Abstract
Background:
Immunizations for emergency medical services (EMS) professionals during pandemics are an important tool to increase the safety of the workforce as well as their patients. The purpose of this study was to better understand EMS professionals’ decisions to receive or decline a COVID-19 vaccine.
Methods:
We conducted a cross-sectional analysis of nationally certified EMS professionals (18–85 years) in April 2021. Participants received an electronic survey asking whether they received a vaccine, why or why not, and their associated beliefs using three validated scales: perceived risk of COVID-19, medical mistrust, and confidence in the COVID-19 vaccine. Data were merged with National Registry dataset demographics. Analyses included descriptive analysis and multivariable logistic regression (OR, 95% CI). Multivariate imputation by chained equations was used for missingness.
Results:
A total of 2,584 respondents satisfied inclusion criteria (response rate = 14%). Overall, 70% of EMS professionals were vaccinated. Common reasons for vaccination among vaccinated respondents were to protect oneself (76%) and others (73%). Common reasons for non-vaccination among non-vaccinated respondents included concerns about vaccine safety (53%) and beliefs that vaccination was not necessary (39%). Most who had not received the vaccine did not plan to get it in the future (84%). Hesitation was most frequently related to wanting to see how the vaccine was working for others (55%). Odds of COVID-19 vaccination were associated with demographics including age (referent <28 years; 39–50 years: 1.56, 1.17–2.08; >51 years: 2.22, 1.64–3.01), male sex (1.26, 1.01–1.58), residing in an urban/suburban area (referent rural; 1.36, 1.08–1.70), advanced education (referent GED/high school and below; bachelor’s and above: 1.72, 1.19–2.47), and working at a hospital (referent fire-based agency; 1.53, 1.04–2.24). Additionally, vaccination odds were significantly higher with greater perceived risk of COVID-19 (2.05, 1.68–2.50), and higher vaccine confidence (2.84, 2.40–3.36). Odds of vaccination were significantly lower with higher medical mistrust (0.54, 0.46–0.63).
Conclusion:
Despite vaccine availability, not all EMS professionals had been vaccinated. The decision to receive a COVID-19 vaccine was associated with demographics, beliefs regarding COVID-19 and the vaccine, and medical mistrust. Efforts to increase COVID-19 vaccination rates should emphasize the safety and efficacy of vaccines.
Keywords: COVID-19, vaccine hesitancy, workforce safety, patient safety, medical mistrust
Introduction
Large-scale vaccination for SARS-CoV2, the virus that causes COVID-19, is a crucial step toward controlling the international pandemic (1). Vaccinations are also a tool to improve safety of workers at high risk of occupational exposure to COVID-19 (2), as well as patient safety (3). However, many are hesitant to receive the vaccine. In the United States, prior evidence before the release of the vaccine suggested that 52–57% of adults indicated willingness to take the vaccine when available (4–6), but 23–40% reported being unsure (5, 6), and approximately 7–14% indicated that they were unlikely or definitely did not intend to receive the COVID-19 vaccine (5–7). Along these lines, despite widespread availability of the vaccine in the US, only 76% of adults have received at least one dose of a COVID-19 vaccine as of September 2021 (8).
Emergency Medical Services (EMS) professionals are often a first contact for many people in the US accessing healthcare, making vaccination of this workforce particularly important to reduce the risk of COVID-19 infection for these professionals and the patients they treat. Yet few studies to date have examined vaccine hesitancy among EMS professionals. In Germany, prior to the release of vaccines, an evaluation of EMS personnel found that 57% were willing to be vaccinated and 27.6% were undecided (9). A similarly timed study of firefighters, paramedics, and emergency medical technicians (EMTs) in the US found that 48.2% reported high acceptability of a COVID-19 vaccine, while 24% were unsure, and 27% indicated low acceptability (10). Prior work has noted higher EMS professional acceptance levels of other vaccines that are associated with occupational hazards in this field (e.g., 78% for hepatitis B vaccine (11)).
As vaccine availability has improved and multiple studies have demonstrated vaccine efficacy and effectiveness (12–16), further evaluations of the attitudes and drivers of vaccine hesitancy are needed. COVID-19 vaccines have been available to EMS professionals in the US since January 2021, but the prevalence of vaccination and extent of hesitancy for this group is unknown. Therefore, the purpose of this study was to evaluate the prevalence of vaccination and hesitancy among EMS professionals to improve our understanding of factors that may be influencing the decision to receive or decline a COVID-19 vaccine.
Methods
Study Design, Population, and Setting
We designed a survey that aimed to assess vaccination prevalence and vaccine hesitancy among a sample of EMS professionals across the US. The survey asked questions about vaccination status (for COVID-19 and for the 2020–2021 flu vaccine), demographics, workforce characteristics, and beliefs concerning COVID-19 and vaccination. Beliefs were measured using three validated scales of perceived COVID-19 risk (17), confidence in COVID-19 vaccines (18) and mistrust of healthcare organizations (medical mistrust) (19). Inclusion criteria included all nationally registered EMTs and paramedics who responded to the survey and reported their COVID-19 vaccination status.
Survey distribution began on April 20th, 2021, which was after vaccinations had been released to all Centers for Disease Control and Prevention (CDC) phase 1a and 1b groups [including emergency medical services personnel (20–22)] and after the Department of Health and Human Services had released a directive on March 17th, 2021 to vaccinate all adults due to sufficient vaccine supply (23). Thus, all EMS professionals had had an opportunity to be vaccinated prior to study participation.
We distributed this survey to civilian EMTs and paramedics aged 18–85 years old in the National Registry of Emergency Medical Technicians’ (National Registry) database. The National Registry is the national certification agency, maintaining the largest database of EMS providers in the US, with contact information available for approximately 420,000 EMS professionals at the time of the study (24). The National Registry provides initial EMS certification in greater than 95% of U.S. states and territories. Based on a sample size calculation (n=(z2*p*(1−p))/c2 where n represents sample size, z the 95% confidence interval z score, p an alpha of 0.05, and c the 3% margin of error) we determined that 1,560 responses from EMS professionals would be needed to make estimates with 95% confidence. After including an inflation factor (0.08) to account for anticipated low response rates based on previous studies conducted with this population (25, 26), we selected a simple random sample of 19,062 nationally-certified EMS professionals drawn from the National EMS Certification database to ensure a sufficient number of respondents.
Emails containing a unique link to the questionnaire were sent to this random sample of EMS professionals. Participants were not advised of the study goals or objectives. After the initial survey release, follow-up reminder messages were sent approximately one and two weeks after the original email invitation, following the tailored Dillman methodology (27). Completion of this survey had no bearing on National EMS Certification. The American Institutes for Research’s Institutional Review Board approved this study, and the study was deemed exempt from further review.
An abbreviated non-responder survey was also administered to assess non-response bias. The abbreviated questionnaire asked whether respondents had received a COVID-19 vaccine. The survey was open for 1 week and received 1,125 responses, yielding approximately 92% power to detect a clinically meaningful 10% difference between respondents and non-respondents.
Measures
COVID-19 vaccination status was determined by asking participants “Have you received a COVID-19 vaccine?” Based on their response to this vaccination status item, using survey logic, participants were asked why they did or did not receive a COVID-19 vaccine. Participants were able to mark-all-that-apply on a list of response options (see Appendix A, online supplemental). Participants who were vaccinated were also asked whether they received the vaccine as soon as they were eligible or if they waited. If a participant said they waited (or were waiting), they were asked why using a mark-all-that-apply format (see Appendix A, online supplemental). Participants who were unvaccinated were asked whether they planned to receive the vaccine or not.
We assessed perceived risk of COVID-19 by adapting a prior scale of perceived threat of COVID-19 and perceived risk of contracting COVID-19 from the Understanding America Survey (17). Our adapted version asked participants to rate the severity of their perceived risk for 8 items associated with COVID-19 infection on a four-point response scale (1 = almost no chance, 4 = very high chance). (See Appendix A, online supplemental for survey instrument). We measured confidence in the COVID-19 vaccine with 6 items adapted from the Oxford COVID-19 Vaccine Confidence and Complacency scale (18) using a 5-point scale (1 = least confidence, 5 = most confidence). We used the validated, 7-item Medical Mistrust Index (19) to measure medical mistrust. We adapted this measure to use a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree).
Demographic characteristics were collected from respondents’ National EMS Certification database profile and linked to the survey results using a common identification number. Demographics of currently nationally-certified EMS professionals included sex, age, race/ethnicity, urbanicity (residing in urban/suburban vs. rural), EMS certification level (EMT or Paramedic) and education level. The nominal variable of sex was categorically designated as male or female. Age was analyzed as a continuous variable and categorized by quartiles for modeling. Due to the small proportion of minority EMS professionals, race and ethnicity were dichotomized to non-minority (white, non-Hispanic) or minority. The minority category included any person who self-identified as Black or African American, Asian, Hispanic or Latino, Asian or Native Hawaiian or Pacific Islander. Educational level was categorized into less than high school/completed high school/obtained GED, some college, Associate’s degree, and Bachelor’s degree or above. For the agency type where respondents worked, responses were categorized into fire, governmental non-fire, hospital, private, or other; of note, although some EMS professionals work at multiple agencies, the database captures their primary agency.
Analysis
Survey results were merged with demographic characteristics from the National Registry dataset and all identifying data were removed generating a deidentified analysis dataset. From this deidentified dataset, descriptive statistics were evaluated for demographics, vaccine receipt, and rationale for vaccine decision. For Likert scales, items were reverse coded when necessary, and mean composites were computed.
Missingness was low overall with the highest rates found in three areas of workforce demographics: agency type (22.95%), education level (16.68%), and urbanicity (16.14%). Missing data were handled using multivariate imputation by chained equations with 100 imputed datasets.
Subsequently, to examine the relationships between variables, a multivariable logistic regression model was fit for each imputed dataset to describe the associations between COVID-19 vaccine receipt (as the dependent variable) and respondent demographics, workforce characteristics, perceived risk of COVID-19, COVID-19 vaccine confidence, and medical mistrust (as predictor variables). Model fit was evaluated using the Hosmer-Lemeshow test and receiver operating characteristic curves. The reported coefficients and standard errors were calculated using the coefficient values and standard errors from the imputed datasets, and they can be interpreted in the same way as the coefficient values from a single logistic regression model based on complete data.
Results
Descriptive Statistics
A total of 2,584 participants satisfied study inclusion criteria and responded to the survey (response rate = 14%). As shown in Table 1, participants were approximately two-thirds male, largely white and Non-Hispanic, and ranged in age from 18 to 83 years. Over half of the participants had an Associate’s degree or higher, and approximately two-thirds lived in urban/suburban areas. Participants were most frequently full-time EMS employees (73.3%), but also included those who were part-time (12.4%) and volunteers (14.4%). Participants had an average of 14 years of experience; both Advanced Life Support (ALS) and Basic Life Support (BLS) personnel were represented. Respondents worked in a variety of agency types, and most worked in 911 services. Demographics were largely similar between unvaccinated and vaccinated participants with some notable exceptions: vaccinated participants skewed older and were more educated.
Table 1.
Demographic and workforce characteristics of participants.
| Characteristic | Overall | Non-vaccinated (N = 780, 30.2%) | Vaccinated (N = 1,804, 69.8%) |
|---|---|---|---|
| Male – n (%) | 1701 (66.7) | 493 (64.4) | 1205 (67.7) |
| Age – n (%) | |||
| <28 years | 649 (25.1) | 232 (29.8) | 416 (23.1) |
| 29–38 years | 667 (25.8) | 223 (28.7) | 443 (24.6) |
| 39–50 years | 640 (24.8) | 191 (24.6) | 448 (24.9) |
| > 51 years | 627 (24.3) | 132 (17.0) | 495 (27.5) |
| Race and ethnicity – n (%) | |||
| White, Non-Hispanic | 2170 (87.0) | 661 (87.9) | 1506 (86.7) |
| All others | 323 (13.0) | 91 (12.1) | 232 (13.3) |
| Certification – n (%) | |||
| Basic life support | 1072 (41.5) | 343 (44.1) | 728 (40.4) |
| Advanced life support | 1512 (58.5) | 435 (55.9) | 1075 (59.6) |
| Educational Level – n (%) | |||
| HS/GED | 249 (11.6) | 92 (14.6) | 157 (10.3) |
| Some College | 690 (32.0) | 248 (39.5) | 441 (29.0) |
| Associate’s | 462 (32.0) | 140 (22.3) | 321 (21.1) |
| Bachelor’s | 561 (26.1) | 117 (18.6) | 443 (29.1) |
| Master’s/Doctorate | 191 (8.9) | 31 (4.9) | 160 (10.5) |
| Urbanicity – n (%) | |||
| Urban/suburban | 1365 (63.7) | 773 (73.7) | 1028 (66.3) |
| Rural | 779 (36.3) | 276 (26.3) | 523 (33.7) |
| Agency type – n (%) | |||
| Fire | 642 (32.2) | 208 (36.0) | 434 (30.8) |
| Private | 532 (26.7) | 143 (24.8) | 388 (27.5) |
| Government non-fire | 320 (16.1) | 97 (16.8) | 222 (15.7) |
| Hospital | 271 (13.6) | 61 (10.6) | 210 (14.9) |
| Other* | 226 (11.4) | 68 (11.8) | 157 (11.1) |
| Service type – n (%) | |||
| 911 | 728 (69.9) | 227 (72.3) | 500 (68.8) |
| All others** | 314 (30.1) | 87 (27.7) | 227 (31.2) |
| Years in EMS – mean (IQR) | 14.3 (18.0) | 12.4 (17.0) | 15.0 (20.0) |
| Employment status – n (%) | |||
| Full-time | 1409 (73.3) | 422 (77.0) | 985 (71.8) |
| Part-time | 238 (12.4) | 63 (11.5) | 174 (12.7) |
| Volunteer | 276 (14.4) | 63 (11.5) | 213 (15.5) |
Abbreviations: HS/GED, high school/General Educational Development; IQR, Interquartile range; MIHCP, Mobile Integrated Healthcare or Community Paramedicine.
Note.
Other includes air medical, tribal, military, and other;
Other includes medical transport, 911 & medical transport, clinical services, MIHCP, and other.
In terms of beliefs concerning COVID-19 and vaccination, participants generally felt that COVID-19 was of low risk to them (Median [Mdn] = 1.88, Interquartile range (IQR) = 0.88; n = 2488), had moderate confidence in COVID-19 vaccines (Mdn = 3.80, IQR = 1.00; n = 2378), and had moderate levels of medical mistrust (Mdn = 3.14, IQR = 1.14; n = 2204).
Prevalence of COVID-19 Vaccination/Rationale for COVID-19 Vaccine Decision
Overall, 1804 (69.8%) EMS professionals reported having received a COVID-19 vaccine and 780 (30.2%) indicated they had not received one. This is similar to the proportions in our non-responder survey: of 1,111 EMS professionals who completed the non-responder survey, 26.82% (n = 298) reported not having had a COVID-19 vaccine and 73.18% (n = 813) reported they had. Most EMS professionals who received the vaccine reported they did so as soon as they could (n = 1455, 80.7%), but some (n = 339, 18.7%) noted they had waited to get it. The most common reasons cited for getting the vaccine were protection for oneself (75.7%) and protection for others (72.8%) (Table 2). The most common reasons for not getting the vaccine as soon as eligible was to see how it was working for other people (55.9%) and to allow higher risk people to have the chance to get it first (27.2%) (see Table 3).
Table 2.
Rationale for either receiving the vaccine or choosing not to receive the vaccine.
| COVID-19 Vaccine status | Reason | n (%) |
|---|---|---|
| Yes, received vaccine (n = 1804, 69.8%) | ||
| I chose to get it for my own protection | 1365 (75.7) | |
| I chose to get it to protect others | 1312 (72.8) | |
| I was required or pressured to get it for work | 241 (13.4) | |
| I was required or pressured to get it for other activities | 88 (4.9) | |
| I was pressured to get it by my family or household members | 63 (3.5) | |
| I got it for another reason | 150 (8.3) | |
| No, did not receive vaccine (n = 780, 30.2%) | ||
| I do not think it is safe | 411 (52.8) | |
| I do not think I need it | 303 (38.9) | |
| Plan to get it, but waiting | 67 (8.6) | |
| I have a previous history of vaccine reaction/allergy | 51 (6.6) | |
| My religion or culture prevents me from getting it | 37 (4.8) | |
| My doctor recommended I do not get it | 33 (4.2) | |
| I had difficulty scheduling or getting an appointment | 28 (3.6) | |
| I have a health condition that prevents me from getting it | 24 (3.1) | |
| I have a fear of needles and/or the pain of the shot | 14 (1.8) | |
| Another reason | 258 (33.2) | |
Table 3.
Reasons for waiting to get the vaccine, for those who did not get it right away.
| Reason | Yes, got vaccine but hesitated (N = 338) n (%) | No, still waiting to get vaccine (N = 67) n (%) |
|---|---|---|
| To see how it was working for other people | 189 (55.9) | 37 (55.2) |
| Want higher risk people to have the chance to get it first | 92 (27.2) | 20 (29.9) |
| COVID-19 positive or exposed/quarantined | 24 (7.1) | 14 (20.9) |
| Waiting for another type of COVID-19 vaccine not yet available | N/A | 4 (6.0) |
| Waiting for a COVID-19 vaccine from another manufacturer not yet available | N/A | 6 (9.0) |
| Waiting until after pregnancy | 3 (0.9) | 1 (1.5) |
| Waiting until done breastfeeding | 1 (0.3) | 1 (1.5) |
| Waiting until after the first trimester of pregnancy | 0 (0.0) | 0 (0.0) |
| Another reason | 113 (33.4) | 18 (26.9) |
Among respondents who did not receive the COVID-19 vaccine, most did not plan to do so (n = 636, 83.5%); some indicated they were going to get it, but were still waiting (126, 16.5%). Reasons for not getting the vaccine were most commonly related to concerns about its safety (52.8%) or the perception that the vaccine was not needed (38.9%) (see Table 2). Those who were still waiting to get the vaccine most frequently indicated that they were still waiting to see how it was working for others (55.2%), wanted higher risk people to have the chance to get it first (29.9%), or were COVID-19 positive or exposed/quarantined (20.9%) (Table 3).
Predictors of Vaccine Receipt
The odds of COVID-19 vaccination significantly increased with age (referent <28 years; 39–50 years: adjusted OR (aOR) = 1.56, 95% CI = 1.17–2.08; >51 years: aOR = 2.22, 95% CI = 1.64–3.01), male sex (aOR = 1.26, 95% CI = 1.01–1.58), living in an urban/suburban area (referent rural; aOR = 1.36, 95% CI = 1.08–1.70), having advanced education (referent GED/high school and below; bachelors and above: aOR = 1.72, 95% CI = 1.19–2.47), and working at a hospital (referent fire-based agency; aOR = 1.53, 95% CI = 1.04–2.24). Additionally, the odds of vaccination were significantly higher for respondents with a greater mean perceived risk of COVID-19 (aOR = 2.05, 95% CI = 1.68–2.50), and with a higher mean score for vaccine confidence (aOR = 2.84, 95% CI = 2.40–3.36). The odds of vaccination were significantly lower among respondents with higher levels of medical mistrust (aOR = 0.54, 95% CI = 0.46–0.63). See Figure 1.
Figure 1.
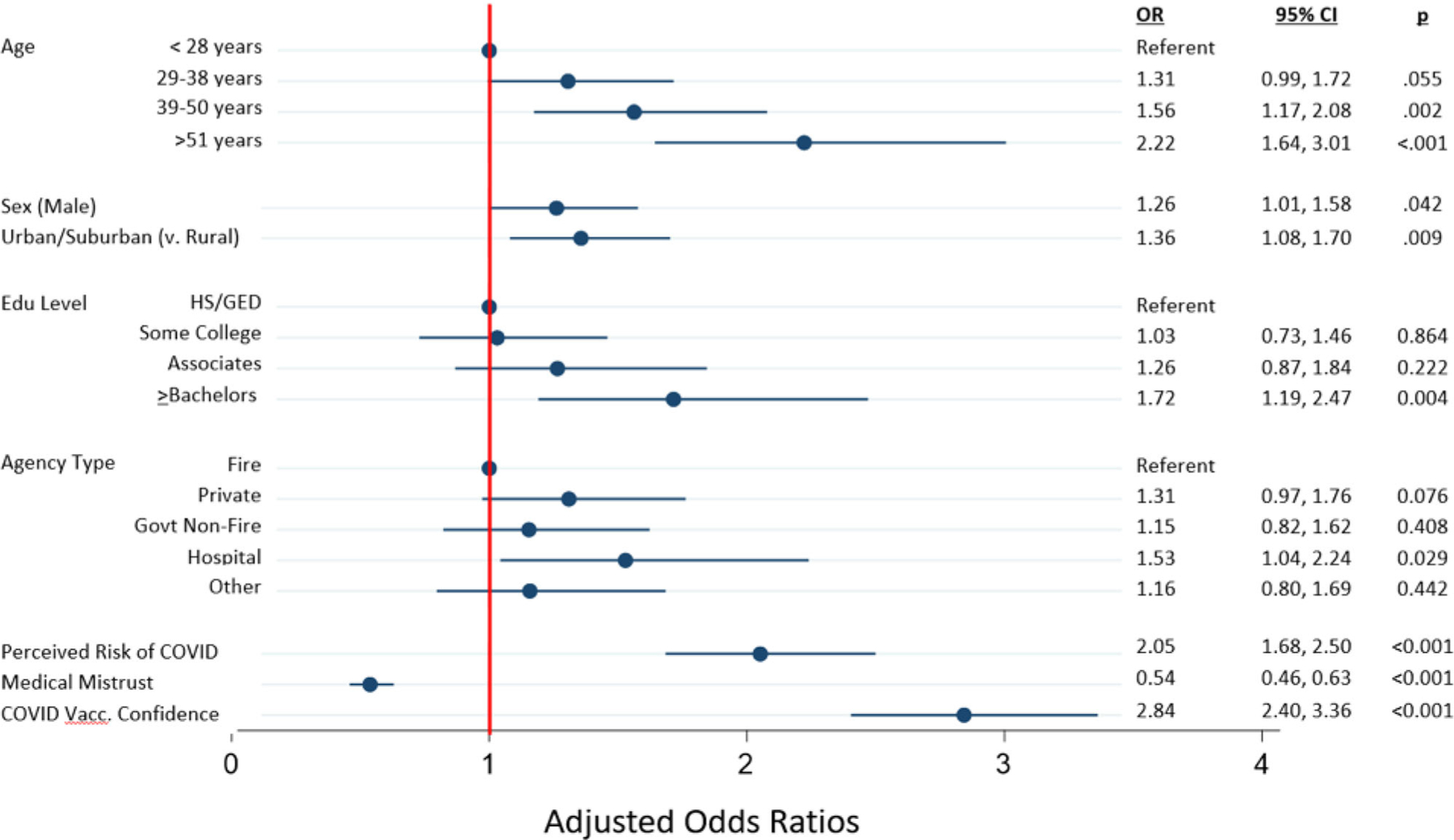
Forest plot. Abbreviations: Edu, Education; Govt, Government; Vacc, Vaccine.
Discussion
EMS professionals play a critical role at the front line of the pandemic as they triage and treat patients with suspected COVID-19 infection while trying to prevent the spread of infection. Due to the responsibilities of their positions, EMS professionals are at increased risk for acquiring a COVID-19 infection (28). Yet, despite their heightened risk of exposure and vaccine availability, our results indicate that nearly one-third (30%) of EMS professionals had not received a COVID-19 vaccine at the time of our study. Notably, this rate is lower than vaccination rates of healthcare workers for other occupational hazards such as Hepatitis B (78% of EMS workers vaccinated in one study (11)), and measles/mumps/rubella (up to 95% medical and health professions students vaccinated in one study (29)). Vaccine hesitancy has been a major barrier to controlling the pandemic, especially in the context of the more contagious Delta variant that now accounts for the vast majority of COVID-19 cases in the U.S. (30). Further, vaccine hesitancy in the EMS population can result in harmful outcomes among these providers, as well as a temporary reduction in the EMS workforce due to the time required to quarantine and/or recover. Such exposure can also result in further spread of the disease to patients, EMS colleagues, and emergency department (ED) providers and staff. We also found that EMS professionals’ decisions about getting vaccinated were associated with both demographic and EMS characteristics as well as their perceived risk of COVID-19, the extent of their mistrust in medicine, and their beliefs about the safety of the COVID-19 vaccine.
Our results echo findings from other studies that evaluated COVID-19 vaccine acceptability among EMS professionals and firefighters that were conducted prior to the release of vaccines. In comparison to these earlier findings where over 50% of those respondents reported uncertain or low acceptability of the COVID-19 vaccine when it became available (10), our results are encouraging in that 70% of surveyed EMS professionals reported having received a vaccine. Nonetheless, vaccination prevalence remains far short of emerging recommendations that all healthcare workers should be vaccinated (31), making our findings about the different factors influencing vaccination decisions timely and important.
In this study we also noted three strong associations with COVID-19 vaccination: perceived risk, medical mistrust, and vaccine confidence. For EMS professionals, occupational risks are perceived as career-associated, making this population risk tolerant (32). As such, EMS professionals may see COVID-19 infection as just another risk that they accept on the job (32). In addition, among those respondents who did not receive the vaccine, nearly 39% reported that they did not think they needed the vaccine, perhaps reflecting the sentiment that as a generally younger and healthier group, EMS professionals perceived less risk of serious illness caused by infection. Nonetheless, those respondents with heightened perceived risk had higher odds of being vaccinated.
Medical mistrust was also associated with respondents’ reported decisions to not receive a COVID-19 vaccine. Medical mistrust has been demonstrated in prior work to impact decisions to utilize healthcare (19), including decisions about vaccines (33). As the work of EMS personnel involves multiple points of interaction with the health system, this may provide EMS professionals with a more nuanced view of healthcare than the general public that, in turn, might impact their level of trust in the system. Our finding that high levels of medical mistrust were associated with decreased odds of receiving a COVID-19 vaccine suggests that campaigns to increase vaccination rates among EMS professionals may need to be led by organizations outside the healthcare system. Further work is needed to better understand these issues in the EMS population. Outside of the EMS population, prior work has found that parents were less likely to give their sons the human papillomavirus (HPV) vaccine after watching an advertisement if they perceived the ad was from a drug company (34), indicating that mistrust of medical and pharmaceutical institutions does play a role in vaccination decisions.
Additionally, confidence in the COVID-19 vaccine was strongly associated with respondents’ receipt of a COVID-19 vaccine. Notably, there have been numerous attempts to improve the public’s perceptions of and confidence in COVID-19 vaccines (35), as well as efforts to disseminate evidence-based guidance to support messaging and communication about the vaccines (35, 36). One recent evaluation of EMS professionals noted that as a result of extensive time and resources devoted to educate this group and increase vaccine awareness, confidence in the vaccine increased, the number of vaccinations also increased (37). While promising, results across our and other studies highlight the challenge of promoting COVID-19 vaccination in the face of medical mistrust. Simplifying the message to emphasize the safety and necessity of COVID-19 vaccines may be effective for EMS professionals, but this remains a critical area for further study to increase vaccination rates in the future.
Lastly, to examine the possibility that COVID-19 vaccinations were driven primarily by behaviors and attitudes toward vaccines more broadly, we also examined the prevalence of receiving a vaccine for the 2020–2021 flu season. We found that there was only small-to-moderate overlap in the group who rejected both vaccines: 43.2% of those who did not get a flu vaccine did get a COVID-19 vaccine, and 17.2% of those who did get a flu vaccine did not get a COVID-19 vaccine. This suggests there are differences in decision-making about the two vaccines.
There are a number of limitations associated with this evaluation. First, the data collected in this study are self-reported from EMS professionals concerning their vaccinations and both demographic and agency-level characteristics, thus may result in misclassification of respondents and social desirability bias. Our sample was also limited to nationally certified EMS professionals and, since this certification is not required by all states, these results may not be generalizable. In addition, compared to a demography study of EMS professionals (38), our respondents included more individuals with a Bachelor’s or higher degrees (35% vs 26%), fewer EMS personnel working in Fire Departments (32% vs 48%), and more working in governmental non-fire agencies (16% vs 12%) and hospitals (14% vs 11%). Though small, these differences may suggest that national population estimates may have lower vaccination rates that our study population. Fourth, our survey response rate was relatively low. While this response rate is typical for an EMS population (25, 26, 39–41), a low rate could increase the possibilities of response and selection bias. However, recent work has suggested these concerns may be unfounded (42), and our analysis of a survey of non-responders demonstrated no difference in our primary outcome of vaccination, giving us confidence in the results we report. Finally, our survey was conducted at a single time point and captured respondents’ answers and beliefs at that time. Recognizing that the COVID-19 pandemic remains dynamic in the US, a reevaluation of this population may be needed to reflect evolving perspectives about COVID-19 and COVID-19 vaccines.
Conclusion
As of April 2021, only 70% of EMS professionals in our sample had received a COVID-19 vaccine. The remainder who had not been vaccinated indicated that they did not plan to get a vaccine, and frequently cited concerns about the safety of the vaccines. Interestingly, we found that the likelihood of COVID-19 vaccination was associated with age, gender, urbanicity, education, workplace, perceived risk of COVID-19, confidence in the vaccine, and medical mistrust. Efforts to increase COVID-19 vaccination rates in this population may need to emphasize vaccine safety and effectiveness, especially in the context of COVID-19 infection risks. Given that EMS professionals hesitant to receive a vaccine have high levels of medical mistrust, education efforts may be more effective if led or coordinated by trusted sources.
Supplementary Material
Acknowledgments
The authors thank Alice Gaughan, Jaclyn Volney, and Laura Rush, all affiliated with the authors’ organization, for their assistance with this project. They also are grateful to the individuals who participated in this study, and to the National Registry of Emergency Medical Technicians that facilitated survey distribution.
This study was supported by a grant [# CA260582] from the National Cancer Institute (NCI), but the NCI was not involved in the data collection, analysis, nor the decision to present these findings.
Footnotes
No potential conflict of interest was reported by the authors.
Supplemental data for this article can be accessed online at http://dx.doi.org/10.1080/10903127.2021.1993391
References
- 1.World Health Organization. Accelerating a safe and effective COVID-19 vaccine. 2021. [cited 2021 Aug 18]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/accelerating-a-safe-and-effective-covid-19-vaccine.
- 2.Department of Labor, Occupational Safety and Health Administration. Occupational exposure to COVID-19; Emergency Temporary Standard. 2021. [cited 2021 Oct 4]. Available from: https://www.govinfo.gov/content/pkg/FR-2021-06-21/pdf/2021-12428.pdf.
- 3.Talbot TR. COVID-19 vaccination of health care personnel as a condition of employment: a logical addition to institutional safety programs. JAMA. 2021;326(1):23–4. doi: 10.1001/jama.2021.8901. [DOI] [PubMed] [Google Scholar]
- 4.Sallam M COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173(12): 964–73. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 vaccination hesitancy in the United States: a rapid national assessment. J Community Health. 2021;46(2):270–7. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021; 39(7):1080–6. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. COVID-19 vaccinations in the United States. 2021. [cited 2021 Sept 20]. Available from: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total.
- 9.Nohl A, Afflerbach C, Lurz C, Brune B, Ohmann T, Weichert V, Zeiger S, Dudda M. Acceptance of COVID-19 vaccination among front-line health care workers: a nationwide survey of emergency medical services personnel from Germany. Vaccines. 2021;9(5):424. doi: 10.3390/vaccines9050424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caban-Martinez AJ, Silvera CA, Santiago KM, Louzado-Feliciano P, Burgess JL, Smith DL, Jahnke S, Horn GP, Graber JM. COVID-19 vaccine acceptability among US firefighters and emergency medical services workers: a cross-sectional study. J Occup Environ Med. 2021;63(5):369–73. doi: 10.1097/JOM.0000000000002152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee DJ, Carrillo L, Fleming L. Epidemiology of hepatitis B vaccine acceptance among urban paramedics and emergency medical technicians. Am J Infect Control. 1997;25(5):421–3. doi: 10.1016/s0196-6553(97)90091-2. [DOI] [PubMed] [Google Scholar]
- 12.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, Perez JL, Pérez Marc G, Moreira ED, Zerbini C, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–15. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, Diemert D, Spector SA, Rouphael N, Creech CB, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403–16. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sadoff J, Gray G, Vandebosch A, Cárdenas V, Shukarev G, Grinsztejn B, Goepfert PA, Truyers C, Fennema H, Spiessens B, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. 2021;384(23):2187–201. doi: 10.1056/NEJMoa2101544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pilishvili T, Fleming-Dutra KE, Farrar JL, Gierke R, Mohr NM, Talan DA, Krishnadasan A, Harland KK, Smithline HA, Hou PC, et al. Interim estimates of vaccine effectiveness of Pfizer-BioNTech and Moderna COVID-19 vaccines among health care personnel – 33 U.S. sites, January-March 2021. MMWR Morb Mortal Wkly Rep. 2021;70(20):753–8. doi: 10.15585/mmwr.mm7020e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benenson S, Oster Y, Cohen MJ, Nir-Paz R. BNT162b2 mRNA Covid-19 vaccine effectiveness among health care workers. N Engl J Med. 2021;384(18):1775–7. doi: 10.1056/NEJMc2101951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Center for Economic and Social Research. Understanding America Study. 2017. [cited 2021 Aug 16]. Available from: https://uasdata.usc.edu/index.php.
- 18.Freeman D, Loe BS, Chadwick A, Vaccari C, Waite F, Rosebrock L, Jenner L, Petit A, Lewandowsky S, Vanderslott S, et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2020. doi: 10.1017/S0033291720005188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009;44(6):2093–105. doi: 10.1111/j.1475-6773.2009.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Interim considerations for COVID-19 vaccination of healthcare personnel and long-term care facility residents. 2020. [cited 2021 Aug 16]. Available from: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19/clinical-considerations.html.
- 21.Dooling K, Marin M, Wallace M, McClung N, Chamberland M, Lee GM, Talbot HK, Romero JR, Bell BP, Oliver SE. The advisory committee on immunization practices’ updated interim recommendation for allocation of COVID-19 vaccine—United States, December 2020. MMWR Morb Mortal Wkly Rep. 2021;69:1657–60. doi: 10.15585/mmwr.mm695152e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Evidence table for COVID-19 vaccines allocation in phases 1b and 1c of the vaccination program. 2020. [cited 2021 Aug 16]. Available from: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19/evidence-table-phase-1b-1c.html.
- 23.Department of Health and Human Services. Secretarial directive on eligibility to receive COVID-19 vaccines. 2021. [cited 2021 Aug 16]. Available from: https://www.hhs.gov/sites/default/files/secretarial-directive-eligibility-for-covid-19-vaccines.pdf.
- 24.National Registry of Emergency Medical Technicians. The national registry dashboard. 2021. [cited 2021 Aug 16]. Available from: https://www.nremt.org/maps.
- 25.Schmuhl P, Van Duker H, Gurley KL, Webster A, Olson LM. Reaching emergency medical services providers: is one survey mode better than another? Prehosp Emerg Care. 2010; 14(3):361–9. doi: 10.3109/10903121003760184. [DOI] [PubMed] [Google Scholar]
- 26.Cash RE, Rivard MK, Camargo CA, Powell JR, Panchal AR. Emergency medical services personnel awareness and training about personal protective equipment during the COVID-19 pandemic. Prehosp Emerg Care. 2020. doi: 10.1080/10903127.2020.1853858. [DOI] [PubMed] [Google Scholar]
- 27.Dillman DA, Smyth JD, Christian LM. Internet, mail, and mixed-mode surveys: the tailored design method. 3rd ed. Hoboken, NJ: Wiley & Sons; 2009. [Google Scholar]
- 28.Prezant DJ, Zeig-Owens R, Schwartz T, Liu Y, Hurwitz K, Beecher S, Weiden MD. Medical leave associated with COVID-19 among emergency medical system responders and firefighters in New York city. JAMA Netw Open. 2020; 3(7):e2016094. doi: 10.1001/jamanetworkopen.2020.16094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trevisan A, Bertoncello C, Artuso E, Frasson C, Lago L, Nuzzo DD, Nicolli A, Maso S. Will we have a cohort of healthcare workers full vaccinated against measles, mumps, and rubella? Vaccines. 2020;8(1):104. doi: 10.3390/vaccines8010104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Variant proportions. 2021. [cited 2021 Aug 24]. Available from: https://covid.cdc.gov/covid-data-tracker/#variant-proportions.
- 31.Weber DJ, Al-Tawfiq J, Babcock H, Bryant K, Drees M, Elshaboury R, Essick K, Fakih M, Henderson D, Javaid W, et al. Multisociety statement on COVID-19 vaccination as a condition of employment for healthcare personnel. Infect Control Hosp Epidemiol. 2021. doi: 10.1017/ice.2021.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marietta ML. Vaccine hesitancy and mission alignment in the emergency services. 2021. [cited 2021 Aug 13]. Available from: https://www.jems.com/commentary/vaccine-hesitancy-and-mission-alignment-in-the-emergency-services/.
- 33.Kluger J Too many Americans still mistrust the COVID-19 vaccines. Here’s why. 2021. [cited 2021 Aug 16]. Available from: https://time.com/5925467/covid-19-vaccine-hesitancy/. [Google Scholar]
- 34.Pepper JK, Reiter PL, McRee A-L, Brewer NT. Advertisements promoting human papillomavirus vaccine for adolescent boys: does source matter? Sex Transm Infect. 2012;88(4):264–5. doi: 10.1136/sextrans-2011-050197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. Building confidence in COVID-19 vaccines. 2021. [cited 2021 Aug 16]. Available from: https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence.html.
- 36.Kaiser Permanente. COVID-19 vaccine confidence toolkit. 2021. [cited 2021 Aug 16]. Available from: https://about.kaiserpermanente.org/content/dam/kp/mykp/documents/instructions/covid19-vaccine-confidence-toolkit.pdf.
- 37.Halbrook M, Gadoth A, Martin-Blais R, Gray AN, Kashani S, Kazan C, Kane B, Tobin NH, Ferbas KG, Aldrovandi GM, et al. Longitudinal assessment of COVID-19 vaccine acceptance and uptake among frontline medical workers in Los Angeles, California. Clin Infect Dis. 2021. [DOI] [PubMed] [Google Scholar]
- 38.Rivard MK, Cash RE, Mercer CB, Chrzan K, Panchal AR. Demography of the national emergency medical services workforce: a description of those providing patient care in the prehospital setting. Prehosp Emerg Care. 2021;25(2): 213–20. doi: 10.1080/10903127.2020.1737282. [DOI] [PubMed] [Google Scholar]
- 39.Cash RE, Crowe RP, Rodriguez SA, Panchal AR. Disparities in feedback provision to emergency medical services professionals. Prehosp Emerg Care. 2017;21(6):773–81. doi: 10.1080/10903127.2017.1328547. [DOI] [PubMed] [Google Scholar]
- 40.Crowe RP, Fernandez AR, Pepe PE, Cash RE, Rivard MK, Wronski R, Anderson SE, Hogan TH, Andridge RR, Panchal AR, et al. The association of job demands and resources with burnout among emergency medical services professionals. J Am Coll Emerg Physicians Open. 2020;1(1):6–16. doi: 10.1002/emp2.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Andel SA, Pindek S, Spector PE. Being called to safety: occupational callings and safety climate in the emergency medical services. J Occup Environ Med. 2016;58(12):1245–9. doi: 10.1097/JOM.0000000000000899. [DOI] [PubMed] [Google Scholar]
- 42.Hendra R, Hill A. Rethinking response rates: new evidence of little relationship between survey response rates and non-response bias. Eval Rev. 2018;43(5):307–30. doi: 10.1177/0193841X18807719. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


