Abstract
Background
Lesbian, gay, bisexual, transgender, and queer (LGBTQ) children and adolescents continue to experience unmet healthcare needs, partly because of clinician biases, discrimination, and inadequate education. Although clinician attitudes and knowledge related to sexual and gender minority health have been well studied in other medical specialties, these have been scarcely studied in orthopaedics.
Questions/purposes
(1) What are pediatric orthopaedic healthcare professionals’ attitudes (perceived importance, openness, comfort, and confidence) toward caring for sexual and gender minority youth? (2) What do pediatric orthopaedic healthcare professionals know about caring for this patient population? (3) What factors are associated with clinician attitude and/or knowledge? (4) What existing initiatives to improve orthopaedic care for this population are clinicians aware of at their home institutions?
Methods
All 123 orthopaedic healthcare professionals at two pediatric academic hospitals in the Midwestern and Northeastern United States were sent a 34-question, internet-based, anonymous survey. The survey queried respondent demographics, attitudes, knowledge, and practice behaviors at their home institutions related to the care of sexual and gender minority youth. Respondent attitudes were queried using the Attitudes Summary Measure, which is a survey instrument that was previously validated to assess clinicians’ attitudes regarding sexual and gender minority patients. Items used to assess knowledge and practice behaviors were developed by content experts in LGBTQ health and/or survey design, as well as orthopaedic surgeons to improve face validity and to mitigate push-polling. Attitude and knowledge items used a 5-point Likert scale. Sixty-six percent (81 of 123) of clinicians completed the survey. Of those, 47% (38 of 81) were physicians, 73% (59 of 81) were licensed for fewer than 20 years, 63% (51 of 81) were women, and 53% (43 of 81) described themselves as liberal-leaning. The response proportions were 73% (38 of 52) among eligible physicians specifically and 61% (43 of 71) among other clinicians (nurse practitioners, physician assistants, and registered nurses). To assess potential nonresponse bias, we compared early responders (within 2 weeks) with late responders (after 2 weeks) and found no differences in responder demographics or in questionnaire responses (all p > 0.05). The main outcome measures included responses to the attitude and knowledge questionnaire, as well as the existing practices questionnaire. To answer our research questions regarding clinician attitudes knowledge and awareness of institutional initiatives, we compared participant responses using chi-square tests, the Student t-test, and the McNemar tests, as appropriate. To answer our research question on factors associated with questionnaire responses, we reported data for each question, stratified by hospital, years since licensure, and political leaning. Comparisons were conducted across strata using chi-square tests for Likert response items and ANOVA for continuous response items. All p values less than 0.05 were considered significant.
Results
Of the respondents who reported feeling comfortable treating lesbian, gay, and bisexual (sexual minority) youth, a small proportion reported feeling confident in their knowledge about these patients’ health needs (99% [80 of 81] versus 63% [51 of 80], 36% reduction [95% confidence interval 23% to 47%]; p < 0.001). Similarly, of those who reported feeling comfortable treating transgender (gender minority) youth, a smaller proportion reported feeling confident in their knowledge of their health needs (94% [76 of 81] versus 49% [37 of 76], 45% reduction [95% CI 31% to 59%]; p < 0.001). There was substantial interest in receiving more education regarding the health concerns of LGBTQ people (81% [66 of 81]) and being listed as an LGBTQ-friendly clinician (90% [73 of 81]). Factors that were associated with select attitude and knowledge items were duration of licensure and political leaning; gender identity, institutional affiliation, educational degree, or having LGBTQ friends and family were not associated. Many respondents were aware of the use of clinic intake forms and the electronic medical record to collect and provide patient gender identity and sexual orientation data at their practice, as well as signage and symbols (for example, rainbow posters) to cultivate LGBTQ-welcoming clinic spaces.
Conclusion
There were varying degrees of confidence and knowledge regarding the health needs of sexual and gender minority youth among pediatric orthopaedic healthcare professionals. There was considerable interest in more focused training and better use of medical technologies to improve care for this population.
Clinical Relevance
The study findings support the further investment in clinician training opportunities by healthcare administrators and orthopaedic associations related to the care of sexual and gender minority patients, as well as in the expansion of medical documentation to record and report important patient information such as pronouns and gender identity. Simultaneously, based on these findings, clinicians should engage with the increasing number of educational opportunities, explore their personal biases, and implement changes into their own practices, with the ultimate goal of providing equitable and informed orthopaedic care.
Introduction
An estimated 5.6% of the United States population identified as a sexual and/or gender minority (lesbian, gay, bisexual, transgender, and queer [LGBTQ]) in 2020 [19]. With increasing acceptance and legislative protections across the United States, there has been steady growth in the reported prevalence of LGBTQ individuals, especially children and adolescents [26]. Across 41,884 United States high school students in 2019, 11.7% of boys and 17.8% of girls identified as nonheterosexual [33]; in 2020, nearly 16% of 19- to 24-year-olds identified as LGBTQ [19]. In a recent survey of 3200 high school students from a large urban school district, 9.2% of students identified as a gender other than the sex on their birth certificate [22]. Even the term “queer,” once considered a pejorative term, has been reclaimed by many LGBT people as a more fluid and inclusive term to describe any gender identity or sexual orientation that is distinct from traditional social norms (that is, not straight or cisgender). Despite societal advancements in many countries around the world, LGBTQ youth continue to experience unmet healthcare needs, partly because of clinicians’ biases, discrimination (such as refusal to treat), and inadequate education (for example, incorrect use of pronouns) [18, 27]. These factors jeopardize the basic patient-clinician relationship and perpetuate existing health disparities compared with their heterosexual, cisgender (a person whose gender identity aligns with the person’s assigned sex at birth) peers [18, 25].
Although mounting evidence has documented the disparities in access to orthopaedic care associated with sex assigned at birth, race or ethnicity, socioeconomic status, insurance status, and language proficiency [8, 13, 28], to our knowledge, there have been no published reports on research to identify and understand disparities in care by sexual orientation and gender identity. These factors are critical determinants of patient outcomes [18]. LGBTQ individuals demonstrate lower rates of healthcare use, with associated delays in diagnosis and treatment and reduced proportions of routine and emergency follow-up [17, 20, 38, 49]. Increased medical distrust by LGBTQ patients because of personal and community experiences of discrimination harms the patient-clinician relationship and leads to worse healthcare outcomes [3, 29, 41]. Additionally, the use of hormone therapy, specifically antiandrogen and estrogen, by transgender patients can weaken bones, increasing the risk of musculoskeletal injury (for example, fragility fractures) and slow bone healing [7, 32, 39]. Similarly, the risk of musculoskeletal injury is greater given the higher prevalence of negative coping skills among LGBTQ youth (such as smoking and alcohol use) [5, 18], and higher proportions of violence against these individuals (for example, intimate-partner violence, hate crimes, and bullying) [11, 35]. These trends have been documented across medical specialties in LGBTQ adults and youth alike [18, 40].
Furthermore, LGBTQ-informed care saves lives. For example, upholding respect by simply using the correct pronouns can decrease the rates of suicide in transgender and nonbinary youth by more than 40% [47]. Although other medical specialties such as internal medicine, pediatrics, oncology, and neurology have prioritized the assessment and implementation of strategies to curb LGBTQ healthcare disparities [36, 40, 45], orthopaedic surgery has been slower to address these concerns. This delay can be attributed, in part, to the dearth of reports examining how sexual and gender minorities are perceived and treated by orthopaedic healthcare professionals.
We therefore asked: (1) What are pediatric orthopaedic healthcare professionals’ attitudes (perceived importance, openness, comfort, and confidence) toward caring for sexual and gender minority youth? (2) What do pediatric orthopaedic healthcare professionals know about caring for this patient population? (3) What factors are associated with clinician attitude and/or knowledge? (4) What existing initiatives to improve orthopaedic care for this population are clinicians aware of at their home institutions?
Materials and Methods
Study Design
A 34-question, anonymous, internet-based survey was sent via email to all eligible orthopaedic healthcare professionals (n = 123) on the departmental listservs of two tertiary academic, pediatric hospitals located in large metropolitan areas in the Midwestern (Nationwide Children’s Hospital, Columbus, OH, USA) and Northeastern United States (Boston Children’s Hospital, Boston, MA, USA). Eligible orthopaedic health professionals included attendings and fellows (allopathic and osteopathic) (42% [52 of 123]), advanced practice providers (nurse practitioners and physician assistants) (37% [46 of 123]), and nurses (20% [25 of 123]). Orthopaedic residents were excluded because of the transiency of their pediatric rotations. Responses were collected anonymously for 4 weeks (28 days) during February 2021 and March 2021. After the initial email, two additional email reminders were sent on Days 10 and 20.
Survey Design
The survey was designed in accordance with the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) checklist to collect information regarding orthopaedic clinicians’ attitudes, knowledge, and practices related to the care of LGBTQ youth [9]. The questionnaire was developed on Research Electronic Data Capture [15, 16]. The survey contained five sections: attitudes (12 items, 5-point Likert scale), knowledge (five items, 5-point Likert scale), institutional practices (six items), demographics (nine items), and open comments (four items). Items were modeled after physician surveys conducted on this topic in oncology and internal medicine [40, 43, 45, 46]. Specifically, respondent attitudes were queried using the Attitudes Summary Measure, which is a survey instrument that was previously validated to assess clinicians’ attitudes regarding sexual and gender minority patients [40]. Items used to assess knowledge and practice behaviors were developed by content experts in LGBTQ health and/or survey design as well as orthopaedic clinicians and surgeons to improve face validity and to mitigate push-polling. Key terms were defined at the beginning of the survey (Appendix 1; http://links.lww.com/CORR/A742).
Ultimately, 66% (81 of 123) of the clinicians completed the survey. The response proportion among physicians was 73% (38 of 52) compared with 61% (43 of 71) among the other clinicians (nurse practitioners, physicians assistants, and nurses). Sixty-five percent (53 of 81) of the respondents were from Boston Children’s Hospital, and the other 35% (28 of 81) were from Nationwide Children’s Hospital. The plurality of respondents were physicians (47% [38 of 81]), licensed for fewer than 20 years (73% [59 of 81]), women (63% [51 of 81]), and described themselves as liberal-leaning (53% [43 of 81]). Seventy-eight percent (63 of 81) reported they had a family member and/or close friend who identified as LGBTQ, and 64% (52 of 81) reported that 1% to 10% of their patients during the past year identified as LGBTQ (Table 1).
Table 1.
Respondent demographics (n = 81)
| Characteristic | % (n) |
| Hospital affiliation | |
| Boston Children’s Hospital | 65 (53) |
| Nationwide Children’s Hospital | 35 (28) |
| Licensure or terminal degree | |
| MD | 46 (37) |
| DO | 1 (1) |
| NP | 20 (16) |
| PA | 12 (10) |
| RN | 15 (12) |
| ATC | 1 (1) |
| Prefer not to answer | 5 (4) |
| Years since earning licensure or terminal degree | |
| ≤ 10 | 41 (33) |
| 11-20 | 32 (26) |
| 21-30 | 12 (10) |
| 31 + | 14 (11) |
| Prefer not to answer | 1 (1) |
| Provider type | |
| Surgical | 42 (34) |
| Clinical | 56 (45) |
| Prefer not to answer | 2 (2) |
| Gender identity | |
| Woman | 63 (51) |
| Man | 36 (29) |
| Transgender | 0 (0) |
| Nonbinary or gender-queer | 0 (0) |
| Prefer not to answer | 1 (1) |
| Sexual orientation | |
| Heterosexual | 91 (74) |
| Lesbian | 3 (2) |
| Gay | 0 (0) |
| Bisexual | 2 (2) |
| Queer | 1 (1) |
| Prefer not to answer | 1 (1) |
| Political leaning | |
| Very conservative | 1 (1) |
| Conservative | 6 (5) |
| Centrist or moderate | 30 (24) |
| Liberal | 41 (33) |
| Very liberal | 12 (10) |
| Other | 9 (7) |
| Prefer not to answer | 1 (1) |
| Any family members or close friends who identify as LGBTQ? | |
| Yes | 78 (63) |
| No | 20 (16) |
| Not sure | 2 (2) |
| Approximate % of your patients in the past year who have identified themselves as LGBTQ + | |
| None | 4 (3) |
| 1%-10% | 64 (52) |
| 11%-20% | 9 (7) |
| > 20% | 1 (1) |
| Not sure | 22 (18) |
MD = doctor of medicine; DO = doctor of osteopathic medicine; NP = nurse practitioner; PA = physician assistant; RN = registered nurse; ATC = certified athletic trainer; gender-queer/queer = describes people who think of their gender identity or sexual orientation outside of societal norms (that is, not cisgender or straight); LGBTQ = lesbian, gay, bisexual, transgender, and queer.
To evaluate for nonresponse bias, we compared early responders (within 2 weeks; n = 64) with late responders (after 2 weeks; n = 17) as a proxy for nonrespondents and found no differences in responder demographics or in questionnaire responses (all p > 0.05) (Appendix 2; http://links.lww.com/CORR/A743). This strategy has been described in prior work [48]. We also compared our response rate to another multiinstitution survey of orthopaedic surgeons, as well as to the standards set for medical literature more broadly. For instance, in a 2019 survey of residents at 10 United States orthopaedic surgery programs, the response rate was 64% (178 of 279) [2].
Ethical Approval
The institutional review boards at Boston Children’s Hospital and Nationwide Children’s Hospital deemed the study exempt from approval because it is not human subject research.
Statistical Analyses
All statistical analyses were performed using R version 4.0.1 (R Core Team). Survey responses were summarized for all respondents and stratified by responder characteristics, including gender identity, hospital affiliation, licensure, years since licensure, political leaning, and having LGBTQ family and/or friends. Responses across individual questions, as well as across Attitudes Summary Measure summary scores, were compared across strata. Comparisons were conducted using a chi-square test or t-test, as appropriate, ANOVA for Attitudes Summary Score summary scores, and the McNemar test for reported comfort versus knowledge. P value adjustments were carried out to control the false discovery rate using the Benjamini-Hochberg procedure [4]. All p values less than 0.05 were considered significant.
Results
What Are Pediatric Orthopaedic Healthcare Professionals’ Attitudes Towards Sexual and Gender Minority Youth?
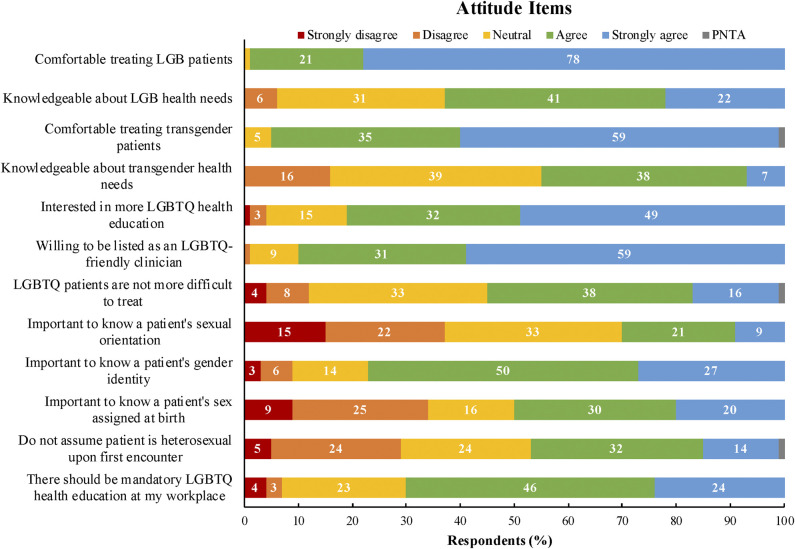
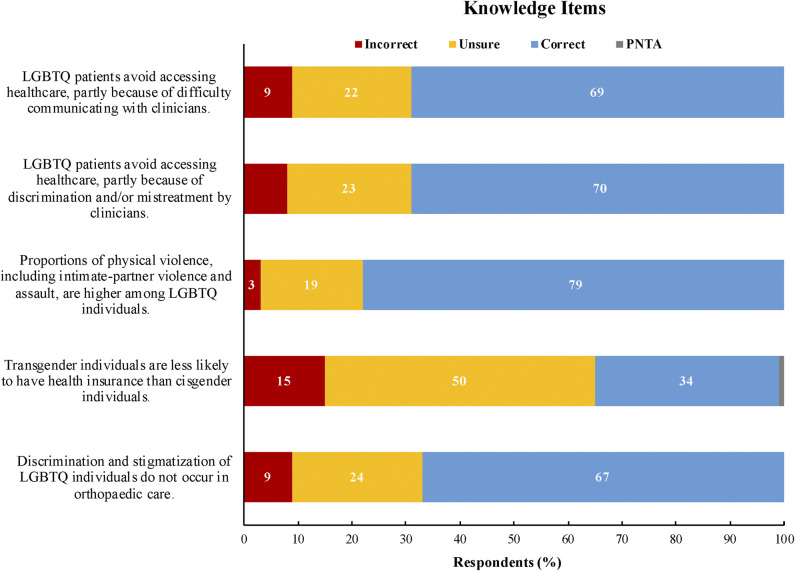
Overall, the surveyed pediatric orthopaedic healthcare professionals were generally comfortable caring for LGBTQ youth, but were less confident in their ability to do so and expressed interest in more education on the subject. Of the respondents who reported feeling comfortable treating lesbian, gay, and bisexual (sexual minority) youth, a small proportion reported feeling confident in their knowledge about these patients’ health needs (99% [80 of 81] versus 63% [51 of 80], 36% reduction [95% CI 23% to 47%]; p < 0.001) (Fig. 1A). Similarly, of the respondents who reported feeling comfortable treating transgender (gender minority) youth, a smaller proportion reported feeling confident in their knowledge of the health needs of these patients (94% [76 of 81] versus 49% [37 of 76], 45% reduction [95% CI 31% to 59%]; p < 0.001) (Fig. 1B). Eighty-one percent (66 of 81) of respondents reported interest in receiving education about the unique health needs of LGBTQ people, and 70% (57 of 81) believed there should be mandatory LGBTQ health education at their workplace (Fig. 2). For the Attitudes Summary Measure subscales, there was a mean comfort-confidence score of 4.1 ± 0.56, practice-beliefs score of 3.4 ± 0.85, and education-involvement score of 4.2 ± 0.68 (Table 2).
Fig. 1.
A-B This graph compares respondents’ (n = 81) self-reported comfort in treating (A) lesbian, gay, and bisexual (LGB)a and (B) transgender patients, and their self-reported confidence in their knowledge of the unique health needs of these populations. A larger proportion of respondents reported feeling comfortable treating LGB and transgender patients than those who reported feeling confident in their knowledge of LGB and/or transgender health needs (p < 0.001, McNemar test). aAttitudes regarding LGB and transgender patients were examined separately because the health needs and disparities differ between sexual (for example, LGB) and gender (for example, transgender) minorities; PNTA = preferred not to answer or missing. A color image accompanies the online version of this article.
Fig. 2.
This graph shows the distribution of responses to the attitude items. Data labels were removed for values less than 3%. Some questions refer to lesbian, gay, and bisexual (LGB) and transgender patients separately because the health needs and disparities differ between sexual (for example, LGB) and gender (for example, transgender) minorities; LGBTQ = lesbian, gay, bisexual, transgender, and queer; PNTA = prefer not to answer or missing. A color image accompanies the online version of this article.
Table 2.
Stratified analyses for attitude items
| Item | Hospital affiliation | Years since earning licensure | ||||||
| Boston Children’s Hospital (n = 53) | Nationwide Children’s Hospital (n = 28) | p value | ≤ 10 (n = 33) | 11-20 (n = 26) | 21-30 (n = 10) | 31 + (n = 11) | p value | |
| I am comfortable treating LGBa people | > 0.99 | > 0.99 | ||||||
| Agree | 98 (52) | 100 (28) | 97 (32) | 100 (26) | 100 (10) | 100 (11) | ||
| Neutral | 2 (1) | 0 (0) | 3 (1) | 0 (0) | 0 (0) | 0 (0) | ||
| Disagree | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||
| I am confident in my knowledge of the health needs of LGB people | 0.63 | 0.88 | ||||||
| Agree | 60 (32) | 68 (19) | 61 (20) | 73 (19) | 50 (5) | 64 (7) | ||
| Neutral | 34 (18) | 25 (7) | 33 (11) | 27 (7) | 20 (2) | 36 (4) | ||
| Disagree | 6 (3) | 7 (2) | 6 (2) | 0 (0) | 30 (3) | 0 (0) | ||
| I am comfortable treating transgender people | > 0.99 | 0.74 | ||||||
| Agree | 94 (50) | 96 (27) | 94 (31) | 100 (26) | 80 (8) | 100 (11) | ||
| Neutral | 6 (3) | 4 (1) | 6 (2) | 0 (0) | 20 (2) | 0 (0) | ||
| Disagree | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||
| I am confident in my knowledge of the health needs of transgender people | 0.86 | 0.88 | ||||||
| Agree | 42 (22) | 54 (15) | 48 (16) | 50 (13) | 30 (3) | 45 (5) | ||
| Neutral | 42 (22) | 32 (9) | 42 (14) | 35 (9) | 20 (2) | 45 (5) | ||
| Disagree | 17 (9) | 14 (4) | 9 (3) | 15 (4) | 50 (5) | 9 (1) | ||
| I would be interested in education regarding the unique health needs of LGBTQ patients | > 0.99 | 0.74 | ||||||
| Agree | 79 (42) | 86 (24) | 88 (29) | 73 (19) | 90 (9) | 73 (8) | ||
| Neutral | 15 (8) | 14 (4) | 12 (4) | 23 (6) | 0 (0) | 18 (2) | ||
| Disagree | 6 (3) | 0 (0) | 0 (0) | 4 (1) | 10 (1) | 9 (1) | ||
| I would be willing to be listed as an LGBTQ-friendly provider | > 0.99 | 0.001b | ||||||
| Agree | 89 (47) | 93 (26) | 94 (31) | 96 (25) | 50 (5) | 100 (11) | ||
| Neutral | 9 (5) | 7 (2) | 6 (2) | 4 (1) | 40 (4) | 0 (0) | ||
| Disagree | 2 (1) | 0 (0) | 0 (0) | 0 (0) | 10 (1) | 0 (0) | ||
| The LGBTQ population is often more difficult to treat | 0.86 | 0.74 | ||||||
| Agree | 13 (7) | 7 (2) | 6 (2) | 12 (3) | 10 (1) | 27 (3) | ||
| Neutral | 38 (20) | 29 (8) | 42 (14) | 35 (9) | 30 (3) | 9 (1) | ||
| Disagree | 49 (26) | 64 (18) | 52 (17) | 54 (14) | 60 (6) | 64 (7) | ||
| It is important to know the sexual orientation of my patients to provide the best care | 0.65 | 0.90 | ||||||
| Agree | 25 (13) | 39 (11) | 27 (9) | 31 (8) | 20 (2) | 45 (5) | ||
| Neutral | 32 (17) | 36 (10) | 39 (13) | 27 (7) | 30 (3) | 27 (3) | ||
| Disagree | 43 (23) | 25 (7) | 33 (11) | 42 (11) | 50 (5) | 27 (3) | ||
| It is important to know the gender identity of my patients to provide the best care | 0.65 | 0.74 | ||||||
| Agree | 72 (38) | 89 (25) | 82 (27) | 77 (20) | 60 (6) | 91 (10) | ||
| Neutral | 17 (9) | 7 (2) | 12 (4) | 15 (4) | 20 (2) | 0 (0) | ||
| Disagree | 11 (6) | 4 (1) | 6 (2) | 8 (2) | 20 (2) | 9 (1) | ||
| It is important to know the patient’s assigned sex at birth to provide the best care | > 0.99 | 0.88 | ||||||
| Agree | 51 (27) | 50 (14) | 55 (18) | 54 (14) | 40 (4) | 36 (4) | ||
| Neutral | 15 (8) | 18 (5) | 21 (7) | 8 (2) | 20 (2) | 18 (2) | ||
| Disagree | 34 (18) | 32 (9) | 24 (8) | 39 (10) | 40 (4) | 45 (5) | ||
| Upon first encounter, I assume a patient is heterosexual | 0.65 | 0.95 | ||||||
| Agree | 25 (13) | 39 (11) | 30 (10) | 27 (7) | 40 (4) | 27 (3) | ||
| Neutral | 21 (11) | 32 (9) | 27 (9) | 19 (5) | 20 (2) | 27 (3) | ||
| Disagree | 55 (29) | 29 (8) | 42 (14) | 54 (14) | 40 (4) | 36 (4) | ||
| There should be mandatory education on LGBTQ health needs at my workplace | 0.65 | 0.10 | ||||||
| Agree | 64 (34) | 82 (23) | 79 (26) | 81 (21) | 40 (4) | 45 (5) | ||
| Neutral | 28 (15) | 14 (4) | 21 (7) | 14 (4) | 40 (4) | 36 (4) | ||
| Disagree | 8 (4) | 4 (1) | 0 (0) | 4 (1) | 20 (2) | 18 (2) | ||
| Attitudes Summary Measure, subscale score | ||||||||
| Comfort confidence, overall = 4.1 ± 0.56 | 4.1 ± 0.57 | 4.1 ± 0.55 | 0.89 | 4.2 ± 0.56 | 4.2 ± 0.49 | 3.8 ± 0.70 | 4.2 ± 0.56 | 0.32 |
| Practice beliefs, overall = 3.4 ± 0.85 | 3.2 ± 0.91 | 3.6 ± 0.69 | 0.20 | 3.5 ± 0.78 | 3.3 ± 0.80 | 2.9 ± 0.99 | 3.4 ± 1.02 | 0.32 |
| Education involvement, overall = 4.2 ± 0.68 | 4.1 ± 0.74 | 4.3 ± 0.55 | 0.50 | 4.3 ± 0.55 | 4.2 ± 0.60 | 3.8 ± 0.92 | 4 ± 0.88 | 0.32 |
Data presented as % (n) or mean ± SD; responses for “strongly agree” and “agree” were combined; responses for “strongly disagree” and “disagree” were combined; “disagree” responses were combined with “neutral” when there were few responses (multiple cell counts < 5); included demographic factors were those for which statistical differences were observed (duration of licensure) in the knowledge or attitude items, or to depict overall response distribution (hospital affiliation).
Attitudes regarding LGB and transgender patients were examined separately because the health needs and disparities differ between sexual (LGB) and gender (transgender) minorities.
Respondents with 21 to 30 years of licensure were 93% less likely to be willing to be listed as an LGBTQ-friendly clinician compared to those with shorter licensure (OR 0.07 [95% CI 0.01 to 0.47); p = 0.001); LGB = lesbian, gay, and bisexual; LGBTQ = lesbian, gay, bisexual, transgender, and queer.
The proportion of respondents who reported feeling confident in their knowledge of the health needs of lesbian, gay, and bisexual (sexual minority) youth at the beginning of the questionnaire decreased when asked again at the end of the questionnaire, with a total of 20 respondents changing their response at the end of the questionnaire (63% [51 of 81] versus 51% (41 of 81), 12% reduction [95% CI 16% to 36%]; p = 0.03). However, there was no change in the proportion of respondents who reported feeling confident in their knowledge of the health needs of transgender (gender minority) youth at the beginning of the questionnaire compared with when asked again at the end of the questionnaire, with a total of 19 respondents changing their responses (46% [37 of 81] versus 37% [30 of 81], 9% reduction [95% CI 15% to 35%]; p = 0.16).
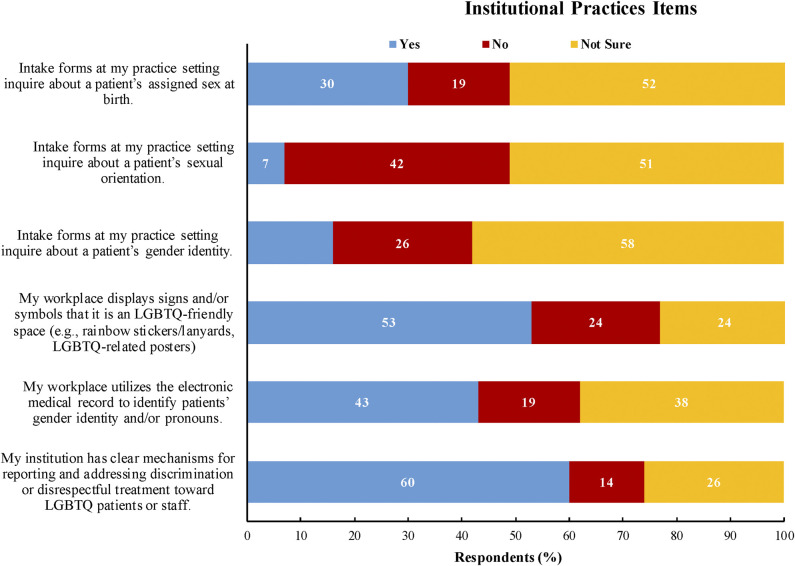
What Knowledge Do Pediatric Orthopaedic Healthcare Professionals Have of the Healthcare Concerns of Sexual and Gender Minority Youth?
There was considerable variability in respondents’ knowledge of the healthcare concerns of sexual and gender minority youth, especially those of transgender patients. Respondents correctly identified that LGBTQ patients generally avoided accessing healthcare, partly because of difficulty communicating with clinicians (69% [56 of 81]) as well as discrimination and/or mistreatment by clinicians (70% [57 of 81]) (Fig. 3) [18]. Sixty-seven percent (54 of 81) stated that discrimination against and stigmatization of LGBTQ individuals occur in orthopaedic care [44]. Seventy-nine percent (64 of 81) of respondents identified that proportions of physical violence, including assault, child abuse, and intimate-partner violence, are higher among LGBTQ communities [11]. Thirty-three percent (27 of 81) of respondents indicated that transgender individuals are less likely to have health insurance than cisgender individuals [23] (Table 3).
Fig. 3.
This graph shows the distribution of responses to the knowledge items. Data labels were removed for values less than 3%. Responses for “strongly agree” and “agree,” and “strongly disagree” and “disagree” were assigned to “correct” and “incorrect” according to existing studies on this topic [11, 18, 23, 44]; LGBTQ = lesbian, gay, bisexual, transgender, and queer; PNTA = prefer not to answer or missing. A color image accompanies the online version of this article.
Table 3.
Stratified analyses for knowledge items
| Item | Hospital affiliation | Years since earning licensure | ||||||
| Boston Children’s Hospital (n = 53) | Nationwide Children’s Hospital (n = 28) | p value | ≤ 10 (n = 33) | 11-20 (n = 26) | 21-30 (n =10) | 31 + (n = 11) | p value | |
| LGBTQ patients avoid accessing healthcare, partly because of difficulty communicating with clinicians | 0.89 | 0.86 | ||||||
| Agreea | 74 (39)a | 61 (17)a | 73 (24)a | 58 (15)a | 70 (7)a | 82 (9)a | ||
| Neutral | 19 (10) | 29 (8) | 21 (7) | 31 (8) | 20 (2) | 9 (1) | ||
| Disagree | 8 (4) | 11 (3) | 6 (2) | 12 (3) | 10 (1) | 9 (1) | ||
| LGBTQ patients avoid accessing healthcare, partly because of discrimination and/or mistreatment by clinicians | 0.89 | 0.86 | ||||||
| Agree | 66 (35)a | 75 (21)a | 70 (23)a | 65 (17)a | 70 (7)a | 73 (8)a | ||
| Neutral | 25 (13) | 21 (6) | 27 (9) | 27 (7) | 20 (2) | 9 (1) | ||
| Disagree | 9 (5) | 4 (1) | 3 (1) | 8 (2) | 10 (1) | 18 (2) | ||
| Proportions of physical violence, including intimate-partner violence and assault, are higher among LGBTQ individuals | 0.89 | 0.86 | ||||||
| Agree | 79 (42)a | 79 (22)a | 85 (28)a | 77 (20)a | 70 (7)a | 82 (9)a | ||
| Neutral | 17 (9) | 21 (6) | 12 (4) | 19 (5) | 30 (3) | 18 (2) | ||
| Disagree | 4 (2) | 0 (0) | 3 (1) | 4 (1) | 0 (0) | 0 (0) | ||
| Transgender individuals are less likely to have health insurance than cisgender individuals | 0.89 | 0.86 | ||||||
| Agree | 30 (16)a | 39 (11)a | 33 (11)a | 42 (11)a | 20 (2)a | 27 (3)a | ||
| Neutral | 57 (30) | 43 (12) | 61 (20) | 38 (10) | 60 (6) | 45 (5) | ||
| Disagree | 13 (7) | 18 (5) | 6 (2) | 19 (5) | 20 (2) | 18 (2) | ||
| Discrimination and stigmatization of LGBTQ individuals do not occur in orthopaedic care | 0.72 | 0.86 | ||||||
| Agree | 13 (7) | 0 (0) | 9 (3) | 12 (3) | 10 (1) | 0 (0) | ||
| Neutral | 25 (13) | 25 (7) | 18 (6) | 19 (5) | 30 (3) | 45 (5) | ||
| Disagree | 62 (33)a | 75 (21)a | 73 (24)a | 69 (18)a | 60 (6)a | 55 (6)a | ||
Data presented as % (n); responses for “strongly agree” and “agree” were combined; responses for strongly disagree” and “disagree” were combined; to maintain statistical integrity, the incorrect answer (either “agree” or “disagree”) was combined with “neutral” when there were few responses (multiple cell counts < 5); included demographic factors were those for which statistical differences were observed (duration of licensure) in the knowledge or attitude items, or to depict overall response distribution (hospital affiliation). aCorrect response based on published studies; LGBTQ = lesbian, gay, bisexual, transgender, and queer.
What Factors Are Associated with Clinician Attitudes and Knowledge?
Of the demographic factors queried, there were few associations detected between demographics and responses. Most notably, respondents with 21 to 30 years of licensure were 93% less likely to be willing to be listed as an LGBTQ-friendly clinician compared with those with shorter licensure (50% [5 of 10] versus 95% [56 of 59], odds ratio = 0.07 [95% CI 0.01 to 0.47]; p = 0.001) (Table 2). There was no difference in responses to any attitude or knowledge items when stratified by the other demographic characteristics (political affiliation, gender identity, institutional affiliation, educational degree, or having LGBTQ friends and family were not associated).
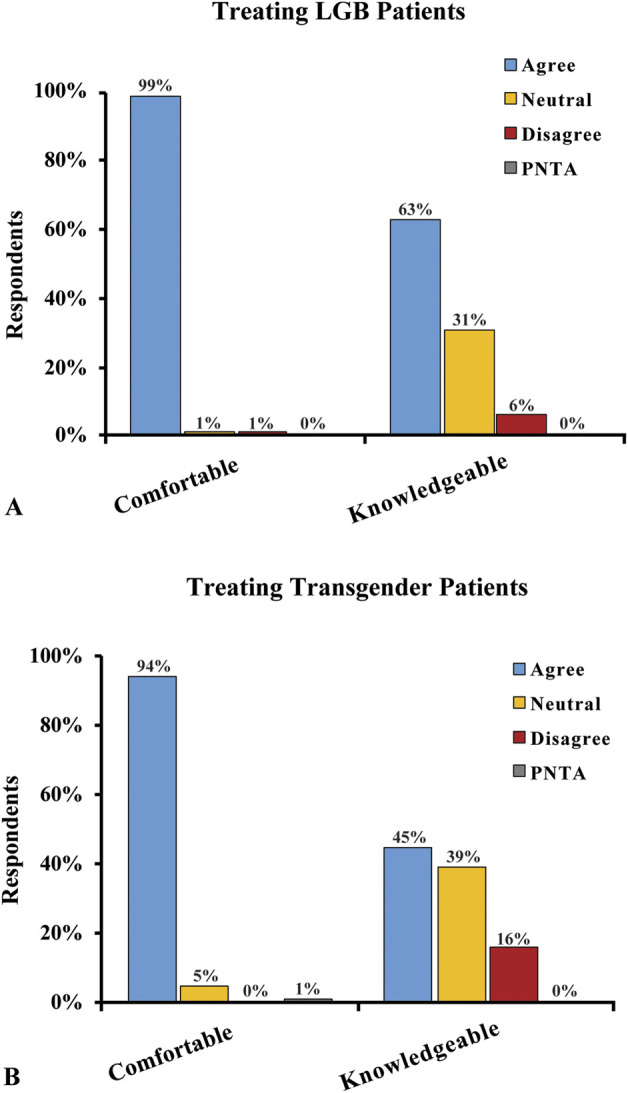
What Existing Initiatives to Improve Orthopaedic Care for LGBTQ Youth are Clinicians Aware of At Their Home Institutions?
Although many respondents were not aware of the main initiatives at their respective home institutions to improve the care of LGBTQ patients, respondents at the Nationwide Children’s Hospital (the Midwestern institution) were more aware of technology-based initiatives, and respondents at Boston Children’s Hospital (the Northeastern institution) were more aware of efforts to cultivate a more LGBTQ-welcoming environment. Thirty-eight percent (31 of 81) and 58% (47 of 81) of respondents were “not sure” about their institution’s use of the electronic medical record and/or intake forms to collect and/or display gender identity and sexual orientation data (Fig. 4). A higher proportion of Midwest-based respondents were aware of the use of intake forms to collect data on patients’ sex assigned at birth, sexual orientation, and gender identity at their home institution than were Northeast-based respondents (sex assigned at birth: 92% [12 of 13] versus 46% [12 of 26], 46% difference [95% CI 16% to 76%]; p = 0.007; sexual orientation: 56% [5 of 9] versus 3% [1 of 31], 53% difference [95% CI 12% to 93%]; p = 0.002; gender identity: 88% [7 of 8] versus 23% [6 of 26], 65% difference [95% CI 28% to 100%]; p = 0.003). Similarly, a higher proportion of Midwest-based respondents were aware of institutional inclusion of patients’ gender identity and/or pronouns in the electronic medical record at their respective home institution than were the Northeast-based respondents (96% [23 of 24] versus 46% [12 of 26], 50% difference [95% CI 25% to 74%]; p < 0.001). However, a higher proportion of Northeast-based respondents were aware of the display of LGBTQ-welcoming signs and/or symbols in their workplace than were the Midwest-based respondents (82% [37 of 45] versus 35% [6 of 17], 47% difference [95% CI 18% to 65%]; p = 0.002) (Table 4).
Fig. 4.
This graph shows the distribution of responses to the institutional practice items; LGBTQ = lesbian, gay, bisexual, transgender, and queer. A color image accompanies the online version of this article.
Table 4.
Institutional practices by hospital
| Item | Hospital affiliation | ||
| Boston Children’s Hospital | Nationwide Children’s Hospital | p value | |
| The intake forms where I primarily practice inquire about a patient’s sex assigned at birth (n = 39) | 0.007 | ||
| Yes | 46 (12 of 26) | 92 (12 of 13) | |
| No | 54 (14 of 26) | 8 (1 of 13) | |
| The intake forms where I primarily practice setting inquire about a patient’s sexual orientation (n = 40) | 0.002 | ||
| Yes | 3 (1 of 31) | 56 (5 of 9) | |
| No | 97 (30 of 31) | 44 (4 of 9) | |
| The intake forms where I primarily practice inquire about a patient’s gender identity (n = 34) | 0.003 | ||
| Yes | 23 (6 of 26) | 88 (7 of 8) | |
| No | 77 (20 of 26) | 13 (1 of 8) | |
| My workplace displays signs and/or symbols that it is an LGBTQ-friendly space (n = 62) | 0.002 | ||
| Yes | 82 (37 of 45) | 35 (6 of 17) | |
| No | 18 (8 of 45) | 65 (11 of 17) | |
| My workplace utilizes the electronic medical record to identify patients’ gender identity and/or pronouns (n = 50) | < 0.001 | ||
| Yes | 46 (12 of 26) | 96 (23 of 24) | |
| No | 54 (14 of 26) | 4 (1 of 24) | |
| My institution has clear mechanisms for reporting and addressing discrimination or disrespectful treatment toward LGBTQ patients or staff (n = 59) | > 0.99 | ||
| Yes | 82 (32 of 39) | 80 (16 of 20) | |
| No | 18 (7 of 39) | 20 (4 of 20) | |
Data presented as % (n); n indicates the number of respondents who responded “yes” or “no”; responses of “not sure” were excluded from this analysis; LGBTQ = lesbian, gay, bisexual, transgender, and queer.
Other Findings: Free-text Comments
Several themes formed among the open comments (Table 5) that were completed by a quarter of the respondents (20 of 81). The first was the desire for more education and research regarding gender identity and sexual orientation in orthopaedic surgery, particularly to better understand the impact of hormone replacement therapy on bone health and surgical recovery and to provide equitable care to the growing number of transgender patients being treated. This theme paralleled provider concerns about unintentionally offending and/or harming LGBTQ patients because of implicit biases and inadequate training. To improve the care of LGBTQ patients, respondents requested that electronic medical records display patient pronouns, gender identity, and name, if it differs from their legal name. Although 14 of 20 respondents in their comments emphasized the importance of knowing patients’ pronouns, gender identity, and sex assigned at birth to provide quality and informed care, 2 of 20 respondents felt that one or more of these elements were not applicable to pediatric orthopaedic care.
Table 5.
Representative free-text comments from respondents
| Important personal experiences treating LGBTQ patients |
| “We have had a long-time patient prefer to be known by a different name, and change to they/them pronouns, and it was a bit of a difficult adjustment because we had known them for so long. But the team has worked hard to recognize their pronouns and name change.” |
| “We treat many transgender patients — I have found that it is very important to take into account gender identity and sex assigned at birth when developing treatment plans, including when based on prevalence of disease.” |
| “Providing gender-affirming care, including using preferred pronouns, always allows for a more productive visit.” |
| “Bone health is incredibly important for those that have transitioned and taking hormones or for those that are female sex and identify as male. I’ve had many women who have transitioned express their frustrations with providers not knowing how to take care of their body in the way of sexual health, STDs, cancer screenings, and orthopaedic care.” |
| Reservations in treating LGBTQ patients |
| “I don’t want to accidentally offend anyone.” |
| “I feel like I might do something ‘wrong’ unintentionally.” |
| “No personal reservations, but lack of overall knowledge and recognizing my own discomfort to make sure patient feels seen and heard in a way that is not stigmatizing or presumptuous.” |
| “Have not received much training in this area.” |
| “I don't think it's necessary to discuss gender identity and sexual orientation in a pediatric orthopaedic clinic visit for an acute injury. I would like to have ways to show support without asking invasive questions.” |
| Suggestions or additional comments on how to improve orthopaedic care for LGBTQ patients |
| “More education.” |
| “It would be preferential to know if they prefer a different pronoun or identify as a different gender than their assigned gender, as well as if they prefer a different name than their legal name.” |
| “More poster/signage identifying us LGBTQ+-friendly providers.” |
| “More questions [on intake forms] about gender identity/sexual orientation. Recognize that hormones/HRT are going to affect how a patient recovers from fracture repair/other surgical intervention.” |
| “Need much more research in this area.” |
| “Own the bone. Important to recognize fragility fractures in at-risk populations, which includes LGBTQ+.” |
LGBTQ = lesbian, gay, bisexual, transgender, and queer.
Discussion
Sexual and gender minority youth experience unmet healthcare needs, partly because of clinicians’ biases, discrimination (such as refusal to treat), and inadequate education (for example, incorrect use of pronouns) [18]. These factors jeopardize the basic patient-clinician relationship and perpetuate existing health disparities [18]. Communication skills, such as referring to patients by their correct pronouns and using gender-neutral terminology, such as “significant other/partner” rather than “husband/wife,” build trust and improve the quality of care [21]. Although other medical specialties have prioritized the assessment and implementation of strategies to curb LGBTQ healthcare disparities [36, 40, 45], orthopaedic surgery has been slower to address these concerns. This delay can be attributed, in part, to the dearth of reports examining how sexual and gender minorities are perceived and treated by orthopaedic healthcare professionals. This study demonstrated varying degrees of confidence and knowledge about the health needs of sexual and gender minority youth among orthopaedic healthcare professionals; survey respondents also expressed considerable interest in further training and using medical technologies to communicate with and care for these patients more effectively. Based on these discoveries, we believe orthopaedic clinicians should engage with the increasing number of educational opportunities, reflect upon their own biases, and implement changes into their own practices to ensure the delivery of equitable orthopaedic care to this growing population. Furthermore, given this gap in knowledge, future studies should assess the attitudes and knowledge of adult orthopaedic healthcare professionals, as well as investigate disparities in the care received by sexual and gender minority patients.
Limitations
This study has several limitations. One important limitation is the potential for response bias. We could only assess those who chose to respond to the survey, resulting in a self-selecting study population. The overall response proportion was 66% (81 of 123), which is considered excellent by medical research standards [10]. It could be that these responders were more interested in the topic of LGBTQ health and may be more comfortable and knowledgeable in caring for LGBTQ patients than the general population of orthopaedic healthcare professionals. Ideally, we would compare the demographics of the respondents compared with those of the population surveyed, but these data do not exist for the entire orthopaedic listservs at both institutions. However, we evaluated nonresponse bias by comparing proxy response variables by early responders (within 2 weeks) and late responders (after 2 weeks) [48], and we found no differences in responder demographics or in questionnaire responses (all p > 0.05) (Appendix 2).
Of those who responded, there is also concern for response acquiescence, or social desirability bias, with respondents hoping to depict themselves as more comfortable treating LGBTQ patients or open to education on LGBTQ concerns. This is a limitation to many self-assessment instruments, and while there may be some inflation in the true comfort, confidence, and openness of some respondents, we believe that the findings are still valuable to study. Perhaps the most susceptible to social desirability bias is the assessment of clinician attitudes toward the care of LGBTQ patients, however, the Attitudes Summary Measure has been previously validated using principal axis factoring and varimax rotation for use in the evaluation of attitudes toward LGBTQ patients [40]. Of note, the Attitudes Summary Measure was not validated for the pediatric population specifically; however, we believe that the items in the questionnaire are not age-dependent.
Another limitation to this study is the possibility that clinician characteristics such as years since licensure (as a proxy for age) and clinician type (surgeon versus nonsurgeon), or gender and clinician type, may interact in confounding ways with survey responses. Due to the ordinal nature of the primary survey responses and the categorical nature of clinician characteristics, our sample was not sufficient to conduct such multivariable ordinal logistic regression analyses. Nonetheless, we believe that interactions between respondent characteristics would not necessarily influence the key takeaways regarding the current comfort and confidence in caring for LGBTQ patients and the overall interest in more education.
A final limitation is that the study population only represents orthopaedic healthcare providers at two large pediatric academic institutions located in two urban areas within the United States where there is a high proportion of LGBTQ patients. Although these two institutions attract diverse clinicians from around the country and the world, these respondents may be more comfortable and knowledgeable about treating sexual and gender minorities given their exposure to this population and existing institutional initiatives. In addition, many respondents were young (41% [33 of 81] having practiced for no more than 10 years) and women (63% [51 of 81]), which is not representative of the broader orthopaedic community that is comprised primarily of men (more than 90%) between the ages of 40 and 59 years old [6]. Furthermore, LGBTQ youth have different health concerns related to orthopaedic care than LGBTQ adults. As such, these findings may apply predominantly to pediatric orthopaedic healthcare professionals in academic urban centers, and they warrant and support further research. This study is functioning as a foundation for subsequent investigations of clinician knowledge and attitudes at the national level among pediatric and adult orthopaedic clinicians.
What Are Pediatric Orthopaedic Healthcare Professionals’ Attitudes Towards Sexual and Gender Minority Youth?
The present study demonstrates overall comfort among respondents in providing orthopaedic care to sexual and gender minority youth and to receiving more education on the subject; however, there was a notable discrepancy between reported comfort treating LGBTQ youth versus confidence in their knowledge about the orthopaedic health concerns of this population, particularly related to the care of transgender patients. This comfort-confidence discrepancy is consistent with the results of similar studies conducted among neurologists and oncologists [36, 40].
Although this comfort-confidence discrepancy may suggest that clinicians feel comfortable treating a population about which they feel that they have limited knowledge, it seems more likely that this disproportionately high clinician confidence is attributable to the variation among respondents regarding the importance of knowing patients’ sex assigned at birth (51% [41 of 81] agreed), gender identity (78% [63 of 81] agreed), and sexual orientation (30% [24 of 81] agreed) in providing quality and compassionate orthopaedic care. As has been well-documented in medical literature, all three characteristics are important on the provider level for clinical decision-making and delivering patient-centered care, as well as on the population level [18]. On the provider level, incorporation of this information may include clinical risk stratification by biological and social factors (for example, recognizing higher rates of smoking among LGBTQ youth when considering wound healing) or building the patient-provider relationship by addressing patients by their correct pronouns.
On the population level, various organizations, including the American Medical Association and the Institute of Medicine, have underscored the need to collect these data on gender identity and sexual orientation to understand the health and treatment of sexual and gender minority patients and to develop policies and programs to combat barriers in the provision of quality, affirming care [1, 18]. Because this variable insight held by respondents regarding the importance of sexual orientation and gender identity data might slow efforts to improve the collection and use of this valuable resource, it is important for orthopaedic healthcare professionals to recognize the relevance of these data. Consistent with existing recommendations by clinicians and LGBTQ health experts, we believe that routinely collecting these data (name, pronoun, gender identity, sex assigned at birth, sexual orientation) on clinic intake forms, rather than during clinical encounters, gives patients the autonomy to choose if they feel comfortable sharing within their personal circumstances (for example, privacy, cultural norms, and whether they yet know this information about themselves) [14].
What Knowledge Do Pediatric Orthopaedic Healthcare Professionals Have of the Healthcare Concerns of Sexual and Gender Minority Youth?
The study identified considerable gaps among respondents in their basic knowledge of sexual and gender minority disparities in healthcare access, utilization, and risk factors, particularly as they relate to the concerns of transgender patients. Such gaps include the awareness of ongoing discrimination and bias impacting the healthcare of LGBTQ youth, as well as the lower rates of insurance among transgender youth. Filling these knowledge gaps is important to providing compassionate care to LGBTQ patients by understanding, for instance, the reasons that LGBTQ youth, as with adults, may delay seeking orthopaedic care or be less likely to attend follow-up visits [34]. Among oncologists, Schabath et al. [40] determined that clinicians with a stronger foundation of basic LGBTQ health knowledge were more likely to understand the importance of integrating this knowledge into their practices.
To build this basic knowledge foundation, we support the development of evidence-based training, resources, and curricular inclusion around topics related to the care of sexual and gender minority patients. Some initiatives are already underway at local residency programs and hospitals, as well as through national and international orthopaedic organizations, including the Ruth Jackson Orthopaedic Society [37], the American Academy of Orthopaedic Surgeons [12], and the Pediatric Orthopaedic Society of North America [37]. Given the considerable interest reported among respondents in receiving more LGBTQ health education expressed in the attitude items and open comments and their agreement with mandating education on these topics, we believe that the Accreditation Council for Graduate Medical Education should formally implement education on sexual and gender minority health into resident curricula. There has been strong advocacy for this policy across medical specialties over the past several years to standardize education on sexual and gender minority health for the next generation of physicians [30]. Such efforts would complement the aforementioned local and national educational initiatives that target orthopaedic clinicians across practice levels.
What Factors Are Associated With Clinician Attitudes and Knowledge?
In our study, only duration of licensure was weakly associated with reported willingness to be listed as an LGBTQ-friendly clinician; other demographic factors, including gender identity, were not associated. These trends were similar to those demonstrated among other medical specialties [40]. As educational resources and opportunities continue to grow, it will be important to better understand the effectiveness of these interventions on clinicians at various stages in their training and how materials should be adapted to target the spectrum of orthopaedic clinicians across subspecialties, as well as across communities where views on these topics may differ. For example, awareness of the delay in cancer diagnoses and treatment among LGBTQ patients is more pertinent in orthopaedic oncology than other subspecialities [31], and training on how to elicit this sensitive information from patients would differ depending on hospital policy or laws. In addition, subsequent larger, multi-institutional studies are necessary to ensure that we achieve sufficient statistical power to detect true differences among other demographic groups if they exist.
What Existing Initiative to Improve Orthopaedic Care for LGBTQ Youth Are Clinicians Aware of at Their Home Institutions?
Many respondents were aware of existing initiatives at their respective pediatric institutions intended to improve care for sexual and gender minority patients. These initiatives include the use of systems-based interventions (for example, eliciting gender identity and sexual orientation on clinic intake forms, and banners displaying patients’ gender identity and pronouns in the electronic medical record) and environment-based efforts to cultivate a more LGBTQ-welcoming healthcare environment (for example, rainbow signage in clinical spaces). These strategies have been found to facilitate the delivery of high-quality care to sexual and gender minority youth [21, 42]. Respondent awareness of these initiatives suggest that larger practice-based interventions are indeed achievable in orthopaedic care. In conjunction with provider-level actions and further education on LGBTQ healthcare, we believe that these institutional efforts will help to build patient trust, strengthen the patient-clinician relationship, and promote more equitable, compassionate, and informed orthopaedic care. This pathway to better healthcare outcomes has been well-established in health disparities research and practice [21, 24]. As healthcare systems increasingly collect data on gender identity and sexual orientation, we will be able to conduct important future studies to evaluate the true impact of institutional patient-facing initiatives (systems- and environment-based) on both patient-reported and objective orthopaedic outcomes across LGBTQ populations—pediatric and adult—for such research has yet to be performed in orthopaedic surgery.
Conclusion
In this study of two pediatric orthopaedic institutions, there were varying degrees of confidence and knowledge regarding the health needs of sexual and gender minority youth among pediatric orthopaedic healthcare professionals. There was considerable interest in more focused training and better use of medical technologies to improve care for this population. The findings support the further investment in clinician training opportunities by healthcare administrators and orthopaedic associations related to the care of sexual and gender minority patients, as well as in the expansion of medical documentation to record and report important patient information such as pronouns and gender identity. Simultaneously, based on these discoveries, clinicians should engage with the increasing number of educational opportunities, explore their personal biases, and implement changes into their own practices, with the ultimate goal of providing equitable and informed orthopaedic care. Finally, given the knowledge gaps, our future studies will assess the attitudes and knowledge of a broader sample of orthopaedic healthcare professionals, and investigate disparities in the care received by sexual and gender minority patients.
Acknowledgments
We thank Jessica Halem MBA, for her thorough review and thoughtful feedback as a consultant on LGBTQ issues and inclusive communication strategies. We also thank Dr. Matthew Schabath PhD, for permission to modify the knowledge, attitudes, and practices assessment developed and validated by his research team.
Footnotes
Each author certifies that there are no funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article related to the author or any immediate family members.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was waived by Boston Children’s Hospital, Boston, MA, USA (IRB-P00037730) and Nationwide Children’s Hospital, Columbus, OH, USA (STUDY00001691).
This work was performed at Boston Children’s Hospital, Boston, MA, USA, and Nationwide Children’s Hospital, Columbus, OH, USA.
Contributor Information
Aliya G. Feroe, Email: aliya_feroe@hms.harvard.edu.
Lauren E. Hutchinson, Email: Lauren_Hutchinson@childrens.harvard.edu.
Patricia E. Miller, Email: Patricia_Miller@childrens.harvard.edu.
Julie Balch Samora, Email: Julie.Samora@nationwidechildrens.org.
References
- 1.American Medical Association. Health care needs of lesbian, gay, bisexual, transgender and queer populations H-160.991. Available at: https://policysearch.ama-assn.org/policyfinder/detail/Health%20Care%20Needs%20of%20Lesbian,%20Gay,%20Bisexual,%20Transgender%20and%20Queer%20Populations%20H-160.991?uri=%2FAMADoc%2FHOD.xml-0-805.xml. Accessed February 24, 2021.
- 2.Araoye I, He JK, Gilchrist S, Stubbs T, McGwin G, Jr, Ponce BA. A national survey of orthopaedic residents identifies deficiencies in the understanding of medical statistics. J Bone Joint Surg Am. 2020;102:e19. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong K, Rose A, Peters N, et al. Distrust of the health care system and self-reported health in the United States. J Gen Intern Med. 2006;21:292-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57:289-300. [Google Scholar]
- 5.Buchting FO, Emory KT, Scout, et al. Transgender use of cigarettes, cigars, and e-cigarettes in a national study. Am J Prev Med. 2017;53:e1-e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cherf J. A snapshot of U.S. orthopaedic surgeons: results from the 2018 OPUS survey. Available at: https://www.aaos.org/aaosnow/2019/sep/youraaos/youraaos01/. Accessed May 23, 2021.
- 7.Dubon ME, Abbott K, Carl RL. Care of the transgender athlete. Curr Sports Med Rep. 2018;17:410-418. [DOI] [PubMed] [Google Scholar]
- 8.Dykes DC, White AA, 3rd. Getting to equal: strategies to understand and eliminate general and orthopaedic healthcare disparities. Clin Orthop Relat Res. 2009;467:2598-2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6:e34-e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fincham JE. Response rates and responsiveness for surveys, standards, and the journal. Am J Pharm Educ. 2008;72:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flores AR, Langton L, Meyer IH, Romero AP. Victimization rates and traits of sexual and gender minorities in the United States: results from the National Crime Victimization Survey, 2017. Sci Adv. 2020;6:eaba6910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Franklin C. A better understanding of gender identity can improve transgender patient care. Available at: https://www.aaos.org/aaosnow/2021/feb/clinical/clinical01/. Accessed February 10, 2021.
- 13.Greene NE, Fuentes-Juárez BN, Sabatini CS. Access to orthopaedic care for Spanish-speaking patients in California. J Bone Joint Surg Am. 2019;101:e95. [DOI] [PubMed] [Google Scholar]
- 14.Guss CE, Eiduson R, Khan A, Dumont O, Forman SF, Gordon AR. “It'd be great to have the options there”: a mixed-methods study of gender identity questions on clinic forms in a primary care setting. J Adolesc Health. 2020;67:590-596. [DOI] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heck JE, Sell RL, Gorin SS. Health care access among individuals involved in same-sex relationships. Am J Public Health. 2006;96:1111-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Institute of Medicine. The Health Of Lesbian, Gay, Bisexual, And Transgender People: Building A Foundation For Better Understanding. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 19.Jones JM. LGBT identification rises to 5.6% in latest U.S. estimate. Available at: https://news.gallup.com/poll/329708/lgbt-identification-rises-latest-estimate.aspx. Accessed February 24, 2021.
- 20.Kachen A, Pharr JR. Health care access and utilization by transgender populations: a United States transgender survey study. Transgender Health. 2020;5:141-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keuroghlian AS, Ard KL, Makadon HJ. Advancing health equity for lesbian, gay, bisexual and transgender (LGBT) people through sexual health education and LGBT-affirming health care environments. Sex Health. 2017;14:119-122. [DOI] [PubMed] [Google Scholar]
- 22.Kidd KM, Sequeira GM, Douglas C, et al. Prevalence of gender-diverse youth in an urban school district. Pediatrics. 2021:e2020049823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koma W, Rae M, Ramaswamy A, Neuman T, Kates J, Dawson L. Demographics, insurance coverage, and access to care among transgender adults. Available at: https://www.kff.org/health-reform/issue-brief/demographics-insurance-coverage-and-access-to-care-among-transgender-adults/. Accessed March 15, 2021.
- 24.McClain Z, Hawkins LA, Yehia BR. Creating welcoming spaces for lesbian, gay, bisexual, and transgender (LGBT) patients: an evaluation of the health care environment. J Homosex. 2016;63:387-393. [DOI] [PubMed] [Google Scholar]
- 25.Meyer IH, Brown TN, Herman JL, Reisner SL, Bockting WO. Demographic characteristics and health status of transgender adults in select US regions: behavioral risk factor surveillance system, 2014. Am J Public Health. 2017;107:582-589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Academies of Sciences, Engineering, and Medicine Committee on Understanding the Well-Being of Sexual Gender Diverse Populations. The National Academies Collection: reports funded by National Institutes of Health. In: White J, Sepúlveda MJ, Patterson CJ, eds. Understanding the Well-being of LGBTQI+ Populations. National Academies Press; 2020. [PubMed] [Google Scholar]
- 27.Newport F. In U.S., estimate of LGBT population rises to 4.5%. Available at: https://news.gallup.com/poll/234863/estimate-lgbt-population-rises.aspx. Accessed February 24, 2021.
- 28.Pandya NK, Wustrack R, Metz L, Ward D. Current concepts in orthopaedic care disparities. J Am Acad Orthop Surg. 2018;26:823-832. [DOI] [PubMed] [Google Scholar]
- 29.Peterson M, Nowotny K, Dauria E, Arnold T, Brinkley-Rubinstein L. Institutional distrust among gay, bisexual, and other men who have sex with men as a barrier to accessing pre-exposure prophylaxis (PrEP). AIDS Care. 2019;31:364-369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pregnall AM, Churchwell AL, Ehrenfeld JM. A call for LGBTQ content in graduate medical education program requirements. Acad Med. 2021;96:828-835. [DOI] [PubMed] [Google Scholar]
- 31.Quinn GP, Sanchez JA, Sutton SK, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA Cancer J Clin. 2015;65:384-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ramsey DC, Lawson MM, Stuart A, Sodders E, Working ZM. Orthopaedic care of the transgender patient. J Bone Joint Surg Am. 2021;103:274-281. [DOI] [PubMed] [Google Scholar]
- 33.Rapoport E, Athanasian CE, Adesman A. Prevalence of nonheterosexual identity and same-sex sexual contact among high school students in the US from 2015 to 2019. JAMA Pediatrics. 2021;175:970-972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reisner SL, Mateo C, Elliott MN, et al. Analysis of reported health care use by sexual orientation among youth. JAMA Network Open. 2021;4:e2124647-e2124647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reisner SL, Sava LM, Menino DD, et al. Addressing LGBTQ student bullying in Massachusetts schools: perspectives of LGBTQ students and school health professionals. Prev Sci. 2020;21:408-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosendale N, Ostendorf T, Evans DA, et al. American Academy of Neurology members' preparedness to treat sexual and gender minorities. Neurology. 2019;93:159-166. [DOI] [PubMed] [Google Scholar]
- 37.Jackson Orthopaedic Society Ruth. Orthopaedic care of the transgender patient. Available at: https://www.youtube.com/watch?v=MC2Fina1lDQ. Accessed May 24, 2021.
- 38.Safer JD, Coleman E, Feldman J, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016;23:168-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sanchez NF, Sanchez JP, Danoff A. Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. Am J Public Health. 2009;99:713-719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schabath MB, Blackburn CA, Sutter ME, et al. National survey of oncologists at National Cancer Institute–designated Comprehensive Cancer Centers: attitudes, knowledge, and practice behaviors about LGBTQ patients with cancer. J Clin Oncol. 2019;37:547-558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schuller KA, Crawford RP. Impact of interpersonal client-provider relationship on satisfaction with mental healthcare among the LGBTQ+ population. J Ment Health. 2020:1-8. [DOI] [PubMed] [Google Scholar]
- 42.Sequeira GM, Kidd K, Coulter RWS, Miller E, Garofalo R, Ray KN. Affirming transgender youths’ names and pronouns in the electronic medical record. JAMA Pediatrics. 2020;174:501-503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shetty G, Sanchez JA, Lancaster JM, Wilson LE, Quinn GP, Schabath MB. Oncology healthcare providers' knowledge, attitudes, and practice behaviors regarding LGBT health. Patient Educ Couns. 2016;99:1676-1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith DM, Mathews WC. Physicians' attitudes toward homosexuality and HIV: survey of a California Medical Society- revisited (PATHH-II). J Homosex. 2007;52:1-9. [DOI] [PubMed] [Google Scholar]
- 45.Streed CG, Jr., Hedian HF, Bertram A, Sisson SD. Assessment of internal medicine resident preparedness to care for lesbian, gay, bisexual, transgender, and queer/questioning patients. J Gen Intern Med. 2019;34:893-898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tamargo CL, Quinn GP, Sanchez JA, Schabath MB. Cancer and the LGBTQ population: quantitative and qualitative results from an oncology providers' survey on knowledge, attitudes, and practice behaviors. J Clin Med. 2017;6:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.The Trevor Project. National survey on LGBTQ youth mental health 2020. Available at: https://www.thetrevorproject.org/survey-2020/. Accessed August 20, 2021.
- 48.Voigt LF, Koepsell TD, Daling JR. Characteristics of telephone survey respondents according to willingness to participate. Am J Epidemiol. 2003;157:66-73. [DOI] [PubMed] [Google Scholar]
- 49.Wolstein J, Charles SA, Babey SH, Diamant AL. Disparities in health care access and health among lesbians, gay men, and bisexuals in California. Policy Brief UCLA Cent Health Policy Res. 2018;2018:1-8. [PubMed] [Google Scholar]