Abstract
OBJECTIVE
The health care field has been faced with unprecedented challenges during the COVID 19 pandemic. One such challenge was the implementation of enhanced telehealth capabilities to ensure continuity of care. In this study, we aim to understand differences between subspecialties with regard to patient consent and satisfaction following telehealth implementation.
METHODS
A retrospective review of the electronic medical record was performed from March 2 to May 8, 2020 to evaluate surgical consents before and after telehealth implementation. Press Ganey survey results were also obtained both pre- and posttelehealth implementation and compared.
RESULTS
There was no significant difference in the percentage of new patients consented for surgery (after being seen via telehealth only) between the cranial and spine services. For procedures in which >10 patients were consented for surgery, the highest proportion of patients seen only via telehealth was for ventriculoperitoneal shunt placement/endoscopic third ventriculostomy for the cranial service, and lumbar laminectomy and microdiscectomy for the spine service. Additionally, the spine service experienced marked improvement in Press Ganey scores posttelehealth implementation with overall doctor ranking improving from the 29th to the 93rd percentile, and likelihood to recommend increasing from the 24th to the 94th percentile.
CONCLUSIONS
There were clear trends with regard to which pathologies and procedures were most amenable to telehealth visits, which suggests a potential roadmap for future clinic planning. Additionally, the notable improvement in spine patient satisfaction following the implementation of a telehealth program suggests the need for long-term process changes.
Key words: Coronavirus 19 (COVID-19), Neurosurgery subspecialty, Neurosurgery telehealth, Neurosurgery telemedicine, Telehealth, Telemedicine
Abbreviations and Acronyms: COVID-19, Coronavirus 19
Introduction
The integration of telemedicine into modern medical practice has been discussed for years, often in the context of providing care to remote areas with limited resources.1, 2, 3 Although telemedicine has achieved varying levels of success in different subspecialties,4, 5, 6, 7, 8 its widespread integration into neurosurgical practice had yet to occur prior to the coronavirus 19 (COVID-19) pandemic.9 The reasons for this lag in adoption are multiple but are at least partially explained by the inherently physical nature of neurosurgical practice and examination.
With the outbreak of the global COVID-19 pandemic, the entire medical community has been forced to dramatically reconsider our traditional practice patterns. Many of us have realized that it is no longer safe to “lay hands” on every patient that walks through the doors of our emergency rooms, ambulatory centers, and outpatient clinics. Therefore telemedicine, once considered an afterthought, is increasingly being viewed as an integral tool to neurosurgical practice. However, although some may view telemedicine as a temporary “stop-gap” during the global pandemic, it is more likely that there will be a more permanent shift in the way that medicine is practiced. Many will wisely reconsider their traditional practice and adopt some hybrid version with both telemedicine and traditional in-person visits.
Recognizing this reality, our department embarked on an effort to rapidly implement a neurosurgical telehealth program.10 Although Florida did not enact a “shelter in place” order until March 24, our department began scaling back “in-person” clinic activity by the second week of March. This ramp-down also coincided with a University-wide policy of mandated clinic closings, beginning in the third week of March. During this implementation, face-to-face visits were reserved for special cases in which telehealth visits alone were deemed insufficient or not possible. As a part of this implementation, we examined differences between neurosurgical subspecialties. In this manuscript, we present our experience and discuss possible explanations for our findings.
Methods
Data for this manuscript were obtained by performing a chart review of the electronic medical record from March 2, 2020 to May 8, 2020 to determine the number of patients who had been consented for surgery via telehealth during this time along with the type of surgery they were consented for. March 2 was chosen as a reasonable starting time based on the fact that our University had not yet scaled back “in-person” clinic visits at this time. To establish a “pre-COVID” activity level, we queried the clinic activity from March 2019, and used the weekly average clinic volume from this period as our baseline. For the purposes of this analysis, all cranial, neurovascular, and cranial trauma clinic results were bucketed into the “cranial” category. Press Ganey survey results were also obtained for both before and after telehealth implementation. These surveys were aggregated by subspecialty to determine if there were meaningful differences in patient experience both before and after telehealth implementation. We additionally performed a query of our billing system from March 2, 2020 until August 21, 2020 to determine overall trends in telehealth adoption over time.
Results
We have previously published the overall results of our initial telehealth implementation. To summarize these findings, our department experienced a progressive decline in face-to-face clinic visits beginning in the second week of March.10 By the second week of April, the step-off amounted to a 96% decline in baseline activity.10 This amounted to a decrease in face-to-face visits from 414 in the first week of March to 14 visits by the week of April 13th. Concurrently, our efforts to implement a telehealth program allowed a department recapture of 70% of average weekly baseline activity by the fourth week of implementation.10 There was, however, a progressive recovery in face-to-face visits over time, and by the third week of August, in-person visits again accounted for a majority of clinic visits (55%).
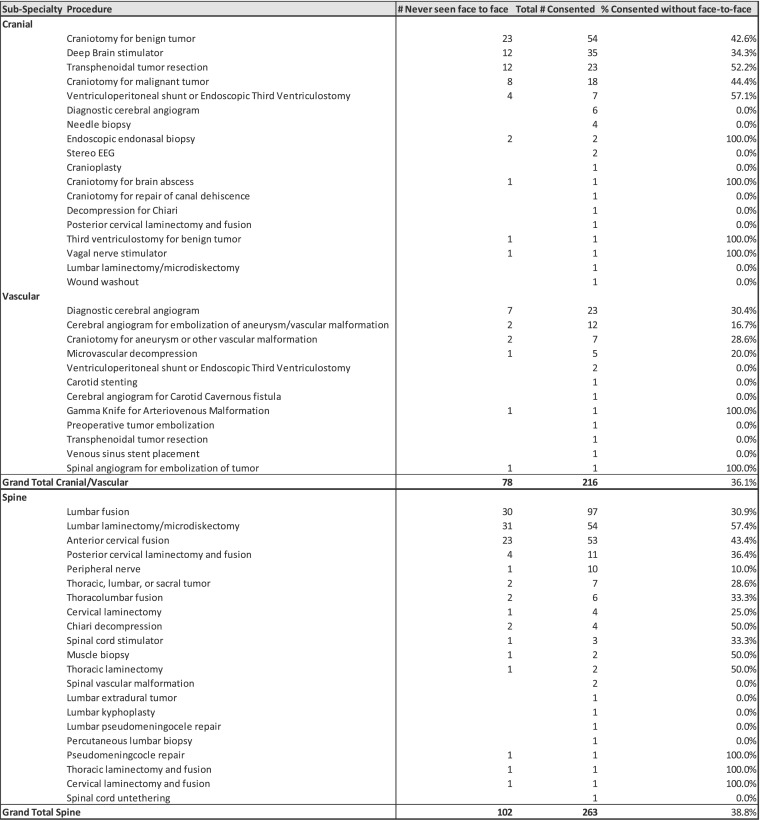
Additionally, although our initial 2 weeks of data collection demonstrated that the cranial service consented a higher proportion of new patients for surgery (seen only via telehealth) than the spine service,10 this difference was nonsignificant after additional data were collected (Figure 1 ). Our latest numbers indicate that cranial service consented 36.1% of patients with only a telehealth visit, whereas the spine service consented 38.8%.
Figure 1.
Breakdown of patients consented for surgery via telehealth by subspecialty and procedure type.
For categories of procedures in which there were >10 patients consented for surgery, the highest proportion of patients seen only via telehealth for the cranial and spine services were for ventriculoperitoneal shunt placement/endoscopic third ventriculostomy, lumbar laminectomy, and microdiscectomy, respectively. The lowest proportion of patients consented after only a telehealth visit for cranial, and spine services were seen for deep brain stimulator placement and peripheral nerve procedures.
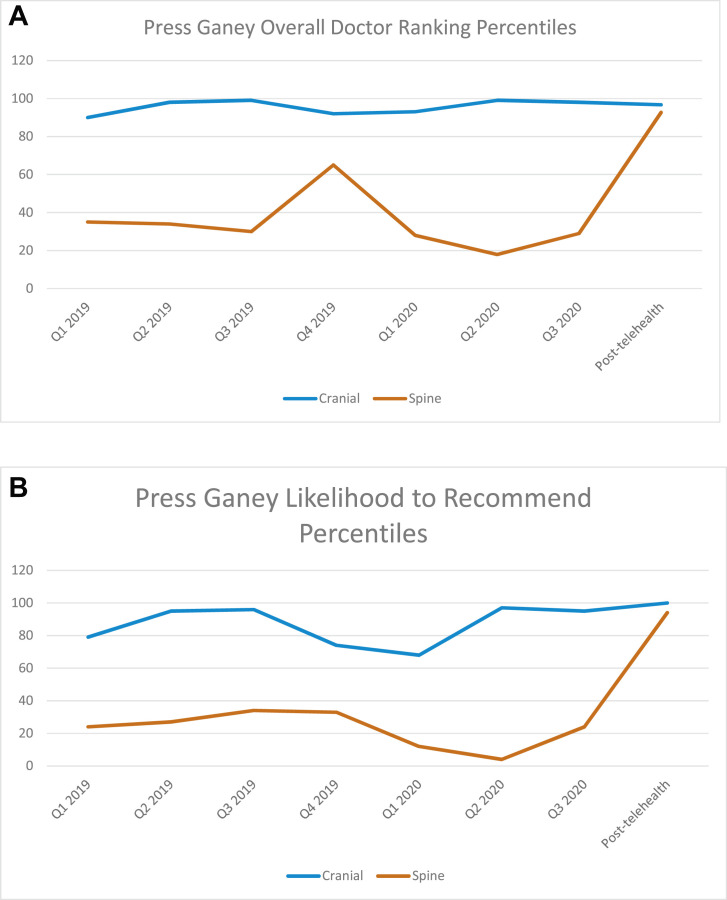
With regard to Press Ganey results, the cranial service did not see large changes in either overall doctor ranking or likelihood to recommend (Figure 2 ). Specifically, the overall doctor ranking percentile decreased slightly from the third quarter of 2020 to post telehealth implementation from the 98th to 97th percentile. Likelihood to recommend improved from the 95th to the 100th percentile over the same comparison period.
Figure 2.
Press Ganey overall doctor ranking (A), and likelihood to recommend percentiles (B) from the first quarter (Q1) of 2019 to post-telehealth implementation.
The spine service contrastingly experienced large changes in both arenas (Figure 2). Overall doctor ranking improved from the 29th to the 93rd percentile, and likelihood to recommend increased from the 24th to the 94th percentile.
Discussion
The implementation of a comprehensive neurosurgical telehealth program poses a number of unique challenges. We have previously discussed some of these challenges, which include socioeconomic issues, technological challenges, and workflow design.10 In our initial analysis of our telehealth implementation, we also noted clear differences between the cranial and spine services in terms of their ability to recapture clinic volume and consent patients for surgery.10 In this manuscript, we aimed to more closely examine these differences by performing an in-depth analysis of types of procedures consented via telehealth, and perhaps most interestingly, by including patient feedback via Press Ganey surveys.
Although our initial research had found the cranial service consenting a larger percentage of patients with telehealth only visits,10 this difference was minimal with additional data collection. Perhaps more compelling are the findings regarding which types of procedures were able to be consented via telehealth visits only. For the spine service, as an example, lumbar laminectomies and microdiscectomies represented the highest proportion of patients consented via telehealth without an in-person visit, whereas peripheral nerve patients represented the lowest proportion of patients (for procedures in which >10 total consents were performed). These findings intuitively make sense, as lumbar stenosis presents with a classic constellation of symptoms and imaging findings, which can be diagnosed in a relatively straightforward fashion via telehealth. Peripheral nerve injuries, contrastingly, require a detailed and in-person physical examination. It also stands to reason that new cases of peripheral nerve entrapment would be far less likely to seek out care in the midst of a global pandemic.
For the cranial service, the largest percentage of patients consented having been only seen via telehealth (for cases in which >10 total consents were performed) were patients consented for ventriculoperitoneal shunts or endoscopic third ventriculostomy. Again, this logically makes sense, as patients presenting with hydrocephalus (either normal pressure or otherwise) will have a very classic constellation of symptoms along with an extensive previous workup by neurology. Contrastingly, the lowest percentage of patients consented only via telehealth were patients with deep brain stimulation. Again, this finding is in line with the fact that the placement of a deep brain stimulation system requires extensive workup, physical examination, and discussions with the patient.
The Press Ganey surveys yielded incredibly interesting findings as well. There is good evidence in the literature that spine patients, in general, rate their care experience significantly lower than cranial patients.11 , 12 The reasons posited for this are multiple, but may at least partially be owing to the fact that patients with cancer diagnoses are generally more grateful for their care than patients with nononcologic diagnoses.11 Communication with the provider and pain management are 2 other possible explanations for differences in satisfaction between these 2 groups.11 , 13 , 14 In our analysis, we found marked differences in patient satisfaction between the cranial and spine groups prior to the implementation of a telehealth program. Interestingly, however, the implementation of a telehealth program resulted in dramatic improvement in patient satisfaction with the spine surgery providers. Indeed, overall doctor rating and likelihood to recommend increased from the 29th to the 93rd percentile and from the 24th to the 94th percentile, respectively. The cranial service had extremely high baseline satisfaction levels both before and after telehealth implementation, thus improvement in Press Ganey scores by the cranial service would be limited due to a “ceiling” effect. This large increase in spine patient satisfaction deserves close attention, specifically because nothing other than the mechanism of care delivery (from in-person to virtual clinic) was changed. A number of possible explanations for this difference can be implied. First, because there is a known association between pain and patient satisfaction, it is possible that the spine patients appreciated the fact that the visits could be performed in the comfort of their own home, without the need for transportation, ambulation, or long wait times in the clinic setting. Alternatively, it is possible that these patients were appreciative of our efforts to ensure continuity of care even in the midst of a global pandemic. It also may be that overall spine volumes are still down despite the telehealth, and consequently the time dedicated by the health care team to each patient is longer leading to exponential increases in patient satisfaction when compared with overbooked patients in a live clinic setting in the pre-telehealth era.
In general, these findings can help begin to build a road-map of which neurosurgical patients are best served by telehealth visits and which will require in-person encounters as well. This distinction will become increasingly important as we move toward a hybrid in-person and telehealth model. Additionally, the dramatic improvement in spine surgery patient satisfaction suggests the need for further introspection and investigation. If this difference is due to increased convenience and decreased pain associated with clinic visits, we should certainly make concerted efforts to at least prescreen patients via telehealth, and then bring patients to clinic, if needed, for further examination or discussion.
We would, however, be remiss if we did not also address the need for further studies investigating whether telehealth visits inherently exclude certain socioeconomic groups. Indeed, because the very purpose of telehealth is inclusion and increased access to care, any concerted transition to a long-term telehealth model must consider these issues. Likewise, we fully recognize that the integration of telehealth into future clinical practice will require legislation on the state and federal level along with changes to the current reimbursement models.
Conclusions
There are clear subspecialty differences that are critical to consider when implementing a telehealth program. Specifically, it is critical to consider which patients are good candidates for telehealth only visits, and which will require in-person consultation. Furthermore, the improved patient satisfaction experienced during our telehealth era suggests the need for long-term process changes.
CRediT authorship contribution statement
Gregory W. Basil: Writing - original draft, Conceptualization, Writing - review & editing. Daniel G. Eichberg: Writing - original draft, Conceptualization, Writing - review & editing. Maggy Perez-Dickens: Writing - original draft, Conceptualization, Writing - review & editing. Ingrid Menendez: Writing - original draft, Conceptualization, Writing - review & editing. Michael E. Ivan: Writing - original draft, Conceptualization, Writing - review & editing. Timur Urakov: Writing - original draft, Conceptualization, Writing - review & editing. Ricardo J. Komotar: Writing - original draft, Conceptualization, Writing - review & editing. Michael Y. Wang: Writing - original draft, Conceptualization, Writing - review & editing. Allan D. Levi: Writing - original draft, Conceptualization, Writing - review & editing.
Footnotes
Conflict of interest statement: Dr. Levi receives grant support from the NIH/NINDS and the Department of Defense, and teaching honoraria from the AANS and Medtronic. Dr. Basil has direct stock ownership in Kinesiometrics LLC. Dr. Wang is a consultant for DePuy Synthes Spine, K2M, Stryker, and Spineology; he is a patent holder with DePuy Synthes Spine; and he has direct stock ownership in ISD, Kinesiometrics LLC and Medical Device Partners. Dr. Urakov is a consultant for Medtronic. Dr. Ivan is a consultant to and is receiving research funding from Medtronic and the NX Development Corporation.
References
- 1.Fraser H.S., McGrath S.J. Information technology and telemedicine in sub-Saharan Africa. BMJ. 2000;321:465–466. doi: 10.1136/bmj.321.7259.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Higgins C.A., Conrath D.W., Dunn E.V. Provider acceptance of telemedicine systems in remote areas of Ontario. J Fam Pract. 1984;18:285–289. [PubMed] [Google Scholar]
- 3.Casey M., Hayes P.S., Heaney D., et al. Implementing transnational telemedicine solutions: a connected health project in rural and remote areas of six Northern Periphery countries series on European collaborative projects. Eur J Gen Pract. 2013;19:52–58. doi: 10.3109/13814788.2012.761440. [DOI] [PubMed] [Google Scholar]
- 4.Olson C.A., Thomas J.F. Telehealth: no longer an idea for the future. Adv Pediatr. 2017;64:347–370. doi: 10.1016/j.yapd.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 5.Davis P., Howard R., Brockway P. An evaluation of telehealth in the provision of rheumatologic consults to a remote area. J Rheumatol. 2001;28:1910–1913. [PubMed] [Google Scholar]
- 6.Tenforde A.S., Hefner J.E., Kodish-Wachs J.E., Iaccarino M.A., Paganoni S. Telehealth in physical medicine and rehabilitation: a narrative review. PM R. 2017;9:S51–S58. doi: 10.1016/j.pmrj.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 7.Loh P.K., Ramesh P., Maher S., Saligari J., Flicker L., Goldswain P. Can patients with dementia be assessed at a distance? The use of telehealth and standardised assessments. Intern Med J. 2004;34:239–242. doi: 10.1111/j.1444-0903.2004.00531.x. [DOI] [PubMed] [Google Scholar]
- 8.Polisena J., Tran K., Cimon K., et al. Home telehealth for chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Telemed Telecare. 2010;16:120–127. doi: 10.1258/jtt.2009.090812. [DOI] [PubMed] [Google Scholar]
- 9.Kahn E.N., La Marca F., Mazzola C.A. Neurosurgery and telemedicine in the United States: assessment of the risks and opportunities. World Neurosurg. 2016;89:133–138. doi: 10.1016/j.wneu.2016.01.075. [DOI] [PubMed] [Google Scholar]
- 10.Basil G.W., Eichberg D.G., Perez-Dickens M., et al. Letter: Implementation of a neurosurgery telehealth program amid the COVID-19 crisis-challenges, lessons learned, and a way forward. Neurosurgery. 2020;87:E260–E262. doi: 10.1093/neuros/nyaa215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kerezoudis P., Alvi M.A., Ubl D.S., et al. The impact of spine disease, relative to cranial disease, on perception of health and care experience: an analysis of 1484 patients in a tertiary center. J Neurosurg. 2018;129:1630–1640. doi: 10.3171/2017.7.JNS17991. [DOI] [PubMed] [Google Scholar]
- 12.Chen Y.R., Johnson E., Montalvo C., et al. Patient satisfaction and Press Ganey scores for spine versus nonspine neurosurgery clinics. Clin Spine Surg. 2019;32:E188–E192. doi: 10.1097/BSD.0000000000000825. [DOI] [PubMed] [Google Scholar]
- 13.Kliot T., Zygourakis C.C., Imershein S., Lau C., Kliot M. The impact of a patient education bundle on neurosurgery patient satisfaction. Surg Neurol Int. 2015;6(suppl 22):S567–S572. doi: 10.4103/2152-7806.169538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buvanendran A., Fiala J., Patel K.A., Golden A.D., Moric M., Kroin J.S. The incidence and severity of postoperative pain following inpatient surgery. Pain Med. 2015;16:2277–2283. doi: 10.1111/pme.12751. [DOI] [PubMed] [Google Scholar]