Abstract
Background
Pregnant and postpartum women are at increased risk for severe illness from COVID-19. We assessed COVID-19 vaccination coverage, intent, and attitudes among women of reproductive age overall and by pregnancy status in the United States.
Methods
Data from the National Immunization Survey Adult COVID Module collected during April 22-November 27, 2021, were analyzed to assess COVID-19 vaccination (receipt of ≥1 dose), intent for vaccination, and attitudes towards vaccination among women aged 18–49 years overall and by pregnancy status (trying to get pregnant, currently pregnant, breastfeeding, and not trying to get pregnant or currently pregnant or breastfeeding). Logistic regression and predictive marginals were used to generate unadjusted and adjusted prevalence ratios (PRs and aPRs). Trend analyses were conducted to assess monthly changes in vaccination and intent.
Results
Our analyses included 110,925 women aged 18–49 years. COVID-19 vaccination coverage (≥1 dose) was 63.2% overall (range from 53.3% in HHS Region 4 to 76.5% in HHS Region 1). Vaccination coverage was lowest among pregnant women (45.1%), followed by women who were trying to get pregnant (49.5%), women who were breastfeeding (51.5%), and all other women (64.9%). Non-Hispanic (NH) Black women who were pregnant or breastfeeding had significantly lower vaccination coverage (aPR: 0.74 and 0.66, respectively) than NH White women.
Discussion
Our findings are consistent with other studies showing lower vaccination coverage among pregnant individuals, with substantially lower vaccination coverage among NH Black women who are pregnant or breastfeeding. Given the overlapping and disproportionate risks of COVID-19 and maternal mortality among Black women, it is critical that COVID-19 vaccination be strongly recommended for these populations and all women of reproductive age. Healthcare and public health providers may take advantage of every opportunity to encourage vaccination and enlist the assistance of community leaders, particularly in communities with low vaccination coverage.
Keywords: COVID-19, Pregnancy, Vaccination, Intent, Reproductive age
1. Introduction
As of January 31, 2022, over 75 million cases of COVID-19 were reported in the United States, with more than 880,000 reported deaths [1]. COVID-19 vaccines have been available in the United States since December 2020 and are currently recommended for everyone aged 5 years and older, including people who are pregnant, lactating, trying to get pregnant now, or who might become pregnant in the future [2], [3]. Pregnant and postpartum women are at increased risk for severe illness from COVID-19, including intensive care admission, mechanical ventilation, or death, compared with nonpregnant women of reproductive age [4], [5], [6], [7], [8]. Pregnant women with COVID-19 are also at increased risk for pregnancy complications such as preterm birth and stillbirth [4], [5], [8], [9], [10].
Although 87% of adults aged ≥18 years have received ≥1 dose of a COVID-19 vaccine in the United States [11], national and state level data on COVID-19 vaccination coverage in pregnant women, as well as women who are trying to get pregnant or breastfeeding are limited. The information provided in this report is intended to aid in improving these populations’ vaccination rates. The main objective of this study was to assess COVID-19 vaccination coverage, intent, and factors associated with receipt of a COVID-19 vaccine among women of reproductive age by pregnancy status, including women who are currently pregnant, breastfeeding, trying to get pregnant, or of reproductive age who are not part of the three aforementioned groups. Secondary objective was to assess attitudes and behavior towards COVID-19 disease and vaccines. The final objective was to provide COVID-19 vaccination coverage among women of reproductive age by HHS regions and state. In addition, given the strong association between provider recommendation for vaccination and receipt of vaccination [12], [13], [14], this study also provided the prevalence of provider recommendation for COVID-19 vaccination among women of reproductive age overall, by pregnancy status, and HHS regions.
2. Methods
The National Immunization Survey Adult COVID Module (NIS-ACM) is a household telephone survey of adults aged ≥18 years that uses the NIS random-digit-dialed sample of cellular telephone numbers [15]. The interviews are conducted in English, Spanish, and any other language. Data from seven data collection cycles in 2021 were used for these analyses (April 22-May 29, May 30-June 26, June 27-July 31, August 1-August 28, August 29-September 25, September 26-October 30, and October 31-November 27). Response rates were calculated according to the American Association for Public Opinion Research [16] and ranged from 17.2% to 23.4%.
Pregnancy status was assessed through the following question: “Are you currently trying to get pregnant, pregnant, or breastfeeding?” where respondents could choose one of the categories. An additional 866 pregnant women were included who answered yes to the question “Do you have a health condition that may put you at higher risk for COVID-19?” and reported pregnancy as the health condition that may put them at higher risk for COVID-19 (these women were not asked the question on whether they were currently pregnant). COVID-19 vaccination coverage was assessed by asking, “Have you received at least one dose of a COVID-19 vaccine?”; those who answered “no” were asked “How likely are you to get a COVID-19 vaccine? would you say you would definitely get a vaccine, probably get a vaccine, probably not get a vaccine, definitely not get a vaccine, or are not sure?”.
Race and ethnicity were self-reported through two questions, “Please choose one or more of the following categories to describe your race. Are you White, Black or African American, American Indian, Alaska Native, Asian, Native Hawaiian or other Pacific Islander”, and “Are you of Hispanic or Latino origin?”. For the purpose of analysis, American Indian, Alaska Native, and Native Hawaiian or other Pacific Islander were combined together. Respondents who identified as “other” or chose multiple categories to describe their race were grouped into “other/multiple races”.
Attitudes toward vaccination were assessed based on the Behavioral and Social Drivers of Vaccination framework and the Increasing Vaccination Model. This framework identified three domains influencing vaccine uptake and intent: what people think and feel, social process, and practical issues [17]. Attitudes were assessed by responses to four questions: “How concerned are you about getting COVID-19? “How important do you think getting a COVID-19 vaccine is to protect yourself against COVID-19?”, “How safe do you think a COVID-19 vaccine is for you?, and “If you had to guess, about how many of your family and friends have received a COVID-19 vaccine? Would you say none; some; many; or almost all?” [18].
COVID-19 vaccination coverage for receipt of ≥1 dose and intent for vaccination was assessed among all women aged 18–49 years and four subgroups—women who are trying to get pregnant, pregnant, breastfeeding, and those who were not trying to get pregnant, pregnant, or breastfeeding—overall and by sociodemographic characteristics and Department of Health and Human Services (HHS) regions [19].
Multivariable analyses examined factors associated with receiving ≥1 dose of a COVID-19 vaccine overall and by the aforementioned subgroups. Analyses used logistic regression and predictive marginals to generate unadjusted and adjusted prevalence ratios (PRs and aPRs). Adjusted analyses controlled for age group, race and ethnicity, education, income, insurance status, metropolitan statistical area, receipt of any other vaccine in the past two years, comorbidity status, provider recommendation for COVID-19 vaccination, essential worker status, and work or school requirement for vaccination. Trend analyses were conducted to assess monthly changes in vaccination and intent from the start to the end of the data collection period. Additionally, COVID-19 vaccination status was assessed among pregnant women before (May-July 2021) and after (August-November 2021) CDC strengthened their recommendation to vaccinate before, during, and after pregnancy [20]. Data were analyzed using SAS (version 9.4) and SUDAAN (version 11.0.3; Research Triangle Institute). Results were weighted to represent the noninstitutionalized U.S. adult population aged ≥18 years and calibrated to COVID-19 vaccine administration data by jurisdiction, age group, and sex [1]. Accompanying 95% Confidence Intervals were calculated. For all analyses, statistical significance was defined as p < 0.05. This activity was reviewed by the CDC and was conducted consistent with applicable federal law and CDC policy (See, e.g., 45 C.F.R. part 46.102 (l) (2), 21 C.F.R. part 56; 42 U.S.C. §241 (d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.).
3. Results
Our analyses included 110,925 women aged 18–49 years, of whom 3.7% were trying to get pregnant, 3.4% were pregnant, 3.2% were breastfeeding, and 89.7% were not trying to get pregnant, were not pregnant or breastfeeding (all other women 18–49 years). Overall, 63.2% of women reported receiving ≥1 dose of a COVID-19 vaccine, 4.6% reported that they “will definitely” get a vaccine, 5.4% “will probably” get a vaccine, 7.7% were “unsure” about getting a vaccine, 6.1% “probably will not”, and 12.9% “definitely will not” receive a vaccine. Vaccination coverage was lowest among pregnant women (45.1%), followed by women who were trying to get pregnant (49.5%), women who were breastfeeding (51.5%), and all other women 18–49 years (64.9%). We observed the highest vaccination coverage, regardless of pregnancy status, among women who were aged 35–49 years, non-Hispanic (NH) Asian, college-educated, insured, living in non-rural areas, received other vaccines in the previous two years, had comorbidities in addition to pregnancy, received a provider recommendation for a COVID-19 vaccine, had school or work requirement for vaccination, never had COVID-19, and worked at school and childcare setting (except for women who were breastfeeding, among whom vaccination coverage was higher among those who considered themselves essential healthcare workers) (Table 1 , Supplementary Table 1).
Table 1.
Receipt of ≥1 dose of a COVID-19 vaccine among women aged 18–49 years by pregnancy status and select characteristics ─ National Immunization Survey-Adult COVID Module, United States, April 22-November 27, 2021.
| All women aged 18–49 years |
Women who were trying to get pregnant at the time of the survey |
Women who were pregnant at the time of the survey |
Women who were breastfeeding at the time of the survey |
All other women aged 18–49 years |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Receipt of ≥1 dose | Total | Receipt of ≥1 dose | Total | Receipt of ≥1 dose | Total | Receipt of ≥1 dose | Total | Receipt of ≥1 dose | |
| N(Weighted %) | Weighted % (95 %CI) | N(Weighted %) | Weighted % (95 %CI) | N(Weighted %) | Weighted % (95 %CI) | N(Weighted %) | Weighted % (95 %CI) | N(Weighted %) | Weighted % (95 %CI) | |
| Total | 110,925 (1 0 0) | 63.2 (62.6–63.8) | 3,949 (1 0 0) | 49.5 (46.4–52.6) | 3,433 (1 0 0) | 45.1 (42.0–48.3) | 3,740 (1 0 0) | 51.5 (48.2–54.7) | 99,803 (1 0 0) | 64.9 (64.3–65.5) |
| Age Groups (in years) | ||||||||||
| 18–24 | 19,053 (20.5) | 59.5 (58.1–60.9) | 389 (15.1) | 20.6 (15.4–26.9) | 531 (21.8) | 29.7 (23.8–36.3) | 325 (15.5) | 28.7 (20.9–37.9) | 17,808 (20.9) | 62.7 (61.3–64.0) |
| 25–34 | 35,492 (30.8) | 57.7 (56.6–58.8) | 2,051 (51.7) | 47.9 (44.0–51.9) | 1,857 (52.2) | 43.7 (39.6–47.9) | 2,069 (54.4) | 49.8 (45.6–54.1) | 29,515 (28.2) | 60.0 (58.8–61.2) |
| 35–49 | 56,380 (48.7) | 68.3 (67.5–69.1) | 1,509 (33.2) | 64.9 (59.6–69.8) | 1,045 (26.0) | 61.0 (54.3–67.4) | 1,346 (30.1) | 66.3 (60.3–71.7) | 52,480 (50.9) | 68.6 (67.7–69.5) |
| Race and Ethnicity | ||||||||||
| Non-Hispanic White | 62,829 (54.5) | 62.7 (61.9–63.5) | 2,005 (51.7) | 47.4 (43.2–51.5) | 1,917 (51.5) | 45.3 (41.2–49.5) | 2,155 (53.6) | 54.5 (50.2–58.8) | 56,752 (54.8) | 64.2 (63.4–65.1) |
| Non-Hispanic Black | 13,605 (13.0) | 53.4 (51.8–55.0) | 605 (14.9) | 45.0 (37.5–52.8) | 402 (14.4) | 31.3 (24.3–39.4) | 367 (11.2) | 31.1 (23.8–39.5) | 12,231 (13.0) | 55.4 (53.7–57.1) |
| Hispanic | 18,851 (22.1) | 66.5 (65.1–67.9) | 683 (21.2) | 54.9 (47.5–62.0) | 645 (25.1) | 48.2 (41.2–55.3) | 667 (26.1) | 49.0 (41.9–56.2) | 16,856 (21.8) | 68.5 (67.1–70.0) |
| Non-Hispanic Asian | 7,286 (5.4) | 88.7 (86.8–90.4) | 329 (5.6) | 79.1 (68.6–86.8) | 206 (5.1) | 69.8 (54.1–81.9) | 265 (4.5) | 81.7 (69.7–89.6) | 6,486 (5.5) | 90.0 (88.0–91.8) |
| Non-Hispanic AI/AN/NHOPI | 2,430 (1.4) | 54.3 (49.7–58.9) | 110 (1.4) | 27.6 (14.8–45.5) | 86 (1.7) | 45.2 (20.6–72.4) | 100 (1.2) | 60.8 (35.4–81.5) | 2,134 (1.4) | 55.7 (50.9–60.5) |
| Non-Hispanic other/multiple racesa | 4,675 (3.6) | 55.5 (52.3–58.7) | 186 (5.0) | 34.1 (21.9–48.9) | 140 (2.1) | 41.7 (30.3–54.1) | 153 (3.5) | 43.5 (28.3–60.0) | 4,196 (3.6) | 57.5 (54.0–60.8) |
| Educational Status | ||||||||||
| High school or less | 22,072 (33.3) | 52.1 (51.0–53.3) | 718 (30.8) | 34.8 (29.2–40.8) | 699 (37.1) | 33.3 (28.1–38.9) | 603 (29.9) | 31.4 (26.0–37.4) | 20,052 (33.4) | 54.2 (53.0–55.4) |
| Some college | 31,890 (33.1) | 58.5 (57.5–59.6) | 1,119 (33.6) | 45.6 (40.3–51.0) | 857 (30.1) | 41.3 (35.6–47.1) | 857 (30.3) | 47.7 (41.5–54.0) | 29,057 (33.3) | 60.0 (58.9–61.1) |
| College graduate | 32,877 (22.1) | 75.6 (74.5–76.7) | 1,116 (21.2) | 64.0 (58.5–69.1) | 1,021 (20.4) | 56.0 (49.5–62.3) | 1,108 (23.4) | 62.1 (56.0–67.8) | 29,632 (22.2) | 77.3 (76.1–78.4) |
| Above college graduate | 24,086 (11.5) | 85.3 (84.2–86.4) | 996 (14.4) | 68.3 (61.2–74.7) | 856 (12.3) | 72.3 (63.7–79.5) | 1,172 (16.4) | 79.7 (73.1–85.0) | 21,062 (11.1) | 87.1 (85.9–88.2) |
| Annual Household Incomeb, USD | ||||||||||
| Below poverty | 12,853 (14.5) | 48.4 (46.8–50.0) | 396 (12.0) | 33.7 (26.3–41.9) | 414 (15.4) | 26.7 (20.5–33.9) | 433 (14.9) | 33.4 (26.0–41.7) | 11,610 (14.5) | 50.3 (48.6–52.0) |
| Above poverty and <$75,000 | 35,685 (32.9) | 59.7 (58.7–60.8) | 1,142 (34.5) | 41.3 (36.1–46.7) | 935 (33.2) | 38.5 (33.1–44.1) | 877 (29.9) | 38.8 (32.9–45.1) | 32,731 (32.9) | 62.0 (60.9–63.1) |
| Above poverty and ≥ $75,000 | 42,362 (32.0) | 76.4 (75.5–77.3) | 1,793 (35.5) | 62.2 (57.2–67.0) | 1,475 (30.8) | 65.9 (60.5–70.9) | 1,813 (36.1) | 73.5 (68.8–77.8) | 37,281 (31.7) | 77.6 (76.6–78.6) |
| Unknown income | 20,025 (20.7) | 58.8 (57.5–60.2) | 618 (18.0) | 50.3 (43.0–57.7) | 609 (20.6) | 38.7 (32.0–46.0) | 617 (19.0) | 43.6 (36.4–51.0) | 18,181 (20.8) | 60.4 (59.0–61.8) |
| Insurance status | ||||||||||
| Insured | 99,110 (88.1) | 65.1 (64.4–65.7) | 3,533 (88.8) | 50.4 (47.1–53.7) | 3,164 (91.1) | 46.0 (42.7–49.3) | 3,399 (90.0) | 53.5 (50.0–57.0) | 89,014 (87.9) | 66.9 (66.2–67.5) |
| Not insured | 10,241 (11.9) | 50.9 (49.0–52.7) | 357 (11.2) | 40.7 (31.9–50.2) | 226 (8.9) | 36.7 (26.4–48.3) | 308 (10.0) | 35.4 (27.3–44.4) | 9,350 (12.1) | 52.1 (50.2–54.0) |
| MSAc | ||||||||||
| MSA, Principal City | 39,497 (33.0) | 67.3 (66.3–68.3) | 1,398 (33.1) | 53.3 (47.9–58.7) | 1,236 (35.5) | 47.1 (41.6–52.7) | 1,260 (29.2) | 57.2 (51.6–62.6) | 35,603 (33.0) | 69.1 (68.0–70.1) |
| MSA, Non-Principal City | 53,888 (54.9) | 63.8 (63.0–64.6) | 1,897 (54.5) | 50.0 (45.7–54.3) | 1,666 (53.3) | 46.8 (42.5–51.0) | 1,865 (57.2) | 51.6 (47.1–56.1) | 48,460 (54.9) | 65.4 (64.6–66.3) |
| Non-MSA | 17,540 (12.2) | 49.7 (48.1–51.3) | 654 (12.5) | 37.0 (29.9–44.7) | 531 (11.2) | 31.2 (24.1–39.4) | 615 (13.6) | 38.5 (30.7–46.9) | 15,740 (12.1) | 51.4 (49.6–53.1) |
| Receipt of any vaccine other than COVID-19 in the past 2 years | ||||||||||
| Yes | 63,760 (50.3) | 78.0 (77.2–78.7) | 2,165 (45.6) | 62.7 (58.0–67.2) | 2,137 (51.4) | 56.8 (52.4–61.1) | 2,761 (63.7) | 65.9 (62.0–69.6) | 56,697 (50.0) | 80.0 (79.2–80.7) |
| No | 46,518 (49.7) | 48.3 (47.5–49.2) | 1,755 (54.4) | 38.2 (34.2–42.4) | 1,282 (48.6) | 32.7 (28.4–37.2) | 956 (36.3) | 27.2 (22.7–32.2) | 42,525 (50.0) | 49.9 (49.0–50.8) |
| Comorbidities other than pregnancyd | ||||||||||
| Yes | 26,703 (23.8) | 68.1 (66.8–69.2) | 922 (22.3) | 56.3 (50.1–62.3) | 1,417 (33.2) | 54.5 (49.1–59.8) | 575 (13.9) | 63.9 (54.6–72.3) | 23,789 (23.9) | 69.3 (68.0–70.6) |
| No | 83,398 (76.2) | 61.9 (61.2–62.6) | 2,999 (77.7) | 47.8 (44.2–51.4) | 1,986 (66.8) | 40.7 (36.8–44.6) | 3,145 (86.1) | 49.4 (45.9–52.8) | 75,268 (76.1) | 63.7 (63.0–64.4) |
| Provider recommendation for COVID-19 vaccination | ||||||||||
| Yes | 47,977 (39.8) | 74.1 (73.2–75.0) | 1,821 (40.2) | 64.2 (59.3–68.9) | 1,905 (48.2) | 58.5 (53.8–63.0) | 2,167 (50.4) | 71.0 (66.7–74.9) | 47,977 (39.8) | 75.4 (74.5–76.3) |
| No | 62,130 (60.2) | 56.0 (55.2–56.8) | 2,111 (59.8) | 39.5 (35.7–43.4) | 1,509 (51.8) | 33.2 (29.3–37.3) | 1,543 (49.6) | 31.7 (27.9–35.8) | 56,967 (61.0) | 58.1 (57.3–58.9) |
| Does your school or work require COVID-19 vaccinatione | ||||||||||
| Yes | 24,759 (20.3) | 88.7 (87.7–89.6) | 894 (19.5) | 77.8 (69.9–84.1) | 670 (17.0) | 76.0 (67.9–82.5) | 702 (15.5) | 80.0 (70.9–86.7) | 22,493 (20.6) | 89.8 (88.8–90.7) |
| No | 81,158 (79.7) | 57.6 (56.9–58.3) | 2,903 (80.5) | 43.0 (39.6–46.4) | 2,587 (83.0) | 39.4 (36.0–42.9) | 2,737 (84.5) | 47.0 (43.3–50.7) | 72,931 (79.4) | 59.3 (58.6–60.1) |
| Frontline or essential workerf | ||||||||||
| Essential healthcare | 21,434 (16.9) | 73.1 (71.8–74.4) | 976 (22.5) | 56.4 (50.2–62.5) | 698 (15.4) | 58.4 (51.1–65.5) | 747 (14.5) | 66.8 (58.9–73.9) | 19,013 (16.8) | 74.8 (73.4–76.1) |
| School and Childcare | 7,037 (4.9) | 80.8 (78.7–82.6) | 244 (5.0) | 56.9 (44.6–68.3) | 183 (3.9) | 63.5 (48.0–76.7) | 203 (3.6) | 65.7 (51.0–77.8) | 6,407 (4.9) | 82.7 (80.6–84.6) |
| Other frontline worker | 6,434 (6.8) | 57.3 (55.0–59.7) | 231 (6.8) | 43.2 (32.2–55.0) | 163 (6.3) | 51.8 (38.5–64.9) | 133 (4.7) | 51.7 (35.8–67.2) | 5,907 (6.9) | 58.2 (55.7–60.7) |
| Other essential worker | 10,187 (9.7) | 58.7 (56.7–60.7) | 419 (12.0) | 45.0 (36.8–53.5) | 272 (8.6) | 42.6 (32.9–52.9) | 229 (7.3) | 47.6 (33.5–62.1) | 9,267 (9.7) | 60.3 (58.2–62.4) |
| Persons who are not essential workers | 65,339 (61.7) | 60.7 (60.0–61.5) | 2,057 (53.7) | 47.9 (43.6–52.3) | 2,102 (65.8) | 40.4 (36.6–44.3) | 2,412 (69.9) | 48.3 (44.4–52.2) | 58,768 (61.6) | 62.5 (61.7–63.3) |
| Ever had COVID-19 | ||||||||||
| Yes | 21,666 (23.4) | 51.3 (50.1–52.6) | 856 (28.6) | 42.4 (36.3–48.7) | 689 (24.6) | 32.3 (26.6–38.5) | 642 (21.7) | 39.6 (32.7–47.0) | 19,479 (23.2) | 53.0 (51.6–54.3) |
| No | 88,233 (76.6) | 67.1 (66.5–67.8) | 3,053 (71.4) | 52.6 (49.1–56.2) | 2,719 (75.4) | 49.5 (45.8–53.2) | 3,062 (78.3) | 55.0 (51.2–58.7) | 79,399 (76.8) | 68.8 (68.1–69.5) |
Abbreviations: AI/AN/NHOPI = American Indian/Alaska Native/ Native Hawaiian and Other Pacific Islander; MSA = metropolitan statistical area; Ref = referent group; USD = U.S. dollars.
Respondents who identified as non-Hispanic or Latino origin and identified as “other” or chose multiple categories to describe their race were grouped into “other/multiple races”.
Household income is derived from the number of persons reported in the household, the reported household income, and the 2020 U.S. Census poverty thresholds.
MSA status was determined based on household reported city and county of residence and was grouped into three categories: MSA principal city (urban), MSA nonprincipal city (suburban), and non-MSA (rural). MSAs and principal cities were as defined by the U.S. Census Bureau (https://www.census.gov/programs-surveys/metro-micro.html). Non-MSA areas include urban populations not located within an MSA as well as completely rural areas.
Comorbidity status was ascertained by the following question: “Do you have a health condition that may put you at higher risk for COVID-19?”. This was followed by the question “Can you tell me what that is?” Responses to this second question indicate at least 75% of respondents interpreted the question as medical conditions that have been associated with higher risk of severe COVID-19.
Work or school requirement was assessed by the following question: “Does your work or school require you to get a COVID-19 vaccine?” Response options were yes, no, or unemployed/not applicable. Responses for “no” and “not applicable” were combined into one category.
Essential worker status was defined based on the following questions: “Are you a frontline or essential worker according to your state or region?” and “In what location or setting do you currently work?” Essential worker groups were categorized as “essential healthcare,” “school and childcare,” “other frontline,” “other essential,” and “nonessential.” Nonessential could include both employed and unemployed individuals.
When assessing factors independently associated with receiving ≥1 dose of a COVID vaccine, compared to referent groups defined in Table 2 , NH Black race and ethnicity was significantly associated with lower vaccination among pregnant women [aPR (95% CI): 0.74 (0.58–0.91)], women who were breastfeeding [aPR (95% CI): 0.66 (0.50–0.82)], and all other women 18–49 years [aPR (95% CI): 0.92 (0.89–0.95)]. NH Asian race and ethnicity, having received vaccines other than COVID-19 vaccines in the past two years, having had comorbidities in addition to pregnancy, having received a provider recommendation, and school or work requirement for COVID-19 vaccination were associated with significantly higher vaccination among all women 18–49 years regardless of pregnancy status. In addition, Hispanic ethnicity was associated with significantly higher vaccination among all other women 18–49 years [aPR (95% CI): 1.12 (1.10–1.14)]. Furthermore, lower education status and having had COVID-19 were significantly associated with lower vaccination among all women 18–49 years regardless of pregnancy status. Finally, lower household income and living in rural areas was significantly associated with lower vaccination among certain groups of women of reproductive age (Table 2).
Table 2.
Factors associated with receipt of ≥1 dose of a COVID-19 vaccine among women aged 18–49 years by pregnancy status ─ National Immunization Survey-Adult COVID Module, United States, April 22-November 27, 2021.
| Women who were trying to getpregnant at the time of the survey |
Women who were pregnant at the timeof the survey |
Women who were breastfeeding at the time of the survey |
All other women 18–49 years |
|||||
|---|---|---|---|---|---|---|---|---|
| PR (95 %CI) | aPR (95 %CI) | PR (95 %CI) | aPR (95 %CI) | PR (95 %CI) | aPR (95 %CI) | PR (95 %CI) | aPR (95 %CI) | |
| Age Groups (in years) | ||||||||
| 18–24 | 0.31 (0.23–0.42)a | 0.48 (0.35–0.62)a | 0.49 (0.39–0.62)a | 0.68 (0.54–0.82)a | 0.44 (0.32–0.59)a | 0.86 (0.71–1.02) | 0.91 (0.89–0.94)a | 0.94 (0.92–0.96)a |
| 25–34 | 0.74 (0.66–0.83)a | 0.81 (0.72–0.91)a | 0.72 (0.62–0.83)a | 0.80 (0.69–0.92)a | 0.76 (0.67–0.85)a | 0.88 (0.78–0.97)a | 0.87 (0.85–0.90)a | 0.91 (0.89–0.93)a |
| 35–49 (Referent) | – | – | – | – | – | – | – | – |
| Race/ethnicity | ||||||||
| Non-Hispanic White (Referent) | – | – | – | – | – | – | – | – |
| Non-Hispanic Black | 0.95 (0.79–1.16) | 0.97 (0.80–1.14) | 0.69 (0.53–0.89)a | 0.74 (0.58–0.91)a | 0.56 (0.43–0.74)a | 0.66 (0.50–0.82)a | 0.86 (0.83–0.89)a | 0.92 (0.89–0.95)a |
| Hispanic | 1.15 (0.98–1.35) | 1.13 (0.97–1.29) | 1.06 (0.89–1.26) | 1.11 (0.93–1.29) | 0.90 (0.76–1.06) | 1.11 (0.97–1.25) | 1.07 (1.04–1.09)a | 1.12 (1.10–1.14)a |
| Non-Hispanic Asian | 1.67 (1.44–1.93)a | 1.28 (1.04–1.51)a | 1.54 (1.23–1.92)a | 1.34 (1.00–1.68)a | 1.50 (1.29–1.73)a | 1.46 (1.23–1.69)a | 1.40 (1.37–1.44)a | 1.28 (1.24–1.33)a |
| Non-Hispanic AI/AN/NHOPI | 0.58 (0.33–1.03)a | 0.59 (0.29–0.89)a | 1.00 (0.53–1.89) | 0.85 (0.13–1.57) | 1.11 (0.74–1.69) | 1.39 (0.92–1.86) | 0.87 (0.80–0.95)a | 0.99 (0.93–1.05) |
| Non-Hispanic other/multiple racesb | 0.69 (0.46–1.04)a | 0.64 (0.39–0.88)a | 0.90 (0.67–1.23) | 1.04 (0.81–1.27) | 0.80 (0.54–1.17) | 0.93 (0.58–1.27) | 0.89 (0.84–0.95)a | 0.93 (0.88–0.98)a |
| Educational Status | ||||||||
| High school or less | 0.51 (0.42–0.61)a | 0.77 (0.61–0.94)a | 0.46 (0.38–0.56)a | 0.79 (0.63–0.95)a | 0.39 (0.32–0.48)a | 0.73 (0.59–0.87)a | 0.62 (0.61–0.64)a | 0.78 (0.76–0.80)a |
| Some college | 0.66 (0.57–0.77)a | 0.88 (0.74–1.03) | 0.57 (0.48–0.68)a | 0.79 (0.64–0.93)a | 0.60 (0.51–0.70)a | 0.92 (0.78–1.06) | 0.69 (0.67–0.70)a | 0.80 (0.78–0.82)a |
| College graduate | 0.94 (0.82–1.07) | 0.98 (0.83–1.13) | 0.77 (0.66–0.90)a | 0.81 (0.66–0.95)a | 0.78 (0.69–0.88)a | 0.90 (0.77–1.02) | 0.89 (0.87–0.90)a | 0.92 (0.90–0.95)a |
| Above college graduate (Referent) | – | – | – | – | – | – | – | – |
| Annual Household Incomec, USD | ||||||||
| Below poverty | 0.53 (0.42–0.68)a | 0.83 (0.65–1.01) | 0.40 (0.31–0.53)a | 0.63 (0.49–0.78)a | 0.45 (0.35–0.58)a | 0.70 (0.56–0.85)a | 0.65 (0.62–0.67)a | 0.81 (0.79–0.84)a |
| Above poverty and <$75,000 | 0.66 (0.57–0.77)a | 0.92 (0.80–1.05) | 0.58 (0.50–0.69)a | 0.76 (0.63–0.89)a | 0.53 (0.45–0.63)a | 0.75 (0.64–0.86)a | 0.80 (0.78–0.82)a | 0.92 (0.90–0.94)a |
| Above poverty & ≥ $75,000 (Referent) | – | – | – | – | – | – | – | – |
| Unknown income | 0.81 (0.68–0.96)a | 1.02 (0.85–1.19) | 0.59 (0.48–0.72)a | 0.76 (0.62–0.89)a | 0.59 (0.49–0.71)a | 0.84 (0.71–0.96)a | 0.78 (0.76–0.80)a | 0.90 (0.87–0.92)a |
| Insurance status | ||||||||
| Insured (Referent) | – | – | – | – | – | – | – | – |
| Not insured | 0.80 (0.63–1.02)a | 0.92 (0.74–1.10) | 0.80 (0.58–1.09) | 0.88 (0.67–1.08) | 0.66 (0.51–0.85)a | 0.98 (0.81–1.14) | 0.78 (0.75–0.81)a | 0.98 (0.95–1.00) |
| MSAd | ||||||||
| MSA, Principal City (Referent) | – | – | – | – | – | – | – | – |
| MSA, Non-Principal City | 0.94 (0.82–1.08) | 1.00 (0.89–1.12) | 0.99 (0.86–1.15) | 0.99 (0.86–1.12) | 0.91 (0.79–1.03) | 0.94 (0.84–1.04) | 0.95 (0.93–0.97)a | 0.96 (0.94–0.98)a |
| Non-MSA | 0.69 (0.55–0.87)a | 0.91 (0.75–1.07) | 0.66 (0.50–0.87)a | 0.89 (0.71–1.08) | 0.67 (0.53–0.85)a | 0.88 (0.75–1.01) | 0.74 (0.72–0.77)a | 0.87 (0.85–0.90)a |
| Receipt of any vaccine other than COVID-19 in the past 2 years | ||||||||
| Yes | 1.64 (1.44–1.87)a | 1.38 (1.22–1.54)a | 1.74 (1.49–2.03)a | 1.28 (1.10–1.46)a | 2.42 (2.01–2.91)a | 1.51 (1.29–1.74)a | 1.60 (1.57–1.63)a | 1.34 (1.31–1.37)a |
| No (Referent) | – | – | – | – | – | – | – | – |
| Comorbidities other than pregnancye | ||||||||
| Yes | 1.18 (1.03–1.35)a | 1.11 (0.97–1.24) | 1.34 (1.16–1.53)a | 1.05 (0.92–1.17) | 1.29 (1.11–1.51)a | 1.14 (0.99–1.29) | 1.09 (1.06–1.11)a | 1.07 (1.04–1.09)a |
| No (Referent) | – | – | – | – | – | – | – | – |
| Provider recommendation for COVID-19 vaccination | ||||||||
| Yes | 1.61 (1.43–1.82)a | 1.34 (1.19–1.49)a | 1.76 (1.52–2.04)a | 1.38 (1.20–1.56)a | 2.24 (1.95–2.57)a | 1.62 (1.43–1.81)a | 1.30 (1.27–1.32)a | 1.13 (1.11–1.15)a |
| No (Referent) | – | – | – | – | – | – | – | – |
| Does your school or work require COVID-19 vaccinationf | ||||||||
| Yes | 1.80 (1.59–2.02)a | 1.61 (1.43–1.79)a | 1.93 (1.70–2.20)a | 1.76 (1.52–1.99)a | 1.70 (1.50–1.93)a | 1.50 (1.32–1.68)a | 1.51 (1.49–1.54)a | 1.40 (1.38–1.43)a |
| No (Referent) | – | – | – | – | – | – | – | – |
| Frontline or essential workerg | ||||||||
| Essential healthcare | 1.17 (1.02–1.35)a | 0.89 (0.77–1.01) | 1.45 (1.24–1.69)a | 1.03 (0.87–1.20) | 1.39 (1.21–1.59)a | 0.95 (0.81–1.08) | 1.19 (1.17–1.22)a | 1.00 (0.98–1.03) |
| School and Childcare | 1.20 (0.95–1.51) | 1.01 (0.76–1.25) | 1.57 (1.23–2.02)a | 1.27 (0.92–1.62) | 1.36 (1.09–1.70)a | 1.12 (0.92–1.32) | 1.32 (1.29–1.36)a | 1.16 (1.13–1.20)a |
| Other frontline worker | 0.91 (0.68–1.20) | 1.09 (0.87–1.31) | 1.28 (0.97–1.70) | 1.26 (0.99–1.53)a | 1.07 (0.77–1.48) | 1.04 (0.84–1.23) | 0.93 (0.89–0.97)a | 1.00 (0.96–1.03) |
| Other essential worker | 0.94 (0.76–1.16) | 0.92 (0.76–1.09) | 1.06 (0.82–1.37) | 0.99 (0.78–1.21) | 0.99 (0.72–1.36) | 0.85 (0.65–1.04) | 0.96 (0.93–1.00) | 0.98 (0.95–1.01) |
| Persons who are not essential workers (Referent) | – | – | – | – | – | – | – | – |
| Ever had COVID-19 | ||||||||
| Yes | 0.80 (0.68–0.94)a | 0.86 (0.74–0.97)a | 0.65 (0.54–0.80)a | 0.70 (0.57–0.82)a | 0.72 (0.59–0.88)a | 0.79 (0.69–0.89)a | 0.77 (0.75–0.79)a | 0.81 (0.79–0.83)a |
| No (Referent) | – | – | – | – | – | – | – | – |
Abbreviations: PR: Prevalence Ratio; aPR: adjusted Prevalence Ratio; AI/AN/NHOPI = American Indian/Alaska Native/ Native Hawaiian and Other Pacific Islander; MSA = metropolitan statistical area; Ref = referent group; USD = U.S. dollars.
Note: models are adjusted for all the characteristics included in the table.
Significant at p < 0.05.
Respondents who identified as non-Hispanic or Latino origin and identified as “other” or chose multiple categories to describe their race were grouped into “other/multiple races”.
Household income is derived from the number of persons reported in the household, the reported household income, and the 2020 U.S. Census poverty thresholds.
MSA status was determined based on household reported city and county of residence and was grouped into three categories: MSA principal city (urban), MSA nonprincipal city (suburban), and non-MSA (rural). MSAs and principal cities were as defined by the U.S. Census Bureau (https://www.census.gov/programs-surveys/metro-micro.html). Non-MSA areas include urban populations not located within an MSA as well as completely rural areas.
Comorbidity status was ascertained by the following question: “Do you have a health condition that may put you at higher risk for COVID-19?”
Work or school requirement was assessed by the following question: “Does your work or school require you to get a COVID-19 vaccine?” Response options were yes, no, or unemployed/not applicable. Responses for “no” and “not applicable” were combined into one category.
Essential worker status was defined based on the following questions: “Are you a frontline or essential worker according to your state or region?” and “In what location or setting do you currently work?” Essential worker groups were categorized as “essential healthcare,” “school and childcare,” “other frontline,” “other essential,” and “nonessential.” Nonessential could include both employed and unemployed individuals.
When examining attitudes and beliefs regarding COVID-19 and COVID-19 vaccination, among those who were not sure about getting a COVID-19 vaccine, beliefs that COVID-19 vaccines are not at all safe were highest among women who were trying to get pregnant (23.2%) and lowest among women who were breastfeeding (19.0%). Furthermore, among women who were unsure about getting a COVID-19 vaccine, being very concerned about getting COVID-19 was low and ranged from 7.2% among pregnant women to 16.5% among women who were trying to get pregnant. Concerns about getting COVID-19 varied within each intent category for vaccination, with a larger prevalence of being very and moderately concerned among those who reported that they would definitely or probably get a COVID-19 vaccine. Finally, regardless of pregnancy status, the prevalence of knowing that almost all of one’s family and friends were vaccinated against COVID-19 were highest among vaccinated (range: 57.2%-59.5%), followed by those who reported that they would definitely will (range: 30.9%-52.0%) or probably will (range: 15.0%-25.1%) get a COVID-19 vaccine, were unsure (range: 5.1%-17.5%) about getting a COVID-19 vaccine, and would probably not (range: 7.0%-10.3%) or definitely not (range: 5.6%-8.1%) get a COVID-19 (Table 3 , Supplementary Table 2).
Table 3.
COVID-19 illness and vaccination beliefs among women aged 18–49 years vaccinated with ≥1 dose of a COVID-19 vaccine by pregnancy status ─ National Immunization Survey-Adult COVID Module, United States, April 22-November 27, 2021.
| All women aged 18–49 years | Women who were trying to get pregnant at the time of the survey | Women who were pregnant at the time of the survey | Women who were breastfeeding at the time of the survey | All other women aged 18–49 years | |
|---|---|---|---|---|---|
| %a (95 %CI) | %a (95 %CI) | %a (95 %CI) | %a (95 %CI) | %a (95 %CI) | |
| How concerned are you about getting COVID-19? | |||||
| Not at all concerned | 17.3 (16.8–17.8) | 18.4 (15.8–21.3) | 14.3 (11.6–17.5) | 12.5 (10.1–15.3) | 17.5 (17.0–18.0) |
| A little concerned | 31.3 (30.7–31.9) | 29.1 (25.8–32.7) | 32.2 (28.4–36.2) | 28.8 (25.6–32.2) | 31.4 (30.8–32.1) |
| Moderately concerned | 32.0 (31.4–32.6) | 32.9 (29.5–36.5) | 30.9 (27.5–34.5) | 35.3 (31.6–39.1) | 31.9 (31.2–32.5) |
| Very concerned | 19.4 (18.9–20.0) | 19.6 (16.7–23.0) | 22.6 (19.2–26.5) | 23.5 (20.1–27.2) | 19.2 (18.7–19.8) |
| How safe do you think a COVID-19 vaccine is for you? | |||||
| Not at all safe | 1.5 (1.3–1.7) | 2.6 (1.6–4.0) | 0.9 (0.5–1.6) | 1.4 (0.6–3.5) | 1.5 (1.3–1.7) |
| Somewhat safe | 22.8 (22.2–23.3) | 28.0 (24.5–31.9) | 21.1 (17.9–24.6) | 18.9 (15.6–22.7) | 22.8 (22.2–23.4) |
| Very safe | 40.7 (40.1–41.4) | 38.0 (34.5–41.7) | 41.2 (37.2–45.4) | 42.4 (38.6–46.2) | 40.8 (40.1–41.5) |
| Completely safe | 35.0 (34.4–35.6) | 31.4 (27.9–35.1) | 36.8 (32.9–40.9) | 37.3 (33.7–41.1) | 35.0 (34.3–35.7) |
| How important do you think getting a COVID-19 vaccine is to protect yourself against COVID-19? | |||||
| Not at all important | 1.4 (1.2–1.6) | 3.5 (2.3–5.3) | 1.7 (0.9–3.2) | 1.6 (0.7–3.7) | 1.3 (1.2–1.5) |
| A little important | 2.8 (2.6–3.1) | 3.3 (2.2–4.8) | 3.7 (2.5–5.6) | 2.6 (1.5–4.4) | 2.8 (2.6–3.0) |
| Somewhat important | 12.9 (12.5–13.4) | 14.4 (11.9–17.3) | 11.1 (8.7–14.2) | 12.5 (9.7–16.1) | 12.9 (12.5–13.4) |
| Very important | 82.9 (82.3–83.4) | 78.8 (75.5–81.8) | 83.5 (80.1–86.4) | 83.3 (79.5–86.6) | 82.9 (82.4–83.5) |
| If you had to guess, about how many of your family and friends have received a COVID-19 vaccine? | |||||
| None | 0.7 (0.6–0.8) | 0.6 (0.2–1.6) | 0.8 (0.4–2.0) | 0.5 (0.2–1.1) | 0.7 (0.6–0.8) |
| Some | 16.8 (16.3–17.3) | 16.9 (14.4–19.8) | 17.0 (14.2–20.2) | 13.9 (11.4–16.9) | 16.9 (16.4–17.4) |
| Many | 25.2 (24.6–25.8) | 23.0 (20.1–26.2) | 23.7 (20.5–27.2) | 26.3 (23.1–29.8) | 25.3 (24.7–25.9) |
| Almost all | 57.3 (56.7–58.0) | 59.5 (55.8–63.1) | 58.5 (54.5–62.4) | 59.3 (55.4–63.0) | 57.2 (56.5–57.8) |
Percentages reported are weighted percentage.
COVID-19 vaccination coverage with ≥1 dose ranged from 53.3% in HHS Region 4 to 76.5% in HHS Region 1 among women aged 18–49 years. The lowest and highest COVID-19 vaccination coverage was observed among women who resided in U.S. Virgin Islands (39.7%) and Vermont (80.5%), respectively (Table 4 ). We observed similar patterns for the prevalence of provider recommendation by jurisdiction; vaccination coverage was higher in HHS regions where the prevalence of provider recommendation for COVID-19 vaccination was higher and lower in regions where the prevalence of provider recommendation for vaccination was low (Supplementary Table 3).
Table 4.
Receipt of ≥1 dose of a COVID-19 vaccine among women aged 18–49 years by pregnancy status and HHSa regions ─ National Immunization Survey-Adult COVID Module, United States, April 22-November 27, 2021.
| All women 18–49 years |
Women who were trying to get pregnant at the time of the survey |
Women who were pregnant at the time of the survey |
Women who were breastfeeding at the time of the survey |
All other women 18–49 years |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | %b (95 %CI) | N | %b (95 %CI) | N | %b (95 %CI) | N | %b (95 %CI) | N | %b (95 %CI) | |
| National | 110,668 | 63.2 (62.7–63.8) | 3,935 | 49.4 (46.3–52.5) | 3,431 | 45.1 (42.0–48.2) | 3,737 | 51.4 (48.1–54.7) | 99,565 | 64.9 (64.3–65.6) |
| HHS Region 1 | 10,847 | 76.5 (74.9–78.1) | 338 | 51.6 (41.7–61.4) | 303 | 58.1 (48.7–67.0) | 356 | 68.8 (58.4–77.7) | 9,850 | 78.2 (76.5–79.8) |
| Connecticut | 1,380 | 78.1 (74.7–81.1) | 33 | 49.5 (28.3–70.9) | 41 | 49.3 (31.9–66.9) | 51 | 69.1 (50.2–83.2) | 1,255 | 79.9 (76.3–83.0) |
| Maine | 1,694 | 71.1 (68.1–74.0) | 59 | 61.4 (44.1–76.2) | 47 | 55.4 (37.3–72.1) | 62 | 70.7 (54.5–83.0) | 1,526 | 72.0 (68.8–75.0) |
| Massachusetts | 2,474 | 78.2 (75.3–80.9) | 97 | 47.1 (32.5–62.3) | 70 | 66.8 (48.3–81.2) | 87 | 70.6 (51.5–84.5) | 2,220 | 80.0 (76.9–82.7) |
| New Hampshire | 1,858 | 69.0 (65.9–71.9) | 61 | 57.1 (40.2–72.5) | 46 | 56.7 (35.8–75.4) | 55 | 57.3 (39.0–73.9) | 1,696 | 70.2 (66.9–73.2) |
| Rhode Island | 1,689 | 73.7 (70.2–76.9) | 43 | 63.8 (40.5–82.0) | 52 | 46.6 (29.2–64.9) | 51 | 65.8 (45.6–81.5) | 1,543 | 75.4 (71.8–78.7) |
| Vermont | 1,752 | 80.5 (77.7–83.1) | 45 | 70.7 (51.4–84.6) | 47 | 58.0 (39.6–74.5) | 50 | 66.9 (46.9–82.2) | 1,610 | 81.9 (79.0–84.5) |
| HHS Region 2 | 11,005 | 72.6 (70.8–74.3) | 378 | 59.9 (50.7–68.5) | 318 | 49.9 (40.5–59.3) | 352 | 52.6 (42.9–62.1) | 9,957 | 74.8 (73.0–76.5) |
| New Jersey | 2,086 | 75.3 (72.4–77.9) | 86 | 63.3 (47.9–76.3) | 57 | 57.5 (38.0–74.9) | 70 | 62.2 (44.4–77.2) | 1,873 | 76.7 (73.8–79.5) |
| New York | 4,128 | 70.9 (68.4–73.2) | 154 | 57.9 (45.5–69.3) | 147 | 49.1 (37.0–61.2) | 134 | 48.2 (35.7–60.9) | 3,693 | 73.4 (70.7–75.8) |
| NY-City of New York | 2,459 | 72.3 (69.1–75.3) | 90 | 58.1 (40.9–73.5) | 85 | 49.0 (32.8–65.3) | 68 | 45.4 (30.2–61.5) | 2,216 | 74.8 (71.5–77.9) |
| NY-Rest of State | 1,669 | 69.7 (65.9–73.2) | 64 | 57.7 (40.2–73.5) | 62 | 49.2 (32.1–66.4) | 66 | 49.6 (32.9–66.3) | 1,477 | 72.1 (68.1–75.8) |
| HHS Region 3 | 17,792 | 69.1 (67.7–70.6) | 680 | 51.8 (43.9–59.6) | 547 | 55.7 (46.9–64.1) | 566 | 54.9 (46.4–63.2) | 15,999 | 70.8 (69.3–72.3) |
| Delaware | 1,486 | 62.8 (59.4–66.0) | 61 | 37.3 (24.2–52.5) | 48 | 48.9 (32.1–66.1) | 40 | 54.1 (35.8–71.3) | 1,337 | 65.2 (61.6–68.6) |
| District of Columbia | 3,046 | 72.9 (70.4–75.2) | 117 | 64.9 (52.0–75.9) | 96 | 54.5 (41.1–67.2) | 84 | 65.8 (50.6–78.3) | 2,749 | 74.2 (71.7–76.7) |
| Maryland | 3,350 | 75.6 (72.8–78.1) | 146 | 71.6 (54.9–83.9) | 101 | 60.6 (43.7–75.3) | 133 | 63.7 (48.2–76.8) | 2,970 | 76.6 (73.8–79.2) |
| Pennsylvania | 5,164 | 69.0 (66.5–71.4) | 185 | 42.9 (30.9–55.8) | 157 | 50.0 (36.1–64.0) | 158 | 54.3 (39.3–68.5) | 4,664 | 70.8 (68.3–73.3) |
| PA-Philadelphia | 2,183 | 70.2 (67.6–72.7) | 90 | 57.2 (43.7–69.7) | 68 | 46.8 (33.0–61.2) | 68 | 54.2 (39.3–68.3) | 1,957 | 72.4 (69.7–74.9) |
| PA-Rest of State | 2,981 | 68.8 (65.9–71.5) | 95 | 39.3 (25.5–55.0) | 89 | 50.9 (33.7–67.8) | 90 | 54.3 (36.0–71.5) | 2,707 | 70.6 (67.6–73.4) |
| Virginia | 2,849 | 69.3 (65.9–72.5) | 107 | 47.7 (30.4–65.6) | 100 | 63.6 (44.8–78.9) | 108 | 51.9 (34.8–68.6) | 2,534 | 71.1 (67.5–74.5) |
| West Virginia | 1,897 | 44.7 (41.9–47.6) | 64 | 32.6 (20.2–48.1) | 45 | 29.2 (16.5–46.2) | 43 | 26.0 (14.5–42.1) | 1,745 | 46.3 (43.3–49.3) |
| HHS Region 4 | 14,405 | 53.3 (51.9–54.8) | 494 | 46.6 (38.9–54.5) | 406 | 36.6 (29.3–44.5) | 405 | 40.2 (31.8–49.2) | 13,100 | 54.7 (53.1–56.2) |
| Alabama | 1,802 | 46.4 (43.5–49.4) | 65 | 40.6 (27.2–55.4) | 51 | 22.4 (11.7–38.6) | – | .c | 1,660 | 47.9 (44.8–51.1) |
| Florida | 2,140 | 58.0 (54.5–61.4) | 79 | 48.5 (31.0–66.5) | 65 | 53.4 (34.6–71.3) | 72 | 49.6 (33.1–66.2) | 1,924 | 59.0 (55.3–62.6) |
| Georgia | 2,035 | 51.0 (47.7–54.3) | 82 | 47.2 (32.8–62.1) | 66 | 36.3 (23.2–51.9) | 53 | 32.0 (17.5–51.0) | 1,834 | 52.2 (48.7–55.8) |
| Kentucky | 1,940 | 56.5 (53.6–59.3) | 51 | 31.7 (19.8–46.7) | 48 | 52.8 (35.9–69.2) | 42 | 40.4 (24.5–58.6) | 1,799 | 57.7 (54.7–60.6) |
| Mississippi | 1,778 | 41.1 (38.3–44.1) | 55 | 30.3 (18.4–45.5) | 47 | 24.9 (14.4–39.5) | 47 | 29.6 (16.9–46.3) | 1,629 | 42.3 (39.3–45.4) |
| North Carolina | 1,568 | 57.9 (53.8–62.0) | 57 | 54.9 (35.2–73.1) | 48 | 30.7 (16.8–49.2) | 67 | 41.1 (21.9–63.4) | 1,396 | 60.0 (55.6–64.2) |
| South Carolina | 1,746 | 47.6 (44.6–50.6) | 54 | 34.1 (21.7–49.0) | 50 | 30.7 (18.8–45.9) | 45 | 25.6 (15.0–40.2) | 1,597 | 49.4 (46.2–52.6) |
| Tennessee | 1,396 | 49.7 (45.7–53.8) | 51 | 51.6 (33.9–68.9) | 31 | 14.9 (6.0–32.4) | 53 | 29.4 (16.8–46.3) | 1,261 | 51.4 (47.1–55.7) |
| HHS Region 5 | 11,277 | 58.3 (56.6–60.0) | 401 | 41.6 (34.0–49.7) | 380 | 34.3 (28.0–41.2) | 387 | 52.2 (44.1–60.2) | 10,109 | 60.2 (58.4–62.0) |
| Illinois | 3,715 | 68.3 (65.9–70.7) | 130 | 57.4 (45.8–68.3) | 143 | 56.3 (44.9–67.0) | 112 | 46.4 (33.7–59.7) | 3,330 | 69.9 (67.4–72.4) |
| IL-City of Chicago | 1,352 | 68.6 (63.9–72.8) | 44 | 49.5 (29.2–70.0) | 55 | 47.4 (30.1–65.3) | 40 | 47.7 (24.2–72.4) | 1,213 | 71.1 (66.2–75.5) |
| IL-Rest of State | 2,363 | 68.3 (65.4–71.0) | 86 | 60.0 (46.4–72.2) | 88 | 60.7 (46.8–73.1) | 72 | 46.0 (31.4–61.4) | 2,117 | 69.6 (66.6–72.5) |
| Indiana | 1,407 | 48.0 (44.5–51.6) | 43 | 22.9 (12.8–37.6) | 39 | 21.8 (11.6–37.2) | 38 | 46.7 (26.2–68.5) | 1,287 | 50.2 (46.5–54.0) |
| Michigan | 1,451 | 54.8 (50.3–59.2) | 48 | 26.3 (13.6–44.6) | 40 | 35.1 (18.3–56.6) | 52 | 60.8 (40.6–77.8) | 1,311 | 56.8 (52.0–61.5) |
| Minnesota | 1,759 | 65.1 (61.6–68.5) | 64 | 49.5 (33.4–65.6) | 55 | 38.2 (23.2–55.8) | 77 | 43.9 (29.9–59.0) | 1,563 | 67.8 (64.1–71.4) |
| Ohio | 1,308 | 53.0 (48.2–57.7) | 59 | 47.2 (29.5–65.6) | 50 | 15.0 (7.8–26.9) | 50 | 58.7 (34.7–79.2) | 1,149 | 54.8 (49.5–59.9) |
| Wisconsin | 1,637 | 59.1 (55.8–62.3) | 57 | 49.6 (34.4–64.9) | 53 | 41.6 (27.0–57.9) | 58 | 55.9 (38.3–72.1) | 1,469 | 60.2 (56.7–63.6) |
| HHS Region 6 | 15,030 | 59.6 (58.2–61.0) | 550 | 43.2 (36.8–49.9) | 493 | 43.7 (37.1–50.5) | 443 | 45.0 (37.3–52.9) | 13,544 | 61.4 (60.0–62.9) |
| Arkansas | 1,738 | 50.2 (47.0–53.4) | 62 | 37.3 (24.8–51.8) | 67 | 38.5 (26.1–52.6) | 55 | 38.7 (24.1–55.6) | 1,554 | 51.7 (48.2–55.1) |
| Louisiana | 2,029 | 45.3 (42.6–48.1) | 85 | 35.1 (24.2–47.7) | 73 | 17.9 (11.3–27.2) | 54 | 31.4 (19.0–47.1) | 1,817 | 47.9 (45.0–50.9) |
| New Mexico | 1,697 | 72.2 (69.3–74.8) | 54 | 63.9 (47.5–77.6) | 55 | 48.6 (33.4–64.0) | 58 | 50.8 (36.0–65.4) | 1,530 | 74.2 (71.2–77.0) |
| Oklahoma | 1,717 | 53.4 (50.3–56.4) | 64 | 35.3 (23.7–49.0) | 53 | 37.5 (24.0–53.4) | 52 | 58.8 (40.4–75.0) | 1,548 | 54.7 (51.5–57.9) |
| Texas | 7,849 | 62.8 (60.9–64.7) | 285 | 45.4 (36.4–54.8) | 245 | 51.2 (41.2–61.2) | 224 | 45.4 (34.8–56.4) | 7,095 | 64.5 (62.4–66.5) |
| TX-Bexar County | 1,966 | 61.6 (58.6–64.4) | 62 | 43.3 (28.4–59.4) | 63 | 49.2 (34.7–63.8) | 50 | 51.3 (35.1–67.3) | 1,791 | 63.2 (60.1–66.2) |
| TX-City of Houston | 1,680 | 61.6 (58.4–64.7) | 62 | 50.9 (35.9–65.8) | 58 | 50.0 (34.5–65.5) | 54 | 36.9 (23.7–52.2) | 1,506 | 63.6 (60.2–66.9) |
| TX-Rest of State | 4,203 | 63.0 (60.8–65.2) | 161 | 45.1 (34.6–56.0) | 124 | 51.6 (39.6–63.5) | 120 | 45.8 (33.2–59.0) | 3,798 | 64.7 (62.3–66.9) |
| HHS Region 7 | 5,099 | 55.7 (53.3–58.0) | 172 | 36.3 (26.1–47.9) | 184 | 37.2 (27.1–48.5) | 201 | 52.2 (40.5–63.6) | 4,542 | 57.6 (55.0–60.1) |
| Iowa | 1,183 | 56.8 (51.6–61.8) | -c | 40 | 28.5 (11.6–54.7) | 53 | 49.9 (28.4–71.4) | 1,061 | 59.2 (53.9–64.3) | |
| Kansas | 1,393 | 60.0 (56.5–63.3) | 43 | 28.7 (17.0–44.2) | 48 | 35.2 (22.6–50.4) | 65 | 54.6 (39.5–69.0) | 1,237 | 62.6 (59.0–66.2) |
| Missouri | 1,400 | 51.5 (47.4–55.7) | 50 | 31.2 (16.9–50.3) | 58 | 42.6 (26.0–61.0) | 44 | 53.6 (30.1–75.6) | 1,248 | 53.0 (48.5–57.5) |
| Nebraska | 1,123 | 60.9 (56.8–64.9) | 50 | 62.5 (43.2–78.5) | 38 | 42.7 (26.7–60.5) | 39 | 48.9 (29.1–69.0) | 996 | 62.3 (57.9–66.4) |
| HHS Region 8 | 7,775 | 64.3 (61.9–66.6) | 251 | 55.8 (43.2–67.7) | 259 | 51.0 (38.6–63.2) | 309 | 48.8 (37.2–60.6) | 6,956 | 65.9 (63.4–68.3) |
| Colorado | 1,589 | 68.9 (65.0–72.6) | 49 | 64.0 (40.8–82.1) | 50 | 55.8 (34.3–75.3) | 64 | 66.5 (43.1–83.8) | 1,426 | 69.7 (65.5–73.5) |
| Montana | 1,662 | 53.4 (50.5–56.4) | 46 | 31.7 (19.4–47.1) | 42 | 33.9 (20.7–50.1) | 58 | 45.5 (31.6–60.1) | 1,516 | 55.1 (51.9–58.2) |
| North Dakota | 1,311 | 49.3 (45.7–53.0) | 52 | 28.6 (17.0–44.1) | 39 | 30.4 (16.4–49.2) | 36 | 46.2 (27.0–66.6) | 1,184 | 51.3 (47.5–55.2) |
| South Dakota | 1,283 | 58.6 (55.0–62.1) | 33 | 49.3 (30.4–68.4) | 55 | 51.7 (34.8–68.2) | 61 | 58.1 (41.5–73.1) | 1,134 | 59.2 (55.3–63.0) |
| Utah | 836 | 67.1 (61.5–72.2) | 34 | 62.0 (35.2–83.0) | 42 | 52.5 (29.2–74.8) | 47 | 33.1 (17.2–54.0) | 713 | 70.4 (64.4–75.8) |
| Wyoming | 1,094 | 44.7 (40.7–48.8) | 37 | 31.9 (17.3–51.2) | 31 | 41.4 (22.5–63.2) | 43 | 27.1 (14.4–45.2) | 983 | 46.3 (42.0–50.6) |
| HHS Region 9 | 10,700 | 71.3 (69.5–73.0) | 438 | 61.3 (51.3–70.5) | 317 | 56.4 (45.5–66.7) | 406 | 61.6 (50.8–71.4) | 9,539 | 72.6 (70.7–74.4) |
| Arizona | 1,673 | 56.8 (53.7–59.9) | 60 | 46.8 (32.9–61.3) | 45 | 39.2 (24.6–56.1) | 49 | 61.6 (42.1–77.9) | 1,519 | 57.7 (54.5–60.9) |
| California | 4,382 | 74.5 (72.2–76.6) | 166 | 64.7 (51.6–76.0) | 134 | 60.6 (46.9–72.9) | 165 | 63.0 (49.4–74.8) | 3,917 | 75.8 (73.4–78.0) |
| Hawaii | 1,861 | 76.4 (73.8–78.9) | 82 | 59.8 (46.2–72.0) | 45 | 47.9 (31.4–64.9) | 78 | 59.0 (45.0–71.6) | 1,656 | 78.6 (75.9–81.1) |
| Nevada | 1,607 | 59.8 (56.5–62.9) | 54 | 54.0 (37.2–69.9) | 45 | 39.0 (24.4–55.9) | 45 | 47.1 (29.8–65.1) | 1,463 | 61.1 (57.7–64.4) |
| HHS Region 10 | 6,738 | 67.2 (64.7–69.6) | 233 | 46.5 (33.2–60.3) | 224 | 48.5 (34.7–62.6) | 312 | 57.6 (46.6–67.9) | 5,969 | 69.2 (66.7–71.7) |
| Alaska | 1,490 | 56.6 (53.0–60.1) | 63 | 42.1 (28.6–56.9) | 63 | 28.5 (17.7–42.7) | 96 | 54.0 (38.9–68.4) | 1,268 | 59.2 (55.3–63.0) |
| Idaho | 1,383 | 47.3 (44.1–50.4) | 47 | 35.2 (22.2–50.9) | 38 | 38.8 (23.1–57.2) | 48 | 31.7 (20.0–46.3) | 1,250 | 48.6 (45.2–52.0) |
| Oregon | 2,184 | 70.4 (67.6–73.0) | 58 | 56.4 (39.6–71.8) | 66 | 48.2 (33.9–62.8) | 80 | 53.8 (39.4–67.6) | 1,980 | 72.6 (69.7–75.3) |
| Washington | 1,681 | 70.7 (66.4–74.6) | 65 | 45.5 (25.4–67.3) | 57 | 53.5 (27.5–77.7) | 88 | 63.6 (45.3–78.7) | 1,471 | 72.7 (68.2–76.7) |
| Territories | ||||||||||
| Puerto Rico | 3,452 | 77.1 (74.6–79.3) | 76 | 68.8 (52.5–81.4) | 78 | 41.7 (28.7–56.0) | 101 | 62.4 (46.2–76.2) | 3,197 | 79.2 (76.7–81.5) |
| U.S. Virgin Islands | 1,339 | 39.7 (36.1–43.3) | 62 | 31.7 (19.1–47.6) | 36 | 16.5 (8.1–30.7) | 47 | 26.4 (14.3–43.4) | 1,194 | 41.6 (37.7–45.6) |
HHS regions were defined according to: https://www.hhs.gov/about/agencies/iea/regional-offices/index.html.
Percentages reported are weighted percentage.
Estimates do not meet the National Center for Health Statistic’s standards of reliability. https://www.cdc.gov/nchs/data/series/sr_02/sr02_175.pdf.
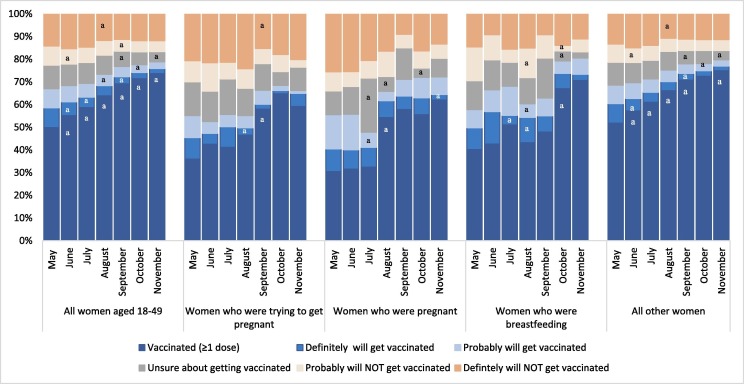
When examining trends in COVID-19 vaccination and intent, we observed significant increases in COVID-19 vaccination with ≥1 dose from May (49.9%) to November (73.6%) among all women aged 18–49 years. Among women trying to get pregnant at the time of the survey, vaccination coverage increased significantly from August (46.6%) to September (58.0%). Among women who were pregnant at the time of the survey, vaccination coverage increased significantly from July (32.5%) to August (54.2%) (Fig. 1 ). Additionally, vaccination coverage was significantly higher among pregnant women during August-November (57.2%; 95% CI: 52.7–61.7%) than during May-July (31.4%; 95% CI: 27.6–35.5%) (Data not shown).
Fig. 1.
COVID-19 vaccination (receipt of ≥1 dose) and vaccination intent among women aged 18–49 years by pregnancy status — National Immunization Survey-Adult COVID Module, United States, April 22–November 27, 2021.
aSignificant (p < 0.05) changes in percentage points from previous month.
4. Discussion
According to data from the CDC COVID Data Tracker, as of February 1, 2022, national coverage with ≥1 dose of COVID-19 vaccine ranges from 79.1% for women aged 18–24 years to 85.9% for women aged 40–49 years [21]. Findings from this study using survey data from NIS-ACM indicated that as of mid-November 2021, national coverage with ≥1 dose of COVID-19 vaccine was 73.6% among women aged 18–49 years. The lowest vaccination coverage was observed among pregnant women and women trying to get pregnant which may be explained, in part, by limited information on vaccine safety among pregnant women, many studies have not been published on the safety of COVID-19 vaccines in pregnant women, particularly vaccination with mRNA vaccines [22], [23], [24]. To date, vaccine safety surveillance systems, including VAER, v-safe, and vaccine safety data link, have not detected any safety signals for people who received COVID-19 vaccines before or during pregnancy, which may explain the increase in vaccination coverage over time [25], [26], [27], [28]. Additionally, several studies have found that COVID-19 vaccination in pregnancy significantly lowers the risk of infection from SARS-CoV-2 and serious illness from COVID-19 in pregnant women. Data indicate that there is passage of maternal antibodies against COVID-19 through the placenta to the developing baby [29], [30], [31], [32], [33].
Furthermore, the observed increase in vaccination coverage among pregnant women in August 2021 is likely due to the strengthening of recommendations for vaccination of pregnant women by CDC on August 11th along with other clinical organizations [20], [34], [35]. In response to a national trend of increased deaths and ICU admission among pregnant women in August and September, CDC issued a Health Advisory in September 2021 as a call to action to increase COVID-19 vaccination among people who are pregnant, who were recently pregnant (including those who are lactating), who are trying to become pregnant now, or who might become pregnant in the future. In September 2021, data from the COVID-19-Associated Hospitalization Surveillance Network (COVID-NET) indicated that in 2021, approximately 97% of pregnant people hospitalized with confirmed SARS-CoV-2 infection were unvaccinated [36]. COVID-19 vaccines received during pregnancy are safe and effective, and the best way to prevent severe illness and adverse outcomes is to get vaccinated. CDC strongly recommends COVID-19 vaccination either before or during pregnancy because the benefits of vaccination outweigh potential risks [20].
Consistent with prior reports, sociodemographic disparities in vaccination coverage were observed [12], [14], [37], [38]. Vaccination coverage was lowest among non-Hispanic Black women of reproductive age overall. Only 1 in 3 Black pregnant women had received ≥1 dose of a COVID-19 vaccine, and approximately 1 in 3 reported that they would probably/definitely NOT get a COVID-19 vaccine. Previous studies reported that several factors, including knowledge, attitudes, and beliefs about vaccines, mistrust resulting from past medical racism and experimentation, and barriers related to accessing vaccines and healthcare services contribute to lower vaccination rates in Black adults [39], [40], [41]. Household income below poverty, not having received other vaccines in the previous two years or a recommendation for COVID-19 vaccination from a healthcare provider, and not having any comorbidities were more commonly observed among unvaccinated women of reproductive age who were not sure about receiving a COVID-19 vaccine. These characteristics suggest that these women, particularly those who are not pregnant, may not have routine access to health care. Community-based approaches and leveraging trusted influencers such as faith leaders or vaccine workers that are of the same race and ethnicity in their communities might have more impact on improving vaccination for this population [42]. Continuing to monitor vaccination and intent for vaccination by race and ethnicity and socio-demographics is important to ensure equitable access to COVID-19 vaccines for all women of reproductive age, especially pregnant women and those of NH Black and other race and ethnicity groups (including American Indian/Alaska Native/ Native Hawaiian and Other Pacific Islander) who have experienced disproportionately higher rates of hospitalization and death attributable to COVID-19 than White persons [4], [7], [8], [41], [43].
Overall less than half of women of reproductive age in this study received a provider recommendation for vaccination, with approximately 48% of pregnant women and 40% of those who were trying to get pregnant. Provider recommendation varied greatly by state and HHS regions of residence. The reasons for such low provider recommendations are not clear; we could not assess whether a provider recently saw the individuals. Given that our study, along with many previous studies, has found that provider recommendation is one of the strongest factors associated with vaccination [12], [13], [14], healthcare providers play a vital role in communicating the risks of COVID-19, the benefits of vaccination, and information on the safety and effectiveness of COVID-19 vaccination. By strongly recommending that people who are pregnant, who were recently pregnant (including those who are lactating), who are trying to become pregnant now, or who might become pregnant in the future receive all recommended COVID-19 vaccines doses through a variety of resources including healthcare providers, pharmacists, and allied health professionals can help increase vaccination rates and protect women and their infants from the severe effects from COVID-19. Finally, while these data highlight the importance of provider recommendation in COVID-19 vaccination uptake, additional strategies should be leveraged to make vaccination a standard of care; for example, improving reimbursement to providers who practice motivational interviewing may help overcome barriers to administration of vaccines or health systems could consider offering vaccination at all medical encounters including ensuring COVID-19 vaccine is readily available for administration at all clinic visits, emergency departments, obstetrical triage units and at discharge following delivery [44], [45], [46], [47], [48], [49].
The findings in this study are subject to at least five limitations. First, response rates were low (approximately 20%) but consistent with other NIS surveys [16]. Bias in estimates might remain after weighting for household nonresponse and the incomplete sample frame (households with only landline or no telephone service were excluded). Second, receipt of vaccination, pregnancy status, and other characteristics were self-reported and subject to recall and misclassification bias. Survey weights were further calibrated to COVID-19 vaccine administration data1 to mitigate possible bias from incomplete sample frame, nonresponse, and misclassification of vaccination status. Third, the timing of vaccination was not asked in the survey; therefore, we could not assess whether COVID-19 vaccinations occurred before or during pregnancy or the breastfeeding period. Fourth, attitudes might have changed over time with changes in the Advisory Committee on Immunization Practices vaccination recommendations or the emergence of the highly transmissible SARS-CoV-2B.1.617.2 (Delta) and B.1.1.529 (Omicron) variants [50]. Finally, the survey is cross-sectional; thus, causal relationships cannot be inferred.
Given that COVID-19 vaccination is low among women of reproductive age, especially pregnant women, dissemination of information on the safety and effectiveness of vaccines to pregnant women, those who are breastfeeding, and trying to become pregnant is critical. Additionally, messaging that is strong, clear, concise, consistent that is delivered by a trusted source is essential. As observed in this study, vaccination rates in pregnancy increased by more than 20 percentage points from July 2021 to August 2021 when CDC strengthened its recommendations for pregnant people to get vaccinated. This study demonstrates that the availability of safety data and strong recommendations from both trusted organizations and healthcare providers results in higher vaccination coverage in this population. Continued focus to improve vaccination in this population as well as populations with lower vaccination coverage such as those with lower household income, without insurance, and of Black or Hispanic race and ethnicity is critical, including ensuring the availability of vaccination in all medical encounters.
Funding Source
This study was funded by the Center for Disease Control and Prevention.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.06.029.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Centers for Disease Control and Prevention. COVID data tracker. https://covid.cdc.gov/covid-data-tracker/#datatracker-home. [accessed June 24, 2021].
- 2.Centers for Disease Control and Prevention. Use of COVID-19 vaccines in the United States. https://www.cdc.gov/vaccines/covid-19/info-by-product/clinical-considerations.html. [accessed June 24, 2021].
- 3.Centers for Disease Control and Prevention. COVID-19 vaccines while pregnant or breastfeeding. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/pregnancy.html. [accessed August 12, 2021].
- 4.Allotey J., Stallings E., Bonet M., et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370 doi: 10.1136/bmj.m3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. People with certain medical conditions. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. [accessed June 24, 2021].
- 6.Kasehagen L., Byers P., Taylor K., et al. COVID-19-associated deaths after SARS-CoV-2 Infection During Pregnancy - Mississippi, March 1, 2020-October 6, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(47):1646–1648. doi: 10.15585/mmwr.mm7047e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zambrano L.D., Ellington S., Strid P., Galang R.R., Oduyebo T., Tong V.T., et al. Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status - United States, January 22-October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(44):1641–1647. doi: 10.15585/mmwr.mm6944e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McClymont E., Fell D.B., Albert A., Alton G.D., Barrett J., El-Chaar D., et al. Canadian surveillance of COVID-19 in pregnancy: Epidemiology and maternal and infant outcomes. Am J Obstet Gynecol. 2020;223(6):969–970. doi: 10.1016/j.ajog.2020.08.137. [DOI] [Google Scholar]
- 9.Wei S.Q., Bilodeau-Bertrand M., Liu S., Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. Can Med Assoc J. 2021;193(16):E540–E548. doi: 10.1503/cmaj.202604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Woodworth K.R., Olsen E.O., Neelam V., Lewis E.L., Galang R.R., Oduyebo T., et al. Birth and Infant Outcomes Following Laboratory-Confirmed SARS-CoV-2 Infection in Pregnancy - SET-NET, 16 Jurisdictions, March 29-October 14, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(44):1635–1640. doi: 10.15585/mmwr.mm6944e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. COVID-19 vaccinations in the United States. https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-people-onedose-pop-5yr. [accessed December 9, 2021].
- 12.Razzaghi H., Kahn K.E., Black C.L., Lindley M.C., Jatlaoui T.C., Fiebelkorn A.P., et al. Influenza and Tdap Vaccination Coverage Among Pregnant Women - United States, April 2020. MMWR Morb Mortal Wkly Rep. 2020;69(39):1391–1397. doi: 10.15585/mmwr.mm6939a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nguyen K.H., Yankey D., Lu P.-J., Kriss J.L., Brewer N.T., Razzaghi H., et al. Report of Health Care Provider Recommendation for COVID-19 Vaccination Among Adults, by Recipient COVID-19 Vaccination Status and Attitudes - United States, April-September 2021. MMWR Morb Mortal Wkly Rep. 2021;70(50):1723–1730. doi: 10.15585/mmwr.mm7050a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kahn KE, Razzaghi H, Jatlaoui TC, et al. Flu and Tdap Vaccination Coverage Among Pregnant Women – United States, April 2021; 2021. https://www.cdc.gov/flu/fluvaxview/pregnant-women-apr2021.htm. [DOI] [PMC free article] [PubMed]
- 15.NORC. National Immunization Survey-Child: A user's guide for the 2019 public-use data file; 2020. https://www.cdc.gov/vaccines/imz-managers/nis/downloads/NIS-PUF19-DUG.pdf.
- 16.American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys; 2016. https://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169theditionfinal.pdf.
- 17.Brewer N.T. What Works to Increase Vaccination Uptake. Acad Pediatr. 2021;21(4s):S9–s16. doi: 10.1016/j.acap.2021.01.017. [DOI] [PubMed] [Google Scholar]
- 18.NORC. NIS adult COVID module (NIS-ACM); 2021. https://www.cdc.gov/vaccines/imz-managers/nis/downloads/NIS-ACM-Questionnaire-Q2-2021_508.pdf.
- 19.U.S. Department of Health & Human Services. HHS Regional Offices. https://www.hhs.gov/about/agencies/iea/regional-offices/index.html. [accessed December 10, 2021].
- 20.Centers for Disease Control and Prevention. New CDC data: COVID-19 vaccination safe for pregnant people. https://www.cdc.gov/media/releases/2021/s0811-vaccine-safe-pregnant.html. [accessed January 13, 2022].
- 21.Centers for Disease Control and Prevention. Demographic trends of people receiving COVID-19 vaccinations in the Unites States. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographics-trends. [accessed February 2, 2022].
- 22.Goncu Ayhan S., Oluklu D., Atalay A., Menekse Beser D., Tanacan A., Moraloglu Tekin O., et al. COVID-19 vaccine acceptance in pregnant women. Int J Gynaecol Obstet. 2021;154(2):291–296. doi: 10.1002/ijgo.13713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Skjefte M., Ngirbabul M., Akeju O., Escudero D., Hernandez-Diaz S., Wyszynski D.F., et al. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol. 2021;36(2):197–211. doi: 10.1007/s10654-021-00728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Battarbee A.N., Stockwell M.S., Varner M., et al. Attitudes toward COVID-19 illness and COVID-19 vaccination among pregnant women: a cross-sectional multicenter study during August-December 2020. Am J Perinatol. 2022;39(1):75–83. doi: 10.1101/2021.03.26.21254402. [DOI] [PubMed] [Google Scholar]
- 25.Shimabukuro T.T., Kim S.Y., Myers T.R., Moro P.L., Oduyebo T., Panagiotakopoulos L., et al. Preliminary Findings of mRNA Covid-19 Vaccine Safety in Pregnant Persons. N Engl J Med. 2021;384(24):2273–2282. doi: 10.1056/NEJMoa2104983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kharbanda E.O., Haapala J., DeSilva M., Vazquez-Benitez G., Vesco K.K., Naleway A.L., et al. Spontaneous Abortion Following COVID-19 Vaccination During Pregnancy. JAMA. 2021;326(16):1629. doi: 10.1001/jama.2021.15494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lipkind H.S., Vazquez-Benitez G., DeSilva M., Vesco K.K., Ackerman-Banks C., Zhu J., et al. Receipt of COVID-19 Vaccine During Pregnancy and Preterm or Small-for-Gestational-Age at Birth - Eight Integrated Health Care Organizations, United States, December 15, 2020-July 22, 2021. MMWR Morb Mortal Wkly Rep. 2022;71(1):26–30. doi: 10.15585/mmwr.mm7101e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zauche L.H., Wallace B., Smoots A.N., Olson C.K., Oduyebo T., Kim S.Y., et al. Receipt of mRNA Covid-19 Vaccines and Risk of Spontaneous Abortion. N Engl J Med. 2021;385(16):1533–1535. doi: 10.1056/NEJMc2113891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldshtein I., Nevo D., Steinberg D.M., Rotem R.S., Gorfine M., Chodick G., et al. Association Between BNT162b2 Vaccination and Incidence of SARS-CoV-2 Infection in Pregnant Women. JAMA. 2021;326(8):728. doi: 10.1001/jama.2021.11035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dagan N., Barda N., Biron-Shental T., Makov-Assif M., Key C., Kohane I.S., et al. Effectiveness of the BNT162b2 mRNA COVID-19 vaccine in pregnancy. Nat Med. 2021;27(10):1693–1695. doi: 10.1038/s41591-021-01490-8. [DOI] [PubMed] [Google Scholar]
- 31.Morgan J.A., Biggio J.R., Martin J.K., Mussarat N., Chawla H.K., Puri P., et al. Maternal Outcomes After Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection in Vaccinated Compared With Unvaccinated Pregnant Patients. Obstet Gynecol. 2022;139(1):107–109. doi: 10.1097/AOG.0000000000004621. [DOI] [PubMed] [Google Scholar]
- 32.Theiler R.N., Wick M., Mehta R., Weaver A.L., Virk A., Swift M. Pregnancy and birth outcomes after SARS-CoV-2 vaccination in pregnancy. Am J Obstet Gynecol MFM. 2021;3(6) doi: 10.1016/j.ajogmf.2021.100467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gray K.J., Bordt E.A., Atyeo C., et al. Coronavirus disease 2019 vaccine response in pregnant and lactating women: a cohort study. Am J Obstet Gynecol. 2021;225(3):303.e1–303.e17. doi: 10.1016/j.ajog.2021.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Society for Maternal Fetal Medicine. COVID-19 vaccination if you are pregnant or breastfeeding. https://s3.amazonaws.com/cdn.smfm.org/media/3040/COVID_vaccine__Patients_JULY_29_2021_final.pdf. [accessed August 12, 2021].
- 35.The American College of Obstetricians and Gynecologists. COVID-19 vaccination consideration for obstetric-gynecologic care. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/covid-19-vaccination-considerations-for-obstetric-gynecologic-care. [accessed August 12, 2021].
- 36.Centers for Disease Control and Prevention. COVID-19 vaccination for pregnant people to prevent serious illness, deaths, and adverse pregnancy outcomes from COVID-19. https://emergency.cdc.gov/han/2021/han00453.asp. [accessed September 30, 2021].
- 37.Razzaghi H., Meghani M., Pingali C., Crane B., Naleway A., Weintraub E., et al. COVID-19 Vaccination Coverage Among Pregnant Women During Pregnancy - Eight Integrated Health Care Organizations, United States, December 14, 2020-May 8, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(24):895–899. doi: 10.15585/mmwr.mm7024e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. COVID-19 vaccination among pregnant people aged 18-49 years overall, by race/ethnicity, and date reported to CDC - Vaccine Safety Datalink, United States. https://covid.cdc.gov/covid-data-tracker/#vaccinations-pregnant-women. [accessed December 8, 2021].
- 39.Brewer L.I., Ommerborn M.J., Nguyen A.L., Clark C.R. Structural inequities in seasonal influenza vaccination rates. BMC Public Health. 2021;21(1):1166. doi: 10.1186/s12889-021-11179-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lu P.-J., O'Halloran A., Bryan L., Kennedy E.D., Ding H., Graitcer S.B., et al. Trends in racial/ethnic disparities in influenza vaccination coverage among adults during the 2007–08 through 2011–12 seasons. Am J Infect Control. 2014;42(7):763–769. doi: 10.1016/j.ajic.2014.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Uscher-Pines L., Maurer J., Harris K.M. Racial and ethnic disparities in uptake and location of vaccination for 2009–H1N1 and seasonal influenza. Am J Public Health. 2011;101(7):1252–1255. doi: 10.2105/AJPH.2011.300133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. A guide for community partners. https://www.cdc.gov/vaccines/covid-19/downloads/guide-community-partners.pdf. [accessed May 3, 2022].
- 43.Smith A.R., DeVies J., Caruso E., Radhakrishnan L., Sheppard M., Stein Z., et al. Emergency Department Visits for COVID-19 by Race and Ethnicity - 13 States, October-December 2020. MMWR Morb Mortal Wkly Rep. 2021;70(15):566–569. doi: 10.15585/mmwr.mm7015e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gabarda A., Butterworth S.W. Using Best Practices to Address COVID-19 Vaccine Hesitancy: The Case for the Motivational Interviewing Approach. Health Promot Pract. 2021;22(5):611–615. doi: 10.1177/15248399211016463. [DOI] [PubMed] [Google Scholar]
- 45.Magill M., Apodaca T.R., Borsari B., Gaume J., Hoadley A., Gordon R.E.F., et al. A meta-analysis of motivational interviewing process: Technical, relational, and conditional process models of change. J Consult Clin Psychol. 2018;86(2):140–157. doi: 10.1037/ccp0000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Opel D.J., Mangione-Smith R., Robinson J.D., Heritage J., DeVere V., Salas H.S., et al. The Influence of Provider Communication Behaviors on Parental Vaccine Acceptance and Visit Experience. Am J Public Health. 2015;105(10):1998–2004. doi: 10.2105/AJPH.2014.302425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gagneur A. Motivational interviewing: A powerful tool to address vaccine hesitancy. Can Commun Dis Rep. 2020;46(4):93–97. doi: 10.14745/ccdr.v46i04a06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Opel D.J., Robinson J.D., Spielvogle H., Spina C., Garrett K., Dempsey A.F., et al. 'Presumptively Initiating Vaccines and Optimizing Talk with Motivational Interviewing' (PIVOT with MI) trial: a protocol for a cluster randomised controlled trial of a clinician vaccine communication intervention. BMJ Open. 2020;10(8):e039299. doi: 10.1136/bmjopen-2020-039299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Committee N.V.A. Assessing the State of Vaccine Confidence in the United States: Recommendations from the National Vaccine Advisory Committee: Approved by the National Vaccine Advisory Committee on June 9, 2015 [corrected] Publ Health Rep. 2015;130(6):573–595. doi: 10.1177/003335491513000606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Centers for Disease Control and Prevention. SARS-CoV-2 Variant classifications and definitions. https://www.cdc.gov/coronavirus/2019-ncov/variants/variant-classifications.html. [accessed December 15, 2021].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.