Abstract
Background
To assess the impacts of prolonged protective face masks (PFM) wear on ocular surface symptoms among healthcare professionals (HCPs), and how these symptoms affected PFM wear.
Methods
Thirty-question survey forms were distributed via social media platform to 396 HCPs (110 doctors, 164 nurses, and 122 health technicians) between September 8 and 30, 2021. Participants who could not be reached via social media were given a face-to-face questionnaire. Aside from sociodemographic data, the questionnaire inquired about PFM wear, PFM types, ocular surface symptoms, and how PFM wear has changed during the COVID-19 pandemic.
Results
A total of 74.5% of HCPs reported wearing PFMs, mostly surgical ones (76.8%), for half a day at work but not at home, with redness (29.3%) being the most frequently encountered ocular surface symptom, followed by burning (15.7%), pain (14.1%), tingling (10.9%), and rash (6.6%). The presence of associated restrictions in conjunction with PFM-related ocular symptoms was more likely in dry and hot environments. There was no significant relationship between PFM type, PFM-wearing duration, and HCPs’ daily activities (p > 0.05). Despite the lack of a significant relationship between PFM types and ocular surface symptoms (p > 0.05), there was a significant relationship between PFM-wearing duration and ocular pain (p < 0.05).
Conclusions
PFM-related ocular surface symptoms can be alleviated by properly wearing PFMs, reducing wear time, and using long-acting topical lubricants. This could improve PFM wear compliance, prevent disease transmission, and ultimately help with COVID-19 protection.
Keywords: COVID -19, Healthcare professionals, Ocular symptoms, Protective face masks, Questionnaire
Background
Following the COVID-19 pandemic, the entire world had to adjust to a “new normal,” which included maintaining physical distance, practicing hand hygiene, and wearing protective face masks (PFMs) [1]. Protective face masks of various types have been worn by the general public, aiming to reduce disease transmission by infected individuals and protect the healthy population from infection. Physical distances of ≥ 1.5 m, as well as optimal ocular protection and wearing PFMs in public and healthcare settings, have been shown to decrease COVID-19 infection risk by reducing the spread of contaminated saliva and droplets from infected individuals [2]. However, concerns have been raised about the effectiveness of PFMs in preventing the COVID-19 pandemic from various perspectives. Despite this, the World Health Organization continues to strongly recommend wearing PFMs. It is universally agreed that wearing a PFM, whether cloth, surgical, or respiratory, is preferable to not wearing one [3].
Despite the lack of definitive reports on the ocular effects of the COVID-19 pandemic, cases of conjunctivitis, keratitis, and episcleritis in infected individuals have been reported [4]. Although this virus is not commonly found in tears [5], ocular manifestations such as dry eyes have been observed in COVID-19 patients and may occur prior to the onset of respiratory symptoms [6, 7]. There is, however, very little information available on prolonged PFM-associated dry eye symptoms [8], especially among healthcare professionals (HCPs). The term “mask-associated dry eye (MADE)” refers to an increase in mask-associated dry eye symptoms as the frequency and duration of wearing PFMs increase [9]. Dislodging or improperly wearing PFMs may disperse the air around the eyes, potentially causing rapid tear evaporation [10–12], which may also lead to worsening ocular surface symptoms and increased daily use of lubricants [12]. Despite numerous reports on MADE, objective studies have yet to be published.
Many people complained of dry eye symptoms during the COVID-19 pandemic. This is especially important for HCPs, who frequently work in hospitals and are more vulnerable to transmission risk due to their inability to isolate themselves at home for extended periods of time [13]. During this pandemic, wearing PFMs became more common, paralleling an increase in the number of patients visiting ophthalmology clinics with dry eye complaints.
Thus, the purpose of this study was to assess the impacts of prolonged PFM wear on ocular surface symptoms among HCPs as well as how these symptoms influence mask wear.
Materials and methods
Study design and participants
This cross-sectional questionnaire study included 396 HCPs (110 doctors, 164 nurses, and 122 health technicians) from Afyonkarahisar Health Sciences University Hospital. Thirty-question survey forms, created with “Google Surveys,” were distributed to HCPs as a link through social media platform (WhatsApp) between September 8 and 30, 2021.
The study protocol adhered to the Declaration of Helsinki’s ethical principles and was fully approved by the Afyonkarahisar Health Sciences University Ethics Committee Institutional Review Board with the approval code and date: 2011–KAEK 2/03.09.2021. All participants were called one at a time and informed about the questionnaire, after which their consent was obtained. A face-to-face questionnaire was used after manually obtaining consent from participants who could not be reached through social media platforms.
The questionnaire began with sociodemographic data such as age, gender, and occupation before moving on to questions about PFM wear, PFM types, ocular surface symptoms, and how PFM wear has changed during the COVID-19 pandemic.
Statistical analysis
Data was transferred to the Windows Excel program via Google forms, and statistical analysis was performed using a statistical package for the social sciences, version 26.0 (SPSS Inc., Chicago, IL, USA), assuming that the questionnaires remained true to their original form. Categorical variables were presented as percentages and frequencies. The chi-square test was used to compare categorical variables between groups. The stepwise logistic regression model included descriptive variables that achieved a p-value of less than 0.05 in demographic and univariate analyses.
Results
Demographics
The majority of HCPs (31.8%) ranged in age from 35 to 44 years (Table 1 and Fig. 1). The female-to-male ratio was 49.7/50.3%. A total of 49% of HCPs wore glasses, 50.3% did not, and 0.2% did not specify. There were 19.2% contact lens users and 77.8% non-users, with 3.03% not specifying. 74.5% of participants wore masks for half a day at work but not at home, 17.2% wore masks at work and when in close contact with others, 6.8% wore masks all day, and 1.5% did not specify. 76.8% of HCPs wore surgical masks, 13.6% N95, 6.3% cloth, 1.3% N80, and 1.3% wore N99 (Fig. 2a, b).
Table 1.
Age ranges of the healthcare professionals
| Number of participants (n and %) | Age range (years) |
|---|---|
| 92 (23.2%) | 18–24 |
| 77 (19.4%) | 25–34 |
| 126 (31.8%) | 35–44 |
| 71 (17.9%) | 45–54 |
| 10 (2.5%) | > 55 |
| 20 (5.1%) | Unspecified |
Fig. 1.
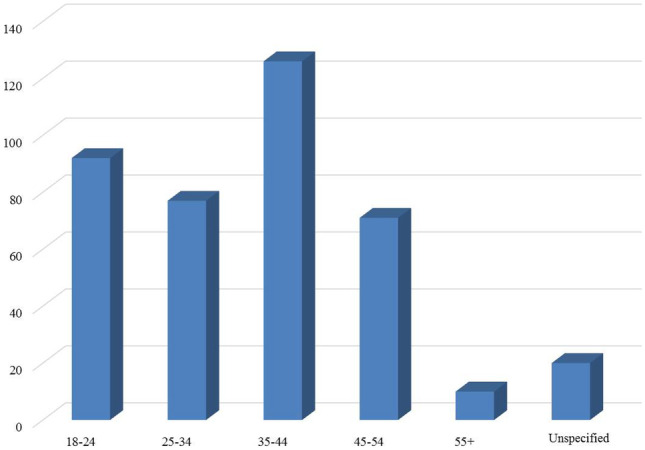
Graphical distribution of the age ranges among healthcare professionals
Fig. 2.
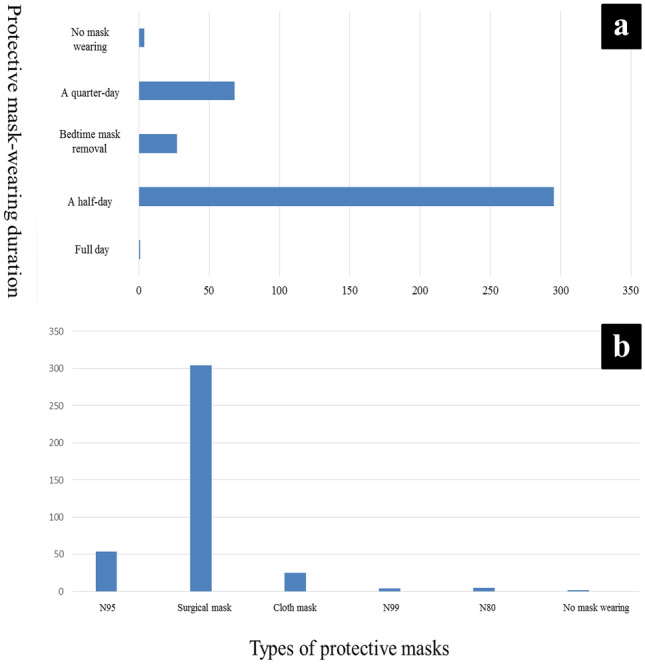
Graphical distribution of a protective face mask-wearing durations, as well as b face mask-wearing behavior and mask types used by healthcare professionals
Ocular surface symptom analysis
Ocular surface symptoms among HCPs who wore PFMs included redness (29.3%), burning (15.7%), pain (14.1%), tingling (10.9%), and rash (6.6%), with 23.5% reporting no symptoms at all (Fig. 3). Analysis of PFM-associated ocular surface symptoms revealed an increased tendency for associated restrictions in conjunction with ocular symptoms in dry and hot environments, airless areas such as elevators, and windy weather. No significant relationship was found between PFM type and activities performed by HCPs, such as night driving, using a computer/TV/mobile phone, being in a dry and hot environment, being in an airless environment such as an elevator, and being in windy weather (p > 0.05). There was also no significant relationship between PFM-wearing duration and the aforementioned types of activities (p > 0.05).
Fig. 3.
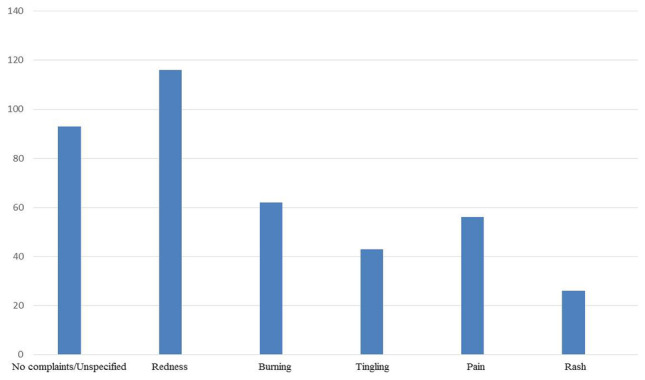
Graphical distribution of ocular surface symptoms among healthcare professionals who wore protective face masks
Further, there was no significant relationship between PFM types and ocular surface symptoms reported by HCPs, such as photophobia, foreign body sensation, decreased vision, redness, pain, itching, and burring (p > 0.05). On the other hand, the assessment of PFM-wearing duration and the aforementioned symptoms revealed a significant relationship between PFM-wearing duration and ocular pain (p < 0.05), but not with other symptoms (p > 0.05).
Discussion
People’s social lives have changed dramatically as a result of the COVID-19 pandemic containment measures. In the early days, when there was no vaccine or approved treatment, unprecedented public health measures, including physical distance, hand hygiene, and the use of personal protective equipment such as PFMs, had to be implemented [14–16]. It is now well established that COVID-19 is primarily transmitted through respiratory droplets during close contact or, in some cases, by aerosol [16]. Although PFM wear is still debatable, experts acknowledge and strongly recommend its importance in preventing disease transmission. This was also true in the current study, where the vast majority of HCPs wore PFMs, with 76.8% being surgical ones.
The current study assessed the impacts of prolonged PFM wear on ocular surface symptoms as well as how these symptoms influenced mask wear among HCPs, the vast majority of whom were < 55 years of age. Protective face mask-wearing duration was found to be significantly related to increased ocular pain. There was also a higher likelihood of associated restrictions in conjunction with ocular surface symptoms in dry and hot environments, airless areas such as elevators, and windy weather. However, PFM-wearing duration, as well as PFM types, had no effect on the daily activities performed by HCPs. The most common symptom among HCPs was PFM-associated ocular redness. However, the ocular surface symptoms were unrelated to PFM type.
Prolonged PFM wear may result in a variety of adverse effects, including increased respiratory resistance, pain and pressure in the nose and ears, a feeling of strain in the temporomandibular joint, itching, as well as ocular discomfort [17–19]. This may be one of the contributing factors that could potentially explain a high prevalence of ocular surface symptoms during the COVID-19 pandemic [10, 20]. An ad hoc survey of university students conducted to investigate the prevalence and risk factors for ocular surface symptoms during the COVID-19 pandemic revealed that increased use of visual display terminals and prolonged PFM wear were the two main reasons. Concentrating on the masks, exhaling with upward airflow or having limited lower eyelid movement may lead to increased tear evaporation, resulting in the onset or worsening of ocular surface symptoms [10].
PFMs have become a new item of clothing in our daily lives as society adapts to the ever changing circumstances surrounding the COVID-19 pandemic. Despite the fact that wearing PFMs on a regular basis may have negative effects on the ocular surface, they have been promoted for safe resocialization. Prolonged PFM wearers, including the elderly, immunocompromised, and medical personnel, are more likely to experience ocular surface symptoms.
This is consistent with the current study, which found that HCPs with no prior dry eye symptoms who were randomly selected from a group of regular PFM users had significantly higher dry eye symptoms and described a subjective worsening of ocular surface symptoms. Prolonged PFM wear is highly probable to result in increased tear film evaporation, which, if continued for hours or days, may cause ocular surface irritation or inflammation, leading to dry eye symptoms. Ocular surface symptoms were also reported by HCPs who used PFMs that were taped to prevent airflow towards the eyes, indicating that there are other potential contributing factors besides airflow. Taping to the upper cheek skin may interfere with normal lower eyelid movement, resulting in evaporative dry eye due to possibly induced mechanical ectropion with secondary lagophthalmos.
There have been no reports of prolonged PFM wear-associated ocular effects in the literature, particularly with respect to HCPs. However, ocular symptoms have been reported, such as exposure to keratopathy caused by lagophthalmos, ectropion, or mechanical ventilation [20, 21]. Dry eye symptoms have been found to be exacerbated by devices such as powered air-purifying respirators that blow air mechanically around the face [22]. Moreover, ocular surface symptoms have been reported in patients wearing chemical protective caps that blow air into the mask [23]. Continuous positive airway pressure masks may also cause ocular discomfort due to air leakage through the nasolacrimal system [12, 23, 24]. Misplacement of a continuous positive airway pressure mask, especially while sleeping, may also result in further dry eye symptoms in eyes with more pronounced airflow [12]. Indeed, among other things, this appears to be evidence that increased airflow has an effect on the ocular surface, though this process has not been fully described from the standpoint of PFM wear.
Dry eye symptoms have recently been reported in COVID-19 positive patients, leading to speculation that these findings, rather than being a complication of the disease [7, 25], may be related to the patients’ compulsory and prolonged PFM wear [8]. Also, due to the unpleasant sensation of airflow into the eyes as a result of continuous PFM wear, frequent eye touch may increase disease transmission [26]. While wearing PFM in public places is required to prevent transmission through the mouth and nose, exposed eyes continue to be a transmission route. The COVID-19 transmission risk via this route may be heightened by PFM-associated ocular surface symptoms. The tear film serves as an important barrier against pathogens; however, wearing PFMs causes this barrier to evaporate faster, significantly reducing the tear film and potentially increasing contamination [27]. Dry eye symptoms may result in increased ocular rubbing and face touching, as well as itching and stinging [26]. All these factors contribute to an increased risk of ocular infections associated with prolonged PFM wear. This risk is especially concerning during the COVID-19 pandemic because ocular transmission is more likely [25, 27]. One survey found that 26.9% of participants with a prior dry eye had worsening symptoms, and 18.3% of the total participants had dry eye symptoms as a result of wearing PFMs [13].
Moreover, dry eye has been reported more commonly in females than in males [28]. No significant difference, however, was found in the current study, which could be attributed to the same environmental factors to which all HCPs were exposed. Further, in the current study, 92.4% of HCPs were under the age of 55 and had never experienced menopause or hormonal effects [29]. The absence of any systemic or dermatological diseases [30, 31] in either male or female HCPs was also considered effective in the current study findings.
Until the COVID-19 pandemic, PFMs were not considered an additional risk factor for ocular surface symptoms. As a result of the pandemic, they are now being used for a longer period of time and have become an indispensable part of our lives and health. Nonetheless, prolonged PFM wear may cause dry eye-like symptoms in people who have no prior dry eye history. In this circumstance, physicians should be cautious and aware, as well as capable of addressing the underlying cause.
The COVID-19 pandemic, as well as the use of PFMs, is anticipated to last for the years ahead. Hence, it is presumed that many people will suffer from ocular surface symptoms as a result of prolonged PFM wear, which may be associated with an increased risk of disease transmission. Confirmation of the current study findings with prolonged PFM-associated ocular surface symptoms in all PFM wearers will necessitate both patient and HCP awareness of the likely consequences. Ophthalmologists, in particular, should consider this possibility, inform patients about preventive ocular care, and, if necessary, organize training. In the current study, nearly half of HCPs wore glasses, with the vast majority not wearing contact lenses. The use of topical lubricants during initial therapy and ocular protection devices may be recommended along with protective PFMs. If ocular surface symptoms deteriorate, the treatment regimen must be modified. Moreover, prolonged PFM wearers are supposed to be highly cautious, as are patients with preexisting dry eye, new eye surgery, or other chronic ocular surface inflammations. Protective face masks with flexible nose wires, with special attention paid to the shape of the mask wire, may be recommended to prevent airflow towards the eyes. In addition to increasing their blinking rate, people experiencing dry eye symptoms as a result of prolonged PFM wear may be recommended to remove PFMs, give some time for the eyes to rest, and apply topical lubricants to preserve tear film every few hours. Above all, the proper PFM wear may provide drug-free relief from ocular surface symptoms.
Conclusions
Being on the frontlines HCPs are frequently at increased risk of COVID-19 exposure. If masks are not properly fitted or hand hygiene is not fully practiced, infected HCPs may also transmit COVID-19 to patients. Prolonged PFM wear by HCPs, on the other hand, has consequences, and it could be one of the factors explaining the high prevalence of ocular surface symptoms during the COVID-19 pandemic. Aside from a significant relationship with increased ocular pain, prolonged PFM-wearing duration was associated with restrictions in conjunction with ocular surface symptoms in dry and hot environments, airless areas such as elevators, and windy weather. Improving prolonged PFM wear-related ocular surface symptoms may be achieved by properly wearing PFMs, shortening PFM wear time, using long-acting topical lubricants before and after PFM wear, and ocular protection devices. This may even significantly raise PFM wear compliance, prevent disease transmission, and eventually aid in COVID-19 protection.
Acknowledgements
The authors would like to thank Sinan SARAÇLI, from Afyon Kocatepe University, Faculty of Science & Literature, Statistics Department, Afyonkarahisar, Turkey, E-mail: ssaracli@aku.edu.tr, for his insightful suggestions and careful reading of the manuscript’s statistical analysis.
Author contributions
All authors contributed significantly to the conception and design of the current study, acquisition, analysis and interpretation of the data, the drafting and essential revision of the manuscript for relevant intellectual content, and the endorsement of the final version of the manuscript.
Availability of data and materials
Data are available from the corresponding author on reasonable request.
Declarations
Ethics approval
The study protocol adhered to the Declaration of Helsinki’s ethical principles and was fully approved by the Afyonkarahisar Health Sciences University Ethics Committee Institutional Review Board with the approval code and date: 2011–KAEK 2/03.09.2021. All participants were called one at a time and informed about the questionnaire, after which their consent was obtained.
Consent to participate
Informed consent was obtained from all participants included in the study.
Conflict of interest
The authors declare no competing interests.
Footnotes
The original online version of this article was revised: Originally, the article was published with an error. The affiliation of the corresponding author Hamidu Hamisi Gobeka should be changed to “Department of Ophthalmology, Faculty of Medicine, Afyonkarahisar Health Sciences University, Afyonkarahisar, Turkey.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/21/2022
A Correction to this paper has been published: 10.1007/s11845-022-03078-8
Contributor Information
Ozgur Erogul, Email: ozgur_erogul@hotmail.com.
Hamidu Hamisi Gobeka, Email: hgobeka@gmail.com.
Murat Kasikci, Email: drmuratk10@gmail.com.
Leyla Eryigit Erogul, Email: eyeleyla@gmail.com.
Aydin Balci, Email: draydnbalc@gmail.com.
References
- 1.Wang C, Horby PW, Hayden FG, et al. A novel coronavirus outbreak of global health concern [published correction appears in Lancet. 2020 Jan 29;:] Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395:1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronavirus disease (COVID-19) advice for the public [Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public
- 4.Zhang X, Chen X, Chen L, et al. The evidence of SARS-CoV-2 infection on ocular surface. Ocul Surf. 2020;18:360–362. doi: 10.1016/j.jtos.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xia J, Tong J, Liu M, et al. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92:589–594. doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen L, Deng C, Chen X, et al. Ocular manifestations and clinical characteristics of 535 cases of COVID-19 in Wuhan, China: a cross-sectional study. Acta Ophthalmol. 2020;98:e951–e959. doi: 10.1111/aos.14472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hong N, Yu W, Xia J et al (2020) Evaluation of ocular symptoms and tropism of SARS-CoV-2 in patients confirmed with COVID-19 [published online ahead of print, 2020 Apr 26]. Acta Ophthalmol 10.1111/aos.14445 [DOI] [PMC free article] [PubMed]
- 8.Moshirfar M, West WB, Jr, Marx DP. Face mask-associated ocular irritation and dryness. Ophthalmol Ther. 2020;9:397–400. doi: 10.1007/s40123-020-00282-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White DE (2020) BLOG: MADE: a new coronavirus-associated eye disease. https://www.healio.com/news/ophthalmology/20200622/blog-a-new-coronavirusassociated-eye-disease
- 10.Giannaccare G, Vaccaro S, Mancini A, et al. Dry eye in the COVID-19 era: how the measures for controlling pandemic might harm ocular surface. Graefes Arch Clin Exp Ophthalmol. 2020;258:2567–2568. doi: 10.1007/s00417-020-04808-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chadwick O, Lockington D. Addressing post-operative mask-associated dry eye (MADE) Eye (Lond) 2021;35:1543–1544. doi: 10.1038/s41433-020-01280-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hayirci E, Yagci A, Palamar M, et al. The effect of continuous positive airway pressure treatment for obstructive sleep apnea syndrome on the ocular surface. Cornea. 2012;31(6):604–608. doi: 10.1097/ICO.0b013e31824a2040. [DOI] [PubMed] [Google Scholar]
- 13.Boccardo L. Self-reported symptoms of mask-associated dry eye: a survey study of 3,605 people [published online ahead of print, 2021 Jan 20] Cont Lens Anterior Eye. 2021;45:101408. doi: 10.1016/j.clae.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kratzel A, Todt D, V’kovski P, et al. Inactivation of severe acute respiratory syndrome coronavirus 2 by WHO-recommended hand rub formulations and alcohols. Emerg Infect Dis. 2020;26:1592–1595. doi: 10.3201/eid2607.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang J, Pan L, Tang S, et al. Mask use during COVID-19: a risk adjusted strategy. Environ Pollut. 2020;266:115099. doi: 10.1016/j.envpol.2020.115099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sommerstein R, Fux CA, Vuichard-Gysin D, et al. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of healthcare workers from COVID-19. Antimicrob Resist Infect Control. 2020;9:100. doi: 10.1186/s13756-020-00763-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kyung SY, Kim Y, Hwang H, et al. Risks of N95 face mask use in subjects with COPD. Respir Care. 2020;65:658–664. doi: 10.4187/respcare.06713. [DOI] [PubMed] [Google Scholar]
- 18.Kainth GS. Novel tip to prevent ear irritation with surgical face masks (FRSM) during the coronavirus (COVID-19) pandemic. Ann R Coll Surg Engl. 2020;102:470–471. doi: 10.1308/rcsann.2020.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang X, Cen X, Liu J. Effect of protraction facemask on the temporomandibular joint: a systematic review. BMC Oral Health. 2018;18:38. doi: 10.1186/s12903-018-0503-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vallabhanath P, Carter SR. Ectropion and entropion. Curr Opin Ophthalmol. 2000;11:345–351. doi: 10.1097/00055735-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Kousha O, Kousha Z, Paddle J. Exposure keratopathy: incidence, risk factors and impact of protocolised care on exposure keratopathy in critically ill adults. J Crit Care. 2018;44:413–418. doi: 10.1016/j.jcrc.2017.11.031. [DOI] [PubMed] [Google Scholar]
- 22.Powell JB, Kim JH, Roberge RJ. Powered air-purifying respirator use in healthcare: effects on thermal sensations and comfort. J Occup Environ Hyg. 2017;14:947–954. doi: 10.1080/15459624.2017.1358817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salinas R, Puig M, Fry CL, et al. Floppy eyelid syndrome: a comprehensive review. Ocul Surf. 2020;18:31–39. doi: 10.1016/j.jtos.2019.10.002. [DOI] [PubMed] [Google Scholar]
- 24.Singh NP, Walker RJ, Cowan F, et al. Retrograde air escape via the nasolacrimal system: a previously unrecognized complication of continuous positive airway pressure in the management of obstructive sleep apnea. Ann Otol Rhinol Laryngol. 2014;123:321–324. doi: 10.1177/0003489414525924. [DOI] [PubMed] [Google Scholar]
- 25.Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138:575–578. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lazzarino AI (2020) Rapid response to: face masks for the public during the COVID-19 crisis. BMJ 369:m1435. https://www.bmj.com/content/369/bmj.m1435/rr-40 [DOI] [PubMed]
- 27.Sun CB, Wang YY, Liu GH, et al. Role of the eye in transmitting human coronavirus: what we know and what we do not know. Front Public Health. 2020;8:155. doi: 10.3389/fpubh.2020.00155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334–365. doi: 10.1016/j.jtos.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 29.Garcia-Alfaro P, Garcia S, Rodriguez I, et al. Dry eye disease symptoms and quality of life in perimenopausal and postmenopausal women. Climacteric. 2021;24:261–266. doi: 10.1080/13697137.2020.1849087. [DOI] [PubMed] [Google Scholar]
- 30.Palamar M, Degirmenci C, Ertam I, et al. Evaluation of dry eye and meibomian gland dysfunction with meibography in patients with rosacea. Cornea. 2015;34:497–499. doi: 10.1097/ICO.0000000000000393. [DOI] [PubMed] [Google Scholar]
- 31.Adiguzel S, Palamar M, Yargucu F, et al. Evaluation of ocular surface and meibomian glands in patients with scleroderma. Cornea. 2021;40(8):977–981. doi: 10.1097/ICO.0000000000002551. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from the corresponding author on reasonable request.


