Abstract
Objectives:
The aim of this review was to describe malnutrition and poor oral hygiene, the most common risk factors for noma.
Methods:
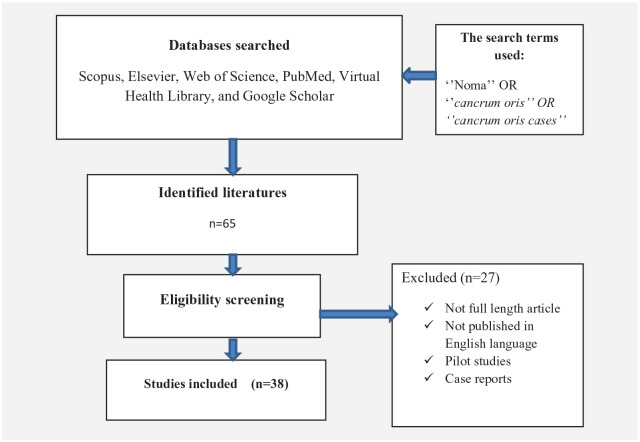
A vigorous literature searches were conducted on databases such as Scopus, Elsevier, Web of Science, PubMed, Virtual Health Library, and Google Scholar by inserting keywords such as ‘noma’ OR ‘cancrum oris’ OR ‘cancrum oris cases’. A total of 65 articles gathered. Of these, 38 articles found to be eligible for this study.
Results:
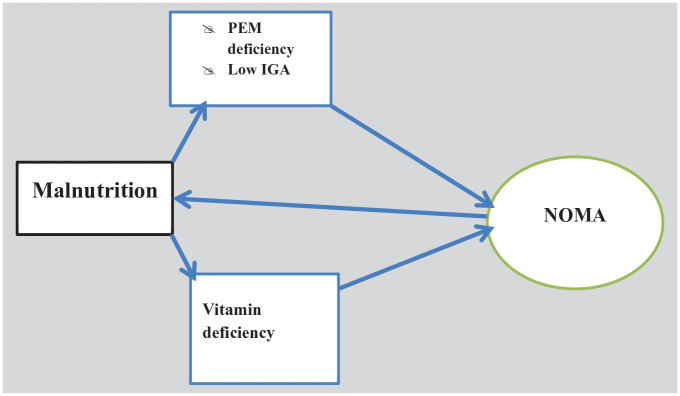
A total of 38 full-length articles were included in the review. According to the evidence gathered and summarized in this review, malnutrition, especially protein-energy malnutrition and vitamin deficiencies, makes the oral mucosa susceptible to opportunistic pathogens of noma, and then, in so doing, pathogens invade the oral cavities. Malnutrition has a bidirectional relationship with noma. Since noma is a disease of the oral cavity, poor oral hygiene has the potential of predispose and worsen the disease’s progress.
Conclusion:
Malnutrition and poor oral hygiene found to be ingrained in the pathogenesis of noma. For effective management and prevention of noma, it is necessary to underpin adequate nutritional supplementation (including vitamins). As a primary prevention strategy, healthcare workers’ training should be strengthened to improve the diagnosis and treatment of oral infections, including noma.
Keywords: Noma, malnutrition, poor oral hygiene
Introduction
Noma, or cancrum oris, 1 is a non-communicable disease of small children that has occurred for centuries. 2 Previously, noma was common in North America and Europe but disappeared with economic and public health developments. However, it commonly affects the children living in developing regions currently.1,3,4 Noma often affects neglected populations, peoples living in the poorest region of the world such as sub-Saharan Africa.4–6 The ‘noma belt’ runs from Senegal to Ethiopia. 7 Of the 11 regional states and the two administrative cities in Ethiopia, most of the cases have been reported from Amhara regional state. 8
Noma is thought to be a neglected tropical disease (NTD) because there is a knowledge deficit among healthcare workers about the disease’s management and even less emphasis has been given by policymakers.2,9–12 Despite noma’s fulfilment of the World Health Organization’s (WHO) NTD disease inclusion criteria, it is excluded from the list. For this reason, noma is sometimes called a ‘neglected-neglected tropical disease’. 13
Noma is described as a violation of human rights. The United Nations Human Rights Council Advisory Committee cited children affected by noma as ‘Noma, the face of poverty, represents the worst violations of the rights of the child’. 14
This forgotten disease affects about 140,000 children annually with an 80%–90% untreated mortality rate. 2 According to the WHO, about 770,000 noma survivors are living with sequelae. 15
Noma starts from the gum 15 and progressively damages both the soft and hard tissue of the facial zone. The exact causative agent of the noma is unknown, but it is thought to be caused by ulcerative microorganisms (normal oral flora).16–18 There are five stages (acute necrotizing ulcerative gingivitis (ANUG), oedema stage, gangrenous stage, scarring stage, and sequelae stage) in the disease progression. If detected promptly, noma is treatable; but, if left untreated, it is fatal and could result in serious physical, psychological, and social sequelae. 2 Noma is an opportunistic infection. 19 It mostly affects victims of hunger 1 and is also triggered by malnutrition, poor oral hygiene, low birth weight, and infections such as malaria, human immune deficiency virus (HIV), and measles.1,11,20,21 Prompt identification of the early stage is a key to prevent progression, mortality, and morbidity. This review describes the most common risk factors for noma, including malnutrition and poor oral hygiene.
Methodology
This is a mini-review that summarizes the two risk factors for noma, malnutrition and oral hygiene. We have conducted extensive literature searches for journal articles, books, dissertations, government reports, and conference proceedings that were published in English language by using Scopus, Elsevier, Web of Science, PubMed, Virtual Health Library, and Google Scholar search engines. The keywords used were ‘noma’ OR ‘cancrum oris’ OR ‘cancrum oris cases’. All peer-reviewed primary studies, regardless of the study design and the year of publication, were included in this review. On the contrary, articles that were not full length, were not primary studies, pilot studies, case reports, and were published in a language other than English were excluded. All the gathered full articles were sent to Mendeley library, and then the data extraction and summary were done by the three authors. From the total of 65 articles gathered, 38 eligible articles were included in this review (Figure 1).
Figure 1.
A Flow diagram of literature searches.
Result
In this review, we used a total of 38 articles. Accordingly, of the reviewed studies from which we gathered data, majority of studies identified malnutrition as a risk factor for noma. In addition, this review exclusively pointed out the bilateral association between noma and malnutrition.
About 26.3% of the reviewed articles identified poor oral hygiene as a risk factor for noma. It also identified the role of poor hygiene in the disease severity of noma.
Discussion
Noma and malnutrition
Malnutrition is defined as a deviation from sufficient and optimal nutrition. It includes both under- and overnutrition. 22 In our context, undernutrition, found as a major risk factor for noma disease, was discussed in this review. Undernutrition occurs when a person intakes insufficient dietary energy that might result in depletion of fatty tissue, emaciation, and atrophy of muscles.22,23 Undernutrition is diagnosed by being underweight (low weight for age), stunting (low height for age), and wasting (low weight for height). The most well-known risk factor for noma is malnutrition, which is why the disease has earned the moniker ‘the face of poverty’.1,20,24–26 Until the early 20th century, noma was common in North America and Europe, when there was an inadequate supply of nutrition for people. Nonetheless, after economic advancement and appropriate nourishment of people, the disease was eliminated from these regions. 25 Undernutrition primarily compromises the child’s immune system and then creates a favourable environment for noma.5,27
Acute, protein-energy malnutrition (PEM) is one of the most common causes of compromised immunity in malnourished children.28,29 As evidence shows, PEM syndrome was revealed in noma patients. 27
In addition, in undernourished individuals, the immunoglobulin A (IgA) that is a crucial part of the mucosal immune system may diminish and their bodies may produce a surplus of pro-inflammatory substances such as C-proteins, cytokines, tumour necrosis factors (TNFs), and interleukins (ILs). This creates a favourable environment for ulceration of oral mucosa.17,28 Salivary IgA is very important for oral mucosal integrity, and it is thought to be the first line of defence against oral pathogens. 30 In the deficiency of cellular defensive factor, the child’s oral mucosa can be easily invaded by the surrounding microorganisms and in turn disseminated to the orofacial regions.
Vitamin deficiency
Vitamins are components of nutrition that have an important role in the integrity of the oral mucosa, especially vitamins such as vitamin A, C, and B-complex.
Vitamin C (ascorbic acid) deficiency results in bleeding of gums, delayed wound healing, and depletion of collagen tissue, which may create favourable conditions for microbial invasion. 31 In addition, ascorbic acid deficiency causes periodontal distraction. 32
In the case of vitamin A deficiency, there is a prompt breakdown of epithelial tissue and pathologic changes to the oral mucosa. 27 Vitamin A deficiency, in addition to nutritional inadequacies, has indeed been related to measles, which is another risk factor for noma. 1
The oral condition of children could be affected by any of vitamin B deficiencies. As a result, lip cracking, sore tongue, haemorrhagic gingivitis, and tongue inflammation are all linked to vitamin B1, B6, B12, and B2/B3 deficiencies. 31 According to a shared evidence, noma cases were frequently found in children who have vitamins A, B, and C deficiency. 33 Thus, vitamin supplementation has a vital role in both the prevention and treatment of noma cases.
How does noma in turn cause malnutrition?
The relationship between noma and malnutrition is not only unidirectional; rather, it is a bit vicious (Figure 2). Thus, the risk of malnutrition among noma survivors is high. Noma survivors face feeding difficulties as a result of oral lesions and deformity of their teeth and masticatory muscles, which lead to further malnutrition.19,27
Figure 2.
A diagrammatic view of how malnutrition jeopardizes noma and vice versa.
Noma and poor oral hygiene
Oral hygiene is fundamental to the whole well-being of an individual. However, the prevention of oral diseases has been the least prioritized issue globally. The marginalized and poor people are commonly and adversely affected by oral diseases. 34
Poor oral hygiene is an attribute of noma disease, which expedites the disease’s progress.20,26,33 It refers to the presence of debris, calculus, or extrinsic stains covering one-third to two-thirds of the tooth surface. 35 Poor oral hygiene plays an important role in the pathophysiology of noma, and it is typically seen in children from low-income families whose parents may lack the knowledge or resources to protect their children’s oral health.33–36 The extremely poor oral condition has been recognized in noma survivors. 32 According to a study conducted in Ibadan, Nigeria, the magnitude and severity of noma were higher in children with poor oral hygiene.5,35 Evidence from the North-western and South-western provinces of Nigeria revealed the impact of poor oral hygiene on both the risk and severity of noma. 37 Moreover, in a study from Ethiopia, poor oral hygiene was diagnosed from noma survivors. 29 The bad oral condition of the noma patient even challenges management because in the case of poor oral hygiene, the infected area may be surrounded by microorganisms that further deteriorate the condition. 32
The prevention and control of noma disease requires good oral hygiene. Indubitably, small children cannot keep their oral hygiene self-sufficiently, so their caregivers need to follow and support them during a daily cleansing of their oral cavity. Furthermore, the entities who work on the prevention and treatment of noma disease need to incorporate the assessment of children’s oral cavities into the prevention and treatment guidelines and also need to strengthen the management of oral problems. Thus, the training of healthcare workers is an important step to improving the diagnosis of gingivitis and oral infections, leading to the primary prevention of noma. 38
The use of all relevant studies conducted on noma, regardless of geography and publication year, is strength of this study. However, there may be some limitations in this review. Since the majority of primary studies conducted on noma have been undertaken in small sample sizes, this review may lack generality. Moreover, there has been limited number of available and published articles on the risk factors of noma.
Conclusion
This review describes the risk of malnutrition on noma and vice versa. Moreover, it emphasizes the effect of poor oral hygiene on pathophysiology of noma. In malnourished children, their bodies lack important nutrients and vitamins used to maintain the integrity of the oral mucosa, which results in an opportunistic invasion by oral flora. Poor oral hygiene in the absence of routine mouth care in children exposes and adversely affects the control of noma. Therefore, as a treatment and prevention strategy, nutritional supplementation needs to be prioritized in both clinical and community settings where noma is prevalent. In addition, in noma endemic regions, including sub-Saharan Africa, all the concerned entities need to work to endorse and strengthen oral hygiene programmes.
Acknowledgments
We thank all the authors of the original articles used in this review.
Footnotes
Author contribution: All authors were equally participated in concept development, searching relevant databases, critical appraisals, methods, interpretation, draft writing, and summarization.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Wubishet Gezimu  https://orcid.org/0000-0002-5503-1360
https://orcid.org/0000-0002-5503-1360
Abdissa Duguma  https://orcid.org/0000-0001-7725-6061
https://orcid.org/0000-0001-7725-6061
References
- 1. Enwonwu CO. Noma: a neglected scourge of children in sub-Saharan Africa. Bull World Health Organ 1995; 73(4): 541–545. [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Non communicable Diseases Cluster (NCD) regional Programme for noma control noma, 2016, https://www.afro.who.int/sites
- 3. Falkler WA, Enwonwu CO, Idigbe EO. Microbiological understandings and mysteries of noma (cancrum oris). Oral Dis 1999; 5: 150–155. [DOI] [PubMed] [Google Scholar]
- 4. Jeff W, July C, Aitken M, et al. Mismanagement as a prelude to privatisation of the UK NHS manifestations of severe RSV bronchiolitis. Lancet 2006; 368: 988. [DOI] [PubMed] [Google Scholar]
- 5. Ashdown N. The missing faces of Ethiopia’s poor. Inter press Service, 2021, pp. 1–2, https://reliefweb.int/report/ethiopia/missing-faces-ethiopia-s-poor
- 6. Caulfield A, Alfvén T. Improving prevention, recognition and treatment of noma. Bull World Heal Org 2020; 98: 365–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marck KW. Noma: a neglected enigma. Lancet Glob Heal 2013; 1(2): e58–e59. [DOI] [PubMed] [Google Scholar]
- 8. Rickart AJ, Rodgers W, Mizen K, et al. Perspective piece facing Africa: describing noma in Ethiopia. Am Soc Trop Med Hyg 2020; 103(2): 613–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Leila Srour M, Marck KW, Baratti-Mayer D. Noma: neglected, forgotten and a human rights issue. Int Health 2015; 7(3): 149–150. [DOI] [PubMed] [Google Scholar]
- 10. Speiser S, Langridge B, Birkl MM, et al. Update on noma: systematic review on classification, outcomes and follow-up of patients undergoing reconstructive surgery after noma disease. BMJ Open 2021; 11: e046303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Reksodiputro MH, Yosia M. Noma: a neglected tropical disease. ORLI 2021; 51(1): 56–63. [Google Scholar]
- 12. Farley E, Ariti C, Amirtharajah M, et al. Noma, a neglected disease: a viewpoint article. PLoS Negl Trop Dis 2021;15: e0009437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Srour ML, Baratti-Mayer D. Why is noma a neglected-neglected tropical disease? PLoS Negl Trop Dis 2020; 2020: 4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Study on Severe Malnutrition Childhood Diseases With Children Affected by Noma as an Example (A/HRC/AC/8/7) United Nations Human Rights Council Advisory Committee Eighth session, 2012, https://www.ohchr.org/EN/HRBodies/HRC/AdvisoryCommittee/Session8/Pages/Index.aspx
- 15. Bourgeois DM, Leclercq MH. The World Health Organization initiative on noma, 1999. pp. 172–174, http://www.stockton-press.co.uk/od%250 [DOI] [PubMed]
- 16. Feller L, Altini M, Chandran R, et al. Noma (cancrum oris) in the South African context. J Oral Pathol Med 2014; 43(1): 1–6. [DOI] [PubMed] [Google Scholar]
- 17. Ashok N, Tarakji B, Darwish S, et al. A review on noma: a recent update. Glob J Health Sci 2016; 8(4): 53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization. Information brochure for early detection and management of Noma, 2016; 1–24.
- 19. Auluck A, Pai KM. Noma: life cycle of a devastating sore – case report and literature review. J Can Dent Assoc 2005; 71: 10. [PubMed] [Google Scholar]
- 20. Baratti-Mayer D, Gayet-Ageron A, Hugonnet S, et al. Risk factors for noma disease: a 6-year, prospective, matched case-control study in Niger. Lancet 2013; 1: 87–96. [DOI] [PubMed] [Google Scholar]
- 21. Srour ML, Marck K, Baratti-Mayer D. Noma: overview of a neglected disease and human rights violation. Am J Trop Med 2017; 96(2): 268–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shetty P. Malnutrition and Undernutrition, 2003, pp. 18–22, https://www.researchgate.net/publication/257524504_Malnutrition_and_Undernutrition
- 23. Blössner M, Onis M, De Prüss-Üstün A, et al. Malnutrition: quantifying the health impact at national and local levels. Geneva: World Health Organization, 2005. [Google Scholar]
- 24. Maley A, Desai M, Parker S. Noma: a disease of poverty presenting at an urban hospital in the United States. JAAD Case Reports 2015; 1(1): 18–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Marck KW. A history of Noma, the “Face of Poverity”. Plast Reconstr Surg 2003; 111(5): 1702–1707. [DOI] [PubMed] [Google Scholar]
- 26. Enwonwul CO, Falkler WA, Jr, Idigbe EO. Oro-facial gangrene (noma/cancrum oris): pathogenetic mechanisms. Crit Rev Oral Biol Med 2000; 11(2): 159–171. [DOI] [PubMed] [Google Scholar]
- 27. Weledji EP, Edin F, Njong S. Cancrum oris (noma): the role of nutrition in management. J Am Coll Clin Wound Spec 2016; 7(1–3): 50–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Słotwińska SM, Słotwiński R. Host response, malnutrition and oral diseases. Part 1. Cent Eur J Immunol 2014; 39(4): 518–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lafferty N. Changing the face of Africa: estimating the burden of noma in rural Ethiopia and identifying options for prevention and improvement in its diagnosis and management. Dissertation for the Liverpool School of Tropical Medicine; 2021. [Google Scholar]
- 30. Marcotte H, Lavoie MC. Oral microbial ecology and the role of salivary immunoglobulin A. Microbiol Mol Biol Rev 1998; 62(1): 71–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sheetal A, Hiremath VK, Patil AG, et al. Malnutrition and its oral outcome – a review. J Clin Diagn Res 2013; 7(1): 178–180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ogisi F. Cancrum Auris in children: report of two cases. Niger J Paediatr 2002; 29(4). 10.4314/njp.v29i4.12021 [DOI] [Google Scholar]
- 33. Farley E, Mehta U, Srour ML, et al. Noma (cancrum oris): a scoping literature review of a neglected disease (1843 to 2021). Plos Negl Trop Dis 2021; 15(12): e0009844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. World Health Organization. Oral health: Achieving better oral health as part of the universal health coverage noncommunicable disease agendas towards, 2020, https://apps.who.int/gb/ebwha/pdf_files/EB148/B148_8-en.pdf
- 35. Taiwo JO. Oral hygiene status and necrotizing ulcerative gingivitis in Nigerian children. J Periodontol 1993; 64(11): 1071–1074. [DOI] [PubMed] [Google Scholar]
- 36. Sheiham A. The epidemiology of chronic periodontal disease in Western Nigerian school children. J Periodontal Res 1968; 3(4): 257–267. [DOI] [PubMed] [Google Scholar]
- 37. Idigbe EO, Enwonwu CO, Falkler WA, et al. Living conditions of children at risk for noma: Nigerian experience. Oral Dis 1999; 5(2): 156–162. [DOI] [PubMed] [Google Scholar]
- 38. Brattström-Stolt L, Funk T, Sie A, et al. Noma – knowledge and practice competence among primary healthcare workers: a cross-sectional study in Burkina Faso. Int Health 2019; 11: 290–296. [DOI] [PubMed] [Google Scholar]