.57 ± 1.05 | −0.03 | −0.08, 0.01 | 0.1553 | 3.55 ± 1.01 | 0.02 | −0.05, 0.08 | 0.5305 |
| Education level5 | ||||||||
| Low | 3.56 ± 1.37 | Ref | 3.52 ± 1.27 | Ref | ||||
| Medium | 3.58 ± 0.97 | 0.02 | −0.03, 0.06 | 0.4544 | 3.58 ± 0.99 | 0.02 | −0.04, 0.08 | 0.5115 |
| High | 3.61 ± 0.91 | 0.04 | 0.00, 0.08 | 0.0588 | 3.57 ± 0.93 | 0.11 | 0.06, 0.16 | <0.0001* |
| Income adequacy | — | 0.12 | 0.11, 0.14 | <0.0001* | — | 0.10 | 0.08, 0.12 | <0.0001* |
| BMI, kg/m2 | ||||||||
| 18.5–24.99 | 3.65 ± 1.04 | Ref | 3.62 ± 0.99 | Ref | ||||
| <18.5 | 3.70 ± 1.15 | 0.06 | −0.05, 0.17 | 0.2790 | 3.56 ± 1.17 | −0.06 | −0.21, 0.09 | 0.4146 |
| 25.0–29.99 | 3.58 ± 1.05 | −0.06 | −0.10, −0.01 | 0.0076* | 3.53 ± 1.03 | −0.05 | −0.11, 0.00 | 0.0490 |
| ≥30.0 | 3.57 ± 1.09 | −0.08 | −0.13, −0.03 | 0.0010* | 3.49 ± 1.07 | −0.09 | −0.15, −0.03 | 0.0066* |
| Missing | 3.42 ± 1.14 | −0.11 | −0.16, −0.05 | 0.0002* | 3.50 ± 1.10 | −0.05 | −0.12, 0.02 | 0.1619 |
| Food shopping role | ||||||||
| Not primary shopper | 3.46 ± 1.14 | Ref | 3.43 ± 1.13 | Ref | ||||
| Share equally with others | 3.54 ± 1.05 | 0.07 | 0.00, 0.16 | 0.0766 | 3.53 ± 1.13 | 0.08 | −0.03, 0.19 | 0.1574 |
| Primary shopper | 3.61 ± 1.07 | 0.16 | 0.08, 0.23 | <0.0001* | 3.57 ± 1.04 | 0.14 | 0.03, 0.25 | 0.0078* |
| Dietary practices | ||||||||
| No specific dietary practices | 3.57 ± 1.07 | Ref | 3.54 ± 1.04 | Ref | ||||
| ≥1 dietary practices (i.e., vegetarian, vegan, pescatarian, religious practices) | 3.63 ± 1.10 | 0.09 | 0.04, 0.15 | 0.0010* | 3.62 ± 1.04 | 0.08 | 0.01, 0.14 | 0.0161* |
| Dietary efforts score6 | — | −0.05 | −0.06, −0.04 | <0.0001* | — | −0.04 | −0.05, −0.03 | <0.0001* |
| FoodProK score6, 7 | — | 0.06 | 0.05, 0.07 | <0.0001* | — | 0.08 | 0.06, 0.09 | <0.0001* |
Data presented have been weighted. FoodProK, Food Processing Knowledge; FOP, front-of-package; NFt , Nutrition Facts table; Ref, reference category.
Sample size is 21,586 for NFt understanding model, and 12,360 for the FOP label understanding model.
Variables marked with an asterisk are significant (P < 0.05) after post hoc adjustment using the Benjamini–Hochberg procedure.
“Majority” ethnicity refers to respondents who identified as “white,” “predominantly English-speaking,” or “non-Indigenous” based on country-specific ethnic identity questions.
“Low” education refers to high school completion or lower, “medium” education refers to some post–secondary school qualifications including some university, and “high” refers to respondents who received a university degree or higher.
The dietary efforts score reflects consumers’ efforts to consume more or less of the following nutrient categories: trans fats, sugar/added sugars, salt/sodium, calories, and processed foods. On a scale of 0–10, 0 represents “consume less” responses to all categories, 10 represents “consume more” responses to all categories, and the range in between reflects all other response combinations.
The FoodProK score reflects consumers’ functional nutrition knowledge based on level of food processing. On a scale of 0–8, scores reflect whether respondents correctly ordered foods according to the NOVA classification for level of processing, with higher scores reflecting higher functional nutrition knowledge.
Respondents from Australia, Canada, the United Kingdom, and the United States scored significantly higher on the Newest Vital Sign measure than respondents in Mexico, indicative of higher functional NFt understanding (Table 5). Functional NFt understanding in respondents in Australia was significantly lower compared with Canadian and US respondents, adjusting for other covariates. Respondents from Canada received significantly higher scores for functional NFt understanding than those in the United Kingdom, and UK respondents received significantly lower scores than US respondents. The differences in functional NFt understanding scores between respondents in Australia and the United Kingdom, and Canada and the United States were not statistically significant.
TABLE 5.
Sociodemographic and behavioral correlates of functional NFt understanding (n = 21,586)1
| β | 95% CI | P value2 | |
|---|---|---|---|
| Country | |||
| Australia vs. Canada | −0.31 | −0.40, −0.21 | <0.0001* |
| Australia vs. Mexico | 0.46 | 0.36, 0.57 | <0.0001* |
| Australia vs. United Kingdom | −0.06 | −0.15, 0.03 | 0.1957 |
| Australia vs. United States | −0.38 | −0.48, −0.29 | <0.0001* |
| Canada vs. Mexico | 0.77 | 0.67, 0.87 | <0.0001* |
| Canada vs. United Kingdom | 0.25 | 0.15, 0.34 | <0.0001* |
| Canada vs. United States | −0.08 | −0.17, 0.02 | 0.1134 |
| United Kingdom vs. Mexico | 0.52 | 0.43, 0.62 | <0.0001* |
| United Kingdom vs. United States | −0.32 | −0.42, −0.23 | <0.0001* |
| United States vs. Mexico | 0.84 | 0.75, 0.95 | <0.0001* |
| Age | −0.004 | −0.006, −0.002 | <0.0001* |
| Sex at birth | |||
| Female vs. male | 0.23 | 0.17, 0.29 | <0.0001* |
| Ethnicity3 | |||
| Majority vs. minority | 0.63 | 0.55, 0.72 | <0.0001* |
| Education level4 | |||
| Medium vs. low | 0.36 | 0.28, 0.43 | <0.0001* |
| High vs. low | 0.52 | 0.44, 0.58 | <0.0001* |
| High vs. medium | 0.16 | 0.80, 0.23 | <0.0001* |
| Income adequacy | 0.00 | −0.02, 0.03 | 0.8572 |
| BMI | |||
| Missing vs. <18.5 | −0.72 | −0.92, −0.53 | <0.0001* |
| Missing vs. 18.5–24.9 | −0.69 | −0.79, −0.59 | <0.0001* |
| Missing vs. 25–29.9 | −0.70 | −0.80, −0.60 | <0.0001* |
| Missing vs. ≥30 | −0.80 | −0.90, −0.69 | <0.0001* |
| ≥30 vs. <18.5 | 0.07 | −0.11, 0.26 | 0.4494 |
| ≥30 vs. 18.5–24.9 | 0.10 | 0.02, 0.19 | 0.0148* |
| ≥30 vs. 25–29.9 | 0.09 | 0.01, 0.18 | 0.0297* |
| 25–29.9 vs. 18.5–24.9 | 0.01 | −0.07, 0.08 | 0.8023 |
| 25–29.9 vs. <18.5 | −0.02 | −0.21, 0.16 | 0.8186 |
| <18.5 vs. 18.5–24.9 | 0.03 | −0.15, 0.21 | 0.7349 |
| Food shopping role | |||
| Primary shopper vs. not primary shopper | −0.34 | −0.48, −0.21 | <0.0001* |
| Primary shopper vs. share equally with others | −0.24 | −0.31, −0.17 | <0.0001* |
| Not primary shopper vs. share equally with others | −0.10 | −0.25, 0.04 | 0.1725 |
| Dietary practices | |||
| ≥1 dietary practices (i.e., vegetarian, vegan, pescatarian, religious practices) vs. no specific dietary practices | −0.45 | −0.54, −0.36 | <0.0001* |
| Dietary efforts score5 | −0.10 | −0.11, −0.09 | <0.0001* |
| FoodProK score5, 6 | 0.38 | 0.36, 0.40 | <0.0001* |
| Self-reported NFt understanding | 0.19 | 0.16, 0.22 | <0.0001* |
Data presented have been weighted. FoodProK, Food Processing Knowledge; NFt, Nutrition Facts table.
Variables marked with an asterisk are significant (P < 0.05) after post hoc adjustment using Benjamini–Hochberg procedure.
“Majority” ethnicity refers to respondents who identified as “white,” “predominantly English-speaking,” or “non-Indigenous” based on country-specific ethnic identity questions.
“Low” education refers to high school completion or lower, “medium” education refers to some post–secondary school qualifications including some university, and “high” refers to respondents who received a university degree or higher.
The dietary efforts score reflects consumers’ efforts to consume more or less of the following nutrient categories: trans fats, sugar/added sugars, salt/sodium, calories, and processed foods. On a scale of 0–10, 0 represents “consume less” responses to all categories, 10 represents “consume more” responses to all categories, and the range in between reflects all other response combinations.
The FoodProK score reflects consumers’ functional nutrition knowledge based on level of food processing. On a scale of 0–8, scores reflect whether respondents correctly ordered foods according to the NOVA classification for level of processing, with higher scores reflecting higher functional nutrition knowledge.
Self-reported NFt and FOP label understanding was higher in respondents with higher FoodProK scores, primary food shoppers, those who engaged in specific dietary practices, as well as respondents reporting efforts to consume less sodium, sugars, trans fats, calories, or processed food. Similarly, respondents who scored higher on the FoodProK, those who reported efforts to consume less sodium, sugars, trans fats, calories, or processed food, and those with higher self-reported NFt understanding received significantly higher scores for functional NFt understanding. In contrast to self-reported label understanding, respondents who were primary food shoppers had lower functional NFt understanding than those who were not primary food shoppers or who shared the responsibility equally with others in their households. Also, respondents engaging in vegetarian or other dietary practices had lower functional NFt understanding scores than those with no specific practice.
With respect to sociodemographic characteristics, self-reported NFt and FOP label understanding was lower with higher age. Education was not significantly associated with self-reported NFt understanding; however, self-reported FOP label understanding was higher in respondents with “high” education compared with “low” education levels. Both self-reported NFt and FOP label understanding were higher with higher income adequacy. Sex and ethnicity were not significantly associated with self-reported label understanding. For functional NFt understanding, females, younger respondents, and those from “majority” ethnic groups in their respective countries scored higher than their male, older, or “minority” counterparts. Respondents with “high” education scored higher for functional NFt understanding compared with those with “medium” and “low” education levels.
Respondents with BMIs ≥30, between 25 and 29.9, <18.5, or “missing” self-reported lower NFt understanding compared with those with a BMI between 18.5 and 24.9. Moreover, respondents with missing BMI or BMI ≥30 self-reported lower NFt understanding compared with those with BMIs <18.5. Respondents with BMIs ≥30 also self-reported lower FOP label understanding compared with those with BMIs between 18.5 and 24.9. Similarly, respondents with missing BMI data scored significantly lower for functional NFt understanding compared with all other BMI categories (P < 0.0001 for all); however, those with BMIs ≥30 scored higher compared with respondents with BMIs between 18.5 and 24.9.
Discussion
Several studies have assessed consumer understanding of front- and back-of-package nutrition labeling systems across multiple countries (15–18); however, to our knowledge, this is the only population-based, multicountry analysis to report on levels of understanding for different label types and various consumer characteristics. The results therefore provide several unique insights.
Respondents in the United States self-reported the highest level of NFt understanding, and also scored highest on the functional test of NFt understanding, followed by Canada, Australia, the United Kingdom, and Mexico. Given that NFts are mandatory and similarly formatted in all countries, these differences can be explained by parallel healthy eating policies or food labeling campaigns in each country. For example, the United States and Canada released fact sheets, websites, and updates to school curricula alongside changes to food labeling policy to increase exposure to and education about food labels (31, 45). Other countries have developed similar campaigns; however, it is possible that more aggressive NFt label promotion in Canada and the United States resulted in relatively higher self-reported NFt understanding. It is also possible that the findings reflect differences in levels of numeracy across countries (6, 10).
The functional test of NFt understanding (Newest Vital Sign) showed that respondents performed poorly on questions requiring mathematical calculations or numeracy skills. These findings suggest that poor NFt understanding can reflect problems with numeracy and low health literacy. Although formal education is a factor in literacy and numeracy skills (46), inadequate nutrition education and promotional strategies can contribute to consumers being ill-equipped to interpret NFt information. For instance, although most countries have created guides for nutrition label use, consumers must actively seek out these resources because they are seldom promoted in publicly accessible domains (i.e., television advertising) or outside of educational settings.
Another potential explanation for cross-country differences lies in the prominence of processed, packaged foods: countries with a greater reliance on packaged food consumption could have greater exposure to—and therefore understanding of—NFts. Americans obtain ≤60% of their total energy intake from ultraprocessed foods—potentially the highest of all the countries in this study (27, 47).
As expected, mean self-reported NFt understanding was higher with higher functional NFt understanding in all countries, but with a weak correlation between these measures (r = 0.18). Moreover, many respondents in this study self-reported high NFt understanding while performing poorly on the functional measure. These findings are consistent with research indicating that consumers tend to overestimate their nutrition knowledge (6, 10, 19). In particular, studies have shown that consumers perform poorly on functional tasks, in part due to low awareness about what percentage daily value means, and in some cases, confusion about terminology (i.e., calories compared with kilojoules) (5, 6, 10).
Self-reported FOP label understanding was highest in Australia, followed by the United Kingdom and Mexico. Although self-reported understanding of FOP labels was higher than for NFts in Australia and the United Kingdom, the differences were more modest than some experimental studies might suggest. This could reflect that FOP labels are voluntary in both countries and appear on a minority of products (13, 14, 48). Mexico was the only country in which self-reported understanding of GDA labels was lower than that for the NFts, despite having a mandatory FOP labeling policy. This finding likely reflects the shortcomings of the design and type of information included on the Mexican FOP label. HSR and traffic light labels in Australia and the United Kingdom use symbols and provide interpretive information, whereas Mexico's industry-based GDA system provides reductive nutrient information similar to the NFt—simply replicating this information from the back to FOP. Previous research has demonstrated that consumers have poor understanding of the numeric information on GDA labels, which is consistent with the current findings (14, 49). This is likely compounded by lower levels of literacy and numeracy in Mexican respondents, which could limit their ability to use nutrition labels (50). This finding highlights the importance of simple, interpretive information, particularly in countries that have lower levels of numeracy. Accordingly, Mexico recently approved a new regulation to replace the GDA with FOP “high-in” labels similar to those used in Chile (51).
Food processing knowledge was associated with greater label understanding, particularly for functional NFt understanding. Packaged foods are predominantly highly processed; thus, it is expected that consumers with an increased interest in or knowledge of nutrition would have a better understanding of levels of food processing and how to interpret the information on NFts. Given the repercussions for noncommunicable disease risk (35), consumers with a greater understanding of the relative healthiness of food products based on processing would be better equipped to navigate the increasingly processed food landscape (27).
Respondents with a primary food shopping role had higher self-reported NFt and FOP label understanding, but lower functional NFt understanding than those who were not primary shoppers. This finding is surprising given that primary shoppers likely have greater exposure to labels. Those engaging in vegetarian or other dietary practices also reported higher NFt and FOP understanding, but scored lower on the functional test of NFt understanding. These findings point to discrepancies in self-report compared with functional measures. Although self-reported measures can still be informative in labeling policy research, they might not accurately reflect consumers’ ability to read and interpret NFts—particularly for labels involving numeracy skills.
With respect to sociodemographic characteristics, self-reported label understanding decreased with age, which might reflect lower awareness of labels or lower numeracy skills in older age groups (9, 52, 53). Consistent with existing literature (54, 55), this study found higher functional NFt understanding in females, “majority” ethnic groups, and respondents with higher income adequacy and education levels compared with their respective counterparts. These differences might be explained by disparities in label comprehension, because consumers with lower education, in particular, could have lower numeracy skills than those with higher educational attainment (8, 9). FOP labels were designed to be accessible to consumers with lower education or literacy levels; however, differences in understanding were observed in this study based on income adequacy and education. Research has shown that respondents with lower incomes demonstrate poorer understanding and responsiveness to FOP labels than those with higher incomes (14), although some evidence points to FOP “high-in” labels, in particular, having similar benefits across sociodemographic subgroups compared with other labeling systems (20, 56). More research is needed to explore whether disparities persist for FOP label understanding across various label types; however, this evidence is important to consider because lower label comprehension can be compounded by competing priorities in food selection. Consumers identifying as ethnic minorities in their respective countries and those with low incomes might prioritize cultural preferences or affordability in food purchasing and consumption, which could impact attention to NFts and resultant comprehension or use (55, 57, 58).
Respondents with BMIs between 18.5 and 24.9 self-reported higher NFt understanding than all other BMI categories. Similarly, self-reported FOP label understanding was higher for respondents in this BMI range compared with those with BMIs ≥30. In contrast, those with BMIs ≥30 scored higher for functional NFt understanding compared with respondents with BMIs of 18.5–24.9 and 25–29.9. The literature demonstrates mixed findings regarding label understanding and BMI (59). The use of self-reported measures of label comprehension suggests a possible role of weight-based goals in shaping NFt use; however, more research is needed to unpack patterns and differences in functional NFt understanding based on weight status, either objectively measured or perceived.
There were several limitations of the current analysis. The sample was recruited using nonprobability sampling, which does not enable nationally representative population estimates. For example, although data were weighted by age, sex, and region, the Mexico sample had higher levels of education than the Mexican population based on census estimates, whereas mean BMI was lower than national estimates in each of the 5 countries (22). The primary outcomes, NFt and FOP label understanding, as well as BMI, are subject to social desirability bias given the use of self-reported measures. There are also limitations of the functional NFt understanding measure, because the Newest Vital Sign has been tested across a variety of age and ethnic groups in different countries, but has not yet been validated as a self-administered measure (60). Moreover, despite being tested in Hispanic American populations (61), the Newest Vital Sign has not been tested in Mexico. The FoodProK score is also limited in its ability to assess overall nutrition knowledge, because only 1 component (knowledge of level of food processing based on nutritional recommendations) is assessed. Other important factors associated with diet quality (i.e., frequency of consumption of processed foods) are not captured by the FoodProK score. This study was also limited to understanding of labels and did not examine the implications of label understanding for food choices and dietary quality.
Overall, the between-country differences in self-reported and functional label understanding across countries reflect the extent to which mandatory compared with voluntary nutrition labeling policies are implemented and effective, as well as the uptake of parallel healthy eating policies or food labeling campaigns in each country. The differences found in label understanding by consumer characteristics such as sex, ethnicity, income adequacy, and education suggest that current nutrition labeling policies are contributing to existing disparities in nutrition-related health behaviors and outcomes, because nutrition labels are less accessible to certain groups. Given the relative ease of understanding of simple, interpretative FOP labels, future research should examine the extent to which FOP labeling policies affect consumers’ functional label understanding, as well as implications for dietary patterns across different sociodemographic groups.
Supplementary Material
ACKNOWLEDGEMENTS
We acknowledge Christine M White for her role in the development of measures for the International Food Policy Study and support of this article.
The authors’ responsibilities were as follows—JB, DH: collected the data, conducted analyses, and wrote the first draft with contributions from SIK, LV, MGH, and JFT; and all authors: contributed to development of the survey, reviewed and commented on subsequent drafts, and read and approved the final manuscript.
Notes
This supplement was supported by funding from a Project Grant from the Canadian Institutes of Health Research (PJT-162167). The views expressed herein are solely the responsibility of the authors and do not necessarily represent the official views of the Canadian Institutes for Health Research or other sources of funding. Funding for this project was provided by a Population Health Intervention Research operating grant from the Canadian Institutes of Health Research (CIHR) and the Public Health Agency of Canada. Additional funding for this project has been provided by a PHAC – CIHR Chair in Applied Public Health (DH).
Author disclosures: DH has served as a paid expert witness on behalf of public health authorities in the legal challenge to San Francisco’s health warning ordinance for sugar-sweetened beverages. All remaining authors declare no conflicts of interest.
Supplemental Tables 1 and 2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/jn/.
Abbreviations used: FoodProK, Food Processing Knowledge; FOP, front-of-package; GDA, Guideline Daily Amount; HSR, Health Star Rating; IFPS, International Food Policy Study; NFt, Nutrition Facts table; Q, question; rs, Spearman's rank correlation coefficient.
Contributor Information
Jasmin Bhawra, School of Public Health Sciences, University of Waterloo, Waterloo, Ontario, Canada.
Sharon I Kirkpatrick, School of Public Health Sciences, University of Waterloo, Waterloo, Ontario, Canada.
Marissa G Hall, Department of Health Behavior, Gillings School of Global Public Health, and Lineberger Comprehensive Cancer Center, University of North Carolina, Chapel Hill, NC, USA.
Lana Vanderlee, École de Nutrition, Centre Nutrition, santé et société (Centre NUTRISS), and Institut sur la nutrition et les aliments fonctionnels (INAF), Université Laval, Québec, Canada.
James F Thrasher, Department of Health Promotion, Education, and Behavior, Arnold School of Public Health, University of South Carolina, Columbia, SC, USA; Center for Population Health Research, National Institute of Public Health, Cuernavaca, Morelos, México.
David Hammond, School of Public Health Sciences, University of Waterloo, Waterloo, Ontario, Canada.
References
- 1. Feteira-Santos R, Fernandes J, Virgolino A, Alarcao V, Sena C, Viera CP, Gregorio MJ, Nogueira P, Costa A, Graca Pet al. Effectiveness of interpretative front-of-pack nutritional labelling schemes on the promotion of healthier food choices: a systematic review. Int J Evid Based Healthc. 2020;18(1):24–37. [DOI] [PubMed] [Google Scholar]
- 2. International Food Information Council (IFIC) . 2018 food and health survey. [Internet]. Food Insight; 2018; [cited July 2, 2020]. Available from: https://foodinsight.org/2018-food-and-health-survey [Google Scholar]
- 3. Ollberding NJ, Wolf RL, Contento I. Food label use and its relation to dietary intake among us adults. J Am Diet Assoc. 2010;110(8):1233–7. [DOI] [PubMed] [Google Scholar]
- 4. Campos S, Doxey J, Hammond D. Nutrition labels on pre-packaged foods: a systematic review. Public Health Nutr. 2011;14(8):1496–506. [DOI] [PubMed] [Google Scholar]
- 5. Cowburn G, Stockley L. Consumer understanding and use of nutrition labelling: a systematic review. Public Health Nutr. 2005;8(1):21–8. [DOI] [PubMed] [Google Scholar]
- 6. Sinclair S, Goodman S, Hammond D. Socio-demographic differences in the comprehension of nutritional labels on food products. J Nutr Educ Behav. 2013;45(6):767–72. [DOI] [PubMed] [Google Scholar]
- 7. Van der Horst K, Bucher T, Duncanson K, Murawski B, Labbe D. Consumer understanding, perception and interpretation of serving size information on food labels: a scoping review. Nutrients. 2019;11(9):2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nieto C, Castillo A, Alcalde-Rabanal J, Mena C, Carriedo A, Barquera S. Perception of the use and understanding of nutrition labels among different socioeconomic groups in Mexico: a qualitative study. Salud Publica Mex. 2020;62(3):288–97. [DOI] [PubMed] [Google Scholar]
- 9. Nogueira LM, Thai CL, Nelson W, Oh A. Nutrition label numeracy: disparities and association with health behaviors. Am J Health Behav. 2016;40(4):427–36. [DOI] [PubMed] [Google Scholar]
- 10. Vanderlee L, Goodman S, Yang WS, Hammond D. Consumer understanding of calorie amounts and serving size: implications for nutritional labelling. Can J Public Health. 2012;103(5):e327–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Micha R, Khatibzadeh S, Shi P, Andrews KG, Engell RE, Mozaffarian D. Global, regional and national consumption of major food groups in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys worldwide. BMJ Open. 2015;5(9):e008705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Health Organization (WHO) . Global nutrition policy review 2016-2017: country progress in creating enabling policy environments for promoting healthy diets and nutrition. Geneva: WHO; 2018. [Google Scholar]
- 13. Lichtenstein AH. IOM report on front-of-package nutrition rating systems and symbols. [Internet]. World Health Organization; 2013; [cited September 8, 2020]. Available from: http://www.who.int/nutrition/events/2013_FAO_WHO_workshop_frontofpack_nutritionlabelling_presentation_Lichtenstein.pdf [PubMed] [Google Scholar]
- 14. Hammond D, Goodman S, Acton R. Front-of-package (FOP) nutrition labelling: evidence review. 2018. University of Waterloo: Waterloo, ON. [Google Scholar]
- 15. Grunert KG, Wills JM. A review of European research on consumer response to nutrition information on food labels. J Public Health. 2007;15(5):385–99. [Google Scholar]
- 16. Hawley KL, Roberto CA, Bragg M, Liu PJ, Schwartz MB, Brownell KD. The science of front-of-package labels. Public Health Nutr. 2013;16(3):430–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Feunekes GI, Gortemaker IA, Willems AA, Lion R, van den Kommer M. Front-of-pack nutrition labelling: testing effectiveness of different nutrition labelling formats front-of-pack in four European countries. Appetite. 2008;50(1):57–70. [DOI] [PubMed] [Google Scholar]
- 18. Egnell M, Talati Z, Hercberg S, Pettigrew S, Julia C. Objective understanding of front-of-package nutrition labels: an international comparative experimental study across 12 countries. Nutrients. 2018;10(10):1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Acton RB, Vanderlee L, White C, Hammond D. The efficacy of calorie labelling formats on pre-packaged foods: an experimental study among adolescents and young adults in Canada. Can J Public Health. 2016;107(3):e296–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jauregui A, Vargas-Meza J, Nieto C, Contreras-Manzano A, Zacarias-Alejandro N, Tolentino-Mayo L. Impact of front-of-pack nutrition labels on consumer purchasing intentions: a randomized experiment in low- and middle-income Mexican adults. BMC Public Health. 2020;20(1):463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Miller LMS, Cassady DL. The effects of nutrition knowledge on food label use. a review of the literature. Appetite. 2015;92:207–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hammond D, White CM, Rynard VL, Vanderlee L. International Food Policy Study: technical report – 2018 survey (wave 2) [Internet]. University of Waterloo; May2019; [cited May 30, 2020]. Available from: www.foodpolicystudy.com/methods [Google Scholar]
- 23. Lin C-T J, Zhang Y, Carlton ED, Lo SC. 2014 FDA health and diet survey. [Internet]. Food and Drug Agency; 2014; [cited July 27, 2020]. Available from: https://www.fda.gov/media/96883/download [Google Scholar]
- 24. Canadian Council on Learning (CCL) . Health literacy in Canada: a healthy understanding. [Internet]. CCL; 2008; [cited July 1, 2020]. Available from: http://www.en.copian.ca/library/research/ccl/health/health.pdf [Google Scholar]
- 25. Yuen EYN, Thomson M, Gardiner H. Measuring nutrition and food literacy in adults: a systematic review and appraisal of existing measurement tools. Health Lit Res Pract. 2018;2(3):e134–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bhawra J, Kirkpatrick SI, Hall MG, Hammond D. Development and evaluation of the food processing knowledge score: a functional test of consumer nutrition knowledge based on level of food processing. J Acad Nutr Diet. 2021;121(8):1542–50. [DOI] [PubMed] [Google Scholar]
- 27. Monteiro CA, Cannon G, Levy RB, Moubarac JC, Louzada ML, Ruber F, Khandpur N, Cediel G, Neri D, Martinez-Steel Eet al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 2019;22(5):936–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Australia Government . Australian guide to healthy eating. Eat for health. [Internet]. Updated2015; [cited September 8, 2020]. Available from: https://www.eatforhealth.gov.au/guidelines/australian-dietary-guidelines-1-5 [Google Scholar]
- 29. FAO . Food-based dietary guidelines – Mexico. [Internet]. 2015; [cited April 20, 2020]. Available from: http://www.fao.org/nutrition/education/food-based-dietary-guidelines/regions/countries/mexico/en/ [Google Scholar]
- 30. FAO . Food-based dietary guidelines – United States of America. [Internet]. 2016; [cited April 20, 2020]. Available from: http://www.fao.org/nutrition/education/food-dietary-guidelines/regions/countries/united-states-of-america/en/ [Google Scholar]
- 31. Government of Canada . Health Canada's healthy eating strategy. Vision for a healthy Canada. [Internet]. 2020; [cited February 14, 2020]. Available from: https://www.canada.ca/en/services/health/campaigns/vision-healthy-canada/healthy-eating.html [Google Scholar]
- 32. National Health Service . Eating processed foods. Eat well. [Internet]. Updated January2020; [cited April 21, 2020]. Available from: https://www.nhs.uk/live-well/eat-well/what-are-processed-foods/ [Google Scholar]
- 33. Canadian Foundation for Dietetic Research (CFDR) . Tracking nutrition trends(2015) [Internet]. [cited February 13, 2022]. Available from: https://www.cfdr.ca/Downloads/Tracking-Nutrition-Trends/Tracking-Nutrition-Trends-IX-2015.aspx [Google Scholar]
- 34. United States Department of Agriculture . Eating and health module 2014-16 questionnaire. [Internet]. December2017; [cited July 1, 2020]. Available from: https://www.bls.gov/tus/ehmquestionnaire1416.pdf [Google Scholar]
- 35. World Health Organization (WHO) . Global action plan for the prevention and control of NCDs 2013-2020. [Internet]. 2013; [cited February 24, 2019]. Available from: https://www.who.int/nmh/events/ncd_action_plan/en/ [Google Scholar]
- 36. Centers for Disease Control and Prevention . NHANES demographics information - DMQ - SP. [Internet]. 2016; [cited July 1, 2020]. Available from: https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/questionnaires/DMQ_I.pdf [Google Scholar]
- 37. UK Data Service . Household questionnaire England: 2011 census. [Internet]. [cited July 1, 2020]. Available from: https://census.ukdataservice.ac.uk/media/50966/2011_england_household.pdf [Google Scholar]
- 38. Statistics Canada . Canadian community health survey – annual component (CCHS). Detailed information for 2014. [Internet]. 2014; [cited July 2, 2020]. Available from: https://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getInstanceList&Id=1263799 [Google Scholar]
- 39. International Tobacco Control . Policy evaluation project. 4-Country smoking and vaping w1. [Internet]. 2019; [cited July 2, 2020]. Available from: https://itcproject.s3.amazonaws.com/uploads/documents/ITC_4CV1_web_Eng_09May.pdf [Google Scholar]
- 40. Office for National Statistics . Ethnic group, national identity and religion. [Internet]. [cited July 2, 2020]. Available from: https://www.ons.gov.uk/methodology/classificationsandstandards/measuringequality/ethnicgroupnationalidentityandreligion [Google Scholar]
- 41. Statistics Canada . Canadian community health survey (CCHS)– 2017; [Internet]. [cited June 2, 2020]. Available from: https://www23.statcan.gc.ca/imdb/p3Instr.pl?Function=getInstrumentList&Item_Id=507367&UL=1V [Google Scholar]
- 42. Litwin H, Sapir EV. Perceived income adequacy among older adults in 12 countries: findings from the survey of health, ageing and retirement in Europe. Gerontologist. 2009;49(3):397–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. WHO . Body mass index – BMI. [Internet]. [cited July 2, 2020]. Available from: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi [Google Scholar]
- 44. Benjamini Y, Hochberg Y. Controlling the false discovery rate. A practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57:289–300. [Google Scholar]
- 45. US Food and Drug Administration . Social media toolkit on the new nutrition facts label. [Internet]. [cited June 25, 2020]. Available from: https://www.fda.gov/media/135197/download. [Google Scholar]
- 46. Greenhalgh T . Health literacy: towards system level solutions. BMJ. 2015;350:h1026. [DOI] [PubMed] [Google Scholar]
- 47. Baraldi LG, Martinez Steele E, Silva Canella D, Monteiro CA. Consumption of ultra-processed foods and associated sociodemographic factors in the USA between 2007 and 2012: evidence from a nationally representative cross-sectional study. BMJ Open. 2018;8(3):e020574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Storcksdieck genannt Bonsmann S, Celemin LF, Larranaga A, Egger S, Wills JM, Hodgkins C, Raats MM. Penetration of nutrition information on food labels across the EU-27 plus Turkey. Eur J Clin Nutr. 2010;64(12):1379–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Vargas-Meza J, Jauregui A, Contreras-Manzano A, Nieto C, Barquera S. Acceptability and understanding of front-of-pack nutritional labels: an experimental study in Mexican consumers. BMC Public Health. 2019;19(1):1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Organization for Economic Co-operation and Development (OECD) . Reading performance (PISA) (indicator). [Internet]. 2020; [cited September 21, 2020]. Available from: https://data.oecd.org/pisa/reading-performance-pisa.htm [Google Scholar]
- 51. White M, Barquera S. Mexico adopts food warning labels, why now?. Health Syst Reform. 2020;6(1):e1752063. [DOI] [PubMed] [Google Scholar]
- 52. Chen Y, Wang J, Kirk RM, Pethtel OL, Kiefner AE. Age differences in adaptive decision-making: the role of numeracy. Educ Gerontol. 2014;40(11):825–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Taha J, Sharit J, Czaja SJ. The impact of numeracy ability and technology skills on older adults’ performance of health management tasks using a patient portal. J Appl Gerontol. 2014;33(4):416–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mahshid MP. The correlation between nutrition knowledge and eating behavior in an American school: the role of ethnicity. Nutr Health. 2000;14:89–107. [DOI] [PubMed] [Google Scholar]
- 55. McKinnon L, Giskes K, Turrell G. The contribution of three components of nutrition knowledge to socio-economic differences in food purchasing choices. Public Health Nutr. 2014;17(8):1814–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Vargas-Meza J, Jauregui A, Pacheco-Miranda S, Contreras-Manzano A, Barquera S. Front-of-pack nutritional labels: understanding by low- and middle-income Mexican consumers. PLoS One. 2019;14(11):e0225268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. French SA, Tangney CC, Crane MM, Wang Y, Appelhans BM. Nutrition quality of food purchases varies by household income. The SHoPPER study. BMC Public Health. 2019;19(1):231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. McLeod ER, Campbell KJ, Hesketh KD. Nutrition knowledge: a mediator between socioeconomic position and diet quality in Australian first-time mothers. J Am Diet Assoc. 2011;111(5):696–704. [DOI] [PubMed] [Google Scholar]
- 59. O'Brien G, Davies M. Nutrition knowledge and body mass index. Health Educ Res. 2007;22(4):571–5. [DOI] [PubMed] [Google Scholar]
- 60. Malloy-Weir L, Cooper M. Health literacy, literacy, numeracy and nutrition label understanding and use: a scoping review of the literature. J Hum Nutr Diet. 2017;30(3):309–25. [DOI] [PubMed] [Google Scholar]
- 61. Sharif MZ, Rizzo S, Prelip ML, Glik DC, Belin TR, Langellier BA, Kuo AA, Garza JR, Ortega AN. The association between nutrition facts label utilization and comprehension among Latinos in two east Los Angeles neighborhoods. JAcad Nutr Diet. 2014;114(12):1915–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.