Abstract
Background
Satisfaction with treatment results is an important outcome domain in striving for patient-centered and value-based healthcare. Although numerous studies have investigated factors associated with satisfaction with treatment results, most studies used relatively small samples. Additionally, many studies have only investigated univariable associations instead of multivariable associations; to our knowledge, none have investigated the independent association of baseline sociodemographics, quality of life, improvement in pain and function, experiences with healthcare delivery, and baseline measures of mental health with satisfaction with treatment results.
Questions/purposes
(1) What factors are independently associated with satisfaction with treatment results at 3 months post-treatment in patients treated for common hand and wrist conditions? (2) What factors are independently associated with the willingness to undergo the treatment again at 3 months post-treatment in patients treated for common hand and wrist conditions? Among the factors under study were baseline sociodemographics, quality of life, improvement in pain and function, experiences with healthcare delivery, and baseline measures of mental health.
Methods
Between August 2018 and May 2020, we included patients who underwent carpal tunnel release, nonsurgical or surgical treatment for thumb-base osteoarthritis, trigger finger release, limited fasciectomy for Dupuytren contracture, or nonsurgical treatment for midcarpal laxity in one of the 28 centers of Xpert Clinics in the Netherlands. We screened 5859 patients with complete sociodemographics and data at baseline. Thirty-eight percent (2248 of 5859) of these patients had complete data at 3 months. Finally, participants were eligible for inclusion if they provided a relevant answer to the three patient-reported experience measure (PREM) items. A total of 424 patients did not do this because they answered “I don’t know” or “not applicable” to a PREM item, leaving 31% (1824 of 5859) for inclusion in the final sample. A validated Satisfaction with Treatment Result Questionnaire was administered at 3 months, which identified the patients’ level of satisfaction with treatment results so far on a 5-point Likert scale (research question 1, with answers of poor, moderate, fair, good, or excellent) and the patients’ willingness to undergo the treatment again under similar circumstances (research question 2, with answers of yes or no). A hierarchical logistic regression model was used to identify whether baseline sociodemographics, quality of life, change in outcome (patient-reported outcome measures for hand function and pain), baseline measures of mental health (including treatment credibility [the extent to which a patient attributes credibility to a treatment] and expectations, illness perception, pain catastrophizing, anxiety, and depression), and PREMs were associated with each question of the Satisfaction with Treatment Result Questionnaire at 3 months post-treatment. We dichotomized responses to our first question as good and excellent, which were considered more satisfied, and poor, moderate, and fair, which were considered less satisfied. After dichotomization, 57% (1042 of 1824) of patients were classified as more satisfied with the treatment results.
Results
The following variables were independently associated with satisfaction with treatment results, with an area under the curve of 0.82 (95% confidence interval 0.80 to 0.84) (arranged from the largest to the smallest standardized odds ratio [SOR]): greater decrease in pain during physical load (standardized odds ratio 2.52 [95% CI 2.18 to 2.92]; p < 0.001), patient’s positive experience with the explanation of the pros and cons of the treatment (determined with the question: “Have you been explained the pros and cons of the treatment or surgery?”) (SOR 1.83 [95% CI 1.41 to 2.38]; p < 0.001), greater improvement in hand function (SOR 1.76 [95% CI 1.54 to 2.01]; p < 0.001), patients’ positive experience with the advice for at-home care (determined with the question: “Were you advised by the healthcare providers on how to deal with your illness or complaints in your home situation?”) (SOR 1.57 [95% CI 1.21 to 2.04]; p < 0.001), patient’s better personal control (determined with the question: “How much control do you feel you have over your illness?”) (SOR 1.24 [95% CI 1.1 to 1.40]; p < 0.001), patient’s more positive treatment expectations (SOR 1.23 [95% CI 1.04 to 1.46]; p = 0.02), longer expected illness duration by the patient (SOR 1.20 [95% CI 1.04 to 1.37]; p = 0.01), a smaller number of symptoms the patient saw as part of the illness (SOR 0.84 [95% CI 0.72 to 0.97]; p = 0.02), and less concern about the illness the patient experiences (SOR 0.84 [95% CI 0.72 to 0.99]; p = 0.04). For willingness to undergo the treatment again, the following variables were independently associated with an AUC of 0.81 (95% CI 0.78 to 0.83) (arranged from the largest to the smallest standardized OR): patient’s positive experience with the information about the pros and cons (determined with the question: “Have you been explained the pros and cons of the treatment or surgery?”) (SOR 2.05 [95% CI 1.50 to 2.80]; p < 0.001), greater improvement in hand function (SOR 1.80 [95% CI 1.54 to 2.11]; p < 0.001), greater decrease in pain during physical load (SOR 1.74 [95% CI 1.48 to 2.07]; p < 0.001), patient’s positive experience with the advice for at home (determined with the question: “Were you advised by the healthcare providers on how to deal with your illness or complaints in your home situation?”) (SOR 1.52 [95% CI 1.11 to 2.07]; p = 0.01), patient’s positive experience with shared decision-making (determined with the question: “Did you decide together with the care providers which care or treatment you will receive?”) (SOR 1.45 [95% CI 1.06 to 1.99]; p = 0.02), higher credibility the patient attributes to the treatment (SOR 1.44 [95% CI 1.20 to 1.73]; p < 0.001), longer symptom duration (SOR 1.27 [95% CI 1.09 to 1.52]; p < 0.01), and patient’s better understanding of the condition (SOR 1.17 [95% CI 1.01 to 1.34]; p = 0.03).
Conclusion
Our findings suggest that to directly improve satisfaction with treatment results, clinicians might seek to: (1) improve the patient’s experience with healthcare delivery, (2) try to influence illness perception, and (3) boost treatment expectations and credibility. Future research should confirm whether these suggestions are valid and perhaps also investigate whether satisfaction with treatment results can be predicted (instead of explained, as was done in this study). Such prediction models, as well as other decision support tools that investigate patient-specific needs, may influence experience with healthcare delivery, expectations, or illness perceptions, which in turn may improve satisfaction with treatment results.
Level of Evidence
Level III, therapeutic study.
Introduction
Satisfaction with treatment results is an important outcome domain in striving for patient-centered and value-based healthcare. In these frameworks, the patient is central, and the aim is to achieve high value at low cost [1, 2, 15, 21, 39, 40]. After all, is there value in a technically perfect surgical procedure, with no complications and excellent objective outcomes afterward, if the patient is not satisfied with the treatment results? Although recognized as an important outcome domain [53], the interpretation of satisfaction with treatment results is difficult, and there are doubts about the face validity of questionnaires to measure satisfaction with treatment results [43]. However, the Satisfaction with Treatment Result Questionnaire has good-to-excellent construct validity and very high test-retest reliability [9], and we believe it is reasonable to use it in a study exploring this topic.
Several studies have investigated factors associated with satisfaction with treatment results [3, 4, 12, 14, 17, 20, 22, 27-35, 37, 38, 47, 49, 51]. Marks et al. [31] found associations between satisfaction and pain and symptoms, activities of daily living or function, esthetics, embodiment, strength, ROM, fulfillment of expectations, deformity, workers compensation status, and length of follow-up. Additionally, strong associations have been found between satisfaction and better patient-reported experience measures (PREMs), such as the provision of general and treatment information, and with physician communication and shared decision-making [3, 4, 12, 29, 35, 49]. Furthermore, the relationship with the surgeon, particularly perceived empathy, is a driver of satisfaction with treatment results [22, 32, 38, 51]. Associations with several measures of mental health have also been found. For instance, higher preoperative pain catastrophizing is associated with lower satisfaction after hand surgery [33, 34], and more symptoms of depression are associated with greater dissatisfaction after carpal tunnel release [27]. There is no consensus on the association between treatment expectations and satisfaction with treatment results; several authors suggested that higher expectations may lead to lower satisfaction [14, 20, 30], whereas other studies found a reverse association [12, 17, 28, 37, 47].
Although the aforementioned studies investigated factors associated with patient satisfaction with treatment results, most studies used relatively small samples or used a univariable approach instead of a multivariable approach. Therefore, the independent association of baseline sociodemographics, quality of life, improvement in pain and function, experiences with healthcare delivery, and baseline measures of mental health with satisfaction with treatment results is still unclear. More knowledge on independent factors that are associated with satisfaction with treatment results may help clinicians to directly improve satisfaction with treatment results, as well as inform future studies aiming to develop interventions that improve satisfaction with treatment results.
Therefore, we asked: (1) What factors are independently associated with satisfaction with treatment results at 3 months post-treatment in patients treated for common hand and wrist conditions? (2) What factors are independently associated with the willingness to undergo the treatment again at 3 months post-treatment in patients treated for common hand and wrist conditions? Among the studied factors were baseline sociodemographics, quality of life, improvement in pain and function, experiences with healthcare delivery, and baseline measures of mental health.
Patients and Methods
Study Design
This was a cohort study using a longitudinally maintained, population-based sample of patients with hand and wrist conditions from the Hand Wrist Study Group cohort, reported following the Strengthening the Reporting of Observational Studies in Epidemiology guidelines [50].
Setting
Data collection using GemsTracker electronic data capture tools (GemsTracker 2020) was part of usual care and occurred between August 2018 and May 2020 at Xpert Clinics. GemsTracker is a secure, internet-based application for distributing questionnaires and forms during clinical research and quality registrations. The start date of the current PREM determined the start date of the study. Xpert Clinics comprises 28 clinics for hand surgery and therapy in the Netherlands. Twenty-three surgeons who have been certified by the Federation of European Societies for Surgery of the Hand and more than 150 hand therapists are employed at our treatment centers. At Xpert Clinics, treatment outcomes are evaluated in measurement tracks, each of which consists of treatments with similar relevant outcome domains and timepoints. After a diagnosis is registered during the first consultation, a measurement track is automatically activated, and patient-reported outcome measure forms are emailed to the patient. Details of this procedure have been published [44].
Participants
Participants were eligible for inclusion if they were adults who completed all relevant questionnaires. We included patients who underwent one of the following common treatments: trigger finger release (23% [423 of 1824]), limited fasciectomy (17% [307 of 1824]), trapeziectomy with or without ligament reconstruction tendon interposition for thumb base osteoarthritis (12% [213 of 1824]), carpal tunnel release (29% [521 of 1824]), hand therapy for midcarpal laxity (2% [35 of 1824]), and hand therapy for thumb base osteoarthritis (18% [325 of 1824]) (Table 1). Because the aim of this study was to investigate which factors explain satisfaction with treatment results in a general population of patients treated for hand and wrist disorders, we selected the largest pathology of each of the six largest measurement tracks from our cohort [44]. Patients who underwent operative treatment were assessed at 3 months postoperatively, and patients who underwent nonoperative treatment were assessed 3 months after treatment was initiated.
Table 1.
Characteristics at baseline of all included patients (n = 1824)
| Variable | Value |
| Age in years | 59 ± 11 |
| Sex (male) | 39 (704) |
| Second opinion | 2 (42) |
| Recurrence (yes) | 8 (146) |
| Hand dominance | |
| Right | 88 (1607) |
| Left | 8 (153) |
| Both | 4 (64) |
| Dominant hand treated | 49 (902) |
| Symptom duration in months median (interquartile range) | 12 (6-24) |
| Workload | |
| Not employed | 40 (734) |
| Light | 27 (492) |
| Medium | 23 (427) |
| Heavy | 9 (171) |
| BMI in kg/m2 | 27 ± 5 |
| Smoking (no) | 86 (1571) |
Data presented as mean ± SD or % (n), unless otherwise noted.
We screened 5859 patients with complete sociodemographics and data at baseline. Thirty-eight percent (2248 of 5859) of patients had complete data at 3 months. Finally, participants were eligible for inclusion if they provided a relevant answer to the three PREM items. A total of 424 patients did not do this because they answered “I don’t know” or “not applicable” to a PREM item, leaving 31% (1824 of 5859) for inclusion in the final sample (Fig. 1). There were no additional exclusion criteria.
Fig. 1.
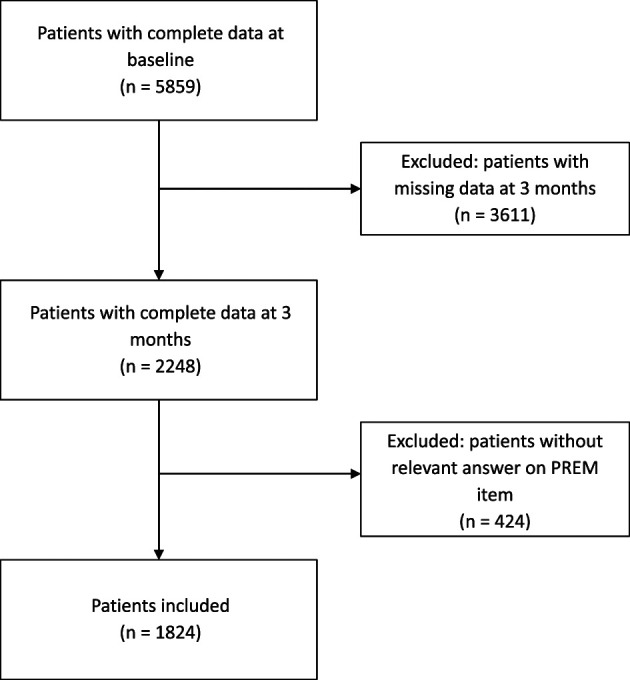
This flowchart illustrates the patient selection for this study.
To assess potential selection bias, we compared responder and nonresponder demographics and measures of mental health using the standardized mean difference as an indication of imbalance [13]. Nonresponders were defined as patients who did not complete questionnaires at 3 months or did not provide a relevant answer to a PREM item. Responders were defined as patients who completed all relevant questionnaires at baseline and at 3 months. Responders and nonresponders both received treatment and remained in care. Besides difference in treatment type (standardized mean difference 0.26), all standardized mean difference values were < 0.2, indicating that the magnitude of the standardized mean difference was even smaller than that defined as small by Cohen [6] (Supplementary Table 1; http://links.lww.com/CORR/A725). Additionally, we conducted a Little test (p = 0.27), which supported the idea that nonresponders could be considered missing at random [7, 25, 26].
Variables and Measurements
The primary outcomes in this study were the two questions of the Satisfaction with Treatment Result Questionnaire at 3 months after the start of treatment. The first question evaluates patients’ satisfaction with treatment results on a 5-point Likert scale (answering options: poor, moderate, fair, good, and excellent). For the second question, patients indicated whether they would undergo the same procedure again under similar circumstances (yes or no). The Satisfaction with Treatment Result Questionnaire has a good-to-excellent construct validity and very high test-retest validity [9].
We classified the variables that were potentially associated with satisfaction into four categories: sociodemographics, clinical patient-reported outcome measures, PREMs, and measures of mental health.
Sociodemographic characteristics included sex (we report sex, not gender, because our data comes from the Dutch Citizen Service Administration; we did not want to make any unsupported assumptions about gender), age, occupational status (unemployed or light, medium, or heavy physical labor), whether the patient visited the clinic for a second opinion, self-reported duration of symptoms (in months), whether the dominant hand was treated, and whether the disease was recurrent (measured by the question: “Have you been treated for the same disease before?”; the answer yes was coded as recurrent).
Clinical patient-reported outcome measures included the change in patient-reported outcome measures for pain and hand function between baseline and 3 months and health-related quality of life at 3 months. We used a VAS score (range 0 to 100) to measure pain during physical load (higher scores indicate more pain) and hand function (higher scores indicate better function). The VAS is a validated and widely used tool for measuring these constructs [16]. Although we also used more disease-specific questionnaires in our cohort (such as the Boston Carpal Tunnel Questionnaire, the Patient-Rated Wrist/Hand Evaluation, and the Michigan Hand outcomes Questionnaire), these differed among the treatments in our study sample and therefore are less well-suited to use for the current research question aiming at all patients with the most common hand and wrist conditions.
We measured health-related quality of life using the VAS of the EuroQol-5 Dimensions (EQ-5D) self-rated health questionnaire as an indication of the overall perceived health status (range 0 to 100; higher scores indicate better perceived health) [19].
To measure the patients’ experience with healthcare delivery (which is different from satisfaction with treatment results [56]), we used the PREM questionnaire, based on the Consumer Quality Index, which is widely used in private practice clinics in the Netherlands [10]. The 11 items evaluate the patients’ experience with healthcare delivery using a 5-point Likert scale (with answers ranging from no, not at all to yes, completely). Of this questionnaire, we only included three items because in the other items, ceiling effects were present that did not allow us to run our models. These items were experience with the explanation about the pros and cons of the treatment, experience with shared decision-making, and experience with the advice for at home.
Measures of mental health included anxiety and depression, pain catastrophizing, illness perceptions, and expectations. Anxiety and depression were measured with the Patient Health Questionnaire-4 (higher scores indicate more anxiety and depression), and pain catastrophizing was measured with the Pain Catastrophizing Scale (higher scores indicate a higher amount of catastrophizing). Illness perception was measured with the Brief Illness Perception Questionnaire [5, 8]. The Brief Illness Perception Questionnaire measures how patients perceive their illness across eight domains (consequences, timeline, personal control, treatment control, identity, concern, coherence, and emotional response). Each domain is assessed with a single question (higher scores indicate more negative illness perceptions except for personal control, treatment control, and coherence) [23]. We excluded the domain of treatment control (“How much do you think your treatment can help your illness?”) from our analyses because we considered that item to have a strong conceptual overlap with the expectancy subscale of the Credibility/Expectancy Questionnaire. Treatment outcome expectations were measured with the Credibility/Expectancy Questionnaire [11]. The credibility subscale consists of three items measuring the credibility that the patient attributes to the treatment. A higher score reflects a higher attribution of credibility to a treatment. The expectancy subscale consists of three items measuring the expected magnitude of improvement because of the prescribed treatment. A higher score reflects a more positive treatment outcome expectation.
Ethical Approval
We obtained ethical approval for this study from Erasmus MC, Rotterdam, the Netherlands (MEC-2018-1088). Written informed consent was obtained from all patients.
Statistical Methods and Study Size
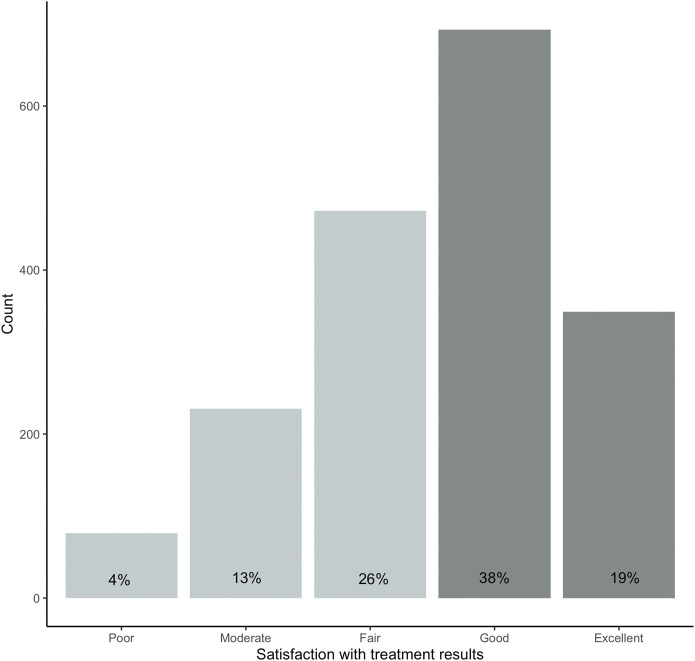
We dichotomized the outcome of satisfaction with treatment results as follows: poor, moderate and fair as less satisfied, and good and excellent as more satisfied. After dichotomization, 57% (1042 of 1824) of participants were classified as more satisfied with the treatment results (19% [349 of 1824] said their results were excellent and 38% [693 of 1824] said they were good) and 43% (782 of 1824) of patients were classified as less satisfied with the treatment results (26% [472 of 1824] reported their satisfaction was fair, 13% [231 of 1824] reported that it was moderate, and 4% [79 of 1824] reported that it was poor) (Fig. 2). This is comparable with other findings in our population [17, 48, 54, 55, 57]. Similarly, to further account for ceiling effects, we dichotomized the PREM items into negative experience (answering options: no, not at all, a little bit, partly, and mostly) and positive experience (answering option: yes, completely). The items used in the final analysis were: “Did you decide together with the care providers which care or treatment you will receive?” (hereinafter referred to as shared decision-making), “Have you been explained the pros and cons of the treatment or surgery?” (henceforth referred to as pros and cons), and “Were you advised by the healthcare providers on how to deal with your illness or complaints in your home situation?” (henceforth referred to as advice).
Fig. 2.
This graph shows the distribution of satisfaction with treatment results at 3 months, before and after dichotomization. Light gray indicates patients who are less satisfied; dark gray indicates those who are more satisfied.
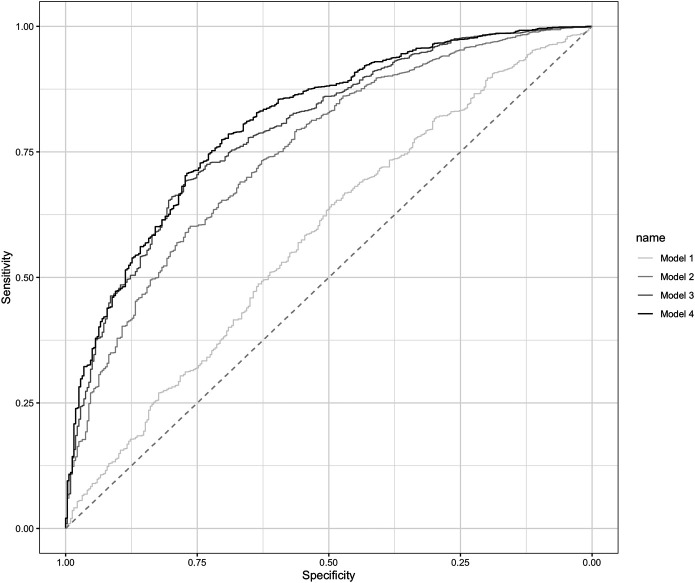
Because this study evaluated a diverse population of patients with common hand and wrist conditions, we adjusted for the type of treatment in the analyses. By adjusting for treatment in our analysis, we accounted for a potential influence of treatment on satisfaction with treatment results. To test the association of specific patient characteristics with satisfaction, we performed a hierarchical logistic regression analysis. In this hierarchical regression analysis, a set of variables is entered in a specific sequence to illustrate the added amount of explained variance of each set. In the first model, sociodemographic patient characteristics were entered, including age, sex, symptom duration, treatment side, dominance, type of work, and second-opinion visit. In the second step, we added clinical patient-reported outcome measures, including the EQ-5D VAS self-rated health at 3 months, the change in VAS pain score during physical load, and VAS function score between baseline and 3 months. In the third step, we added the three items of the PREM: shared decision-making, pros and cons, and advice. In the fourth step, we added measures of mental health, including the Brief Illness Perception Questionnaire items of consequences, timeline, personal control, identity, concern, coherence, emotional response, Patient Health Questionnaire anxiety and depression subscales, Pain Catastrophizing Scale, and Credibility/Expectancy Questionnaire subscales. An advantage of a hierarchical multivariable model is that by entering the next set of variables, certain variables might be pushed out of significance because variables may have shared variance. Therefore, in the most definitive multivariable model, only the variables that truly explain variance in the dependent variable remain. To account for potential strong correlations and multiple variables measuring the same construct, we evaluated multicollinearity using a correlation matrix (Supplementary Table 2; http://links.lww.com/CORR/A726) and variance inflation factor (Supplementary Table 3; http://links.lww.com/CORR/A727). A correlation coefficient of the Spearman rho greater than 0.7 was considered a strong correlation. A variance inflation factor greater than 3 was considered an indication of multicollinearity [24]. Based on the variance inflation factor (the highest variance inflation factor = 2.2) and the correlation matrix (highest Spearman rho = 6.8, which is only a moderate correlation), we did not find any indication for multicollinearity in the hierarchical logistic regression model. To illustrate the goodness of fit of the different models, we determined the area under the curve, the Nagelkerke r2, and the receiver operating characteristic curves for each model.
With 1824 patients, 33 variables, an alpha of 0.05, and a conventional small effect size f2 of 0.02, this study had a power of 95%. We additionally computed univariable associations between all variables. In addition to odds ratios, we reported standardized ORs (SORs) by converting them to the same scale [45]. The nonstandardized ORs in our most definitive model indicate that with every unit increase in either a continuous, dichotomous, or categorical independent variable, the odds of being satisfied with the treatment results or being willing to undergo the treatment again increase or decrease by the value of the nonstandardized OR. Standardized ORs were converted to the same scale, which made it easier to make between-variable comparisons and determine the relative association of each explanatory variable.
All analyses were performed using R Statistical Programming, version 3.3.4 (R Project for Statistical Computing). For all tests, a p value < 0.05 was considered statistically significant.
Results
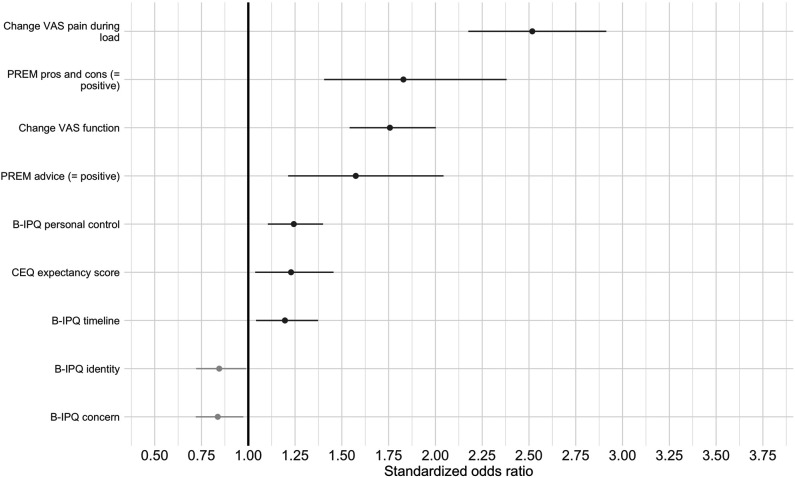
Satisfaction with Treatment Results
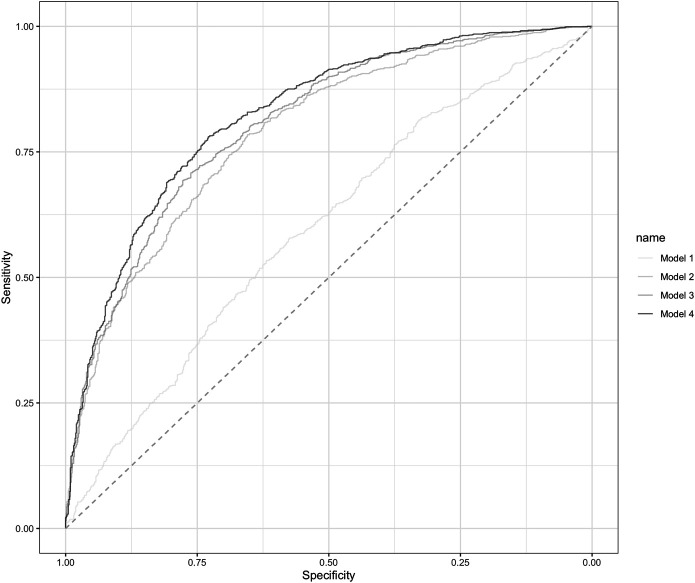
In our most definitive model, we found an area under the curve (AUC) of 0.82 (Table 2), indicating an excellent ability to distinguish more satisfied from less satisfied patients [18]. Satisfaction with the treatment results was associated with the following variables (arranged from the largest to the smallest SOR): greater decrease in pain during physical load (SOR 2.52 [95% CI 2.18 to 2.92]; p < 0.001), patient’s positive experience with the explanation of the pros and cons of the treatment (determined with the question: “Have you been explained the pros and cons of the treatment or surgery?”) (SOR 1.83 [95% CI 1.41 to 2.38]; p < 0.001), greater improvement in hand function (SOR 1.76 [95% CI 1.54 to 2.01]; p < 0.001), patients’ positive experience with the advice for at-home care (determined with the question: “Were you advised by the healthcare providers on how to deal with your illness or complaints in your home situation?”) (SOR 1.57 [95% CI 1.21 to 2.04]; p < 0.001), patient’s better personal control (determined with the question: “How much control do you feel you have over your illness?”) (SOR 1.24 [95% CI 1.10 to 1.40]; p < 0.001), patient’s more positive treatment expectations (SOR 1.23 [95% CI 1.04 to 1.46]; p = 0.02), longer expected illness duration by the patient (SOR 1.20 [95% CI 1.04 to 1.37]; p = 0.01), a smaller number of symptoms the patient saw as part of the illness (SOR 0.84 [95% CI 0.72 to 0.97]; p = 0.02), and less concern about the illness the patient experiences (SOR 0.84 [95% CI 0.72 to 0.99]; p = 0.04) (Fig. 3). When analyzing the separate steps of the different models, sociodemographics alone provided an AUC of 0.60 (95% CI 0.57 to 0.62) for the level of satisfaction with treatment results. When adding clinical characteristics, the AUC was 0.79 (95% CI 0.77 to 0.81). This further increased to 0.81 (95% CI 0.79 to 0.81) when adding PREMs, and finally, the AUC increased to 0.82 (95% CI 0.80 to 0.84) for the level of satisfaction with treatment results after adding measures of mental health (Fig. 4).
Table 2.
Most definitive model after the hierarchical logistic regression analyses (n = 1824) using sociodemographics, clinical characteristics, experience, and mental health characteristics explaining satisfaction with treatment results
| Variables | Range (when applicable) | Nonstandardized OR (95% CI) | Standardized OR (95% CI) | p value |
| Age in years | 0.99 (0.98-1.01) | 0.92 (0.79-1.07) | 0.27 | |
| Sex (male) | 1.22 (0.95-1.59) | 1.22 (0.95-1.59) | 0.13 | |
| BMI | 0.98 (0.96-1.00) | 0.91 (0.81-1.02) | 0.11 | |
| Dominant side treated (yes) | 0.87 (0.69-1.10) | 0.87 (0.69-1.10) | 0.24 | |
| Workload (reference = unemployed) | ||||
| Light | 1.04 (0.76-1.42) | 1.04 (0.76-1.42) | 0.81 | |
| Medium | 1.07 (0.77-1.48) | 1.07 (0.77-1.48) | 0.70 | |
| Heavy | 0.79 (0.50-1.24) | 0.79 (0.50-1.24) | 0.30 | |
| Symptom duration in months | 1.00 (1.00-1.00) | 1.03 (0.91-1.16) | 0.66 | |
| Second opinion (no) | 1.02 (0.48-2.18) | 1.02 (0.48-2.18) | 0.96 | |
| Recurrence (yes) | 0.95 (0.63-1.45) | 0.95 (0.63-1.45) | 0.81 | |
| Smoking (no) | 0.94 (0.67-1.32) | 0.94 (0.67-1.32) | 0.73 | |
| EQ-5D VAS self-rated health | 0-100 | 1.01 (1.00-1.01) | 1.13 (1.00-1.28) | 0.05 |
| Change in VAS pain during load | 0-100 | 1.03 (1.02-1.03) | 2.52 (2.18-2.92) | < 0.001 |
| Change in VAS function | 0-100 | 1.02 (1.01-1.02) | 1.76 (1.54-2.01) | < 0.001 |
| PREM shared decision-making positive (yes) | 1.04 (0.80-1.36) | 1.04 (0.80-1.36) | 0.77 | |
| PREM pros/cons positive (yes) | 1.83 (1.41-2.38) | 1.83 (1.41-2.38) | < 0.001 | |
| PREM advice positive (yes) | 1.57 (1.21-2.04) | 1.57 (1.21-2.04) | < 0.001 | |
| B-IPQ consequences | 0-10 | 0.95 (0.89-1.01) | 0.88 (0.75-1.04) | 0.12 |
| B-IPQ timeline | 0-10 | 1.06 (1.01-1.12) | 1.20 (1.04-1.37) | 0.01 |
| B-IPQ personal control | 0-10 | 1.09 (1.04-1.14) | 1.24 (1.10-1.40) | < 0.001 |
| B-IPQ identity | 0-10 | 0.93 (0.88-0.99) | 0.84 (0.72-0.97) | 0.02 |
| B-IPQ concern | 0-10 | 0.94 (0.89-1.00) | 0.84 (0.72-0.99) | 0.04 |
| B-IPQ coherence | 0-10 | 0.98 (0.92-1.04) | 0.95 (0.84-1.08) | 0.43 |
| B-IPQ emotional response | 0-10 | 1.00 (0.95-1.06) | 1.01 (0.86-1.18) | 0.94 |
| CEQ credibility score | 3-27 | 1.03 (0.98-1.08) | 1.11 (0.95-1.30) | 0.19 |
| CEQ expectancy score | 3-27 | 1.05 (1.01-1.09) | 1.23 (1.04-1.46) | 0.02 |
| PCS total score | 0-52 | 0.99 (0.97-1.00) | 0.90 (0.78-1.04) | 0.17 |
| PHQ-4 total score | 0-12 | 1.01 (0.95-1.08) | 1.03 (0.89-1.18) | 0.70 |
Nonstandardized and standardized odds ratios, 95% CIs, and p values are displayed, along with the AUC and the Nagelkerke r2 for the model; the nonstandardized ORs in our most definitive model indicate that with every unit increase in either a continuous, dichotomous, or categorical independent variable, the odds of being satisfied with the treatment results increase or decrease by the value of the nonstandardized OR; standardized ORs are converted to the same scale, which makes it easier to make between-variable comparisons and determine the relative association of each explanatory variable. Interpretation AUC (ability of the model to discriminate between more satisfied and less satisfied patients) = 0.82; interpretation Nagelkerke r2 (goodness of fit of the model) = 0.39; EQ-5D = EuroQol-5 Dimensions; PREM = patient-reported experience measure; B-IPQ = Brief Illness Perception Questionnaire; CEQ = Credibility/Expectancy Questionnaire; PCS = Pain Catastrophizing Scale; PHQ = Patient Health Questionnaire; OR = odds ratio.
Fig. 3.
This figure shows the standardized ORs of the associated variables for patient satisfaction with treatment results. Positive associations are shown in dark grey; negative associations are shown in light grey; PREM = patient-reported experience measures; CEQ = Credibility/Expectancy Questionnaire; B-IPQ = Brief Illness Perception Questionnaire.
Fig. 4.
This graph shows the area under the receiver operating characteristic curve (AUC) for all models explaining the level of satisfaction with treatment results, using the 5-point Likert scale (question 1). The dashed line indicates a discriminative ability of 0.50. Model 1, including sociodemographics, had an AUC of 0.60, and Model 2, after adding clinical patient-reported outcome measures, had an AUC of 0.79. Model 3, after adding PREMs, had an AUC of 0.81, and after adding measures of mental health, the most definitive model had an AUC of 0.82.
Analyzing differences in variables between the different steps of the model for satisfaction with treatment results, we found that there were two differences (Supplementary Table 4; http://links.lww.com/CORR/A728). First, in Model 1, recurrence (determined with the question: “Have you been treated for the same disease before?”) was associated with a smaller probability of being satisfied with the treatment results (SOR 0.70 [95% CI 0.50 to 1.00]), but after adding the clinical patient-reported outcome measures in Model 2, there was no association. This implies that a different change in patient-reported outcome measure score has a shared variance with recurrence and pushes recurrence out of significance. Furthermore, a different change in patient-reported outcome measure score is the stronger variable. A higher EQ-5D self-rated health score was associated with a larger probability of being satisfied with the treatment results in Model 2 (SOR 1.32 [95% CI 1.18 to 1.48) and Model 3 (SOR 1.29 [95% CI 1.15 to 1.45]). However, after adding measures of mental health and treatment expectations in Model 4, we found that the EQ-5D self-rated health score was no longer associated, and several illness perception items and more positive expectations became associated with being satisfied with the treatment results, which suggests that EQ-5D self-rated health has shared variance with specific measures of mental health, such as illness perception. This means that the mental health measures are the stronger variables (Supplementary Table 5; http://links.lww.com/CORR/A729).
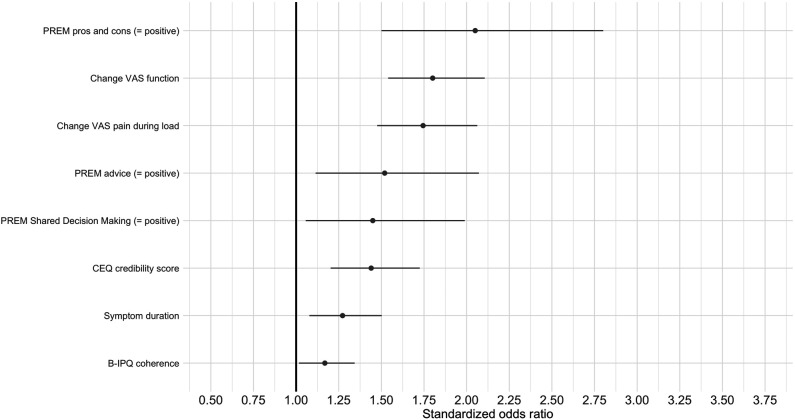
Willingness to Undergo the Treatment Again
In our most definitive model, we found an AUC of 0.81 (Table 3), indicating an excellent ability to distinguish patients who would be willing to undergo the treatment again from patients who would not [18]. Being willing to undergo the treatment again was associated with the following variables (arranged from the largest to the smallest SOR): patient’s positive experience with the information about the pros and cons (determined with the question: “Have you been explained the pros and cons of the treatment or surgery?”) (SOR 2.05 [95% CI 1.50 to 2.80]; p < 0.001), greater improvement in hand function (SOR 1.80 [95% CI 1.54 to 2.11]; p < 0.001), greater decrease in pain during physical load (SOR 1.74 [95% CI 1.48 to 2.07]; p < 0.001), patient’s positive experience with the advice for at-home care (determined with the question: “Were you advised by the healthcare providers on how to deal with your illness or complaints in your home situation?”) (SOR 1.52 [95% CI 1.11 to 2.07]; p = 0.01), patient’s positive experience with shared decision-making (determined with the question: “Did you decide together with the care providers which care or treatment you will receive?”) (SOR 1.45 [95% CI 1.06 to 1.99]; p = 0.02), higher credibility that the patient attributes to the treatment (SOR 1.44 [95% CI 1.20 to 1.73]; p < 0.001), longer symptom duration (SOR 1.27 [95% CI 1.09 to 1.52]; p < 0.01), and patient’s better understanding of the condition (SOR 1.17 [95% CI 1.01 to 1.34]; p = 0.03) (Fig. 5).
Table 3.
Most definitive model after the hierarchical logistic regression analyses (n = 1824) using sociodemographics, clinical characteristics, experience, and mental health characteristics explaining undergo treatment again
| Variables | Range (when applicable) | Nonstandardized OR (95% CI) | Standardized OR (95% CI) | p value |
| Age in years | 0.99 (0.97-1.01) | 0.90 (0.75-1.09) | 0.28 | |
| Sex (male) | 1.11 (0.80-1.54) | 1.11 (0.80-1.54) | 0.53 | |
| BMI | 0.99 (0.96-1.02) | 0.93 (0.81-1.07) | 0.33 | |
| Dominant side treated (yes) | 0.84 (0.63-1.11) | 0.84 (0.63-1.11) | 0.23 | |
| Workload (reference = unemployed) | ||||
| Light | 1.30 (0.87-1.93) | 1.30 (0.87-1.93) | 0.20 | |
| Medium | 0.85 (0.56-1.27) | 0.85 (0.56-1.27) | 0.42 | |
| Heavy | 0.77 (0.44-1.35) | 0.77 (0.44-1.35) | 0.35 | |
| Symptom duration in months | 1.01 (1.00-1.01) | 1.27 (1.09-1.52) | < 0.01 | |
| Second opinion (no) | 1.30 (0.52-3.00) | 1.30 (0.52-3.00) | 0.55 | |
| Recurrence (yes) | 1.00 (0.62-1.64) | 1.00 (0.62-1.64) | 0.99 | |
| Smoking (no) | 0.87 (0.56-1.32) | 0.87 (0.56-1.32) | 0.51 | |
| EQ-5D VAS self-rated health | 0-100 | 1.00 (0.99-1.01) | 0.96 (0.82-1.12) | 0.65 |
| Change in VAS pain during load | 0-100 | 1.02 (1.01-1.02) | 1.74 (1.48-2.07) | < 0.001 |
| Change in VAS function | 0-100 | 1.02 (1.01-1.02) | 1.80 (1.54-2.11) | < 0.001 |
| PREM shared decision-making positive (yes) | 1.45 (1.06-1.99) | 1.45 (1.06-1.99) | 0.02 | |
| PREM pros/cons positive (yes) | 2.05 (1.50-2.80) | 2.05 (1.50-2.80) | < 0.001 | |
| PREM advice positive (yes) | 1.52 (1.11-2.07) | 1.52 (1.11-2.07) | 0.01 | |
| B-IPQ consequences | 0-10 | 0.95 (0.87-1.02) | 0.87 (0.71-1.06) | 0.17 |
| B-IPQ timeline | 0-10 | 1.01 (0.95-1.07) | 1.02 (0.86-1.21) | 0.82 |
| B-IPQ personal control | 0-10 | 1.02 (0.97-1.08) | 1.06 (0.92-1.23) | 0.41 |
| B-IPQ identity | 0-10 | 1.00 (0.93-1.07) | 1.00 (0.82-1.20) | 0.96 |
| B-IPQ concern | 0-10 | 0.99 (0.92-1.06) | 0.96 (0.79-1.17) | 0.71 |
| B-IPQ coherence | 0-10 | 1.08 (1.01-1.16) | 1.17 (1.01-1.34) | 0.03 |
| B-IPQ emotional response | 0-10 | 1.00 (0.94-1.07) | 1.01 (0.83-1.23) | 0.93 |
| CEQ credibility score | 3-27 | 1.11 (1.06-1.18) | 1.44 (1.20-1.73) | < 0.001 |
| CEQ expectancy score | 3-27 | 0.99 (0.94-1.04) | 0.96 (0.78-1.18) | 0.71 |
| PCS total score | 0-52 | 1.00 (0.98-1.02) | 0.97 (0.82-1.15) | 0.73 |
| PHQ-4 total score | 0-12 | 0.98 (0.90-1.06) | 0.96 (0.81-1.13) | 0.59 |
Nonstandardized and standardized odds ratios, 95% CIs, and p values are displayed, along with the AUC and Nagelkerke r2 for the model; the nonstandardized ORs in our most definitive model indicate that with every unit increase in either a continuous, dichotomous, or categorical independent variable, the odds of being willing to undergo the treatment again increase or decrease by the value of the nonstandardized OR; standardized ORs are converted to the same scale, which makes it easier to make between-variable comparisons and determine the relative association of each explanatory variable. Interpretation AUC (ability of the model to discriminate between willing or not willing to undergo again) = 0.81; interpretation of the Nagelkerke r2 (goodness of fit of the model) = 0.29; EQ-5D = EuroQol-5 Dimensions; PREM = patient-reported experience measures; B-IPQ = Brief Illness Perception Questionnaire; CEQ = Credibility/Expectancy Questionnaire; PCS = Pain Catastrophizing Scale; PHQ = Patient Health Questionnaire; OR = odds ratio.
Fig. 5.
This figure shows standardized ORs of the associated variables for the patient’s willingness to undergo the treatment again; PREM = patient-reported experience measures; CEQ = Credibility/Expectancy Questionnaire; B-IPQ = Brief Illness Perception Questionnaire.
For the willingness to undergo treatment again, sociodemographics alone provided an AUC of 0.58 (95% CI 0.55 to 0.62). When adding clinical characteristics, the AUC was 0.75 (95% CI 0.72 to 0.78). This further increased to 0.79 (95% CI 0.77 to 0.82) when adding PREMs, and finally, the AUC was 0.81 (95% CI 0.78 to 0.83) for the willingness to undergo treatment again after adding measures of mental health (Fig. 6).
Fig. 6.
This graph shows the area under the receiver operating characteristic curve (AUC) for all models explaining the patient’s willingness to undergo the treatment again (yes or no; question 2). The dashed line indicates a discriminative ability of 0.50. Model 1, including sociodemographics, had an AUC of 0.58, and after adding clinical patient-reported outcome measures, Model 2 had an AUC of 0.75. After adding PREMs, Model 3 had an AUC of 0.79. After adding measures of mental health, the most definitive model had an AUC of 0.81.
Discussion
In the framework of patient-centered and value-based healthcare, satisfaction with treatment results is an important outcome domain. Before our study, it was unclear which factors were independently associated with satisfaction with treatment results and with a willingness to undergo the treatment again. We found a high explained variance in our models. The following variables were independently associated with satisfaction in either or both models: greater decrease in pain during physical load, patient’s positive experience with the explanation of the pros and cons of the treatment, positive experience with the advice for at-home care (determined with the question: “Were you advised by the healthcare providers on how to deal with your illness or complaints in your home situation?”), patient’s positive experience with shared decision-making, higher credibility that the patient attributes to the treatment, longer symptom duration, better personal control (determined with the question: “How much control do you feel you have over your illness”), patient’s more positive treatment expectations, longer expected illness duration by the patient, patient’s better understanding of the condition, a smaller number of symptoms the patient sees as part of the illness, and less concern about the illness the patient experiences. Many of these variables may be guided and can be used directly in daily clinic or in studies that develop interventions to improve satisfaction with treatment results.
Limitations
One advantage of our observational study design is its representation of daily practice; however, a limitation of the observational design is that a substantial proportion of patients did not respond. However, the nonresponder analysis did not show substantial differences, and the Little test strongly suggests that the data were missing at random. Therefore, we are confident that the high percentage of nonresponders did not influence our results.
A second limitation is the follow-up time in our study. We chose this timepoint because follow-up measurements for the PREM were only obtained at 3 months. As a result, the more extensive surgical treatments may not have reached their endpoint yet, and evaluating satisfaction with treatment results may be too soon at this timepoint. However, theoretically, this should not influence factors explaining variance in satisfaction with treatment results. In fact, there might be more variation in satisfaction with treatment results at 3 months, which may yield better results. Nevertheless, future studies may investigate different timepoints.
Another limitation is the variety of treatment types in our study. Combining different treatment types may have led to dilution of the results because certain variables might interact with the treatment type. However, we aimed to investigate which factors explain satisfaction with treatment results in a general population of patients treated for hand and wrist disorders. Therefore, we selected the most commonly used treatment type in each of the six largest measurement tracks from our cohort and adjusted for the treatment type in our models. By adjusting for the treatment type in our analysis, a potential influence of treatment type on satisfaction with treatment results is accounted for, and the remaining significant variables are independent of treatment type in the final hierarchical model. Therefore, these remaining variables can be generalized to a broader population of patients with hand and wrist conditions. The standardized mean difference between the treatment types was small. This further strengthens the generalizability of our study findings, perhaps even to patients with other musculoskeletal conditions such as hip osteoarthritis. However, future studies should validate our findings in other populations.
Additionally, because satisfaction with treatment results is a multidimensional construct, there are still doubts about the validity of instruments measuring this domain [43, 46]. Although the Satisfaction with Treatment Result Questionnaire has good-to-excellent construct validity and very high test-retest reliability, future studies should further investigate its face validity.
Finally, a very high proportion of our findings can be explained by the variables in our models, and there was relatively little unexplained variance, which may be due to the fact that we did not include all relevant variables in our models, such as additional aspects of experiences with healthcare delivery, coping strategies, goal attainment, the occurrence of complications, personal injury lawsuits, social health, or the specific course of rehabilitation. Additionally, our dichotomization may be a reason for unexplained variance, although this also has added value because our model thereby distinguishes between more satisfied and less satisfied patients. Moreover, although the Brief Illness Perception Questionnaire and Patient Health Questionnaire are valid tools, they might be interpreted differently by individuals, and they function as screening tools and lack the conceptual depth of more extensive questionnaires. Because satisfaction with treatment results is a complex domain, using more comprehensive measures of mental health may yield an even larger proportion of explained variance. Future studies may include these variables when investigating satisfaction with treatment results.
Discussion of Key Findings
Interestingly, all three included PREM items (positive experience with the explanation of the pros and cons, advice for how to deal with the complaints at home, and shared decision-making) were associated with one or both of the Satisfaction with Treatment Result Questionnaire questions (which were: Are you satisfied with the treatment result so far? Would you be willing to undergo the treatment again under similar circumstances?). These findings confirm that the patients’ experience with healthcare delivery is associated with their satisfaction with the result. Based on these findings, healthcare providers may try to improve the experience with healthcare delivery, that is, by always explaining the pros and cons of a treatment and by providing adequate advice on how to deal with the complaints at home (such as by sending emails with treatment-specific information and educational movies). Also, healthcare providers may strive for better shared decision-making. Future research should help determine if this will indeed improve satisfaction with treatment results.
In contrast to previous studies [27, 41, 43, 46, 51], depression was not associated with satisfaction in our most definitive model. However, we did find a univariable association. This suggests that depression has a shared variance with other variables in our models; for example, other mental health items, such as the Illness Perception Questionnaire item of emotional response. Similarly, we did not find an association with pain catastrophizing, while other studies did [33, 34, 42, 51]. No other study on this topic that we know of has investigated the association of depression or pain catastrophizing in combination with illness perception, which may explain why our findings are different from those reported by others.
Another interesting finding here was that a higher score on the Credibility/Expectancy Questionnaire expectancy subscale (the more positive expectations a patient has of a treatment) was associated with better satisfaction with treatment results. This is especially noteworthy because several studies have suggested that clinicians ought to try to temper patients’ expectations [14, 20, 30, 52], and many surgeons believe that it is important to help patients to cultivate reasonable expectations before surgery. By contrast, several other studies have suggested that boosting expectations is associated with better outcomes [12, 17, 28, 36, 37, 47]. Our findings support the latter suggestion. Related to this, the credibility subscale (the extent to which a patient attributes credibility to a treatment) was associated with the patient’s willingness to undergo the treatment again. To our knowledge, no other studies have investigated factors explaining this willingness to undergo treatment again, but it seems sensible that someone who does not find a treatment credible may be less willing to undergo that treatment again. Hence, it might be helpful to investigate possible interventions to boost expectations and improve the credibility of specific treatments.
A possible intervention to influence the experience with healthcare delivery, expectations, and illness perception may be, for example, the creation of a decision-support tool to specifically investigate the patients’ needs for the clinician to respond accordingly. Further, future studies should investigate whether satisfaction with treatment results can be predicted (instead of explained, such as in this study), so that a prediction model could be used as a decision tool and to show what outcomes the patient may expect. Another option is to provide more personalized information relevant to the patient, such as emailing treatment-specific pros and cons. Additionally, to influence illness perception, future studies might investigate the effect of discussing illness perceptions and expectations during the first consultation. However, these suggestions are all hypothetical, and future research should investigate their added value.
Conclusion
We identified several influenceable factors independently associated with satisfaction with treatment results. To directly improve satisfaction with treatment results, clinicians might seek to: (1) improve the patient’s experience with healthcare delivery, (2) influence illness perception, and (3) boost treatment expectations and credibility. However, these recommendations are all hypothetical, and future research should investigate their added value. Moreover, future studies should investigate whether satisfaction with treatment results can be predicted (instead of explained, as was done in this study), so that a prediction model could be used as a decision-support tool that may inform shared decision-making and expectation management. Also, decision-support tools that investigate patient-specific needs may positively influence experience with healthcare delivery, expectations, and illness perception, which in turn may improve satisfaction with treatment results.
Group Authors
Members of the Hand-Wrist Study Group include: Dirk-Johannes Jacobus Cornelis van der Avoort MD; RichardArjen Michiel Blomme MD; Herman Luitzen de Boer MD; Gijs Marijn van Couwelaar MD; Jan Debeij MD, PhD; Jak Dekker MSc; Alexandra Fink PT; Klazina Paulina de Haas MD; Kennard Harmsen MD; Steven Eric Ruden Hovius MD, PhD; Rob van Huis PT; Richard Koch MD; Alexander Kroeze MD; Thybout Matthias Moojen MD, PhD; Mark Johannes Willem van der Oest PhD; Pierre-Yves Alain Adriaan Pennehouat PT; Willemijn Anna de Ridder PT, MSc; Johannes Pieter de Schipper MD; Karin Schoneveld PT, MSc; Berbel Jeannee Rinel Sluijter MD, PhD; Jeronimus Maria Smit MD, PhD; Xander Smit MD, PhD; John Sebastiaan Souer MD, PhD; Marloes Hendrina Paulina ter Stege MSc; Johannes Frederikes Maria Temming MD; Joris Sebastiaan Teunissen BSc; Jeroen Hein van Uchelen MD, PhD; Joris Jan Veltkamp PT; Guus Maarten Vermeulen MD, PhD; Erik Taco Walbeehm MD, PhD; Oliver Theodor Zöphel MD, PhD; Jelle Michiel Zuidam.
Acknowledgments
We thank all the patients who completed questionnaires as part of their clinical care and who agreed that their data could be used anonymously for the present study. We thank the caregivers and other personnel of Xpert Clinics and Equipe Zorgbedrijven for assisting in the routine outcome measurements that are the basis for this study.
Footnotes
Members of the Hand-Wrist Study Group are listed in an Appendix at the end of this article.
The institution of one or more of the authors (RMW, RWS) has received, during the study period, funding from ZonMw.
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from Erasmus MC, Rotterdam, the Netherlands (number MEC-2018-1088).
This work was performed at Erasmus MC, Rotterdam, the Netherlands.
Contributor Information
Robbert Maarten Wouters, Email: r.wouters@erasmusmc.nl.
Lisa Hoogendam, Email: l.hoogendam@erasmusmc.nl.
Guus Maarten Vermeulen, Email: g.vermeulen@xpertclinics.nl.
Harm Pieter Slijper, Email: harm.slijper@gmail.com.
Ruud Willem Selles, Email: r.selles@erasmusmc.nl.
Collaborators: Dirk-Johannes Jacobus Cornelis van der Avoort, Richard Arjen Michiel Blomme, Herman Luitzen de Boer, Gijs Marijn van Couwelaar, Jan Debeij, Jak Dekker, Alexandra Fink, Klazina Paulina de Haas, Kennard Harmsen, Steven Eric Ruden Hovius, Rob van Huis, Richard Koch, Alexander Kroeze, Thybout Matthias Moojen, Mark Johannes Willem van der Oest, Pierre-Yves Alain Adriaan Pennehouat, Willemijn Anna de Ridder, Johannes Pieter de Schipper, Karin Schoneveld, Berbel Jeannee Rinel Sluijter, Jeronimus Maria Smit, Xander Smit, John Sebastiaan Souer, Marloes Hendrina Paulina ter Stege, Johannes Frederikes Maria Temming, Joris Sebastiaan Teunissen, Jeroen Hein van Uchelen, Joris Jan Veltkamp, Guus Maarten Vermeulen, Erik Taco Walbeehm, Oliver Theodor Zöphel, and Jelle Michiel Zuidam
References
- 1.Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med. 2012;366:780-781. [DOI] [PubMed] [Google Scholar]
- 2.Basch E. Patient-Reported outcomes - harnessing patients' voices to improve clinical care. N Engl J Med. 2017;376:105-108. [DOI] [PubMed] [Google Scholar]
- 3.Bernstein J, Kupperman E, Kandel LA, Ahn J. Shared decision making, fast and slow: implications for informed consent, resource utilization, and patient satisfaction in orthopaedic surgery. J Am Acad Orthop Surg. 2016;24:495-502. [DOI] [PubMed] [Google Scholar]
- 4.Bot AG, Bossen JK, Herndon JH, et al. Informed shared decision-making and patient satisfaction. Psychosomatics. 2014;55:586-594. [DOI] [PubMed] [Google Scholar]
- 5.Broadbent E, Petrie KJ, Main J, Weinman J. The Brief Illness Perception questionnaire. J Psychosom Res. 2006;60:631-637. [DOI] [PubMed] [Google Scholar]
- 6.Cohen J. Statistical Power Analysis for the Behavioral Sciences . Lawrence Erlbaum Associates, Publishers; 1988 [Google Scholar]
- 7.de Groot JA, Janssen KJ, Zwinderman AH, et al. Correcting for partial verification bias: a comparison of methods. Ann Epidemiol. 2011;21:139-148. [DOI] [PubMed] [Google Scholar]
- 8.de Raaij EJ, Schröder C, Maissan FJ, Pool JJ, Wittink H. Cross-cultural adaptation and measurement properties of the Brief Illness Perception Questionnaire-Dutch language version. Man Ther. 2012;17:330-335. [DOI] [PubMed] [Google Scholar]
- 9.De Ridder WA, van Kooij YE, Vermeulen GM, et al. Test-retest reliability and construct validity of the satisfaction with treatment result questionnaire in patients with hand and wrist conditions: a prospective study. Clin Orthop Relat Res. 2021;479:2022-2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Delnoij DM, Rademakers JJ, Groenewegen PP. The Dutch consumer quality index: an example of stakeholder involvement in indicator development. BMC Health Serv Res. 2010;10:88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31:73-86. [DOI] [PubMed] [Google Scholar]
- 12.Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: a systematic review. Lancet. 2001;357:757-762. [DOI] [PubMed] [Google Scholar]
- 13.Faraone SV. Interpreting estimates of treatment effects: implications for managed care. P T. 2008;33:700-711. [PMC free article] [PubMed] [Google Scholar]
- 14.Frouzakis R, Herren DB, Marks M. Evaluation of expectations and expectation fulfillment in patients treated for trapeziometacarpal osteoarthritis. J Hand Surg Am. 2015;40:483-490. [DOI] [PubMed] [Google Scholar]
- 15.Goldhahn J, Angst F, Simmen BR. What counts: outcome assessment after distal radius fractures in aged patients. J Orthop Trauma. 2008;22:S126-130. [DOI] [PubMed] [Google Scholar]
- 16.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(suppl 11):S240-252. [DOI] [PubMed] [Google Scholar]
- 17.Hoogendam L, van der Oest MJW, Wouters RM, et al. Patients with higher treatment outcome expectations are more satisfied with the results of nonoperative treatment for thumb base osteoarthritis: a cohort study. Arch Phys Med Rehabil. 2021;102:1533-1540. [DOI] [PubMed] [Google Scholar]
- 18.Hosmer DW, Jr, Lemeshow S, Sturdivant RX. Applied Logistic Regression. John Wiley & Sons; 2013:160-164 [Google Scholar]
- 19.Janssen MF, Bonsel GJ, Luo N. Is EQ-5D-5L better than EQ-5D-3L? A head-to-head comparison of descriptive systems and value sets from seven countries. Pharmacoeconomics. 2018;36:675-697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kadzielski J, Malhotra LR, Zurakowski D, et al. Evaluation of preoperative expectations and patient satisfaction after carpal tunnel release. J Hand Surg (USA). 2008;33:1783-1788. [DOI] [PubMed] [Google Scholar]
- 21.Karnezis IA, Fragkiadakis EG. Association between objective clinical variables and patient-rated disability of the wrist. J Bone Joint Surg Br. 2002;84:967-970. [DOI] [PubMed] [Google Scholar]
- 22.Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27:237-251. [DOI] [PubMed] [Google Scholar]
- 23.Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613-621. [DOI] [PubMed] [Google Scholar]
- 24.Kutner MH, Nachtsheim CJ, Neter J, Li W. Applied Linear Statistical Models. McGraw-Hill; 2005. [Google Scholar]
- 25.Little RJ, D'Agostino R, Cohen ML, et al. The prevention and treatment of missing data in clinical trials. N Engl J Med. 2012;367:1355-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Little RJA. A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association. 1988;83:1198-1202. [Google Scholar]
- 27.Lozano Calderón SA, Paiva A, Ring D. Patient satisfaction after open carpal tunnel release correlates with depression. J Hand Surg (USA). 2008;33:303-307. [DOI] [PubMed] [Google Scholar]
- 28.Mandl LA, Burke FD, Shaw Wilgis EF, et al. Could preoperative preferences and expectations influence surgical decision making? Rheumatoid arthritis patients contemplating metacarpophalangeal joint arthroplasty. Plast Reconstr Surg. 2008;121:175-180. [DOI] [PubMed] [Google Scholar]
- 29.Mandl LA, Galvin DH, Bosch JP, et al. Metacarpophalangeal arthroplasty in rheumatoid arthritis: what determines satisfaction with surgery? J Rheumatol. 2002;29:2488-2491. [PubMed] [Google Scholar]
- 30.Marks M, Audigé L, Reissner L, et al. Determinants of patient satisfaction after surgery or corticosteroid injection for trapeziometacarpal osteoarthritis: results of a prospective cohort study. Arch Orthop Trauma Surg. 2015;135:141-147. [DOI] [PubMed] [Google Scholar]
- 31.Marks M, Herren DB, Vliet Vlieland TPM, et al. Determinants of patient satisfaction after orthopedic interventions to the hand: a review of the literature. J Hand Ther. 2011;24:303-312. [DOI] [PubMed] [Google Scholar]
- 32.Menendez ME, Chen NC, Mudgal CS, Jupiter JB, Ring D. Physician empathy as a driver of hand surgery patient satisfaction. J Hand Surg (USA). 2015;40:1860-1865. [DOI] [PubMed] [Google Scholar]
- 33.Mosegaard SB, Stilling M, Hansen TB. Higher preoperative pain catastrophizing increases the risk of low patient reported satisfaction after carpal tunnel release: a prospective study. BMC Musculoskelet Disord. 2020;21:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mosegaard SB, Stilling M, Hansen TB. Pain Catastrophizing Scale as a predictor of low postoperative satisfaction after hand surgery. J Orthop. 2020;21:245-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Parrish RC, Menendez ME, Mudgal CS, et al. Patient satisfaction and its relation to perceived visit duration with a hand surgeon. J Hand Surg (USA). 2016;41:257-262e254. [DOI] [PubMed] [Google Scholar]
- 36.Peerdeman KJ, van Laarhoven AIM, Keij SM, et al. Relieving patients' pain with expectation interventions: a meta-analysis. Pain. 2016;157:1179-1191. [DOI] [PubMed] [Google Scholar]
- 37.Poelstra R, Selles RW, Slijper HP, et al. Better patients' treatment experiences are associated with better postoperative results in Dupuytren's disease. J Hand Surg Eur Vol. 2018;43:848-854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pollak KI, Alexander SC, Tulsky JA, et al. Physician empathy and listening: associations with patient satisfaction and autonomy. J Am Board Fam Med. 2011;24:665-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477-2481. [DOI] [PubMed] [Google Scholar]
- 40.Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2013;70:351-379. [DOI] [PubMed] [Google Scholar]
- 41.Ring D, Kadzielski J, Fabian L, et al. Self-reported upper extremity health status correlates with depression. J Bone Joint Surg Am. 2006;88:1983-1988. [DOI] [PubMed] [Google Scholar]
- 42.Ring D, Kadzielski J, Malhotra L, Lee SG, Jupiter JB. Psychological factors associated with idiopathic arm pain. J Bone Joint Surg Am. 2005;87:374-380. [DOI] [PubMed] [Google Scholar]
- 43.Ring D, Leopold SS. Editorial-Measuring satisfaction: can it be done? Clin Orthop Relat Res. 2015;473:3071-3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Selles RW, Wouters RM, Poelstra R, et al. Routine health outcome measurement: development, design, and implementation of the Hand and Wrist Cohort. Plast Reconstr Surg. 2020;146:343-354. [DOI] [PubMed] [Google Scholar]
- 45.Sjölander A. Regression standardization with the R package stdReg. Eur J Epidemiol. 2016;31:563-574. [DOI] [PubMed] [Google Scholar]
- 46.Sraj SA. CORR Insights: Test-retest reliability and construct validity of the satisfaction with treatment result questionnaire in patients with hand and wrist conditions: a prospective study. Clin Orthop Relat Res. 2021;479:2033-2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Swarup I, Henn CM, Gulotta LV, Henn RF, 3rd. Patient expectations and satisfaction in orthopaedic surgery: a review of the literature. J Clin Orthop Trauma. 2019;10:755-760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tsehaie J, Spekreijse KR, Wouters RM, et al. Outcome of a hand orthosis and hand therapy for carpometacarpal osteoarthritis in daily practice: a prospective cohort study. J Hand Surg Am. 2018;43:1000-1009.e1001. [DOI] [PubMed] [Google Scholar]
- 49.Tsehaie J, van der Oest MJW, Poelstra R, et al. Positive experience with treatment is associated with better surgical outcome in trapeziometacarpal osteoarthritis. J Hand Surg Eur Vol. 2019;44:714-721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453-1457. [DOI] [PubMed] [Google Scholar]
- 51.Vranceanu AM, Ring D. Factors associated with patient satisfaction. J Hand Surg (USA). 2011;36:1504-1508. [DOI] [PubMed] [Google Scholar]
- 52.Waljee JF, Chung KC. Commentary regarding “Evaluation of expectations and expectation fulfillment in patients treated for trapeziometacarpal osteoarthritis”. J Hand Surg Am. 2015;40:491-492. [DOI] [PubMed] [Google Scholar]
- 53.Wouters RM, Jobi-Odeneye AO, de la Torre A, Joseph A, Hovius SER. A standard set for outcome measurement in patients with hand and wrist conditions: consensus by the International Consortium For Health Outcomes Measurement Hand And Wrist Working Group. J Hand Surg Am. 2021;46:841-855.e847. [DOI] [PubMed] [Google Scholar]
- 54.Wouters RM, Slijper HP, Esteban Lopez L, Hovius SER, Selles RW. Beneficial effects of nonsurgical treatment for symptomatic thumb carpometacarpal instability in clinical practice: a cohort study. Arch Phys Med Rehabil. 2020;101:434-441. [DOI] [PubMed] [Google Scholar]
- 55.Wouters RM, Tsehaie J, Slijper HP, et al. Exercise therapy in addition to an orthosis reduces pain more than an orthosis alone in patients with thumb base osteoarthritis: a propensity score matching study. Arch Phys Med Rehabil. 2019;100:1050-1060. [DOI] [PubMed] [Google Scholar]
- 56.York Health Economics Consortium. Patient-Reported Experience Measure (PREM). 2016. Available at: https://www.yhec.co.uk/glossary/patient-reported-experience-measure-prem/. Accessed November 30, 2021.
- 57.Zhou C, Hovius SER, Pieters AJ, et al. Comparative effectiveness of needle aponeurotomy and collagenase injection for dupuytren's contracture: a multicenter study. Plast Reconstr Surg Glob Open. 2017;5:e1425. [DOI] [PMC free article] [PubMed] [Google Scholar]