Abstract
Preterm birth is a risk factor for early experience of pain. Despite advances in neonatal care, evidence‐based knowledge of the importance of adequate pain management and strong international guidelines for assessment and treatment of neonatal pain, only 10% of sick term and preterm infants were assessed for pain and stress on a daily basis. The aim of this quality improvement (QI) project is evaluation of implemented guidelines for pain assessment and management, and increased parental involvement in a Norwegian single‐family room NICU. Method: The different steps of the project entailed translation of the English version of COMFORTneo, development and implementation of guidelines with flowcharts for pain management, and pain assessment certification of the interprofessional staff. Part two of the project is supervision of the interprofessional staff in parental involvement in stress‐ and painful procedures. Our study showed that one year after implementation, 88.8% of the COMFORTneo assessments were performed according to the pain management guidelines. The staff used the flowcharts to assess, treat and reassess pain and stress. There was a high interrater reliability with linearly weighted Cohen's kappa values ranging from 0.81 to 0.95, with a median of 0.90. In addition, our study showed increased parental involvement in procedures, from 50.3% before to 82.3% after the quality improvement project. The success of this quality improvement project is explained by systematic use of flowcharts and implemented guidelines for pain management, interprofessional collaboration, and cultural change agents. Theoretical lectures and practical bedside supervision to interprofessional staff increased parental involvement in stress‐ and painful procedures.
Keywords: pain management, preterm infant, quality improvement, single‐family room
The aim of this quality improvement (QI) project is evaluation of implemented guidelines for pain assessment and management and increased parental involvement in a Norwegian single‐family room (SFR) NICU. The main steps were translation and implementation of the COMFORTneo scale and development of flowcharts and pain management guidelines. The study showed high compliance to guidelines, high COMFORTneo assessment inter‐rater reliability, and increased parental involvement in procedures.

1. INTRODUCTION
Every year, an estimated 15 million infants are born preterm, and the number is increasing. 1 Preterm birth is a risk factor which exposes the immature brain to a sequence of adverse effects during a period of developmental vulnerability. 2 A large amount of the preterm and ill term infant population are hospitalized in a neonatal intensive care unit (NICU) after birth due to immaturity, illness, and the need for life support. During hospitalization, a preterm and ill term infant often undergoes several painful procedures daily. 3 In less than half of the procedures, the infant receives an intervention to reduce pain. 3 In addition, they often experience prolonged pain and stress related to medical technical support, nursing care, noisy environments, and parental separation.
Repeated painful procedures together with the prolonged experience of pain and stress could have negative short‐ and long‐term consequences for the vulnerable infant. 2 Pain can cause cardiovascular instability 4 and may lead to behavioral changes, disturbed feeding, and reduced ability to sleep. 5 Several studies show that painful experiences in infants have long‐term negative effects on altered postnatal growth, 6 neurobehavioral‐ 7 , 8 and brain development. 9
Preterm infants have weak expression of pain and stress and lack the ability to self‐report. Therefore, international clinical guidelines recommend systematic assessment of pain with clinical tools, 4 , 10 non‐pharmacological interventions, developmental supportive care, and parental involvement in procedures. 10 , 11 , 12 , 13 Despite advances in neonatal care, evidence‐based knowledge of the importance of adequate pain management and strong international guidelines for assessment and treatment of neonatal pain, only 10% of preterm and ill term infants were assessed for pain and stress on a daily basis. 11
The aim of this quality improvement (QI) project is evaluation of implemented guidelines for pain assessment and management, and increased parental involvement in a Norwegian single‐family room NICU.
2. METHODS
2.1. Setting
The setting is a 17‐bed, level II single‐family room (SFR) NICU in Norway. The unit provides care for infants with a gestational age (GA) of 28 weeks or more, and infants born before 28 weeks are transferred from a level IIII university hospital when no longer in need of high‐technological intensive care. NICU staff consists of neonatologists, pediatric trainees, nurse assistants, registered nurses, clinical nurse specialists, and midwives. The unit offers SFRs with two different levels of care to all infants and their families. A family care room is provided for infants in a stable phase, while an intensive care room is provided for infants in need of breathing support and intensive medical treatment and care. SFRs give parents an opportunity to stay with their infants 24/7. Tandberg et al found that mothers in our unit were present 20 hours daily versus seven hours daily in the reference open bay unit; both units were in Norway, and the parents were given the same possibilities due to Norwegian social benefits. 14 Parents are encouraged to participate in daily care, which includes support to the infant in stress‐ and painful procedures, but this has not been systematically implemented at the time of the QI project. The unit had no systematic assessment of pain and lacked guidelines for treatment of pain prior to the project. Participation in the EUROPAIN study 11 raised awareness of the importance of improved pain assessment and management to the preterm and ill term infant population, which led to planning of the QI project.
2.2. The QI project framework
An interprofessional Pain Group, with four registered nurses, two clinical nurse specialists and a consultant neonatologist was established in August 2015, as well as a collaboration with a university college educating neonatal nurse specialists. The project was conducted via a stepwise approach based on a Plan‐Do‐Study‐Act (PDSA) framework (Table 1). The PDSA framework was introduced by the Vermont Oxford Network to improve neonatal intensive care. 15 This structured framework supports practice change as follows: Plan a desired change, execute the elements of the change (do), study the change by measured outcomes, and then adjust on the gained information (act) to begin another cycle.
TABLE 1.
Quality improvement project: a stepwise approach
| Steps | Description |
|---|---|
| 1. Assessment of the problem |
Founded in NICU management Common understanding of inadequate pain management Establishment of an interprofessional Pain Group |
| 2. Literature review |
Choice on pain assessment tool Pain management for prolonged and procedural pain Parental involvement in procedures |
| 3. Development of a pain management strategy |
PDSA cycle as a QI framework Certification of the Pain Group Translation of the English version of COMFORTneo Development of a flowchart Development of comprehensive material for staff education Development of procedures for treatment of pain and stress |
| 4. Education of the NICU staff |
Certification of the staff with theory and bedside supervision Development of a cultural guide |
| 5. Implementation of new pain tool and guidelines |
Systematic use of COMFORTneo, flowcharts, and protocols Kick off Daily supervision, report, and discussion during the medical rounds Parental involvement in procedures |
| 6. Monitoring of quality improvement data |
Staff interrater reliability Compliance with pain management guidelines Parental involvement in procedures |
| 7. Continually improvement |
Increased pain assessment Revised flowchart |
Abbreviations: NICU, Neonatal intensive care unit; PDSA, Plan‐Do‐Study‐Act; QI, Quality improvement.
2.3. The COMFORTneo scale
A literature review on pain assessment instruments and pain management strategies in sick term and preterm infants was conducted. The COMFORTneo scale was chosen because it is validated to assess prolonged pain and stress. 16 , 17 It is an unidimensional tool successfully implemented in all Danish NICUs. 18 , 19 The COMFORTneo scale is a modified version of the COMFORT scale and is eligible for use in infants from 23 weeks of GA to one month postnatal age. The observer must have visual access to the face and body during the period of observation. The score value is summarized after a two‐minute observation period of the following seven different behavioral variables: alertness, calmness, respiratory response, crying, movement, facial tone, and muscle tone. Each variable is rated on a Likert scale ranging from 1 to 5, where 1 is minimal and 5 is maximal activity. The most extreme appearance observed should be taken into account. Since respiratory response applies to ventilated infants and crying to spontaneously breathing infants, the observer rates only six variables, with total scores ranging from 6 to 30. COMFORTneo score values between 9 and 13 indicate no pain or stress, values between 14 and 21 indicate moderate pain or stress, and values between 22 and 30 indicate severe pain or stress. Score values below 9 in sedated infants indicate oversedation. 16
The COMFORTneo scale includes the Numeric Rating Scale (NRS) to distinguish between pain and stress (NRS pain and NRS stress). 16 The NRS assessment is based on the nurses’ evaluation and knowledge of GA, current treatment, and severity of illness. NRS is performed on a scale ranging from 0 to 10, with 0 to 3 indicating no pain or stress, 4 to 6 indicating moderate pain or stress, and 7 to 10 indicating severe pain or stress.
Two authors (LTL and SS) translated the English version of the COMFORTneo scale into Norwegian following Wild's 10 steps (Table 2). 20 The scale was pilot tested for content validity and clinical utility in a focus group interview.
TABLE 2.
Translation of the English version of COMFORTneo to Norwegian following Wild's 10 step 20
| Step 1. Preparation | Contact with Dr VanDijk, developer of the COMFORTneo, who gave the permission for translation of the English version. 16 Recruitment of translators and nurses for the cognitive interview. |
|---|---|
| Step 2. Forward translation | 2 neonatal nurses translated the instrument from English into Norwegian. Both were bilingual in English and Norwegian and worked in a level 3 NICU. |
| Step 3. Reconciliation | The two different translated versions were discussed and reconciled into a single forward translation. |
| Step 4. Back translation | The back translation was carried out by a native English speaking professional translator. The translation was more literal than conceptual. |
| Step 5. and Step 6. Back translation review and harmonization | LTL and SS analyzed the back translation. Several items varied from the original instrument. The back translation review included a skype meeting with the instrument developer, where conceptual issues were discussed. In the harmonization, the concepts of the translated items were discussed. The Danish version and the Norwegian version of the COMFORTneo scale were scrutinized, with the purpose of deciding on the best possible wording. |
| Step 7. and Step 8. Cognitive debriefing and review, involving pilot testing of content and clinical utility | A focus group interview was conducted to assess item comprehensibility. 6 neonatal nurses specializing in neonatology and experienced in pain assessment participated. Three were familiar with the Danish version of the COMFORTneo. The nurses scored a neonate undergoing a painful procedure (heelprick) and discussed thoroughly all items of the scale including NRS. They found that the COMFORTneo scale is user friendly and comprehensive. |
| Step 9. and Step 10. Proofreading and final report. | LTL and SS finalized the last steps. The Norwegian version was published on the COMFORTneo website. |
Abbreviation: NICU, Neonatal intensive care unit.
A local guide for interpretation of behavior was developed by the Pain Group to ensure high interrater reliability, with cultural adjustment. After the evaluation phase, the guide was adjusted and modified.
2.4. Non‐pharmacological interventions and parental involvement in procedures
Non‐pharmacological interventions 21 is defined in our study as an adjusted environment with reduced light and noise, as well as interventions to support the infant and promote self‐regulation. The most commonly used nurse‐driven interventions are positioning, swaddling, pacifier, sucrose, and wrapping the infant in a warm cloth. Parental presence has a positive impact on the treatment and alleviation of pain during procedures. 22 Parental involvement is defined in our study as comfort measures like holding, rocking, provide pacifier and sucrose, breastfeeding, skin‐to‐skin care, and sensorial saturation. 21
Parents are encouraged to comfort the infant during painful procedures. Skin‐to‐skin holding, often combined with non‐nutritive sucking and sucrose, are interventions introduced to parents whenever they are ready to participate .
2.5. Development of pain management guidelines
The pain management guidelines (PMG) include flowcharts for assessment and treatment of pain, and procedures for non‐pharmacological interventions and pharmacological treatment. To ensure that every pain assessment led to adequate interventions, two flowcharts for pain assessment‐ and management were constructed using the available literature with cut‐off values for pain, treatment and time of reassessment 23 , 24 (Supporting information). PMG recommended a minimum of one assessment per day for infants admitted in family care rooms and three assessments per day for infants in intensive care rooms. The first assessment should be performed within 2 hours after admission. Additional assessments should be carried out if pain or stress were suspected, and after non‐pharmacological interventions and pharmacological treatments. Scores above the threshold for pain and stress were to be followed by non‐pharmacological interventions, reassessment, pharmacological treatment, and reassessment in accordance with the flowcharts until the score was below threshold. 23 , 24 During the first week of implementation, the comprehension of the flowcharts was tested with an evaluation of the registered assessments and interventions. The journals of the first 15 patients were checked to see whether the interprofessional staff had understood and followed the flowchart algorithms. An evaluation of the PMG led to a change in the recommended COMFORTneo assessment frequency. The number of assessments was increased from one to three for infants in family rooms. The 2‐minute assessment period was perceived as a useful overall observation of the infant by the nursing staff. Furthermore, we decided that all admitted infants should be systematically assessed for pain and stress every eight hours as a minimum.
2.6. COMFORTneo implementation
The interprofessional Pain Group visited NICU at Rigshospitalet, Denmark, for a two‐day lecture and certification. Each member of the Pain Group performed 100 assessments prior to the visit and certification. The Pain Group nurses supervised the staff with half‐day theoretical lectures on pain assessment, pain management and parental involvement in procedures, and half‐day bedside training and conference. The certification was based on 10 assessments in 10 different infants, performed simultaneously but independently, together with a certified Pain Group nurse. Each certification was measured by the linearly weighted Cohen's kappa value calculated from 10 paired assessments. 25 If the linearly weighted Cohen's kappa value was below 0.65, the staff had to do additional training and paired assessments. The implementation of the COMFORTneo scale as part of the PMG and parental involvement in procedures was carried out from February 2017. T‐shirts, posters, and social media were used to bring attention to and create enthusiasm for the project. Oral‐adjusted information was given to parents. The COMFORTneo scale and flowcharts were laminated and available in all patient rooms and working areas. The daily presence of Pain Group members encouraged and supervised the staff's assessment of pain and stress, the use of NRS, and parental involvement in procedures. COMFORTneo scores were systematically reported and discussed for all patients during medical rounds.
2.7. Facilitating parental involvement in procedures
The PMG emphasized the importance of parental involvement. The Pain Group provided theoretical lectures on the subject of non‐pharmacological interventions and parental involvement in procedures, practical supervision 24/7 and daily reflections to the interprofessional staff during the implementation. The focus on ergonomic equipment to facilitate parental involvement was determinant for the implementation. New flexible chairs for the interprofessional staff and tables for equipment to place in the parents’ beds were introduced to make it more practical and comfortable for both parents and staff.
2.8. Evaluation of the QI project
Three studies were conducted to evaluate the impact of the QI project.
Study 1. Staff interrater reliability. The COMFORTneo certification included 10 assessments of 10 different patients together with a Pain Group nurse. The interrater reliability was calculated using Cohen's kappa calculation with linear weighting. Cohen's kappa provides a measure of the degree to which two people have an independent but simultaneous correlation in the interpretation of pain and stress. 25
Study 2. Compliance with PMG. A prospective study of all admitted infants was conducted one year after the QI project from March 1st to March 31st, 2018. Demographic data and compliance with the implemented flowchart and pain management guidelines for prolonged pain were registered. Compliance with the guidelines was defined as the percentage of scores assessed according to the flowchart.
Study 3. Registration of parental involvement in procedures. A one month pre‐study was conducted from August 15th to September 15th , 2016 and a one month post‐study from March 1st to March 31st, 2018. Demographic data were retrieved from the Norwegian medical quality registry. Nurses were asked to register every procedure which they perceived as stress‐ and painful, whether the parents were involved or not. In addition, the nurses were asked to list the reasons why the parents were not involved in the procedure.
3. RESULTS
Study 1. Staff interrater reliability. Three nurse assistants, 60 registered nurses, 20 clinical nurse specialists, and seven neonatologists working at the unit at the time of the QI project were certified. Linearly weighted Cohen's kappa values ranged from 0.81 to 0.95, with a median of 0.90. The members of the pain Group had a median value >0.95.
Study 2. Compliance with PMG. Patients’ demographic is available in Table 3. All admitted infants were systematically assessed with the COMFORTneo scale.
TABLE 3.
Demographics Study 2 & 3
|
Pre‐study † Patients (n = 37) |
Post‐study ‡ Patients (n = 52) |
|
|---|---|---|
| Weight at birth (g), mean (min‐max) | 2545 (638‐4460) | 2649 (570‐4440) |
| Gestational age (weeks), mean (min‐max) | 34.1 (24.6‐42.0) | 35.6 (26.6‐42.2) |
| Post‐menstrual age (weeks), mean (min‐max) | 34.5 (26.2‐43.4) | 37.2 (31.4‐42.3) |
| Gastric tube§, n (%) | 25 (67.6) | 41 (78.9) |
| Ventilation support§, n (%) | ||
| High flow | 4 (10.8) | 10 (19.2) |
| CPAP | 4 (10.8) | 6 (11.5) |
| Mechanical ventilation | 1 (2.7) | 0 (0) |
| PVC, n (%) | 18 (48.6) | 12 (23.1) |
Abbreviations: CPAP, Continuous positive airway pressure; PVC, peripheral venous cannula.
†Information was retrieved from the Norwegian medical quality registry
‡Same patients in study
In total, 75.0% of the infants had at least one score over 13 (moderate or severe pain or stress), and 34.6% had at least one score over 21 (severe pain or stress). A total of one quarter of the infants received pharmacological pain treatment. A total number of 932 COMFORTneo scores were registered with a median number of 9,5 IQR [5‐27] for the 52 patients (Figure 1).
FIGURE 1.
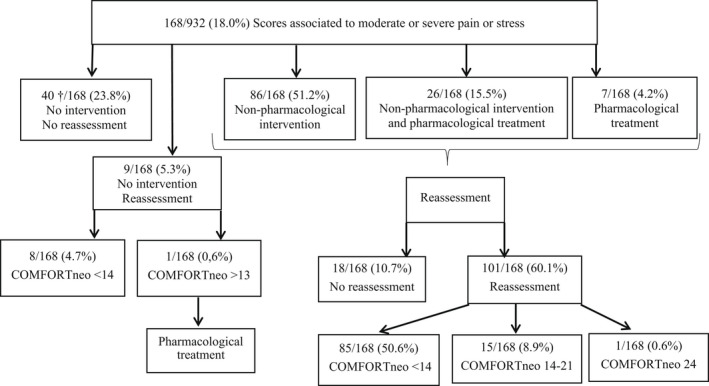
Results study 2 (compliance to pain management guidelines). †75.0% of the scores were 14 and 90.0% of the scores were associated with low NRS pain or low NRS stress
168 (18.0%) scores were associated with pain or stress, whereas 114 (12.2%) were associated with moderate and 54 (5.8%) with severe pain and stress. As recommended, the staff used the flowchart to systematically assess and act to reduce pain and stress and reassess (Supplementary material). A total of 88.8% of the registered assessments were done according to the guidelines. All COMFORTneo assessments were paired with an NRS pain and stress expert opinion. In all, 99.9% of COMFORTneo scores under 14 were associated with NRS pain under 4 and 99.7% were associated with NRS stress under 4. However, 35.7% of COMFORTneo scores over 13 were associated with NRS pain over 3 and 52.4% were associated with NRS stress over 3.
Study 3. Parental involvement in procedures. Patients’ demographic is available in Table 3. One or both parents were involved in 50.3% of the registered stress‐ and painful procedures before the QI project and 82.3% after (Table 4). Four procedures were perceived by the nurses as pain‐ and stressful before the QI project, whereas 16 after (Supplementary material). The reasons registered for parents lack of involvement before the QI project was reluctance from staff, parents sleeping during nighttime or parents not being present in the unit. After the QI project, the reasons for parents´ lack of involvement partly changed. The extern laboratory staff preferred not to involve the parents, the parents were asleep or not present.
TABLE 4.
Results Study 3
| Pre‐study Pain‐ or stressful procedures with parental involvement § | Post‐study Pain‐ or stressful procedures with parental involvement § | |
|---|---|---|
| Venipuncture, n/N (%) | 66/101 (65.3) | 133/153 (86.9) |
| Insertion of gastric tube, n/N (%) | 19/38 (50.0) | 33/45 (73.3) |
| Insertion of PVC, n/N (%) | 0/31 (0.0) | 19/27 (70.4) |
| Airway suction, n/N (%) | 24/47 (51.1) | 19/25 (76.0) |
| Total of procedures, n/N (%) | 109/217 (50.2) | 204/250 (81.6) |
Abbreviation: PVC, Peripheral venous cannula
†n/N: number of painful or stressful procedures with parental involvement/total amount of painful or stressful procedures.
§Parental involvement.
4. DISCUSSION
The QI project results showed high compliance with guidelines and increased parental involvement in pain‐ and stressful procedures. The compliance with guidelines in our study remained high one year after the QI project. It is nevertheless important to keep evaluating the implementation as sustainability may decrease over the years. Aukes et al implemented a protocol for pain assessment‐ and management and conducted a prospective evaluation study. They reported a compliance with guidelines of 60.2% six years after implementation. 23 The high compliance in our study could be due to the flowcharts with specific actions for each level of pain and stress, and protocols for non‐pharmacological interventions and pharmacological treatment.
Structured pain assessment‐ and management strategies are shown to reduce pain, 26 increase non‐pharmacological interventions, 27 and increase opiate prescriptions. 28 Flowcharts with algorithms for pain management contributed to better communication and collaboration between nurses and doctors, which is seen as a strong predicator for successful pain management in NICUs. 29 Nevertheless, a planned, systematic, and interprofessional implementation process impacted positively on the study result.
NRS was included in the flowchart to help caregiving nurses to separate pain from stress. The NRS score is based upon the nurses` expert opinion and evaluation of the infants’ GA, treatment, and medical history. 16 The results showed that only one‐third of the high COMFORTneo scores were associated with a high NRS pain, and one‐half of the high COMFORTneo scores were associated with a high NRS stress. The results displayed the importance of comparing behavioral assessment with an NRS evaluation of the infants’ pain and stress. Patients with high COMFORTneo scores associated with low NRS pain and stress received either no intervention or non‐pharmacological interventions followed by a moderate or low COMFORTneo score (Figure 1). High COMFORTneo score values associated with high NRS pain or high NRS stress interpretation received interventions according to the implemented pain management guidelines. This may indicate that the combination of COMFORTneo assessment paired with a NRS evaluation may contribute to a more targeted pain‐ and stress management in preterm infants.
4.1. Increased parental involvement in painful procedures
Parents were registered as more actively involved in procedures one year after the QI project, which could be explained by the education and supervision of staff, and information provided to parents on how to support their infant. A study showed that parents wanted to be involved in support of their infant during painful and stressful procedures, but they needed individualized information and emotional support in order to make it accessible and understandable. 30 Lack of information and suitable facilities posed barriers to parental involvement. 31 The parental presence was high during the two study periods, due to the SFR accommodations. Our pre‐post study indicated that parents were involved in painful procedures if they were included by the staff. None of the parents included in the study were reluctant to participate in the procedures when present in the unit and awake. This finding suggests that staff knowledge and attitude toward parental involvement play an important role in whether parents engage in pain‐ and stressful procedures. The nurses reported in the pre‐study registration that “staff were not comfortable with the parents participating in the procedure.” Facilitating parental involvement in stress‐ and painful procedures requires security and a certain level of experience with the procedure. If the nurse or doctor feel insecure in procedure performance, they may be more likely to reject parental presence and involvement. The fact that the study population was healthy and not critically ill may also have contributed to the overall high parental involvement.
The nurses reported an increased number of procedures to be pain‐ and stressful for the infant after the QI project implementation. The study did not investigate the staff´s attitudes or knowledge toward pain‐ and stressful procedures and parental involvement in comforting the infant. The change in perception toward whether a procedure is stress‐ and painful for the infant could be due to the provided education and practical supervision of the staff. It is essential that healthcare professionals are aware of the risk of infants experiencing pain during care and treatment to ensure adequate pain alleviation and treatment. 32 The project increased the nurses’ and doctors’ awareness of procedural pain and the importance of parental involvement.
4.2. Practice change in SFR NICUs
The members of the interprofessional Pain Group acted as cultural change agents and stakeholders in the QI project, which was perceived as crucial for achieving compliance and successful implementation. 33 The Pain Group involved the staff from the beginning of the QI project. Both doctors and nurses received the same information and certification, and they were all committed to follow the pain management guidelines. To change the NICU culture and impact daily practice, involvement and support at all levels are needed. The implementation of PMG and parents as active caretakers requires a change in staff attitudes. In a changing process, it could be important to build upon current routines and make improvements based on the existing workflow. 34 The COMFORTneo assessments and use of flowcharts were integrated into the daily routines. It was crucial that the staff perceived the PMG as a positive supplement rather than a burden and source of extra workload. 34 The non‐pharmacological interventions included in the PMG were based on the nurses’ already existing practice. A cultural change was portrayed as a key element in securing sustainability of practice improvements. 33 , 35 , 36 Change can be even more challenging in SFR NICUs where staff work in a more isolated manner and with reduced peer‐to‐peer support. Education, certification, high interrater reliability, and discussion on medical rounds contributed to the practice change with improvement in pain management and parental involvement in stress‐ and painful procedures. The members of the Pain Group are currently active. They are in charge of the education and certification of recently employed staff, as well as members of pain groups in 8/21 NICUs in Norway.
5. LIMITATIONS
The implementation was a QI project, and we intended to measure whether the staff followed the detailed flowcharts and guidelines for pain management. Our results do not say anything about the actual impact on the infants and we perceive this as a limitation. Parental presence and involvement in pain‐ and stressful procedures will be more complex and demanding for both the parents and the staff when the infants are in need of high intensive treatment and care. It may be seen as a limitation for the study results, both on implementing flowcharts and guidelines for pain and stress and parental involvement in procedures that the infant population are overall healthy and not critically ill. The pre‐ and post‐study registration of parental involvement in procedures have some missing data regarding the reported reasons why parents were not involved in procedures (Results section, study 3). We understand that the registered data on parental involvement in procedures are questionable. The registration was carried out one month before and one month after the implementation. All admitted infants had available registration sheets for the nurses and the Pain group followed up with detailed description of when and how to register on the sheet. It is possible that there were some missing data in the registration, and we fully see the limitation. The purpose was to measure whether the nurse's perception of pain and stress changed during the QI project, and we believe that the post‐registration show a positive change in the nurses´ attitudes toward the matter, but we also agree upon the limitation in how the registration was carried out.
6. CONCLUSION
All preterm and ill term infants should be systematically assessed for pain and stress, even if they are not critically ill or receiving high intensive care. Systematic pain assessment is an important step toward adequate pain management. The success of this quality improvement project is explained by the systematic use of guidelines for pain management including flowcharts, interprofessional collaboration, and cultural change agents. Parental presence in SFR NICUs, in countries with social benefits for parents after child birth, makes it possible for staff to include the parents as caregivers in stress‐ and painful procedures, but this depends on the interprofessional staff's knowledge and attitude, and the NICU culture. Systematic implementation with theoretical lectures and practical bedside supervision increased parental involvement in pain‐ and stressful procedures in our SFR NICU.
Supporting information
Supplementary Material
Supplementary Material
Lyngstad LT, Steinnes S, Le Marechal F. Improving pain management in a neonatal intensive care unit with single‐family room—A quality improvement project. Paediatr Neonatal Pain. 2022;4:69–77. doi: 10.1002/pne2.12075
Abbreviations: FCC, Family‐Centered Care; GA, Gestational Age; NICU, Neonatal Intensiv Care Unit; NRS, Numeric Rating Scale; PDSA, Plan‐Do‐Study‐Act; PMA, Post‐Menstrual Age; QI, Quality Improvement Project; SFR, Single‐family room.
REFERENCES
- 1. Beck S, Wojdyla D, Say L, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88:31‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Valeri BO, Holsti L, Linhares MB. Neonatal pain and developmental outcomes in children born preterm: a systematic review. Clin J Pain. 2015;31(4):355‐362. [DOI] [PubMed] [Google Scholar]
- 3. Cruz MD, Fernandes AM, Oliveira CR. Epidemiology of painful procedures performed in neonates: a systematic review of observational studies. Eur J Pain. 2016;20(4):489‐498. [DOI] [PubMed] [Google Scholar]
- 4. Anand K. Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med. 2001;155(2):173‐180. [DOI] [PubMed] [Google Scholar]
- 5. Abdulkader HM, Freer Y, Garry EM, Fleetwood‐Walker SM, McIntosh N. Prematurity and neonatal noxious events exert lasting effects on infant pain behaviour. Early Hum Dev. 2008;84(6):351‐355. [DOI] [PubMed] [Google Scholar]
- 6. Vinall J, Miller SP, Chau V, Brummelte S, Synnes AR, Grunau RE. Neonatal pain in relation to postnatal growth in infants born very preterm. Pain. 2012;153(7):1374‐1381. [DOI] [PubMed] [Google Scholar]
- 7. Grunau RE, Holsti L, Haley DW, et al. Neonatal procedural pain exposure predicts lower cortisol and behavioral reactivity in preterm infants in the NICU. Pain. 2005;113(3):293‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Doesburg SM, Chau CM, Cheung TP, et al. Neonatal pain‐related stress, functional cortical activity and visual‐perceptual abilities in school‐age children born at extremely low gestational age. Pain. 2013;154(10):1946‐1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ranger M, Chau CM, Garg A, et al. Neonatal pain‐related stress predicts cortical thickness at age 7 years in children born very preterm. PLoS One. 2013;8(10):e76702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pediatrics AAo, Fetus, Committee N . Prevention and management of pain in the neonate: an update. Pediatrics. 2006;118(5):2231‐2241. [DOI] [PubMed] [Google Scholar]
- 11. Anand KJ, Eriksson M, Boyle EM, et al. Assessment of continuous pain in newborns admitted to NICU s in 18 E uropean countries. Acta Paediatr. 2017;106(8):1248‐1259. [DOI] [PubMed] [Google Scholar]
- 12. Johnston C, Campbell‐Yeo M, Disher T, et al. Skin‐to‐skin care for procedural pain in neonates. Cochrane Database Syst Rev. 2017;2(2):Cd008435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McNair C, Yeo MC, Johnston C, Taddio A. Nonpharmacological management of pain during common needle puncture procedures in infants: current research evidence and practical considerations. Clin Perinatol. 2013;40(3):493‐508. [DOI] [PubMed] [Google Scholar]
- 14. Tandberg BS, Frøslie KF, Flacking R, Grundt H, Lehtonen L, Moen A. Parent‐Infant Closeness, parents' participation, and nursing support in single‐family room and open bay NICUs. J Perinat Neonatal Nurs. 2018;32(4):E22‐E32. [DOI] [PubMed] [Google Scholar]
- 15. Horbar JD, Plsek PE, Leahy K, Ford P. The vermont oxford network: improving quality and safety through multidisciplinary collaboration. NeoReviews. 2004;5(2):e42‐e49. doi: 10.1542/neo.5-2-e42 [DOI] [Google Scholar]
- 16. van Dijk M, Roofthooft DW, Anand KJ, et al. Taking up the challenge of measuring prolonged pain in (premature) neonates: the COMFORTneo scale seems promising. Clin J Pain. 2009;25(7):607‐616. [DOI] [PubMed] [Google Scholar]
- 17. Hummel P, Puchalski M, Creech S, Weiss M. Clinical reliability and validity of the N‐PASS: neonatal pain, agitation and sedation scale with prolonged pain. J Perinatol. 2008;28(1):55‐60. [DOI] [PubMed] [Google Scholar]
- 18. Sygeplejersken O, Hovedstaden K, Midtjylland K, Nordjylland K, Sjælland K, Syddanmark K. Oversættelse af et smertescoringsredskab til nyfødte. Sygeplejersken. 2014;4:84‐88. [Google Scholar]
- 19. Stenkjaer RL, Pedersen PU, Hundrup YA, Weis J. Evaluation of NICU nurses' competence in pain assessment 5 years after implementation of the COMFORTneo scale. Adv Neonatal Care. 2019;19(5):409‐415. [DOI] [PubMed] [Google Scholar]
- 20. Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for patient‐reported outcomes (PRO) Measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8(2):94‐104. [DOI] [PubMed] [Google Scholar]
- 21. McNair C, Campbell‐Yeo M, Johnston C, Taddio A. Nonpharmacologic management of pain during common needle puncture procedures in infants: current research evidence and practical considerations: an update. Clin Perinatol. 2019;46(4):709‐730. [DOI] [PubMed] [Google Scholar]
- 22. Johnston C, Barrington KJ, Taddio A, Carbajal R, Filion F. Pain in canadian NICUs: have we improved over the past 12 years? Clin J Pain. 2011;27(3):225‐232. [DOI] [PubMed] [Google Scholar]
- 23. Aukes DI, Roofthooft DWE, Simons SHP, Tibboel D, van Dijk M. Pain management in neonatal intensive care: evaluation of the compliance with guidelines. Clin J Pain. 2015;31(9):830‐835. [DOI] [PubMed] [Google Scholar]
- 24. Harris J, Ramelet A‐S, van Dijk M, et al. Clinical recommendations for pain, sedation, withdrawal and delirium assessment in critically ill infants and children: an ESPNIC position statement for healthcare professionals. Intensive Care Med. 2016;42(6):972‐986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20(1):37‐46. [Google Scholar]
- 26. Eriksson M, Campbell‐Yeo M. Assessment of pain in newborn infants. Semin Fetal Neonatal Med. 2019;24(4):101003. doi: 10.1016/j.siny.2019.04.003. Epub 2019 Apr 4. PMID: 30987943. [DOI] [PubMed] [Google Scholar]
- 27. Anand KJ. Prevention and management of procedural pain in the neonate: an update. Pediatrics. 2016;137(2):e20154271. [DOI] [PubMed] [Google Scholar]
- 28. Deindl P, Giordano V, Fuiko R, et al. The implementation of systematic pain and sedation management has no impact on outcome in extremely preterm infants. Acta Paediatr. 2016;105(7):798‐805. [DOI] [PubMed] [Google Scholar]
- 29. Latimer MA, Johnston CC, Ritchie JA, Clarke SP, Gilin D. Factors affecting delivery of evidence‐based procedural pain care in hospitalized neonates. J Obstet Gynecol Neonatal Nurs. 2009;38(2):182‐194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bäcke P, Hjelte B, Hellström Westas L, Ågren J, Thernström BY. When all I wanted was to hold my baby—The experiences of parents of infants who received therapeutic hypothermia. Acta Paediatr. 2021;110(2):480‐486. [DOI] [PubMed] [Google Scholar]
- 31. Palomaa A‐K, Korhonen A, Pölkki T. Factors influencing parental participation in neonatal pain alleviation. J Pediatr Nurs. 2016;31(5):519‐527. [DOI] [PubMed] [Google Scholar]
- 32. Cong X, McGrath JM, Cusson RM, Zhang D. Pain assessment and measurement in neonates: an updated review. Adv Neonatal Care. 2013;13(6):379‐395. [DOI] [PubMed] [Google Scholar]
- 33. Lehtonen L, Axelin A. Medical champions can make a difference in initiating culture change. Acta Paediatr. 2016;105(9):994‐995. doi: 10.1111/apa.13482. PMID: 27514001. [DOI] [PubMed] [Google Scholar]
- 34. Reavey DA, Haney BM, Atchison L, Anderson B, Sandritter T, Pallotto EK. Improving pain assessment in the NICU: a quality improvement project. Adv Neonatal Care. 2014;14(3):144‐153. [DOI] [PubMed] [Google Scholar]
- 35. Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: medical research council guidance. BMJ. 2015;350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Soni A, Amin A, Patel DV, et al. The presence of physician champions improved kangaroo mother care in rural western India. Acta Paediatr. 2016;105(9):e390‐e395. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Supplementary Material


