Abstract
Background and Aims:
Intubation in head and neck carcinoma (HNC) is difficult due to many reasons. Various guidelines recommend strategies for airway management in such anticipated difficult airway cases. However, literature is limited on airway management planning as per the level of difficulty based on airway assessment in these patients. EL-Ganzouri risk index (EGRI) has been proposed to aid in making airway management plan in HNC cases by some authors. This retrospective study was conducted to look at the data related to the pre-anesthetic airway assessment and the airway management plan executed by the anesthesiologists in 1000 patients of HNC in the previous nearly four years in order to determine how the choices made conformed to EGRI scores.
Material and Methods:
Records of all the patients with oral cancer posted for surgery over four years from January 2014 to December 2017 were retrospectively analyzed for preoperative airway assessment using El Ganzouri risk index assessment (EGRI), the intraoperative technique for nasotracheal intubation, airway management plan, and any intraoperative complications.
Results:
The risk of predicted airway difficulty was low (EGRI <4) in 38 patients and was high in the rest. The EGRI score was higher in the FOB group [4-9] as compared to DL [2-3] and VL [1-6]. The patients with EGRI >7 were intubated awake and those with EGRI <7 were intubated under general anesthesia (79.8%). Overall, the technique of choice for intubation was fibreoptic bronchoscopy (54%) followed by video laryngoscopy (42.6%).
Conclusion:
The airway management plan used in a tertiary care cancer center conformed to the approach suggested by the multivariate El Ganzouri risk index (EGRI). EGRI appears to be a useful means to ascertain the appropriate strategies for intubation in head and neck cancer patients.
Keywords: Airway management, anesthesia intubation, complications, head and neck neoplasm, retrospective study
Introduction
Head and neck carcinomas (HNC) constitute one of the most common cancers in India.[1] They include carcinomas (ca) involving lip, tongue, gingiva, palate, the floor of the mouth, oropharynx, nasopharynx, hypopharynx, and larynx.[2] The majority of patients have advanced disease (stage 3 and 4), and often require extensive surgery with reconstruction. Airway management usually requires nasotracheal intubation (NTI) in such patients and may be challenging because of associated swelling, decreased submandibular compliance, limited mouth opening, and neck movements. Also, upper airway anatomy is distorted due to tumor, radiation-induced fibrosis, and scarring, which reduces the maneuverability of the oropharynx.[3] Airway assessment can be done using several techniques but considering multiple issues that are expected in such patients a multivariate score like El Ganzouri risk index assessment (EGRI) may be beneficial in providing comprehensive airway assessment for formulating appropriate intubation strategies.[4] Various guidelines suggest planning for potential difficult airway in advance, but these need to be customized as per patient profile, availability of equipment, and expertise of the anesthesiologists. The available techniques to secure the nasotracheal tube in such patients include fibreoptic bronchoscope (FOB), blind, conventional laryngoscope-guided or through video laryngoscope (VL). However, there is no set protocol to help us choose a specific intubation method over others. Awake fibreoptic intubation remains a standard of care for NTI in such cases; however, it has its drawbacks like trauma which can lead to bleeding in cancer patients and affect its outcome. We have retrospectively reviewed the perioperative airway management in patients posted for head and neck cancer surgery to assess how the choices made by anesthesiologists in a tertiary care cancer center conformed to EGRI scores. We have also tried to formulate a plan for intubation strategies in such patients based on the EGRI airway risk assessment score.
Material and Methods
After ethics committee approval (IEC/505/8/2018 dated 24/11/2018), the records of patients undergoing HNC surgery (floor of mouth, tongue, alveolar-buccal complex, and retromolar tumors) were analyzed retrospectively over four years from January 2014 to December 2017 at a tertiary care center. Patients requiring emergency re-exploration and those with incomplete data were excluded. These patients were reviewed for demographic parameters (gender, age, and weight); preoperative airway assessment including nasal patency, intraoperative technique for NTI (direct laryngoscopy/video laryngoscopy/fibreoptic/retrograde), airway management plan (awake vs under anesthesia without muscle relaxant vs. under anesthesia with muscle relaxant), any intraoperative complications for example, epistaxis (visualized while intubation) and oxygen desaturation during intubation (monitored by pulse oximetry), postoperative airway management strategies, time for extubation, postoperative complications, and need for a surgical airway. Using preoperative airway assessment parameters entered in the case records including weight, history of difficult intubation, mouth opening, modified Mallampati score, ability to prognath, thyromental distance, and degree of neck movement, El-Ganzouri multivariate risk index[4] was calculated retrospectively. The intubation strategy adopted by the anesthesiologists was also recorded.
Statistical analysis
The data collected were analyzed using SPSS version 20 (IBM Inc., Chicago, IL, USA). The data are presented as mean (SD), actual numbers, percentage, and median (inter-quartile range). A Chi-square test was done to compare the intubation choices with airway assessment parameters. The EGRI scores for various intubation choices was presented as median (IQR) and range and compared amongst choices. Kruskal Wallis test and pair wise comparison was done using the Mann-Whitney U test. The P value was adjusted as Bonferroni correction.
Results
We reviewed the records of 1050 patients and excluded 50 patients because of incomplete data. Data were analyzed for 1000 patients, out of which the majority (86.1%) were males. The El-Ganzouri risk index (EGRI) score was ≥4 in 962 patients out of 1000.
Majority (97.5%) of the patients with EGRI score >7 underwent awake fibreoptic intubation and 2.5% were intubated through retrograde technique. Two hundred and two patients underwent awake intubation and rest after induction of general anesthesia [Figure 1]. Out of 760 patients with EGRI score of 4-7, 54.2% (412) were intubated using a VL, 45.1% (343) were intubated with FOB under general anesthesia, and only 0.7% (5) were intubated using retrograde intubation. Most of the patients with EGRI <4 (63.5%) were intubated using direct laryngoscopy and the rest (36.5%) using a VL. All patients with EGRI >7 were intubated awake, while the patients with EGRI <7 (both 4-7 and less than 4) were intubated under GA [Figure 2]. Median (range) for EGRI was lesser for those intubated using a DL (2[2-3]) and VL (4[1-6]). However, it was higher for those who were intubated using FOB (5[4-9]) or retrograde intubation 6.5[4-9])[Table 1]. The median (Range) EGRI score was 8 (8-9) in the awake intubation category and 4 (1-4) in patients who were intubated under GA [Table 1].
Figure 1.

Intubation Technique
Figure 2.

Intubation technique based on EL-Ganzouri risk index
Table 1.
Perioperative demographic characteristics and airway assessment and intubation techniques in patients posted for head and neck cancer surgeries
| Parameter | Value | ||||
|---|---|---|---|---|---|
| Gender (M/F) * | 861/139 | ||||
| Age (years)^ | 49.2 (17.4) | ||||
| Weight (kg)^ | 55.1 (7.7) | ||||
| Intubation technique and EGRI | |||||
| <4 (DL/VL/FOB/R) (n (%)) | 38 (24 (63)/14 (37)/0/0) | ||||
| 4-7 (DL/VL/FOB/R) (n (%)) | 760 (0/412 (54)/343 (45)/5 (1)) | ||||
| >7 (DL/VL/FOB/R) (n (%)) | 202 (0/0/197 (98)/5 (2)) | ||||
| Intubation under GA | Median (IQR) - 4.0 (4.0-5.0) * Range - 1.0-7.0 |
||||
| Awake intubation | Median (IQR) - 8.0 (8.0-8.0) Range - 8.0-9.0 |
||||
|
| |||||
| Pair wise comparison between different intubation strategies | |||||
|
| |||||
| Technique | Pair-wise Comparison EGRI | DL | VL | FOB | Retrograde |
| DL Median (IQR) Range |
2.0 (2.0-3.0) 2.0-3.0 |
NA | <0.001 | <0.001 | <0.001 |
| VL Median (IQR) Range |
4.0 (4.0-5.0) 1.0-6.0 |
<0.001 | NA | <0.001 | 0.006 |
| FOB Median (IQR) Range |
5.0 (4.0-8.0) 4.0-9.0 |
<0.001 | <0.001 | NA | 0.300 |
| Retrograde Median (IQR) Range |
6.5 (4.75-8.0) 4.0-9.0 |
<0.001 | 0.006 | 0.300 | NA |
*Values in numbers, ^Mean (SD). M: Male; F: Female, DL: direct laryngoscope; FOB: Fiberoptic bronchoscope; VL: Videolaryngosocpe; R: retrograde; GA: general anaesthesia
Majority (91.9%) of the patients were shifted to the ICU and extubated the next day, only 28 (2.8%) patients were extubated on the table and another 53 (5.3%) underwent tracheostomy before shifting to recovery [Figure 3]. There were no life-threatening complications in any of the patients in the perioperative period. Nasal bleeding occurred in 96 cases and desaturation (fall in oxygen saturation below 92%) occurred in 24 cases.
Figure 3.

Post-operative airway management
Discussion
Our retrospective analysis demonstrated that a DL was used for intubation only in patients with <4 EGRI, a VL used from intubation if EGRI was less than seven (usage increased from 37% in those with EGRI <4 to 54% in those with EGRI 4-7) and a FOB was used for EGRI >4 onwards (usage increased from 5% at EGRI 4-7 to 98% at EGRI >7). A comprehensive airway assessment using a multivariate score like EGRI may help to strategize the airway management plans in patients with potential difficult airways.
The techniques of airway management have undergone significant improvement over the years, but it is still a critical skill and failure to manage the airway may lead to increased complications.[5] HNC is one of the most common malignancies worldwide.[6] Most of the patients present with late complications concerning airway management such as trismus, restricted neck movements, and decreased mouth opening due to radiation fibrosis.[7,8] These patients commonly chew tobacco, gutka, or a pan which leads to oral submucosal fibrosis and makes the airway assessment difficult.[6,9] The foremost concern while anaesthetizing these patients is possible difficulties during both intubation and extubation. Hence, proper assessment and preparation in due consultation with the surgical colleagues are needed.
Preoperative assessment of the airway is utmost necessary to predict a difficult airway. Individual airway assessment parameters do not help in deciding the strategies available for airway management especially in such cases where multiple causes may be responsible for the difficult airway. A comprehensive airway assessment based on focused history, and focused airway assessment is needed to make appropriate strategies for management of airway. The studies assessing the intubation choices in patients with anticipated difficult airway based on comprehensive airway assessment are lacking. Airway assessment methods like the AMF approach that uses the “line of sight” method to ascertain the level of difficulty and risk indices like EGRI, which combine various airway parameters, provide a comprehensive method for airway assessment.[4,10]
EGRI [Table 2] includes seven parameters with a maximum score of 12, a score more than 4 indicates a high risk of the difficult airway. This was described in 1996 when the airway management devices available to anesthesiologists were limited.[4]We tested this risk index retrospectively in our study and found that all the patients with EGRI >7 had undergone awake fibreoptic intubation. Caldiroli and Cortellazzi in their study,[11] also showed that scores more than 7 were more suitable for awake fibreoptic intubation.
Table 2.
El-Ganzouri Risk Index score
| Variable | Finding | Points |
|---|---|---|
| Mouth opening (cm) | >4 | 0 |
| <4 | 1 | |
| Thyromental distance (cm) | >6.5 | 0 |
| 6-6.5 | 1 | |
| <6 | 2 | |
| Mallampati Score | I | 0 |
| II | 1 | |
| III | 2 | |
| Neck movement (°) | >90 | 0 |
| 80-90 | 1 | |
| <80 | 2 | |
| Ability to prognathy | Yes | 0 |
| No | 1 | |
| Body weight (Kg) | <90 | 0 |
| 90-110 | 1 | |
| >110 | 2 | |
| History of difficult intubation | None | 0 |
| Questionable | 1 | |
| Definite | 2 | |
| Total score | 12 |
Traditional teaching suggests all patients with anticipated difficult airway should undergo awake FOB-guided intubation. However, trauma during awake intubation in cancer patients can lead to devastating bleeding in the airway. Also, there may be a situation of potential loss of airway in case appropriate patients are not selected for intubation under GA. In our study also only 20.2% of the patients (EGRI >7) underwent awake intubation, rest 79.8% of the patients underwent intubation under anesthesia. With the recent advent in airway devices, understanding of airway endoscopic anatomy and proficiency in providing local anesthetics and sedation required for intubation, it is advised to do awake fibreoptic intubation for specific airway situations only.[12,13] According to recent ATI guidelines for topicalization, the co-phenylcaine spray (maximum dose of 9 mg/kg of lean body weight) is used for the nasal route, with testing of topicalization atraumatically.[14] In the study conducted by Knudsen et al.,[15] they found that application of local anesthetic during ATI caused more pain, coughing, and suffocation and also it was more discomforting compared to conventional intubation. In our retrospective study we found that preparation for awake FOB-guided intubation included a combination of counseling regarding the need for awake intubation, explanation of the procedure details to the patient, intramuscular glycopyrrolate administered 1h before surgery, nebulization with 4ml of 4% lignocaine, and spray-as-you-go technique using lignocaine. Also, sedation was used as per anesthesiologist preference and patients need in select cases.
In our study, the patients with EGRI 4-7 were intubated by VL or FOB under GA. Hazarika et al.[16] also reported that all patients with EGRI 4-7 except one (had inadequate exposure) could be intubated using a videolaryngoscope under general anesthesia instead of awake fibreoptic intubation. Thus, preemptive use of multivariate risk index scores like El-Ganzouri may help us to decide the intubation technique suitable for such patients.
FOB-guided intubation requires expertise[17,18] but may not be available and not feasible because of bleeding from the tumor mass. In our study, we saw that all the patients with EGRI score of 4-7 were intubated under general anesthesia with videolaryngoscope technique or fibreoptic bronchoscope.
A EGRI <4 is a predicted easy intubation. In our study, we could easily intubate all patients with EGRI <4 using a DL or VL. A laryngoscope-assisted NTI may be an option in these patients, but its usefulness is limited in patients with reduced mouth opening because space is required for its insertion and manipulation is difficult. A video laryngoscope (VL) provides a better glottic view with minimum airway distortion and provides a more direct route to navigate the endotracheal tube (ETT) into the glottis. However, despite a good glottis view, it may be difficult to intubate the trachea and still require the help of devices like Magill’s forceps. But Magill’s forceps has problems like cuff rupture and is traumatic and difficult to guide under vision. The cuff inflation technique has been used to guide the nasal ETT into the glottis by lifting it towards the glottis. It has its advantages over Magill’s and minimizes the risk of cuff rupture and trauma and helps us to guide ET tube under vision.[19] We found that cuff inflation technique with up to 20 ml of air to guide NTI was preferred by anesthesiologists in our study.
We found that retrograde intubation was done in 10 cases. This was not the recommended technique considering the availability of a wide variety of equipment available and we could not find clear reasons why this method was chosen in the presence of flexible fiberscope and patent nasal route. We feel that the senior experienced anesthetists might have used this technique to demonstrate it to residents.
Extubation in these patients maybe more difficult because of pre-existing pathology, extensive, and prolonged surgery, neck dissection, presence of a flap and the expertise available during emergencies to manage edema and bleeding in the oral cavity and neck. Nikhar et al.[20] reported that they could extubate the majority of these patients (50.7%) with proper planning and management and averted complications like tracheostomy, bleeding, obstruction, dislocation, infection, etc.[21]According to Difficult Airway Society Extubation Guidelines,[22] head and neck cancer cases come under the “At risk” category. In our retrospective cohort as well, delayed extubation was done in the majority of cases and airway exchange catheter (AEC) was used as part of the extubation strategy in a few patients extubated in ICU. Some cases still needed tracheostomy, but this was done mainly due to surgical indication. Out of a total of 53 cases that underwent tracheostomy, 15 had involvement of floor of the mouth, 20 had extension into posterior tongue, 10 had involvement of tonsillar pillar, and 8had involvement of hypopharynx.
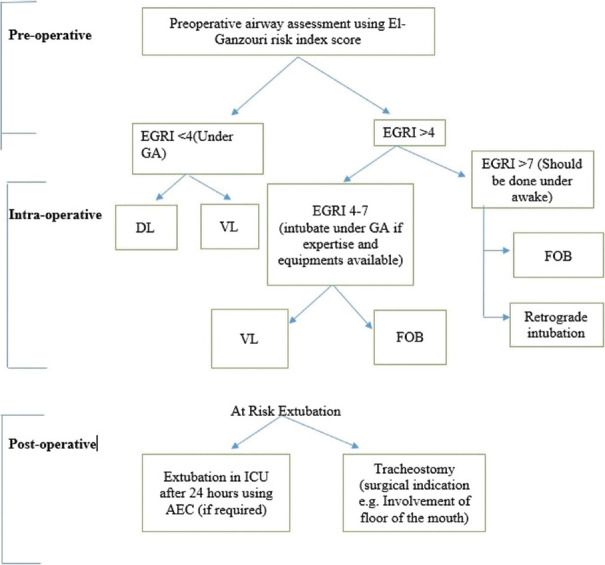
Considering the limited availability and expertise of fibreoptic bronchoscope, videolaryngoscopes and retrograde intubation at many institutions (unlike our institution where this study was conducted), one cannot afford to rely on single equipment as a sole plan for intubation. So, based on this retrospective analysis, we propose a protocol for comprehensive airway management planning in these patients [Figure 4]. This protocol needs to be tested prospectively for validation. If the score is less than four one can consider laryngoscopy (preferably video laryngoscope) as plan A for intubation provided mouth opening is sufficient to introduce it. If the score is more than 7, awake intubation using fibreoptic bronchoscope or video laryngoscope as per availability and expertise should be done. Awake VL has been described in the literature as easier and faster compared to awake FOB[13] but very limited mouth opening can make the use of VL impossible, as an inter-dental distance of at least 18–20 mm is required to insert even the narrow blades.[23] Awake VL was not used in the cases studied probably because consultants at our institution feel that conducting, demonstrating, and teaching FOB is more important than awake VL. In the process, they are short of expertise in doing awake VL. Also, many of our patients had intra-oral cancer and there was a possibility of bleeding during awake VL intubation, which may be disastrous. Patients with score 4-7 come under the gray zone and Plan A should be individualized as per available equipment, setup, and expertise.
Figure 4.
Suggested airway management protocol in Head and neck cancer patients. *Difficult airway cart, emergency drugs (e.g. Atropine, adrenaline) and defibrillator should always be ready at all stages. DL: Direct laryngoscopy, VL: Video laryngoscopy, FOB: Fibreoptic bronchoscopy
Our study has a few limitations. First, this is a retrospective study wherein the EGRI score and management carried out were recorded from the documentation done by the anesthesiologists who had managed those cases, and this could have led to missing information. Second, the airway choices were made by experienced anesthesiology consultants in a single center. The practices may be variable at other centers with less experienced anesthesiologists. It is not clear how these findings will apply to resource limited settings where all the airway management devices and/or skills may not be present.
Conclusion
Airway management in head and neck cancer patients remains a challenge to anesthesiologists and needs to be individualized. The airway management choices made in head and neck cancer cases by experienced anesthesiologists over four years in a tertiary care cancer center conformed to the suggestions made by the simplified multivariate El-Ganzouri risk index score. We feel that the usage algorithm of EGRI should be modified slightly to make it even more useful. Proper airway assessment and planning of management using the modified EGRI may help in better planning and may further reduce morbidity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mehrotra R, Singh M, Gupta RK, Singh M, Kapoor AK. Trends of prevalence and pathological spectrum of head and neck cancers in North India. Indian J Cancer. 2005;42:89–93. doi: 10.4103/0019-509x.16698. [DOI] [PubMed] [Google Scholar]
- 2.Shah JP, Gil Z. Current concepts in management of oral cancer--surgery. Oral Oncol. 2009;45:394–401. doi: 10.1016/j.oraloncology.2008.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bhurgri Y, Bhurgri A, Hassan SH, Zaidi SH, Rahim A, Sankaranarayanan R, et al. Cancer incidence in Karachi, Pakistan:First results from Karachi Cancer Registry. Int J Cancer. 2000;85:325–9. doi: 10.1002/(sici)1097-0215(20000201)85:3<325::aid-ijc5>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 4.El-Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD. Preoperative airway assessment:Predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197–204. doi: 10.1097/00000539-199606000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Bhatnagar S, Mishra S, Jha RR, Singhal AK. Predicting difficult laryngoscopy in oral cancer patients. Indian J Anaesth. 2005;49:413–6. [Google Scholar]
- 6.Siddiqui AS, Dogar SA, Lal S, Akhtar S, Khan F. A. Airway management and postoperative length of hospital stay in patients undergoing head and neck cancer surgery. J Anaesth Clin Pharmaco. 2016;32:49–53. doi: 10.4103/0970-9185.173341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhurgri Y, Bhurgri A, Usman A, Pervez S, Kayani N, Bashir I, et al. Epidemiological review of head and neck cancers in Karachi. Asian Pac J Cancer Prev. 2006;7:195–200. [PubMed] [Google Scholar]
- 8.Tumino R, Vicario G. Head and neck cancers:Oral cavity, pharynx, and larynx. Epidemiol Prev. 2004;28:28–33. [PubMed] [Google Scholar]
- 9.Anila K, Kaveri H, Naikmasur VG. Comparative study of oral micronucleated cell frequency in oral submucous fibrosis patients and healthy individuals. J Clin Exp Dent. 2011;3:201–6. [Google Scholar]
- 10.Kumar R, Kumar S, Misra A, Kumar NG, Gupta A, Kumar P, et al. A new approach to airway assessment—“Line of Sight”and more. Recommendations of the Task Force of Airway Management Foundation (AMF) J Anaesthesiol Clin Pharmacol. 2020;36:303–15. doi: 10.4103/joacp.JOACP_236_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caldiroli D, Cortellazzi P. A new difficult airway management algorithm based upon the El Ganzouri risk index and GlideScope®videolaryngoscope:A new look for intubation? Minerva Anestesiol. 2011;77:1011–7. [PubMed] [Google Scholar]
- 12.Ahmad I, Bailey CR. Time to abandon awake fibreoptic intubation? Anaesthesia. 2016;71:12–6. doi: 10.1111/anae.13333. [DOI] [PubMed] [Google Scholar]
- 13.Leslie D, Stacey M. Awake intubation. Continuing Educ Anaesth Crit Care Pain. 2015;15:64–7. [Google Scholar]
- 14.Ahmad I, El-Boghdadly K, Bhagrath R, Hodzovic I, McNarry AF, Mir F, et al. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. 2020;75:509–28. doi: 10.1111/anae.14904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knudsen K, Nilsson U, Högman M, Pöder U. Awake intubation creates feelings of being in a vulnerable situation but cared for in safe hands:A qualitative study. BMC Anesthesiol. 2016;16:71. doi: 10.1186/s12871-016-0240-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hazarika H, Saxena A, Meshram P, Bhargava AK. A randomized controlled trial comparing C Mac D Blade and Macintosh laryngoscope for nasotracheal intubation in patients undergoing surgeries for head and neck cancer. Saudi J Anaesth. 2018;12:35–41. doi: 10.4103/sja.SJA_239_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hall CE, Shutt LE. Nasotracheal intubation for head and neck surgery. Anaesthesia. 2003;58:249–56. doi: 10.1046/j.1365-2044.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 18.Ovassapian A. Fiberoptic-assisted management of the airway. In: Barash PG, Deutsch S, Tinker JH, editors. ASA Refresher Course. Vol. 19. Lippincott; 1991. [Google Scholar]
- 19.Gupta N, Garg R, Saini S, Kumar V. GlideScope video laryngoscope-assisted nasotracheal intubation by cuff-inflation technique in head and neck cancer patients. Br J Anaesth. 2016;116:559–60. doi: 10.1093/bja/aew042. [DOI] [PubMed] [Google Scholar]
- 20.Nikhar SA, Sharma A, Ramdaspally M, Gopinath R. Airway management of patients undergoing oral cancer surgery:A retrospective analysis of 156 patients. Turkish J Anaesthesiol Reanim. 2017;45:108–11. doi: 10.5152/TJAR.2017.67365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crosher R, Baldie C, Mitchell R. Selective use of tracheostomy in surgery for head and neck cancer:An audit. Br J Oral Maxillofac Surg. 1997;35:43–5. doi: 10.1016/s0266-4356(97)90008-5. [DOI] [PubMed] [Google Scholar]
- 22.Popat M, Mitchell V, Dravid R, Patel A, Swampillai C, Higgs A. Difficult Airway Society Guidelines for the management of tracheal extubation. Anaesthesia. 2012;67:318–40. doi: 10.1111/j.1365-2044.2012.07075.x. [DOI] [PubMed] [Google Scholar]
- 23.Xue FS, Liu YY, Li HX, Yang GZ. Videolaryngoscopy in airway management-what every anesthesiologist should know. J Anesth Perioper Med. 2018;5:23–33. [Google Scholar]