Abstract
Background
Thoracic trauma (TT) is common among people with multiple traumatic injuries. One of the injuries caused by TT is the loss of thoracic stability resulting from multiple fractures of the rib cage, otherwise known as flail chest (FC). A person with FC can be treated conservatively with orotracheal intubation and mechanical ventilation (internal pneumatic stabilization) but may also undergo surgery to fix the costal fractures.
Objectives
To evaluate the effectiveness and safety of surgical stabilization compared with clinical management for people with FC.
Search methods
We ran the search on the 12 May 2014. We searched the Cochrane Injuries Group's Specialised Register, the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library), MEDLINE (OvidSP), EMBASE Classic and EMBASE (OvidSP), CINAHL Plus (EBSCO), ISI WOS (SCI‐EXPANDED, SSCI, CPCI‐S, and CPSI‐SSH), and clinical trials registers. We also screened reference lists and contacted experts.
Selection criteria
Randomized controlled trials of surgical versus nonsurgical treatment for people diagnosed with FC.
Data collection and analysis
Two review authors selected relevant trials, assessed their risk of bias, and extracted data.
Main results
We included three studies that involved 123 people. The methods used for blinding the participants and researchers to the treatment group were not reported, but as the comparison is surgical treatment with medical treatment this bias is hard to avoid. There was no description of concealment of the randomization sequence in two studies.
All three studies reported on mortality, and deaths occurred in two studies. There was no clear evidence of a difference in mortality between treatment groups (risk ratio (RR) 0.56, 95% confidence interval (CI) 0.13 to 2.42); however, the analysis was underpowered to detect a difference between groups. Out of the 123 people randomized and treated, six people died; the causes of death were pneumonia, pulmonary embolism, mediastinitis, and septic shock.
Among people randomized to surgery, there were reductions in pneumonia (RR 0.36, 95% 0.15 to 0.85; three studies, 123 participants), chest deformity (RR 0.13, 95% CI 0.03 to 0.67; two studies, 86 participants), and tracheostomy (RR 0.38, 95% CI 0.14 to 1.02; two studies, 83 participants). Duration of mechanical ventilation, length of intensive care unit stay (ICU), and length of hospital stay were measured in the three studies. Due to differences in reporting, we could not combine the results and have listed them separately. Chest pain, chest tightness, bodily pain, and adverse effects were each measured in one study.
Authors' conclusions
There was some evidence from three small studies that showed surgical treatment was preferable to nonsurgical management in reducing pneumonia, chest deformity, tracheostomy, duration of mechanical ventilation, and length of ICU stay. Further well‐designed studies with a sufficient sample size are required to confirm these results and to detect possible surgical effects on mortality.
Plain language summary
Surgical versus nonsurgical interventions for flail chest (ribs with more than one fracture)
Background
Flail chest is a medical term describing multiple rib fractures, when ribs are broken or dislocated in more than one place and are no longer completely connected to the other rib bones. When a person injured in this way breathes, the broken segment may move in a different way compared to the rest of the chest wall. Flail chest can cause a person to have difficulty breathing, in which case they may be given mechanical ventilation (machine‐assisted breathing). Surgery is sometimes performed in order to reconnect the broken ribs.
The authors of this review aimed to evaluate the effects and safety of surgery compared with no surgery for people with flail chest.
Study characteristics
We searched scientific databases for studies comparing surgical treatment with nonsurgical treatment in adults or children with flail chest.
Key results
We included three studies in this review, which involved 123 people. In these studies, people with flail chest were randomly allocated into the surgery or no surgery study groups.
The results show that surgery to repair the broken ribs reduces pneumonia, chest deformity, tracheostomy, duration of mechanical ventilation and length of ICU stay. There was no difference in deaths between people treated with surgery or no surgery. Since only six people died across the three studies, due to a variety of causes, more research is needed in order to know for certain which treatment is better for reducing deaths.
These three small studies have shown that surgical treatment is preferable to nonsurgical treatment in reducing pneumonia, chest deformity, tracheostomy, mechanical ventilation and length of stay in the ICU. More research is needed in order to know which treatment is better for reducing deaths. Three more studies are being undertaken by researchers in the USA and Canada at the moment, and the results will be incorporated into the review in the future.
Background
Description of the condition
Flail chest (FC) is defined as a segment of chest wall that moves paradoxically with respiration relative to the rest of the chest wall. It is usually caused by comminuted costal fractures or dislocations leading to loss of bone continuity of this segment from the rest of the rigid thoracic wall (Jones 1980). FC can affect any face of the thoracic wall but is more frequent in the anterior and lateral faces as a result of direct impact or compression on these regions. Besides rib fractures, FC can be associated with fractures of the costal cartilages and sternum and eventually compromise both sides of the thorax. Usually FC is associated with other intra‐ and extrathoracic injuries (Besson 1982); 40% to 60% of people with FC have pulmonary contusion and about 70% have pneumothorax or hemothorax, or both (Besson 1982; Freedland 1990; Ciraulo 1994). Mediastinal injuries and diaphragmatic injuries can also be present (Wilson 1977). Extrathoracic injuries affect around 90% of people with FC, the most frequent being brain injury in 66%, skeletal fractures in 64%, and abdominal injuries in 34% of people (Besson 1982).
FC is present in 10% to 20% of people admitted to trauma centers, with traffic crashes being the main cause (Besson 1982; LoCicero 1989; Perna 2010), followed by domestic falls and occupational injuries (Galan 1992). The clinical presentation and prognosis of people with FC depends on the extent of the thoracic wall injury and the presence of other associated intra‐ or extrathoracic injuries, mainly pulmonary contusion and brain injury (Trinkle 1975; Shackford 1976; Shackford 1981; Besson 1982; Richardson 1982; Perna 2010). Diagnosis of FC is by physical exam, observation, and palpation of paradoxical movement of the affected thoracic wall (Pate 1989; Fullerton 1995). In some people, chest wall edema, hematomas or subcutaneous emphysema can delay diagnosis (Ebert 1967). In one retrospective study, Clark 1988 found an overall mortality of 25% for FC and 16% for isolated pulmonary contusion, the association of both increasing mortality to 42%. Perna 2010, in a prospective study on thoracic trauma (TT), found an incidence of 17%, and mortality of 13%, for people with FC.
Description of the intervention
The treatment of FC is directed toward the maintenance of good ventilation through minimization of progressive pulmonary injury and the prevention of complications (Pate 1989). As FC is always associated with other intra‐ and extrathoracic injuries, such as pulmonary contusion and brain injury, there is a debate about the role of FC in pulmonary and cardiac functions and its contribution to the clinical picture and a person's prognosis (Maloney 1961). This debate has promoted different strategies for the treatment of FC. Avery 1956 proposed pneumatic internal stabilization (PIS), tracheal intubation, and controlled ventilation. This treatment became very popular and was given to all people with FC (Wilson 1977), leading to a situation of over‐treatment (Fullerton 1995). The combination of FC, pulmonary contusion, prolonged intubation, and mechanical ventilation is a risk factor for adult respiratory distress syndrome and sepsis leading to a mortality rate near to 50% (Pepe 1984; Montgomery 1985). To decrease the high rate of morbidity and mortality some authors proposed the use of PIS in a more selective way (Trinkle 1975; Ginsberg 1977). Today fewer than one‐half of people with FC require PIS (Richardson 1982; Fullerton 1995). Some studies have argued that surgical stabilization of FC improves the overall results of the treatment of this condition (reduced mortality, morbidity, length of ventilatory assistance, and hospital stay) (Adkins 1968; Moore 1975; París 1975; Thomas 1978; Kim 1981; Schmit‐Neuerburg 1982).
How the intervention might work
The objective of surgical stabilization is to recover thoracic wall rigidity and restore normal ventilation (Adkins 1968; Moore 1975; París 1975; Thomas 1978; Kim 1981; Schmit‐Neuerburg 1982), thus decreasing mortality and morbidity due to causes such as pneumonia, adult respiratory distress syndrome and sepsis, length of mechanical ventilatory support, and length of stay in the intensive care unit (ICU). The surgical stabilization consists of immobilization of the fractured structures (ribs, costal cartilages, and sternum). Different structures of metal such as wires, bars, and plaques are used to accomplish the stabilization (Judet 1973; París 1975; Ginsberg 1977; Di Fabio 1995; Lardinois 2001). The procedure is performed by a thoracotomy and the structure is placed intramedullary or external to the rib.
Why it is important to do this review
FC may require a long stay in the ICU and ventilatory support, and may result in high morbidity and mortality. Some authors argue that surgical stabilization of all fractured ribs can improve the overall results of the treatment of this condition (reduce mortality, morbidity, the length of ventilatory assistance, and hospital stay) (Adkins 1968; Moore 1975; París 1975; Thomas 1978; Kim 1981; Schmit‐Neuerburg 1982). Others argue that clinical management alone is safer and more effective and if necessary a pneumatic stabilization should be performed (Todd 1989).
Objectives
To evaluate the effectiveness and safety of surgical stabilization compared with clinical management for people with FC.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs), using a parallel design, comparing surgical stabilization (any type) with clinical management.
Types of participants
Adults or children with FC.
Types of interventions
Any type of surgical intervention to stabilize FC compared with clinical management. Clinical management included any type of chest wall stabilization without surgical intervention such as straps or bags and any type of ventilatory assistance.
Types of outcome measures
Primary outcomes
-
Mortality:
early mortality (death from any cause within the 30 days following trauma);
late mortality (death from any cause more than 30 days after trauma).
Secondary outcomes
Long‐term sequelae (chronic chest wall pain or deformity).
Adverse effects related to the interventions (wounds infection, bone infection, pain).
Adverse pulmonary evolution (pneumonia, adult respiratory distress syndrome, and sepsis).
Tracheostomy.
Duration of mechanical ventilation.
Length of ICU stay.
Length of hospital stay.
We analyzed pain severity in the early period (until 30 days after trauma), intermediate period (from 31 to 90 days after trauma), and late period (more than 90 days after trauma). We accepted any validated instrument assessing pain severity (scales, questionnaires, tests, or other method) if presented in the studies. By definition, thoracic deformity is considered to be any change of form or chest modification.
Information size for the primary outcome
The mortality attributed to FC is similar around the world and has not changed over time. In 2014, in one retrospective analysis of 3467 people with FC found the mortality rate was 16% (Dehghan 2014). The mortality rate among people with FC who were given mechanical ventilation was 21% in one study performed in 1975 (Trinkle 1975), and 25% in one study performed in 1988 (Clark 1988).
Considering an approximate mortality rate of 20% for people with FC and considering that the intervention (surgical stabilization) will reduce the mortality rate by 10%, a study designed as two‐sided, with a 5% significance level (α = 0.05) and 90% power (β = 0.1), 263 participants must be randomized to each intervention group (Pocock 1983).
Search methods for identification of studies
In order to reduce publication and retrieval bias, we did not restrict our search by language, date, or publication status.
Electronic searches
The Cochrane Injuries Group's Trials Search Co‐ordinator searched the following:
Cochrane Injuries Group Specialised Register (2 May 2014);
Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library) (Issue 4 of 12, 2014);
Ovid MEDLINE(R), Ovid MEDLINE(R) In‐Process and Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid OLDMEDLINE(R) (1946 to 2 May 2014);
EMBASE Classic + EMBASE (OvidSP) (1947 to 2 May 2014);
CINAHL Plus (EBSCO) (1937 to 2 May 2014);
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) (1970 to May 2014);
ISI Web of Science: Conference Proceedings Citation Index‐Science (CPCI‐S) (1990 to May 2014);
Clinicaltrials.gov (www.clinicaltrials.gov) (accessed 12 May 2014);
International Clinical Trials Registry Platform (apps.who.int/trialsearch/) (accessed 12 May 2014).
Appendix 1 reports the search strategies.
Searching other resources
We screened the bibliographies of relevant publications found by the search for further studies and contacted experts in the field.
Data collection and analysis
The Cochrane Injuries Group's Trials Search Coordinator ran the searches and collated the search results, using reference management software, before passing them on to the review authors.
Selection of studies
Two review authors (OFHS and CDC) independently:
examined titles and abstracts to remove irrelevant reports;
retrieved full‐text copies of the potentially relevant reports;
identified multiple reports from the same study by checking authors' names, location, and setting; details of the intervention; date and duration of the study;
examined full‐text reports for compliance with eligibility criteria;
if necessary corresponded with authors to clarify any questions relating to the study;
made a final decision on study inclusion.
We resolved disagreements by consensus with participation of all review authors.
Data extraction and management
Two review authors (OFHS and CAJM) independently extracted data from eligible studies and summarized them using a data extraction form (Appendix 2). This summary contained the baseline characteristics of the study and control group participants and included their number, age, gender, interventions, and main outcome measures. In addition, we extracted duration of follow‐up and numbers lost to follow‐up. Where more than one publication has arisen from a study, we extracted data from all relevant publications but removed any duplications. We resolved disagreements by discussion. If this did not result in consensus, the third review author's opinion (OCPE) was decisive (Higgins 2011).
Assessment of risk of bias in included studies
Two review authors (CDC and OFHS) assessed each trial independently. We resolved possible disagreements by consensus, or with consultation of a third party (OCPE). We calculated inter‐rater agreement for key bias indicators (e.g. allocation concealment, incomplete outcome data) using the kappa statistic (Higgins 2011). In cases of disagreement, the rest of the group was consulted and a judgment was made based on consensus.
We assessed the risk of bias using The Cochrane Collaboration's 'Risk of bias' tool (Higgins 2011). We used the following criteria.
Was the allocation sequence adequately generated?
Was the allocation adequately concealed?
Was knowledge of the allocated intervention adequately prevented during the study?
Were incomplete outcome data adequately addressed?
Were reports of the study free of suggestion of selective outcome reporting?
Was the study apparently free of other problems that could put it at a high risk of bias?
We made a judgment of 'low risk of bias', 'high risk of bias', or 'unclear risk of bias' for each of the criteria, according to the guidance in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We produced a 'Risk of bias' graph and 'Risk of bias' summary table.
Measures of treatment effect
We presented binary outcomes as risk ratios (RR) with corresponding 95% confidence intervals (CI). We analyzed continuous outcomes as mean differences (MD) with corresponding 95% CIs.
Unit of analysis issues
Given the surgical nature of the interventions, we did not consider cross‐over trials to be a suitable study design. Similarly, we did not consider cluster randomized trials to be appropriate as there could be other factors at a particular trial site (e.g. the skill of the surgeon, resources of the ICU), which could affect outcomes. These two study designs were not eligible for inclusion in the review. We considered RCTs using a simple parallel group design where the unit of analysis was the participant.
Dealing with missing data
We sought to obtain relevant missing data from authors, and carefully perform the evaluation of important numerical data such as screened, randomized participants as well as intention‐to‐treat (ITT), as‐treated, and per‐protocol (PP) populations. We investigated attrition rates, for example drop‐outs, losses to follow‐up, and withdrawals, and critically appraised issues of missing data and imputation methods (e.g. last‐observation‐carried‐forward) (Higgins 2011).
Assessment of heterogeneity
We first assessed statistical heterogeneity using the I2 statistic, which examines the percentage of total variation across studies due to heterogeneity rather than chance (Higgins 2011). Values of I2 under 40% indicate a low level of heterogeneity and justify use of a fixed‐effect model for meta‐analysis. Values of I2 between 40% and under 75% are considered moderate and a random‐effects model can be used. Values of I2 higher than 75% indicate a high level of heterogeneity and so it is inappropriate to combine the results (Higgins 2011).
Assessment of reporting biases
We planned to create funnel plots if we included 10 or more studies in the review, in order to assess the potential existence of small‐study bias. However, as this review included only three RCTs, we were unable to perform this analysis. There are a number of explanations for the asymmetry of a funnel plot (Sterne 2002), therefore, we would have carefully interpreted the results (Lau 2006).
Data synthesis
Where the data available were sufficiently similar, we summarized them statistically using Review Manager 5 (RevMan 2011). In the event of low heterogeneity, we planned to use a fixed‐effect model for meta‐analysis (Higgins 2011).
Subgroup analysis and investigation of heterogeneity
We planned the following subgroup analyses, but due to lack of data none were performed. In the future, when more studies are included in the review, these subgroup analyses may be performed.
Age.
Isolated FC.
FC associated with other pleural, mediastinal, or pulmonary lesions.
Injury severity score (less than, equal to, or greater than 15) (Baker 1974).
Sensitivity analysis
We planned to perform sensitivity analyses in order to explore the influence of allocation concealment on effect size. However, as this review included only three RCTs we were unable to perform this analysis. In the future, when more studies are included in the review, we may perform sensitivity analyses.
Results
Description of studies
Results of the search
The electronic database search retrieved 1798 references (Figure 1). We selected 20 articles to review in full‐text. Three studies met the inclusion criteria (Tanaka 2002; Granetzny 2005; Marasco 2013).
1.
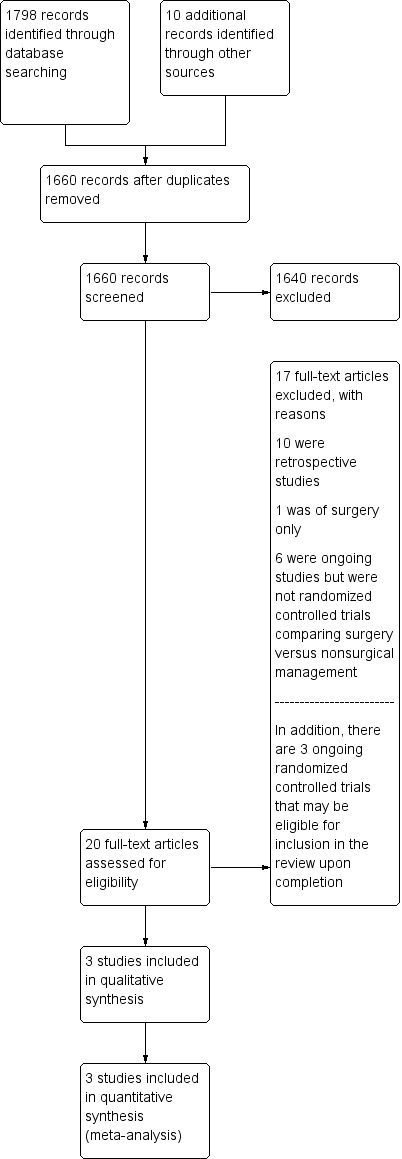
Study flow diagram.
Included studies
The three studies involved 123 participants and were described as RCTs (Tanaka 2002; Granetzny 2005; Marasco 2013). Granetzny 2005 reported a follow‐up of two months, Marasco 2013 followed participants for six months, and Tanaka 2002 followed participants for 12 months. See Characteristics of included studies and Characteristics of excluded studies.
Tanaka 2002 was performed at Kyorin University Hospital in Tokyo, Japan; Granetzny 2005 was conducted in Cairo, Egypt; and Marasco 2013 was performed in Melbourne, Australia.
Types of interventions
Tanaka 2002 randomized 37 people to surgical or nonsurgical management groups. The participants were recruited from emergency room admissions for chest trauma and FC with the need for mechanical ventilation. The surgical group consisted of 18 people who underwent the surgical fixation of fractured ribs and 19 people were treated conservatively. For the fixation of fractured ribs, surgeons used metal plates (Judet struts). People in the control group were treated per the standard of care, that is, with orotracheal intubation and intermittent positive pressure ventilation.
Granetzny 2005 randomized 40 people with thoracic injuries that were associated with three or more rib fractures accompanied by FC. After 24 to 36 hours in the ICU, people were randomized into two groups: conservative or surgical treatments. Twenty participants were allocated to each group. For the participants allocated to the nonsurgical management group, straps and plastic packaging with an adhesive segment were fixed 5 cm anteriorly and posteriorly and one rib above and one below the unstable chest segment. This adhesive was held in place for at least seven to 10 days. Participants in the surgical group were treated for the fixation of fractured ribs with either stainless steel wire or Kirschner wire, or both.
Marasco 2013 randomized 46 people with FC that required invasive mechanical ventilation. Twenty‐three people were randomized to surgical rib fixation and the remaining 23 to nonsurgical management. Rib fractures between levels three and 10 were fixed for the people assigned to surgical management. Ribs fractured more than once were addressed by fixing one fracture per rib and converting a flail segment into simple fractured ribs. People assigned to nonsurgical management were treated with the standard of care, that is, mechanical ventilator management.
Types of outcomes measured
Tanaka 2002 evaluated pneumonia, tracheotomy, length of mechanical ventilation, ICU stay, long‐term respiratory function, dyspnea, costs, return to employment, lung contusion, and a questionnaire including a variety of outcomes given at six and 12 months following injury.
Granetzny 2005 measured pulmonary status, mechanical ventilation time, ICU stay, hospital stay, chest deformity, chest infections, and mortality.
The outcomes of interest in Marasco 2013 were the duration of mechanical ventilation, ICU stay, pneumonia, pneumothorax, chest deformity, failed extubation, tracheostomy, readmission to the ICU, duration of hospital stay, costs, return to employment, and a QoL questionnaire (36‐item Short Form (SF‐36)) given at six months following injury.
Excluded studies
We excluded 10 studies because they were retrospective studies (Ohresser 1972; Kim 1981; Borrelly 1985; Ahmed 1995; Karev 1997; Voggenreiter 1998; Balci 2005; Nirula 2006; Teng 2009; Althausen 2011), and one study because it evaluated a surgical intervention only (Lardinois 2001).
Ongoing studies
We identified three ongoing studies, which we will include in updates of this review if they meet eligibility criteria (NCT01147471; NCT01308697; NCT01367951).
Risk of bias in included studies
2.
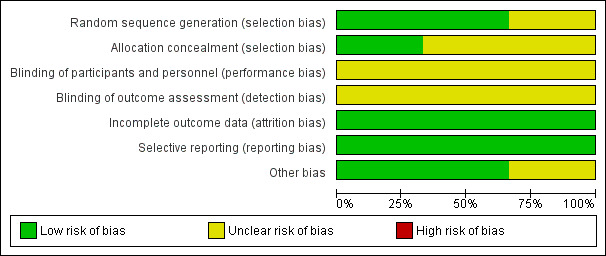
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies. Three studies are included in this review.
3.
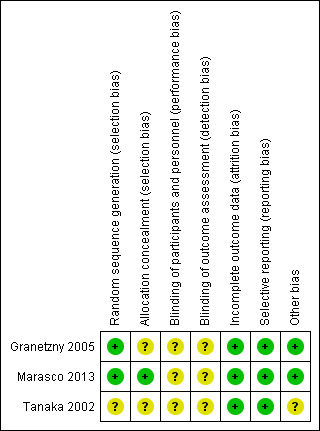
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Generation of the randomization sequence (selection bias)
Tanaka 2002 did not report on the generation of the randomization sequence, thus we classified this study as having an unclear risk of bias. Granetzny 2005 used a table of random numbers in blocks of 10 participants, and Marasco 2013 used a computer‐generated code using block randomization with a block size of four. Therefore, we classified both studies as having low risks of bias.
Allocation
The Granetzny 2005 and Tanaka 2002 studies did not describe allocation concealment; thus, we judged this as unclear risk of bias. The Marasco 2013 study used opaque envelopes to conceal allocation. We considered this to be adequate, and assigned low risk of bias to this domain.
Blinding
None of the three studies included descriptions of blinding; thus, we judged this as unclear risk of bias (Tanaka 2002; Granetzny 2005; Marasco 2013).
Incomplete outcome data
Two studies did not mention participant withdrawals (Tanaka 2002; Granetzny 2005). In Marasco 2013, one participant who was assigned to the nonsurgical group died prior to hospital discharge. Another participant assigned to the surgical group did not have surgery due to the development of sepsis, but was later analyzed in the surgical group on an ITT basis. Therefore, we classified this domain as low risk of bias in all included studies (Tanaka 2002; Granetzny 2005; Marasco 2013).
Selective reporting
We judged all included studies to be free of selective reporting; therefore, we classified this item as low risk of bias (Tanaka 2002; Granetzny 2005; Marasco 2013).
Other potential sources of bias
We identified no other potential sources of bias (Tanaka 2002; Granetzny 2005; Marasco 2013).
Effects of interventions
We wrote to the authors of all included studies to clarify methodological issues and to request complete data for the analyses (Tanaka 2002; Granetzny 2005; Marasco 2013).
Primary outcome
Mortality
Three studies involving 123 people reported deaths. There was no statistically significant difference in deaths between the treatment groups (RR 0.56, 95% CI 0.13 to 2.42, I2 = 0%, P value = 0.70) (Analysis 1.1).
1.1. Analysis.
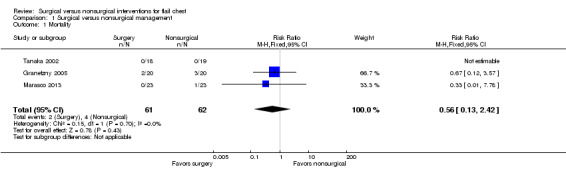
Comparison 1 Surgical versus nonsurgical management, Outcome 1 Mortality.
Among the six people who died, the causes of death were pneumonia, pulmonary embolism, mediastinitis, and septic shock. There were no deaths in the Tanaka 2002 study. The time of the five deaths that occurred during the Granetzny 2005 study was not given. The one death in the Marasco 2013 study was due to sepsis and occurred at day 92 postinjury. As there is only information about one late death, and there was no information about the time of the other five deaths, it was not possible to separate early and late mortality.
Secondary outcomes
Long‐term sequelae (deformity, chronic chest wall pain)
Deformity
Two studies involving 86 participants reported chest wall deformity (Granetzny 2005; Marasco 2013). Neither study reported how deformity was measured. There was a statistically significant difference favoring the surgical group (RR 0.13, 95% CI 0.03 to 0.67, I2 = 0%, P value = 0.75, number needed to treat for an additional beneficial outcome (NNTB) = 4) (Analysis 1.2).
1.2. Analysis.
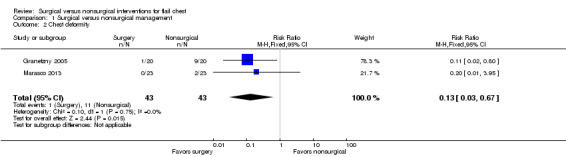
Comparison 1 Surgical versus nonsurgical management, Outcome 2 Chest deformity.
Chronic chest wall pain
As the studies used different questionnaires, the results could not be combined. It was only possible to analyze chronic pain, because the three studies did not report on pain in the early or intermediate period.
The Marasco 2013 study measured bodily pain according to the SF‐36 Quality of Life Questionnaire at six months following injury. Answers to the questionnaire were converted to a score with a range from 0 to 100. A score of 0 represents the worst quality of life, and a score of 100 the best quality of life. Thirty‐seven of the 46 participants (80%) completed the questionnaire. There was no difference between treatment groups in pain score ((mean group score ± standard deviation) surgical group: 42.2 ± 9.4, nonsurgical group: 37.9 ± 11.0, P value = 0.22).
All 37 participants in the Tanaka 2002 study completed a questionnaire 12 months following injury, which included a question about pain and feeling tightness in the chest. The internal pneumatic stabilization group continued to experience thoracic cage pain and chest tightness more frequently than those in the surgical stabilization group (persistent pain: 89% with no surgery versus 39% with surgery, P value < 0.05; persistent chest tightness: 84% with no surgery versus 33% with surgery, P value < 0.05).
Adverse effects related to the interventions (wound infection, bone infection, pain)
Wound infection
In the Granetzny 2005 study, 2/20 people in the surgical group had a wound infection compared with 0/20 in the nonsurgical group (RR 5.00, 95% CI 0.26 to 98.00, P value = 0.29) (Analysis 1.3).
1.3. Analysis.
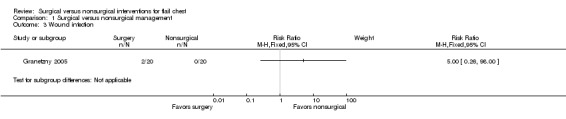
Comparison 1 Surgical versus nonsurgical management, Outcome 3 Wound infection.
Bone infection
None of the studies reported on bone infection.
Pain
None of the studies reported intervention‐related pain.
Adverse pulmonary evolution (pneumonia, adult respiratory distress syndrome, sepsis)
Pneumonia
All three included studies reported pneumonia but none of the studies provided a definition for pneumonia (Tanaka 2002; Granetzny 2005; Marasco 2013). There was a statistically significant difference favoring the surgical group (RR 0.36, 95% CI 0.15 to 0.85, I2 = 66%, P value = 0.05, NNTB 2) (Analysis 1.4).
1.4. Analysis.
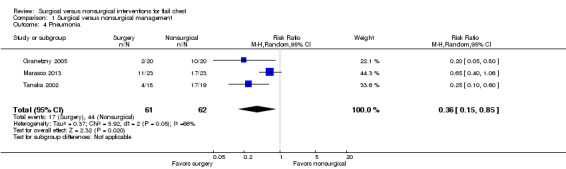
Comparison 1 Surgical versus nonsurgical management, Outcome 4 Pneumonia.
Adult respiratory distress syndrome
None of the studies reported on adult respiratory distress syndrome.
Sepsis
None of the studies describe any participants as having survived sepsis. One participant in the Marasco 2013 study died from sepsis. There was insufficient information given in the study report to enable an analysis of this outcome.
Tracheostomy
Two studies involving 83 participants reported using a tracheostomy (Tanaka 2002; Marasco 2013). They reported 43 events, and the RR was sensitive to the analysis model used (I2 = 66%). There was a difference favoring the surgical group (RR 0.38, 95% CI 0.14 to 1.02, I2 = 64%, P value = 0.05, NNTB 2) (Analysis 1.5).
1.5. Analysis.
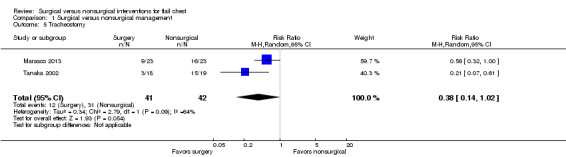
Comparison 1 Surgical versus nonsurgical management, Outcome 5 Tracheostomy.
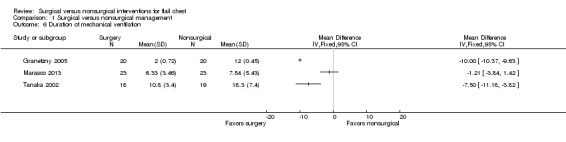
Duration of mechanical ventilation
All three studies reported on the duration of mechanical ventilation. There was wide variation in the duration of mechanical ventilation between studies, and so it was inappropriate to combine the results (I2 = 95%).
In the Tanaka 2002 study, participants receiving surgery required less mechanical ventilation (MD 7.50 fewer days, 95% CI ‐11.18 to ‐3.82).
In the Granetzny 2005 study, participants receiving surgery required less mechanical ventilation (MD 10.00 fewer days, 95% CI ‐10.37 to ‐9.63).
In the Marasco 2013 study, there was no difference in the duration of mechanical ventilation between treatment groups (MD 1.21 fewer days, 95% CI ‐3.84 to 1.42).
Length of intensive care unit stay
All three studies reported on the length of ICU stay, but we could not combine the results.
The Marasco 2013 study reported length of ICU stay in different ways, but none of the data could be combined with other study data for meta‐analysis due to the way it was reported.
| Outcomes | Surgical group (n = 23) | Nonsurgical group (n = 23) | P value |
| Duration of ICU stay prerandomization (h, mean ± SD) | 61.6 ± 36.1 | 81.3 ± 84.2 | 0.31 |
| Duration of ICU stay between randomization and surgery (h, mean ± SD) | 49.4 ± 35.9 | N/A | N/A |
| Duration of ICU stay postrandomization (h, median (IQR)) | 285 (191‐319) | 359 (270‐581) | 0.03 |
| Total ICU stay (h, median (IQR)) | 324 (238‐380) | 448 (323‐647) | 0.03 |
| h: hours; ICU: intensive care unit; IQR: interquartile range; n: number; SD: standard deviation. | |||
There was wide variation in the length of stay between the Granetzny 2005 and Tanaka 2002 studies, and so it was inappropriate to combine the results (I2 = 96%) (Analysis 1.7).
1.7. Analysis.
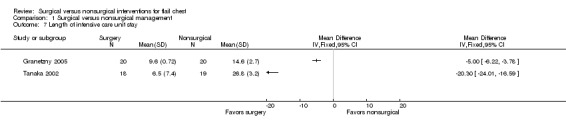
Comparison 1 Surgical versus nonsurgical management, Outcome 7 Length of intensive care unit stay.
In the Tanaka 2002 study, participants receiving surgery spent fewer days in the ICU (MD 20.30 fewer days, 95% CI ‐24.01 to ‐16.59).
In the Granetzny 2005 study, participants receiving surgery spent fewer days in the ICU (MD 5.00 fewer days, 95% CI ‐6.22 to ‐3.78).
Length of hospital stay
Two of the three studies reported on the length of hospital stay, but we could not combine the data due to incomplete reporting.
Tanaka 2002 did not report length of hospital stay.
The Marasco 2013 study reported the median number of days participants spent in the hospital.
| Outcome | Surgical group (n = 23) | Nonsurgical group (n = 23) | P value |
| Duration of hospital stay (days, median (IQR)) | 20 (18‐28) | 25 (18‐38) | 0.24 |
| IQR: interquartile range; n: number. | |||
The authors pointed out that the five‐day reduction in hospital stay reflected the five‐day reduction in total ICU stay (given above in hours).
In the Granetzny 2005 study, participants receiving surgery spent fewer days in the hospital. We could not include the data in a forest plot as no standard deviation values were reported.
| Outcome | Surgical group (n = 20) | Nonsurgical group (n = 20) | P value |
| Mean hospital stay, days | 11.7 | 23.1 | < 0.001 |
| n: number. | |||
Discussion
Summary of main results
There was no evidence that surgical intervention reduced mortality in people with FC compared with nonsurgical management. There was some evidence that surgical intervention could reduce the risk of developing pneumonia and thoracic deformity; need for tracheostomy; duration of mechanical ventilation, length of ICU stay, and hospital stay; and chronic pain, but the trials to date have been small.
Overall completeness and applicability of evidence
This review included three small studies, undertaken in Egypt, Australia, and Japan, involving people with FC. The review did not provide an answer as to whether surgery or no surgery is better in preventing death. This is because there were too few people included in the studies to be able to detect a difference in the effects of the treatment. There needed to be at least 550 people included in the analysis before we could have reliable information about the benefits of one treatment or the other. At the moment, only 123 people have been included in RCTs of surgery for FC.
Although the number of people included in the analyses for the secondary outcomes (i.e. pneumonia, chest deformity, tracheostomy, duration of mechanical ventilation, and length of ICU and hospital stay) was small, surgery appeared to be beneficial. This may due to a large benefit between the two groups for those outcomes, or it could be chance findings. The uncertainty in the true benefit of surgery for FC will be partly resolved when the results of the three ongoing studies are included in the review in the future (NCT01147471; NCT01308697; NCT01367951). However, even the ongoing studies are small and so larger multicenter RCTs are needed.
Quality of the evidence
The quality of the included trials was generally poor with only one of the included studies having good allocation concealment. There was no blinding of outcome assessment in the included trials. However, as the comparison was surgical treatment versus medical treatment, this bias is difficult to avoid. One further limitation that decreases the quality of evidence was the lack of definitions for outcomes such as pneumonia, which was defined only in one study (Tanaka 2002).
Potential biases in the review process
Although we conducted a comprehensive search, we cannot be sure that we have included all relevant trials, as some trials may have never been published. The possibility that the trials we have identified are those that show stronger treatment effects is also a potential threat to validity.
Agreements and disagreements with other studies or reviews
Retrospective studies have shown lower mortality (Karev 1997), lower risk of developing pneumonia (Kim 1981; Borrelly 1985; Ahmed 1995; Balci 2005; Teng 2009), lower chest deformity rates (Teng 2009), lower need for tracheostomy, and lower duration of mechanical ventilation and length of ICU stay (Ahmed 1995; Teng 2009) with surgical fixation of rib fractures. Two meta‐analyses, one including 11 studies (Slobogean 2013) and another including nine studies (Leinicke 2013) also found reductions in ICU stay, duration of mechanical ventilation, mortality, pneumonia, thoracic deformity, and need for tracheostomy in people who were treated surgically, but these reviews included only two RCTs, combined with the retrospective studies.
The results of this systematic review of RCTs are consistent with what retrospective studies have already shown. Further RCTs are required to confirm the results of this review.
Authors' conclusions
Implications for practice.
There is some evidence from three small studies that surgical intervention is superior to nonsurgical intervention in the treatment of flail chest in reducing pneumonia, chest deformity, tracheostomy, duration of mechanical ventilation, and length of intensive care unit stay.
Implications for research.
There is an urgent need for larger high‐quality randomized controlled trials.
We identified three ongoing studies:
In one US study, the primary outcome is mortality and the target sample size is 100 participants (NCT01147471).
In one Canadian study, the primary outcome is ventilator‐free days and the target sample size is 206 participants (NCT01367951).
One pilot study conducted in Canada enrolled 14 participants, and did not specify a primary outcome (NCT01308697).
Because of the small sample sizes, it is unlikely that these studies will resolve this research question. Larger multicenter randomized controlled trials are needed.
Acknowledgements
We would like to thank Emma Sydenham and Deirdre Beecher from the Cochrane Injuries Group for their help in preparing this review.
This project was supported by the UK National Institute for Health Research (NIHR), through Cochrane Infrastructure funding to the Cochrane Injuries Group. The views and opinions expressed are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health System, or the Department of Health.
Appendices
Appendix 1. Search strategies
Cochrane Injuries Group Specialised Register
("flail chest" or "rib fractures" or "thoracic injuries" or "stove‐in chest") and ((thoracic and surg*) or (rib and fracture* and surg*) or (pneumatic* and internal* and stabili*) or (tracheal and intub*) or (surg* and stabil* ) or (control* and ventillat*))
Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library)
#1MeSH descriptor: [Flail Chest] explode all trees #2MeSH descriptor: [Rib Fractures] this term only #3MeSH descriptor: [Thoracic Injuries] explode all trees #4((flail or stove?in) near/3 chest):ti,ab,kw #5((intra* or extra) near/3 thora*):ti,ab,kw #6"costal fracture* ":ti,ab,kw (Word variations have been searched) #7((mediastinal or diaphragmatic) near/3 injuries):ti,ab,kw (Word variations have been searched) #8#1 or #2 or #3 or #4 or #5 or #6 or #7 #9MeSH descriptor: [Thoracic Surgical Procedures] this term only #10(tracheal near/5 intub*):ti,ab,kw (Word variations have been searched) #11"fracture fixation":ti,ab,kw (Word variations have been searched) #12(intubation or ventilation):ti,ab,kw (Word variations have been searched) #13#9 or #10 or #11 or #12 #14#8 and #13
Ovid MEDLINE(R), Ovid MEDLINE(R) In‐Process and Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid OLDMEDLINE(R)
1. Flail Chest/ 2. exp Thoracic Injuries/ 3. Rib Fractures/ 4. ((intra* or extra) adj3 thora* adj3 injur*).ab,ti. 5. ((flail or stove?in) adj3 chest).ab,ti. 6. "rib fracture* ".ab,ti. 7. "costal fracture* ".ab,ti. 8. ((mediastinal or diaphragmatic) adj3 injuries).ab,ti. 9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 10. Thoracic Surgical Procedures/ 11. (tracheal adj5 intub*).ab,ti. 12. "fracture fixation".ti,ab. 13. (intubation or ventilation).ti,ab. 14. surgery.fs. 15. 10 or 11 or 12 or 13 or 14 16. 9 and 15 17. randomi?ed.ab,ti. 18. randomized controlled trial.pt. 19. controlled clinical trial.pt. 20. placebo.ab. 21. clinical trials as topic.sh. 22. randomly.ab. 23. trial.ti. 24. Comparative Study/ 25. 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 26. (animals not (humans and animals)).sh. 27. 25 not 26 28. 16 and 27
EMBASE Classic + EMBASE (OvidSP)
1. Flail Chest/ 2. exp Thoracic Injuries/ 3. Rib Fractures/ 4. ((intra* or extra) adj3 thora* adj3 injur*).ab,ti. 5. ((flail or stove?in) adj3 chest).ab,ti. 6. "rib fracture* ".ab,ti. 7. "costal fracture* ".ab,ti. 8. ((mediastinal or diaphragmatic) adj3 injuries).ab,ti. 9. 1 or 2 or 3 or 4 or 6 or 7 or 8 10. Thoracic Surgical Procedures/ 11. (tracheal adj5 intub*).ab,ti. 12. "fracture fixation".ti,ab. 13. (intubation or ventilation).ti,ab. 14. 10 or 11 or 12 or 13 15. 9 and 14 16. exp Randomized Controlled Trial/ 17. exp controlled clinical trial/ 18. exp controlled study/ 19. comparative study/ 20. randomi?ed.ab,ti. 21. placebo.ab. 22. *Clinical Trial/ 23. exp major clinical study/ 24. randomly.ab. 25. (trial or study).ti. 26. 16 or 17 or 18 or 20 or 21 or 22 or 23 or 24 or 25 27. exp animal/ not (exp human/ and exp animal/) 28. 26 not 27 29. 15 and 28 30. limit 29 to embase
CINAHL Plus (EBSCO)
Limiters ‐ Exclude MEDLINE records S26S14 and S25 S25S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 S24MH quantitative studies S23TX random* N3 allocat* S22(MH "Random Assignment") S21TX placebo* S20(MH "Placebos") S19TX randomi?ed N3 control* N3 trial* S18TI ( (singl* N3 blind*) or (doubl* N3 blind*) or (trebl* N3 blind*) or (tripl* N3 blind*) ) or TI ( (singl* N3 mask*) or (doubl* N3 mask*) or (trebl* N3 mask*) or (tripl* N3 mask*) ) or AB ( (singl* N3 blind*) or (doubl* N3 blind*) or (trebl* N3 blind*) ) or AB ( (singl* N3 mask*) or (doubl* N3 mask*) or (trebl* N3 mask*) or (tripl* N3 mask*) ) S17TX clinical N3 trial* S16PT clinical trial* S15(MH "Clinical Trials") S14S7 and S13 S13S8 or S9 or S10 or S11 or S12 S12(surg N5 stabil*) S11TX (tracheal N5 intub*) S10TX (pneumatic* N3 internal* N3 stabili*) S9(MH "Rib Fractures/SU") S8(MH "Thoracic Surgery/MT") S7S1 or S2 or S3 or S4 or S5 or S6 S6TX ((intra* or extra) N3 thora* N3 injur*) S5TX ((flail or stove?in) N3 chest) S4(MH "Thoracic Injuries/CO") S3(MH "Thoracic Surgery") S2(MH "Rib Fractures/CO") S1(MH "Flail Chest")
Clinical trials registries
Condition: Flail chest
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) and Conference Proceedings Citation Index‐Science (CPCI‐S)
#8#7 AND #6 #7TS=("flail chest" or "rib fractures" or "thoracic injuries" or "stove‐in chest") #6#5 AND #4 #5TS=(human*) #4#3 OR #2 OR #1 #3TS=((singl* OR doubl* OR trebl* OR tripl*) SAME (blind* OR mask*)) #2TS=(controlled clinical trial OR controlled trial OR clinical trial OR placebo) #1TS=(randomised OR randomized OR randomly OR random order OR random sequence OR random allocation OR randomly allocated OR at random OR randomized controlled trial)
Appendix 2. Data extraction form
| Methods | Study design: Method of randomization: Concealment of allocation: Blinded ‐ No ( ) Single ( ) Double ( ) Triple ( ) Unclear ( ) Power calculation: Number of participants randomized: Number of participants analyzed: Number of participants excluded after randomization: Number of participants withdraws and reasons: Intention‐to‐treat analysis: Source of funding: Not stated ( ) Industry ( ) Other ( ) Description: |
| Participants | Country Location: Number of centers: No: Age: Sex: Inclusion criteria: Exclusion criteria: Extension and location of the flail chest: Injury severity score: Intrathoracic associated injuries: Extrathoracic associated injuries: |
| Interventions | Technique of surgical stabilization of flail chest: Nonsurgical attempts of flail chest stabilization: Technique of the ventilatory support or assistance: |
| Outcomes |
Primary: Secondary: |
Data and analyses
Comparison 1. Surgical versus nonsurgical management.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality | 3 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.13, 2.42] |
| 2 Chest deformity | 2 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.03, 0.67] |
| 3 Wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4 Pneumonia | 3 | 123 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.15, 0.85] |
| 5 Tracheostomy | 2 | 83 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.14, 1.02] |
| 6 Duration of mechanical ventilation | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7 Length of intensive care unit stay | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
1.6. Analysis.
Comparison 1 Surgical versus nonsurgical management, Outcome 6 Duration of mechanical ventilation.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Granetzny 2005.
| Methods | Study design: RCT
Multicenter Setting: Cairo University and Zagazig Clinics, Cairo, Egypt Study period: not reported Sample size: not reported Follow‐up: 2 months |
|
| Participants | 40 participants Sex: 31 males Age (mean ± SD): surgical group: 40.5 ± 8.2 years, clinical group: 36 ± 14.9 years Inclusion criteria: all participants with flail chest with ≥ 3 fractures of ribs and paradoxical breathing Exclusion criteria: head trauma with disturbed conscious level; associated injuries such as myocardial contusion that might be adversely affected by general anesthesia; severe associated trauma to other systems; fractures of the upper 3 ribs only, as immobilizing bandages are inefficient in fractures of the upper ribs for anatomic reasons |
|
| Interventions | Group I: conservative treatment using strapping and packing in the form of dressing and fixing with an adhesive bandage, which was put adhesively to the flail segment within 5 cm anterior and posterior to the flail segment and 1 rib above and below it. This adhesive plaster was put in place for at least 7‐10 days, during this period of follow‐up ABGs and chest X‐rays were obtained. Group II: surgical fixation of fractured ribs with stainless steel wire or Kirschner wires, or both after 24‐36 hours of ICU admission. Until the participants were operated upon, they were treated conservatively as if they were in Group I |
|
| Outcomes | Thoracic deformity, lung function, mortality, incidence of pneumonia, duration of mechanical ventilation, length of hospital stay, length of ICU stay, pleural empyema, pulmonary embolism, mediastinitis, scoliosis, and wound infection | |
| Notes | We contacted the main author to request additional information on methodological aspects of the trial and further statistical data. The author of the study replied providing us only with the statistical data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "random numbers balanced in blocks of 10" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no withdrawals |
| Selective reporting (reporting bias) | Low risk | No evidence |
| Other bias | Low risk | No evidence |
Marasco 2013.
| Methods | Study design: RCT Single‐center Setting: Monash University and The Alfred Hospital, Melbourne, Australia Study period: January 2007 ‐ December 2011 Sample size: 23 participants per group Follow‐up: 6 months |
|
| Participants | 46 participants Sex: 40 males Age (mean ± SD): surgical group: 57.8 ± 17.1 years, nonsurgical group: 59.3 ± 10.4 years Inclusion criteria: presence of a flail segment defined as ≥ 3 consecutive ribs fractured in more than 1 place, producing a free‐floating segment of chest wall, diagnosis was made clinically with confirmation on 3‐dimensional computed tomography imaging, ventilator dependent with no prospect of successful weaning within the next 48 hours Exclusion criteria: aged > 80 years, spinal injuries, open rib fractures with soiling or infection, sepsis, severe traumatic brain injury (Glasgow Coma Scale < 10 at the scene of accident or at presentation to the hospital, as its management may have received priority over the study protocol), and uncorrected coagulopathy |
|
| Interventions | Surgery: only rib fractures between the levels of ribs 3 and 10 were fixed. Ribs fractured more than once were usually addressed by fixing 1 fracture per rib, converting a flail segment to simple fractured ribs. Ribs with a single fracture were not fixed unless there was gross deformity mandating intervention. Anterior and lateral rib fractures were preferentially fixed over posterior rib fractures Nonsurgical management: mechanical ventilation |
|
| Outcomes | Primary: duration of mechanical ventilation and ICU stay Secondary: number of respiratory complications (pneumonia, pneumothorax, intercostal catheter usage), rate of failed extubation, rate of tracheostomy, readmission to ICU, duration of hospital stay, and cost assessment of the operation. Pneumonia was defined as a new infiltrate on chest X‐ray, with positive sputum culture. ICU discharge time was recorded as the time the participant was deemed ready for discharge so that ward bed access did not affect the results. A 36‐item Short Form Health Status Questionnaire was sent to all participants at 6 months, to assess physical functioning |
|
| Notes | We contacted the main author to request additional information on methodological aspects of the trial and further statistical data. The author has not yet been in contact with us | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was via a computer generated code using block randomization with block size of 4" |
| Allocation concealment (selection bias) | Low risk | Quote: "After consent and enrolment, an opaque envelope with the treatment assignment was opened and the time of enrolment documented" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 person assigned to the nonsurgical group died before hospital discharge. 1 person assigned to the surgical group did not have surgery due to the development of sepsis, but was analyzed in the surgical group on an intention‐to‐treat basis |
| Selective reporting (reporting bias) | Low risk | No evidence |
| Other bias | Low risk | No evidence |
Tanaka 2002.
| Methods | Study design: Quote: "randomized controlled study"
Single‐center Setting: Kyorin University Hospital, Tokyo, Japan Study period: April 1992 to March 1998 Sample size: 37 participants Follow‐up: 12 months |
|
| Participants | 37 participants (surgical group: 18, nonsurgical group: 19) Sex: 26 males Age (mean ± SD): surgical group: 43 ± 12 years, clinical group: 46 ± 9 years Inclusion criteria: chest trauma and flail chest Exclusion criteria: not requiring mechanical ventilation; fractures of < 6 ribs; people who did not develop acute respiratory failure; severe closed head injury (head Abbreviated Injury Scale score > 3 with unconsciousness) or spinal injury, or both; age < 14 years; consent not given; chronic preexisting heart, pulmonary, hepatic, renal disease, or a combination; and questionnaire not completed |
|
| Interventions | Group S: surgical stabilization Group I: internal pneumatic stabilization |
|
| Outcomes | Incidence of pneumonia, incidence of tracheotomy, length of mechanical ventilation, length of ICU stay, total medical expense, long‐term respiratory function by spirometry, subjective dyspnea, and questionnaire | |
| Notes | We contacted the main author to request additional information on methodological aspects of the trial and further statistical data. The author has not yet responded to us | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "each patient was randomly assigned to either the surgical stabilization group or an internal pneumatic stabilization group according to a randomization chart" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no withdrawals |
| Selective reporting (reporting bias) | Low risk | No evidence |
| Other bias | Unclear risk | No evidence |
ABG: arterial blood gas; ICU: intensive care unit; RCT: randomized controlled study; SD: standard deviation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ahmed 1995 | Retrospective study |
| Althausen 2011 | Retrospective study |
| Balci 2005 | Retrospective study |
| Borrelly 1985 | Retrospective study |
| Karev 1997 | Retrospective study |
| Kim 1981 | Retrospective study |
| Lardinois 2001 | Only surgical intervention |
| Nirula 2006 | Case‐control study |
| Ohresser 1972 | Retrospective study |
| Teng 2009 | Retrospective study |
| Voggenreiter 1998 | Retrospective study |
Characteristics of ongoing studies [ordered by study ID]
NCT01147471.
| Trial name or title | Flail Chest: Early Operative Fixation Versus Non‐operative Management ‐ a Prospective Randomized Study |
| Methods | Study design: RCT Multicenter Setting: Virginia Commonwealth University, Virginia, US Period: ongoing, but not recruiting participants Sample size: 100 participants Follow‐up: 6 months |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Surgical rib fixation: randomized participants will be operated upon within 72 hours of ventilation (early fixation) to stabilize the stove‐in segment. Where all fractured ribs are accessible and the number of fractured ribs is few, stabilization of all fractured ribs would be the goal. However, where fractured ribs are in areas difficult to access, enough ribs, based on surgeon judgment, would be fixed to stabilize the stove‐in segment. Postoperatively, the participants will receive the standard of care, similar to what is outlined for the nonoperative arm. Operative fixation will be accomplished utilizing the MatrixRIB Fixation System (Synthes CMF, West Chester, PA, US) according to the device's instructions for use. Sites will obtain the product based on their medical center's normal purchasing practices Nonsurgical management: randomized participants will receive standard of care therapy for blunt thoracic trauma (as per each participating institution's own protocols): ventilatory support; timing of extubation (removal from ventilator); analgesia: institution should provide adequate analgesia utilizing available resources including oral, parenteral, epidural, local nerve blocks, etc.; chest physical therapy; postural drainage; incentive spirometry ‐ after extubation |
| Outcomes |
Primary outcomes
Pain as measured on analog pain scale, infections, days on ventilator, days in ICU, days in hospital, and surgical complications during hospital stay. At 3 and 6 months postdischarge analog pain measurement, infections and surgical complications
Secondary outcomes
SF‐36 Health Survey
Pulmonary function tests to measure forced vital capacity and forced expiratory volume in 1 second |
| Starting date | September 2010 |
| Contact information | Trauma Research & Education Foundation of Fresno, Fresno, CA, US Carolinas Medical Center, Charlotte, NC, US Wake Forest University Health Sciences, Winston‐Salem, NC, US The Board of Regents of the University of Oklahoma, Oklahoma City, OK, US The University of Tennessee, Knoxville, TN, US Eastern Virginia Medical School, Norfolk, VA, US Virginia Commonwealth University, Richmond, VA, US |
| Notes | This study is ongoing, but not recruiting participants |
NCT01308697.
| Trial name or title | Operative Versus Non Operative Management of Flail Chest: A Randomized Controlled Feasibility Study |
| Methods | Study design: RCT Single‐center Setting: University of British Columbia Period: not reported Sample size: not reported Follow‐up: not reported |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Procedure: surgical fixation of flail chest Other: nonsurgical management |
| Outcomes | Pilot study intends to review numerous clinical outcomes or variables of interest to assist in selecting a primary outcome and sample size for the future definitive trial. Currently length of stay in a high acuity unit is the planned primary outcome measure for the definitive trial |
| Starting date | Not reported |
| Contact information | Royal Columbian Hospital, New Westminster, BC, Canada Vancouver General Hospital, Vancouver, BC, Canada |
| Notes | Pilot study: study start April 2011, study completion August 2013 (final data collection date for primary outcome measure). Enrollment: 14. According to clinicaltrials.gov and PubMed on 8 July 2015, this study has completed recruitment but the results have not yet been published |
NCT01367951.
| Trial name or title | A Multi Centre Randomized Controlled Trial of Operative Versus Non‐operative Treatment of Acute, Unstable Chest Wall Injuries |
| Methods | Study design: RCT Multicenter Setting: St. Michael's Hospital, Toronto, ON, Canada Period: 2011‐2015 Sample size: 206 participants Follow‐up: 12 months |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Surgical fixation
Nonsurgical
|
| Outcomes |
Primary outcome:
To compare early surgical fixation vs. conventional, nonsurgical treatment of unstable chest injuries on the basis of our primary outcome measure of days spent free from a mechanical ventilator in the first 28 days following injury Secondary outcomes:
The total number of days in ICU will be calculated over the 12‐month period postinjury. If no ICU stay is needed the total days in ICU will be 0
The total daily pain medication administration will be calculated, and converted to daily oral morphine equivalence
The number of times participant is diagnosed with pneumonia over 12 months postinjury
Spirometry measurement of total lung capacity, forced vital capacity, and forced expiratory volume in 1 second measured at 3 and 12 months postinjury
To assess if participant has returned to work at 12 months, and at what capacity
Using 36‐item Short Form questionnaire to assess the participant's wellbeing and functional health |
| Starting date | July 2011 |
| Contact information | Michael McKee, MD, FRCS(C), 416‐864‐5880, mckeem@smh.ca Emil Schemitsch, MD, FRCS(C), 416‐864‐6003, schemitsche@smh.ca |
| Notes |
GCS: Glasgow Coma Score; ICU: intensive care unit; ORIF: open reduction and internal fixation; PaO2/FIO2 ratio: arterial oxygen partial pressure to fractional inspired oxygen ratio; PEEP: positive end‐expiratory pressure; RCT: randomized controlled trial.
Differences between protocol and review
We intended to report mortality in two groups ‐ early (all‐cause mortality within 30 days of trauma) and late (all‐cause mortality more than 30 days following trauma). We identified three studies for this review; in one study there were no deaths (Tanaka 2002), in one study the deaths occurred prior to hospital discharge but the time of measurement was not specified (Granetzny 2005), and one study reported a single death of a participant at 92 days postinjury (Marasco 2013). We combined all mortality data in the review.
Based on feedback from the peer reviewers, we added four new secondary outcomes when completing the review: tracheostomy, duration of mechanical ventilation, length of intensive care unit stay, and length of hospital stay. These outcomes were identified as important, and we decided to include them in the review before seeing the results.
An information size was estimated for the primary outcome.
We inserted more information on type of participants, studies, and definition of deformity as requested by one of the peer reviewers.
Contributions of authors
Antonio José Maria Cataneo: provided a clinical perspective, wrote the review.
Frederico HS de Oliveira: wrote the review.
Daniele C Cataneo: provided a clinical perspective, wrote the review.
Karine A Arruda: wrote the review and inserted data into Review Manager.
Regina El Dib: provided a methodological perspective, wrote the review.
Paulo Eduardo de Olivira Carvalho: provided methodological and clinical perspective, wrote the review.
Sources of support
Internal sources
-
São Paulo State University (UNESP), Brazil.
Assistance with computers with access to the Internet, and library and database use.
External sources
No sources of support supplied
Declarations of interest
Frederico HS de Oliveira: none known.
Daniele C Cataneo: none known.
Karine A Arruda: none known.
Antonio José Maria Cataneo: none known.
Regina El Dib: none known.
Paulo Eduardo de Olivira Carvalho: none known.
New
References
References to studies included in this review
Granetzny 2005 {published data only}
- Granetzny A, El‐Aal MA, Emam E, Shalaby A, Boseila A. Surgical versus conservative treatment of flail chest. Evaluation of the pulmonary status. Interactive Cardiovascular and Thoracic surgery 2005;4:583‐7. [PUBMED: 17670487] [DOI] [PubMed] [Google Scholar]
Marasco 2013 {published data only}
- Marasco SF, Davies AR, Cooper J, Varma D, Bennett V, Nevill R, et al. Prospective randomized controlled trial of operative rib fixation in traumatic flail chest. Journal of American College of Surgeons 2013;on line:1‐9. [PUBMED: 23415550] [DOI] [PubMed] [Google Scholar]
Tanaka 2002 {published data only}
- Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. Journal of Trauma Injury, Infection, and Critical Care 2002;52:727‐32. [PUBMED: 11956391] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ahmed 1995 {published data only}
- Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation and ventilation. Journal of Thoracic and Cardiovascular Surgery 1995;110:676‐80. [DOI] [PubMed] [Google Scholar]
Althausen 2011 {published data only}
- Althausen PL, Shannon S, Watts C, Thomas K, Bain MA, Coll D, et al. Early surgical stabilization of flail chest with locked plate fixation. Journal of Orthopaedic Trauma 2011;25(11):641‐7. [DOI] [PubMed] [Google Scholar]
Balci 2005 {published data only}
- Balci AE, Eren S, Cakir O, Eren MN. Open fixation in flail chest: review of 64 patients. Asian Cardiovascular and Thoracic Annals 2005;12:11‐5. [DOI] [PubMed] [Google Scholar]
Borrelly 1985 {published data only}
- Borrelly J, Grosdidier G, Wack B. The stabilization of the flail chest by sliding staples [Traitement chirurgical de I'instabilité pariétale thoracique par I'attelle‐agrafeà glissières (AAG)]. Revue de Chirurgie Orthopédique 1985;71:241‐50. [PubMed] [Google Scholar]
Karev 1997 {published data only}
- Karev DV. Operative management of the flail chest. Operative management of the flail chest. Wiadomo Lekarskie 1997;50:205‐8. [PubMed] [Google Scholar]
Kim 1981 {published data only}
- Kim M, Brutus P, Christides C, Dany F, Paris H, Gastinne H, et al. Compared results of flail chests treatments: standard internal pneumatic stabilization, new technics of assisted ventilation, osteosynthesis [Résultats compares du traitement des volets thoraciques: stabilization penumatique interne classique, nouvelle modalité de la ventilation artificielle, agrafage]. Journal de Chirurgie 1981;118(8‐9):499‐503. [PubMed] [Google Scholar]
Lardinois 2001 {published data only}
- Lardinois D, Krueger T, Dusmet M, Ghisletta N, Gugger M, Ris HB. Pulmonary function testing after operative stabilisation of the chest wall for flail chest. European Journal of Cardio‐Thoracic Surgery 2001;20(3):496‐501. [DOI] [PubMed] [Google Scholar]
Nirula 2006 {published data only}
- Nirula R, Allen B, Layman R, Falimirski ME, Somberg LB. Rib fracture stabilization in patients sustaining blunt chest injury. American Surgeon 2006;72:307‐9. [DOI] [PubMed] [Google Scholar]
Ohresser 1972 {published data only}
- Ohresser P, Amoros JF, Leonardelli M, Sainty JM, Vanuxem P, Autran P, et al. The functional sequelae of cIosed thoracic traumatisms (about 92 cases) [Les sequelles fonctionnelles des traumatismes fermes du thorax (a propos de 92 observations)]. Le Poumon et le Coeur 1972;28:145‐50. [PubMed] [Google Scholar]
Teng 2009 {published data only}
- Teng JP, Cheng YG, Ni D, Pan RH, Cheng YS, Zhu ZJ, et al. Outcomes of traumatic flail chest treated by operative fixation versus conservative approach. Journal of the Shanghai Jiaotong University (Medical Science) 2009;29:1495‐8. [Google Scholar]
Voggenreiter 1998 {published data only}
- Voggenreiter G, Neudeck F, Aufmkolk M, Obertacke U, Neuerburg KPS. Operative chest wall stabilization in flail chest ‐ outcomes of patients with or without pulmonary contusion. Journal of American College of Surgeons 1998;187:130‐8. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT01147471 {unpublished data only}
- NCT01147471. Flail chest: early operative fixation versus non‐operative management ‐ a prospective randomized study. clinicaltrials.gov/ct2/show/NCT01147471 (accessed 26 July 2015).
NCT01308697 {unpublished data only}
- NCT01308697. Operative versus non operative management of flail chest: a randomized controlled feasibility study. clinicaltrials.gov/ct2/show/NCT01308697 (accessed 26 July 2015).
NCT01367951 {unpublished data only}
- NCT01367951. A multi centered randomized controlled trial of operative versus non‐operative treatment of acute, unstable chest wall injuries. clinicaltrials.gov/ct2/show/NCT01367951 (accessed 26 July 2015).
Additional references
Adkins 1968
- Adkins PC, Groff DB 3rd, Blades B. Experiences with metal struts for chest wall stabilization. Annals of Thoracic Surgery 1968;5(3):246‐54. [DOI] [PubMed] [Google Scholar]
Avery 1956
- Avery EE, Benson DW, Morch ET. Critically crushed chests; a new method of treatment with continuous mechanical hyperventilation to produce alkalotic apnea and internal pneumatic stabilization. Journal of Thoracic Surgery 1956;32(3):291‐311. [PubMed] [Google Scholar]
Baker 1974
- Baker SP, O'Neil B, Haddon W. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma 1974;14(3):187‐96. [PubMed] [Google Scholar]
Besson 1982
- Besson A, Segesser F. Blunt trauma of the chest wall. A Colour Atlas of Chest Trauma and Associated Injuries. 1. Vol. 1, Weert, Netherlands: Wolfe Medical Publications Ltd, 1982:153‐98. [Google Scholar]
Ciraulo 1994
- Ciraulo DL, Marini CP, Lloyd GT, Fisher J. Flail chest as a marker for significant injuries. Journal of the American College of Surgeons 1994;178(5):466‐70. [PubMed] [Google Scholar]
Clark 1988
- Clark GC, Schecter WP, Trunkey DD. Variables affecting outcome in blunt chest trauma: flail chest vs. pulmonary contusion. Journal of Trauma 1988;28(3):298‐304. [DOI] [PubMed] [Google Scholar]
Dehghan 2014
- Dehghan N, Mestral C, McKee MD, Schemitsch EH, Nathens A. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. Journal of Trauma and Acute Care Surgery 2014;76(2):462‐8. [DOI] [PubMed] [Google Scholar]
Di Fabio 1995
- Fabio D, Benetti D, Benvenuti M, Mombelloni G. Surgical stabilization of post‐traumatic flail chest. Our experience with 116 cases treated. Minerva Chirurgica 1995;50(3):227‐33. [PubMed] [Google Scholar]
Ebert 1967
- Ebert PA. Physiologic principles in the management of the crushed‐chest syndrome. Monographs in the Surgical Sciences 1967;4(2):69‐91. [PubMed] [Google Scholar]
Freedland 1990
- Freedland M, Wilson RF, Bender JS, Levison MA. The management of flail chest injury: factors affecting outcome. Journal of Trauma 1990;30(12):1460‐8. [DOI] [PubMed] [Google Scholar]
Fullerton 1995
- Fullerton DA, Grover FL. Blunt trauma: trauma to the chest wall. In: Pearson GF, Deslauries J, Ginsberg RJ, Hiebert CA, McKneally MF, Urschel HC Jr editor(s). Thoracic Surgery. 1. New York, NY: Churchill Livingstone, 1995:1555‐60. [Google Scholar]
Galan 1992
- Galan G, Peñalver JC, París F, Caffarena JM Jr, Blasco E, Borro JM, et al. Blunt chest injuries in 1696 patients. European Journal of Cardio‐Thoracic Surgery 1992;6(6):284‐7. [DOI] [PubMed] [Google Scholar]
Ginsberg 1977
- Ginsberg RJ, Kostin RF. New approaches to the management of flail chest. Canadian Medical Association Journal 1977;116(6):613‐5. [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Jones 1980
- Jones KW. Thoracic trauma. Surgical Clinics of North America 1980;60(4):957‐81. [DOI] [PubMed] [Google Scholar]
Judet 1973
- Judet R. Costal osteosynthesis. Revue de Chirurgie Orthopedique et Reparatrice de l'Appareil Moteur 1973;Suppl 1:334‐5. [PubMed] [Google Scholar]
Lau 2006
- Lau J, Ioannidis JPA, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. BMJ 2006;333(7568):597‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leinicke 2013
- Leinicke JA, Elmore L, Freeman BD, Colditz GA. Operative management of rib fractures in the setting of flail chest: a systematic review and meta‐analysis. Annals of Surgery 2013;258(6):914‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
LoCicero 1989
- LoCicero J 3rd, Mattox KL. Epidemiology of chest trauma. Surgical Clinics of North America 1989;69(1):15‐9. [DOI] [PubMed] [Google Scholar]
Maloney 1961
- Maloney JV Jr, Schmutzer KJ, Raschke E. Paradoxical respiration and "pendelluft". Journal of Thoracic and Cardiovascular Surgery 1961;41:291‐8. [PubMed] [Google Scholar]
Montgomery 1985
- Montgomery AB, Stager MA, Carrico CJ, Hudson LD. Causes of mortality in patients with the adult respiratory distress syndrome. American Review of Respiratory Disease 1985;132(3):485‐9. [DOI] [PubMed] [Google Scholar]
Moore 1975
- Moore BP. Operative stabilization of nonpenetrating chest injuries. Journal of Cardiovascular Surgery 1975;70(4):619‐30. [PubMed] [Google Scholar]
París 1975
- París F, Tarazona V, Blasco E, Cantó A, Casillas M, Pastor J, et al. Surgical stabilization of traumatic flail chest. Thorax 1975;30(5):521‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pate 1989
- Pate JW. Chest wall injuries. Surgical Clinics of North America 1989;69(1):59‐70. [DOI] [PubMed] [Google Scholar]
Pepe 1984
- Pepe PE, Hudson LD, Carrico CJ. Early application of positive end‐expiratory pressure in patients at risk for the adult respiratory‐distress syndrome. New England Journal of Medicine 1984;311(5):281‐6. [DOI] [PubMed] [Google Scholar]
Perna 2010
- Perna V, Morera R. Prognostic factors in chest traumas: a prospective study of 500 patients. Cirugía Espanola 2010;87(3):165‐70. [DOI] [PubMed] [Google Scholar]
Pocock 1983
- Pocock SJ. Clinical Trials: a Practical Approach. Chichester: John Wiley & Sons Ltd, 1983. [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre. Review Manager (RevMan). Version 5.1. Copenhagen: The Cochrane Collaboration, 2011.
Richardson 1982
- Richardson JD, Adams L, Flint LM. Selective management of flail chest and pulmonary contusion. Annals of Surgery 1982;196(4):481‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schmit‐Neuerburg 1982
- Schmit‐Neuerburg KP, Weiss H, Labitzke R. Indication for thoracotomy and chest wall stabilization. Injury 1982;14(1):26‐34. [DOI] [PubMed] [Google Scholar]
Shackford 1976
- Shackford SR, Smith DE, Zarins CK, Rice CL, Virgilio RW. The management of flail chest. A comparison of ventilatory and nonventilatory treatment. American Journal of Surgery 1976;132(6):759‐62. [DOI] [PubMed] [Google Scholar]
Shackford 1981
- Shackford SR, Virgilio RW, Peters RM. Selective use of ventilator therapy in flail chest injury. Journal of Thoracic and Cardiovascular Surgery 1981;81(2):194‐201. [PubMed] [Google Scholar]
Slobogean 2013
- Slobogean GP, MacPherson CA, Sun T, Pelletier ME, Hameed SM. Surgical fixation vs nonoperative management of flail chest: a meta‐analysis. Journal of the American College Surgeons 2013;216(2):302‐11.e1. [DOI] [PubMed] [Google Scholar]
Sterne 2002
- Sterne JA, Jüni P, Schulz KF, Altman DG, Bartlett C, Egger M. Statistical methods for assessing the influence of study characteristics on treatment effects in 'meta‐epidemiological' research. Statistics in Medicine 2002;15‐21(11):1513‐24. [DOI] [PubMed] [Google Scholar]
Thomas 1978
- Thomas AN, Blaisdell FW, Lewis FR Jr, Schlobohm RM. Operative stabilization for flail chest after blunt trauma. Journal of Thoracic and Cardiovascular Surgery 1978;75(6):793‐801. [PubMed] [Google Scholar]
Todd 1989
- Todd TR, Keenan R. Ventilatory support of the postoperative surgical patient. In: Shilelds TW editor(s). General Thoracic Surgery. 3rd Edition. Philadelphia: Lea & Febiger, 1989:325‐42. [Google Scholar]
Trinkle 1975
- Trinkle JK, Richardson JD, Franz JL, Grover FL, Arom KV, Holmstrom FM. Management of flail chest without mechanical ventilation. Annals of Thoracic Surgery 1975;19(4):355‐63. [DOI] [PubMed] [Google Scholar]
Wilson 1977
- Wilson RF, Murray C, Antonenko DR. Nonpenetrating thoracic injuries. Surgical Clinics of North America 1977;57(1):17‐36. [DOI] [PubMed] [Google Scholar]


