Abstract
Objectives
To investigate changes in moderate and vigorous physical activity (PA), and find correlation with psychological well-being and perceived health status in university students prior to versus 4–6 weeks following the outbreak of coronavirus pandemic
Methods
Registered students to the 2020/2021 academic year participated in an online survey representing four Hungarian universities in the framework of “COVID-19 International Student Well-being Study” project. Moderate and vigorous PA were measured with a single question, psychological well-being was evaluated using the Center for Epidemiological Studies − Depression Scale (CES-D) short form and perceived health status on the 11-point Cantril ladder respectively. Statistical analyses were calculated using SPSS 26.0 software
Results
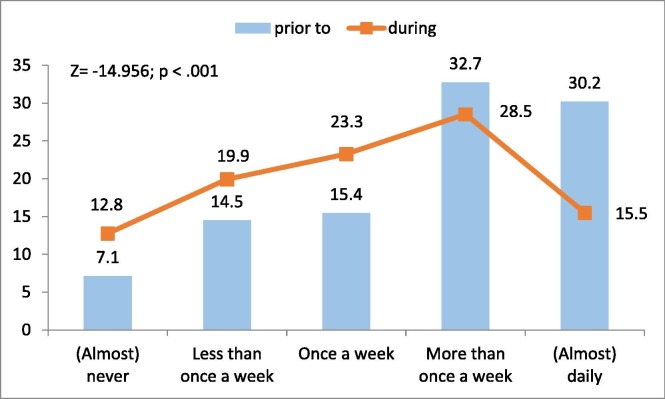
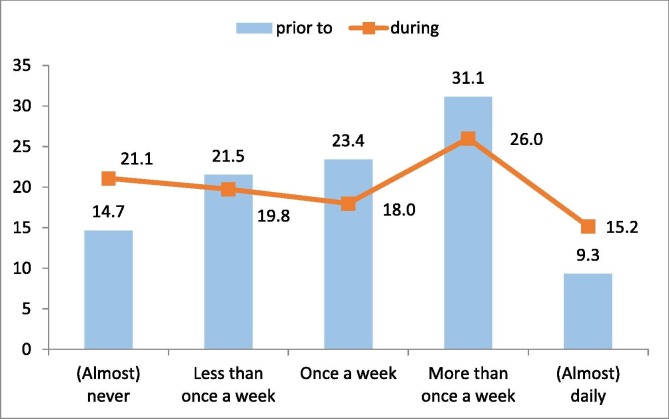
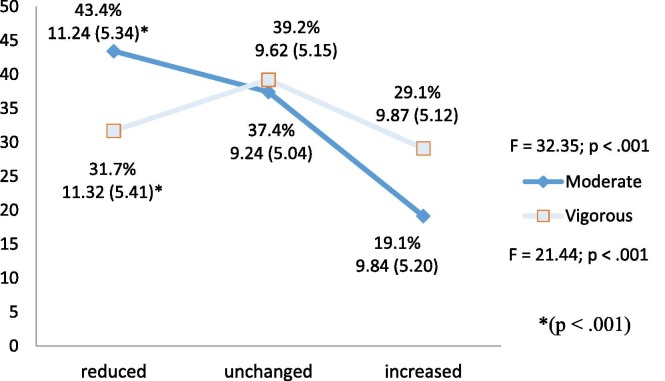
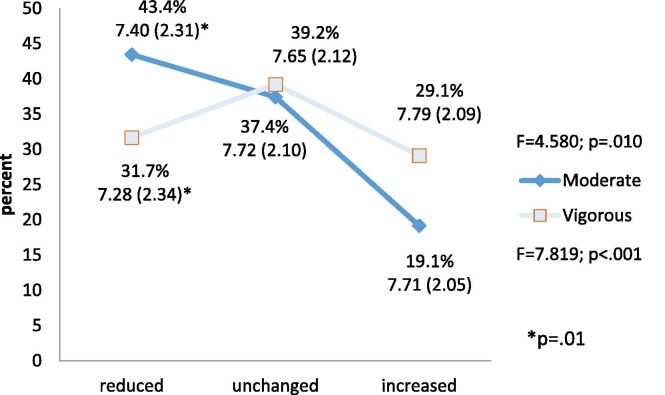
A total of 2779 Hungarian citizen students completed the questionnaire and 2162 (27.7% males) provided full information on PA. Mean age was 24.52 (SD = 7.15) years. A significant decrease was observed in moderate PA prior to and during social isolation (Z = -14.956; p < .001). Students mean well-being was 10.23, SD = 5.28)/32. After analyzing changes (decreased, unchanged, increased) of PA in the context of well-being, it was found students with reduced PA had significantly less favorable scores on well-being scale than students who unchanged or increased their PA level, both in moderate (F = 32.35; p < .001) and vigorous (F = 21.44; p < .001) PA. Regarding the perceived health status there was significant reduction during the pandemic (M = 7.58, SD = 2.19) compared to the preceding period (M = 7.94, SD = 1.85; p < .001). This reduction was most notable in the group that reduced PA
Conclusions
The closure of universities and sport facilities unfavorably influenced the students’ previous PA level. Based on the result, there is a negative relationship between PA and psychological wellbeing also between PA and perceived health status. Universities may pay more attention to keep their students physically active even during a pandemic as it may be far from being over yet.
Keywords: COVID-19, Health, Physical activity, University students, Well-being
1. Introduction
In 2020, the new SARS-CoV-2 infection originated from Vuhan, China developed rapidly into a worldwide epidemic. Governments had to put in place swift measures to counteract the spread of virus. The first case of COVID-19 was reported on March 4, 2020 in Hungary, and the Government implemented various containment measures within a week. Social distance, self-isolation, travel restricting were imposed, stores and services were ordered to close except for essential business and activities. The university campuses and facilities were closed for students and education switched to distance learning. Students had to face various challenges and uncertainties in their life circumstances that can lead to psychological consequences (Liu et al., 2020). Due to academic stressors, university students are considered as vulnerable population for psychological disorders (Sharp and Theiler, 2018, Wörfel et al., 2016). In addition with pre-existing reduced psychological well-being, they are likely to be more susceptible to the negative impact of COVID-19 (Yao et al., 2020, Rajkumar, 2020).
It is well documented in relevant literature that regular physical activity (PA) has an effect on immunity system, infections and inflammation all of that come to the fore during coronavirus pandemic as the virus can cause severe acute respiratory syndrome (Huang et al., 2020, Rothan and Byrareddy, 2020, Mohamed and Alawna, 2020). Furthermore, PA can be a powerful counterbalance against psychological distress (Min et al., 2017, Sheikh et al., 2018) and physical health (Füzéki et al., 2017). Giuntella et al. (2021) evaluated US university students found large disruptions to PA and psychological health before and during the pandemic. Decline in PA was associated with higher depressive symptoms. Interestingly, the restoration of physical activity through a short-term intervention did not improve psychological health, highlighting the importance of maintaining continuous PA during the pandemic. Sallis et al. (2020) pointed out more research is needed on PA during pandemic because of its multiple benefits and calls for immediate action to increase PA during the COVID-19 as the pandemic continues.
Since students are vulnerable to psychological distress, and regular PA can reduce symptoms, it is vital to study how psychological well-being, perceived health status and PA among university students alter during coronavirus pandemic.
The purpose of the study is to investigate changes in moderate and vigorous PA, and find relationship with mental well-being and health in Hungarian university students prior to versus after 4–6 weeks of social distancing orders.
Based on the latest literature on coronavirus, it is hypothesized university students reduce the amount of PA during the coronavirus breakdown (Gallo et al., 2020) (H1); perceive poor physical (H2) and mental health (Dong and Bouey, 2020, Zhai and Du, 2020) (H3), and students who reduce PA have unfavorable scores on well-being scale and perceive poorer health than those who increase or do not change PA (Maugeri et al., 2020) (H4).
2. Material and Methods
2.1. Study design participants and ethics
This study is part of an international project named “COVID-19 International Student Well-being Study” elaborated and conducted by Antwerp University, Belgium. Information about the international study is available on the https://www.uantwerpen.be/en/research-groups/centre-population-family-health/research2/covid-19-internation/ webpage. In this study, data of the Hungarian participants were used in cleaned form sent by the project leaders. Hungarian data collection was conducted between 15 and 28 May 2020, 4–6 weeks after the official university closures due to coronavirus outbreak in Hungary. Four state universities took part in the survey, Corvinus University of Budapest, University of Debrecen, University of Miskolc, and University of Szeged. All the registered students for the 2020/2021 academic year were invited to complete an online questionnaire via Student Administration System accompanied by the students’ personal e-mails. Completion of the questionnaire took 20 min. At the start of the questionnaire a brief description of the study was provided and students were informed about the objectives of the survey, its anonym and voluntary nature. Students agreed to take part in the survey by clicking the consent button.
The research project was approved by the Ethics Committee for the Social Sciences and Humanities in Antwerp (SHW_20_38) and by the institutional ethics committee, the vice-rector for research, the vice-rector for education of all participating universities in Hungary in accordance with the Declaration of Helsinki. The four universities received no financial support for conducting the survey.
2.2. Measures
2.2.1. Sociodemographics
Students provided information on their age, gender, relationship status, educational level, parents’ educational level, and funding of studies.
2.2.2. Physical activity
Two forms of PA (moderate and vigorous) were measured using two single item questions. On average, how often did you perform moderate physical activities like easy cycling or walking for at least 30 min?” On average, how often did you perform vigorous physical activities like lifting weights, running, aerobics, or fast cycling for at least 30 min?” The possible categories for these questions were: “(almost) never”, “less than once a week”, “once a week”, “more than once a week” and “(almost) daily” Students indicated the frequency prior to and during the COVID-19 outbreak. Single item measure is an alternative way to gather information on PA when objective measures or longer self-report measures are not feasible (Milton et al., 2011, O’Halloran et al., 2020).
2.2.3. Mental Well-Being
Mental well-being was measured using the Center for Epidemiological Studies-Depression Scale (CES-D) short form (Van de Velde et al., 2010) originally published by Radloff (1977). Hungarian adaptation of the scale is established in the study of Van de Velde et al. (2010). The scale included 8 items (“you felt depressed”, “you felt everything you did was an effort”, “your sleep was restless”, “you were happy”, “you felt lonely”, “you enjoyed life”, “you felt sad”, “you could not get going”) rated on a 4-point scale from rarely or none of the time (1) to most or all of the time (4). Two items (“you were happy” and “you enjoyed life”) were reversed scored. Answers were summed and the lower scores indicated better well-being, whereas higher scores indicated the presence of more depressive symptomatology (Siddaway et al, 2017). Reliability and validity of the scale in university student population was established by Jiang et al. (2019). Internal consistency coefficient was good in the study population (Cronbach’s alpha = 0.854)
2.2.4. Perceived health status
Perceived health status was measured on Cantril Self-Anchoring Striving Scale (Cantril 1965) where 0 indicates the worst health status, whereas 10 refers to the best status.
2.3. Statistical analyses
Data were analyzed using IBM SPSS version 26 for Windows (IBM Corp., Armonk, NY, USA). The significance level for all analyses was p ≤ 0.05. Descriptive statistics were presented as means and standard deviations (SD) for continuous variables, and as percentage (%) for categorical variables. Wilcoxon signed-rank tests were applied to determine any changes in PA prior to and during COVID-19 outbreak. ANOVA with Tukey post-hoc test was used to find differences among groups (reduced, unchanged and increased PA) in psychological well-being and physical health.
3. Results
3.1. Participants
Database included 2779 questionnaires completed by Hungarian citizens (72.8% females, Mage = 24.45, SD = 6.95), however 617 were discarded due to incomplete information on PA. Student participants studied in different fields of education (30.9% - social sciences, business and law, 21.4% - health and welfare, 16.2% - social and behavioral sciences, 11.1% - engineering, manufacturing and construction, 9.9% - humanities and arts, 5.2% - education, 2.5% - personal services, 1.1% - agriculture, and 1.7% - other). Descriptive statistics of the students are presented in Table 1 .
Table 1.
Descriptive statistics of the study participants (N = 2162).
| Mean (SD), frequency | Participants |
|---|---|
| sample | 2162 |
| Gender – male:female:other (%) | 27.7:71.8:0.5 |
| Age (years) | 24.52 (7.15) |
| Relationship status – single:in relationship:other (%) | 43.6:52.7:3.7 |
| Mother’s education – less than secondary:secondary:higher education:no information (%) | 8.1:45.3:45.9:0.6 |
| Father’s education – less than secondary:secondary:higher education:no information (%) | 10.7:51.5:36.2:1.5 |
| Current educational program – bachelor:master:undivided training:doctoral:other (%) | 60.6:13.1:18.7:3.3:4.3 |
| Funding of studies – state-funded:parents:self-supported:bank loan:scholarship:other (%) | 77.2:6.7:8.9:4.6:1.2:1.4 |
3.2. Change in physical activity
Wilcoxon signed-rank test revealed significant change in moderate PA prior to and during social isolation (Z = -14.956; p < .001). Some negative changes were observed in vigorous PA, however, it was statistically not significant (Z = − 1.551, P = .121). (Fig. 1 and Fig. 2 ) (Supplementary data 1)
Fig. 1.
Change (%) of moderate PA prior to and during pandemic outbreak (N = 2162).
Fig. 2.
Change (%) of vigorous PA prior to and during pandemic outbreak (N = 2162).
3.3. Relationship between well-being and physical activity change
Students’ mean well-being score was 10.23, SD = 5.28 / 32. Both floor and ceiling effects were detectable. (Lower scores indicate favorable well-being.) Analyzing well-being in the context of PA change, it turns out that there are significant differences among groups. ANOVA with Tukey post-hoc test indicated students with reduced moderate and vigorous PA had significantly less favorable well-being scores than students who unchanged (p < .001) or increased their activities (p < .001). (Fig. 3 ) (Supplementary data 2)
Fig. 3.
Relationship between well-being scores (M and SD) and changes in PA (%) (N = 2087).
3.4. Relationship between perceived health status and physical activity change
Significant reduction was observed in students’ mean perceived health status prior to COVID-19 pandemic (M = 7.94, SD = 1.85) compared to the level anticipated after (M = 7.58, SD = 2.19; p < .001). Analyzing health status in the context of PA change, there were no significant differences among groups prior to COVID-19 outbreak (moderate: F = 1.243, p = .289; vigorous: F = 0.213; p = 0.818), however, on the week students completed the survey, significant changes were detected (moderate: F = 4.580p = .010; vigorous: F = 7.819, p < .001). These reductions were more notable in the groups with reduced PA. (Fig. 4 ) (Supplementary data 3)
Fig. 4.
Relationship between perceived health status and moderate and vigorous PA change prior to and during COVID-19 outbreak (N = 1756).
4. Discussion
This study evaluated if there were any changes in the frequency of moderate and vigorous PA before and after the self-confinement orders due to the COVID-19 pandemic, and determined any relationship between PA changes, psychological well-being and perceived physical health status. (H1) In general, a decrease was observed in PA except in everyday vigorous PA where some increase was noticed. It has been previously demonstrated that substantial reduction of PA can be detected in adults (Maugeri et al., 2020, Bourdas and Zacharakis, 2020) and student population (Luciano et al., 2020, Coughenour et al., 2020). The precautionary measures implemented by the government included closure of gym halls, swimming pools, sport and recreational centers not only within university campuses, but also all over the country. As the sport facilities became unavailable, the primary forms of physical exercise were home workout and walking, jogging or running outside. It seems students were not enthusiastic enough to maintain PA based on self-physical literacy (Whitehead, 2001). Without mates to exercise with and without easy accessible sport facilities, students are struggling to maintain the former level of their PA. Nonetheless, there was a small proportion of students who did more vigorous PA in self-confinement than before. Possible reason can be the higher desire and inner motivation to be physically active of these individuals. As they experienced increasing free time due to distance learning they could increase frequency of the regular PA. This result is consistent with findings by Pálvölgyi et al. (2020) noting that a small number of students increased the amount of PA during stay-at-home orders. It is known fact the virus does not spare physically active individuals, however can successfully counteract with the consequences of coronavirus with reducing inflammatory cytokines and chemokines and increasing leukocytes (Matthews et al., 2002). (H2, H3) Findings of this study are in line with previously mentioned studies that coronavirus pandemic, as expected, is detrimental to the students’ physical and mental health. (H4) This study also suggests the reduction of PA level is related to unfavorable psychological well-being and perceived health status. Since the inadequate psychological well-being and health is common in countries affected by the COVID-19 (Alfawaz et al., 2021, Rohde et al., 2020, Vindegaard and Benros, 2020, Ashdown-Franks et al., 2020, Meyer et al., 2020), the positive effects of regular PA on psychological health of university students are indisputable during pandemic. Schuch et al. (2016) in their meta-analyses confirmed and strengthened PA and physical exercise in an evidence-based treatment for depression.
There are some limitations to be taken into considered. First, universities joined on voluntarily basis to the international project “COVID-19 International Student Well-being Study” and only 4 universities took part, yet, they are among the most prestigious ones in Hungary. Psychological well-being was measured during the outbreak of the pandemic, so there was no opportunity to determine the difference between two sets of observations (prior to pandemic versus during). To mitigate self-reported bias in the study, scales and single items were used which were clear and easy to complete and respondents have the ability to answer questions accurately. Pre-pandemic status of PA frequency was retrospectively self-reported, making it prone to recall bias. A 7-day memory recall is considered a normal level of bias especially in the case of university students. Considering this, author relies on accurate answers from the respondents in the study (Podsakoff et al., 2012). The cross-sectional study design precludes causal associations among variables. Despite of these facts, this study gives evidence that closure of universities and self-isolation influence the previous PA habit and detriments mental and physical health in the university student population.
5. Conclusion
Considering the findings of the study and available evidences, closure of sport facilities, and the call for social distancing prevent the majority of university students from maintaining their earlier frequency of PA. These undesirable changes in PA negatively affect the students’ psychological well-being and general self-rated health, suggesting that maintaining or enhancing regular PA during stressful life events such as COVID-19 pandemic is indispensable. In times of worldwide economic downturn, PA is an easy, efficacious and economical way to maintain health and cope with adverse effect of pandemic. Universities should develop effective interventions to increase the level of PA in university population based on the practical guidelines (World Health Organisation., 2020, Ricci et al., 2020, Nyenhuis et al., 2020).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
“This study is part of the COVID-19 International Student Well-Being Study (C19 ISWS). C19 ISWS is the result of a study design, study protocol and questionnaire developed by a team of the University of Antwerp, Belgium (prof. Sarah Van de Velde, dr. Veerle Buffel and prof. Edwin Wouters)“
Footnotes
Peer review under responsibility of King Saud University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jksus.2021.101531.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Alfawaz H.A., Wani K., Aljumah A.A., Aldisi D., Ansari M.G.A., Yakout S.M., Sabico S., Al-Daghri N.M. Psychological well-being during COVID-19 lockdown: Insights from a Saudi State University’s Academic Community. J. King Saud Univ. Sci. 2021;33(1):101262. doi: 10.1016/j.jksus.2020.101262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashdown-Franks G., Firth J., Carney R., Carvalho A.F., Hallgren M., Koyanagi A.i., Rosenbaum S., Schuch F.B., Smith L., Solmi M., Vancampfort D., Stubbs B. Exercise as medicine for mental and substance use disorders: a meta-review of the benefits for neuropsychiatric and cognitive outcomes. Sports Med. 2020;50(1):151–170. doi: 10.1007/s40279-019-01187-6. [DOI] [PubMed] [Google Scholar]
- Bourdas D.I., Zacharakis E.D. Impact of COVID-19 Lockdown on physical activity in a sample of Greek adults. Sports (Basel). 2020;8(10):139. doi: 10.3390/sports8100139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantril H. Rutgers Univ. Press; New Brunswick, NJ: 1965. The pattern of human concerns. [Google Scholar]
- Dong L., Bouey J. Public Mental Health Crisis during COVID-19 Pandemic. China. Emerg Infect Dis. 2020;26(7):1616–1618. doi: 10.3201/eid2607.200407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughenour C., Gakh M., Pharr J.R., Bungum T., Jalene S. Changes in depression and physical activity among college students on a diverse campus after a COVID-19 stay-at-home order. J Community Health. 2020 doi: 10.1007/s10900-020-00918-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Füzéki E., Engeroff T., Banzer W. Health benefits of light-intensity physical activity: a systematic review of accelerometer data of the National Health and Nutrition Examination Survey (NHANES) Sports Med. 2017;47(9):1769–1793. doi: 10.1007/s40279-017-0724-0. [DOI] [PubMed] [Google Scholar]
- Gallo L.A., Gallo T.F., Young S.L., Moritz K.M., Akison L.K. The impact of isolation measures due to COVID-19 on energy intake and physical activity levels in Australian university students. Nutrients. 2020;12(6):1865. doi: 10.3390/nu12061865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuntella O., Hyde K., Saccardo S., Sadoff S. Lifestyle and mental health disruptions during COVID-19. Proceedings of the National Academy of Sciences of the United States of America. 2021;118(9) doi: 10.1073/pnas.2016632118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y.i., Zhang L.i., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L.i., Xie J., Wang G., Jiang R., Gao Z., Jin Q.i., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luciano F., Cenacchi V., Vegro V., Pavei G. COVID-19 lockdown: physical activity, sedentary behaviour and sleep in Italian medicine students. Eur J Sport Sci. 2020;6:1–10. doi: 10.1080/17461391.2020.1842910. [DOI] [PubMed] [Google Scholar]
- Matthews C.E., Ockene I.S., Freedson P.S., Rosal M.C., Merriam P.A., Hebert J.R. Moderate to vigorous physical activity and risk of upper-respiratory tract infection. Med Sci Sport Exerc. 2002;34(8):1242–1248. doi: 10.1097/00005768-200208000-00003. [DOI] [PubMed] [Google Scholar]
- Maugeri G., Castrogiovanni P., Battaglia G., Pippi R., D'Agata V., Palma A., Di Rosa M., Musumeci G. The impact of physical activity on psychological health during COVID-19 pandemic in Italy. Heliyon. 2020;6(6):e04315. doi: 10.1016/j.heliyon.2020.e04315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J., McDowell C., Lansing J., Brower C., Smith L., Tully M., Herring M. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int J Environ Res Public Health. 2020;17(18):6469. doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milton K., Bull F.C., Bauman A. Reliability and validity testing of a single-item physical activity measure. Br J. Sports Med. 2011;45(3):203–208. doi: 10.1136/bjsm.2009.068395. [DOI] [PubMed] [Google Scholar]
- Min J.H., Lee E.Y., Spence J.C., Jeon J.Y. Physical activity, weight status and psychological well-being among a large national sample of South Korean adolescents. Mental Health and Physical Activity. 2017;12:44–49. doi: 10.1016/j.mhpa.2017.02.004. [DOI] [Google Scholar]
- Mohamed A.A., Alawna M. Role of increasing the aerobic capacity on improving the function of immune and respiratory systems in patients with coronavirus (COVID-19): a review. Diabetes Metab Syndr. 2020;14(4):489–496. doi: 10.1016/j.dsx.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyenhuis S.M., Greiwe J., Zeiger J.S., Nanda A., Cooke A. Exercise and fitness in the age of social distancing during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8(7):2152–2155. doi: 10.1016/j.jaip.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Halloran P., Kingsley M., Nicholson M., Staley K., Randle E., Wright A., Bauman A., Weston K.L. Responsiveness of the single item measure to detect change in physical activity. PloS one. 2020;15(6):e0234420. doi: 10.1371/journal.pone.0234420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pálvölgyi Á., Makai A., Prémusz V., Trpkovici M., Ács P., Betlehem J., Morvay-Sey K. A preliminary study on the effect of the COVID-19 pandemic on sporting behavior, mindfulness and well-being. Health Prob Civil. 2020;14(3):157–164. doi: 10.5114/hpc.2020.97898. [DOI] [Google Scholar]
- Podsakoff P.M., MacKenzie S.B., Podsakoff N.P. Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology. 2012;63(1):539–569. doi: 10.1146/annurev-psych-120710-100452. [DOI] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricci F., Izzicupo P., Moscucci F., Sciomer S., Maffei S., Di Baldassarre A., Mattioli A.V., Gallina S. Recommendations for physical inactivity and sedentary behavior during the coronavirus disease (COVID-19) Pandemic. Front Public Health. 2020;8(199):2020. doi: 10.3389/fpubh.2020.00199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde C., Jefsen O.H., Nørremark B., Danielsen A.A., Østergaard S.D. Psychiatric symptoms related to the COVID-19 pandemic. Acta Neuropsychiatr. 2020;32(5):274–276. doi: 10.1017/neu.2020.24. [DOI] [PubMed] [Google Scholar]
- Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis J.F., Adlakha D., Oyeyemi A., Salvo D. An international physical activity and public health research agenda to inform coronavirus disease-2019 policies and practices. J Sport Health Sci. 2020;9(4):328–334. doi: 10.1016/j.jshs.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp J., Theiler S. A review of psychological distress among university students: pervasiveness, implications and potential points of intervention. Int J Adv Counsell. 2018;40(3):193–212. doi: 10.1007/s10447-018-9321-7. [DOI] [Google Scholar]
- Sheikh M.A., Vancampfort D., Stubbs B. Leisure time physical activity and future psychological distress: a thirteen year longitudinal population-based study. J Psychiatr Res. 2018;101:50–56. doi: 10.1016/j.jpsychires.2018.02.025. [DOI] [PubMed] [Google Scholar]
- Siddaway A.P., Wood A.M., Taylor P.J. The Center for Epidemiologic Studies-Depression (CES-D) scale measures a continuum from well-being to depression: Testing two key predictions of positive clinical psychology. J Affect Disor. 2017;213:180–186. doi: 10.1016/j.jad.2017.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch F.B., Vancampfort D., Richards J., Rosenbaum S., Ward P.B., Stubbs B. Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. Journal of psychiatric research. 2016;77:42–51. doi: 10.1016/j.jpsychires.2016.02.023. [DOI] [PubMed] [Google Scholar]
- Van de Velde S., Bracke P., Levecque K., Meuleman B. Gender differences in depression in 25 European countries after eliminating measurement bias in the CES-D 8. Soc Sci Res. 2010;39(3):396–404. doi: 10.1016/j.ssresearch.2010.01.002. [DOI] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehead M. The concept of physical literacy. Phys Educ Sport Pedagogy. 2001;6(2):127–138. doi: 10.1080/1740898010060205. [DOI] [Google Scholar]
- World Health Organisation., 2020. Stay Physically Active during Self-quarantine. Available online at: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/technical-guidance/stay-physically-active-during-self-quarantine (accessed December 4, 2020).
- Wörfel F., Gusy B., Lohmann K., Töpritz K., Kleiber D. Mental health problems among university students and the impact of structural conditions. J Public Health. 2016;24(2):125–133. doi: 10.1007/s10389-015-0703-6. [DOI] [Google Scholar]
- Yao H., Chen J.-H., Xu Y.-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiat. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai Y., Du X. Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Res. 2020;288:113003. doi: 10.1016/j.psychres.2020.113003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.