Abstract
Background and Aims:
General anesthesia induces endocrine, immunologic, and metabolic responses. Anesthetic drugs affect endocrine system by changing the level of stress hormones and hemodynamic of the patient . The purpose of this study was to compare the effects of propofol and isoflurane on hemodynamic parameters and stress-induced hormones in laparoscopic cholecystectomy (LC) surgery.
Material and Methods:
Seventy patients of elective LC were included in this study. Patients were randomly divided into two equal groups of 35 patients; group P received propofol (70–120 μg/kg/min) and group I received isoflurane (mac: 1.28%) as anesthesia maintenance. The following parameters were monitored, checked, and recorded from preanesthesia period to 10 min after PACU entry according to a planned method: hemodynamic parameters (heart rate and mean atrial pressure), level of blood sugar, and serum epinephrine level.
Results:
Heart rate and mean atrial pressure changes did not show significant differences between the two groups in all stage (P > 0.05), but isoflurane group tolerated lower fluctuating changes. Blood glucose and serum epinephrine level rise in the isoflurane group were significantly higher than the propofol group (P < 0.05).
Conclusion:
Maintenance anesthesia by inhalation gas base on isoflurane has not shown a significant difference with total intravenous anesthesia base on propofol on hemodynamic parameter. However, propofol has a consistent effect on decreasing stress hormone and suggested for LC surgery.
Keywords: Hemodynamic parameters, isoflurane, laparoscopic cholecystectomy, propofol, stress hormones
Introduction
Recently, among multiple surgical techniques for the treatment of cholelithiasis and cholecystitis, laparoscopic cholecystectomy (LC) is a method of choice.[1] Both neuraxial and general anesthesia are common anesthetic techniques in these patients. Anesthesia for laparoscopic surgery has various physiological changes associated with it, which may lead to hemodynamic instability, increase in intra-abdominal pressure caused by pneumoperitoneum, patient position, and raising Co2 saturation.[2] Following the painful irritations that occur after the induction of anesthesia and during surgery, the person’s stress responses are triggered and choosing a method that minimizes the hormonal fluctuations caused by stress response will be desirable.[3] Todays, one of the important concerns of researchers and doctors involved in this is the search for and testing newer drugs to find a drug with more impact on controlling the increase of inflammatory and stress responses. Epinephrine is a hormonal and neurotransmitter of the endogenous catecholamines’ group, which causes an increase in heart rate, vasoconstriction, and dilatation of airways.[4] After the induction of general anesthesia, to maintain anesthesia, anesthetic gases or intravenous drugs such as propofol are used.
Propofol generates the most pronounced decrease in systemic blood pressure compared with other anesthetics, which, in addition to rapid anesthetic effects and lower side effects, has a faster anesthesia return than other intravenous anesthetics,[5] and is known as the best anesthetic drug for continuous infusion due to its rapid metabolism and the lack of cumulative effects.
Propofol may result in bradycardia, and decrease in blood pressure after induction of anesthesia due to inhibition of the sympathetic nervous system compared to parasympathetic.[6] Isoflurane is a halogenated anesthetic substance that acts on the central nervous system to produce general anesthesia and has faster anesthesia than the previous generations. Isoflurane decreases the mean arterial pressure by increasing the concentration, which is related to the reduction of systemic vascular resistance, rather than the decrease in cardiac output. Because of the negligible effect of isoflurane on the heart, it is suitable for use in patients with previous failure.[7] Main hypothesis of this study is comparison maintenance of inhalation anesthesia with Total intra venous Anesthesia (TIVA). Considering the beneficial effects of both propofol and isoflurane that have been observed so far, we intend to study the effects of these drugs, in the identical BIS, on hemodynamic parameters and inflammatory and stress factors in patients undergoing laparoscopic cholecystectomy surgery.
Material and Methods
Study design
After approving the research in the ethics committee of Jundishapur University of Medical Sciences of Ahvaz (code of ethics: IR.AJUMS.REC.1397.631), registration in Iranian Clinical Trial Website (IRCT2019.222.428.6N1) and obtaining informed consent from the patients, the study was conducted as a single-blind randomized clinical trial. In this study, 70 patients with ASA class I-II, aged 20–60 years old, who were undergoing elective laparoscopic cholecystectomy surgery, were included. Patients were divided into two groups: propofol (n = 35) and isoflurane (n = 35) [Figure 1].
Figure 1.
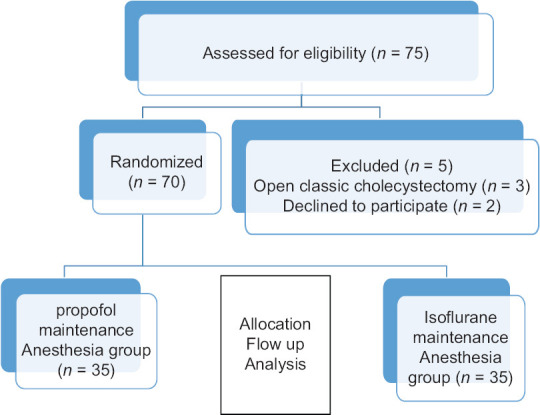
Consort Flow chart of study
Common standard monitoring, including electrocardiogram (ECG), blood pressure monitors, pulse oximetry, and BIS (Cerebral State Monitor. Model CSM 2Danmeter A/S), was performed upon entry to the operating room for patients. Demographic information (age, sex, height, weight) and changes in hemodynamic parameters (MAP, heart rate) and end-tidal Co2 (Capnography Monitor, Model M3B Edan) were recorded. The patients were oxygenated at a rate of 5 liters per minute with 100% oxygen for 3 min. All patients received a combination of midazolam of Chemidarou Iran Co. (0.05 mg/kg), fentanyl of Aburaihan Iran Co. (2 μg/kg), sodium thiopental (Trittau Germany) (mg/kg 4), atracurium (Caspian Tamin) (0.5 mg/kg) for induction and morphine of darupakhsh Iran Co (0.1 mg/kg) was administered for analgesia after induction. The maintenance of anesthesia in propofol group was infusion of propofol (Dongkook pharm. co. ltd Korea) (50–150 μg/kg/min) and in isoflurane group was isoflurane (Aerrane/Puerto Rico) with mac: 1.28% atm/mmHg that was converted into steam using a Drager Medicine device made by Germany and was inhaled via anesthesia machine. Atracurium (0.1 mg/kg) was used alternately every 20 min as a relaxant (36). The depth of anesthesia in both groups was maintained between 45 and 50 BIS through propofol injection and inhalation of isoflurane.
This study was carried out from January 2017 to October 2018 in the Ahvaz Jundishapur University of Medical Sciences at Razi Hospital, IRAN.
Study patients
A total of 70 consecutive patients scheduled for elective laparoscopic cholecystectomy were enrolled. Inclusion criteria: the patients who are not having urgent/emergency surgery, patients with obesity grade II or III (BMI >35), chronic liver disease, diabetes, renal failure, endocrine problems (pheochromocytoma), rheumatic disease, cardiovascular disease or malignancy, egg allergy, patients receiving drugs with known effects on sympathetic response or hormonal secretion such as beta blockers, epinephrine, and insulin, patients consuming benzodiazepines, dextrose serum, and dexmedetomidine, and pregnant or lactating mothers. Exclusion Criteria were: Declined to participate in the study and changing method of surgery to open classic cholecystectomy.
Study variables
Demographic data (age, sex, and body mass index), duration of anesthesia and surgery, patient’s hemodynamic parameters including HR and MAP were recorded during the following stages of the study: preinduction, induction time, and intraoperatively every 5 min till the end of anesthesia and 10 min after PACU entry.
Plasma level of epinephrine and blood glucose (BS) had been measured immediately after induction and at the end of surgery (before reversal of neuromuscular blocked). The questionnaires were completed by an anesthetist researcher who did not know the groups. Epinephrine and glucose level was consider as primary outcomes and hemodynamic parameter as secondary outcomes of this study.
Laboratory measurement
Before and after each surgery, blood samples were collected and plasma was prepared. Epinephrine level was measured by human epinephrine ELISA kit (Taoyuan, Taiwan; Catalog Number: KA1877), with 18 to 6667 pg/ml normal value range. Glucose was measured by a biochemical colorimetric method (karaj, IRAN, parsazmon; Catalog Number: G45215).
Statistical analysis
Categoric variables are reported as percentages, and continuous variables are reported as the mean ± standard deviation or median (interquartile range) as appropriate, attending normal distribution. The assumption of normality was evaluated using the Shapiro–Wilk or Kolmogorov–Smirnov test.
Categoric variables are reported mean ± standard deviation or median (interquartile range) as appropriate, attending normal distribution. Epinephrine and glucose levels were compared using ANOVA and Tukey post-hoc tests. HR and MAP were analyzed by Wilcoxon matched-pairs signed rank test. Data were analyzed using GraphPad prism® version 6.1 software.
Results
A total of 70 patients (each P and I n = 35) were studied. The median age in P group was 54 years (median + IQR, 54 49–58), and I group (median + IQR, 56 48–59). In P group, 60% of the patients (n = 21) and In I group, 67.58% of the patients (n = 24) were female. All of the demographic data are listed in Table 1, and comparison in two groups has not shown any significant value.
Table 1.
Demographic data
| Variables | Propofol (n=35) | Isoflurane (n=35) | P |
|---|---|---|---|
| Gender | |||
| Female | 21 (60%) | 24 (68.57%) | 0.621 |
| Male | 14 (40%) | 11 (31.43%) | |
| Age (year) IQR | 54 (49-58) | 56 (49-59) | 0.532 |
| Height (cm) | 165.71±5.15 | 165.94±5.51 | 0.858 |
| Weight (kg) | 67.06±6.06 | 68.20±7.50 | 0.4857 |
Results of tests showed the level of epinephrine in P group immediately after induction (median + IQR, 49 48–50) and end of surgery (median + IQR, 52 51–53) and in I group immediately after induction [Figure 2a] (median + IQR, 50 49–51) and end of surgery (median + IQR, 61 58–64). Kruskal–Wallis test showed a significant difference between groups (P < 0.0001) and post-hoc (Dunn’s multiple comparisons test) showed a significant difference between immediately after induction P vs. end of surgery P (P < 0.0001), immediately after induction I vs. end of surgery I (P < 0.0001), and end of surgery P vs. end of surgery I (P = 0.0002). Results of tests showed the level of glucose in P group immediately after induction (mean ± SD, 94.60 ± 7.105) and end of surgery (mean ± SD, 105 ± 8.155) and in I group immediately after induction (mean ± SD, 95.54 ± 10.22) and end of surgery (mean ± SD, 109.8 ± 11.10) [Figure 2b]. ANOVA test showed a significant difference between groups (P < 0.0001) and post-hoc (Tukey’s multiple comparisons test) showed a significant difference between immediately after induction P vs. end of surgery P (P < 0.0001) and immediately after induction I vs. end of surgery I (P < 0.0001).
Figure 2.

Changes immediately after induction and end of surgery in two groups under maintenance of anesthetic propofol (P, n = 35) and isoflurane (I, n = 35) administration. a) Plasma level Kruskal–Wallis test analysis (P < 0.0001), (*P < 0.0001,** P < 0.0001, *** P = 0.0002). b) Plasma level of glucose ANOVA analysis (P < 0.0001), (*,** P < 0.0001)
Trends of changes in HR, MAP, and EtCo2 have not shown a significant difference between the two groups of study [Figures 3 and 4]. Repeated measure analysis confirms that there is a significant difference with include time as a factor.
Figure 3.

a Changes in heart rate (HR) in the P group (n = 35,) and the I group (n = 35). Preoperative (-20), operative, and postoperative (PACU) measurements. P = 0.073 (Wilcoxon matched-pairs signed rank test). b Changes in mean arterial pressure (MAP) in the P group (n = 35) and the I group (n = 35). Preoperative (-20), operative, and postoperative (PACU) measurements. P = 0.1228 (Wilcoxon matched-pairs signed rank test)
Figure 4.

End-tidal Co2 form intubation till extubation in two groups of study
Discussion
Epinephrine and glucose
Although surgical techniques have been developed, general stress response is an inseparable part of surgery. This stress is induced by surgical incision and is a complex of reactions that happen in the site of incision such as increases in cAMP, epinephrine, and other catecholamine.[8] This physiologic response reduction is anesthesiology goal for maintaining a patient under stable hemodynamic level during surgery. In molecular view, this response induced biochemical changes such as: epinephrine, norepinephrine, cortisol, ACTH, IL1, and IL6 which are detectable in blood as central compartment of body.[9] Epinephrine is a rational index in surgical stress. LC in comparison to conventional cholecystectomy has low-stress response.[10] According to the study of Glaser et al., different types of cholecystectomy catecholamine have same trend and have a significant low significant amount in catecholamine level.[11] In this study epinephrine level as rational index and glucose as an indirect marker of catecholamine level were measured. Although epinephrine increases were significantly after the LC in both groups of treated, this study confirms that the patients under maintenance of propofol significantly have low-stress profile than isoflurane group. The trends of changes in glucose with a little difference were the same to those of epinephrine. This difference was in comparison level of epinephrine and glucose in end of surgery position. The difference between level blood sugar could be explain by this fact that changes of glucose have very low speed versus epinephrine.
Hemodynamic parameter
The HR level has not a statistically significant difference in all stages of measurement in two groups. The trend of HR changes in both propofol and isoflurane groups was declining for 35 min after intubation, and then it was increasing. HR changes in the isoflurane group were more uniform than those in the propofol group, and the pressure drop was higher in the propofol group up to 15 min after intubation. In the study by Mortazavi et al. (2016) on older patients undergoing upper femoral surgery, there was no significant difference in heart rate between patients receiving propofol and isoflurane,[12] which was consistent with the results of the present study. In the another RCT study in Iran[13], after induction, mean HR significantly decreased in both propofol and isoflurane groups compared to baseline, and remained below baseline until the end of surgery (30). In the present study, in both groups, a significant reduction in mean HR was observed after 15 min of intubation, and although it was again increasing, it remained less than baseline at the end of surgery, which was consistent with the results of the study by Azemati et al. The mean of MAP in any of the steps before and after induction in two groups has not shown a statistically significant difference (P > 0.05). In another study, the mean arterial pressure at 20, 25 and 35 min was significantly lower in the propofol group[12], which was not consistent with the result of the present study in terms of the significance of the difference between the two groups. The mean of MAP in any of the steps before and after induction in both groups has not shown a statistically significant difference (P > 0.05). The trend of MAP changes in the propofol group was reduced for 40 min after intubation and then it was increasing, but 20 min after entering the recovery room, its mean value was significantly less than that before induction (P = 0.046). The trend of MAP changes in the isoflurane group was reduced for 35 min after intubation and then it was increasing, but 20 min after entering the recovery room, its mean value was approximately the same as before induction and did not show significant differences (P = 0.605). In addition, the trend of MAP changes in the isoflurane group was more uniform than that in the propofol group. In the propofol group, the MAP was reduced for 40 min after intubation, and then the increase was accompanied by higher rates [Figure 3]. The results of Mortazavi et al. (2016) showed that in anesthesia with identical bispectral indexes, isoflurane group provides more hemodynamic stability than the propofol group for elderly patients undergoing femoral surgery,[12] which is consistent with the results of the present study in patients undergoing laparoscopic cholecystectomy. In another study, comparing the effect of propofol and sevolfurane on hemodynamic changes in laparoscopic surgeries, there was no significant difference between the two groups in hemodynamic changes[14]. In the study of Azameti et al. (2013), arterial blood pressure was significantly reduced in both propofol and isoflurane groups,[13] which is consistent with the results of this study, in which only the propofol receiving group had a significantly lower MAP at the end of surgery. In the propofol group, the mean of MAP at the end of surgery was significantly lower than baseline and in the isoflurane group, this factor was not significantly different from baseline. After the end of the surgery, the mean blood glucose in the patients receiving propofol was significantly lower than that in the isoflurane group and increased glucose levels in the isoflurane group were significantly higher. In the study of Azemati et al. (2013), glucose was significantly increased in both of propofol and isoflurane receiving groups, but one hour after cutting and one hour after surgery, there was a significant decrease in propofol group[13], which was consistent with the results of the present study. At the end of surgery, the mean epinephrine plasma levels in patients receiving propofol were significantly lower, and increasing in epinephrine levels in the isoflurane group was significantly more than that in the propofol group. In the study of Azemati et al. (2013), in the propofol group, cortisol decreased significantly after an hour of cutting but increased in the isoflurane group. They concluded that the combination of remifentanil and propofol in coping with laparoscopic stress response indexes is more effective than the combination of remifentanil with isoflurane (30), which is consistent with the results of the present study.
Conclusion
Regarding the results of this study and confirmation of the previous studies [Table 2], Making a decision to select maintenance Anesthesia base on propofol has a consistent effect on controlling the release of stress hormones in comparison with inhalation anesthesia based on isoflurane. Although epinephrine level was low in the propofol group, there was not a significant difference in hemodynamic parameter and glucose level in both groups, which is a big controversy. Many factors such as limitation of long-term monitoring, other regulatory processes that affect glucose, and lack of inclusion in diabetic patients caused the controversy. Consistent hemodynamic and lack of significant difference like above but major factor like monitoring depth anesthesia by BIS and documents of both agent effect on cardiovascular could explain that. Finally, with regard to the normal range of results and reported changes in both groups, maintenance of anesthesia based on propofol is appropriate for laparoscopic cholecystectomy and total intravenous anesthesia can be used as selective anesthesia for LC.
Table 2.
Pervious studies
| Type of surgery | Researcher | Year of publication | Variables measured | Anesthesia methods | Results | references | |
|---|---|---|---|---|---|---|---|
| Laparoscopic Surgery | Cholecystectomy | Glaser et al. | 1995 | The level N, E, ACTH, Cortisol LC versus CC | Mixed | LC↓in stress response versus CC | [10] |
| Non- cholecystectomy | Marana et al. | 2010 | N, E, ACTH, Cortisol, GH, PRL, TSH, FT3, FT4 | Induction: STP Maintenance: Propofol vs. sevoflurane |
In propofol group level E↓, Sevoflurane group: E↑ | [15] | |
| Azemati et al. | 2013 | CRP, Glucose, cortisol, HR. MAP | Maintenance: Propofol vs. isoflurane |
In propofol group level E↓, Isoflurane group: E↑ | [13] | ||
| Non- Laparoscopic surgery | Not define type of surgery | Adams et al. | 1994 | N, E, ACTH, Cortisol, ADH, HR and arterial pressure was measured | Induction: STP and Propofol Maintenance: Propofol vs isoflurane |
Level EPI in propofol group significantly was lower | [16] |
| Ihn et al. | 2009 | N, E, ACTH, Cortisol, Glucose and Il-6 | Induction: STP Maintenance: Propofol vs. sevoflurane | Level E and Glucose↑in sevoflurane Level E and Glucose in propofol↑and is lower than sevofluarne |
[17] | ||
| Femoral surgery | Mortazavi et al. | 2016 | HR, MAP | Maintenance: Propofol vs. isoflurane | In propofol HR and MAP↓ | [12] | |
Financial support and sponsorship
This research was supported by grants (Pain-9710) from the Pain Research Center by the Vice Chancellor of Research and Development, Ahvaz Jundishapur University of Medical Sciences (Iran).
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This research was supported by grants (Pain-9710) from the Pain Research Center and Clinical Research Development Center Unit, Imam Khomeini Hospital funded by the Vice Chancellor of Research and Development, Ahvaz Jundishapur University of Medical Sciences (Iran). This study is residency thesis of Dr. Elham Shaida Golbad.
References
- 1.Longo MA, Cavalheiro BT, de Oliveira Filho GR. Laparoscopic cholecystectomy under neuraxial anesthesia compared with general anesthesia:Systematic review and meta-analyses. J Clin Anesth. 2017;41:48–54. doi: 10.1016/j.jclinane.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 2.Hayden P, Cowman S. Anaesthesia for laparoscopic surgery. Continuing education in anaesthesia. Crit Care Pain. 2011;11:177–80. [Google Scholar]
- 3.McCarthy C, Saldova R, Wormald MR, Rudd PM, McElvaney NG, Reeves EP. The role and importance of glycosylation of acute phase proteins with focus on alpha-1 antitrypsin in acute and chronic inflammatory conditions. J Proteome Res. 2014;13:3131–43. doi: 10.1021/pr500146y. [DOI] [PubMed] [Google Scholar]
- 4.Wehrwein EA, Joyner MJ. Regulation of blood pressure by the arterial baroreflex and autonomic nervous system, in Handbook of clinical neurology. Handbook Clin Neurol. 2013;117:89–102. doi: 10.1016/B978-0-444-53491-0.00008-0. [DOI] [PubMed] [Google Scholar]
- 5.Kavakbasi E, Wieneke A, Baune BJEP. Differences in cognitive side-effects and seizure parameters between thiopental and propofol narcosis in ECT. 2021;64:S782–3. doi: 10.1097/YCT.0000000000000893. [DOI] [PubMed] [Google Scholar]
- 6.Ghomeishi A, Mohtadi AR, Behaeen K, Nesioonpour S, Bakhtiari N, Khalvati Fahlyani F. Comparison of the Effect of Propofol and Dexmedetomidine on Hemodynamic Parameters and Stress Response Hormones During Laparoscopic Cholecystectomy Surgery. 2021;11:e119446. doi: 10.5812/aapm.119446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Constantinides C, Mean R, Janssen BJ. Effects of isoflurane anesthesia on the cardiovascular function of the C57BL/6 mouse. ILAR J. 2011;52:e21–31. [PMC free article] [PubMed] [Google Scholar]
- 8.Jóźwiak-Bębenista M, Wiktorowska-Owczarek A, Kowalczyk EJMB. Beta-adrenoceptor-mediated cyclic AMP signal in different types of cultured nerve cells in normoxic and hypoxic conditions. 2016;50:740–7. doi: 10.7868/S0026898416050074. [DOI] [PubMed] [Google Scholar]
- 9.Sawyers JL. Current status of conventional (open) cholecystectomy versus laparoscopic cholecystectomy. Ann Surg. 1996;223:1–3. doi: 10.1097/00000658-199601000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glaser F, Sannwald GA, Buhr HJ, Kuntz C, Mayer H, Klee F, et al. General stress response to conventional and laparoscopic cholecystectomy. Ann Surg. 1995;221:372–80. doi: 10.1097/00000658-199504000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glaser F, Kuntz C, Sannwald GA, Mayer H, Herfarth C. General stress response in laparoscopic and conventional cholecystectomy. Swiss Surg. 1996;(Suppl 4):41–4. [PubMed] [Google Scholar]
- 12.Mortazavi MMT, Niazi GM, Rezapour N, Parish M. Comparison of Hemodynamic changes during general anesthesia with low-dose isoflurane or propofol in elderly patients undergoing upper femoral surgery. J Ardabil Univ Med Sci. 2016;15:360–8. [Google Scholar]
- 13.Azemati S, Savai M, Khosravi MB, Allahyari E, Jahanmiri F. Combination of remifentanil with isoflurane or propofol:Effect on the surgical stress response. Acta Anaesthesiol Belg. 2013;64:25–31. [PubMed] [Google Scholar]
- 14.Tilvawala K.R, P.R Panchotiya. A randomized, comparative study of propofol infusion and sevoflurane as the sole maintenance agent in laparoscopic surgery. Anaesthesia, Pain &Intensive Care. 2017;21:154–158. [Google Scholar]
- 15.Marana E, Colicci S, Meo F, Marana R, Proietti R. Neuroendocrine stress response in gynecological laparoscopy:TIVA with propofol versus sevoflurane anesthesia. J Clin Anesth. 2010;22:250–5. doi: 10.1016/j.jclinane.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Adams H, Schmitz C, Baltes-Götz B. Endocrine stress reaction, hemodynamics and recovery in total intravenous and inhalation anesthesia. Propofol versus isoflurane. Anaesthesist. 1994;43:730–7. doi: 10.1007/s001010050115. [DOI] [PubMed] [Google Scholar]
- 17.Ihn C, Joo JD, Choi JW, Kim DW, Jeon YS, Kim YS, et al. Comparison of stress hormone response, interleukin-6 and anaesthetic characteristics of two anaesthetic techniques:Volatile induction and maintenance of anaesthesia using sevoflurane versus total intravenous anaesthesia using propofol and remifentanil. J Int Med Res. 2009;37:1760–71. doi: 10.1177/147323000903700612. [DOI] [PubMed] [Google Scholar]


