Abstract
The emergency medical system, one of the essential elements of public health, has been around for more than 50 years. Although many studies have assessed the factors associated with overcrowding and prolonged length of stay in emergency departments, whether the clinical characteristics and background of a patient are associated with prolonged hospitalization among patients transported by ambulance is unknown. The purpose of this study was to reveal factors associated with the continuation of hospitalization at 21 days after hospital admission among patients transported by ambulance using a population-based patient registry in Osaka, Japan.
This was a retrospective observational study whose study period was the three years from January 2016 to December 2018. In this study, we included patients who were hospitalized after transportation by ambulance in Osaka, Japan. The main outcome was continuation of hospitalization at 21 days after hospital admission. We calculated the adjusted odds ratios (AOR) and 95% confidence interval (CI) with a multivariable logistic regression model to assess factors associated with the outcome.
We included 481,886 patients in this study, of whom 158,551 remained hospitalized at 21 days after hospital admission and 323,335 had been discharged home by 21 days after hospital admission. Factors associated with prolonged hospitalization were elderly (AOR: 1.767 [95% CI: 1.730–1.805]), traffic accident (AOR: 1.231 [95% CI: 1.183–1.282]), no fixed address (AOR: 4.494 [95% CI: 3.632–5.314]), need for nursing care (AOR: 1.420 [95% CI: 1.397–1.443]) and solitary person (AOR: 1.085 [95% CI: 1.050–1.120]).
In this study, the elderly, traffic accidents, no fixed address, need for nursing care, and solitary person were associated with prolonged hospitalization of patients transported by ambulance in Japan.
Keywords: ambulance transport, emergency medical service, epidemiology, prolonged hospitalisation
1. Introduction
The emergency medical system, which is one of the essential elements of public health, has been around for more than 50 years. However, overcrowding in the emergency department (ED) and prolongation of length of stay are public health problems in many countries around the world, and various studies of these problems have been conducted.[1–5] In Japan, the number of patients transported to hospitals by ambulance continues to increase.[6] Thus, it is important to improve overcrowding in the ED and to smoothly discharge inpatients who have been cured to allow acceptance of the next patients transported by ambulance.
Prolongation of length of stay in the ED is associated with overcrowding in the ED, for which several factors have been revealed. In a study of hospital length of stay at a tertiary care center by van der Veen et al, multiple chief complaints, chief complaints such as headache and chest pain, laboratory/radiology testing and consultation were associated with a stay in the ED of 4 hours or more.[7] Asplin et al advocated a conceptual model of partitioned ED crowding divided into 3 interdependent components: input, throughout, and output.[8] In the output component of this model, the most frequently cited reason for ED crowding was the inability to move admitted patients from the ED to an inpatient bed.[9–13] If more patients stay in the hospital for a longer period of time, the number of available inpatient beds will decrease and the ED will become increasingly crowded. However, it has not been revealed whether clinical characteristics and patient background are associated with prolonged hospitalization among patients transported by ambulance.
Osaka Prefecture is the largest metropolitan area in western Japan with a population of about 8.8 million and around 500,000 ambulance dispatches per year. In January 2013, the Osaka Prefectural Government developed an information system called the Osaka Emergency Information Research Intelligent Operation Network (ORION) system using a cell phone application for emergency medical service (EMS) personnel to select a hospital appropriate for the patient. So far, we have found that the introduction of this information system has improved the selection of hospitals by EMS personnel.[14] In addition, not only prehospital data such as ambulance records but also hospital data such as diagnosis and prognosis are registered in the ORION system for all patients transported by ambulance, and these data were merged and collected on a case-by-case basis in this system.[15] The purpose of this study was to reveal factors associated with the continuation of hospitalization at 21 days after hospital admission among patients transported by ambulance using the data in the ORION system.
2. Methods
This study was a retrospective observational study whose study period was the three years from January 2016 to December 2018. We included patients who were hospitalized after transport by ambulance as determined by using the cleaned data that was recorded in the ORION system. Therefore, we excluded patients who returned home from the ED of each hospital, died by 21 days after hospital admission, were transferred to another hospital within 21 days after hospital admission, and had missing data.
In 2015, a total population of 8,839,469 lived in the 1,905-km[2] area of Osaka Prefecture.[16] Of that population, 4,256,049 people (48.2%) were male and 2,278,324 people (25.8%) were elderly, aged 65 years old or more. In 2018, there were 517 medical institutions (105,994 beds) in Osaka Prefecture,[17] of which 288 are emergency medical hospitals including 16 critical care centers that are designated to accept patients with life-threatening emergency diseases such as severe trauma and sepsis.[18] The number of ambulances dispatched by fire departments in Osaka Prefecture was 576,597 in 2017.[19] This study was approved by the ethics committees of Osaka University Graduate School of Medicine (approval no. 15003; Osaka, Japan). Because the ORION data is anonymized without specific personal data, such as patient name and address, the requirement of obtaining patients’ informed consent was waived. This manuscript was written in accordance with the STROBE statement on cohort and cross-sectional studies.[20]
2.1. EMS System and hospitals in Osaka Prefecture and Japan
The EMS system is basically the same as that used in other areas of Japan, as previously described.[21] In Osaka Prefecture, EMS systems such as ambulance dispatch systems are operated by each local government, and ambulances are dispatched by calling 1–1–9. In 2016, the EMS system was operated by 27 fire departments (298 ambulances) and 24 fire control stations. Since the introduction of the ORION system, EMS personnel at the scene select the appropriate hospital for emergency patients rather than a dispatcher.
2.2. The ORION System
Information on the system configuration of ORION was previously described in detail.[14] The EMS personnel at the scene operate the ORION smartphone app for each emergency patient. All of the data input into the cellphone app, such as vital signs and the time of the call to the hospital for acceptance, are also recorded. The cellphone app data are accumulated in the ORION cloud server, and in cooperation with the dispatched EMS personnel, data managers at each fire department directly input or upload the ambulance record of each emergency patient so that it can be connected with the app data. Furthermore, the operators of each hospital also directly input or upload the patient's data, such as diagnoses and outcomes, after hospital acceptance. The results of aggregated data in the ORION system are fed back to every fire department and emergency hospital. The Department of Public Health of Osaka Prefecture can also analyze the effects of health policy on the emergency medical system using these collected data. The ORION system has been in place in all fire departments and emergency hospitals in Osaka Prefecture since January 2016.
2.3. Data collection and quality control
The ORION system checks for errors in the inputted in-hospital data, and the staff of each emergency hospital can correct them, if necessary. Through these tasks, cellphone app data, ambulance records, and the in-hospital data such as diagnosis and prognosis can be comprehensively registered for each patient transported by an ambulance. The registered data is cleaned by the Working Group to analyze the emergency medical care system in Osaka Prefecture.[15] Among the collected and cleaned data, we excluded inconsistent data that did not contain all of the cellphone app data, ambulance records, and in-hospital data such as diagnosis and prognosis. In addition, we also excluded patients whose sex as registered by the fire department did not match that registered by the hospital or whose sex was missing. We also excluded patients whose age input by the fire department and that by the hospital differed by 3 years or more. When this difference was present, we defined the age input by the hospital as the patient's true age.
2.4. Endpoint
The main endpoint was the continuation of hospitalization at 21 days after hospital admission. This endpoint was defined from the outcome data in the ORION dataset.
2.5. Statistical analysis
We calculated the adjusted odds ratio (AOR) and 95% confidence interval (CI) with multivariable logistic regression models to assess the factors associated with the continuation of hospitalization at 21 days after hospital admission. The multivariable logistic regression model was performed by the forced input method. In this study, we selected variables that were expected to be associated with prolonged hospitalization as covariates. Furthermore, the number of covariates inserted into the multivariable logistic regression model was determined to avoid overfitting, and the valiance inflation factor was also used to check for multicollinearity. Potential confounding factors were age group (Infants and young children: 0 to 5 years old, Children: 6 to 17 years old, Adults: 18 to 64 years old, Elderly: 65 to 74 years old, High elderly: 75 to 89 years old, Super elderly: 90 or more years old), sex, seasonality, day of the week, reason for ambulance call, patient characteristics and main diagnosis during hospitalization. We defined seasonality by months in this study. Based on the fire department's definition, reason for the ambulance call was classified into acute disease, traffic accident, industrial accident, sports, other trauma, assault, self-harm, fire accident, inter-hospital transfer and other. Patient characteristics were past history of psychiatric disease, drinking, no fixed address, need for nursing care, drug abuse, trouble at hospitals in past, suicide attempt, living in a nursing faculty, difficulty in hospital acceptance, trauma in children, pregnancy and solitary person based on the data items collected by Osaka Prefecture. The main diagnosis during hospitalization was classified using international classification of diseases-10 codes. We present the data as medians and interquartile range for continuous variables and as percentage for categorical variables. Statistical analyses were performed using SPSS statistical package ver.23.0J (IBM Corp. Armonk, New York). All tests were two-tailed, and p values of <0.05 were considered statistically significant.
3. Results
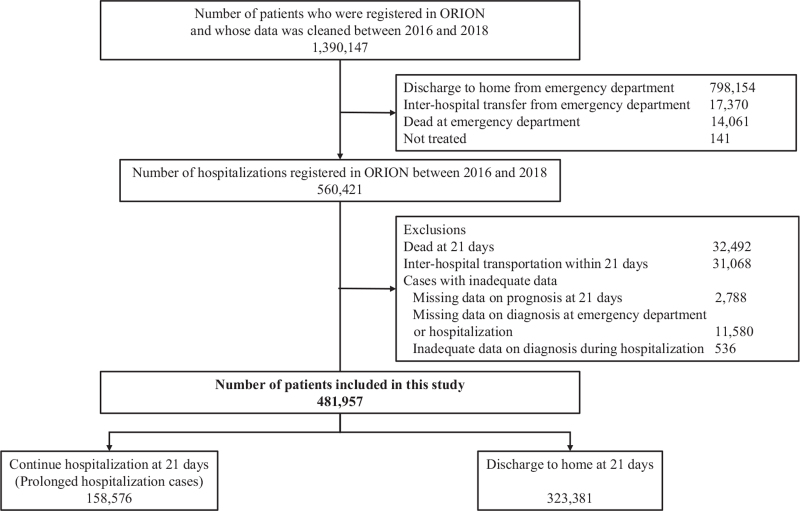
Figure 1 shows the patient flow in this study. The number of patients that were registered in the ORION system whose data were checked was 1,3901,47 during 2016 to 2018. Among these patients, 560,421 were transported and admitted to hospital during 2016–2018, excluding 798,154 patients who returned home from the ED, 17,370 patients who were transferred to another hospital from the ED, 14,061 who died in the ED and 141 patients who did not consult a hospital. Among these 560,421 patients, 32,492 had died by 21 days after hospital admission, 31,068 patients had been transferred to other hospitals by 21 days after hospital admission, 14,904 patients had missing data (outcome at 21 days: 2788 patients, diagnosis during hospitalization: 11,580) and 607 patients had inappropriate data. Finally, we included 481,886 patients in this study. Of them, 158,551 patients had remained hospitalized at 21 days after hospital admission and 323,335 patients had been discharged home by 21 days after hospital admission.
Figure 1.
Patient flow in this study.
Table 1 shows the demographic and clinical characteristics of the patients in this study. The median of age was 75 (interquartile range: 59–83) years old, and 248,899 (51.7%) were men and 232,987 (48.3%) were women. The most common reason for an ambulance call was acute disease, with 337,732 patients (70.1%). The most common patient background factor was need for nursing care, with 102,096 patients (21.2%). The most common medical condition during hospitalization was injury, poisoning and certain other consequences of external causes, with 96,972 patients (20.1%).
Table 1.
Demographic and clinical characteristics of the study patients.
| Total | Infants and young children | Children | Adult | Elderly | High elderly | Super elderly | ||||||||
| (0–5 yr old) | (6–17 yr old) | (18–64 yr old) | (65–74 yr old) | (75–89 yr old) | (over 90 yr old) | |||||||||
| Characteristics | (n=481,886) | (n=13,071) | (n=9025) | (n=117,763) | (n=90,254) | (n=206,707) | (n=45,066) | |||||||
| Age, yr, median (IQR) | 75 | (59–83) | ||||||||||||
| Sex, n(%) | ||||||||||||||
| Male | 248,899 | (51.7) | 7585 | (58.0) | 5564 | (61.7) | 69,812 | (59.3) | 55,139 | (61.1) | 98,058 | (47.4) | 12,741 | (28.3) |
| Female | 232,987 | (48.3) | 5486 | (42.0) | 3461 | (38.3) | 47,951 | (40.7) | 35,115 | (38.9) | 108,649 | (52.6) | 32,325 | (71.7) |
| Seasonality, n(%) | ||||||||||||||
| January | 43,244 | (9.0) | 1171 | (9.0) | 754 | (8.4) | 9406 | (8.0) | 8196 | (9.1) | 19,408 | (9.4) | 4309 | (9.6) |
| February | 37,446 | (7.8) | 1037 | (7.9) | 674 | (7.5) | 8334 | (7.1) | 7092 | (7.9) | 16,592 | (8.0) | 3717 | (8.2) |
| March | 38,031 | (7.9) | 991 | (7.6) | 669 | (7.4) | 9040 | (7.7) | 7231 | (8.0) | 16,387 | (7.9) | 3713 | (8.2) |
| April | 37,796 | (7.8) | 1045 | (8.0) | 702 | (7.8) | 9423 | (8.0) | 7179 | (8.0) | 15,909 | (7.7) | 3538 | (7.9) |
| May | 38,301 | (7.9) | 1063 | (8.1) | 752 | (8.3) | 9787 | (8.3) | 7239 | (8.0) | 16,016 | (7.7) | 3444 | (7.6) |
| June | 37,601 | (7.8) | 1169 | (8.9) | 752 | (8.3) | 9746 | (8.3) | 6899 | (7.6) | 15,658 | (7.6) | 3377 | (7.5) |
| July | 43,895 | (9.1) | 1241 | (9.5) | 906 | (10.0) | 11,235 | (9.5) | 8127 | (9.0) | 18,396 | (8.9) | 3990 | (8.9) |
| August | 41,929 | (8.7) | 1029 | (7.9) | 738 | (8.2) | 10,616 | (9.0) | 7832 | (8.7) | 17,750 | (8.6) | 3964 | (8.8) |
| September | 38,664 | (8.0) | 1006 | (7.7) | 736 | (8.2) | 9892 | (8.4) | 7271 | (8.1) | 16,335 | (7.9) | 3424 | (7.6) |
| October | 40,754 | (8.5) | 1028 | (7.9) | 802 | (8.9) | 10,257 | (8.7) | 7591 | (8.4) | 17,465 | (8.4) | 3611 | (8.0) |
| November | 40,059 | (8.3) | 1055 | (8.1) | 752 | (8.3) | 9637 | (8.2) | 7446 | (8.3) | 17,442 | (8.4) | 3727 | (8.3) |
| December | 44,166 | (9.2) | 1236 | (9.5) | 788 | (8.7) | 10,390 | (8.8) | 8151 | (9.0) | 19,349 | (9.4) | 4252 | (9.4) |
| Day of the week, n(%) | ||||||||||||||
| Sunday | 63,787 | (13.2) | 2037 | (15.6) | 1,398 | (15.5) | 16,224 | (13.8) | 11,728 | (13.0) | 26,526 | (12.8) | 5874 | (13.0) |
| Monday | 75,486 | (15.7) | 1921 | (14.7) | 1,334 | (14.8) | 17,937 | (15.2) | 14,427 | (16.0) | 32,874 | (15.9) | 6993 | (15.5) |
| Tuesday | 70,310 | (14.6) | 1826 | (14.0) | 1,283 | (14.2) | 17,137 | (14.6) | 13,258 | (14.7) | 30,203 | (14.6) | 6603 | (14.7) |
| Wednesday | 67,138 | (13.9) | 1673 | (12.8) | 1,226 | (13.6) | 16,539 | (14.0) | 12,559 | (13.9) | 28,797 | (13.9) | 6344 | (14.1) |
| Thursday | 67,694 | (14.0) | 1780 | (13.6) | 1,246 | (13.8) | 16,423 | (13.9) | 12,803 | (14.2) | 29,010 | (14.0) | 6432 | (14.3) |
| Friday | 70,947 | (14.7) | 1919 | (14.7) | 1,263 | (14.0) | 17,013 | (14.4) | 13,301 | (14.7) | 30,760 | (14.9) | 6691 | (14.8) |
| Saturday | 66,524 | (13.8) | 1915 | (14.7) | 1,275 | (14.1) | 16,490 | (14.0) | 12,178 | (13.5) | 28,537 | (13.8) | 6129 | (13.6) |
| Reason for ambulance call | ||||||||||||||
| Acute disease | 337,732 | (70.1) | 9050 | (69.2) | 4,643 | (51.4) | 76,956 | (65.3) | 65,131 | (72.2) | 149,131 | (72.1) | 32,821 | (72.8) |
| Traffic accident | 16,636 | (3.5) | 124 | (0.9) | 1,106 | (12.3) | 8537 | (7.2) | 3216 | (3.6) | 3494 | (1.7) | 159 | (0.4) |
| Industrial accident | 3,669 | (0.8) | 0 | (0) | 10 | (0.1) | 2890 | (2.5) | 624 | (0.7) | 144 | (0.1) | 1 | (0.0) |
| Sports | 1,106 | (0.2) | 0 | (0) | 582 | (6.4) | 436 | (0.4) | 62 | (0.1) | 26 | (0.0) | 0 | (0) |
| Other trauma | 58,565 | (12.2) | 843 | (6.5) | 1,010 | (11.2) | 7954 | (6.8) | 9536 | (10.6) | 31,090 | (15.0) | 8132 | (18.0) |
| Assault | 765 | (0.2) | 9 | (0.1) | 31 | (0.3) | 521 | (0.4) | 92 | (0.1) | 105 | (0.1) | 7 | (0.0) |
| Self-harm | 2,947 | (0.6) | 0 | (0) | 97 | (1.1) | 2461 | (2.1) | 209 | (0.2) | 169 | (0.1) | 11 | (0.0) |
| Fire accident | 427 | (0.1) | 5 | (0.0) | 16 | (0.2) | 232 | (0.2) | 78 | (0.1) | 86 | (0.0) | 10 | (0.0) |
| Inter-hospital transfer | 59,571 | (12.4) | 3003 | (23.0) | 1,521 | (16.9) | 17,534 | (14.9) | 11,245 | (12.5) | 22,361 | (10.8) | 3907 | (8.7) |
| Other | 468 | (0.1) | 37 | (0.3) | 9 | (0.1) | 242 | (0.2) | 61 | (0.1) | 101 | (0.0) | 18 | (0.0) |
| Patient background | ||||||||||||||
| Past history of psychiatric disease | 19,634 | (4.1) | 13 | (0.1) | 171 | (1.9) | 8702 | (7.4) | 2972 | (3.3) | 6490 | (3.1) | 1289 | (2.9) |
| Drinking | 10,765 | (2.2) | 13 | (0) | 54 | (0.6) | 7629 | (6.5) | 1815 | (2.0) | 1220 | (0.6) | 47 | (0.1) |
| No fixed address | 482 | (0.1) | 13 | (0) | 0 | (0) | 231 | (0.2) | 164 | (0.2) | 81 | (0.0) | 6 | (0.0) |
| Need for nursing care | 102,096 | (21.2) | 13 | (0) | 6 | (0.1) | 1134 | (1.0) | 11,723 | (13.0) | 64,769 | (31.3) | 24,479 | (54.3) |
| Drug abuse | 2,150 | (0.4) | 13 | (0.1) | 58 | (0.6) | 1677 | (1.4) | 144 | (0.2) | 224 | (0.1) | 34 | (0.1) |
| Trouble at hospitals in past | 187 | (0.0) | 13 | (0) | 1 | (0.0) | 102 | (0.1) | 40 | (0.0) | 38 | (0.0) | 6 | (0.0) |
| Suicide attempt | 1,273 | (0.3) | 13 | (0) | 50 | (0.6) | 1008 | (0.9) | 107 | (0.1) | 95 | (0.0) | 13 | (0.0) |
| Living in nursing faculty | 18,772 | (3.9) | 13 | (0.0) | 9 | (0.1) | 666 | (0.6) | 1752 | (1.9) | 11,003 | (5.3) | 5342 | (11.9) |
| Difficulty in hospital acceptance | 101 | (0.0) | 13 | (0.0) | 1 | (0.0) | 67 | (0.1) | 13 | (0.0) | 12 | (0.0) | 7 | (0.0) |
| Trauma in children | 1,759 | (0.4) | 13 | (3.5) | 1,299 | (14.4) | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
| Pregnancy | 2,918 | (0.6) | 13 | (0) | 25 | (0.3) | 2893 | (2.5) | 12 | (0.0) | 27 | (0.0) | 4 | (0.0) |
| Solitary person | 18,471 | (3.8) | 13 | (0) | 8 | (0.1) | 3570 | (3.0) | 4212 | (4.7) | 9210 | (4.4) | 1561 | (3.5) |
| Type of disease and injury causing hospitalization | ||||||||||||||
| Certain infectious and parasitic diseases (A+B) | 17,398 | (3.6) | 1278 | (9.8) | 753 | (8.3) | 5482 | (4.7) | 2259 | (2.9) | 6123 | (3.0) | 1163 | (2.6) |
| Neoplasms (C) | 15,059 | (3.1) | 18 | (0.1) | 23 | (0.3) | 2720 | (2.3) | 4593 | (5.1) | 6920 | (3.3) | 785 | (1.7) |
| Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (D) | 5,446 | (1.1) | 57 | (0.4) | 85 | (0.9) | 1553 | (1.3) | 1071 | (1.2) | 2275 | (1.1) | 405 | (0.9) |
| Endocrine, nutritional and metabolic diseases (E) | 18,856 | (3.9) | 228 | (1.7) | 155 | (1.7) | 3907 | (3.3) | 3703 | (4.1) | 8983 | (4.3) | 1880 | (4.2) |
| Mental and behavioral disorders (F) | 8,316 | (1.7) | 48 | (0.4) | 210 | (2.3) | 6342 | (5.4) | 737 | (0.8) | 876 | (0.4) | 103 | (0.2) |
| Diseases of the nervous system (G) | 19,396 | (4.0) | 716 | (5.5) | 960 | (10.6) | 6516 | (5.5) | 3809 | (4.2) | 6509 | (3.1) | 886 | (2.0) |
| Diseases of the circulatory system (I) | 93,371 | (19.4) | 69 | (0.5) | 182 | (2.0) | 18,838 | (16.0) | 22,336 | (24.7) | 43,131 | (20.9) | 8815 | (19.6) |
| Diseases of the respiratory system (J) | 69,966 | (14.5) | 3797 | (29.0) | 1,171 | (13.0) | 7247 | (6.2) | 10,375 | (11.5) | 36,247 | (17.5) | 11,129 | (24.7) |
| Diseases of the digestive system (K) | 56,509 | (11.7) | 254 | (1.9) | 582 | (6.4) | 16,989 | (14.4) | 11,607 | (12.9) | 22,747 | (11.0) | 4330 | (9.6) |
| Diseases of the musculoskeletal system and connective tissue (M) | 14,848 | (3.1) | 119 | (0.9) | 101 | (1.1) | 3977 | (3.4) | 2653 | (2.9) | 6,798 | (3.3) | 1200 | (2.7) |
| Diseases of the genitourinary system (N) | 22,954 | (4.8) | 131 | (1.0) | 170 | (1.9) | 4438 | (3.8) | 3794 | (4.2) | 11,510 | (5.6) | 2911 | (6.5) |
| Pregnancy, childbirth and the puerperium (O) | 4,999 | (1.0) | 8 | (0.1) | 39 | (0.4) | 4944 | (4.2) | 3 | (0.0) | 5 | (0.0) | 0 | (0) |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R) | 22,191 | (4.6) | 3759 | (28.8) | 811 | (9.0) | 4431 | (3.8) | 3563 | (3.9) | 8038 | (3.9) | 1589 | (3.5) |
| Injury, poisoning and certain other consequences of external causes (S+T) | 96,972 | (20.1) | 2065 | (15.8) | 3,645 | (40.4) | 25,923 | (22.0) | 15,711 | (17.4) | 40,501 | (19.6) | 9127 | (20.3) |
| Other | 15,605 | (3.2) | 524 | (4.0) | 138 | (1.5) | 4456 | (3.8) | 3700 | (4.1) | 6044 | (2.9) | 743 | (1.6) |
Table 2 shows the results of the main analysis. Factors associated with the continuation of hospitalization at 21 days after hospital admission were elderly (AOR: 1.767 [95% CI: 1.730–1.805]), high elderly (AOR: 2.233 [95% CI: 2.191–2.276]), super elderly (AOR: 2.401 [95% CI: 2.337–2.466]) and female (AOR: 1.027 [95% CI: 1.013–1.040]). Among the reasons for an ambulance call, traffic accident (AOR: 1.231 [95% CI: 1.183–1.282]), other trauma (AOR: 1.672 [95% CI: 1.630–1.716]) and inter-hospital transfer (AOR: 1.158 [95% CI: 1.134–1.181]) were associated with the continuation of hospitalization at 21 days after hospital admission. Among the patient background factors, past history of psychiatric disease (AOR: 1.078 [95% CI: 1.041–1.116]), no fixed address (AOR: 4.494 [95% CI: 3.632–5.314]), need for nursing care (AOR: 1.420 [95% CI: 1.397–1.443]), suicide attempt (AOR: 1.495 [95% CI: 1.238–1.806]), living in a nursing faculty (AOR: 1.115 [95% CI: 1.080–1.150]) and solitary person (AOR: 1.085 [95% CI: 1.050–1.120]) were associated with the continuation of hospitalization at 21 days after hospital admission. Compared to cardiovascular disease, only neoplasm (AOR: 1.301 [95% CI: 1.256–1.348]) was associated with the continuation of hospitalization at 21 days after hospital admission, whereas all other medical conditions were inversely associated with this outcome.
Table 2.
Factors associated with prolonged hospitalization after emergency transport in Osaka.
| Prolonged hospitalization | Adjusted OR (95% CI) | P value | VIF | ||||
| % (n/N) | |||||||
| Age group (yr) | 1.248 | ||||||
| Infants and young children (0–5 yr old) | 3.3 | (429/13071) | 0.147 | (0.133–0.162) | <.001 | ||
| Children (6–17 yr old) | 5.6 | (504/9025) | 0.214 | (0.194–0.237) | <.001 | ||
| Adults (18–64 yr old) | 19.2 | (22607/117763) | Reference | ||||
| Elderly (65–74 yr old) | 33.3 | (30096/90254) | 1.767 | (1.730–1.805) | <.001 | ||
| High elderly (75–89 yr old) | 40.9 | (84483/206707) | 2.233 | (2.191–2.276) | <.001 | ||
| Super elderly (over 90 yr old) | 45.3 | (20432/45066) | 2.401 | (2.337–2.466) | <.001 | ||
| Sex | 1.051 | ||||||
| Male | 30.8 | (76713/248899) | Reference | ||||
| Female | 35.1 | (81838/232987) | 1.027 | (1.013–1.040) | <.001 | ||
| Seasonality | 1.002 | ||||||
| January | 35.6 | (15416/43244) | 1.069 | (1.036–1.102) | <.001 | ||
| February | 35.1 | (13152/37446) | 1.055 | (1.022–1.089) | .001 | ||
| March | 35.0 | (13321/38031) | 1.066 | (1.032–1.100) | <.001 | ||
| April | 33.1 | (12515/37796) | Reference | ||||
| May | 31.5 | (12061/38301) | 0.933 | (0.903–0.963) | <.001 | ||
| June | 31.1 | (11703/37601) | 0.930 | (0.900–0.960) | <.001 | ||
| July | 30.3 | (13294/43895) | 0.899 | (0.871–0.927) | <.001 | ||
| August | 31.0 | (13009/41929) | 0.920 | (0.892–0.950) | <.001 | ||
| September | 32.5 | (12554/38664) | 0.987 | (0.956–1.020) | .441 | ||
| October | 32.4 | (13200/40754) | 0.965 | (0.935–0.996) | .029 | ||
| November | 32.9 | (13170/40059) | 0.965 | (0.935–0.996) | .028 | ||
| December | 34.3 | (15156/44166) | 1.032 | (1.001–1.064) | .045 | ||
| Day of the week | 1.001 | ||||||
| Sunday | 29.8 | (19026/63787) | 0.844 | (0.824–0.865) | <.001 | ||
| Monday | 34.3 | (25924/75486) | Reference | ||||
| Tuesday | 33.8 | (23768/70310) | 0.983 | (0.961–1.006) | .139 | ||
| Wednesday | 33.4 | (22431/67138) | 0.973 | (0.951–0.996) | .024 | ||
| Thursday | 33.3 | (22553/67694) | 0.966 | (0.944–0.989) | .003 | ||
| Friday | 33.6 | (23855/70947) | 0.970 | (0.948–0.992) | .009 | ||
| Saturday | 31.6 | (20994/66524) | 0.898 | (0.877–0.920) | <.001 | ||
| Reason for ambulance call | 1.046 | ||||||
| Acute disease | 30.2 | (102070/337732) | Reference | ||||
| Traffic accident | 33.9 | (5637/16636) | 1.231 | (1.183–1.282) | <.001 | ||
| Industrial accident | 28.8 | (1057/3669) | 1.057 | (0.979–1.141) | .157 | ||
| Sports | 11.6 | (128/1106) | 0.666 | (0.549–0.809) | <.001 | ||
| Other trauma | 51.4 | (30092/58565) | 1.672 | (1.630–1.716) | <.001 | ||
| Assault | 15.4 | (118/765) | 0.524 | (0.428–0.643) | <.001 | ||
| Self-harm | 10.9 | (321/2947) | 0.459 | (0.399–0.528) | <.001 | ||
| Fire accident | 22.5 | (96/427) | 0.632 | (0.500–0.797) | <.001 | ||
| Inter-hospital transfer | 31.7 | (18892/59571) | 1.158 | (1.134–1.181) | .001 | ||
| Other | 29.9 | (140/468) | 1.318 | (1.061–1.637) | .012 | ||
| Patient background | |||||||
| Past history of psychiatric disease | (+) | 28.1 | (5510/19634) | 1.078 | (1.041–1.116) | <.001 | 1.060 |
| (−) | 33.1 | (153041/462252) | Reference | ||||
| Drinking | (+) | 11.4 | (1222/10765) | 0.381 | (0.357–0.407) | <.001 | 1.035 |
| (−) | 33.4 | (157329/471121) | Reference | ||||
| No fixed address | (+) | 55.2 | (266/482) | 4.394 | (3.632–5.314 | <.001 | 1.002 |
| (−) | 32.9 | (158285/481404) | Reference | ||||
| Need for nursing care | (+) | 45.9 | (46843/102096) | 1.420 | (1.397–1.443) | .001 | 1.192 |
| (−) | 29.4 | (111708/379790) | Reference | ||||
| Drug abuse | (+) | 6.7 | (144/2150) | 0.228 | (0.190–0.274) | <.001 | 1.197 |
| (−) | 33.0 | (158407/479736) | Reference | ||||
| Trouble at hospital in past | (+) | 22.5 | (42/187) | 0.823 | (0.570–1.189) | .300 | 1.003 |
| (−) | 32.9 | (158509/481699) | Reference | ||||
| Suicide attempt | (+) | 15.6 | (198/1273) | 1.495 | (1.238–1.806) | <.001 | 1.184 |
| (−) | 32.9 | (158353/480613) | Reference | ||||
| Living in nursing faculty | (+) | 43.3 | (8124/18772) | 1.115 | (1.080–1.150) | <.001 | 1.041 |
| (−) | 32.5 | (150427/463114) | Reference | ||||
| Difficulty in hospital acceptance | (+) | 20.8 | (21/101) | 0.808 | (0.479–1.365) | .426 | 1.002 |
| (−) | 32.9 | (158530/481785) | Reference | ||||
| Trauma in children | (+) | 8.2 | (144/1759) | 1.081 | (0.893–1.307) | .425 | 1.008 |
| (−) | 33.0 | (158407/480127) | Reference | ||||
| Pregnancy | (+) | 11.2 | (311/2918) | 0.694 | (0.599–0.804) | <.001 | 1.041 |
| (−) | 33.0 | (158240/478968) | Reference | ||||
| Solitary person | (+) | 36.5 | (6738/18471) | 1.085 | (1.050–1.120) | <.001 | 1.005 |
| (−) | 32.8 | (151813/463415) | Reference | ||||
| Main disease condition causing hospitalization | 1.044 | ||||||
| Certain infectious and parasitic diseases (A+B) | 22.4 | (3898/17398) | 0.511 | (0.491–0.531) | <.001 | ||
| Neoplasms (C) | 47.3 | (7123/15059) | 1.307 | (1.262–1.354) | <.001 | ||
| Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (D) | 34.6 | (1884/5446) | 0.807 | (0.760–0.856) | <.001 | ||
| Endocrine, nutritional and metabolic diseases (E) | 29.3 | (5527/18856) | 0.584 | (0.564–0.605) | <.001 | ||
| Mental and behavioral disorders (F) | 9.7 | (805/8316) | 0.383 | (0.353–0.415) | <.001 | ||
| Diseases of the nervous system (G) | 19.1 | (3705/19396) | 0.404 | (0.388–0.420) | <.001 | ||
| Diseases of the circulatory system (I) | 41.4 | (38624/93371) | Reference | ||||
| Diseases of the respiratory system (J) | 35.3 | (24697/69966) | 0.715 | (0.700–0.731) | <.001 | ||
| Diseases of the digestive system (K) | 19.9 | (11255/56509) | 0.376 | (0.367–0.385) | <.001 | ||
| Diseases of the musculoskeletal system and connective tissue (M) | 35.7 | (5296/14848) | 0.762 | (0.734–0.791) | <.001 | ||
| Diseases of the genitourinary system (N) | 27.9 | (6413/22954) | 0.512 | (0.496–0.529) | <.001 | ||
| Pregnancy, childbirth and the puerperium (O) | 12.1 | (607/4999) | 0.416 | (0.374–0.464) | <.001 | ||
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R) | 18.2 | (4041/22191) | 0.406 | (0.391–0.422) | <.001 | ||
| Injury, poisoning and certain other consequences of external causes (S+T) | 43.4 | (42103/96972) | 0.994 | (0.969–1.020) | .662 | ||
| Other | 16.5 | (2573/15605) | 0.305 | (0.292–0.319) | <.001 | ||
4. Discussion
In this study, we revealed the factors associated with the continuation of hospitalization after emergency transport using a population-based registry of emergency patients transported by ambulance. Several factors have previously been elucidated regarding ambulance diversion, overcrowding in the ED and the difficulty of hospital acceptance of patients transported by ambulance.[7,21–25] In our previous study, we found that the elderly, foreigners, loss of consciousness, weekends and public holidays, and nighttime were factors associated with the difficulty of hospital selection by EMS personnel at the scene.[21] Thus, factors associated with ambulance diversion, overcrowding in the ED and the difficulty of hospital selection by EMS personnel at the scene do not necessarily coincide with the factors related to prolonged hospitalization of patients transported by ambulance. Therefore, for smooth acceptance of emergency patients transported by ambulance, it is important to take measures not only against ambulance diversion and ED overcrowding but also against factors associated with the prolonged hospitalization of emergency patients transported by ambulance. This study revealed the factors associated with prolonged hospitalization after hospital admission, which can be useful in continuing to build and improve the EMS system.
First, the elderly was associated with prolonged hospitalization in this study. In a single-center retrospective study that compared patients hospitalized for more than 2 weeks with those hospitalized for less than 2 weeks, the elderly and higher Charlson comorbidity index were associated with hospitalization for more than 2 weeks.[26] Pontiroli et al also reported that low albumin levels, low lymphocyte level, the elderly, increased platelets, male sex, and emergency hospitalization were associated with prolonged hospitalization.[27] Because the elderly can be poorly nourished and have comorbidities, these factors may additionally complicate their condition and prolong hospitalization, especially as emergency patients transported by ambulance. In addition, the need for nursing care and living in a nursing facility were patient background factors associated with prolonged hospitalization in this study. Japan is one of the most aged nations in the world, with 5.97 million people receiving nursing care annually.[28] Because medical care is basically not provided with nursing care in Japan, once a person is hospitalized, the patient cannot be transferred to a home where nursing care is provided or to a nursing facility unless the patient's condition has improved to the point that medical care is no longer needed. Therefore, the patients receiving nursing care may have had prolonged hospitalization. However, in a retrospective study at a single tertiary health care center in Mexico, young people, male sex, a lower physician-to-patients rate, weekend hospitalization, presence of surgery, number of complications, residence outside the city and lower socioeconomic status were associated with prolonged hospitalization.[29] According to a World Health Organization report, there were 4.9 million deaths by injury in 2016, of which 1.4 million patients died in road accidents worldwide, three quarters of whom were men or boys.[30] As this study was conducted in a developed country, the differences in health and medical situations in developed and developing countries may affect the results.
Second, while trauma such as traffic accidents and other injury was associated with prolonged hospitalization as the reason for the ambulance call, self-harm was inversely associated with prolonged hospitalization. This may be due to the fact that patients injured by traffic accidents and other injuries had fractures and required prolonged hospitalization due to the need for surgical treatment and rehabilitation. In contrast, although some of the self-harm patients were those who were injured by a fall from heights, the fact that many of the patients required only suturing, such as of wrist cuts, may indicate an opposite relationship with prolonged hospitalization. This result would be consistent with the result that the patient background factor of suicide attempt was associated with prolonged hospitalization.
Third, among the patient background factors, no fixed address and solitary person were also associated with prolonged hospitalization. The universal insurance system in Japan allows Japanese people to receive medical treatment at relatively low cost. However, patients with no fixed address may have unpaid insurance premiums or may not be enrolled in a universal insurance system. It is thus necessary to check the income of these patients, and they need to apply for welfare similar to Medicare in the United States. Therefore, patients with no fixed address may have to be hospitalized for a longer period to check their financial status and perform the necessary application procedure. A previous study also reported that low socioeconomic status was associated with prolonged hospitalization.[29] Because of the limitations of inpatient bed availability, a system to temporarily evacuate patients who have completed treatment would be necessary to accept new emergency patients transported by ambulance. Solitary persons were also associated with prolonged hospitalization. For such people, it is necessary to coordinate with family members and welfare professionals regarding arrangements for an appropriate living environment and follow-up after discharge from hospital. As it is possible to receive medical treatment at a relatively low cost with universal health insurance in Japan, the patient may continue to be hospitalized until the environment is ready after discharge even if the in-hospital treatment is completed. Thus, although the universal health insurance system is an essential system for people, it may be having a negative impact on the emergency medical system, so further welfare measures may be needed to solve this problem.
4.1. Limitations
There are some limitations in this study. First, the ORION system obtains data on emergency medical hospitals and critical care centers in Osaka Prefecture but cannot obtain data on clinics and non-emergency medical hospitals or on patients transported to and from outside Osaka Prefecture because the ORION system is operated only within Osaka Prefecture. We hope that a similar information system can be developed and introduced to enable data linkage in many areas of Japan in the future. In addition, it is unclear whether the patients transferred to other medical hospitals underwent prolonged hospitalization because such data were not collected. Also, no data was collected on detailed medical history, such as medications, pregnancy, and growth and development history. There is a limit to the amount of data that can be input individually by EMS personnel and the staff of medical institutions, and it is necessary to link this data with the personal health record. Finally, as this study was a retrospective observational study, it may have some unknown confounding factors.
5. Conclusion
In this study, the elderly, traffic accidents, other trauma, no fixed address, living in a nursing faculty, need for nursing care, solitary person and neoplasms were associated with prolong hospitalization of patients transported by ambulance. Measures to handle ambulance diversion and overcrowding in the ED, as well as prolonged hospitalization, are important for the smooth hospital acceptance of emergency patients transported by ambulance.
Acknowledgments
The Osaka prefecture government is deeply indebted to all of the Emergency Medical System personnel and concerned physicians in Osaka Prefecture and to the Osaka Medical Association for their indispensable cooperation and support.
Author contributions
Conceptualization: Yusuke Katayama.
Data curation: Yusuke Katayama, Jun Tanaka, Shota Nakao, Masahiko Nitta.
Formal analysis: Yusuke Katayama, Tetsuhisa Kitamura.
Funding acquisition: Takeshi Shimazu.
Project administration: Yusuke Katayama, Tetsuya Matsuoka.
Software: Yusuke Katayama, Tetsuhisa Kitamura.
Supervision: Satoshi Fujimi, Yasuyuki Kuwagata.
Validation: Tetsuhisa Kitamura.
Writing – original draft: Yusuke Katayama, Tetsuhisa Kitamura.
Writing – review & editing: Jun Tanaka, Shota Nakao, Masahiko Nitta, Satoshi Fujimi, Yasuyuki Kuwagata, Takeshi Shimazu, Tetsuya Matsuoka.
Footnotes
Abbreviations: AOR = adjusted odds ratio, CI = confidence interval, ED = emergency department, EMS = emergency medical service, ORION = Osaka Emergency Information Research Intelligent Operation Network system.
How to cite this article: Katayama Y, Kitamura T, Tanaka J, Nakao S, Nitta M, Fujimi S, Kuwagata Y, Shimazu T, Matsuoka T. Factors associated with prolonged hospitalization among patients transported by emergency medical services: a population-based study in Osaka, Japan. Medicine. 2021;100:48(e27862).
This manuscript was supported by the Clinical Investigator's Research Project in the Osaka University Graduate School of Medicine. This manuscript was supported by the Japan Society for the Promotion of Science KAKENHI (grant no. JP18H02902).
The authors have no conflicts of interest to disclose.
The data that support the findings of this study are available from a third party, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are available from the authors upon reasonable request and with permission of the third party.
IQR = interquartile range.
CI = confidence interval, OR = odds ratio, VIF= valiance inflation factor.
References
- [1].Herring A, Wilper A, Himmelstein DU, et al. Increasing length of stay among adult visits to U.S. Emergency departments, 2001-2005. Acad Emerg Med 2009;16:609–16. [DOI] [PubMed] [Google Scholar]
- [2].Fernandes CM, Price A, Christenson JM. Does reduced length of stay decrease the number of emergency department patients who leave without seeing a physician? J Emerg Med 1997;15:397–9. [DOI] [PubMed] [Google Scholar]
- [3].Carr BG, Kaye AJ, Wiebe DJ, Gracias VH, Schwab CW, Reilly PM. Emergency department length of stay: a major risk factor for pneumonia in intubated blunt trauma patients. J Trauma 2007;63:09–12. [DOI] [PubMed] [Google Scholar]
- [4].Mowery NT, Dougherty SD, Hildreth AN, et al. Emergency department of length of stay is an independent predictor of hospital mortality in trauma activation patients. J Trauma 2011;70:1317–25. [DOI] [PubMed] [Google Scholar]
- [5].Chong CP, Haywood C, Barker A, Lim WK. Is emergency department length of stay associated with inpatient mortality? Australas J Ageing 2013;32:122–4. [DOI] [PubMed] [Google Scholar]
- [6].Ambulance Service Planning Office of Fire and Disaster Management Agency of Japan: effect of first aid for emergency patients in 2018. Available at: https://www.fdma.go.jp/publication/rescue/items/kkkg_h30_01_kyukyu.pdf. Accessed February 24, 2020. In Japanese. [Google Scholar]
- [7].van der Veen D, Remejier C, Fogreloo AJ, Heringhaus C, de Groot B. Independent determinants of prolonged emergency department length of stay in a tertiary care centre: a prospective cohort study. Scand J Trauma Resusc Emerg Med 2018;26:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA, Jr. A conceptual model of emergency department crowding. Ann Emerg Med 2003;42:173–80. [DOI] [PubMed] [Google Scholar]
- [9].Derlet R, Richards J, Kravitz R. Frequent overcrowding in US emergency departments. Acad Emerg Med 2001;8:151–5. [DOI] [PubMed] [Google Scholar]
- [10].Andrulis DP, Kellermann A, Hintz EA, Hackman BB, Weslowski VB. Emergency departments and crowding in United States teaching hospitals. Ann Emerg Med 1991;20:980–6. [DOI] [PubMed] [Google Scholar]
- [11].Gallagher EJ, Lynn SG. The etiology of medical gridlock: causes of emergency department overcrowding in New York City. J Emerg Med 1990;8:785–90. [DOI] [PubMed] [Google Scholar]
- [12].Espinosa G, Miró O, Sánchez M, Coll-Vinent B, Millá J. Effects of external and internal factors on emergency department overcrowding. Ann Emerg Med 2002;39:693–5. [DOI] [PubMed] [Google Scholar]
- [13].Forster AJ, Stiell I, Wells G, Lee AJ, van Walraven C. The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med 2003;10:127–33. [DOI] [PubMed] [Google Scholar]
- [14].Katayama Y, Kitamura T, Kiyohara K, et al. Improvements in patient acceptance by hospitals following the introduction of a smartphone app for the emergency medical service system: a population-based before-and-after observational study in Osaka City, Japan. JMIR Mhealth Uhealth 2017;59:e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Okamoto J, Katayama Y, Kitamura T, et al. Profile of ORION (Osaka emergency information Research Intelligent Operation Network system) between 2015 and 2016 in Osaka, Japan: a population-based registry of emergency patients with both ambulance and in-hospital records. Acute Med Surg 2019;6:12–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Statistics Bureau, Ministry of Internal Affairs and Communications of Japan. National Census in 2015. Available at: http://www.stat.go.jp/data/kokusei/2015/kekka/kihon1/pdf/youyaku.pdf . Accessed February 24, 2020. In Japanese. [Google Scholar]
- [17].Ministry of Health, Labour, and Welfare of Japan. Medical facility survey in 2018. Available at: https://www.mhlw.go.jp/toukei/saikin/hw/iryosd/18/dl/04toukei30.pdf. Accessed February 24, 2020. In Japanese. [Google Scholar]
- [18].Emergency Medical Council in Osaka Prefecture. Certification of emergency medical institutions in 2019. Available at: http://www.pref.osaka.lg.jp/attach/3071/00159407/006_s2-2.pdf. Accessed February 24, 2020. In Japanese. [Google Scholar]
- [19].Osaka Prefectural Government. The statistics of ambulance dispatch and emergency patients transported by ambulance in 2017. Available at: http://www.pref.osaka.lg.jp/shobobosai/kyukyu/kyukyu_01.html. Accessed February 24, 2020. In Japanese. [Google Scholar]
- [20].Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative et al. STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344–9. [DOI] [PubMed] [Google Scholar]
- [21].Katayama Y, Kitamura T, Kiyohara K, et al. Factors associated with the difficulty in hospital acceptance at the scene by emergency medical service personnel: a population-based study in Osaka City, Japan. BMJ Open 2016;6:e013849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Olshaker JS, Rathlev NK. Emergency department overcrowding and ambulance diversion: the impact and potential solutions of extended boarding of admitted patients in the Emergency Department. J Emerg Med 2006;30:351–6. [DOI] [PubMed] [Google Scholar]
- [23].Chaou CH, Chiu TF, Yen AM, Ng CJ, Chen HH. Analyzing factors affecting emergency department length of stay-using a competing risk-accelerating failure time model. Medicine 2016;95:e3263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Rose L, Scales DC, Atzema C, et al. Emergency department length of stay for critical care admissions. a population-based study. Ann Am Thorac Soc 2016;13:1324–32. [DOI] [PubMed] [Google Scholar]
- [25].Hofer KD, Saurenmann RK. Parameter affecting length of stay in a pediatric emergency department: a retrospective observational study. Eur J Pediatr 2017;176:591–8. [DOI] [PubMed] [Google Scholar]
- [26].O'Sullivan K, Martensson J, Robbins R, Farley KJ, Johnson D, Jones D. Epidemiology of long stay patients in a university teaching hospital. Intern Med J 2017;47:513–21. [DOI] [PubMed] [Google Scholar]
- [27].Pontiroli AE, Loreggian L, Rovati MPL, et al. Length of hospitalization is associated with selected biomarkers (albumin and lymphocytes) and with co-morbidities: study on 4000 patients. Biomark Res 2017;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ministry of Health, Labour and Welfare. The statistics on nursing care benefits in 2018. Available at: https://www.mhlw.go.jp/toukei/saikin/hw/kaigo/kyufu/18/dl/02.pdf. Accessed February 24, 2020. In Japanese. [Google Scholar]
- [29].Marfil-Ganza BA, Belaunzarán-Zamudio PF, Guilas-Herrero A, et al. Risk factors associated with prolonged hospital length-of-stay: 18-year retrospective study of hospitalizations in a tertiary healthcare center in Mexico. PloS One 2018;13:e0207203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].World Health Organization. Global status report on road safety 2018. Available at: https://apps.who.int/iris/bitstream/handle/10665/277370/WHO-NMH-NVI-18.20-eng.pdf?ua=1. Accessed February 24, 2020. [Google Scholar]