Abstract
Cardiac rehabilitation (CR) following acute myocardial infarction (AMI) improves physical capacities and decreases hospitalizations and cardiovascular mortality. L-arginine is the substrate used by nitric oxide (NO) synthase to generate NO and it has been shown to exert its beneficial effects on endothelium driving vasodilatation, reducing inflammation, and ameliorating physical function. We hypothesized that L-arginine could enhance physical capacities in patients who underwent CR after AMI. We designed a study aimed to assess the effects of L-arginine administration on the physical capacity of patients who underwent coronary revascularization after AMI. The trial was carried out amid the COVID-19 pandemic. Patients were assigned, with a 2:1 ratio, to add to their standard therapy one bottle containing 1.66 g of L-arginine or one bottle of identical aspect apart from not containing L-arginine, twice a day orally for 3 weeks. Patients performed a 6-minute walking test (6MWT), and their Borg modified 0–10 rating of perceived exertion (BRPE) was assessed before starting and at the end of the treatment. Seventy-five patients receiving L-arginine, and 35 receiving placebo successfully completed the study. The 6MWT distance increased significantly in the L-arginine group compared with both baseline and placebo (P < 0.0001). Additionally, we observed a significant improvement in the BRPE in patients treated with L-arginine but not in the placebo group. Taken together, our data indicate that L-arginine potentiates the response to CR independently of age, sex, baseline functional capacity, and comorbid conditions.
SIGNIFICANCE STATEMENT
This study shows for the first time that oral supplementation of L-arginine potentiates the response to cardiac rehabilitation after myocardial infarction and cardiac revascularization. Indeed, we observed a significant improvement in two fundamental parameters, namely, the 6-minute walking test and the Borg modified 0–10 rating of perceived exertion. Strikingly, the beneficial effects of L-arginine were independent of age, sex, comorbid conditions, and baseline functional capacity.
Introduction
Cardiac rehabilitation (CR) following acute myocardial infarction (AMI) is a multicomponent program leading to secondary prevention in cardiovascular diseases, reducing physical decline and improving physical capacities (Price et al., 2016; Ruano-Ravina et al., 2016; Poffley et al., 2017; Dibben et al., 2018; Cieza et al., 2021; Taylor et al., 2022). Furthermore, CR decreases hospitalizations and cardiovascular mortality (Antypas and Wangberg, 2012; Grazzi et al., 2016). Based on the evidence of its beneficial cardiovascular effects, CR has a Class I indication in several European and American guidelines for patients with various heart diseases, including peripheral artery disease, stable angina, heart surgery, AMI, as well as heart failure with reduced left ventricular function (Leon et al., 2005; Balady et al., 2011; Piepoli et al., 2016; Ponikowski et al., 2016; Ibanez et al., 2018).
The exact reasons for the beneficial effect of early CR are mostly unclear, although the consequences of aerobic exercise, defined as physical activity that induces a steady and sustainable increase in aerobic metabolism when performed at an intensity below the anaerobic threshold (Zhou et al., 2021), have been extensively studied, at least from a cardiological point of view (Wahl et al., 2018; Channon, 2020; Gambardella et al., 2020b; Gulsin et al., 2020). Indeed, aerobic exercise training has been shown to improve endothelial function both in the large arteries and microcirculation in patients with cardiovascular risk factors, including hypertension and diabetes (Green et al., 2004; Phillips et al., 2015). Aerobic exercise might exert its favorable effects by modifying the flow pattern at the level of arterial branch points, thereby eliciting a less turbulent flow, which would trigger the expression of atheroprotective genes, including endothelial nitric oxide (NO) synthase, with the ensuing restoration of a vasoprotective and vasodilator phenotype of the endothelium (Phillips et al., 2015). A decline in inflammation and oxidative stress, alongside the improved autonomic tone, may contribute to the beneficial effects of physical exercise on endothelial cell function (Zoladz et al., 2010; Phillips et al., 2015; Green et al., 2017).
L-arginine is a semiessential amino acid involved in a number of biologic processes; among these, L-arginine is the substrate used by nitric oxide synthase to produce NO, which is a fundamental endothelial relaxation factor driving cardiovascular homeostasis (Gambardella et al., 2020a). Thus, L-arginine exerts its beneficial effects on endothelium driving vasodilatation, increasing tissue perfusion, thus improving the delivery of nutrients and oxygen for the generation of ATP, and reducing inflammation (Andrew and Mayer, 1999; Durante et al., 2000; Tousoulis et al., 2012) and has been associated with the improvement of physical function (Bailey et al., 2010; Bescos et al., 2011; Rodrigues-Krause et al., 2018; Gambardella et al., 2021a; Reyes et al., 2022).
Based on these shreds of evidence, we hypothesized that L-arginine could improve physical capacities in patients undergoing CR after AMI and also could not immediately perform a complete CR program due to the COVID-19 pandemic. In particular, this study investigates the impact of L-arginine on physical capacity as assessed by the 6-minute walking test (6MWT) and the Borg modified 0–10 Rate of Perceived Exertion (BRPE) scale (Borg, 1982; Borg et al., 2017). The 6MWT represents a measure for integrated global response of multiple musculoskeletal and cardiopulmonary systems involved in exercise; this test provides valuable information on functional capacity, response to therapy, and prognosis in numerous chronic cardiopulmonary conditions (Enright, 2003; Arena et al., 2007; Beatty et al., 2012). The BRPE scale is a tool for measuring effort and exertion, breathlessness, and fatigue during physical work and is widely considered very relevant for occupational health and safety practice (Borg et al., 2017).
Materials and Methods
Study Design and Participants
We designed an investigator-initiated prospective, randomized, placebo-controlled double-blind parallel-group study aimed to assess the effects of L-arginine administration on the physical capacity of patients who underwent coronary revascularization after AMI.
Ethical approval was obtained from the Institutional Ethical Committee; a written informed consent was collected from all patients. The study was performed following the principles of the 2013 Declaration of Helsinki and the International Conference on Harmonization–Good Clinical Practice guidelines.
Inclusion criteria: eligible patients were men and nonpregnant women aged >18 years admitted to rehabilitation hospital after AMI followed by coronary artery bypass graft (CABG) or percutaneous coronary revascularization (PCI).
Exclusion criteria were: malignant arrhythmias (ventricular fibrillation >24 hours after AMI, ventricular tachycardia, fibrillation or paroxysmal flutter with rapid ventricular response and hemodynamic deterioration, atrial fibrillation in patients with Wolff-Parkinson-White syndrome, grade 2 or 3 atrioventricular block, ventricular extrasystole which increases during exertion and uncontrolled supraventricular tachycardia), valvular heart disease, unstable angina, poorly-controlled high blood pressure, ischemia induced by exercise, disease not amenable to revascularization, disorders of the locomotor, neurologic, or respiratory system that limited walking, glycolic metabolism instability, pacemaker or implantable cardioverter defibrillator–cardiac resynchronization therapy, and/or because they refused to participate in the study.
Procedures
Using a computer-generated randomization table, all eligible patients were assigned, with a 2:1 ratio, to add to their standard therapy one bottle containing 1.66 g of L-arginine (Bioarginina, Farmaceutici Damor) or one bottle of identical aspect except not containing L-arginine, twice a day orally for 3 weeks. The formulation of Bioarginina that we used in this trial consists of oral vials that contain 1.66 g of L-arginine. This dose has been chosen based on a previous study (Gambardella et al., 2021a) in which we had verified that this regimen was safe and effective in ameliorating oxidative metabolism of water polo players. The taste is fully buffered by the addition of anhydrous citric acid and sucrose (Fiorentino et al., 2021; Mone et al., 2022d). Hence, there were no differences in appearance, taste, or smell, between placebo and treatment.
Before randomization, we collected demographic characteristics and other laboratory and clinical data required by routine diagnostic activity. Clinical and laboratory parameters were assessed again at the end of the 3-week treatment period according to routine hospital practice. Safety assessment included daily measurement of vital signs and monitoring for adverse events. Before starting and at the end of the 3-week treatment with L-arginine or placebo the patients performed a 6MWT and underwent BRPE scale evaluation (described below).
6MWT
We performed the 6MWT on a 50-m straight, flat corridor, as previously described (Enright and Sherrill, 1998; D'Ascia et al., 2011; Sardu et al., 2014; Gambardella et al., 2021b).
BRPE
By allowing patients to subjectively rate their level of exertion, this scale represents a powerful indicator to guide and monitor exercise intensity. Thirty minutes after each 6MWT, the nurse asked the patient to rate his/her level of effort at performing the exercise on the BRPE scale (“How hard you feel your body has worked?”) (Borg et al., 2017).
Trial personnel, doctors, patients, and outcome assessors were all unaware of the type of supplementation provided.
Objectives of the Study
The primary clinical endpoint was the % of patients of the two study groups achieving in the post-treatment 6MWT an increase >10% of the baseline 6MWT distance.
The secondary clinical endpoint was the treatment-induced change in the BRPE score. Safety outcomes included serious adverse events, treatment-emergent adverse events, and premature discontinuations of treatment.
Statistical Analysis
According to previous observations, an increase >10% in the distance walked between the two 6MWT should be considered as a real improvement in functional capacity (Opasich et al., 1998), to be attributed to the therapeutic intervention and not intertest variability. Based on these data, we chose as primary end point the percentage of patients achieving an increase >10% of the basal 6MWT distance at the test performed at the end of the experimental treatment.
For the calculation of the sample size, we exploited results from our preliminary experiences with L-arginine and hypothesized a difference of at least 70% in the primary outcome between the two study arms. According to such hypothesis, we determined that we needed to enroll a population of 105 patients to detect a difference with a power of 90% and a two-sided level of 0.05.
Data were analyzed using the SPSS software (version 27.0; SPSS, IBM, Armonk, NY, USA) and expressed as percentages or means ± S.D. or S.E., as indicated. Descriptive statistics were performed using ANOVA (followed by Bonferroni correction) or χ2 distribution, with Monte Carlo simulation to generate exact P value. Multivariable logistic regression analysis was used to assess the association between L-arginine and 6MWT distance, adjusting for potential confounders. Significance was set at P < 0.05.
Results
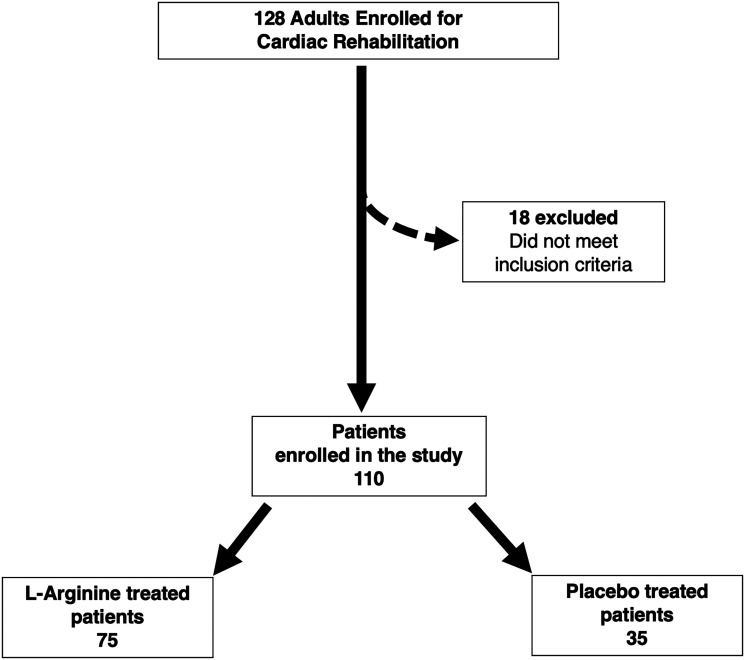
From April 1 to October 31, 2021, during the COVID-19 pandemic, we assessed 128 patients meeting our inclusion criteria who were consecutively admitted to a single center for intensive CR; of these patients, 110 (86%) were able to perform a standard 6MWT; however, 18 patients (14%) were excluded from testing on account of the presence of exclusion criteria.
Seventy-five patients assigned to receive L-arginine and 35 to receive placebo successfully completed the study protocol (Fig. 1).
Fig. 1.
Flowchart of the study.
Fifty-seven patients (51.8% of the sample) performed the 6MWT within 15 days after AMI followed by CABG (Placebo: N = 19, L-arginine: N = 38), and 53 patients (48.2% of the sample) performed the 6MWT shortly after an AMI followed by PCI (52 patients; placebo: N = 15, L-arginine: N = 37).
Baseline clinical and demographic characteristics of the two arms are reported in Table 1. In both groups, gender distribution was well balanced, mean age was below 65 years, more than 50% of the study population had comorbidities such as arterial hypertension or diabetes mellitus or both. Chronic kidney disease might have an impact on cardiac rehabilitation (Thompson et al., 2021; Wilson et al., 2021; Hama et al., 2022); however, we did not detect any significant difference between the two study arms in terms of glomerular filtration rate and serum creatinine level at baseline (Table 1).
TABLE 1.
Baseline characteristics of ourpopulation.
| Placebo | L-Arginine | P Value | |
|---|---|---|---|
| Age (years) | 60.94 ± 6.5 | 61.09 ± 7.5 | 0.919 |
| Male sex (n, %) | 18 (51.4) | 37 (49.3) | 0.838 |
| Weight, Kg, S.D. | 73.97 ± 10.5 | 72.04 ± 11.0 | 0.387 |
| Smoking (n, %) | 11 (31.4) | 22 (29.3) | 0.823 |
| Hypertension (n, %) | 16 (45.7) | 35 (46.7) | 0.926 |
| Diabetes (n, %) | 14 (40.0) | 28 (37.3) | 0.789 |
| PCI (n, %) | 16 (45.7) | 37 (49.3) | 0.723 |
| CABG (n, %) | 19 (54.3) | 38 (50.7) | 0.723 |
| Basal O2 saturation (%) | 97.97 ± 0.9 | 97.56 ± 0.7 | 0.011 |
| BRPE score | 3.91 ± 1.2 | 4.17 ± 1.1 | 0.258 |
| 6MWT (meters) | 434.14 ± 43.8 | 450.17 ± 46.2 | 0.088 |
| Blood glucose (mg/dl) | 93.57 ± 9.3 | 93.48 ± 10.0 | 0.964 |
| GOT (IU/L) | 29.11 ± 4.4 | 29.47 ± 4.1 | 0.685 |
| GPT (IU/L) | 29.31 ± 4.3 | 29.2 ± 3.8 | 0.889 |
| Hb (g/dl) | 12.23 ± 0.9 | 12.44 ± 0.7 | 0.192 |
| Serum creatinine (mg/dl) | 0.87 ± 0.15 | 0.86 ± 0.16 | 0.751 |
| GFREPI (mL/min1.73 m2) | 82.6 ± 17.5 | 83.7 ± 17.6 | 0.771 |
| LVEF (%) | 57.4 ± 3.3 | 57.5 ± 3.3 | 0.859 |
All values are expressed as mean ± S.D. or %. GFREPI: glomerular filtration rate calculated using the equation developed by the Chronic Kidney Disease Epidemiology Collaboration; Hb: hemoglobin; LVEF: left ventricular ejection fraction;.
6MWT Performance
The mean walking distance at baseline was 434.1 ± 43.8 m, corresponding to 82.4 ± 12.0% of the predicted values (which were calculated based on the regression equation obtained in healthy subjects) in the placebo group and 450.2 ± 46.2 m, corresponding to 85.2 ± 12.9% of the predicted values in the L-arginine group (n.s. for both). The distance walked by CABG patients (N = 57: 439.5 ± 43.4 m, 82% predicted) was comparable to that of patients who after AMI received PCI (N = 53: 451.1 ± 48.1 m, 84% predicted); thus, we pooled the data of the patients in each treatment group.
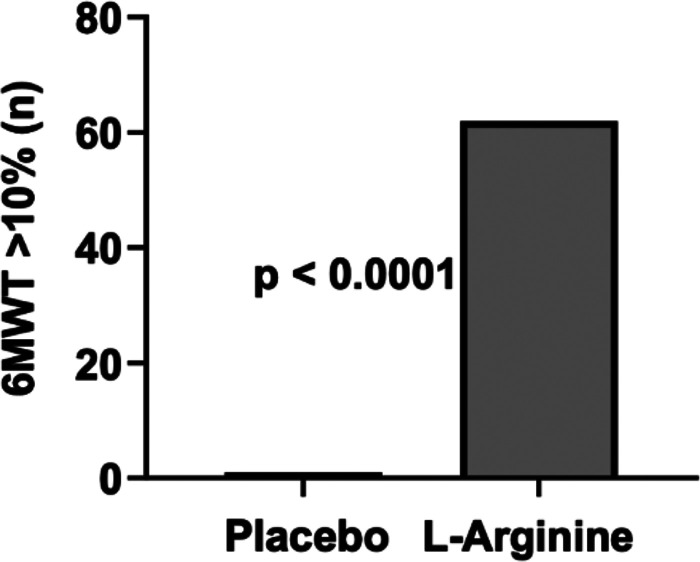
We evaluated the differences in the 6MWT distance between the two tests performed by each patient, and we found that in the placebo group, only 1 patient (2.5%) showed an increase > 10% of the 6MWT distance, while in the L-arginine group 62 patients (82.7%) achieved such an increase (P < 0.0001) (Fig. 2). As a consequence, the mean 6MWT distance was significantly improved in the L-arginine group compared with placebo (505.2 ± 52.4 m, P < 0.0001; Fig. 3), so that after L-arginine treatment, it rose from 85.2 ± 12.9% to 95.6 ± 14.4% of the predicted values (P < 0.0001), while remaining unchanged in the placebo group (baseline 82.4 ± 12.0%, after treatment 86.4 ± 12.5%, n.s.).
Fig. 2.
Patients showing an increase >10% of 6-MWT distance after treatment.
Fig. 3.
Post treatment 6MWT distance. The black bars represent the predicted value of 6MW for each group. Data are means ± S.D.
When performing a multivariate regression analysis with 6MWT distance at follow up in the L-arginine treated group as the dependent variable to verify the impact of the comorbidities and the type of coronary intervention, we did not observe any other significant result.
BRPE
As shown in Table 1, the baseline BRPE score was not significantly different between the 2 study arms nor among patients who after AMI had undergone CABG (N = 57: 4.0 ± 1.1) or PCI (N = 53: 4.1 ± 1.1). Thus, even for these parameters we pooled the data of the patients of each treatment group and found that there was a significant improvement in the Borg score in patients treated with L-arginine but not in the placebo group (Fig. 4).
Fig. 4.
Variation in Borg score after treatment. Data are means ± S.E.
Adverse Events
No serious adverse events were reported.
Discussion
Despite the known benefits of CR, disparities in participation and referral rates are still present in the clinical scenario. For instance, a trial conducted in 56 hospitals that discharged more than 170,000 patients after MI, PCI, or CABG revealed that only 56% of patients who were candidates for CR had been actually referred to a CR program (Brown et al., 2009). A further crucial point is the extent of improvement in physical capacity obtained with the CR program, which is directly related to the number of CR sessions. When comparing patients according to the number of attended sessions (<24 sessions versus ≥25 sessions), at 1 year and 5 years, mortality rates were shown to be significantly lower for those who attended ≥25 CR sessions (2.2% versus 5.3% at 1 year and 16.3% versus 24.6% at 5 years) (Suaya et al., 2009). To overcome this issue, other CR formats have been proposed (Jin et al., 2014; Abell et al., 2016; Pio et al., 2019; Abreu et al., 2020; Purcell et al., 2020; Forman et al., 2022). Home-based CR programs may improve both participation and outcomes, especially for patients who are living far from standard supervised programs (Besnier et al., 2021; Vonk et al., 2021; Terbraak et al., 2022). With these aspects in mind, the possibility to potentiate CR by L-arginine treatment appears extremely interesting.
Our data indicate that functional capacity is significantly reduced shortly after AMI and does not improve after short-term physical training. The simultaneous administration of L-arginine potentiates the response to CR, independently of age, sex, baseline functional capacity, and comorbid conditions, so that after only a 3-week CR program, we were able to detect a statistically and clinically significant increase in the 6MWT distance, while in the placebo group only one patient was showing an increase >10% of the baseline 6MWT distance. The 6MWT has been shown to better reflect the daily activity compared with the treadmill or bicycle, with an acceptable reproducibility (Enright, 2003; Pollentier et al., 2010). Consistent with previous studies revealing a correlation between the results of the 6MWT and changes in symptoms (Schuler et al., 1992a,b), our trial shows a simultaneous reduction in the BRPE score in patients treated with L-arginine. In fact, at baseline, both study groups displayed a mean score on the Borg modified 0–10 scale, which seemed to indicate that a high muscular loading was occurring. After L-arginine treatment, the increase in the 6MWT distance was accompanied by a reduction in Borg score denoting a “moderate” muscular loading.
Our results do not allow any speculation on the mechanisms underlying the favorable effect of L-arginine on CR-induced improvement in physical capacity. However, AMI leads to endothelial dysfunction with inflammation and oxidative stress, contributing to physical impairment, hospitalizations, and mortality (Odegaard et al., 2016; Steven et al., 2019; Kibel et al., 2020; Mone et al., 2021; Tang et al., 2021; Thompson et al., 2021). In this scenario, adding L-arginine in a post-AMI cohort is supported by a strong rationale, inasmuch as L-arginine, among its pleiotropic effects, has been shown to counteract endothelial dysfunction, inflammation, and oxidative stress (Mabalirajan et al., 2010; van der Zwan et al., 2011; Hong et al., 2018; Qiu et al., 2019; Fiorentino et al., 2021). Furthermore, in a recent clinical study, we evidenced that in professional water polo players, chronic L-arginine was effective in ameliorating oxidative metabolism through a mechanism of enhanced mitochondrial function (Gambardella et al., 2021a).
Our study has several limitations worth noting, including the relatively short follow-up and the small sample size. Due to the small size of the two study arms, we cannot draw any conclusion on the difference between the occurrence and the type, if any, of coronary revascularization after AMI. Unfortunately, we did not screen our population for frailty; nevertheless, we reckon that frailty is common in older adults with cardiovascular diseases, especially post-AMI (Mone and Pansini, 2020; Damluji et al., 2021; Mone et al., 2022a,b,c). Finally, we want to emphasize the fact that our data need to be contextualized within the COVID-19 pandemic, with major clinical, social, and economic implications (Ambrosino et al., 2021; Aoyagi et al., 2021; Cattadori, 2022; Desai et al., 2021; Kawada, 2021; Anghel et al., 2022; Kambic et al., 2022; Su et al., 2022; Taylor et al., 2022).
Acknowledgments
The authors thank Dr. X. Wang for critical discussion.
Abbreviations
- AMI
acute myocardial infarction
- BRPE
Borg rate of perceived exertion
- CABG
coronary artery bypass graft
- CR
cardiac rehabilitation
- 6MWT
6-minute walking test
- NO
nitric oxide
- PCI
percutaneous coronary intervention
Authorship Contributions
Participated in research design: Izzo, Marazzi, Santulli, and Trimarco.
Conducted experiments: Marazzi, Manzi, Gallo, Campolongo, Cacciotti, Izzo, Tartaglia, Caminiti, Varzideh, Santulli, Trimarco.
Performed data analysis: Mone, Izzo, Varzideh, Santulli.
Wrote or contributed to the writing of the manuscript: Mone, Marazzi, Santulli, Trimarco.
Footnotes
The Santulli’s Laboratory is supported in part by the National Institutes of Health (NIH): National Heart, Lung, and Blood Institute [Grant R01-HL146691], [Grant R01-HL159062], and [Grant T32-HL144456]; National Institute of Diabetes and Digestive and Kidney Diseases [Grant R01-DK033823] and [Grant R01-DK123259]; National Institute on Aging [Grant R56-AG066431] (to G.S.); by the Irma T. Hirschl and Monique Weill-Caulier Trusts (to G.S.); and by the Diabetes Action Research and Education Foundation (to G.S.). F.V. is supported by a postdoctoral fellowship of the American Heart Association [AHA 21POST836407]. Both L-arginine (Bioarginina) and placebo were kindly provided by Farmaceutici Damor S.p.A., Naples, Italy, which had no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data, preparation, review, or approval of the manuscript, and decision to submit the manuscript for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Abell B, Glasziou P, Briffa T, Hoffmann T (2016) Exercise training characteristics in cardiac rehabilitation programmes: a cross-sectional survey of Australian practice. Open Heart 3:e000374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abreu A, Frederix I, Dendale P, Janssen A, Doherty P, Piepoli MF, and Voller H (2020) Standardization and quality improvement of secondary prevention through cardiovascular rehabilitation programmes in Europe: The avenue towards EAPC accreditation programme: A position statement of the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology (EAPC). Eur J Prev Cardiol. [DOI] [PubMed] [Google Scholar]
- Ambrosino P, Lanzillo A, Maniscalco M (2021) COVID-19 and Post-Acute COVID-19 Syndrome: From Pathophysiology to Novel Translational Applications. Biomedicines 10:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrew PJ, Mayer B (1999) Enzymatic function of nitric oxide synthases. Cardiovasc Res 43:521–531. [DOI] [PubMed] [Google Scholar]
- Anghel R, Adam CA, Marcu DTM, Mitu O, Mitu F (2022) Cardiac Rehabilitation in Patients with Peripheral Artery Disease-A Literature Review in COVID-19 Era. J Clin Med 11:416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antypas K, Wangberg SC (2012) E-Rehabilitation - an Internet and mobile phone based tailored intervention to enhance self-management of cardiovascular disease: study protocol for a randomized controlled trial. BMC Cardiovasc Disord 12:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aoyagi Y, Mori E, Ishii H, Kono Y, Sato A, Okochi Y, Funahashi R, Kagaya H (2021) Poor walking ability outcome and activities of daily living improvement in patients undergoing cardiac rehabilitation during COVID-19 pandemic. Eur J Phys Rehabil Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arena R, Myers J, Williams MA, Gulati M, Kligfield P, Balady GJ, Collins E, Fletcher G; American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Nursing (2007) Assessment of functional capacity in clinical and research settings: a scientific statement from the American Heart Association Committee on Exercise, Rehabilitation, and Prevention of the Council on Clinical Cardiology and the Council on Cardiovascular Nursing. Circulation 116:329–343. [DOI] [PubMed] [Google Scholar]
- Bailey SJ, Winyard PG, Vanhatalo A, Blackwell JR, DiMenna FJ, Wilkerson DP, Jones AM (2010) Acute L-arginine supplementation reduces the O2 cost of moderate-intensity exercise and enhances high-intensity exercise tolerance. J Appl Physiol 109:1394–1403. [DOI] [PubMed] [Google Scholar]
- Balady GJ, Ades PA, Bittner VA, Franklin BA, Gordon NF, Thomas RJ, Tomaselli GF, Yancy CW; American Heart Association Science Advisory and Coordinating Committee (2011) Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation 124:2951–2960. [DOI] [PubMed] [Google Scholar]
- Beatty AL, Schiller NB, Whooley MA (2012) Six-minute walk test as a prognostic tool in stable coronary heart disease: data from the heart and soul study. Arch Intern Med 172:1096–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bescós R, Rodríguez FA, Iglesias X, Ferrer MD, Iborra E, Pons A (2011) Acute administration of inorganic nitrate reduces VO(2peak) in endurance athletes. Med Sci Sports Exerc 43:1979–1986. [DOI] [PubMed] [Google Scholar]
- Besnier F, Dupuy EG, Gagnon C, Vincent T, Grégoire CA, Blanchette CA, Saillant K, Bouabdallaoui N, Grau JI, Bérubé B, et al. (2021) Investigation of the Effects of Home-Based Exercise and Cognitive Training on Cognitive and Physical Functions in Cardiac Patients: The COVEPICARDIO Study Protocol of a Randomized Clinical Trial. Front Cardiovasc Med 8:740834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borg DN, Costello JT, Bach AJ, Stewart IB (2017) Perceived exertion is as effective as the perceptual strain index in predicting physiological strain when wearing personal protective clothing. Physiol Behav 169:216–223. [DOI] [PubMed] [Google Scholar]
- Borg GA (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14:377–381. [PubMed] [Google Scholar]
- Brown TM, Hernandez AF, Bittner V, Cannon CP, Ellrodt G, Liang L, Peterson ED, Piña IL, Safford MM, Fonarow GC; American Heart Association Get With The Guidelines Investigators (2009) Predictors of cardiac rehabilitation referral in coronary artery disease patients: findings from the American Heart Association’s Get With The Guidelines Program. J Am Coll Cardiol 54:515–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Channon KM (2020) Exercise and cardiovascular health: new routes to reap more rewards. Cardiovasc Res 116:e56–e58. [DOI] [PubMed] [Google Scholar]
- Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T (2021) Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:2006–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Ascia SL, D’Ascia C, Marino V, Lombardi A, Santulli R, Chiariello M, Santulli G (2011) Cardiac resynchronisation therapy response predicts occurrence of atrial fibrillation in non-ischaemic dilated cardiomyopathy. Int J Clin Pract 65:1149–1155. [DOI] [PubMed] [Google Scholar]
- Damluji AA, Chung SE, Xue QL, Hasan RK, Moscucci M, Forman DE, Bandeen-Roche K, Batchelor W, Walston JD, Resar JR, et al. (2021) Frailty and cardiovascular outcomes in the National Health and Aging Trends Study. Eur Heart J 42:3856–3865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai K, Anbarasan D, Kayambu G, Yeo TJ (2021) Patient Perspectives on the Utilization of Telehealth in Cardiac Rehabilitation During COVID-19 Pandemic. J Cardiopulm Rehabil Prev 41:436–437. [DOI] [PubMed] [Google Scholar]
- Dibben GO, Dalal HM, Taylor RS, Doherty P, Tang LH, Hillsdon M (2018) Cardiac rehabilitation and physical activity: systematic review and meta-analysis. Heart 104:1394–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durante W, Liao L, Reyna SV, Peyton KJ, Schafer AI (2000) Physiological cyclic stretch directs L-arginine transport and metabolism to collagen synthesis in vascular smooth muscle. FASEB J 14:1775–1783. [DOI] [PubMed] [Google Scholar]
- Enright PL (2003) The six-minute walk test. Respir Care 48:783–785. [PubMed] [Google Scholar]
- Enright PL, Sherrill DL (1998) Reference equations for the six-minute walk in healthy adults. Am J Respir Crit Care Med 158:1384–1387. [DOI] [PubMed] [Google Scholar]
- Fiorentino G, Coppola A, Izzo R, Annunziata A, Bernardo M, Lombardi A, Trimarco V, Santulli G, Trimarco B (2021) Effects of adding L-arginine orally to standard therapy in patients with COVID-19: A randomized, double-blind, placebo-controlled, parallel-group trial. Results of the first interim analysis. EClinicalMedicine 40:101125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman DE, Racette SB, Toto PE, Peterson LR, Glynn NW, Pruskowski J, Byard T, Delligatti A, Lolley R, Mulkareddy V, et al. (2022) Modified Application of Cardiac Rehabilitation in Older Adults (MACRO) Trial: Protocol changes in a pragmatic multi-site randomized controlled trial in response to the COVID-19 pandemic. Contemp Clin Trials 112:106633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambardella J, Fiordelisi A, Spigno L, Boldrini L, Lungonelli G, Di Vaia E, Santulli G, Sorriento D, Cerasuolo FA, Trimarco V, et al. (2021a) Effects of Chronic Supplementation of L-Arginine on Physical Fitness in Water Polo Players. Oxid Med Cell Longev 2021:6684568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambardella J, Jankauskas SS, D’Ascia SL, Sardu C, Matarese A, Minicucci F, Mone P, Santulli G (2021b) Glycation of ryanodine receptor in circulating lymphocytes predicts the response to cardiac resynchronization therapy. J Heart Lung Transplant 21:02629–02622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambardella J, Khondkar W, Morelli MB, Wang X, Santulli G, Trimarco V (2020a) Arginine and Endothelial Function. Biomedicines 8:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambardella J, Morelli MB, Wang XJ, Santulli G (2020b) Pathophysiological mechanisms underlying the beneficial effects of physical activity in hypertension. J Clin Hypertens (Greenwich) 22:291–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grazzi G, Mazzoni G, Myers J, Codecà L, Pasanisi G, Napoli N, Guerzoni F, Volpato S, Conconi F, Chiaranda G (2016) Improved walking speed is associated with lower hospitalisation rates in patients in an exercise-based secondary prevention programme. Heart 102:1902–1908. [DOI] [PubMed] [Google Scholar]
- Green DJ, Hopman MT, Padilla J, Laughlin MH, Thijssen DH (2017) Vascular Adaptation to Exercise in Humans: Role of Hemodynamic Stimuli. Physiol Rev 97:495–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green DJ, Maiorana A, O’Driscoll G, Taylor R (2004) Effect of exercise training on endothelium-derived nitric oxide function in humans. J Physiol 561:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulsin GS, Henson J, Brady EM, Sargeant JA, Wilmot EG, Athithan L, Htike ZZ, Marsh AM, Biglands JD, Kellman P, et al. (2020) Cardiovascular Determinants of Aerobic Exercise Capacity in Adults With Type 2 Diabetes. Diabetes Care 43:2248–2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hama T, Ushijima A, Goto T, Nagamatsu H, Morita N, Yoshimachi F, Ikari Y, Kobayashi Y (2022) Effect of Cardiac Rehabilitation on Glomerular Filtration Rate Using Serum Cystatin C Concentration in Patients With Cardiovascular Disease and Renal Dysfunction. J Cardiopulm Rehabil Prev 42:E15–E22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong MY, Beidler J, Hooshmand S, Figueroa A, Kern M (2018) Watermelon and l-arginine consumption improve serum lipid profile and reduce inflammation and oxidative stress by altering gene expression in rats fed an atherogenic diet. Nutr Res 58:46–54. [DOI] [PubMed] [Google Scholar]
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, et al. ; ESC Scientific Document Group (2018) 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 39:119–177. [DOI] [PubMed] [Google Scholar]
- Jin H, Wei Q, Chen L, Sun Q, Zhang Y, Wu J, Ma G, Liu N (2014) Obstacles and alternative options for cardiac rehabilitation in Nanjing, China: an exploratory study. BMC Cardiovasc Disord 14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kambic T, Hadžić V, Lainscak M (2022) Optimising cardiopulmonary rehabilitation of long COVID-19 syndrome: are we there yet? Eur J Prev Cardiol zwac038. [DOI] [PubMed] [Google Scholar]
- Kawada T (2022) Clinical benefits in patients with home-based cardiac rehabilitation in the era of COVID-19 pandemic. Heart Lung. 52:197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kibel A, Lukinac AM, Dambic V, Juric I, Selthofer-Relatic K (2020) Oxidative Stress in Ischemic Heart Disease. Oxid Med Cell Longev 2020:6627144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AS, Franklin BA, Costa F, Balady GJ, Berra KA, Stewart KJ, Thompson PD, Williams MA, Lauer MS; American Heart Association; Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention); Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity); American association of Cardiovascular and Pulmonary Rehabilitation (2005) Cardiac rehabilitation and secondary prevention of coronary heart disease: an American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation 111:369–376. [DOI] [PubMed] [Google Scholar]
- Mabalirajan U, Ahmad T, Leishangthem GD, Joseph DA, Dinda AK, Agrawal A, Ghosh B (2010) Beneficial effects of high dose of L-arginine on airway hyperresponsiveness and airway inflammation in a murine model of asthma. J Allergy Clin Immunol 125:626–635. [DOI] [PubMed] [Google Scholar]
- Mone P, Gambardella J, Lombardi A, Pansini A, De Gennaro S, Leo AL, Famiglietti M, Marro A, Morgante M, Frullone S, et al. (2022a) Correlation of physical and cognitive impairment in diabetic and hypertensive frail older adults. Cardiovasc Diabetol 21:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mone P, Gambardella J, Minicucci F, Lombardi A, Mauro C, Santulli G (2021) Hyperglycemia Drives Stent Restenosis in STEMI Patients. Diabetes Care 44:e192–e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mone P, Gambardella J, Pansini A, Martinelli G, Minicucci F, Mauro C, Santulli G (2022b) Cognitive dysfunction correlates with physical impairment in frail patients with acute myocardial infarction. Aging Clin Exp Res 34:49–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mone P, Lombardi A, Gambardella J, Pansini A, Macina G, Morgante M, Frullone S, Santulli G (2022c) Empagliflozin improves cognitive impairment in frail older adults with type 2 diabetes and heart failure with preserved ejection fraction. Diabetes Care dc212434 (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mone P, Pansini A (2020) Gait Speed Test and Cognitive Decline in Frail Women With Acute Myocardial Infarction. Am J Med Sci 360:484–488. [DOI] [PubMed] [Google Scholar]
- Mone P, Pansini A, Jankauskas S, Varzideh F, Kansakar U, Lombardi A, Trimarco V, Frullone S, Santulli G (2022d) L-Arginine improves cognitive impairment in hypertensive frail older adults. Front Cardiovasc Med (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattadori G, Di Marco S, Baravelli M, Picozzi A, Ambrosio G (2022) Exercise Training in Post-COVID-19 Patients: The Need for a Multifactorial Protocol for a Multifactorial Pathophysiology. J Clin Med 11:2228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odegaard AO, Jacobs DR Jr, Sanchez OA, Goff DC Jr, Reiner AP, Gross MD (2016) Oxidative stress, inflammation, endothelial dysfunction and incidence of type 2 diabetes. Cardiovasc Diabetol 15:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opasich C, Pinna GD, Mazza A, Febo O, Riccardi PG, Capomolla S, Cobelli F, Tavazzi L (1998) Reproducibility of the six-minute walking test in patients with chronic congestive heart failure: practical implications. Am J Cardiol 81:1497–1500. [DOI] [PubMed] [Google Scholar]
- Phillips SA, Mahmoud AM, Brown MD, Haus JM (2015) Exercise interventions and peripheral arterial function: implications for cardio-metabolic disease. Prog Cardiovasc Dis 57:521–534. [DOI] [PubMed] [Google Scholar]
- Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT, Corrà U, Cosyns B, Deaton C, et al. ; ESC Scientific Document Group (2016) 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pio CSA, Chaves G, Davies P, Taylor R, Grace S (2019) Interventions to Promote Patient Utilization of Cardiac Rehabilitation: Cochrane Systematic Review and Meta-Analysis. J Clin Med 8:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poffley A, Thomas E, Grace SL, Neubeck L, Gallagher R, Niebauer J, O’Neil A (2017) A systematic review of cardiac rehabilitation registries. Eur J Prev Cardiol 24:1596–1609. [DOI] [PubMed] [Google Scholar]
- Pollentier B, Irons SL, Benedetto CM, Dibenedetto AM, Loton D, Seyler RD, Tych M, Newton RA (2010) Examination of the six minute walk test to determine functional capacity in people with chronic heart failure: a systematic review. Cardiopulm Phys Ther J 21:13–21. [PMC free article] [PubMed] [Google Scholar]
- Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, et al. ; ESC Scientific Document Group (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37:2129–2200. [DOI] [PubMed] [Google Scholar]
- Santulli G, Ciccarelli M, Trimarco B, Iaccarino G(2013)Physical activity ameliorates cardiovascular health in elderly subjects: the functional role of the β adrenergic system. Front Physiol.12:4–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell C, Daw P, Kerr C, Cleland J, Cowie A, Dalal HM, Ibbotson T, Murphy C, Taylor R (2020) Protocol for an implementation study of an evidence-based home cardiac rehabilitation programme for people with heart failure and their caregivers in Scotland (SCOT:REACH-HF). BMJ Open 10:e040771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu Y, Yang X, Wang L, Gao K, Jiang Z (2019) L-Arginine Inhibited Inflammatory Response and Oxidative Stress Induced by Lipopolysaccharide via Arginase-1 Signaling in IPEC-J2 Cells. Int J Mol Sci 20:1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes LZ, Figueroa J, Leake D, Khemani K, Kumari P, Bakshi N, Lane PA, Dampier C, Morris CR (2022) Safety of intravenous arginine therapy in children with sickle cell disease hospitalized for vaso-occlusive pain: A randomized placebo-controlled trial in progress. Am J Hematol 97:E21–E24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues-Krause J, Krause M, Rocha IMGD, Umpierre D, Fayh APT (2018) Association of l-Arginine Supplementation with Markers of Endothelial Function in Patients with Cardiovascular or Metabolic Disorders: A Systematic Review and Meta-Analysis. Nutrients 11:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruano-Ravina A, Pena-Gil C, Abu-Assi E, Raposeiras S, van ’t Hof A, Meindersma E, Bossano Prescott EI, González-Juanatey JR (2016) Participation and adherence to cardiac rehabilitation programs. A systematic review. Int J Cardiol 223:436–443. [DOI] [PubMed] [Google Scholar]
- Sardu C, Marfella R, Santulli G (2014) Impact of diabetes mellitus on the clinical response to cardiac resynchronization therapy in elderly people. J Cardiovasc Transl Res 7:362–368. [DOI] [PubMed] [Google Scholar]
- Schuler G, Hambrecht R, Schlierf G, Grunze M, Methfessel S, Hauer K, Kübler W (1992a) Myocardial perfusion and regression of coronary artery disease in patients on a regimen of intensive physical exercise and low fat diet. J Am Coll Cardiol 19:34–42. [DOI] [PubMed] [Google Scholar]
- Schuler G, Hambrecht R, Schlierf G, Niebauer J, Hauer K, Neumann J, Hoberg E, Drinkmann A, Bacher F, Grunze M, et al. (1992b) Regular physical exercise and low-fat diet. Effects on progression of coronary artery disease. Circulation 86:1–11. [DOI] [PubMed] [Google Scholar]
- Steven S, Frenis K, Oelze M, Kalinovic S, Kuntic M, Bayo Jimenez MT, Vujacic-Mirski K, Helmstädter J, Kröller-Schön S, Münzel T, et al. (2019) Vascular Inflammation and Oxidative Stress: Major Triggers for Cardiovascular Disease. Oxid Med Cell Longev 2019:7092151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adebayo A, Varzideh F, Wilson S, Gambardella J, Eacobacci M, Jankauskas SS, Donkor K, Kansakar U, Trimarco V, Mone Pet al. (2021)L-Arginine and COVID-19: An Update.Nutrients 13:3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suaya JA, Stason WB, Ades PA, Normand SL, Shepard DS (2009) Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol 54:25–33. [DOI] [PubMed] [Google Scholar]
- Tang XH, Gambardella J, Jankauskas S, Wang X, Santulli G, Gudas LJ, Levi R (2021) A Retinoic Acid Receptor β 2 Agonist Improves Cardiac Function in a Heart Failure Model. J Pharmacol Exp Ther 379:182–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RS, Dalal HM, McDonagh STJ (2022) The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat Rev Cardiol 19:180–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terbraak M, Verweij L, Jepma P, Buurman B, Jørstad H, Scholte Op Reimer W, van der Schaaf M (2022) Feasibility of home-based cardiac rehabilitation in frail older patients: a clinical perspective. Physiother Theory Pract 1–16. [DOI] [PubMed] [Google Scholar]
- Thompson S, Wiebe N, Arena R, Rouleau C, Aggarwal S, Wilton SB, Graham MM, Hemmelgarn B, James MT (2021) Effectiveness and Utilization of Cardiac Rehabilitation Among People With CKD. Kidney Int Rep 6:1537–1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tousoulis D, Kampoli AM, Tentolouris C, Papageorgiou N, Stefanadis C (2012) The role of nitric oxide on endothelial function. Curr Vasc Pharmacol 10:4–18. [DOI] [PubMed] [Google Scholar]
- van der Zwan LP, Scheffer PG, Dekker JM, Stehouwer CD, Heine RJ, Teerlink T (2011) Systemic inflammation is linked to low arginine and high ADMA plasma levels resulting in an unfavourable NOS substrate-to-inhibitor ratio: the Hoorn Study. Clin Sci (Lond) 121:71–78. [DOI] [PubMed] [Google Scholar]
- Vonk T, Bakker EA, Zegers ES, Hopman MTE, Eijsvogels TMH (2021) Effect of a personalised mHealth home-based training application on physical activity levels during and after centre-based cardiac rehabilitation: rationale and design of the Cardiac RehApp randomised control trial. BMJ Open Sport Exerc Med 7:e001159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl MP, Scalzo RL, Regensteiner JG, Reusch JEB (2018) Mechanisms of Aerobic Exercise Impairment in Diabetes: A Narrative Review. Front Endocrinol (Lausanne) 9:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson S, Mone P, Jankauskas SS, Gambardella J, Santulli G (2021) Chronic kidney disease: Definition, updated epidemiology, staging, and mechanisms of increased cardiovascular risk. J Clin Hypertens (Greenwich) 23:831–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y, Chi J, Lv W, Wang Y (2021) Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (Covid-19). Diabetes Metab Res Rev 37:e3377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoladz JA, Majerczak J, Duda K, Chłopicki S (2010) Endurance training increases exercise-induced prostacyclin release in young, healthy men--relationship with VO2max. Pharmacol Rep 62:494–502. [DOI] [PubMed] [Google Scholar]