Heart failure (HF) is a serious chronic condition affecting older people globally. In 2016, the American Heart Association (AHA) highlighted drugs that may cause or exacerbate HF to assist healthcare providers1. Previous studies have investigated the prescribing pattern of HF-exacerbating medications among older adults in hospital-based practices2, the prevalence of HF-exacerbating medication use among ambulatory adult patients based on the National Health and Nutrition Examination Survey (NHANES)3, and the prevalence of prescribing potentially harmful medications to Medicare patients with HF4. However, no studies have investigated the prescribing trend of HF-exacerbating medications among older outpatients by office-based physicians in the US. We aimed to estimate national prescription trends of HF-exacerbating medications prescribed by office-based physicians among older ambulatory patients with HF.
We conducted an observational study using data collected from 2012 to 2016 through the National Ambulatory Medical Care Survey. If a patient had any diagnostic code (International Classification of Diseases, Ninth Revision (ICD-9) codes 428 in 2012-2015 and Tenth Revision (ICD-10) codes I-50.x in 2016) for HF and was over 65 years old, they were included. Even if no ICD code for HF existed, the patient was included if HF was indicated in the patient’s records. We estimated the prevalence among patients who were prescribed HF-exacerbating medications with a magnitude that could have led to hospitalization and with a high level of evidence to support the potential for harm. We used population weights provided by the Centers for Disease Control and Prevention to generate a national estimate.
Among patients with HF, the average prescription prevalence for HF-exacerbating medications over the 5-year study period was 21% and increased over the observed study period. Among the medications, cyclooxygenase (COX) nonselective inhibitors (nonsteroidal anti-inflammatory drugs, NSAIDs) were the most commonly prescribed, followed by citalopram, diltiazem, and sitagliptin (Figure 1).
Figure 1.
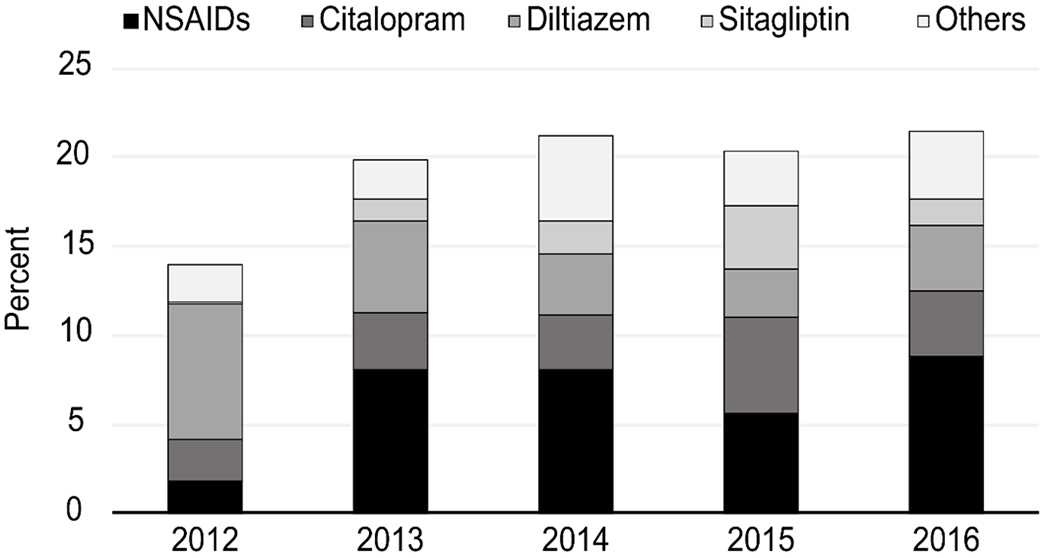
Proportion of older patients with heart failure who required ambulatory care visits because of heart failure-exacerbating medications prescribed by office-based physicians in 2012-2016. Other medications listed in Figure 1 are sotalol, saxagliptin, dronedarone, COX-2 inhibitors, thiazolidinediones, verapamil, appetite suppressants, pramipexole, TNF-alpha inhibitors, cilostazol, and flecainide.
The results are of serious concern given that this analysis was limited to medications with strong scientific evidence of potential harm among patients with HF. The prevalence of HF-exacerbating medications in our study was lower than that in previous studies2–4. However, it is noteworthy that the prescription prevalence for inappropriate medications increased over time. In particular, our results showed that the use of COX-2-selective inhibitors decreased, whereas the use of nonselective NSAIDs persisted. Such a high prevalence of HF-exacerbating medications may be explained by the fact that older adults with HF also have multiple comorbidities requiring other medications. These results hold critical value by becoming the foundation for future studies to determine appropriate NSAID utilization and promote deprescribing for older outpatients with HF by office-based physicians. This study has important limitations. First, this was an observational and cross-sectional study. We did not control for confounders such as other comorbidities that warranted the use of any medications. Second, we assessed the data from 2012 to 2016, and these data predate the AHA scientific statement regarding medications that exacerbate HF. Therefore, contemporary studies are needed.
In conclusion, our study demonstrates that almost 1/5 of older adults with HF were prescribed HF-exacerbating medications by office-based physicians in the US.
Footnotes
Disclosures
The authors have no conflicts of interest to disclose.
References
- 1.Page RL, O’Bryant CL, Cheng D, Dow TJ, Ky B, Stein CM, Spencer AP, Trupp RJ, Lindenfeld J. Drugs that may cause or exacerbate heart failure: a scientific statement from the american heart association. Circulation 2016; 134: e32–69. [DOI] [PubMed] [Google Scholar]
- 2.Goyal P, Kneifati-Hayek J, Archambault A, Mehta K, Levitan EB, Chen L, Diaz I, Hollenberg J, Hanlon JT, Lachs MS, Maurer MS, Safford MM. Prescribing Patterns of Heart Failure-Exacerbating Medications Following a Heart Failure Hospitalization. JACC Heart Fail 2020; 8: 25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kneifati-Hayek J, Kennel P, Bryan J, Safford MM, Goyal P. Use of heart failure exacerbating medications among adults with heart failure. J Card Fail 2019; 25: 72–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Almodóvar AS, Nahata MC. Potentially Harmful Medication Use Among Medicare Patients with Heart Failure. Am J Cardiovasc Drugs 2020; 20: 603–610. [DOI] [PubMed] [Google Scholar]


