Abstract
Aim
This study aimed to determine whether family‐centred care (FCC) intervention reduces the ICU delirium prevalence.
Design
A systematic review and meta‐analysis.
Methods
The databases, including PubMed, Cochrane Central Register of Controlled Trials, Web of Science, CINAHL Complete, China National Knowledge Infrastructure (CNKI), China Biology Medicine disc (CBMdisc), WANFANG Data and VIP Information, were systematically searched up to 30 November 2021. The search term includes keywords related to intensive care units, delirium and family‐centred care. Meta‐analyses were performed and presented by risk ratio (RR), mean difference (MD) and corresponding 95% confidence intervals (CIs).
Results
The meta‐analysis results showed that compared with the usual care, FCC intervention has positive effects on reducing ICU delirium prevalence [RR = 0.54, 95% CIs (0.36, 0.81), p < .05]. However, no effect was observed on ICU stays, mechanical ventilation duration and ICU‐acquired infection between the two groups.
Conclusions
Family‐centred care is an effective intervention to reduce the ICU delirium prevalence. But the result should be treated cautiously as the high levels of heterogeneity, further high‐quality studies are required to determine the effectiveness of FCC intervention in the ICU setting.
Keywords: delirium, family‐centred care, intensive care unit, meta‐analysis
1. INTRODUCTION
Delirium is defined as a neuropsychiatric disorder, which is marked by a fluctuating level of consciousness with impairment of attention and cognition, and disturbed sleep–wake cycles (Maldonado, 2017; Pandharipande et al., 2017). It should be stressed that intensive care unit (ICU) delirium is a vital issue as its incidence ranges from 32% to 87% (Kotfis et al., 2018; Krewulak et al., 2018). For patients, it can result in an increased risk of mortality, infection and readmissions; prolong hospital stay; and increase the cost of hospitalization, further aggravating the associated medical and social burdens (Kalabalik et al., 2014; Vasilevskis et al., 2018). Family members are also greatly affected by patients’ delirium with 75% suffering from anxiety (Partridge et al., 2013; Racine et al., 2019). Recently, the use of non‐pharmacological interventions has been recommended by guidelines (Devlin et al., 2018) and gained considerable attention.
Family‐centred care (FCC) is a non‐pharmacological intervention emphasizing partnership between family members and medical staff (Isaacs, 2020; O'Connor et al., 2019), in which medical staff needs to establish a cooperative relationship with family members, share information and support them to participate in patient's care activities (Park et al., 2018). It acknowledges the essential contribution that family members often make by acting as patients’ representatives. Family‐centred care guidelines (Davidson et al., 2017) recommend more family support and company for ICU patients, however, conflicting evidence of an FCC intervention effect on delirium (Black et al., 2011; McKenzie & Joy, 2020; Rosa et al., 2019). To date, only one systematic review has been published on the effectiveness of FCC on delirium, of which only two articles focused on ICU patients, and a meta‐analysis was not performed. Therefore, it is well warranted to conduct a systematic review to explore the efficacy of FCC intervention to reduce ICU delirium.
2. METHODS
The present systematic review and meta‐analysis complied with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines and was registered on PROSPERO (CRD42020223386).
2.1. Search strategy
We searched the following electronic databases: PubMed, Cochrane Central Register of Controlled Trials, Web of Science, CINAHL Complete, China National Knowledge Infrastructure (CNKI), China Biology Medicine disc (CBMdisc), WANFANG Data and VIP Information. The retrieval strategy uses a combination of subject words and free words. Search terms for English electronic databases were as follows: (Intensive Care Units[MeSH] OR Critical illness OR Critical Care OR Intensive Care OR critical* ill*) AND (delirium[MeSH] OR deliri* OR acute confusion* OR acute organic psychosyndrome OR acute brain syndrome OR metabolic encephalopathy OR acute psycho‐organic syndrome OR clouded state OR clouding of consciousness OR exogenous psychosis) AND (family‐centered OR family‐centered OR partner* OR participat* OR presence OR involv* OR decision* OR communicat* OR negotiat* OR collaborat* OR visit*) AND (intervention OR program OR nursing OR treat* OR manage* OR protocol* OR prevent* OR reduc*). The final search was conducted on 30 November 2021. Hand searching of the literature references was also used during the same period.
2.2. Inclusion and exclusion criteria
The inclusion criteria were formulated based on the PICOS (population, intervention, comparison, outcome and study design) framework. Participants (P): ICU patients at least 18 years old; Intervention (I): used FCC intervention in the experimental group. In this review, FCC intervention was defined as family members’ involvement in any of the following tasks (McKenzie & Joy, 2020): reorienting the patient; completing sensory checks; cognitive stimulation; reminiscing; and completing environmental changes. Comparison (C): involved a comparison with no intervention or usual care; Outcomes (O): Studies resulted in the assessment of one or more of the following outcomes—the delirium prevalence (primary endpoint); delirium duration; mechanical ventilation duration; length of ICU stay; ICU‐acquired infection; and family satisfaction, anxiety and depression; Study design(S): randomized controlled trials (RCTs) or quasi‐RCTs. Languages were restricted to English and Chinese. Exclusion criteria: (1) the full text cannot be obtained after contacting the original authors; (2) literature reviews, meta‐analyses, case reports or meeting abstracts without original data.
2.3. Data extraction and study quality
All identified studies were inputted into EndNote software version X8. Two researchers independently screened the retrieved literature based on the inclusion and exclusion criteria, assessed methodological quality and extracted the data. Any disagreements were resolved by discussion with help of a third expert when needed. We extracted the following literature data: title, first author, year of publication, country, study design, study setting, study participants, intervention details, diagnostic methods of delirium and outcomes. The quality of the included study in our meta‐analysis was evaluated according to Cochrane 5.1.0 (Higgins et al., 2011). It includes seven aspects, and each one is divided into three levels: low, unclear or high risk of bias. Then, the trials were categorized as ‘A’ (all the items had a low risk of bias), ‘B’ (at least one item had an unclear risk of bias) or ‘C’ (at least one item had a high risk of bias). Any discrepancy concerning quality assessment was settled through a discussion.
2.4. Statistical analysis
The meta‐analysis was conducted using RevMan5.3, and p < .05 was considered statistically significant. The inverse variance method with the mean difference (MD) and 95% confidence intervals (CI) as the measure of an effect estimate was used for continuous variables, whereas the Mantel–Haenszel method with risk ratio (RR) with 95% CIs was employed for dichotomous variables. Before the combined data were analysed by meta‐analysis, the heterogeneity of each group was tested. When no obvious heterogeneity exists (p > .10, I 2 < 50%), a fixed‐effect model was used. If heterogeneity was detected (p ≤ .01, I 2 ≥ 50%), a random‐effects model was adopted. If it is not available to conduct a meta‐analysis, we only described the data. In addition, exploratory analyses including subgroup analyses and sensitivity analyses may be performed for the primary outcome to attempt to explain any substantial heterogeneity. Furthermore, publication bias was measured using a funnel plot.
3. RESULTS
3.1. Study selection
We identified a total of 3416 records from electronic searching and no additional articles were located as a result of hand searching. After removing duplicates (n = 1029), 2387 studies were reviewed in phase one screening and 2232 articles were deemed ineligible for inclusion by screening the titles and abstracts. Then, we assessed 155 full‐text articles at the eligibility phase. The systematic review and meta‐analysis were finally included seven studies published in 2010–2021. The flowchart of the study selection process is depicted in Figure 1.
FIGURE 1.
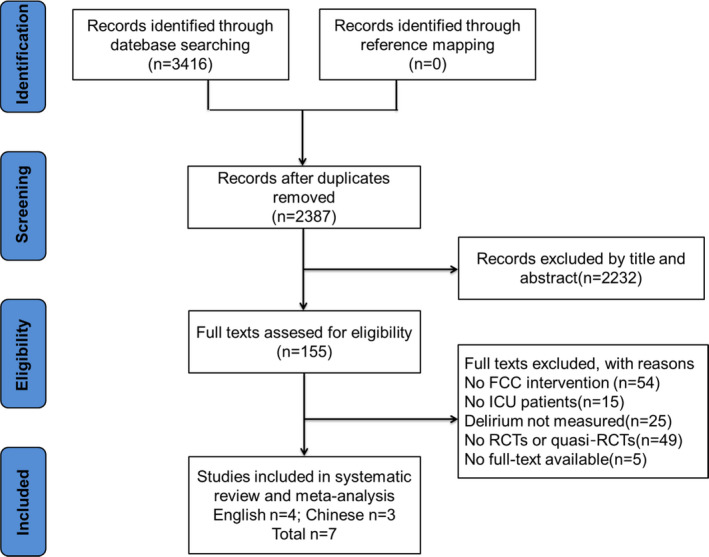
Flow diagram of the study selection
3.2. Study characteristics
The study characteristics of the included studies are presented in Table 1. Among the included studies, three studies were RCTs and four were quasi‐RCTs. The total sample size of included studies was 2662 (range 61–1685), of which 1342 (50.4%) patients were assigned to the FCC group, 1320 (49.6%) patients to the control group. Most studies used multi‐component intervention, and two studies (Black et al., 2011; Rosa et al., 2019) used single‐component intervention. The techniques used for screening for delirium were the confusion assessment method for the intensive care unit (CAM‐ICU) (Eghbali‐Babadi et al., 2017; Mitchell et al., 2017; Rosa et al., 2019; Gan Xiaoqing et al., 2017; Xueping. et al., 2021) and the intensive care delirium screening checklist (ICDSC) (Black et al., 2011; Hong et al., 2015).
TABLE 1.
Characteristics of the included studies
| Reference | Year | Country | Design | Settings | Study participants | Intervention | Outcome | Diagnostic methods of delirium | Quality |
|---|---|---|---|---|---|---|---|---|---|
| Ma et al. | 2015 | China | Quasi‐ RCTs | ICU | Intervention 84 control 80 | Family participation nursing (individual assessment of patients, elimination of potential risks, guidance of patients to produce benign stress response and improvement of patients’ psychological stability) | ① | ICDSC | B |
| Gan et al. | 2017 | China | Quasi‐ RCTs | ICU | Intervention 213 control 178 | Family participation in nursing (20‐min video visit to 30‐min face‐to‐face visit, participate in life care and functional exercise) | ①②③④ | CAM‐ICU | C |
| Jiao et al. | 2021 | China | Quasi‐RCTs | ICU | Intervention 82 control 82 | Family participation nursing (give patients cognitive function training, participate in life care and functional exercise) | ①③④⑥ | CAM‐ICU | C |
| Black et al. | 2010 | Northern Ireland | Quasi‐RCTs | ICU | Intervention 69 control 69 | Nurse‐facilitated family participation in psychological care | ①③ | ICDSC | C |
| Mitchell et al. | 2017 | Australia | RCTs | ICU | Intervention 29 control 32 | Give patient the targeted training, memory induction and avoidance of sensory deprivation | ①⑤ | CAM‐ICU | C |
| Eghbali‐Babadi et al. | 2017 | Iran | RCTs | CSICU | Intervention 34 control 34 | Extension of ICU visiting hours (30–40 min a day), give patient the targeted training, memory induction and avoidance of sensory deprivation | ① | CAM‐ICU | B |
| Rosa et al. | 2019 | Australia | RCTs | ICU | Intervention 837 control 848 | extension of ICU visiting hours (from 4.5–12 hr at most) | ①②③④⑥⑦ | CAM‐ICU | B |
①delirium prevalence; ②mechanical ventilation duration; ③length of ICU stay; ④family satisfaction; ⑤delirium duration; ⑥ICU‐acquired infection; ⑦family anxiety and depression.
Abbreviations: CAM‐ICU, Confusion Assessment Method for the Intensive Care Unit; CSICU, Cardio‐surgery Intensive Care Units; ICDSC, Intensive Care Delirium Screening Checklist; ICU, Intensive Care Units; RCTs, Randomized Controlled Trials.
3.3. Study quality
Three studies were rated ‘B’, and four rated ‘C’, which suggests a high risk of bias. Among them, three studies had a high risk of random sequence generation, and two reported allocation concealment. In most studies, patients or researchers were not blinded because of the nature of the intervention considered in the present review. The quality of the included studies is shown in Figures 2 and 3.
FIGURE 2.
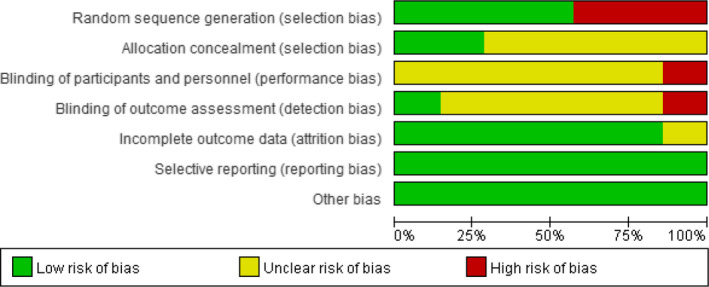
Risk of bias graph: A review of authors’ judgements regarding each risk of bias item presented as percentages across all included studies
FIGURE 3.
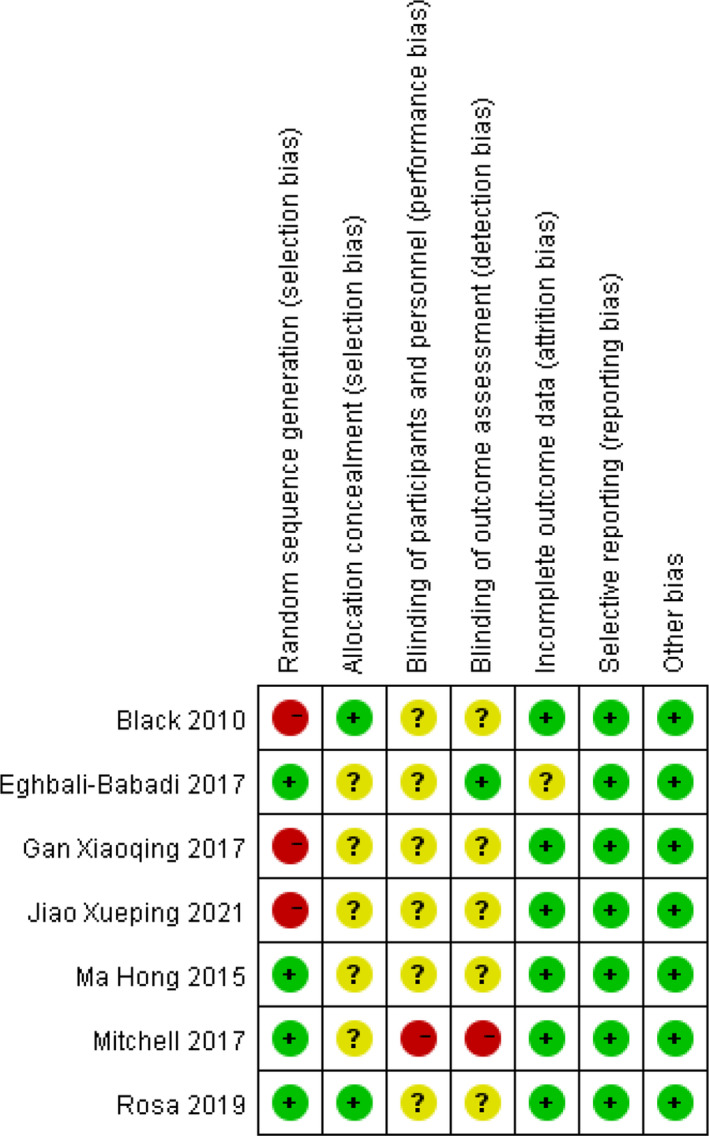
Risk of bias summary: A review of authors’ judgements regarding each risk of bias item for each included study
3.4. Study outcomes
3.4.1. Delirium
All included studies reported delirium prevalence as an outcome measure. According to the results of the heterogeneity test, there was statistically significant heterogeneity among the studies (I 2 = 87%, p < .001). Therefore, a random‐effect model was used to compare the effect value. Figure 4a demonstrates that the delirium prevalence in the FCC group was statistically significantly lower than in the control group [RR = 0.54, 95% CIs (0.36, 0.81), p = .003]. To explore the sources of heterogeneity, subgroup analyses for delirium prevalence were conducted by the FCC component, study design and region as shown in Table 2. When subgroups were stratified by FCC component, we found a significant effect of multi‐component subgroup [RR = 0.50, 95% CIs (0.30, 0.81), p = .005]. However, there were no significant differences in the single‐component subgroup. After sensitivity analyses, more concentrated results were obtained in the multi‐component subgroup, changing from [RR = 0.50, 95% CIs (0.30, 0.81), p = .005] to [RR = 0.39, 95% CIs (0.30, 0.51), p < .001]. When the different study design was considered, summary effects were only statistically significant in the quasi‐RCTs subgroup [RR = 0.41, 95% CIs (0.32, 0.51), p < .001], whereas no significance was found in the RCTs subgroup. After sensitivity analysis, the quasi‐RCTs [RR = 0.46, 95% CIs (0.36, 0.58), p < .001] subgroup was effective and was slightly different. In terms of regions, FCC intervention has a significant effect in the China subgroup [RR = 0.40, 95% CIs (0.29, 0.56), p < .001], but not in the other country subgroup. After sensitivity analysis, more concentrated results were obtained in the China subgroup [RR = 0.48, 95% CIs (0.35, 0.66), p < .001]. The sensitivity analysis is shown in Table 3.
FIGURE 4.
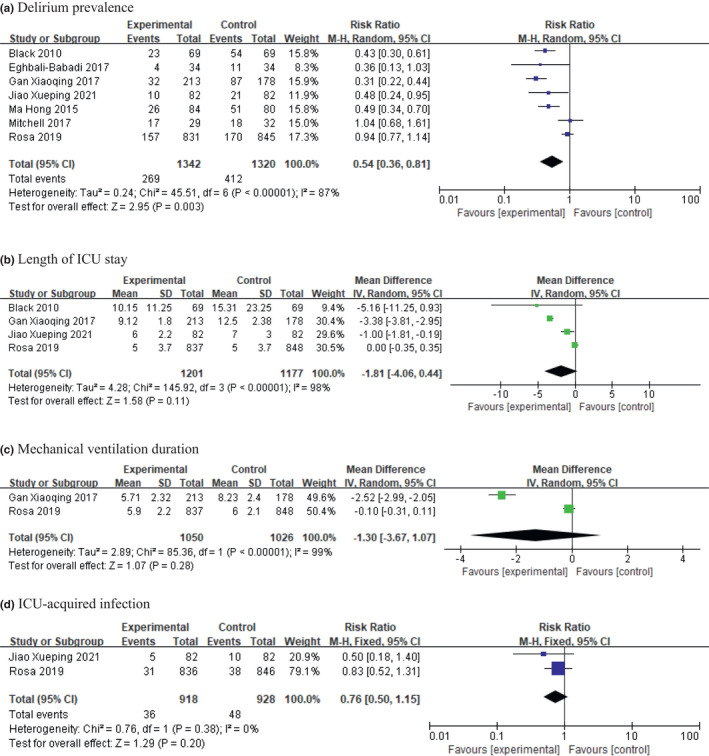
Forrest plots of the effect of family‐centred care on ICU patients; (a) delirium prevalence; (b) length of ICU stay; (c) mechanical ventilation duration; (d) ICU‐acquired infection
TABLE 2.
Subgroup analysis on effects of FCC intervention on delirium prevalence
| Categories | No. of studies | No. of patients | Pooled RR (95% CI) | Heterogeneity | ||
|---|---|---|---|---|---|---|
| Random | p‐Value | I² (%) | p‐Value | |||
| FCC component | ||||||
| Single‐component | 2 | 1814 | 0.64 (0.29, 1.40) | 0.260 | 93 | <0.001 |
| Multi‐component | 5 | 848 | 0.50 (0.30, 0.81) | 0.005 | 80 | <0.001 |
| Study design | ||||||
| RCTs | 3 | 1805 | 0.90 (0.65, 1.24) | 0.500 | 42 | 0.180 |
| Quasi‐RCTs | 4 | 857 | 0.41 (0.32, 0.51) | <0.001 | 18 | 0.300 |
| Region | ||||||
| China | 3 | 719 | 0.40 (0.29, 0.56) | <0.001 | 43 | 0.170 |
| Other countries | 4 | 1943 | 0.68 (0.42, 1.11) | 0.120 | 84 | <0.001 |
Abbreviations: CI, confidence interval; FCC, Family‐centred Care; RR, risk ratio. Bold values are statistically significant.
TABLE 3.
Sensitivity analysis on effects of FCC intervention on delirium prevalence
| Outcome | Before sensitivity analysis | Remove study | After sensitivity analysis | ||||
|---|---|---|---|---|---|---|---|
| Effect estimate | p | I 2 (%) | Effect estimate | p | I 2 (%) | ||
| Delirium prevalence | 0.54 (0.36, 0.81) | 0.003 | 87 | Mitchell et al., (2017); Rosa et al., (2019) | 0.40 (0.33, 0.49) | <0.001 | 0 |
| FCC component | |||||||
| Multi‐component | 0.50 (0.30, 0.81) | 0.005 | 80 | Mitchell et al., (2017) | 0.39 (0.30, 0.51) | <0.001 | 16 |
| Study design | |||||||
| Quasi‐RCTs | 0.41 (0.32, 0.51) | <0.001 | 18 | Gan Xiaoqing et al., (2017) | 0.46 (0.36, 0.58) | <0.001 | 0 |
| Region | |||||||
| China | 0.40 (0.29, 0.56) | <0.001 | 43 | Gan Xiaoqing et al., (2017) | 0.48 (0.35, 0.66) | <0.001 | 0 |
Abbreviations: CI, confidence interval; FCC, Family‐centred care; RR, risk ratio.
Only one study (Mitchell et al., 2017) reported delirium duration, and therefore, a meta‐analysis could not be performed. It showed that the average number of delirium duration in the FCC intervention group and usual care group was 1 day, and the difference was not statistically significant (p > .05).
3.4.2. Length of ICU stay
The length of ICU stay was reported in three studies (Black et al., 2011; Gan Xiaoqing et al., 2017; Rosa et al., 2019; Xueping. et al., 2021). A heterogeneity test showed that there was significant heterogeneity across studies (I 2 = 98%, p < .001). The random‐effect model was used to consolidate the effect value; the result shows that the length of ICU stay was not significantly different between the two groups [MD = −1.81, 95% CIs (−4.06, 0.44), p = .110) (Figure 4b).
3.4.3. Mechanical ventilation duration
Two studies (Gan Rosa et al., 2019; Xiaoqing et al., 2017) provided data on the duration of mechanical ventilation. We found no evidence of a beneficial effect of FCC intervention on mechanical ventilation duration [MD = −1.30, 95% CIs (−3.67, 1.07), p = .280)] (Figure 4c).
3.4.4. ICU‐acquired infection
Two studies (Rosa et al., 2019; Xueping. et al., 2021) reported data on the ICU‐acquired infection prevalence, and the result reveals no statistically significant differences between the two groups [RR = 0.76, 95% CIs (0.50, 1.17), p = .200)] (Figure 4d).
3.4.5. Family satisfaction
Two studies (Rosa et al., 2019; Xueping. et al., 2021) evaluated the effect of FCC intervention on family satisfaction. Between them, one study (Rosa et al., 2019) used the critical care family needs inventory (CCFNI) to assess within the first 7 days of patient discharge from the ICU and the other (Xueping. et al., 2021) used the Chinese critical care family satisfaction survey (C‐CCFSS) to assess within the first 14 days of patient discharge from the ICU. The data of each study are described in different ways, so descriptive analysis is used. Both studies showed that FCC intervention could significantly improve the satisfaction score of family members (p < .05).
3.4.6. Family anxiety and depression
One study (Rosa et al., 2019) evaluated the effect of FCC intervention on family anxiety and depression using the hospital anxiety and depression scale (HADS) when the patient was discharged from the ICU for the first 7 days. The results showed that compared to the usual care, FCC intervention could relieve the depression and anxiety symptoms of family members (p < .05).
3.5. Publication bias
The funnel plot of delirium was visually symmetric, which showed no significant publication risk bias (see Figure 5). Most of the included studies focused on the top of the funnel, which further demonstrated that this review is credible.
FIGURE 5.
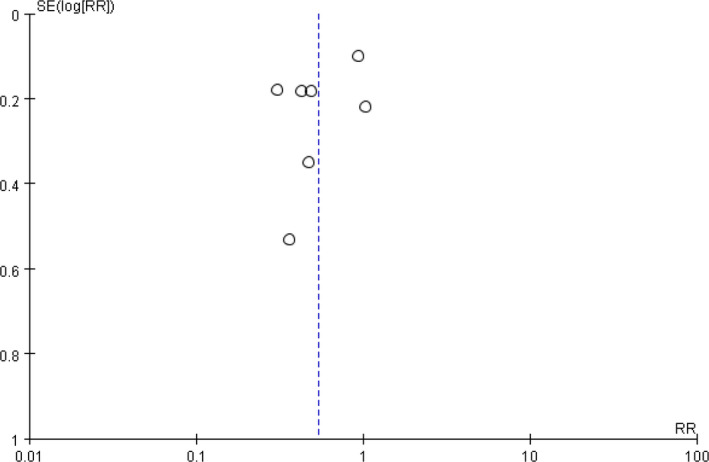
Funnel plot obtained using data from seven trials comparing the delirium in ICU prevalence patients
4. DISCUSSION
In recent years, increasing attention has been paid to FCC intervention in the ICU setting, but its effect on ICU delirium prevalence has not been confirmed. Our study finds that compared to the usual care, FCC intervention has positive effects on reducing delirium prevalence, especially in multi‐component intervention, which was consistent with the results of McKenzie & Joy, (2020); and it may ease depression and anxiety symptoms of family members and improve their satisfaction; however, no effect was observed on ICU days, mechanical ventilation duration and ICU‐acquired infection between the two groups. This systematic review provides a reference for the medical staff regarding the effectiveness of FCC intervention on ICU patients; however, the results should be treated cautiously as the difference in intervention measures of each study.
Previous studies have suggested that fear of the ICU setting is a primary determinant of ICU delirium (Madrid‐Navarro et al., 2015), and ICU patients without family visits have more than a threefold increased risk of delirium (Van Rompaey et al., 2009). The unfamiliar ICU setting, the noisy equipment and instruments, as well as patients’ suspicions about the disease readily cause psychological stress to patients, for example, fear or tension. Considering ICU‐acquired infection, disorganization of care and medical workload, most ICUs still adopt a strict visiting system (Garrouste‐Orgeas et al., 2016b; Nassar Junior et al., 2018). Patients are highly vulnerable to separation anxiety due to less support provided by family members, and it can contribute to delirium (Baron et al., 2015). Family involvement now has been widely applied in delirium management bundles (Balas et al., 2016), which is an effective social support system and plays a major role in the treatment of ICU patients.
Our findings suggest that FCC intervention has positive effects on reducing ICU delirium prevalence. The majority of included studies increased family visiting time or controlled the visiting times flexibly (Eghbali‐Babadi et al., 2017; Gan Xiaoqing et al., 2017; Rosa et al., 2019), which can engage ICU patients with their family members longer time, enable them to fully feel the support of relatives and friends and facilitate adaptation to environmental changes (Garrouste‐Orgeas et al., 2016a; Yakubu et al., 2019). In addition, the targeted training, memory induction and avoidance of sensory deprivation provided by family members (Eghbali‐Babadi et al., 2017; Mitchell et al., 2017) may improve patients’ perception of the environment, relieve fear and alleviate tension and anxiety (Piao et al., 2018). Only one study (Mitchell et al., 2017) reported the outcome of delirium duration, and it is still unclear whether the participation of family members will directly affect it; future studies are needed to further explore this matter. Despite the existence of advocacy, there are still challenges in the uptake and adoption of FCC practices in adult critical care, including high‐demand daily jobs, healthcare provider beliefs, organizational culture etc. (Thirsk et al., 2021). As such, FCC interventions need to be more rigorously designed, for better clinical practices. We found FCC intervention did not have positive effects on ICU days and mechanical ventilation duration, the reason maybe lies in the single interventions in the included studies did not sufficient for these outcomes.
The current study also reveals that FCC intervention has a beneficial effect on relieving families’ anxiety and depression symptoms and improving their satisfaction scores, and the result was in line with the finding of a previous study (Goldfarb et al., 2017). But the present result was descriptive and should be viewed with caution. While patients experience physiological crises, family members may be in a state of psychological crisis. Previous studies pointed out that the ICU setting may contribute to family emotional distress negative emotional distress from lack of information, uncertainty, and lack of support for joint decision‐making (Roze des Ordons et al., 2020; Schmitt et al., 2019; Wong et al., 2019a). Frequent communication generates a better family understanding of the healthcare process and families can receive timely and accurate information, thus meeting their information needs and effectively participating in decision‐making (Hönig & Gündel, 2016). In addition, it promotes family participation in the living care of patients, relatives may feel a sense of usefulness and self‐worth since they contribute to patients’ rehabilitation process (Kang et al., 2020; Wong et al., 2019b; Yakubu et al., 2019). Thus, medical staff should raise awareness of the important role of family members in patients’ rehabilitation process.
5. LIMITATIONS
This systematic review has several limitations. First, this review included only English and Chinese studies, potentially introducing language biases. The terms we used in the search strategy may have been insufficient to contain all the relevant interventions, and the number of included studies was somewhat small (only seven articles). Second, there was high‐level heterogeneity among the included studies which may come from the difference in FCC component, region or duration of intervention. Thirdly, the adverse outcome only included ICU‐acquired infection; other adverse outcomes, for example, mortality or unplanned extubation, were not included in this review, which limits its use in clinical practice to some extent. Finally, some of the literature included in this study is of low quality because of its design, limiting the strength of the conclusions. Therefore, the results in this study should be generalized with caution and are necessary to implement high‐quality studies with rigorous methods to be confirmed further.
6. CONCLUSION
In conclusion, FCC as a non‐pharmacological intervention has positive effects on reducing ICU delirium prevalence, but the results should be treated cautiously as the quality of the studies was low. In the future, a large sample size and high‐quality studies are required to verify the outcomes of this meta‐analysis, and then provide an early basis for the clinical intervention of delirium.
CONFLICT OF INTEREST
The author reports no conflicts of interest in this work.
AUTHOR CONTRIBUTIONS
Lingyu Lin and Yanchun Peng conceived of and designed the study; Yanjuan Lin and Liangwan Chen supported the administration; Haoruo Zhang and Xizhen Huang contributed in the provision of study materials or patients; Lingyu Lin and Yanjuan Lin were involved in the collection and assembly of data; Lingyu Lin and Haoruo Zhang were involved in data analysis. All authors drafted and gave the final approval of the manuscript.
ETHICAL APPROVAL
This study was based on previously published studies; therefore, ethical approval and patient consent were not required.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Lin Li and Qiong Pan for their feedback on the meta‐analysis and expert advice during the writing of the manuscript.
Lin, L. , Peng, Y. , Zhang, H. , Huang, X. , Chen, L. , & Lin, Y. (2022). Family‐centred care interventions to reduce the delirium prevalence in critically ill patients: A systematic review and meta‐analysis. Nursing Open, 9, 1933–1942. 10.1002/nop2.1214
Yanjuan Lin and Liangwan Chen are co‐corresponding authors.
Lingyu Lin and Yanchun Peng are the first co‐authors.
Funding information
This work was supported by the Joint Finds for the Innovation of Science and Technology, Fujian Province (No.2017Y9052); Guiding Project of Fujian Science and Technology (No.2021Y0023); and Fujian Key Laboratory of Cardio‐Thoracic Surgery (Union Hospital, Fujian Medical University)
Contributor Information
Lingyu Lin, Email: 914331343@qq.com.
Yanchun Peng, Email: 1078494566@qq.com.
Haoruo Zhang, Email: 724403400@qq.com.
Xizhen Huang, Email: xwk_hxzh@qq.com.
Liangwan Chen, Email: chenliangwan@tom.com.
Yanjuan Lin, Email: fjxhyjl@163.com, Email: chenliangwan@tom.com.
DATA AVAILABILITY STATEMENT
The data used to support the findings of this study are available from the corresponding author on reasonable request.
REFERENCES
- Balas, M. C. , Devlin, J. W. , Verceles, A. C. , Morris, P. , & Ely, E. W. (2016). Adapting the ABCDEF bundle to meet the needs of patients requiring prolonged mechanical ventilation in the long‐term acute care hospital setting: Historical perspectives and practical implications. Seminars in Respiratory & Critical Care Medicine, 37(1), 119–135. 10.1055/s-0035-1570361 [DOI] [PubMed] [Google Scholar]
- Baron, R. , Binder, A. , Biniek, R. , Braune, S. , Buerkle, H. , Dall, P. , Demirakca, S. , Eckardt, R. , Eggers, V. , Eichler, I. , Fietze, I. , Freys, S. , Fründ, A. , Garten, L. , Gohrbandt, B. , Harth, I. , Hartl, W. , Heppner, H.‐J. , & Horter, J. … Weisshaar, G. (2015). Evidence and consensus based guideline for the management of delirium, analgesia, and sedation in intensive care medicine. Revision 2015 (DAS‐Guideline 2015) ‐ short version. German Medical Science Gms E Journal, 13, Doc19. doi: 10.3205/000223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black, P. , Boore, J. R. , & Parahoo, K. (2011). The effect of nurse‐facilitated family participation in the psychological care of the critically ill patient. Journal of Advanced Nursing, 67(5), 1091–1101. 10.1111/j.1365-2648.2010.05558.x [DOI] [PubMed] [Google Scholar]
- Davidson, J. E. , Aslakson, R. A. , Long, A. C. , Puntillo, K. A. , Kross, E. K. , Hart, J. , Cox, C. E. , Wunsch, H. , Wickline, M. A. , Nunnally, M. E. , Netzer, G. , Kentish‐Barnes, N. , Sprung, C. L. , Hartog, C. S. , Coombs, M. , Gerritsen, R. T. , Hopkins, R. O. , Franck, L. S. , Skrobik, Y. , … Curtis, J. R. (2017). Guidelines for Family‐Centered Care in the Neonatal, Pediatric, and Adult ICU. Critical Care Medicine, 45(1), 103–128. 10.1097/ccm.0000000000002169 [DOI] [PubMed] [Google Scholar]
- Devlin, J. W. , Skrobik, Y. , Gélinas, C. , Needham, D. M. , Slooter, A. J. C. , Pandharipande, P. P. , Watson, P. L. , Weinhouse, G. L. , Nunnally, M. E. , Rochwerg, B. , Balas, M. C. , van den Boogaard, M. , Bosma, K. J. , Brummel, N. E. , Chanques, G. , Denehy, L. , Drouot, X. , Fraser, G. L. , Harris, J. E. , … Alhazzani, W. (2018). Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Critical Care Medicine, 46(9), e825–e873. 10.1097/ccm.0000000000003299 [DOI] [PubMed] [Google Scholar]
- Eghbali‐Babadi, M. , Shokrollahi, N. , & Mehrabi, T. (2017). Effect of family‐patient communication on the incidence of delirium in hospitalized patients in cardiovascular surgery ICU. Iranian Journal of Nursing & Midwifery Research, 22(4), 327–331. 10.4103/1735-9066.212985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrouste‐Orgeas, M. , Vinatier, I. , Tabah, A. , Misset, B. , & Timsit, J. F. (2016a). Reappraisal of visiting policies and procedures of patient's family information in 188 French ICUs: A report of the Outcomerea Research Group. Annals of Intensive Care, 6(1), 82. 10.1186/s13613-016-0185-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrouste‐Orgeas, M. , Vinatier, I. , Tabah, A. , Misset, B. , & Timsit, J. F. (2016b). Reappraisal of visiting policies and procedures of patient's family information in 188 French ICUs: A report of the Outcomerea Research Group. Ann Intensive Care, 6(1), 82. 10.1186/s13613-016-0185-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldfarb, M. J. , Bibas, L. , Bartlett, V. , Jones, H. , & Khan, N. (2017). Outcomes of patient‐ and family‐centered care interventions in the ICU: A systematic review and meta‐analysis. Critical Care Medicine, 45(10), 1751–1761. 10.1097/ccm.0000000000002624 [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. , Altman, D. G. , Gøtzsche, P. C. , Jüni, P. , Moher, D. , Oxman, A. D. , Savovic, J. , Schulz, K. F. , Weeks, L. , Sterne, J. A. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ, 343, d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong, M. A. , Xiaojing, L. I. , Qixia, Z. , & Xiaoyan, Z. (2015). Effect of family participated three stages nursing model in the prevention of delirium for patients in ICU. Nursing Journal of Chinese People's Liberation Army, 32(08), 52–54. [Google Scholar]
- Hönig, K. , & Gündel, H. (2016). Relatives in intensive care units: (Un)Satisfied needs. Nervenarzt, 87(3), 269–275. 10.1007/s00115-016-0069-1 [DOI] [PubMed] [Google Scholar]
- Isaacs, D. (2020). Family‐centred care. Journal of Paediatrics and Child Health, 56(1), 3–4. 10.1111/jpc.14664 [DOI] [PubMed] [Google Scholar]
- Kalabalik, J. , Brunetti, L. , & El‐Srougy, R. (2014). Intensive care unit delirium: A review of the literature. Journal of Pharmacy Practice, 27(2), 195–207. 10.1177/0897190013513804 [DOI] [PubMed] [Google Scholar]
- Kang, J. , Cho, Y. J. , & Choi, S. (2020). State anxiety, uncertainty in illness, and needs of family members of critically ill patients and their experiences with family‐centered multidisciplinary rounds: A mixed model study. PLoS One, 15(6), e0234296. 10.1371/journal.pone.0234296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotfis, K. , Marra, A. , & Ely, E. W. (2018). ICU delirium ‐ a diagnostic and therapeutic challenge in the intensive care unit. Anestezjologia Intensywna Terapia, 50(2), 160–167. 10.5603/AIT.a2018.0011 [DOI] [PubMed] [Google Scholar]
- Krewulak, K. D. , Stelfox, H. T. , Leigh, J. P. , Ely, E. W. , & Fiest, K. M. (2018). Incidence and prevalence of delirium subtypes in an adult ICU: A systematic review and meta‐analysis. Critical Care Medicine, 46(12), 2029–2035. 10.1097/ccm.0000000000003402 [DOI] [PubMed] [Google Scholar]
- Madrid‐Navarro, C. J. , Sanchez‐Galvez, R. , Martinez‐Nicolas, A. , Marina, R. , Garcia, J. A. , Madrid, J. A. , & Rol, M. A. (2015). Disruption of circadian rhythms and delirium, sleep impairment and sepsis in critically ill patients. Potential therapeutic implications for increased light‐dark contrast and melatonin therapy in an ICU environment. Current Pharmaceutical Design, 21(24), 3453–3468. 10.2174/1381612821666150706105602 [DOI] [PubMed] [Google Scholar]
- Maldonado, J. R. (2017). Acute brain failure: Pathophysiology, diagnosis, management, and sequelae of delirium. Critical Care Clinics, 33(3), 461–519. 10.1016/j.ccc.2017.03.013 [DOI] [PubMed] [Google Scholar]
- McKenzie, J. , & Joy, A. (2020). Family intervention improves outcomes for patients with delirium: Systematic review and meta‐analysis. Australasian Journal on Ageing, 39(1), 21–30. 10.1111/ajag.12688 [DOI] [PubMed] [Google Scholar]
- Mitchell, M. L. , Kean, S. , Rattray, J. E. , Hull, A. M. , Davis, C. , Murfield, J. E. , & Aitken, L. M. (2017). A family intervention to reduce delirium in hospitalised ICU patients: A feasibility randomised controlled trial. Intensive & Critical Care Nursing, 40, 77–84. 10.1016/j.iccn.2017.01.001 [DOI] [PubMed] [Google Scholar]
- Nassar Junior, A. P. , Besen, B. , Robinson, C. C. , Falavigna, M. , Teixeira, C. , & Rosa, R. G. (2018). Flexible versus restrictive visiting policies in ICUs: A systematic review and meta‐analysis. Critical Care Medicine, 46(7), 1175–1180. 10.1097/ccm.0000000000003155 [DOI] [PubMed] [Google Scholar]
- O'Connor, S. , Brenner, M. , & Coyne, I. (2019). Family‐centred care of children and young people in the acute hospital setting: A concept analysis. Journal of Clinical Nursing, 28(17–18), 3353–3367. 10.1111/jocn.14913 [DOI] [PubMed] [Google Scholar]
- Pandharipande, P. P. , Ely, E. W. , Arora, R. C. , Balas, M. C. , Boustani, M. A. , La Calle, G. H. , Cunningham, C. , Devlin, J. W. , Elefante, J. , Han, J. H. , MacLullich, A. M. , Maldonado, J. R. , Morandi, A. , Needham, D. M. , Page, V. J. , Rose, L. , Salluh, J. I. F. , Sharshar, T. , Shehabi, Y. , … Smith, H. A. B. (2017). The intensive care delirium research agenda: A multinational, interprofessional perspective. Intensive Care Medicine, 43(9), 1329–1339. 10.1007/s00134-017-4860-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, M. , Giap, T. T. , Lee, M. , Jeong, H. , Jeong, M. , & Go, Y. (2018). Patient‐ and family‐centered care interventions for improving the quality of health care: A review of systematic reviews. International Journal of Nursing Studies, 87, 69–83. 10.1016/j.ijnurstu.2018.07.006 [DOI] [PubMed] [Google Scholar]
- Partridge, J. S. , Martin, F. C. , Harari, D. , & Dhesi, J. K. (2013). The delirium experience: What is the effect on patients, relatives and staff and what can be done to modify this? International Journal of Geriatric Psychiatry, 28(8), 804–812. 10.1002/gps.3900 [DOI] [PubMed] [Google Scholar]
- Piao, J. , Jin, Y. , & Lee, S. M. (2018). Triggers and nursing influences on delirium in intensive care units. Nursing in Critical Care, 23(1), 8–15. 10.1111/nicc.12250 [DOI] [PubMed] [Google Scholar]
- Racine, A. M. , D'Aquila, M. , Schmitt, E. M. , Gallagher, J. , Marcantonio, E. R. , Jones, R. N. , Inouye, S. K. , Schulman‐Green, D. , Brown, C. H. , Cizginer, S. , Clark, D. , Flaherty, J. H. , Gleason, A. , Kolanowski, A. M. , Neufeld, K. J. , O’Connor, M. G. , Pisani, M. A. , Robinson, T. , Verghese, J. , … Schulman‐Green, D. (2019). Delirium burden in patients and family caregivers: Development and testing of new instruments. Gerontologist, 59(5), e393–e402. 10.1093/geront/gny041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosa, R. G. , Falavigna, M. , da Silva, D. B. , Sganzerla, D. , Santos, M. M. S. , Kochhann, R. , de Moura, R. M. , Eugênio, C. S. , Haack, T. D. S. R. , Barbosa, M. G. , Robinson, C. C. , Schneider, D. , de Oliveira, D. M. , Jeffman, R. W. , Cavalcanti, A. B. , Machado, F. R. , Azevedo, L. C. P. , Salluh, J. I. F. , Pellegrini, J. A. S. , … Teixeira, C. (2019). Effect of flexible family visitation on delirium among patients in the intensive care unit: The ICU visits randomized clinical trial. JAMA, 322(3), 216–228. 10.1001/jama.2019.8766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roze des Ordons, A. L. , Stelfox, H. T. , Sinuff, T. , Grindrod‐Millar, K. , Smiechowski, J. , & Sinclair, S. (2020). Spiritual distress in family members of critically ill patients: Perceptions and experiences. Journal of Palliative Medicine, 23(2), 198–210. 10.1089/jpm.2019.0235 [DOI] [PubMed] [Google Scholar]
- Schmitt, E. M. , Gallagher, J. , Albuquerque, A. , Tabloski, P. , Lee, H. J. , Gleason, L. , Weiner, L. S. , Marcantonio, E. R. , Jones, R. N. , Inouye, S. K. , Schulman‐Green, D. (2019). Perspectives on the delirium experience and its burden: Common themes among older patients, their family caregivers, and nurses. Gerontologist, 59(2), 327–337. 10.1093/geront/gnx153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thirsk, L. M. , Vandall‐Walker, V. , Rasiah, J. , & Keyko, K. (2021). A taxonomy of supports and barriers to family‐centered adult critical care: A qualitative descriptive study. Journal of Family Nursing, 27(3), 199–211. 10.1177/1074840721999372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Rompaey, B. , Elseviers, M. M. , Schuurmans, M. J. , Shortridge‐Baggett, L. M. , Truijen, S. , & Bossaert, L. (2009). Risk factors for delirium in intensive care patients: A prospective cohort study. Critical Care, 13(3), R77. 10.1186/cc7892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilevskis, E. E. , Chandrasekhar, R. , Holtze, C. H. , Graves, J. , Speroff, T. , Girard, T. D. , Patel, M. B. , Hughes, C. G. , Cao, A. , Pandharipande, P. P. , Ely, E. W. (2018). The cost of ICU delirium and coma in the intensive care unit patient. Medical Care, 56(10), 890–897. 10.1097/mlr.0000000000000975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, P. , Liamputtong, P. , Koch, S. , & Rawson, H. (2019a). Searching for meaning: A grounded theory of family resilience in adult ICU. Journal of Clinical Nursing, 28(5–6), 781–791. 10.1111/jocn.14673 [DOI] [PubMed] [Google Scholar]
- Wong, P. , Liamputtong, P. , Koch, S. , & Rawson, H. (2019b). Searching for meaning: A grounded theory of family resilience in adult ICU. Journal of Clinical Nursing, 28(5–6), 781–791. 10.1111/jocn.14673 [DOI] [PubMed] [Google Scholar]
- Xiaoqing, G. , Cao, Y. U. , & Zeya, S. (2017). Application of families participatory nursing in the prevention of delirium in ICU patients. Journal of Qilu Nursing, 23(03), 1–3. [Google Scholar]
- Xueping, J. , Ruiyun, L. , Wenjuan, L. , Hua, J. , Yuting, Z. , & Jing, H. (2021). Effect of family‐centered visitation on delirium in ICU patients with cancer. Journal of Nursing Science, 36(06), 1–4. [Google Scholar]
- Yakubu, Y. H. , Esmaeili, M. , & Navab, E. (2019). Family members' beliefs and attitudes towards visiting policy in the intensive care units of Ghana. Nursing Open, 6(2), 526–534. 10.1002/nop2.234 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author on reasonable request.


