Abstract
This study was undertaken in order to characterize Cryptosporidium meleagridis isolated from a turkey in Hungary and to compare the morphologies, host specificities, organ locations, and small-subunit RNA (SSU rRNA) gene sequences of this organism and other Cryptosporidium species. The phenotypic differences between C. meleagridis and Cryptosporidium parvum Hungarian calf isolate (zoonotic genotype) oocysts were small, although they were statistically significant. Oocysts of C. meleagridis were successfully passaged in turkeys and were transmitted from turkeys to immunosuppressed mice and from mice to chickens. The location of C. meleagridis was the small intestine, like the location of C. parvum. A comparison of sequence data for the variable region of the SSU rRNA gene of C. meleagridis isolated from turkeys with other Cryptosporidium sequence data in the GenBank database revealed that the Hungarian C. meleagridis sequence is identical to a C. meleagridis sequence recently described for a North Carolina isolate. Thus, C. meleagridis is a distinct species that occurs worldwide and has a broad host range, like the C. parvum zoonotic strain (also called the calf or bovine strain) and Cryptosporidium felis. Because birds are susceptible to C. meleagridis and to some zoonotic strains of C. parvum, these animals may play an active role in contamination of surface waters not only with Cryptosporidium baileyi but also with C. parvum-like parasites.
Cryptosporidium parvum is a coccidian parasite that was recently recognized as an important intestinal pathogen of humans. Most C. parvum clinical infections are associated with a self-limiting diarrheal illness, but cryptosporidia can cause chronic, life-threatening disease in immunocompromised patients (7). In recent years there has been a dramatic increase in recognition of the importance of waterborne transmission of human cryptosporidiosis worldwide. In 1993, an outbreak in Milwaukee resulted in infection of more than 400,000 people and about 50 deaths (16). The lack of effective therapy for this disease complicates the control of human and animal cryptosporidiosis (7). In many countries, current drinking water regulations require that water intended for human consumption should not contain pathogenic organisms (8). However, little is known about the major source of oocyst contamination of surface and drinking waters and the sources of infection of human populations (14). Currently, PCR-based methods for monitoring water samples for C. parvum oocyst contamination are being developed. The possible existence of many Cryptosporidium species fostered the development of DNA techniques suitable for typing isolates. The commonly used techniques are PCR-restriction fragment length polymorphism analysis (2, 22, 23) and sequence analysis of taxonomically relevant loci (3, 24, 30, 42). However, it has been reported that some PCR methods cannot differentiate among Cryptosporidium meleagridis and various genotypes of C. parvum-like parasites (4).
Compared to the number of reported cases of infection by the other avian Cryptosporidium species, Cryptosporidium baileyi, the number of reported cases of C. meleagridis infection in birds is low (34, 36). To date, only the morphology of putative C. meleagridis isolates (9, 10, 28, 32) and the morphology and infectious potential of C. meleagridis isolates for birds (20) and mammals (6) have been described. Because some bovine isolates of C. parvum are known to infect birds (19, 27, 39) and because C. meleagridis and C. parvum oocysts cannot be differentiated unequivocally on the basis of size or morphology, it is not certain that C. meleagridis and C. parvum were the species analyzed in the studies mentioned above. It has also been suggested that C. meleagridis might be identical or very closely related to C. parvum, which infects more than 100 species of mammals (4, 12). It was recently demonstrated by Xiao et al. that C. meleagridis could be distinguished from C. parvum on the basis of the small-subunit (SSU) rRNA gene sequence (42). However, in this study the researchers did not characterize the morphology or the biologic features of the United States isolate studied.
The goal of the present study was to characterize and determine the taxonomic status of a putative C. meleagridis strain isolated from a turkey in Hungary by combining the traditional methods of classification with a sequence similarity analysis of a variable region of the SSU rRNA gene by using a recently described fast and reliable typing method for Cryptosporidium species (3, 30).
MATERIALS AND METHODS
Parasites.
Oocysts of C. meleagridis CMELH-1 were isolated from an 8-week-old turkey (strain 44 British United Turkeys BIG-6) in Hungary and were passaged in 1-week-old turkey poults of the same strain as described previously (37). Before infection, fecal samples were collected daily and examined to determine whether Cryptosporidium oocysts were present by using Sheather's sugar flotation method (29). Moderate oocyst shedding started on day 4 postinoculation and lasted for 8 to 10 days. Oocysts of C. parvum CPARH-1 were isolated from a 2-week-old calf in Hungary and were passaged in female C57BL/6N specific-pathogen-free mice (Charles River Laboratories, Wilmington, Mass.) by using the method of Healey et al. (15). Oocysts were collected and stored and inocula were prepared by using standard procedures (29).
Morphologic evaluation of oocysts.
Oocysts of C. meleagridis and C. parvum that were less than 2 weeks old were purified by using discontinuous sucrose gradient centrifugation (38) and were washed in phosphate-buffered saline (pH 7.2) to remove potassium dichromate before measurements were obtained. Purified oocysts (40 oocysts of both isolates) were measured by using a magnification of ×1,250 and Nomarski interference contrast microscopy. A statistical analysis was performed by using the InStat 2.0 program (GraphPad Software Inc., San Diego, Calif.). Mean values were compared by performing the Student t test. Differences were considered significant when P was <0.05.
Host specificity and tissue location.
Thirty female C57BL/6N pathogen-free mice (Charles River Laboratories) weighing 14 to 16 g were immunosuppressed with phosphated dexamethasone (15) and were divided into the following three groups: uninfected control mice, mice infected with C. parvum (ICP mice), and mice infected with C. meleagridis (ICM mice). The animals in the ICP and ICM mouse groups were inoculated intragastrically with 106 C. parvum oocysts and 106 C. meleagridis oocysts, respectively. Feed (Charles River Laboratories) and boiled water were available ad libitum. After inoculation, daily fecal samples were obtained from the mice and were examined by using Sheather's sugar flotation method. One-half of the animals were killed on day 10 postinoculation, and the entire digestive tract of each mouse was fixed in 10% buffered formalin and used for histopathology studies. Hematoxylin- and eosin-stained sections were prepared from the stomach, small intestine, and large intestine and were examined by light microscopy. The oocysts were collected and purified as described above. The total oocyst output of mice was determined from the pooled samples by the quantitative method based on the low sedimentation speed of oocysts (41).
Newly hatched Arbor Acres male chickens (Bábolna Co., Bábolna, Hungary) were housed in electrically heated wire bottom batteries with continuous illumination. Feed and boiled water were available ad libitum. The basal diet (Bábolna Co.) consisted of a commercial type of finisher ration that contained 16.6% crude protein and had been specially formulated to exclude anticoccidial agents, antioxidants, and antibiotics. When the birds were 7 days old, they were assigned to three groups of 10 on the basis of body weight (uninfected control, ICM, and ICP chickens) and were inoculated orally with 106 C. meleagridis oocysts or 106 C. parvum oocysts isolated from mice. The experimental design and method were identical to the experimental design and method described above.
DNA extraction and PCR amplification.
Purified C. parvum and C. meleagridis oocysts were harvested by centrifugation, and each pellet was resuspended in 200 μl of saline EDTA (10 mM Tris-HCl, 10 mM EDTA, 50 mM NaCl; pH 7.5) containing 10 μl of 20% (wt/vol) sodium dodecyl sulfate and 10 μl of a 10-mg/ml solution of proteinase K. To release total genomic DNA, the samples were frozen (liquid nitrogen, 5 min) and thawed (75°C, 5 min) three times and then incubated at 58°C for 1 h. DNA was extracted with phenol-chloroform and was further purified with a Prep-A-Gene DNA purification kit as described by the manufacturer (Bio-Rad, Hercules, Calif.). Cryptosporidium genus-specific primers (CPBDIAGF and CPBDIAGR) were used to amplify the Cryptosporidium SSU rRNA variable region as described previously (17). Reactions were performed by using the GeneAmp 2400 PCR system (Perkin-Elmer, Foster City, Calif.). The following conditions were used for PCR: initial denaturation 95°C for 15 min; 35 cycles consisting of denaturation at 94°C for 30 s, annealing at 65°C for 30 s, and extension at 72°C for 1 min; and a final extension step consisting of 72°C for 9 min. Finally, the samples were cooled and kept at 4°C. PCR products were detected on ethidium bromide-stained 2% agarose gels (Gibco, Grand Island, N.Y.) by visualizing them with UV light.
DNA sequencing and sequence analysis.
PCR products were purified by using the Prep-A-Gene DNA purification kit. Sequencing reactions were carried out with the Perkin-Elmer Big Dye kit, and the products were analyzed with a model ABI 310 genetic analyzer (Perkin-Elmer Biosystems, Foster City, Calif.). The partial sequences of SSU rRNA genes were manually aligned with the sequences of other cryptosporidia published previously by using the ARB program package (21).
Nucleotide sequence accession numbers.
The sequences of the SSU rRNA gene diagnostic fragments of C. parvum CPARH-1 and C. meleagridis CMELH-1 have been deposited in the GenBank database under accession no. AJ242471 and AJ242472, respectively.
RESULTS AND DISCUSSION
Morphology.
While the oocysts of C. baileyi, Cryptosporidium muris, and Cryptosporidium serpentis can be clearly distinguished from C. meleagridis oocysts, the oocysts of Cryptosporidium felis, C. meleagridis, Cryptosporidium wrairi, and various C. parvum genotypes are similar in terms of size and morphology (Table 1). The form and structure of the C. parvum and C. meleagridis oocysts examined in this study were identical to the form and structure of oocysts described by other workers (20, 40). We were not able to detect any significant morphologic differences between C. parvum and C. meleagridis oocysts in terms of oocyst wall morphology, the size or localization of the oocyst residuum, and the number or morphology of sporozoites. Like C. felis (31), the differences between the lengths and widths of the oocysts of C. parvum and the oocysts of C. meleagridis were slight, but they were significant (C. parvum oocysts were 5.0 ± 0.05 by 4.4 ± 0.07 μm, while C. meleagridis oocysts were 4.8 ± 0.02 by 4.2 ± 0.03 μm). However, the magnitude of the intraspecific variation in C. parvum isolates is similar to the magnitude (3) observed in this study. Thus, morphologic analysis alone cannot be used to differentiate C. meleagridis from the Cryptosporidium species mentioned above.
TABLE 1.
Host ranges, locations, and morphometric characteristics of Cryptosporidium species that infect mammals, birds, and reptiles
| Taxon | Host rangea
|
Main location(s)c | Oocyst length (μm)d | Oocyst width (μm)d | Oocyst shape indexd | |
|---|---|---|---|---|---|---|
| Group | Occurrenceb | |||||
| C. parvume,f | Mammals | Fg | Small intestine | 4.9 (4.5–5.4)h | 4.4 (4.2–5.2) | 1.1 (1.0–1.3) |
| Birds | Ni | |||||
| Lower vertebrates | N | |||||
| C. meleagridise | Mammals | F | Small intestine | 5.0 (4.5–6.0) | 4.4 (4.2–5.3) | 1.1 (1.0–1.3) |
| Birds | F | |||||
| Lower vertebrates | N | |||||
| C. wrairij | Mammals | Fk | Small intestine | NAl | NA | NA |
| Birds | N | |||||
| Lower vertebrates | N | |||||
| C. felisj | Mammals | F | Small intestine | 4.6 (3.2–5.1) | 4.0 (3.0–4.0) | 1.1 (1.0–1.2) |
| Birds | ND | |||||
| Lower vertebrates | ND | |||||
| C. baileyij | Mammals | N | Cloaca, bursa, trachea | 6.4 (5.6–7.5) | 4.8 (4.8–5.7) | 1.3 (1.1–1.4) |
| Birds | F | |||||
| Lower vertebrates | N | |||||
| C. serpentisj | Mammals | N | Stomach | 6.2 (5.6–6.6) | 5.3 (4.8–5.6) | 1.2 (1.0–1.3) |
| Birds | ND | |||||
| Lower vertebrates | F | |||||
| C. murisj | Mammals | F | Stomach | 7.7 (6.5–8.1) | 5.2 (5.0–6.0) | 1.5 (1.2–1.6) |
| Birds | N | |||||
| Lower vertebrates | N | |||||
F, found; N, not found; ND, no data.
Data from this study and previous studies.
C. parvum is not a uniform species. There are several genotypes (anthroponotic, zoonotic, canine, etc.) that have different host ranges, but the phenotypes are very similar (3).
The host range is narrow to wide, depending on genotype (e.g., anthroponotic versus zoonotic).
Mean (range)
The zoonotic genotype is found in birds.
Data from previous studies.
The host range is narrow.
NA, not available. According to Chrisp et al. (5), “guinea pig cryptosporidia have essentially the same oocyst shape and size … as does C. parvum.”
Host specificity and site of infection.
In some previous studies, mild to moderate infections have been established in chickens following inoculation of C. parvum oocysts isolated from cattle (26). Other attempts to transmit various isolates of C. parvum to birds were unsuccessful (26, 36); nevertheless, anticryptosporidial antibodies were detected in the sera of the birds (25, 35), suggesting that an infection was established. Moreover, after infection with a Belgian bovine isolate of C. parvum, the total oocyst output of infected chickens was only 17% of the oocyst output of previously uninfected birds after oral challenge with C. baileyi, indicating that the parasite became established and that protective immunity developed (35). These findings suggest that strains of C. parvum differ with respect to host specificity. Recently, oocysts of C. meleagridis isolated from chickens proved to be infectious for several species of mammals, including mice, rats, rabbits, and cattle (6). In our study, the oocysts of C. meleagridis isolated from turkeys were successfully passaged in birds and were transmitted to immunosuppressed mice and vice versa. Similarly, the Hungarian bovine isolate of C. parvum passaged in mice was successfully transmitted to birds. In ICM and ICP mice, the prepatent periods (3 days), the patencies (until death between days 10 and 27 postinoculation), and the numbers of excreted oocysts (1.6 × 108 and 2 × 108 oocysts/animal) were almost identical. Oocyst shedding by ICM and ICP chickens started 3 days postinoculation and lasted until 16 and 12 days postinoculation, respectively. The total oocyst outputs of ICM and ICP birds were 7 × 106 and 3 × 106 oocysts/bird. The low oocyst output of ICM birds is consistent with previously described data (18). As observed previously (26, 36), we found that C. meleagridis and C. parvum mainly infected the small intestine.
SSU rRNA-based molecular typing.
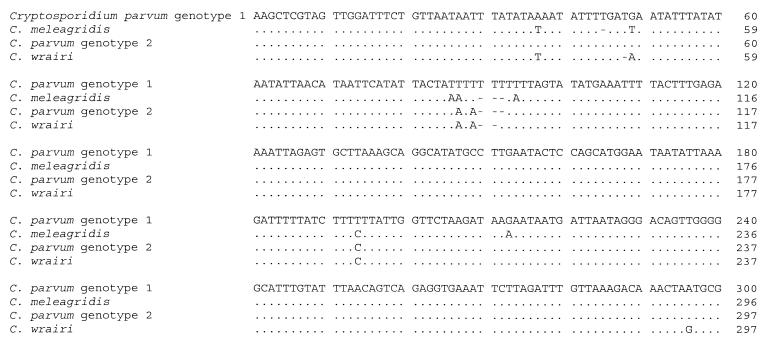
The sequence of the diagnostic fragment of the Hungarian bovine isolate C. parvum isolate CPARH-1 was identical to the sequences described for the C. parvum zoonotic genotype obtained from other geographic regions (30). After our C. meleagridis diagnostic SSU rRNA sequence for Hungarian isolate CMELH-1 was submitted to the GenBank database, another group submitted the complete sequence of the region coding for SSU rRNA for a North Carolina isolate of C. meleagridis (42) (GenBank accession no. AF112574). The overlapping regions of these two sequences are identical, suggesting that there may be very little genetic variation in the SSU rRNA region among geographically distinct isolates of this species. The sequence signature of the variable region of the SSU rRNA gene is unique (Fig. 1). Nevertheless, the high AT content of this region precludes the use of mutation-specific PCR and hybridization with specific probes; this leaves PCR followed by DNA sequencing as the most reliable technique for identifying species.
FIG. 1.
Alignment of the Cryptosporidium SSU rRNA gene diagnostic fragments obtained with primers CPBDIAGF and CPBDIAGR for C. parvum anthroponotic genotype 1, C. meleagridis, C. parvum zoonotic genotype 2, and C. wrairi. Only the first 300 columns of the alignments are shown, as the remaining columns were identical for all of the genotypes. Dashes indicate gaps, and dots indicate bases that are identical to the C. parvum genotype 1 bases. The GenBank accession numbers for the C. parvum genotype 1, C. meleagridis, C. parvum genotype 2, and C. wrairi sequences shown are L16997, AJ242472, AJ242471, and U11440, respectively. In the complete SSU rRNA coding sequence for the anthroponotic genotype of C. parvum (GenBank accession no. L16997), the region shown corresponds to positions 602 to 901.
It was recently demonstrated that C. meleagridis could not be distinguished from C. parvum by simple diagnostic PCR assays (4). Because there are marked differences in the cross-transmission potentials of various Cryptosporidium species or genotypes (Table 1) and because morphological methods are unreliable, it is necessary to use a standardized molecular technique for species identification in this genus. As shown in this study, sequencing the variable region of the SSU rRNA (3, 30) may be a reliable typing (species identification) technique. Other genetic loci, especially those coding for proteins, may be limited to identification of only the zoonotic and anthroponotic C. parvum genotypes (30).
The prevalence of cryptosporidiosis and the number of C. parvum-like oocysts in the feces of some wild bird species can be high (14, 33). Our findings indicate that birds may serve not only as passive carriers, as suggested by others (11, 13), but also as active vectors that increase contamination of water with some C. parvum-like parasites and play a role in waterborne cryptosporidiosis outbreaks. However, accurate identification of bird isolates and studies of the host ranges of these isolates, including studies of the susceptibility of humans to C. meleagridis, will be necessary in order to estimate the relative importance of birds in the epidemiology of cryptosporidiosis in humans and other mammals.
ACKNOWLEDGMENTS
We thank Zsuzsanna Egyed and Jánosné Haluska for technical assistance.
The Netherlands Organization for Scientific Research (NWO-OTKA grant N-28783), the Hungarian Research Fund (OTKA grants F-14646 and T-26057), a Bolyai János Postdoctoral Research Fellowship (grant BO/00480/98), and the European Cooperation in the Field of Scientific and Technical Development (COST Action 820) provided financial support.
REFERENCES
- 1.Békési L, Sréter T, Dobos-Kovács M, Varga I. Attempts to transmit Cryptosporidium baileyi, C. muris and C. parvum to aquatic lower vertebrates. Folia Parasitol. 1998;45:173–174. [Google Scholar]
- 2.Bonnin A, Fourmaux M N, Dubremetz J F, Nelson R G, Gobet P, Harly G, Buisson M, Puygauthier-Toubas D, Gabriel-Pospisil G, Naciri M, Camerlynck P. Genotyping human and bovine isolates of Cryptosporidium parvum by polymerase chain reaction-restriction fragment length polymorphism analysis of a repetitive DNA sequence. FEMS Microbiol Lett. 1996;137:207–211. doi: 10.1111/j.1574-6968.1996.tb08107.x. [DOI] [PubMed] [Google Scholar]
- 3.Bornay-Llinares F J, da Silva A J, Moura I N, Myjak P, Pietkiewicz H, Kruminis-Lozowska W, Graczyk T K, Pieniazek N J. Identification of Cryptosporidium felis in a cow by morphologic and molecular methods. Appl Environ Microbiol. 1999;65:1455–1458. doi: 10.1128/aem.65.4.1455-1458.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Champliaud D, Gobet P, Naciri M, Vagner O, Lopez J, Buisson J C, Varga I, Harly G, Mancassola R, Bonnin A. Failure to differentiate Cryptosporidium parvum from C. meleagridis based on PCR amplification of eight DNA sequences. Appl Environ Microbiol. 1998;64:1454–1458. doi: 10.1128/aem.64.4.1454-1458.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chrisp C E, Suckow M A, Fayer R, Arrowood M J, Healey M C, Sterling C R. Comparison of the host ranges and antigenicity of Cryptosporidium parvum and Cryptosporidium wrairi from guinea pigs. J Protozool. 1992;39:406–409. doi: 10.1111/j.1550-7408.1992.tb01471.x. [DOI] [PubMed] [Google Scholar]
- 6.Darabus G. Experimental studies of inter- and intraspecific transmission of Cryptosporidium parvum and C. meleagridis. Rev Romana Med Vet. 1997;7:155–160. [Google Scholar]
- 7.Fayer R, Speer C A, Dubey J P. The general biology of Cryptosporidium. In: Fayer R, editor. Cryptosporidium and cryptosporidiosis. Boca Raton, Fla: CRC Press; 1997. pp. 1–41. [Google Scholar]
- 8.Fricker C R, Crabb J H. Water-borne cryptosporidiosis: detection methods and treatment options. Adv Parasitol. 1998;40:241–278. doi: 10.1016/s0065-308x(08)60123-2. [DOI] [PubMed] [Google Scholar]
- 9.Goodwin M A. Small-intestinal cryptosporidiosis in a chicken. Avian Dis. 1988;32:844–848. [PubMed] [Google Scholar]
- 10.Goodwin M A, Steffens W L, Russell I D, Brown J. Diarrhea associated with intestinal cryptosporidiosis in turkeys. Avian Dis. 1988;32:63–67. [PubMed] [Google Scholar]
- 11.Graczyk T K, Cranfield M R. Experimental transmission of Cryptosporidium oocyst isolates from mammals, birds and reptiles to captive snakes. Vet Res. 1998;29:187–195. [PubMed] [Google Scholar]
- 12.Graczyk T K, Cranfield M R, Fayer R. Evaluation of commercial enzyme immunoassay (EIA) and immunofluorescent antibody (FA) test kits for detection of Cryptosporidium oocysts of species other than Cryptosporidium parvum. Am J Trop Med Hyg. 1996;54:274–279. doi: 10.4269/ajtmh.1996.54.274. [DOI] [PubMed] [Google Scholar]
- 13.Graczyk T K, Cranfield M R, Fayer R, Anderson M S. Viability and infectivity of Cryptosporidium parvum oocysts are retained upon intestinal passage through a refractory avian host. Appl Environ Microbiol. 1996;62:3234–3237. doi: 10.1128/aem.62.9.3234-3237.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Graczyk T K, Fayer R, Trout J M, Lewis E J, Farley C A, Sulaiman I, Lal A A. Giardia sp. cysts and infectious Cryptosporidium parvum oocysts in the feces of migratory Canada geese (Branta canadensis) Appl Environ Microbiol. 1998;64:2736–2738. doi: 10.1128/aem.64.7.2736-2738.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Healey M C, Yang S, Rasmussen K R, Jackson M K, Du C. Therapeutic efficacy of paromomycin in immunosuppressed adult mice infected with Cryptosporidium parvum. J Parasitol. 1995;81:114–116. [PubMed] [Google Scholar]
- 16.Hoxie N J, Davis J P, Vergeront J M, Nashold R D, Blair K A. Cryptosporidiosis-associated mortality following a massive waterborne outbreak in Milwaukee, Wisconsin. Am J Public Health. 1997;87:2032–2035. doi: 10.2105/ajph.87.12.2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson D W, Pieniazek N J, Griffin D W, Misener L, Rose J B. Development of a PCR protocol for sensitive detection of Cryptosporidium oocysts in water samples. Appl Environ Microbiol. 1995;61:3849–3855. doi: 10.1128/aem.61.11.3849-3855.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lindsay D S. Laboratory models of cryptosporidiosis. In: Fayer R, editor. Cryptosporidium and cryptosporidiosis. Boca Raton, Fla: CRC Press; 1997. pp. 209–223. [Google Scholar]
- 19.Lindsay D S, Blagburn B L, Ernest J A. Experimental Cryptosporidium parvum infections in chickens. J Parasitol. 1987;73:242–244. [PubMed] [Google Scholar]
- 20.Lindsay D S, Blagburn B L, Sundermann C A. Morphometric comparison of the oocysts of Cryptosporidium meleagridis and C. baileyi from birds. Proc Helminthol Soc Wash. 1989;56:91–92. [Google Scholar]
- 21.Ludwig W, Strunk O. ARB: a software environment for sequence data. Munich, Germany: Technical University of Munich; 1997. [Google Scholar]
- 22.Morgan U M, Constantine C C, Forbes D A, Thompson R C A. Differentiation between human and animal isolates of Cryptosporidium parvum using rDNA sequencing and direct PCR analysis. J Parasitol. 1997;83:825–830. [PubMed] [Google Scholar]
- 23.Morgan U M, Deplazes P, Forbes D A, Spano F, Hertzberg H, Sargent K D, Elliot A, Thompson R C A. Sequence and PCR-RFLP analysis of the internal transcribed spacers of the rDNA repeat unit in isolates of Cryptosporidium from different hosts. Parasitology. 1999;118:49–58. doi: 10.1017/s0031182098003412. [DOI] [PubMed] [Google Scholar]
- 24.Morgan U M, Sargent K D, Deplazes P, Forbes D A, Spano F, Hertzberg H, Elliot A, Thompson R C A. Molecular characterization of Cryptosporidium from various hosts. Parasitology. 1998;117:31–37. doi: 10.1017/s0031182098002765. [DOI] [PubMed] [Google Scholar]
- 25.Naciri M, Mancassola R, Reperant J M, Yvore P. Analysis of humoral immune response in chickens after inoculation with Cryptosporidium baileyi or Cryptosporidium parvum. Avian Dis. 1994;38:832–838. [PubMed] [Google Scholar]
- 26.O'Donoghue P J. Cryptosporidium and cryptosporidiosis in man and animals. Int J Parasitol. 1995;25:139–195. doi: 10.1016/0020-7519(94)e0059-v. [DOI] [PubMed] [Google Scholar]
- 27.Palkovič L, Marousek V. The pathogenicity of Cryptosporidium parvum Tyzzer, 1912 and C. baileyi Current, Upton et Haynes, 1986 for chickens. Folia Parasitol. 1989;36:209–217. [PubMed] [Google Scholar]
- 28.Pavlásek I. Localization of endogenous developmental stages of Cryptosporidium meleagridis Slavin, 1955 (Apicomplexa: Cryptosporidiidae) in birds. Vet Med. 1994;39:733–742. [PubMed] [Google Scholar]
- 29.Peeters J E, Villacorta L. Cryptosporidium. In: Eckert J, Braun R, Shirley M W, Coudert P, editors. Biotechnology—guidelines on techniques in coccidiosis research. Luxembourg, Luxembourg: ECSC-EC-EAEC; 1995. pp. 202–240. [Google Scholar]
- 30.Pieniazek N J, Bornay-Llinares F J, Slemenda S B, da Silva A J, Moura I N S, Arrowood M J, Ditrich O, Addiss D G. New Cryptosporidium genotypes in HIV-infected persons. Emerg Infect Dis. 1999;5:444–449. doi: 10.3201/eid0503.990318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sargent K D, Morgan U M, Elliot A, Thompson R C A. Morphological and genetic characterization of Cryptosporidium oocysts from domestic cats. Vet Parasitol. 1998;77:221–227. doi: 10.1016/s0304-4017(98)00122-8. [DOI] [PubMed] [Google Scholar]
- 32.Slavin D. Cryptosporidium meleagridis (sp. nov.) J Comp Pathol. 1955;65:262–266. doi: 10.1016/s0368-1742(55)80025-2. [DOI] [PubMed] [Google Scholar]
- 33.Smith H V, Brown J, Coulson J C, Morris G P, Girdwood R W. Occurrence of oocysts of Cryptosporidium sp. in Larus spp. gulls. Epidemiol Infect. 1993;110:135–143. doi: 10.1017/s0950268800050767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Snyder D B, Current W L, Russek-Cohen E, Gorham S L, Mallinson E T, Marquardt W W, Savage P K. Serologic incidence of Cryptosporidium in Delmarva broiler flocks. Poult Sci. 1988;67:730–735. doi: 10.3382/ps.0670730. [DOI] [PubMed] [Google Scholar]
- 35.Sréter T, Hornok S, Varga I, Békési L, Széll Z. Attempts to immunize chickens against Cryptosporidium baileyi with C. parvum oocysts and Paracox vaccine. Folia Parasitol. 1997;44:77–80. [PubMed] [Google Scholar]
- 36.Sréter T, Varga I. Cryptosporidiosis in birds—a review. Vet Parasitol. 2000;87:261–279. doi: 10.1016/s0304-4017(99)00178-8. [DOI] [PubMed] [Google Scholar]
- 37.Sréter T, Varga I, Békési L. Effects of bursectomy and thymectomy on the development of resistance to Cryptosporidium baileyi in chickens. Parasitol Res. 1996;82:174–177. doi: 10.1007/s004360050090. [DOI] [PubMed] [Google Scholar]
- 38.Suresh P, Rehg J E. Comparative evaluation of several techniques for purification of Cryptosporidium parvum oocysts from rat feces. J Clin Microbiol. 1996;34:38–40. doi: 10.1128/jcm.34.1.38-40.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tzipori S, Angus K W, Campbell I, Gray E W. Cryptosporidium: evidence for a single-species genus. Infect Immun. 1980;30:884–886. doi: 10.1128/iai.30.3.884-886.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Upton S J, Current W L. The species of Cryptosporidium (Apicomplexa: Cryptosporidiidae) infecting mammals. J Parasitol. 1985;71:625–629. [PubMed] [Google Scholar]
- 41.Varga I, Sréter T, Békési L. Quantitative method to assess Cryptosporidium oocyst shedding in the chicken model. Parasitol Res. 1995;81:262–264. doi: 10.1007/BF00937120. [DOI] [PubMed] [Google Scholar]
- 42.Xiao L, Escalante L, Yang C, Sulaiman I, Escalante A A, Montali R J, Fayer R, Lal A A. Phylogenetic analysis of Cryptosporidium parasites based on the small-subunit rRNA gene locus. Appl Environ Microbiol. 1999;65:1578–1583. doi: 10.1128/aem.65.4.1578-1583.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]